Академический Документы
Профессиональный Документы
Культура Документы
Lipids Measurements: Previous (Section 4.) Next (Section 6.)
Загружено:
Genita Savitri EkandariИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Lipids Measurements: Previous (Section 4.) Next (Section 6.)
Загружено:
Genita Savitri EkandariАвторское право:
Доступные форматы
01/10/13
5. Lipids measurements
Contents
Previous (Section 4.)
Next (Section 6.)
5. Lipids measurements
The processes involved in the formation and progression - sometime even regression - of athersclerotic lesions are complex and still not completely known, but ongoing research is constantly refining our understanding. Nevertheless, is is generally accepted that elevated blood lipids play an important role in the genesis of these lesions (1, 2); although many heart attacks occur in persons with "normal" blood lipid levels. However, clinical trials with the so called "statin" group of drugs have shown that reducing blood lipid levels decreases the risk for coronary events. The assessment of blood lipid levels is, therefore, an important component of risk factor monitoring. Lipid transport in the circulation occurs in the form of lipoproteins (protein shells surrounding a lipid core). Lipoproteins are classified according to their source, composition and physiological action. The two types considered to be most important for cardiovascular risk assessment are low density lipoproteins (LDL) and high density lipoproteins (HDL). They are involved in the transport of cholesterol to and away from the body tissues, which led to the suggestion that the ratio LDL/HDL is an important indicator for cardiovascular risk. Besides cholesterol, triglycerides are considered to play an independent role in the formation of atherosclerotic lesions. In a recent review of the epidemiological, clinical, cellular and molecular evidence of the role of triglycerides in atherogenicity, Sprecher (3) comes to the conclusion that high levels of triglycerides are an important risk factor, especially for mild cases of atherosclerotic lesions. Fasting triglycerides or the postprandial rise of triglycerides in response to a test meal have been found to be risk factors. Established methods exist for the direct measurement of total cholesterol (TC), HDL and triglycerides, either from plasma or serum samples. There are now also methods available for the direct measurement of the LDL subfraction, but it is still frequently estimated from TC, HDL and fasting triglycerides by the Friedewald formula. The review of the methods used in the determination of total cholesterol and HDL was prepared based largely on the experience from the WHO MONICA Project (4). The measurement of triglyceride levels was not a part of the WHO MONICA Project . Therefore, no international comparisons were made as was done for the total cholesterol and HDL. However, some centres have collected blood from fasting subjects and measured triglycerides. For them, quality control was provided by the WHO-RLRC in Prague, and the CDC, Atlanta. The review of the triglyceride measurements refers mainly to experience from the WHO MONICA and NHANES III. The National Health Surveys in the UK did not include in their protocol the triglyceride measurement. The German Federal Health Survey 1998 measured triglycerides, but no detailed information is available at this time. For the Monitoring Project on Cardiovascular Disease Risk Factors in the Netherlands we also have, so far, no specific information about measurements of triglyceride.
5.1 Methods
In this section we will consider methodological issues which are relevant to the quality and comparability of survey results. The selection of the issues and the description of their importance is largely based on the retrospective MONICA quality assessment reports of total and HDL cholesterol measurements (4, 5), but in many places more recent information and experience was used to update the assessment. We have classified the methodological issues to pre-analytic and analytic ones. The pre-analytic issues concern
www.thl.fi/publications/ehrm/product1/section5.htm 1/23
01/10/13
5. Lipids measurements
general aspects of organising the surveys and the procedures in the survey field examination centres. The analytic issues are those which relate to the laboratory work. The surveys considered in the review have analysed total cholesterol and subfractions in laboratories from venous blood samples. Issues relating to the pin-prick measurements are complicated and will not be considered here. 5.1.1 Pre-analytic issues 5.1.1.1 Seasonal variation Several studies have shown that total cholesterol levels are increased in winter (6-8). However, little is known about the reasons for the seasonal variation, and the variation may differ between countries. The difference in total cholesterol levels between June and December has been reported to be around 0.19 mmol/l (9, 10). The change in season does not seem to affect significantly HDL cholesterol (11). Several studies have suggested that level of triglycerides are increased during winter months (7, 10, 12). WHO MONICA Project In the WHO MONICA Project , the time of year of the cholesterol measurements was not standardized between the populations. However, to avoid bias in trend estimation in cholesterol levels that may be caused by seasonal variation , all surveys in a population were supposed to take place at the same time of the year. When the blood samples were collected throughout the entire year, it was recommended to keep the proportion of subjects from of each age and sex group equal throughout the period (13). In 13 populations a seasonal change may have affected the trends in cholesterol levels. In these population the seasonal difference between two surveys is at least 2 months which can cause 0.1 mmol/l difference in total cholesterol levels (4). Risk factor monitoring in the Netherlands The Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project collected blood samples through out the year, there for the seasonal variation should not be a problem (14). The REGENBOOG project was conducted between May 1998 and December 2001 and blood samples were collected through out the years (15, 16). NHANES III NHANES III was conducted over several years and seasonal variations were probably averaged out. Risk factor monitoring in Germany The German Federal Health Survey 1998 was conducted between October 1997 and March 1999, but the main part of the survey was completed in November 1998. Therefore, the survey period covered about one full year and seasonal variations should average out. The Italian OEC Project Seasonal variations may average out since the survey lasted the whole year. Other surveys
www.thl.fi/publications/ehrm/product1/section5.htm 2/23
01/10/13
5. Lipids measurements
No information on timing of blood sampling available so far from UK National Health Surveys. 5.1.1.2 Daily variation and fasting status The effect of time of day is estimated to be about 2.5% (coefficient of variation) on total cholesterol and 4.5% on HDL cholesterol (17). Daily variations in cholesterol are detectable if large fluctuations of triglycerides occur during the day (18). In most subjects, the time of blood drawing does not seem to be important. For triglyceride concentration the maximum daily rhythmic variation could reach 63% (19). Total cholesterol level is not significantly influenced by fasting, but HDL cholesterol level decreases transiently postprandially (18). Therefore fasting is usually not considered essential before total cholesterol measurements, but 12-14 hours fasting is often recommended for HDL cholesterol measurements (11). The fasting time may make a difference in cholesterol levels for a small percentage of people (20). Triglycerides are influenced by fasting, although their daily fluctuation does not have a simple relation with intake of meals (18). It is usually recommended that blood for measurement of triglycerides should be collected after at least 12 hours fasting. WHO MONICA Project In the WHO MONICA Project , where the primary lipid of interest was serum total cholesterol and secondarily high density lipoprotein cholesterol (HDL-C), blood could be taken at any time of day from non-fasting subjects; this facilitated scheduling the survey examinations throughout the day (13). About 40% of the centers collected blood samples after overnight fasting (4). Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project in the Netherlands non-fasting samples were used (14, 21). In the MORGEN-project it was asked if person has fasted and time of last meal as recorded (14). In the REGENBOOG project fasting samples were collected in years 1998 and 1999. Samples were collected between 7:30 and 10:30 and subjects were asked to abstain from eating or drinking starting at 22:00 the night before the examination. (16, 22) Risk factor monitoring in Germany In the German Cardiovascular Prevention Study non-fasting samples were used (23). The German Federal Health Survey 1998 required a three hour fast and 24 hour alcohol abstention (24). NHANES III In NHANES III, half of the sample was asked to fast for 12 hours and triglycerides were measured only in this subsample. Total and HDL cholesterol was measured from the entire sample. (25) UK National Health Surveys No information available so far. The Italian OEC Project Fasting blood samples were drawn. (26)
