Академический Документы
Профессиональный Документы
Культура Документы
NCM
Загружено:
CJ AngelesАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
NCM
Загружено:
CJ AngelesАвторское право:
Доступные форматы
Renal Failure the state of total or nearly total loss of kidney function Acute Renal Failure
Acute renal failure (ARF) presents as a rapid decline in renal function, may occur within a few hours or over a period of several weeks Detected by laboratory studies Evidenced by oliguria and elevated blood levels of BUN and creatinine electrolytes and acid-base homeostasis
Categories of ARF ETIOLOGY PRERENAL ARF ------------------------55% Due to diseases that cause renal hypoperfusion without affecting the renal parenchyma (dehydration from fluid loss ,cardiac failure)
Phases of ARF 1. Initiation Period - begins with initial insult to the kidney and ends when oliguria develops 2. OLIGURIC PHASE - Begins when the kidneys are damaged. Typically lasts 10- 15 days to several weeks. Cardinal sign is oliguria (urine output < 400 ml/day) During this phase urine output is low and fluid is retained. Protein is lost because of increased permeability of glomerular membrane, thus fluid diffuses into interstitial tissue Inability to excrete fluid loads Results in fluid overload and edema. This leads to CHF and pulmonary edema. Hypervolemia can lead to hypertension. Oliguria (urine output < 400ml/day) or anuria (< 100 ml/day) Electrolyte imbalances Retention of potassium Metabolic acidosis Potassium imbalance Hyperkalemia, the most sudden hazard in oliguric ARF, exists when the serum K reaches 5.5 or greater. K of 7-10 is incompatible with normal cardiac function In monitoring for signs of K toxicity, the EKG and lab results are the most reliable indicators. Sodium imbalance Hyponatremia develops with overhydration (occurs when the kidney cannot excrete fluid) When the volume of fluid and drugs cannot be reduced to a safe level, dialysis is required to remove excess fluid and restore sodium balance. Signs and sxs of hyponatremia: warm, moist, flushed skin muscle weakness and twitching confusion, delirium, coma, convulsions serum Na concentration < 130 mEq/L
INTRINSIC RENAL ARF ----------------40% Due to diseases that directly involve the renal parenchyma( Glomerulonephritis)
POSTRENAL ARF ------------------------ 5% Due to diseases associated with urinary tract obstruction (enlarged prostate gland, calculus)
Conditions that reduce blood flow to the kidney and impaired kidney function 1. Hypovolemia 2. Hypotension 3. Reduced cardiac output and heart failure 4. Obstruction of the lower urinary tract by tumor, stones, blood clot 5. Bilateral obstruction of the renal arteries or veins Pathophysiology Renal ischemia occurs when blood flow to the kidneys is reduced. The kidney responds with vasoconstriction, further increasing the problem of reduced renal blood flow. Damage to the cells leads to decreased glomerular permeability and tubular obstruction.
