Академический Документы
Профессиональный Документы
Культура Документы
Trauma Thorax
Загружено:
bayuaulАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Trauma Thorax
Загружено:
bayuaulАвторское право:
Доступные форматы
INTRODUCTION
Thank God we pray to God for all His grace and mercy so that I can finish my paper titled "Thoracic Trauma ". Purpose of this paper to meet one of the requirements to follow Kepanitraan Clinic at the RSAU dr. Esnawan Antariksa Jakarta. In this occasion permit the author to express his gratitude to: 1. dr. Aplin Ismunanto, Sp.B as a mentors who have provided guidance on this paper. 2. Friends and all those who have helped in the preparation of this paper. We are fully aware that in the preparation of this case presentation is far from perfect and there are still any mistake that must be fixed. I hope this paper can provide benefits to the reader as well as the development of science, especially in medicine.
Jakarta , 30 July 2013
Bayu Aulia Riensya
CHAPTER I: INTRODUCTION
A. Background Thoracic trauma remains one of the leading causes of death in all age groups with a relatively high incidence, 25-50% of all traumatic injuries (Hunt, Greaves and Owen, 2005). Thoracic injuries ranked third highest in cases of trauma, extremities after injury to the head. The average mortality rate of 10.1%, the highest in patients with cardiac injury or injury-oesophageal trakheobronkhial. Furthermore, the existence of an injury in the setting of thoracic trauma patients multisitemic can significantly increase mortality. Injuries such as flail chest, pulmonary contusion, hemothoraks, and pneumothorax can cause a variety of complications (Kaewlai, Avery, Asrani, and Novelline, 2008). Mostly chest trauma caused by traffic accidents which tend to be particularly sharp trauma. Trauma caused by stab and or shoot. Thoracic injury is often accompanied by abdominal, head, and extremities that are multiple injuries. Many patients died after arriving at the hospital, and many of these deaths could be prevented by improving diagnostic and therapeutic capabilities. Less than 10% of blunt thoracic injuries and only 15-30% of penetrating thoracic injuries requiring thoracotomy measures (American College of Surgeons, 2004). Chest injury requiring emergency action is airway obstruction, massive hemotoraks, cardiac tamponade, pneumothorax, flail chest, open pneumothorax, and tracheal-bronchial air leaks. All of these abnormalities cause severe acute chest or thoracic analogous to acute abdomen, in the sense that the diagnosis should be established as soon as possible and treatment is done immediately to maintain breathing, pulmonary ventilation, and bleeding. Often the actions needed to save the patient is not a surgery, such as aspiration pleural cavity, pericardium cavity aspiration, while closing the chest wound, freeing the airway, pain control, and other supportive care (Lukitto, Rachmad, and Manuaba, 2004; Wanek and Mayberry, 2004).
CHAPTER II: LITERATURE A. Anatomy dan Phisiology Chest containing vital organs, namely the lungs and heart. Breathing takes place with chest wall motion. Lung tissue was formed by millions of alveoli that inflate and deflate depending on expands or shrinks the chest cavity. Inspiration occurs due to contraction of the respiratory muscles, the m. intercostalis and diaphragm, which causes the chest cavity enlarges and expands the lungs so that air sucked into the alveoli through the trachea and bronchi (Lukitto, Rachmad, and Manuaba, 2004). Conversely, if m. intercostalis limp, chest wall shrink back and pushed the air out. Meanwhile, because of intra-abdominal pressure, the diaphragm will rise when m. intercostalis not contracting. The third factor, namely the thoracic wall flexibility, elasticity of lung tissue, and intra-abdominal pressure, causing expiration if the intercostal muscles and diaphragm slack and do not maintain a state of inspiration. Thus, expiration is a passive activity (Lukitto, Rachmad, and Manuaba, 2004). If breathing respiratory muscles fail because it does not work, pulmonary ventilation can be made with a blow strong enough in order to inflate the lungs in thoracic conjunction. Deployment flexibility must exceed the chest wall, lung tissue elasticity, and intra-abdominal pressure. This is done in ventilation with a respirator (Lukitto, Rachmad, and Manuaba, 2004). The existence of a hole in the chest wall or in the visceral pleura will cause air to enter the pleural cavity so that regardless of the visceral pleura and the parietal pleura pulmo no longer involved with the motion of the thoracic wall and diaphragm breathing. This happens in pneumothorax. If that were mounted closed drainage negative pressure, then the air will be sucked and pulmonary expands again (Lukitto, Rachmad, and Manuaba, 2004).
Pictures 2.1. Topografi Thoraks (Martini, 2000)
B.
