Академический Документы
Профессиональный Документы
Культура Документы
Translate Jurnal Irolllll
Загружено:
iroelnafialyskaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Translate Jurnal Irolllll
Загружено:
iroelnafialyskaАвторское право:
Доступные форматы
ABSTRACT We describe a child with blunt eye trauma whose eye was saved with appropriate and timely
treatment with emphasis on providing safe environment for children. (Rawal Med J 2012;37:447-448). Key words Secondary amblyopia, traumatic optic neuropathy, glaucoma, cataract. INTRODUCTION Ocular blunt trauma is a common injury in children, and may result in significant unilateral acquired visual loss.1 It is, therefore, an important public health issue. Predisposing factors of eye injury in children includes manner of play, lack of eye protection, and limitations of common sense.2 In pediatric age group, trauma results in visual loss from direct injury to ocular structures or from its complications.3 Common complications of ocular injury are secondary amblyopia, traumatic optic neuropathy, glaucoma and cataract. We report a case of pediatric ocular injury with relatively late presentation to tertiary center. Key words Ocular blunt trauma, hyphema, intraocular pressure, anterior chamber washout. CASE PRESENTATION A 10 year old Malay boy presented with painful and acute onset of deteriorating vision of the left eye following a three day history of trauma with plastic gun pellet at a close range. He went to consult a general practitioner immediately and was only prescribed panadol 500mg. At that time, eye pain was minimal. The pain became rapidly intolerable in next two days, with dramatic reduction in vision. He vomited a few times and reported headache. On examination, there was marked left pupil dilatation, and total hyphema with visual acuity of perception of light (Fig 1). Intraocular pressure was elevated to 48 mm Hg. Reverse relative afferent pupillary defect was present on the affected eye. Fig 1. Anterior segment showing total hyphema.
He was admitted and started on maximum antiglaucoma medications, topical steroids and was started on tranexamic acid 400mg TID. Anterior chamber washout and evacuation of blood clot was performed for recurrent and non resolving hyphaema associated with persistently high intraocular pressure.
Fig 2.Anterior sub capsular cataract noted post-anterior chamber washout
Post operatively, anterior subcapsular cataract and vitreous haemorrhage was noted, (Fig 2), which was managed conservatively on parents request. There was cyclodialysis and traumatic mydriasis. The intraocular pressure remained normal without antiglaucoma medications. His optic disc was pale and final visual acuity was 6/36 on the left eye. DISCUSSION Blunt trauma is commoner in children than penetrating injury and domestic accidents account assessment for the majority of cases.4 Educational background, social and economic status determines the urgency of patients' presentation to hospitals and delay in seeking treatment is common, which results in poorer outcome.5 Parents prefer to consult general practitioners or primary physicians during any medical occurrence. Hence, family physicians are the frontline persons in providing effective initial treatment and advice on safety measures at home for children. Awareness and education among parents are important steps in prevention of ocular trauma and highlighting the consequences of orbital injury in children, which may have longlasting impacts on their future and health. Cautions against toys which may produce detrimental injury need to be forwarded. Children should be supervised at all times and selfprotection needs to be taught. Complications such as traumatic optic neuropathy, hyphema and secondary glaucoma are often difficult to manage. Recurrent hyphema is common among children as they are generally more active and less compliant to confinements of bed rest. Although outpatient management of traumatic hyphema is feasible,6 associated ocular injuries, severe hyphema and pain warrants admission and close observation. Non- resolving hyphema results in rapid elevation of eye pressure and optic nerve compromise.7 Although intraocular pressure may normalize after washout of hyphema, cylodialysis may actually be the cause of 'normal' intraocular pressure. Criteria for surgical intervention of hyphema have been proposed.8,9 Rapid elevation of intraocular pressure in association with increasing hyphaema is an ocular emergency.10 In children and the young, more aggressive measure is indicated in view of development of amblyopia and long term debilitating effect on vision. Secondary glaucoma, vitreous hemorrhage and traumatic optic, neuropathy often complicate other direct injury to ocular structure further impeding visual rehabilitation. In summary, traumatic eye injury may result in permanent visual loss with detrimental effects on visual functions. Ophthalmology referral is mandatory for comprehensive and evaluation of the extent of eye injury. Provision of safe environment and increasing awareness among parents regarding preventive measures is important in public health education.