www.thl.fi/publications/ehrm/product1/section5.htm 3/23
01/10/13
5. Lipids measurements
Risk factor monitoring in Norway In the National Cardiovascular Screening the non-fasting samples were used (27). 5.1.1.3 Strenuous exercise Strenuous exercise causes hemoconcentration, i.e. filtrable constituents of blood (mainly water and small molecular solutes) are either gained (hemodilution) or lost (hemoconcentration) from the circulating blood volume and the concentration of protein bound constituents decreases or increases accordingly. Strenuous exercise 15 minutes before blood drawing increases cholesterol levels by about 6% (18). Therefore, it is commonly recommended that strenuous exercise should be avoided 2-3 hours before blood drawing. Under normal examination conditions people will remain for some time in the examination centre; even if they do not, it would still be unlikely that they engage in strenuous exercise immediately before blood drawing. WHO MONICA Project In the WHO MONICA Project there was no special recommendations about the strenuous exercise before blood drawing and no information relating to this issue was collected. (4) Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors, the MORGEN-project and REGENBOOG project subject were not advised to avoid strenuous exercise before blood drawing (14, 16). Other surveys No information on exercise prior to blood drawing was found for: Risk factor monitoring in Germany, UK National Health Surveys, and NHANES III. 5.1.1.4 Position of the subject Several studies reported on the effect on total cholesterol levels caused by the position of the subject during blood drawing (28-35). There is evidence that change of posture from 30 minutes supine to 30 minutes standing results in a 9.3% increase of total cholesterol concentration (35). Other studies show that drawing blood after a transition from standing to supine may produce a 4-6% decrease in total cholesterol compared with drawing blood after a transition from standing to sitting (29, 30). The effect is brought about by hemodilution when assuming supine position or hemoconcentration as a result of assuming the upright position. The sympathetic nervous system may also play some role (11). WHO MONICA Project In the WHO MONICA Project , it is recommended that venipunctures should be carried out with the subject in a sitting position (13). Nevertheless, in five populations the blood was drawn in supine position (4). Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors, the MORGEN-project and the REGENBOOG project the blood samples were obtained while the subject was is sitting position (14, 22).
www.thl.fi/publications/ehrm/product1/section5.htm 4/23
01/10/13
5. Lipids measurements
Risk factor monitoring in Germany In the German Cardiovascular Prevention Study blood samples were obtained while the subjects were in supine position (23). The German Federal Health Survey 1998 collected blood samples from sitting subjects and recorded in the data collection form if a deviation from this requirement was necessary (24). UK National Health Surveys In the National Health Surveys in UK it is recommended that venipuncture should be carried out with the subject in a sitting position, or if the subject requires it, lying on a bed or sofa (36). NHANES III In NHANES III it was recommended that venipunctures should be obtained while the subject is sitting (37). Risk factor monitoring in Norway In the National Cardiovascular Screening the venipuncture was carried out while the subject was sitting (27). 5.1.1.5 Type of tubes Traditionally, syringes and glass tubes were used for collecting blood. In the past decades these have been replaced largely with plastic vacuum sealed tubes, which are more expensive but easier to use. The plastic tubes do not brake, and they can be frozen to -80C. In recent years, vacuum sealed tubes which include gel have come on the market. In centrifuging, the gel settles between the serum and cells making the separation of serum easier and providing a higher yield of serum. WHO MONICA Project According to the instruction of the WHO MONICA Project , either 10 ml vacuum sealed tubes or syringes and glass tubes could be used to collect blood. The use of vacuum tubes containing EDTA was recommended if plasma was used for analysis (13). Two thirds of the centres used vacuum sealed containers in the final MONICA surveys. Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors, the MORGEN-project and the REGENBOOG project used vacutainer tubes were to collect blood samples (14, 22). Risk factor monitoring in Germany The German Federal Health Survey 1998 used vacutainer tubes for blood collection. Aliquots for the different analyses were then drawn from the whole-blood sample at the collection site. UK National Health Surveys In the National Health Surveys in UK vacuum tubes were used (36). NHANES III
www.thl.fi/publications/ehrm/product1/section5.htm 5/23
01/10/13
5. Lipids measurements
NHANES III used vacuum tubes (38). 5.1.1.6 Tourniquet use Prolonged venous occlusion produced by tourniquet use is associated with higher cholesterol values compared to results obtained by blood drawing without tourniquet use. Levels can increase by 10-15% after 10 minutes of venous occlusion and 2-5% after 2 minutes. Tourniquet use up to one minute is not associated with any significant increase in cholesterol levels (39). Statland and co-authors (31) found a significant increase in total cholesterol levels (3.5%) when the tourniquet was used for 3 minutes. According to Naito (40), well trained technicians need less than one minute for drawing one tube. Tan and co-authors (30) did not find any significant changes in serum cholesterol concentration when the tourniquet was applied for 0.5 to 1 minute. It has also been demonstrated that the use of a low-pressure tourniquet for 3 minutes does not significantly affect the concentration of serum constituents including total cholesterol (41). Vacuum sealed containers, if correctly used, should not affect these findings. WHO MONICA Project In the WHO MONICA Project , the use of a tourniquet was to be avoided. If the tourniquet was needed to obtain good flow, it had to be released before the withdrawal of blood (13). In most centres the above instruction was followed and use of tourniquet was limited to less than one minute (4). Risk factor monitoring in the Netherlands In the REGENBOOG project, a plastic hose was used as tourniquet if needed (22). Risk factor monitoring in Germany The German Federal Health Survey 1998 required release of the tourniquet before blood started to flow. Longer than normal tourniquet use was recorded on the data collection form (24). UK National Health Surveys In the National Health Surveys in the UK it was recommended that if tourniquet was needed it be applied with minimal pressure and be released as the blood started to be drawn into the tube. (36) NHANES III In NHANES III, a latex strip tourniquet was used for the venipuncture . If the tourniquet has been applied for more than 1 minute while searching a vein, it was recommended to be released for 2 to 3 minutes. (37) 5.1.1.7 Serum or plasma The commonly recommended anticoagulant for plasma is disodium ethylenediaminetetraacetate (EDTA). Its use produces a shift of water from red blood cells to plasma, and therefore dilutes the plama and lowers the concentration of cholesterol. In the 1970s, its use was reported to lower the cholesterol concentration by 3% compared with measurements from serum, and in 1990 a difference of 4.7% was reported. The increase in the difference over the years was explained by a 50% increase in the EDTA concentrations in the commercially manufactured tubes (42, 43).