Patofisiology
Hypoxia, hypercarbia, and acidosis is often caused by thoracic injury, tissue hypoxia is the result of an inadequate transport to the tissue because of hypovolemia (loss of blood), pulmonary ventilation / perfusion mismatch (eg, contusions, hematomas, collapse the alveoli) and changes in intra-thoracic pressure (eg tension pneumothorax, open pneumothorax). Hypercarbia is more often caused by inadequate ventilation due to changes in intrathoracic pressure or decreased level of consciousness. Metabolic acidosis caused by hypoperfusion of tissues (shock) (American College of Surgeons, 2004). C. Mecanism of injury
The most common cause of blunt thoracic trauma are motor vehicle accidents. Although traveling by motor vehicle was more secure in recent decades, at least 44% of the 98,000 accidental injuries in the United States in 2001 due to motor vehicle accidents. In general, the risk of trauma to the thoracic estimated at 7% of serious motor vehicle accidents, and in the United States, at least 1,500 patients per day experienced a life-threatening thoracic trauma from motor vehicle
accidents only. Another mechanism thoracic trauma caused by falls from heights, work injury, and due to violence (Wanek and Mayberry, 2004). Three types of mechanisms that can lead to injury blunt thoracic trauma is compression, cutting, and demolition. Involuntary due to cuts can lead to vascular and soft tissue injury. For response to rapid acceleration or deceleration, movement of organs and soft tissue. Explosion is the mechanism that is deadly, not only because of the blast wave pressure, but also because it can blast victims thrown to great distances and explosion debris objects can poke around victim. Injury primary pulmonary blast pressure wave attack occurs when the chest wall and produce a pressure difference on the surface of the air-pressure difference tissue. The greater involuntary channeled into lung. Severity lung injury depends on the distance of the victim from the source of secondary trauma. Injury generated from moving objects attacking victims of force. Other mekanism are caused by thermal burns and inhalation burns (Wanek and Mayberry, 2004).
D.
Initial Assessment
Principles of initial assessment and management (American College of Surgeons, 2004): 1. Management consists of: a. primary survey b. Resuscitation of vital functions c. Secondary survey d. definitive treatment 2. Because hypoxia is a very serious problem in thoracic injury, early intervention and prevention needs to be done to correct it. 3. Injuries that are life threatening clicking directly, do therapy as quickly and simply as possible. 4. Most cases of life-threatening thoracic injuries treated by controlling the airway or perform hose fitting with thoracic or thoracic needle decompression. 5. Secondary injury history and survey requires high vigilance for the presence of thoracic injury that are special.
E.
Primary Survey:
Primary survey in patients with thoracic injuries begins with airway. The main problem to be corrected once identified (American College of Surgeons, 2004). Management of trauma patients in any still do not forget the principle of initial assessment. Patient circumstances and priorities Assessment based therapy type injury, vital signs, and trauma mechanism. On severely injured patients, therapy should still be given. Vitals sign patient should be assessed quickly and efisient. Manegement patients a rapid primary survey and then resuscitation, secondary survey, and ultimately definitive therapy. This process is ABCDE her trauma, and seeks to identify life-threatening conditions first, sticking to the following sequence (the American College of Surgeons, 2004): 1. Airway
Severe injury on airway should be identified and corrected during the primary survey. Airway patency and ventilation should be judged by listening to the movement of air in the mouth and nose of patients as well as inspections on the chest area for oropharyngeal airway obstruction by a foreign body, and by observing the intercostal muscle retraction and supraclavicular (American College of Surgeons, 2004). Laryngeal injury may coincide with thoracic injuries. Although there are clinical symptoms sometimes not clear, airway obstruction due to laryngeal injury is lifethreatening injuries Some rare conditions that may occur in patients with skeletal injuries that cause significant disruption in the airway and respiratory sufferers. An example is an injury to the upper chest, which causes the direction of posterior dislocation or fracture dislocation of the sternoclavicular joint. This can cause upper airway obstruction that causes dislocation towards the posterior when the displacement of the proximal fragment fracture or distal joint component pressing the trachea. It can also cause injury to the blood vessels in the homolateral extremities due to compression of the fracture fragments or laceration of the main branch of the aortic arch (American College of Surgeons, 2004).