decreased Hgb hemodilution
and
Hct
(from
Complete recovery of renal function is slow (may take months)
Metabolic acidosis This occurs when hydrogen ion secretion and bicarbonate ion production diminish in the tubules. The pH of the blood decreases and CNS sxs of drowsiness progressing to stupor and coma may appear. The lungs attempt to compensate with Kussmaul respirations
- Renal function is normal or near normal when the kidney can both concentrate and dilute urine, control serum electrolytes, and excrete nitrogenous wastes. 4. Recovery phase - improvement of renal function - takes about 2- 3 months of recovery - the pt needs to avoid dietary protein. Observe for UTI because infection is a major cause of death in ARF NON - OLIGURIC RENAL FAILURE (High output renal failure) Represents 60% of all renal failures Does not follow the phases of ARF (oliguric, diuretic, recovery) May excrete 2 L/day BUN & creatinine are high, sodium may be high or low Major complication of burns, nephrotic drugs, anesthesia (fluorothane) Chronic Renal Failure A progressive and irreversible decline in renal function ranging from mild with nearly normal function to ESRD requiring renal replacement therapy. results from a prolonged, progressive and irreversible loss of nephron mass irregardless of cause
Inability to excrete metabolic wastes - Renal failure alters the body's ability to eliminate metabolic waste products, producing signs and sxs of uremia. BUN and creatinine values rise sharply. BUN may increase at a rate of 30 mg/dl/day. (Normal 5-20) Signs and sxs: confusion, convulsions, coma, asterixis. N & V, GI bleeding may result from uremic gastritis or colitis. Decreased cellular immunity causes increased risk of infection. Bruising and bleeding from changes in coagulation factors. Pericarditis develops as a result of pericardial irritation from accumulated metabolic wastes. ** If the oliguric phase lasts longer than 2 weeks, prognosis for renal recovery is poor 3. DIURETIC PHASE Marked by increased urine output Indicates the damaged nephrons are healing Within 1-2 days, urine output up to or > 4-5 L/ day may occur
ETIOLOGY 1. 2. 3. 4. Factors affecting the progression of CRF: Modifiable Risk factors: Systemic hypertension Dyslipidemia Hyperglycemia Proteinuria
BUN and creatinine may rise or remain elevated as urine volume increases Hyponatremia, hypokalemia may occur 25% of deaths from renal failure occur during the diuretic phase (from dehydration & shock) This phase may last 10 days - 4-5 L/day.
But remember it is not really "good" urine because the kidney can't concentrate urine as it should. Urine is VERY diluted in this phase.
Diagnostic Findings 1. BUN 2. Creatinine 3. GFR 4. Acidosis 5. Anemia 6. Calcium decreases, Phosphorus is increased PHARMACOLOGICAL THERAPY IN CRF Calcium carbonate
Recombinant erythropoeitin (Epogen or Procrit) Dihydroxyvitamin D3 (Calcitriol,Rocaltrol) Water soluble replacement for dialysis loss (Folate, Vit C & B) Antihypertensive medications Anti seizure agents Avoid magnesium containing antacids Drug dose or interval adjustment is necessary for most drug dependents on renal clearance Schedule daily drugs after dialysis to prevent dialysis loss
DIALYSIS 1. Hemodialysis 2. Peritoneal Dialysis 3. CRRT
KIDNEY TRANSPLANTATION Continuous Renal Replacement Therapies (CRRT) - Similar to hemodialysis - Removes waste product slowly - Requires more time - Used when uric acid needs to be aggressively managed - Offers lower fluid removal and solute clearance rates - Hemodynamic stability is easily attained Hemodialysis
DIAGNOSTIC TEST Abdominal X-ray of the kidneys, ureters and bladder (KUB)- to determine calculi or renal vascular calcification Renal ultrasound- to identify renal vascular blood flow and to rule out obstruction Bladder scan to detect urinary retention Blood chemistries 24-hour urine collection Chest X-ray- to view pulmonary status ECG- determines presence of severe hyperkalemia