www.thl.fi/publications/ehrm/product1/section5.htm 6/23
01/10/13
5. Lipids measurements
A practical reason for the use of plasma instead of serum is the fact that plasma, unlike serum, can be centrifuged immediately after taking the blood sample. The time delay is not a problem for cholesterol and triglycerides, but may effect glucose levels, since glucose is metabolized by red cells. Plasma is also required if a survey collects information on fibrinogen. WHO MONICA Project In the WHO MONICA Project , serum was recommended in preference to plasma. It was, however, recognised that some centres wanted to continue the same methods that had been used in earlier surveys. For most of the populations serum was used. Only 5 populations used plasma, with EDTA, in the final survey (4). Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors in the Netherlands and the MORGENproject, EDTA plasma was used for determination of total and HDL cholesterol (14, 21). The REGENBOOG project used serum for cholesterol determination (16). Risk factor monitoring in Germany In the German Cardiovascular Prevention Study serum was used for the lipid analysis (23). The German Federal Health Survey 1998 collected serum for total cholesterol, HDL-cholesterol, and triglyceride analysis and plasma for fibrinogen and antithrombin III analysis (24). UK National Health Surveys In the UK National Health Surveys serum was used for total and HDL-cholesterol (36). NHANES III In NHANES III , serum was used for the analysis of total and HDL-cholesterol and triglycerides (25). Risk factor monitoring in Norway In the National Cardiovascular Screening, serum was used for the analyses of cholesterol and triglycerides (27). 5.1.1.8 Centrifuging and storing before centrifuging The time, temperature and force of centrifuging should be standardised. For serum this concerns also the time allowed for clotting before centrifuging. For serum samples, in general, blood should be allowed to clot at least half an hour and then be centrifuged at room temperature (15-24C) and 1500G or more for at least 10 minutes (44). The usually recommended upper limit for storage before centrifuging is 2 hours, although even a longer storage does not seem to influence cholesterol levels (45). For plasma samples, centrifugation can be done immediately If it has to be done later, the storage temperature may vary with the length of the storage. When centrifuging, the tubes should be closed tightly to avoid evaporation. This holds for both serum and plasma samples. WHO MONICA Project The WHO MONICA Project recommended that for serum preparation, blood samples are allowed to clot at not more than 20C usually for up to one hour before centrifugation. Blood specimens should be centrifuged at a
www.thl.fi/publications/ehrm/product1/section5.htm 7/23
01/10/13
5. Lipids measurements
temperature of not more than 20C at a minimum of 1500G for at least 10 minutes. With a refrigerated centrifuge, centrifugation should preferably be done at 4C. Whole blood samples must not be frozen during processing (13). For plasma preparation, after thorough mixing of the blood samples with EDTA, they should be cooled on melting ice. Within 3 hours (and preferably within one hour), the tubes should be centrifuged at 4C in a refrigerated centrifuge at 1500G for 30 minutes. If a refrigerated centrifuge is not available within 3 hours of collection, the samples may be centrifuged at room temperature within 1 hour of collection, and the plasma stored at 4C (13). Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project the plasma was centrifuged for 10 minutes (14). In the REGENBOOG project the sample was centrifuged at 2750 rpm in Roxita/A centrifuge (16). NHANES III For the preparation of serum in NHANES III , the samples were allowed to clot for 30 to 40 min at room temperature. The tubes were centrifuged unopened at 1115G for 15 min. (38) Other surveys No information on the pre-analysis processing of blood samples was located for: Risk factor monitoring in Germany, and UK National Health Surveys 5.1.1.9 Hemolysis Hemolysis may occur during blood drawing and handling. It will result in higher cholesterol values, if the direct "Liebermann-Burchard" method is used. For enzymatic methods, only a gross hemolysis has an increasing effect on cholesterol (44). Lipemia can affect the triglyceride measurements by interfering with absorbance measurement (46). WHO MONICA Project In the WHO MONICA Project , it was recommended that haemolytic samples should be discarded and fresh samples should be drawn from the subjects and analysed (13). Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project the hemolysis was coded on the form and if it was severe, the total cholesterol was not determined (14). NHANES III In NHANES III, if after removal of the clot after centrifuging, the serum in any individual tube for the person was grossly hemolyzed, it was not pooled with clear serum from the remaining tubes. However, if all of the serum from one person was turbid, lipemic, or icteric, it was pooled as usual. (It was noted that all biochemical tests can be performed on such specimens without compromising analytical accuracy, however.) At the analysis stage, when a sample was flagged as turbid by the analyser, the sample was diluted (1 part sample + 1 part saline) and reanalysed. (38)
www.thl.fi/publications/ehrm/product1/section5.htm 8/23
01/10/13
5. Lipids measurements
Other surveys No information on handling of hemolysed samples was located for: Risk factor monitoring in Germany, and UK National Health Surveys. 5.1.1.10 Storage after centrifuging Storage before isolation of HDL: It is usually recommended that isolation of HDL should be done on the day of blood sample collection. Storage of fresh samples for more than three days at +4C leads to a reduction in HDL cholesterol levels of about 8.2% to 14.9%. Storage of frozen samples for more than 14 days at -20C leads to a decrease in HDL cholesterol levels, whereas storage at lower temperatures does not produce such modifications. (47, 48) Storage before analysis of cholesterol and triglycerides: Storage using refrigeration or at room temperature between centrifuging and analysis does not seem to be crucial if the material is analysed within a few days and bacterial contamination is avoided. Freezing in appropriate vials is acceptable at a temperature of -20C for 1 year or at a temperature of -60C for a longer period (49). However, a recent study on long term storage of serum at -70C suggest a decrease of 2% per year for total cholesterol over 7 years, 2.8% per year in triglycerides, and 1.3% (not significant) per year for HDL-cholesterol (50). WHO MONICA Project According to the MONICA Manual, isolation of HDL should preferably be done on fresh serum aliquots on the day of blood collection (18). If impossible, the serum or plasma for HDL cholesterol determination should be frozen at -20C and isolation should be performed within 14 days. In two thirds of the populations in the final survey isolation was done on fresh samples (4). It was recommenced that the total cholesterol and HDL cholesterol levels should be assessed on the day of sample collection. Samples could be stored for up to four days at +4C. If analyses of total cholesterol could not be performed within 4 days, the serum or plasma samples should be immediately stored at -20C or lower in tightly stoppered glass tubes (13). In about half of the centres in the final surveys, cholesterol was measured from fresh samples, and in about a half from frozen samples (4) Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project the samples were stored at -20 o C for a maximum of 3 weeks and after that part of the samples were trasfered to the RIVM for storage, partly at -86 o C and partly at -196 o C (14). In the REGENBOOG project the samples were stored at -80 o C (16). Risk factor monitoring in Germany In the German Federal Health Survey 1998 serum samples were frozen at -40C at the collection sites and transported to a central laboratory on dry ice (24). UK National Health Surveys The samples were dispatched immediately after blood taking (before isolation of HDL) to The Royal Victoria