This injury is known if there are upper airway obstruction (stridor), the sign of the change of the sound quality (if the patient is still able to talk), and on the basis of extensive injuries to the neck joints palpable defect in the region strenoklavikular. Handling on this injury is stabilizing patency of the airway, which is best with endotracheal intubation, Altought it may be difficult to do if there is enough pressure on the trachea. Most importantly, closed repositioning of the injuries incurred by the shoulder, lifting the clavicle with a pointed clamp like towel clip and manually repositioning fractures. Injuries like this when done the above measures will usually remain stable even though the patient in a lying position (American College of Surgeons, 2004). 2. Breathing
Neck chest should be open during the assessment of patients breathing and neck veins. Respiratory movements and breathing quality assessed by observation, palpation and be heard. The most important symptoms of thoracic injury is hypoxia, including increased frequency and changes in breathing patterns, especially breathing slowly deteriorating premises. Cyanosis is a further symptom of hypoxia in patients with trauma. But if cyanosis is not found, is not an indication that adequate tissue oxygenation or adequate airway. Types of thoracic injuries that affect breathing is important and circumstances below (American College of Surgeons, 2004): a) Tension pneumothorax
Tension pneumothorax develops when there is a one-way-valve (ventiles phenomenon), air leaks from the lung or from the outside through the chest wall into the pleural cavity and can not get out again. As a result of the incoming air into the pleural cavity that can not get out again, then in intrapleural pressure will be elevated, a collapsed lung, mediastinum pushed to the opposite side and impede venous return of blood to the heart (venous return), and will suppress lateral lung counter. Common cause of tension pneumothorax is a complication of the use of mechanical ventilation (ventilator) with positive pressure ventilation in patients with damage to the visceral pleura. Tension pneumothorax can also arise from simple pneumothorax caused by thoracic injury with a sharp penetrating injury to
the lung parenchyma that did not close after the wrong direction or at the subclavian catheter or internal jugular vein. Sometimes defect or injury to the chest wall can also cause tension pneumothorax if any defect or how close the wound with an airtight bandage occlusive dressings) which will then cause the valve mechanism (flap valve). Tension pneumothorax can also occur in the thoracic spine fracture-shifted (displaced thoracic spine fractures) (American College of Surgeons, 2004). Clinical Manifestations Diagnosis is made clinically tension pneumothorax and treatment should not be delayed by waiting for radiological confirmation. Tension pneumothorax is characterized by symptoms of chest pain, shortness of severe, respiratory distress, tachycardia, hpotensi, tracheal deviation, loss of breath sounds on one side and distended neck veins. Cyanosis is a further manifestation. Because there are similarities between the symptoms of tension pneumothorax and cardiac tamponade often confuse it at first, but the loss of percussion hipersonor and breath sounds on the affected hemithorax in tension pneumothorax will be able to distinguish (American College of Surgeons, 2004). Management Decompression of a tension pneumothorax requires immediate and initial response to the rapid insertion of a large needle in between the ribs two midclavicular line on the affected hemithorax. This action will change the tension pneumothorax into a simple pneumothorax (pneumothorax is likely to occur is increased due to needle insertion. Reassessment is always required. Therapy definitip always needed to put a chest tube (chest tube) between the ribs on the 5th (nipple height) of the anterior from midaxillaris line (American College of Surgeons, 2004).
Gambar 2.2.Tension Pneumothorax (Eyolfson, 2010)
b)
Open pneumotoraks (sucking chest wound)
Defects or major injury to the chest wall will lead to an open pneumothorax. Pressure in the pleural cavity will be equal to atmospheric pressure. If the defect in the chest wall more than 2/3 the diameter of the trachea, the air will tend to flow through a defect because it has prisoner less or smaller than the trachea. As a result, causing impaired ventilation hypoxia and hypercapnia (American College of Surgeons, 2004). Management The initial step is to close the wound with a sterile gauze occlusive plastered only on 3 sides only. With closing expected to occur as the valve effects (flutter valve type) where the time inspiration gauze covering the wound will close, preventing air leakage from inside. Expiratory gauze cover open to get rid of the air out. Then as soon as possible after the chest tube should be placed far away from the primary injury. Cover the entire side of the wound will lead to accumulation of air in the pleural cavity which will cause tension pneumothorax unless the chest tube was inserted. Gauze that can be used while the cover is plastic wrap or petrolatum gauze, so that patients can be evaluated quickly and followed by suturing the wound. Primary wound suturing is often necessary (American College of Surgeons, 2004)
c)
Flail chest
Flail chest occurs when a segment of the chest wall no longer has continuity with the entire chest wall. The situation occurs because of multiple rib fractures in two or more ribs with two or more fracture lines. Presence of flail chest segment (segment float) results in impaired expand of chest wall. If there is damage to the lung parenchyma beneath the chest wall damage it will cause serious hypoxia. The main difficulty in the disorder flail chest injury to the lung parenchyma may occur (pulmonary contusion) (American College of Surgeons, 2004). Clinical manifestations Although chest wall instability causing paradoxical chest wall movement on inspiration and expiration, this defect alone would not cause hypoxia. Hypoxia caused pain resulting in chest wall movement be retained and tissue injury. Flail chest is not visible at first, because of splinting the chest wall. Movement and thoracic breathing becomes bad move asymmetrically and uncoordinated. Abnormal respiratory motion palpation and crepitus or fractured rib cartilage helps diagnosis. With chest X-ray will be seen more clearly because of multiple rib fractures, but the separation of the costochondral joints will not be visible. Examination of the blood gas analysis showed hypoxia due to failure penafasan also help in the diagnosis flail chest (American College of Surgeons, 2004). Management Given initial therapy is the provision of adequate ventilation, humidified oxygen and fluid resuscitation. If no shock then krostaloid intravenous fluid administration should be more careful to prevent excess fluid administration. Parenchymal damage in flail chest will be very sensitive to lack or excess of fluid resuscitation. More specific measurements must be done so that the liquids really optimal. Definitive therapy is intended to develop a lung and adequate oxygenation and fluid administration and analgesia to improve ventilation. Not all patients require the use of a ventilator. Prevention of hypoxia is important in trauma patients, and intubation and ventilation for a short period of time may be required. Until diagnosis and patterns of injury that occurs in these patients complete. Indication of the time to perform intubation and ventilation depends on careful assessment of
respiratory rate, arterial oxygen pressure, and respiratory performance assessment (American College of Surgeons, 2004).