Diffusion is the process used to remove toxin and wastes in the blood Ultrafiltration water moves from high pressure to an area of lower pressure - applies suctioning force to the dialysis membrane HEMODIALYZER has Dialysis coil which acts as the semipermeable membrane; DIALYSATE fluid is a special solution containing a premixed concentrate of electrolytes HD treatment lasts for 3-4 hours
NURSING DIAGNOSIS Excess fluid volume related to inability of the kidneys to excrete excess fluid Imbalanced nutrition, less than body requirements, related to anorexia, nausea & vomiting, altered taste sensation Anxiety related to major health, lifestyle, role and financial income Disturbed body image related to visible dialysis access, edema, and skin changes NUTRITION Nurse must asses markers of nutrition Restrictions on fluids/ salts Restriction on protein intake Dialysis Purpose: Remove the end products of protein metabolism from blood Maintain safe levels of electrolytes Correct acidosis and replenish blood bicarbonate system Remove excess fluid from the blood RENAL REPLACEMENT THERAPIES
Hemodialysis DIALYZER Nursing Care: femoral/subclavian cannulation Palpate peripheral pulses in cannulized extremity Observe for bleeding/hematoma formation Position catheter properly to avoid dislodgement during dialysis AV FISTULA NURSING CARE: AVF Confirm patency by palpating thrills and bruits along course of AVF Nephrology precautions Teach patient to avoid constrictive clothing and to check fistula patency daily. Teach patient to handle post treatment bleeding at cannula site: apply direct pressure for several minutes to control bleeding then apply dry dressing VASCULAR ACCESS
Nursing Care: for AV Graft Auscultate for a bruit and palpate for a thrill to ensure patency Assess for clotting (color change of blood, absence of pulsations in tubing Change sterile dressing over shunt daily Avoid performing venipuncture, administering IV infusions, giving injections, or taking a blood pressure with a cuff on the shunt arm Nursing Care: before and during hemodialysis Have client void Chart clients weight Assess vital signs before and every 30 minutes during procedure Withhold antihypertensives, sedatives, and vasodilators to prevent hypotensive episodes (unless ordered otherwise) Ensure bed rest with frequent position changes for comfort Inform client that headache and nausea may occur Monitor closely for signs of bleeding since blood has been heparinized for procedure Nursing Care: Postdialysis Chart clients weight Assess for complications:
Fluid removal is by osmotic gradient with dialysate dextrose concentration providing the higher osmotic pressure PD requires filling the peritoneal cavity with a prescribed volume dialysate, allowing it to dwell for a prescribed period of time, then draining and discarding the effluent (waste materials)
Complications of Peritoneal Dialysis peritonitis - most common protein loss malnutrition inguinal or abdominal hernias KIDNEY TRANSPLANTATION HEPATIC CIRRHOSIS - A chronic disease characterized by replacement of normal liver tissue with diffuse fibrosis that disrupts the structure and function of the liver 3 types 1. Alcoholic cirrhosis 2. Post necrotic cirrhosis 3. Biliary cirrhosis Stages of Hepatic Coma
- Hypovolemic shock: may occur as a result of rapid removal or ultrafiltration of fluid from intravascular compartment - Dialysis disequilibrium syndrome due to cerebral fluid shift - painful muscle cramping - exsanguination Complications - Dysrhythmias - Air embolism - Chest Pain Advantages of Hemodialysis short treatment time minimal interruption of lifestyle in between treatments more efficient than PD performed by trained health personnel contact with similarly treated patients