Вам также может понравиться
- Menanti Kemakmuran Negeri: Kumpulan Esai Tentang Pembangunan SosialДокумент2 страницыMenanti Kemakmuran Negeri: Kumpulan Esai Tentang Pembangunan SosialiroelnafialyskaОценок пока нет
- Urnal of Clinical Medicine ResearchДокумент6 страницUrnal of Clinical Medicine ResearchiroelnafialyskaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- British Journal of Sports MedicineДокумент4 страницыBritish Journal of Sports MedicineiroelnafialyskaОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Here's Egg in Your Eye'': A Prospective Study of Blunt Ocular Trauma Resulting From Thrown EggsДокумент5 страницHere's Egg in Your Eye'': A Prospective Study of Blunt Ocular Trauma Resulting From Thrown EggsiroelnafialyskaОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Pityriasis RoseaДокумент2 страницыPityriasis RoseairoelnafialyskaОценок пока нет
- Cardiovascular Examination Part 2Документ56 страницCardiovascular Examination Part 2iroelnafialyskaОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Pemeriksaan Abdomen: Dr. Suhaemi, SPPD, FinasimДокумент179 страницPemeriksaan Abdomen: Dr. Suhaemi, SPPD, FinasimiroelnafialyskaОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- South African Family Practice ManualДокумент468 страницSouth African Family Practice ManualMahiba Hussain96% (23)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Sonus CompleteДокумент4 страницыSonus CompleteSonusОценок пока нет
- Triada de CharcotДокумент1 страницаTriada de Charcotdanitza pilcoОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Mechanical AsphyxiaДокумент73 страницыMechanical Asphyxiaapi-61200414Оценок пока нет
- 1.01 Introduction To EpidemiologyДокумент3 страницы1.01 Introduction To EpidemiologyPim AramОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- SenokotДокумент1 страницаSenokotKatie McPeek100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Arogya KavachaДокумент5 страницArogya KavachaiamgodrajeshОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Enterobacter QuizДокумент8 страницEnterobacter QuizDan Paolo Sanchez100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Sonopuls 490 User ManualДокумент57 страницSonopuls 490 User ManualMaryam BushraОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Artificial MethodsДокумент23 страницыArtificial MethodsJanna Broqueza RodriguezОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- NDT 3 429Документ13 страницNDT 3 429Mohammed AldaffaieОценок пока нет
- CHN 1 Week 13 Lecture MHGAPДокумент71 страницаCHN 1 Week 13 Lecture MHGAPAech EuieОценок пока нет
- Steroid Tapering and Supportive Treatment Guidance V1.0 PDFДокумент1 страницаSteroid Tapering and Supportive Treatment Guidance V1.0 PDFNthutagaol TrusОценок пока нет
- SOP 6-Minute-Walk Test 1. General Considerations: 6-Minute Walking Distance: Covered Distance inДокумент5 страницSOP 6-Minute-Walk Test 1. General Considerations: 6-Minute Walking Distance: Covered Distance inadeОценок пока нет
- Comparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewДокумент6 страницComparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- A Drug Is Any Chemical You Take That Affects The Way Your Body WorksДокумент2 страницыA Drug Is Any Chemical You Take That Affects The Way Your Body Worksjulian londoñoОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Biochemistry Importance for NursesДокумент15 страницBiochemistry Importance for NursesJulius Memeg PanayoОценок пока нет
- Figure 3-1 Comparing Typical Effectiveness of Contraceptive MethodsДокумент1 страницаFigure 3-1 Comparing Typical Effectiveness of Contraceptive MethodsNuttiya WerawattanachaiОценок пока нет
- Pain Pada SyringomyeliaДокумент6 страницPain Pada Syringomyeliavico julendiОценок пока нет
- Androgenetic Alopecia and Current Methods of TreatmentДокумент4 страницыAndrogenetic Alopecia and Current Methods of TreatmentPamela TrujilloОценок пока нет
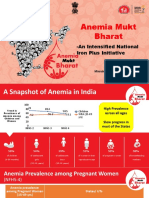
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeДокумент23 страницыAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Yes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtДокумент5 страницYes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtCristian IugaОценок пока нет
- ABO Blood Group SystemДокумент61 страницаABO Blood Group Systemmail2jackal50% (2)
- Health Teaching PPT For HypertensionДокумент13 страницHealth Teaching PPT For HypertensionJeym Quinny ClapanoОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Hensleys Practical Approach To Cardiothoracic Anesthesia Sixth EditionДокумент62 страницыHensleys Practical Approach To Cardiothoracic Anesthesia Sixth Editiontimothy.daniels842100% (39)
- Trauma C1 C2Документ8 страницTrauma C1 C2Karen OrtizОценок пока нет
- Bailey's Othorhinolaryngology and Head and Neck SurgeryДокумент3 775 страницBailey's Othorhinolaryngology and Head and Neck SurgeryDr. Christian Dimitrov92% (12)
- ABG Analysis - 5 Steps ROMEДокумент2 страницыABG Analysis - 5 Steps ROMEKschleseОценок пока нет
- Embryology MCQДокумент10 страницEmbryology MCQTofik MohammedОценок пока нет
- Barrier Free ArchitectureДокумент3 страницыBarrier Free ArchitectureAmarjit SahОценок пока нет