Gambar 2.3. Flail Chest (Wanek dan Mayberry, 2004)
d)
Hemotoraks massive
Accumulation of blood and fluid in one hemithorax may cause business interruptions due to suppression of lung and breathing may inhibit adequate ventilation. Persarahan a lot and will rapidly accelerate the onset of shock and will be discussed further in the discussion of circulation (American College of Surgeons, 2004). 3. Circulation
The pulse of the patient should be assessed the quality, frequency and regularity. In patients with hypovolemia, the pulse of the radial artery and dorsalis pedis artery may be palpated because of its small volume. Blood pressure and pulse pressure should be measured and assessed peripheral circulation through inspection and palpation of skin color and temperature. Neck vein distention should be assessed whether or not. Distended neck veins may be seen in patients with hypovolemia althought no cardiac tamponade, tension pneumothorax or diaphragmatic injury (American College of Surgeons, 2004). Cardiac monitor and pulse oximetry should be installed in people. Patients with suspected thoracic injuries, especially in the sternum area or deceleration injuries are severe myocardial injury should be suspected if there dysrhythmias. Hypoxia or acidosis will facilitate the occurrence. Premature ventricular contractions, dysrhythmias often occur, may require immediate treatment with lidocaine bolus (1mg/kg) followed by lidocaine drip (2-4 mg / min) (American College of Surgeons, 2004). Pulseless Electric Activity (PEA) is a condition in which the ECG rhythm was found, whereas in pulse palpation was not found pulsation. PEA can found in cardiac tamponade, tension pneumothorax, hypovolemia, or worse cardiac rupture (American College of Surgeons, 2004). Thoracic injury that will affect circulation and should be found on primary survey is (American College of Surgeons, 2004): a) Hemotoraks massive
Hemotoraks massive accumulation of blood is quickly more than 1500 cc in the pleural cavity. It is often caused by an injury in penetrating the systemic damage blood vessels or blood vessels in the lung hilum. It can also be caused by blunt
injury. Blood loss causing hypoxia. Neck veins may collapse (flat) due to severe hypovolemia, but can occasionally been recorded distended neck veins, if accompanied by tension pneumothorax. Rare mechanical effects of intrathoracic blood collected is then pushed mediastinum so menyebarbkan distension of the neck veins (American College of Surgeons, 2004). Clinical manifestations Diagnosis is by the shock that accompanied the breath sounds and percussion dullness disappeared on the side of the chest trauma (American College of Surgeons, 2004). Management Initial therapy is massive hemotoraks with blood volume replacement is performed in conjunction with decompression of the pleural cavity. Starting with the rapid infusion of crystalloid fluid with a large needle and then giving blood with spesisfik group immediately. Blood from pleural cavity can be collected in a suitable for autotransfusion. Along with the provision of infusion, a chest tube placed as high as No. 38 F nipples, anterior decompression of the line midaxillaris then immediately pleural cavity. When we suspect hemotoraks massif, consider doing autotransfusion. If at first was out 1500 cc, most likely the patient requires immediate thoracotomy. Some people with blood coming out initially less than 1500 cc, but bleeding persisted. It also requires a thoracotomy. Thoracotomy decisions taken when obtained continuous blood loss of 200 c / h within 2-4 hours, but the physiological status of patients teap precedence. Blood transfusion is needed as long as there indication for thoracotomy. During resuscitated patients, blood volume AWL issued with chest tube and subsequent blood loss should be added to the fluid replacement will be given. The color of blood (arterial or venous) is not a good indicator to be used as the basis for thoracotomy (American College of Surgeons, 2004).
Gambar 2.4.Hemothorax (Eyolfson, 2010) b) Cardiac Tamponade
Often caused by penetrating injuries, blunt injuries but can also lead to better blood filled the pericardium from the heart, large blood vessels, as well as perikard. Pericardial man consists of connective tissue structures are rigid and relatively little thought accumulated blood, but is able to inhibit the activity of the heart and interfere with cardiac filling. Pericardial fluid bleeds or Walalupun only 15-20 cc, already would improve hemodynamics (American College of Surgeons, 2004). Clinical Manifestations Diagnosis of cardiac tamponade is not easy. Diagnosis is the classic triad of Beck that increased venous pressure, arterial pressure, and heart sound away. Assessment of heart sounds away are hard to find when the emergency room in a state crowded, distended neck veins can not be found because of the state of hypovolemia, and hypotension, often caused by hypovolemia. Pulsus paradoxus is a physiological state in which there is a decrease in systolic blood pressure during spontaneous inspiration. When a drop of more than 10 mmHg, then this is another sign of the occurrence of cardiac tamponade, but this sign is not always found. After all if there is a tension pneumothorax on the left side, will greatly with cardiac tamponade.