www.thl.fi/publications/ehrm/product1/section5.htm 9/23
01/10/13
5. Lipids measurements
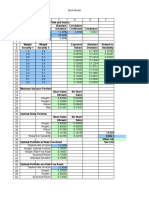
Infirmary (RVI) laboratories in Newcastle upon Tyne, except in 1994-1997, when they were analysed by the laboratories of the West Middlesex University Hospital (WMUH). A part of the serum was stored at -70C for possible future analysis. (36) NHANES III In NHANES III the samples were frozen (before isolation of HDL) at -20C and shipped weekly on dry ice to the Contract Laboratory in Baltimore. Serum was stored at -20C for no longer than 4 weeks. For permanent storage, samples were frozen at -70C. (38) 5.1.2 Analytic issues 5.1.2.1 Isolation of HDL HDL cholesterol measurements are performed after first removing the other lipoproteins from the sample and subsequently measuring the cholesterol content of the remaining HDL-containing fraction. Several precipitation procedures are available for HDL isolation, using one of the following reagents: heparin-Mn++ (hep-Mn++) (51), dextran sulphate-Mg++ (Dxtr), phosphotungstate-Mg++ (PTA) and polyethylene glycol (PEG) (52). However, because no definitive or primary reference methods exist for the separation of HDL, and because differences in the precipitation procedures can alter the population of particles precipitated, not all methods give the same result for HDL cholesterol and therefore standardisation of HDL cholesterol measurement is difficult (5). In recent years, a direct method for assessing HDL-cholesterol, which does not require isolation of HDL, has become available (53). According to the experience of the laboratory of the National Pubic Health Institute of Finland (personal communication), the method works very well, and the results are similar to the traditional method using PTA for isolation of HDL. As the new direct HDL method does not require precipitation, its use is essentially simpler than the use of the traditional methods, and therefore it is less error prone. WHO MONICA Project In the beginning of the WHO MONICA Project , use of the PTA isolation method after Burnstein, Samaille and Lopez-Virella was recommended. During the Project, an improved modification of the PTA method (kit No. 543004 of Boehringer Mannheim) was introduced. This method correlated well with the ultracentrifugation method and it was found to work well on most lyophilised controls. The description of the modification was included in the MONICA Manual in November 1990 (13). In the WHO MONICA Project, different centres used different methods for isolation of HDL. The following table gives a summary of the methods which were used in the final MONICA surveys (5): Method Dextran suplhate-Mg++ (Dxtr) Heparin-Manganese++ (Hep-Mn++) PEG 6000 (PEG) Phosphotungstate-Mg++ (PTA) Updated phosphotungstate-Mg++ after the BoehringerMs (PTA 543004)
www.thl.fi/publications/ehrm/product1/section5.htm
Number of centres using the method in the final MONICA survey 5 3 2 9 10
10/23
01/10/13
5. Lipids measurements
Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project in the Netherlands, PTA was used for isolation of HDL (14, 54). Risk factor monitoring in Germany In the German Cardiovascular Prevention Study, PTA was used for isolation of HDL (23). No information was found for the German Federal Health Survey 1998 . UK National Health Surveys PTA was used for isolation of HDL (36) NHANES III In NHANES III, Hep-Mn++ was used for isolation of HDL, and removal of excess manganese by precipitation with sodium bicarbonate (25, 55). 5.1.2.2 Methods of total cholesterol and triglyceride determination Enzymatic methods with automatic analysers, which have been in use since the 1980s, have become standard methods in cholesterol measurement (56). They allow very good precision, provided that they are used with care and they are calibrated properly (11). Calibration and quality control will be considered separately in sections 5.1.2.3 and 5.2. Triglycerides are measured enzymatically in serum or plasma by using reactions in which triglycerides are first hydrolysed to produce glycerol (56). WHO MONICA Project In the MONICA Project , local laboratories were used by each Collaborating Centre. The use of enzymatic cholesterol method was recommended. It was, however, recognised that some centres may need to use other methods for local reasons (13). In the final MONICA survey, an enzymatic method was used in all laboratories, except one, which used the so-called "direct", "one-step", "Liebermann-Burchard" method (4). Triglycerides were not part of the MONICA core study, and therefore no instructions for its measurement were given. Some centres measured triglycerides as a local option. Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project in the Netherlands, plasma total cholesterol was determined enzymatically in one laboratory (Clinical Chemistry Laboratory of the University Hospital "Dijkzigt" in Rotterdam).(14, 57) Risk factor monitoring in Germany In the German Cardiovascular Prevention Study, cholesterol levels were analysed enzymatically in one laboratory (Institute for Social Medicine and Epidemiology of the German Federal Health Office, Berlin, now called Robert Koch-Institute) (23). For the German Federal Health Survey 1998 lipids were analysed centrally at
www.thl.fi/publications/ehrm/product1/section5.htm 11/23
01/10/13
5. Lipids measurements
the laboratory of the Robert Koch-Institut. No information about the method was located (24). UK National Health Surveys In the National Health Surveys in UK, all cholesterol analyses were carried out in one laboratory (The Royal Victoria Infirmary (RVI) laboratories in Newcastle upon Tyne, except in 1994-1997, when they were analysed by the laboratories of the West Middlesex University Hospital (WMUH) using the DAX Cholesterol Oxidase assay method. (36). Triglycerides were not measured in the UK surveys. NHANES III In NHANES III cholesterol and triglycerides were measured enzymatically. All measurements were done in one laboratory (John's Hopkins University Lipid Research Clinic Laboratory).(25) The Italian OEC Project Lipids were analysed centrally by the laboratory of the hospital in Desio (Lombardia region of Northern Italy). This laboratory participates in the Cholesterol Reference Methods Laboratory Network of CDC, Atlanta through the San Raffaele Institute in Milan. (26) Enzymatic colorimetric methods (CHOD_PAP and ROCHE) were used for the assays. Risk factor monitoring in Norway In the National Cardiovascular Screening the enzymatic method was used to determine total cholesterol and triglycerides in Ullevl Hospital laboratory (27). 5.1.2.3 Low density lipoprotein analysis LDL determination was traditionally made through the Friedewald formula: LDL = total cholesterol - HDL 0.45triglycerides.This approximation has several drawbacks. It requires samples from fasting subjects and works poorly at high triglyceride levels. There are exist now a number of direct methods for LDL measurement that work well for high triglyceride blood (58-60). Also the fasting status of subjects does not affect the results. 5.1.2.4 Calibration Proper calibration of the measurement instrument is essential for the precision and accuracy of the measurements. Particularly important is the secondary calibrator, which should be real human serum or plasma, ideally in the same form as the survey blood samples. Only with such calibrators one can get a reasonable assurance that there are no matrix effects, i.e. that there is no interference from substances in the samples which are not being measured. For the reliability of the secondary calibrator, it should be traceable to an internationally recognised reference method. WHO MONICA Project In the WHO MONICA Project , each participating laboratory was responsible for its own analytical primary standards and/or secondary serum calibrators. The secondary (serum) calibrators should preferably have been prepared and/or labeled with correct total and/or HDL cholesterol concentrations in the WHO Regional Lipid Reference Centre (WHO-RLRC) in Prague, Czech Republic, and/or in the Centres of Disease Control (CDC),