THERAPEUTIC INTERVENTIONS Rest Restriction of alcohol, hepatotoxic drugs Vitamin therapy: especially the fat soluble vitamins A, D, E and K and vitamin B (thiamine chloride and nicotinic acid); zinc and calcium supplements Diuretics to control ascites and edema lactulose may be prescribed for elevated blood ammonia levels (2-4 soft stools) Paracentesis if respiratory distress occurs as a result of ascites LABORATORY ALTERATIONS Serum Albumin Total CHON Cholinesterase SGOT/SGPT Alkaline phosphatase Bilirubin (total & direct) Prothrombin time (PT) Partial thromboplastin time (PTT) Serum ammonia Urine urobilinogen Na & K Hemoglobin Hematocrit Sengstaken-Blakemore tube
PERITONEAL DIALYSIS The capillaries of the peritoneal membrane allow solute clearance down a concentration gradient between the instilled dialysate and the plasma
Sengstaken-Blakemore Tube Management If the gastric balloon is inflated, ensure proper placement, elevate bed 30-45 degrees Maintain the esophageal balloon at inflated level (30-35mm Hg) up to 48 hrs Deflate gastric balloon for a few minutes at specific intervals if ordered to prevent necrosis Gastric lavage as ordered Suction orally as necessary because the client is unable to swallow saliva
Missed anti diabetic drug Physical stress - Trauma - Surgery - Illness PATHOPHYSIOLOGY
NURSING CARE Abdominal girth measurements for baseline data relative to ascites. Skin for presence of jaundice, dryness, petechiae, ecchymoses, spider angiomas, and palmar erythema Signs of hepatic coma such as confusion, flapping of extremities Observe for bleeding Provide special skin care and keep nails trimmed because pruritus is associated with jaundice Maintain the client in a semi-Fowlers position to prevent ascites from causing dyspnea Monitor intake and output, abdominal girth, and daily weight to assess fluid balance DIETARY (CIRRHOSIS) High carbohydrate, moderate fat; provides for energy; vitamin, mineral, and electrolyte supplements Low sodium (500-1000mg daily); helps control increasing ascites Soft foods if esophageal varices are present; prevents danger of rupture and bleeding Alcohol is contraindicated to prevent further damage DIETARY (HEPATIC COMA) Protein: reduced according to tolerance; 1530g High calorie (1500-2000g) Fluid carefully controlled according to output DIABETIC KETO ACIDOSIS DKA Develops as a result of severe insulin deficiency Cardinal symptom is Severe HYPERGLYCEMIA >350mg/dl Elevated Ketone Acidosis (bicarbonate <9.0 meq/L Etiology Undiagnosed diabetes
Laboratory Plasma glucose level 350 1500 mg/dl Ketonuria large ketone bodies Serum bicarbonate <9meq/dl Serum potassium (Low) Treatment Correct volume depletion - 0.9% saline used in general Insulin Drip - 10 units of Regular insulin + 100cc saline Potassium replacements Base medications - NaHCO3
NURSING CONSIDERATION Monitor fluid status Monitor blood glucose levels Prevent aspiration pneumonia Monitor potassium Monitor mental status HYPERGLYCEMIC HYPEROSMOLAR NONKETOTIC COMA HHNK HONK A complication of diabetes No ketoacidosis (+) history of non insulin dependent DM HHNK Has the same pathogenesis with DKA the only difference is that there is no Acidosis due to fat metabolism. It is said that a little insulin is available so glucose is available for the muscles leaving fat in its place Management and consideration are the same with DKA THYROID CRISIS
Thyroid Crisis/ Thyroid Storm/ Thyrotoxic Crisis - Is a form of severe hyperthyroidism, usually of abrupt onset
Precipitating Factors
STRESS - injury - infection - Thyroid and non Thyroid Surgery - tooth extraction - Insulin Reaction - DKA - Pregnancy Precipitating Factors - Digitalis Intoxication - Abrupt withdrawal of anti thyroid medications - extreme emotional stress - Vigorous palpation of the thyroid CLINICAL MANIFESTATIONS High fever- above 38.5 C Extreme tachycardia - >130beat/min Gastrointestinal- weight loss, diarrhea, abdl pain Cardiovascular- edema, chestpain, dyspnea, palpitations Altered mental state- delirium psychosis, somnolence, coma NURSING DIAGNOSIS Imbalanced Nutrition Less than Body Requirements Ineffective Coping rt irritability, hyperexcitability Low Self esteem Altered Body Temperature Management For fever ice packs cool environment TSB Paracetamol Oxygen Therapy D5 containing IV fluids