Kussmaul's sign (increased venous pressure during inspiration usual) is a paradoxical disorder and showed real heart tamonade (American College of Surgeons, 2004). Management Pericardial blood rapid evacuation of an indication if the patient with hemorrhagic shock do not respond to fluid resuscitation and cardiac tamponade may exist. This action saves lives and should never an slowed to hold additional diagnostic examinations. Simple method to remove fluid from perikard round by perikardiosintesis. A high index of suspicion in patients with cardiac tamponade who do not respond to resuscitation efforts, an indication for action perikardiosintesis through subskifoid method. Another alternative is to perform actions surgery or thoracotomy with Pericardial window perikardiotomi by a surgeon. This procedure will be done in the operating room if the condition of the patient allows. Although the suspicion that there is cardiac tamponade, still be giving intravenous fluids will be scaling up early because venous pressure and cardiac output for a while, while making preparations for action perikardiosintesis through subskifoid method. In this action-sheated use plastic or needle insertion with the Seldinger technique is the best way, but in a more serious situation, the priority is the aspiration of blood from Pericardial sac. ECG monitoring can indicate myocardial or the occurrence of dysrhythmias. Because cardiac wound heals by itself, prikardiosintesis will improve symptoms for a while. However, all patients with positive prikardiosintesis necessitates torakotomi or median sternotomi for inspection and repair injured heart. Perikardiosintesis may be negative due to blood clots. For these patients should be prepared to refer to the act of an experienced surgeon (American College of Surgeons, 2004). 4. Disability Towards the end of the primary survey to evaluate the neurological condition rapidly which include level of consciousness, pupil size and reaction, lateralizing signs, and level (level) spinal injury.
5. Exposure / environmental control Patients should be opened the whole clothes, often by cutting, in order to examine and evaluate the patient. After the clothing is opened, patients covered so as not to hypothermia. Blanket used is a warm blanket, the room is warm enough and given intravenous fluids that are heated. During the primary survey, a life-threatening situation should be recognized and carried at the time resusitating. Primary survey is a form of sequential (sequential) order of priority but in practice it is often done at the same time (simultaneously).
F.
SECONDARY SURVEY: THORACIC INJURY POTENTIAL LIFE
THREATENING Secondary survey requires a deeper physical examination and thorough. Upright chest radiograph was made if the patient condition allows, as well as examination of blood gas analysis, monitoring OXYMETRY pulse, and ECG. On chest X-ray should be assessed lung development, the presence of fluid, presence or absence of mediastinal widening. On multiple rib fractures or fractures rib I and / or II should be suspected that the rib injury that occurs in the thoracic and soft tissue beneath very heavy (American College of Surgeons, 2004). Eight thoracic injury that may turn off is a simple pneumothorax, hemotoraks, pulmonary contusions, Tracheo-bronchial branching injury, blunt injury to the heart, aortic injury, injury to the diaphragm, and mediastinal wound transversing. Unlike the immediate life-threatening condition that should be known during the primary survey, usually from injury in the physic examination is unclear. Introduction requires a high index of suspicion. These injuries are often not diagnosed early after injury but can be fatal (American College of Surgeons, 2004). 1. Simple pneumothorax Under normal circumstances the thoracic cavity filled lung development up to the chest wall because of the surface tension (pressure naegatif) between the two pleural surfaces. The presence of air in the pleural space will cause the collapse of the lung tissue. Ventilation-perfusion disturbances occur because the blood had not collapsed lung ventilation so that there is no oxygenation (American College
of Surgeons, 2004). Clinical Manifestations Decreased breath sounds on the affected side and the percussion hipersonor. CXR upright position at the time of expiration will help make the diagnosis (American College of Surgeons, 2004). Management Is the best therapy with chest tube mounting on SIC IV or V, anterior midaxillaris line. When only observed or aspirated, it will pose a risk. Chest tube connected to the WSD and chest radiograph performed again to confirm the re-development of the lung. Or general anesthesia with positive pressure ventilation should not be given to pnderita with traumatic pneumothorax in patients who are at risk or pneumothorax occurs intra opertaif unexpected, until chest tube installed. Simple pneumothorax tension pneumothorax can be life-threatening. Thoracic patients also had didekmpresi before air transportation (American College of Surgeons, 2004). 2004). 1. Hemotoraks
Usually the main cause of lung laceration, laceration darahinterkostal veins or internal mammary artery injury caused by sharp or blunt (American College of Surgeons, 2004). Management Hemotoraks acute enough to be seen on chest radiograph were treated with a chest tube size to remove blood from the pleural cavity, reducing the risk of blood clots, as well as to monitor the subsequent blood loss. When blood is removed from chesttube1,500 cc or more than 200 cc / hour for 2-4 hours, surgical exploration should be considered (American College of Surgeons, 2004). 2. Pulmonary contusions Disorder is most often found in group Potentially lethal chest injury. Breathing failure can arise and evolve slowly with time, so that a definitive treatment plan may change based on rigorous assessment and clinical monitoring should be careful (American College of Surgeons, 2004).