www.thl.fi/publications/ehrm/product1/section5.htm 12/23
01/10/13
5. Lipids measurements
Atlanta, USA (13). During the pre-standardisation period the WHO-RLRC distributed a set of three total cholesterol samples designed for testing linearity over the working range. Risk factor monitoring in the Netherlands No information available so far. Risk factor monitoring in Germany In Germany, most clinical assays have to incorporate legally mandated calibration procedures. No detailed information was available on the calibration method used by the central laboratory for the German Federal Health Survey 1998 . UK National Health Surveys In the UK National Health Survey calibration was done to the CDC by the Biochemistry Department at RVI. (36) NHANES III In NHANES III, the calibrators were obtained from the manufacturer of the analyser (Hitachi 704) and used without further preparation. (38) The laboratory was standardized for cholesterol, triglyceride and HDL cholesterol measurements according to the criteria of the CDC-National Heart, Lung, and Blood Institute Lipid Standardization Program. (25, 61)
5.2 Quality assurance
5.2.1 Training In addition to fixing the procedures to be used for lipid measurements, it is important that the personnel involved in the measurement is fully familiar with them and has the skills to carry them out. This concerns the team members who draw the blood samples and prepare them for transfer to the laboratory, as well as the laboratory personnel. WHO MONICA Project In the WHO MONICA Project , training seminars were organised for the persons who were responsible for the surveys in each centre. These then conducted the training of the local survey personnel. Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project the personnel was trained at the beginning of the project (14). Risk factor monitoring in Germany For the personnel at the sites of the German Federal Health Survey 1998 training sessions were organized prior to the start of the survey and procedures designed for possible re-training during the survey (24).
www.thl.fi/publications/ehrm/product1/section5.htm 13/23
01/10/13
5. Lipids measurements
NHANES III In NHANES III all personnel was required to successfully complete the CDC training course (38). Other surveys No information on the training of of survey or laboratory personnel was found for: Risk factor monitoring in the Netherlands, and UK National Health Surveys. 5.2.2 Laboratory quality control Internal Quality Control (IQC) The purpose of internal quality control is to check the short and long-term stability of the cholesterol measurement. A good performance in IQC is a prerequisite for successful participation in an external quality control programme and for reliable analysis of the survey samples. WHO MONICA Project Preparation of IQC pools: Each laboratory was to prepare at least two control serum pools, which should last through the whole survey period. One pool had to be prepared from non-turbid human serum containing "normal" total cholesterol and triglyceride concentrations. The pool was distributed in suitable aliquots into tightly closed glass vials and kept frozen at -60C or below. The pool was used both for total cholesterol and HDL- cholesterol method control, including the precipitation step in the latter case. The other pool was for low total cholesterol. It was to contain 1.30-1.60 mmol/l cholesterol. It could be prepared from a human serum pool diluted to the appropriate cholesterol concentration with 0.15m NaCL. Alternatively, animal (bovine, horse) serum pool, eventually slightly diluted to the desired cholesterol concentration level, could be used. This was the recommendation for the preparation of IQC pools, but other acceptable systems were specified in the MONICA Manual (13). The quality control specimen had to be treated in exactly the same way as the test samples. Each analytical run begun with calibration standard(s), followed by IQC samples. The results were used to indicate whether the run is in control and whether the analysis of study samples could begin. In each analytical run containing survey samples, quality control material was to be placed in every tenth position among the samples (to monitor within-run stability). This could be other than the IQC material specified above, and needed not necessarily be of human origin nor accurately calibrated because it served only for monitoring within-run reproducibility. The warning limits in the internal quality control were 3% for total cholesterol and 6% for HDL-cholesterol. The maximum allowable limits were 4.5% for total cholesterol and 9% for HDL-cholesterol. It the control values went beyond these, the run had to be stopped, results could not be used, the cause of trouble had to be eliminated, and the method had to be brought under control before the survey samples were started. Risk factor monitoring in Germany The German Federal Health Survey 1998 used two quality control samples before and after each set of 20 survey samples. Tolerance limits were set to between 4% and 6% (24). UK National Health Surveys
www.thl.fi/publications/ehrm/product1/section5.htm 14/23
01/10/13
5. Lipids measurements
The principles of the IQC are not available, except that in the analysis of cholesterol low, medium and high control materials are assayed with every 50 samples. For HDL a control was precipitated with each batch prior to assay. (36) NHANES III The central laboratory for NHANES III monitored its performance by analysing at regular interval throughout the day control material from the Centers for Disease Control and Prevention (CDC). Two control pools were in use, one with normal and one with elevated values (38). Risk factor monitoring in Norway In the National Cardiovascular Screening the stability of the analytical procedures was controlled by inserting a commercial reference serum among the actual sera (27). External Quality Control (EQC) EQC is complementary to the IQC and its main purpose is to check on accuracy (bias). A laboratory's cholesterol determinations can only be trusted if it can demonstrate a successful participation in an external quality control programme organised by a qualified reference laboratory. Two major international quality control programmes were organised, one by the WHO Regional Lipid Reference Centre (WHO-RLRC) in Prague, Czech Republic, and one by CDC, Atlanta, USA. The two reference laboratories were collaborating, to make sure that their standards were in mutual agreement. The reference laboratories prepared quality control pools. The reference values for cholesterol of the quality control pools were determined using the modified Abell Kendall reference method (62). The control systems were based on the repeated analysis of sets of control samples shipped from the reference laboratories to the participating laboratories. The sets usually contained three or four pools, with analytes at different concentrations. The control samples