Medulla Cortex ADRENAL CRISIS
ALTERNATIVE NAMES: Adrenal crisis; Addisonian crisis; Acute adrenal insufficiency Addisons Disease ( Adrenocortical Insufficiency) - Occurs when adrenal cortex function is inadequate to meet the patients need for cortical hormones. Causes: Autoimmune or idiopathic atrophy of the Adrenal Gland ( 80- 90% cases) Infection - Tuberculosis - Histoplasmosis Inadequate secretion of ACTH Therapeutic use of Corticosteroid MANIFESTATIONS Muscle weakness Anorexia Gastrointestinal Symptoms Fatigue Emaciation Hyperpigmentation of the skin Hypotension Low blood glucose Low sodium High potassium Cyanosis Circulatory shock - pallor - rapid, weak pulse - rapid respiration - low blood pressure Management Control of Circulatory shock Place the patient in Trendlenburg position Oral intake of fluids if tolerated
Medications a. PTU or Methimazole b. Hydrocortisone c. Radioactive Iodine d. For patients with cardiac problem- Propanolol combined with digitalis ADRENAL CRISIS Adrenal Gland
Dependent - Administer fluids - Vasopressin - Antibacterial meds - Corticosteroids
SHOCK A condition in which tissue perfusion is inadequate to deliver oxygen and nutrients to support vital organs and cellular functions Components of Adequate Blood Flow 1. Adequate Cardiac pump 2. Effective Circulatory System 3. Sufficient Blood Volume
Decrease tissue perfusion Signs and Symptoms: a. hypotension b. tachycardia c. paleness d. cold clammy skin e. dizziness Medical Management 1. Treatment of the underlying cause 2. Fluid and blood replacement - Crystalloids/ Colloids - Dextran is not to be given to patient with Hemorrhage 3. Redistribution of Fluid Medical Management 4. Pharmacology a. Insulin b. Desmopressin c. Antidiarrheal d. Anti emetic Nursing Management 1. Administration of blood and fluids safely 2. Implementing other measures - Oxygen therapy - Safety and comfort of the patient II. CARDIOGENIC SHOCK - It occurs when the heart has an impaired pumping ability - It maybe coronary or non coronary event in origin Pathophysiology
Inadequate blood flow to the tissue Poor delivery of O2 and nutrients to the cell Cellular starvation Cell Death Organ Dysfunction Organ failure Death MEAN ARTERIAL PRESSURE The average pressure at which the blood moves through the vasculature Normal= > 65mmHg Formula:
MAP= systolic BP + 2(diastolic) -------------------------------3 Classifications of Shock
Decrease cardiac contractility I. HYPOVOLEMIC SHOCK Decrease SV and CO - occurs when there is a decrease in the intravascular volume by 15- 25% ( 750- 1300ml) of blood in a 70 kg person Pathophysiology Pulmonary Congestion decrease systemic tissue perfusion decrease Coronary Artery perfusion Signs and Symptoms:
Decrease blood volume (Intracellular or extracellular) Decrease venous return Decrease stroke volume Decrease Cardiac Output
a. pain of angina b. dysrhythmias c. Hemodynamic Instability
Medical Management
1. Correction of underlying cause a. Coronary cardiogenic shock - Thrombolytics, Angioplasty, CABG, IABP b. Non Coronary Cardiogenic Shock - replacement of a faulty cardiac valve, correction of dysrhythmia, acidosis and electrolyte imbalance Medical Management
Permeability / fluid shifting Poor Tissue Perfusion Signs and symptoms: 1. Confusion 2. Hypotension 3. Tachycardia 4. Tachypnea 1. 2. 3.
coagulation system