Management Patients with significant hypoxia (PaO 2 <65 mmHg or 8.6 kPadalam room air, SaO2 <90%) should be intubated and given assistance ventilasipada first hours after trauma. Some patients with stable conditions can be treated selectively without endotracheal intubation or mechanical ventilation. Monitoring of blood gas analyzers, pulse OXYMETRY, ECG and respiratory aids required for optimal handling. If the condition of the patient deteriorated and need to be transferred should be performed prior intubation and ventilation (American College of Surgeons, 2004). 3. Tracheo-bronchial branching injury Injured trachea and main bronchi are incredible injuries and potentially fatal is often seen as an initial assessment. This injury is often caused by blunt injury and occurs in 1 inch of the carina. Most people died at the scene. When the patient arrived at the hospital, the risk of increased mortality due to other accompanying injuries (American College of Surgeons, 2004). Clinical Manifestations Often found hemoptysis, subcutaneous emphysema and tension pneumothorax with mediastinal shift. Pneuomotoraks presence with a lot of air bubbles in the WSD after chest tube installed this injury should be suspected. Often it takes more than one chest tube on a large leak. Injury diagnosis is made by bronchoscopy (American College of Surgeons, 2004). Management If suspected tracheobronchial injury, should immediately be consulted. Intubation at the main branch of the contralateral bronchus utamam takes the time to meet the need for oxygenation. Intubation is often difficult because of anatomical distortion due paratracheal hematoma, yangmenyertai oropharyngeal injury or injury to the tracheobronchial own. For such patients required operative treatment immediately. For stable patients, surgical treatment may be delayed until the acute inflammation and edema absorbed (American College of Surgeons, 2004).
4. Blunt cardiac injury This injury can cause the heart muscle contusions, ruptured atrium, or ventricle, or valve leakage. Cardiac chamber rupture is characterized by cardiac tamponade should look out for when the primary survey. Sometimes the signs and symptoms occur when experiencing slow rupture is the atrium (American College of Surgeons, 2004). Clinical manifestations Patients with myocardial contusion will complain discomfort in the chest, but the complaint tersebu can also be caused by chest wall contusion or fracture of the sternum or rib fracture. Definitive diagnosis can only be confirmed by inspection yangmengalami myocardial trauma. Important clinical symptoms of hypotension, conduction disturbances yangjelas on ECG or cardiac wall motion is not normal in two-dimensional echocardiography examination. ECG changes can vary and sometimes showed a clear myocardial infarction. Multiple premature ventricular contractions, sinus tachycardia, which can not be explained, atrial fibrillation, RBBB and ST segment changes on ECG sitemukan often. Troponin examination was not performed on myocardial contusion due to the risk of abnormal conduction acute dysrhythmias, and should be monitored in the first 24 hours, because after the interval, significantly reduced the risk of dysrhythmias (American College of Surgeons, 2004). 2. Ruptur aorta
Traumatic aortic rupture often leads to death shortly after a frontal collision car accident or fall from a height. Patients with aortic rupture, laceration usually happens is not total and close to the ligamentum arteriosum (American College of Surgeons, 2004). Clinical manifestations and diagnosis Often the specific symptoms or signs do not exist, but suspicion over the history of trauma, the force of deceleration and typical radiological findings followed by arteriography is fundamental in determining the diagnosis.
Radiological picture below can be used as an indication of injury to major blood vessels in the thoracic cavity, which is a) Widening of the mediastinum b) obliteration of the aortic arch c) tracheal deviation to the right d) Window aorta-pulmonary artery unclear e) depressed left main bronchus down f) Deviation of the esophagus to the right g) paratracheal widening uneven h) Widening paraspinal i) Pleural / apical cap j) left hemotoraks k) fracture ribs I / II / scapula Management Therapy can be carried out primary suture or resection and mounted aortic graft (American College of Surgeons, 2004). 3. Ruptured diaphragm More often diagnosed on the left side due to obliteration of the liver on the right side, while the diagnosis of intestinal or gastric simplify the left side. Blunt injury produces huge rips cause herniation of abdominal organs. Sharp injuries produce small perforations lamam takes to develop into a diaphragmatic hernia. Diagnosis Diagnosis can be missed if one interprets as a chest X-ray diaphragm elevation, acute gastric dilatation, local or hematoma pnemotoraks subpulmonal. If the suspect left diaphragm laceration, NGT should be installed. If the diagnosis is still not clear, upper gastrointestinal examination. Peritoneal fluid discharge from the chest tube can also confirm the diagnosis. Management Treatment in the form of direct suturing (American College of Surgeons, 2004). 4. Transversing mediastinal wound Penetrance across mediastinal injury could hurt the main structure in the mediastinum.
Diagnosis Diagnosis is made when a thorough physical examination showed radiographic entrance wound in one hemithorax and the exit wound in the contralateral hemithorax. Management Surgical consultation to be conducted. Installation of bilateral chest tubes should be done to overcome hemopneumotoraks and blood that comes out should be measured. Indication of immediate thoracotomy together with an indication for hemotoraks massif. Common therapy should be initiated at the side that lost the most blood. Check the neurological function when the bullet passes the spinal cord (American College of Surgeons, 2004)
G.