had to be used in the local laboratories according to the specified instructions for reconstitution and sequence of samples. The local laboratories reported the results of their control sample analyses to the reference laboratory, which evaluated them and sent further sets to the participating laboratories. The reference laboratories reviewed the methods used in the participating laboratories, and calculated the bias and standard deviation of the laboratories' results on the control samples. WHO MONICA Project For most of the MONICA Collaborating Centres, EQC was carried out by WHO-RLRC, and for some by CDC. For the control pools, the bias had to be within 5% for total cholesterol and 7.5% for HDL cholesterol. At the same time, standard deviations had to be smaller than those reported in the MONICA Manual (13). The results of the external quality control have been published in MONICA quality assessment reports (4, 5). For total cholesterol, the results improved during the 10-year period of the Project. For HDL-cholesterol, the report concluded: "In summary, the EQC results indicate that standardization of HDL cholesterol measurements was difficult to achieve and did not improve significantly during the MONICA Project. This can be partly due to (a) the different isolation and measurement procedures used by the participating laboratories, (b) the changes in HDL isolation procedures, (c) the changes in participating laboratories during the study period, (d) the use of lyophilised control pools, which increase the probability of undetectable matrix effects, and (e) the inability of some of the laboratories to maintain a sufficiently high quality of the procedures applied. Whether or not a much better
www.thl.fi/publications/ehrm/product1/section5.htm 15/23
01/10/13
5. Lipids measurements
standardization of HDL cholesterol measurements is feasible in such a multinational setting, remains an open question. The observed trend towards the acceptance of a limited number of HDL isolation and measurement procedures by most participating laboratories is likely to improve the comparability of data between RUAs in future studies." Risk factor monitoring in the Netherlands In the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project in the Netherlands all cholesterol determinations were performed at the Clinical Chemistry Laboratory of the University Hospital "Dijkzigt" in Rotterdam. This laboratory took part in the standardization programs of both WHO RLRC and CDC. It also serves as an international member of the Lipid Reference Laboratories Network in the USA (14, 61). Risk factor monitoring in Germany In the German Cardiovascular Prevention Study a serum was analysed at the laboratory the former Institute for Social Medicine and Epidemiology of the German Federal Health Office, Berlin (now Robert Koch-Institute). The laboratory took part in the standardization program of WHO RLRC. (23). The same laboratory also analysed the samples for the German Federal Health Survey 1998 (24) and participated in an external quality control program organized by DGKC (German Society for Clinical Chemistry) that required analysis of up to eight sets of test samples per year (24). UK National Health Surveys The laboratory participated in two quality assessment schemes: the United Kingdom National External Quality Assessment Schemes (UKNEQAS) and the Welsh External Quality Assessment Schemes (WEQAS). They are networks in which analytes are distributed to the participating laboratories at regular frequency, and the laboratories return the results to the scheme organiser. This then calculates the mean value over the laboratories, a measure of the between-laboratory precision, and the bias. (36) In these programmes, the bias is calculated from the mean of the participating laboratories, whereas in the external quality control provided by WHO RLRC and CDC, bias is calculated from the known reference values of the control pools. NHANES III In NHANES III, EQC was done by CDC (38). 5.2.3 Retrospective quality assessment report WHO MONICA Project In the WHO MONICA Project the quality of data of each MONICA centre was examined in thorough quality assessment reports after each survey (4, 5). The reports helped centres to prevent repetition of identified errors and to correct shortcomings when planning and executing the next surveys. Furthermore, for those who analysed the results of the Project the reports were an important source of information to understand the possible differences and limitations of the data from each population. NHANES III
www.thl.fi/publications/ehrm/product1/section5.htm 16/23
01/10/13
5. Lipids measurements
In NHANES III when analysis of the specimens is complete, the data are reviewed by the data coordinator or by the senior lab technician (preliminary review). After all necessary repeat analyses are completed, the results are then reviewed by the laboratory supervisor, data coordinator, or laboratory director (final review). The results are compared with ranges determined from the normal population distributions for adults. Any specimen whose value is outside the respective range is re-analysed. (38) Other surveys No information on retrospective quality assessment was found for: Risk factor monitoring in the Netherlands, Risk factor monitoring in Germany, and UK National Health Surveys.
5.3 Indicators used for reporting the results
In this section we describe indicators used in reporting the results of the different surveys. Some of the indicators also use data on the subjects' awareness and treatment of high cholesterol. More detailed discussion about the questionnaire data on awareness and treatment of high cholesterol is in chapter 11. WHO MONICA Project In the WHO MONICA Project the age/sex standardized population mean total cholesterol level is used when reporting the results (63). For the HDL cholesterol the age/sex standardized population mean is also used as well as the proportion of HDL cholesterol in total cholesterol (64). For prevalence indicators of total cholesterol the thresholds 5.2 mmol/L and 7.8 mmol/L are used. Prevalence indicators for HDL cholesterol are based on the limits 0.91 mmol/l and 1.30 mmol/l (64). Risk factor monitoring in the Netherlands In reports of the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project in the Netherlands the mean total cholesterol, mean HDL cholesterol, prevalence of hypercholesterolemia, and prevalence of low HDL were used. (14, 21) Hypercholesterolemia was defined according to the Dutch Cholesterol Consensus (total cholesterol > 6.5 mmol/l). (14, 65) The low HDL cholesterol was defined as HDL < 0.9 mmol/l (14). Risk factor monitoring in Germany In the German National Survey the high cholesterol level was reported as equal to or above, respectively, 5.7 mmol/l (220 mg/dl) and 6.5 mmol/l (250 mg/dl) as well as those with HDL cholesterol levels below 0.9 mmol/l (35 mg/dl). (23). No information could be located for the German Federal Health Survey 1998 UK National Health Surveys In the UK National Health Survey elevated cholesterol was considered to be 6.5 mmol/l. (36) NHANES III NHANES III has reported the percentage of the sample in the following categories (66): Total cholesterol
www.thl.fi/publications/ehrm/product1/section5.htm
HDL-cholesterol
LDL-cholesterol*
17/23
01/10/13
5. Lipids measurements
Desirable Borderline-High-Risk High-Risk
<5.2 mmol/l 5.2-6.2 mmol/l 6.2 mmol/l
0.91 mmol/l <0.91 mmol/l
<3.36 mmol/l 3.36-4.13 mmol/l 4.14 mmol/l
*LDL-cholesterol was calculated using the Friedewald formula: LDL = total cholesterol - HDL 0.45triglycerides. Risk factor monitoring in Norway In the National Cardiovascular Screening the proportion of respondents above 8 mmol/l was used for reporting (27).