2. Initiation of First line treatment a. Oxygen Therapy b. Control of chest pain c. Providing Selected Fluid Control d. Implementing mechanical cardiac support Medical Management 3. Pharmacology Therapy a. Dobutamine- has an inotropic effect b. Nitroglycerin- vasodilator which reduces preload and afterload c. Dopamine - increases blood flow to the kidneys and mesentery - inotropic and slight chronotropic effect d. Antiarrhythmic medications e. Fluid Therapy Nursing Management 1. Prevent Cardiogenic Shock - conserve patients energy - Relieves angina - Administer supplemental O2 2. Monitor hemodynamic status 3. Administer medications and intravenous fluids safely 4. Maintaining Mechanical Assistive Devices 5. Enhancing safety and comfort III. CIRCULATORY SHOCK 1. Septic shock- caused by widespread infection Pathophysiology
Medical Management Any potential route for infection is eliminated Fluid replacements Pharmacology Therapy a. antibiotics b. Recombinant human activated protein C
(rhAPC)-antithrombotic,anti inflammatory, profibrinolytic 4. Aggressive nutritional supplementation a. b. c. Nursing Management Hand Hygiene Aseptic technique Obtaining appropriate specimen for culture and sensitivity d. Monitoring of pertinent blood test 2. Neurogenic Shock - Caused by spinal cord injury, spinal anesthesia and nervous system damage Pathophysiology
Parasympathetic stimulation Prolonged vasodilation Blood volume is displaced Hypotensive state Decrease vascular resistance Insufficient perfusion of tissues and cells Signs and symptoms: (parasympathetic effect) 1. Dry, warm skin 2. Hypotension 3. bradycardia Medical Management Stabilization of a spinal cord injury Glucose for hypoglycemia Proper positioning - Spinal Anesthesia
Microorganisms invade body tissues Activation of inflammatory mediators Increased capillary Mediators activate
Nursing Management Elevate the bed at 30 degrees Immobilize the patient to prevent further damage to the spinal cord Application of elastic compression stockings/ elevate foot of the bed Passive range of motion exercises Watched out for signs of internal bleeding if patient has spinal cord injury
Signs and symptoms: 1. Hypotension 2. Respiratory failure 3. Hypermetabolic state- hyperglycemia, hyperlacticacidemia, polyuria 4. Liver failure 5. Renal failure a. b. c. Medical Management Controlling the initiating event Promoting adequate organ perfusion Providing nutritional support Nursing management a. Promoting Communication
3. Anaphylactic Shock - Occurs when patient is already exposed to an antigen and who have developed antibodies to it. Medical Management Removal of causative antigen Epinephrine- vasoconstrictive effect Diphenhydramine- antihistamine Albuterol- bronchodilator
Nursing Management Assess patient for allergies Advise patient to wear identification of what kind of allergies he has Stages of Shock
I. Compensatory Stage - Metabolic acidosis - Increase RR II. Progressive Stage - Decrease MAP - Hypotension Due to: 1. 2. 3. 4. Direct tissue insult SIRS Sepsis shock
III. Irreversible Stage - Severe organ damage - Hypotension - Liver and Renal failure - Cardiac and respiratory failure - Metabolic Acidosis MULTIPLE ORGAN DYSFUNCTION SYSTEM/ MULTISYSTEM ORGAN FAILURE - Altered organ function in acutely ill patients - A complication of any state of shock
Вам также может понравиться
- University of Perpetual Help System Dalta Alabang-Zapote Rd. Pamplona, Las Piñas CityДокумент1 страницаUniversity of Perpetual Help System Dalta Alabang-Zapote Rd. Pamplona, Las Piñas CityCJ AngelesОценок пока нет
- NCPДокумент5 страницNCPCJ AngelesОценок пока нет
- Community Nursing ObjectivesДокумент1 страницаCommunity Nursing ObjectivesCJ AngelesОценок пока нет
- FCL ReflectionДокумент6 страницFCL ReflectionCJ AngelesОценок пока нет
- LoginДокумент5 страницLoginCJ AngelesОценок пока нет
- NHPДокумент13 страницNHPCJ AngelesОценок пока нет
- Certificate of Training: Rolly T. Villones JRДокумент1 страницаCertificate of Training: Rolly T. Villones JRCJ AngelesОценок пока нет
- Hypertension PathophysiologyДокумент2 страницыHypertension PathophysiologyJems60% (5)
- NCM 104 MusculoskeletalДокумент12 страницNCM 104 MusculoskeletalCJ AngelesОценок пока нет
- AnswerДокумент18 страницAnswerCJ AngelesОценок пока нет