OTHER INJURIES THORACIC MANIFESTATION
Other thoracic injuries that must be detected during the secondary survey for a potential worsening although not life threatening are as follows (American College of Surgeons, 2004): 1. Subcutaneous emphysema Can be caused by airway injury, lung parenchyma, or blast injuries. Ika patients using positive pressure ventilation with the chest tube installation considered to be mounted on the side there is a development of emphysema in anticipation of tension pneumothorax (American College of Surgeons, 2004). 2. Traumatic asphyxia Tergencetnya thoracic compression will cause a sudden and temporary to the superior vena cava, causing plethora and petechiae covering the upper body, face and arms. Dpat severe edema. That must be treated is concomitant injury. 3. Fractures of ribs, sternum, and scapula Fracture dapatbersifat costae single or multiple. If multiple, shape and motion of the thoracic may or may not still sufficient. Diagnosis Diagnosis is based on symptoms and signs of pain. Pain may be localized pain, tenderness compression left-right or front-back, and pain in breathing motion. If
multiple fractures, thoracic wall usually remains stable, but if some fractured ribs in two places, a segment of the chest wall can be detached from his unit. Management Fractures costae with chest motion was dealt with adequately or regular analgesic or anesthetic administration. Hars pain eliminated to ensure good breathing or prevent pneumonia caused by respiratory motion is inadequate and impaired cough due to pain. If the administration does not eliminate pain analgesia, intercostal block anesthesia should be performed covering the segments in the caudal and cranial ribs were broken. Installation splint adhesion (adhesive strapping) is not useful though to give a sense of security in people. Adhesion splint will disrupt the development of the chest cavity, disrupting the movement of breath, and can cause dermatitis, whereas in reducing pain is no better than analgesics (Lukitto, Rachmad, and Manuaba, 2004). 4. Blunt injury to esophagus More often caused by a penetrating injury. These injuries are rare but fatal if not identified Clinical manifestations Clinical symptoms such as esophageal rupture after a patient erjadi vomiting. Diagnosis is considered in patients who: a) Suffering hemmotoraks peneumotoraks or left without rib fracture b) Experiencing severe direct injury to the sternum, and the bottom or epigastric pain or shock is not proportional to the injury suffered by c) The rest of the food on the chest tube after the blood out Management Extensive drainage of the pleural cavity and mediastinum with direct suturing of the wound occurs via thoracotomy if possible.
CHAPTER III CONCLUSSION
Thoracic trauma is an injury to the chest, can be caused by blunt cuts or puncture wounds that could cause damage to the organs in the thorax thorax.Trauma unknown (escape) still remains a scourge as the cause of death could have been prevented (preventable death). Based classification is divided into traumatic thoracic trauma caused by compression, explosion / destruction, and trauma caused by deceleration. Assessment of thoracic trauma can be obtained primary survey and secondary survey. Management of thoracic trauma patients initially always a preliminary assessment (initial assessment), especially for airway, breathing and circulation. In patients with thoracic trauma, aggressive treatment should be done with its management and flow depending on the type of trauma. Exact diagnosis is not needed, what is important is the indication for invasive measures. Treatment of thoracic trauma so further divided into conservative or invasive.
REFERENCE
American College of Surgeons Committee on Trauma (ACSCOT). 2008. Rujukan. Dalam: Advanced Trauma Life Support for Doctors, ATLS Student Course Manual . Eight Edition. Chicago. American College of Surgeons. 2004. Cedera Toraks. Dalam: Advanced Trauma Life Support fo Doctors. Chicago. Budiarto, E. 2003.Metodologi Penelitian Kedokteran. EGC, Jakarta. 1-230 hal. Eyolfson, D. 2010. Thoracic Injuries.Paramedic Association of Canada.4-18. Hunt, P.A., I. Greaves, dan W.A. Owens. 2006. Emergency Thoracotomy in Thoracic Trauma-A Review. International Journal of The Care of The Injured. 37: 1-19. Kaewlai, R., L.L. Avery, A.V. Asrani, dan R.A. Novelline. 2008. Multidetector CT of Blunt Thoracic Trauma. Radiographics.28:1555-70. Lukitto, P., K.B. Rachmad, dan T.W. Manuaba. 2004. Dinding Thoraks dan Pleura.Hal. 4040-14. Dalam : W. Karnadihardja, R. Sjamsuhidajat. Dan W. de Jong (Eds.). Buku Ajar Ilmu Bedah.EGC, Jakarta. Martini, Ric. 2000. Fundamentals of Anatomy and Physiology. Pearson Company. Notoatmodjo, Soekidjo. 2005. Metodologi Penelitian Kesehatan. Rineka Cipta, Jakarta. 79. Wanek, S. and J.C. Mayberry. 2008. Blunt Thoracic Trauma. Critical Care Clinics. 20: 71-81.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- SCMS Vol31 No4 Update On The GeneticsДокумент9 страницSCMS Vol31 No4 Update On The GeneticsbayuaulОценок пока нет
- J 1610-0379 2011 07802 XДокумент57 страницJ 1610-0379 2011 07802 XbayuaulОценок пока нет