5.4 Discussion and conclusions
Relatively small systematic bias in the measurements can have a significant effect in the estimates of population values of lipids. Therefore, at the pre-analytic stage, seasonal variation, plasma-serum difference, position of the subject during venipuncture and storage before analysis are issues where standardization is crucial. Serum is usually recommended for lipids because of the diluting effect of the anticoagulants, which are needed for plasma. However, plasma has the advantage that it can be centrifuged and analysed or frozen immediately to avoid deterioration of the sample. The time delay is not a problem for cholesterols or triglycerides, but it may be a problem if for example glucose is to be measured from the same sample. The position of the subject during venipuncture has a large effect on cholesterol. Sitting position appears to be more common than supine in the surveys reviewed. It is also probably easier to standardize in a survey, because in the supine position the subject would have to wait longer before the cholesterol level stabilises. From the analytical point of view, the lipid values should be analysed from fresh samples within a few days of collecting the samples. NHANES III decided to analyse everything in one laboratory and to freeze the samples for the transportation. Regardless of whether the transportation is done on fresh or frozen samples, it should be planned and conducted carefully. Analysis in a central laboratory was also carried out by the National Health Surveys in the UK and the German Federal Health Survey 1998. The logistics of transporting blood samples to a central laboratory obviously depends on the geography of the survey area and may be quite manageable in smaller countries. For triglycerides, 12 hours fasting is a crucial requirement, which implies that the samples are collected in the morning. However, it is often not practical to carry out a survey only in the morning, and this would also lower the comparability with other surveys, which were carried out throughout the day. This is probably one of the reasons why many of the reviewed surveys did not measure triglycerides. NHANES III solved the problem by measuring triglycerides only in a random half of the sample, and this half was examined in the mornings. Concerning the analytic stage, Cooper et al write: "Modern instruments allow remarkable precision (reproducibility of measurements) in cholesterol and other lipid determinations. Accuracy (mean deviation from the true value) is now the major problem." (11) This leaves the responsibility for the quality of the results to the laboratory team and to the standardization of the methods. For the American surveys, the standardization has been in the hands of CDC Atlanta for several decades using methods which guarantee stability of the reference values over the years. They have accumulated remarkable expertise in this regard. In Europe, lipid standardisation was carried out by WHO
www.thl.fi/publications/ehrm/product1/section5.htm 18/23
01/10/13
5. Lipids measurements
RLRC for twenty years, from 1970s to 1990s. It was using methods similar to CDC's, and the two crossvalidated each other's reference values regularly. Now, as WHO RLRC is no longer operating, it would be important to establish a replacement for it, which could serve European surveys. Such a reference laboratory would be needed both for providing secondary calibrators for the survey laboratories and for providing external quality control. Training and internal quality control are the key tools for the laboratory teams to assume their responsibility for data quality. For helping in this regard and in convincing the clients, standards (ISO/IEC 17025) and international cooperation in laboratory accreditation (International Laboratory Accreditation Cooperation, see http://www.ilac.org/) have been established in recent years. Laboratory accreditation provides a means of determining the competence of laboratories to perform testing, measurement and calibration. It also allows a laboratory to determine whether it is performing its work correctly and to appropriate standards. Simple and established methods for analysing total cholesterol have been available since the 1980s. This was also true for HDL-cholesterol, after first precipitating other subfractions of cholesterol from the samples. The complicating step was the precipitation, which added another possibility for human error to the analysis. This, combined with the finding of the MONICA Project that the changes within populations and differences between populations in cholesterol mean values are relatively small compared to the achievable accuracy of the measurements, puts a question mark on the feasibility of population monitoring of HDL cholesterol. (5) Since then, a new enzymatic method which does not require precipitation, has been established. Its use is essentially simpler than the use of the traditional methods, and therefore it is less error prone. This gives hope that monitoring of HDL cholesterol will become more feasible in the future. One reason for measuring triglycerides comes from the fact that, together with total cholesterol and HDLcholesterol, allows the estimatation of LDL-cholesterol. The estimation is done using the so called Friedewald formula. A limitation for this estimation is that it is valid only if triglyceride is less that 2.25-4.5 mmol/l (the cut-point varies between references, depending on the required accuracy). There exist now a number of direct methods for LDL measurement that work well for high triglyceride blood. Also the fasting status of subjects does not affect the results. As a result, the question whether triglycerides and LDL cholesterol should be measured in population studies can now be decided independently. Whether one central laboratory or an number of distributed laboratories close to the collection sites is best for a survey depends on many factors. Central laboratories have been used by NHANES III, the German Federal Health Survey 1998, the UK Health Survey and others. The arguments for a central laboratory are: i) expensive equipment and highly qualified technical expertise have to be maintained only at one site, ii) standardization of the laboratory procedures is easier to monitor, iii) data variance due to inter-laboratory variation is eliminated. The arguments against a central laboratory are: i) it is virtually impossible to perform tests on fresh samples, ii) data collection sites require equipment for sample preparation and storage, iii) an elaborate logistical system may have to be used the arrange and supervise sample transport (NHANES III used overnight courier service, the German Federal Health Survey 1998 maintained constant communication between central laboratory and data collection sites to prevent problems from arising), iv) storage time impacts on sample viability. Therefore, each survey has to decide on its own best solution, weighing the advantages and tradeoffs. References 1. Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta- analysis of population-based prospective studies. J
www.thl.fi/publications/ehrm/product1/section5.htm 19/23
01/10/13
5. Lipids measurements
2. 3. 4.