- Measuring Intake and OutputДокумент1 страницаMeasuring Intake and OutputCJ AngelesОценок пока нет
- FamilyДокумент37 страницFamilyCJ AngelesОценок пока нет
- Bladder Irrigation (Cystoclysis)Документ4 страницыBladder Irrigation (Cystoclysis)CJ Angeles100% (2)
- Vitamins & MineralsДокумент8 страницVitamins & MineralsCJ AngelesОценок пока нет
- Sample QuestionnairesДокумент6 страницSample QuestionnairesCJ AngelesОценок пока нет
- Antibacterial AgentsДокумент4 страницыAntibacterial AgentsCJ AngelesОценок пока нет
- COPARДокумент34 страницыCOPARCJ AngelesОценок пока нет
- The Problem and Review of Related Literature and StudiesДокумент36 страницThe Problem and Review of Related Literature and StudiesCJ AngelesОценок пока нет
- Philippine Eagle: TaxonomyДокумент5 страницPhilippine Eagle: TaxonomyCJ AngelesОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Cardiac CatheterizationДокумент9 страницCardiac CatheterizationAnurag Gupta100% (1)
- ACLS Pretest Exam AnnotatedДокумент21 страницаACLS Pretest Exam AnnotatedMOLLYОценок пока нет
- The Placebo EffectДокумент5 страницThe Placebo EffectIvan JankovicОценок пока нет
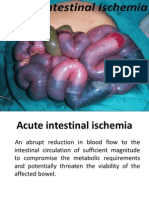
- Acute Intestinal IschemiaДокумент50 страницAcute Intestinal IschemiaRohit ParyaniОценок пока нет
- Volume 11 Jan Dec 2005Документ69 страницVolume 11 Jan Dec 2005Elizabeth GomezОценок пока нет
- Circuit Weight Training in Cardiac PatientsДокумент5 страницCircuit Weight Training in Cardiac PatientsVivin YulvinaОценок пока нет
- 466 Concept MapДокумент6 страниц466 Concept Mapapi-284107243Оценок пока нет
- Chest Pain Notes USMLE Step 3Документ3 страницыChest Pain Notes USMLE Step 3kisria100% (1)
- 5 - Fluorouracilo Ficha TecnicaДокумент317 страниц5 - Fluorouracilo Ficha TecnicaDav SAОценок пока нет
- Evaluation of Chest Pain PDFДокумент2 страницыEvaluation of Chest Pain PDFJaredОценок пока нет
- Condition Chest Pain Symptoms Other Symptoms What It Is: Stable AnginaДокумент4 страницыCondition Chest Pain Symptoms Other Symptoms What It Is: Stable Anginartishaii18Оценок пока нет
- Complications Associated With Intravenous TherapyДокумент18 страницComplications Associated With Intravenous TherapyIyah Jane Villahermosa50% (2)
- 0533FДокумент34 страницы0533Fgregorio250188Оценок пока нет
- Clin Med For PAsДокумент32 страницыClin Med For PAsMaryNguyen100% (2)
- AnginaДокумент16 страницAnginaMc_Lopez_1761Оценок пока нет
- Handbook of PLAB (2nd Ed.)Документ863 страницыHandbook of PLAB (2nd Ed.)blndffl91% (11)
- Wasserman Chest 1997Документ13 страницWasserman Chest 1997Filip BreskvarОценок пока нет
- Pharmacology - A Summary of Common ConditionsДокумент50 страницPharmacology - A Summary of Common ConditionsJeremy YangОценок пока нет
- Haad 1 Questions HeartДокумент17 страницHaad 1 Questions HeartPatpat De GuzmanОценок пока нет
- Fresh Potato Juice TreatmentДокумент12 страницFresh Potato Juice Treatmentlawnmawn100% (1)
- Talley & O'Connor Quiz SampleДокумент5 страницTalley & O'Connor Quiz SamplefilchibuffОценок пока нет
- Chapter 5 Care of The Clients With Cardiovascular DisordersДокумент226 страницChapter 5 Care of The Clients With Cardiovascular DisordersDon Felicisimo EbronОценок пока нет
- Oman Pharmacist Licensing Exam McqsДокумент186 страницOman Pharmacist Licensing Exam McqsMuhammad Amin100% (5)
- Discharge Plan For CADДокумент2 страницыDischarge Plan For CADYannah Mae EspineliОценок пока нет
- Prometric McqsДокумент30 страницPrometric Mcqsjishan8250% (2)
- Post TestДокумент11 страницPost TestDemuel Dee L. BertoОценок пока нет
- Cardio NewДокумент10 страницCardio NewnotadagОценок пока нет
- Management of Patients With Systemic Diseases in Oral SurgeryДокумент42 страницыManagement of Patients With Systemic Diseases in Oral SurgeryRichard Starr100% (2)
- 05 - N031 - 38796 ThesisДокумент22 страницы05 - N031 - 38796 ThesisdrtareksОценок пока нет
- WDDTYДокумент100 страницWDDTYgfrankel72100% (1)