- Promising Therapies For Treating And/or Preventing Androgenic AlopeciaДокумент8 страницPromising Therapies For Treating And/or Preventing Androgenic AlopeciabayuaulОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Finasteride en Minoxidil EffectenДокумент17 страницFinasteride en Minoxidil EffectenbayuaulОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Lapsus IJD FixedДокумент4 страницыLapsus IJD FixedbayuaulОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- SCMS Vol31 No4 Update On The GeneticsДокумент9 страницSCMS Vol31 No4 Update On The GeneticsbayuaulОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- J 1610-0379 2011 07802 XДокумент57 страницJ 1610-0379 2011 07802 XbayuaulОценок пока нет
- SCMS Vol31 No4 Update On The GeneticsДокумент9 страницSCMS Vol31 No4 Update On The GeneticsbayuaulОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- J 1610-0379 2011 07802 XДокумент57 страницJ 1610-0379 2011 07802 XbayuaulОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- 1750 1172 5 39Документ11 страниц1750 1172 5 39Agus TianaОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Morning Report: TuesdayДокумент40 страницMorning Report: TuesdaybayuaulОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Documents StackДокумент1 страницаDocuments StackDan MОценок пока нет
- Intraosseous InfusionДокумент12 страницIntraosseous InfusionbayuaulОценок пока нет
- CSS Osteoarthritis GenuДокумент33 страницыCSS Osteoarthritis Genufatimah putriОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Neet SSДокумент21 страницаNeet SSVaradharajan VijayakumarОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Mist Rolling in - Issue 1 Portrait)Документ15 страницMist Rolling in - Issue 1 Portrait)mistrollinginОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- SMM3Документ194 страницыSMM3shagggadellicОценок пока нет
- Fragments: On Dentistry. Ander MonsonДокумент23 страницыFragments: On Dentistry. Ander MonsonUrsula Fuentesberain100% (1)
- Ocular Trauma Lecture MBBS by Prof Munim SuriДокумент60 страницOcular Trauma Lecture MBBS by Prof Munim SuriMunim SuriОценок пока нет
- Chest Trauma - PIBДокумент21 страницаChest Trauma - PIBJayarasti KusumanegaraОценок пока нет
- Teaching Plan Wound CareДокумент3 страницыTeaching Plan Wound CareAdrian Savastita82% (11)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- 25 4.3 Connective Tissue Supports and ProtectsДокумент17 страниц25 4.3 Connective Tissue Supports and ProtectsJimmy Jamarolin JacaОценок пока нет
- Surgery McqsДокумент43 страницыSurgery McqsDara Harish100% (4)
- Perfect Workout For WomenДокумент6 страницPerfect Workout For Women-MidsummerMan-100% (6)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Decorative ShibariДокумент97 страницDecorative Shibaripapirología100% (1)
- Assignment 7 PDFДокумент2 страницыAssignment 7 PDFmmОценок пока нет
- English To Serbo-CroatianДокумент12 страницEnglish To Serbo-Croatianm2marijaОценок пока нет
- Basic First AidДокумент27 страницBasic First AidPisethSaoОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Fluid & Electrolytes and Acid Base BalanceДокумент108 страницFluid & Electrolytes and Acid Base Balanceapi-3701489100% (12)
- QLD TheraSuit Info KitДокумент6 страницQLD TheraSuit Info Kitrevcruz100% (2)
- Trauma-Case ScenarioДокумент1 страницаTrauma-Case ScenarioLearsi Ray AfableОценок пока нет
- Cracked Tooth SyndromeДокумент4 страницыCracked Tooth SyndromeANUBHAОценок пока нет
- How To Squat - The Definitive Guide - Stronger by ScienceДокумент95 страницHow To Squat - The Definitive Guide - Stronger by ScienceNilgunОценок пока нет
- Trying: Breaking Dawn: EdwardДокумент13 страницTrying: Breaking Dawn: EdwardAlveera ZafarОценок пока нет
- Wound Dressings Update: Carolina Weller, Geoff SussmanДокумент7 страницWound Dressings Update: Carolina Weller, Geoff SussmanKevin AdrianОценок пока нет
- People v. Ravelo: Facts: The Accused Pedro Ravelo, BonifacioДокумент3 страницыPeople v. Ravelo: Facts: The Accused Pedro Ravelo, BonifacioNathalie Jean Yap100% (1)
- Rosh NeuroДокумент11 страницRosh NeuroSoni AliОценок пока нет
- NES 168 Requirements For Polyvinyl Chloride (PVC) Coated Lead Ballast Blocks Category 3Документ34 страницыNES 168 Requirements For Polyvinyl Chloride (PVC) Coated Lead Ballast Blocks Category 3JEORJEОценок пока нет
- DM GN0001 08 EngДокумент118 страницDM GN0001 08 EngMichael MorrowОценок пока нет
- Spastic ParaplegiaДокумент7 страницSpastic ParaplegiaDio ResnaОценок пока нет
- Housekeeping Injuries: It's Time We Talk About The Elephant in The RoomДокумент4 страницыHousekeeping Injuries: It's Time We Talk About The Elephant in The Roomzoltan2011Оценок пока нет
- Kukishinden Ryu Hanbojutsu Kamae 1. Katate Yaburi No KamaeДокумент7 страницKukishinden Ryu Hanbojutsu Kamae 1. Katate Yaburi No KamaetopolevichОценок пока нет
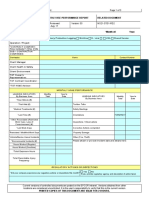
- Monthly Hse Performance Report Related Document: Prime Contractor? Yes NoДокумент3 страницыMonthly Hse Performance Report Related Document: Prime Contractor? Yes NoAKOMOLAFE ABAYOMIОценок пока нет
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)