5.
6. 7.
8. 9.
10.
11. 12. 13.
14. 15. 16. 17. 18. 19. 20. 21.
Cardiovasc Risk 1996;3(2):213-9. Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousdian S, Kannel WB. Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham Study. Jama 1986;256(20):2835-8. Sprecher DL. Triglycerides as a risk factor for coronary artery disease. Am J Cardiol 1998;82(12A):49U56U; discussion 85U-6U. Ferrario M, Kuulasmaa K, Grafnetter D, Moltchanov V, for the WHO MONICA Project. Quality Assessment of Total Cholesterol Measurements in the WHO MONICA Project. (1999). Available from: URL:http://www.thl.fi/publications/monica/tchol/tcholqa.htm, URN:NBN:fi-fe19991083 Marques-Vidal P, Ferrario M, Kuulasmaa K, Grafnetter D, Moltchanov V, for the WHO MONICA Project. Quality assessment of data on HDL cholesterol in the WHO MONICA Project. (1999). Available from: URL:http://www.thl.fi/publications/monica/hdl/hdlqa.htm, URN:NBN:fi-fe19991137 Bleiler R, Yearnick E, Schnur S, Singson I, Ohlson M. Seasonal variation of cholesterol in serum of men and women. Am J Clin Nutr 1963;12:12-6. Frohlich M, Sund M, Russ S, Hoffmeister A, Fischer HG, Hombach V, Koenig W. Seasonal variations of rheological and hemostatic parameters and acute- phase reactants in young, healthy subjects. Arterioscler Thromb Vasc Biol 1997;17(11):2692-7. Robinson D, Bevan EA, Hinohara S, Takahashi T. Seasonal variation in serum cholesterol levels--evidence from the UK and Japan. Atherosclerosis 1992;95(1):15-24. Gordon DJ, Trost DC, Hyde J, Whaley FS, Hannan PJ, Jacobs DR, Jr., Ekelund LG. Seasonal cholesterol cycles: the Lipid Research Clinics Coronary Primary Prevention Trial placebo group. Circulation 1987;76(6):1224-31. Gordon DJ, Hyde J, Trost DC, Whaley FS, Hannan PJ, Jacobs DR, Ekelund LG. Cyclic seasonal variation in plasma lipid and lipoprotein levels: the Lipid Research Clinics Coronary Primary Prevention Trial Placebo Group. J Clin Epidemiol 1988;41(7):679-89. Cooper GR, Myers GL, Smith SJ, Schlant RC. Blood lipid measurements. Variations and practical utility. Jama 1992;267(12):1652-60. Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of serum lipids in an elderly population. Age Ageing 1993;22(4):273-8. WHO MONICA Project. MONICA Manual, Part III: Population Survey; Section 2: Standardization of lipid measurements. (1998). Available from: URL:http://www.thl.fi/publications/monica/manual/part3/iii2.htm, URN:NBN:fi-fe19981152 Verschuren W. The protocol of the Monitoring Project on Cardiovascular Disease Risk Factors and the MORGEN-project. Personal communicaton. 2001 Statistics Netherlands, Finnish National Public Health Institute. Database of the European Health Interview and Health Examination Survey. In; 1999. Viet L. The protocol of the REGENBOOG project. Personal communicaton. 2001 Demacker PN, Schade RW, Jansen RT, Van 't Laar A. Intra-individual variation of serum cholesterol, triglycerides and high density lipoprotein cholesterol in normal humans. Atherosclerosis 1982;45(3):259-66. Cooper GR, Myers GL, Smith SJ, Sampson EJ. Standardization of lipid, lipoprotein, and apolipoprotein measurements. Clin Chem 1988;34(8B):B95-105. Rivera-Coll A, Fuentes-Arderiu X, Diez-Noguera A. Circadian rhythmic variations in serum concentrations of clinically important lipids. Clin Chem 1994;40(8):1549-53. Cohn JS, McNamara JR, Cohn SD, Ordovas JM, Schaefer EJ. Postprandial plasma lipoprotein changes in human subjects of different ages. J Lipid Res 1988;29(4):469-79. Verschuren W, van Leer E, Blokstra A, Seidell J, Smit H, Bueno de Mesquita H, de Oberman-Boer G, Kromhout D. Cardiovascular disease risk factors in the Netherlands. Neth J Cardiol 1993;6:20510.
20/23
www.thl.fi/publications/ehrm/product1/section5.htm
01/10/13
5. Lipids measurements
22. REGENBOOG Project. Draaiboek voor de GGD-medewerker; December 1999. 23. Hoffmeister H, Mensink GB, Stolzenberg H, Hoeltz J, Kreuter H, Laaser U, Nussel E, Hullemann KD, Troschke JV. Reduction of coronary heart disease risk factors in the German cardiovascular prevention study. Prev Med 1996;25(2):135-45. 24. Thierfelder W, Seher C, Thefeld W. Der Bundes-Gesundheitssurvey 1997/98- Untersuchungsteil. Gesundheitswesen 1998;60 Suppl 2:S69-76. 25. Johnson CL, Rifkind BM, Sempos CT, Carroll MD, Bachorik PS, Briefel RR, Gordon DJ, Burt VL, Brown CD, Lippel K, et al. Declining serum total cholesterol levels among US adults. The National Health and Nutrition Examination Surveys. Jama 1993;269(23):3002-8. 26. Giampaoli S. Osservatorio Epidemiologico Cardiovasculare. Personal communicaton. 2001 27. Selmer R. Norwegian 40-year programme and the National Cardiovascular Screening in Norway. Personal communication. 2001 28. Fawcett J, Winn V. Effect of posture on plasma volume and some blood costituents. J Clin Path 1960;13:304-10. 29. Stoker DJ, Wynn V, Robertson G. Effect of posture on the plasma cholesterol level. Br Med J 1966;5483:336-8. 30. Tan MH, Wilmshurst EG, Gleason RE, Soeldner JS. Effect of posture on serum lipids. N Engl J Med 1973;289(8):416-9. 31. Statland BE, Bokelund H, Winkel P. Factors contributing to intra-individual variation of serum constituents: 4. Effects of posture and tourniquet application on variation of serum constituents in healthy subjects. Clin Chem 1974;20(12):1513-9. 32. Dixon M, Paterson CR. Posture and the composition of plasma. Clin Chem 1978;24(5):824-6. 33. Felding P, Tryding N, Hyltoft Petersen P, Horder M. Effects of posture on concentrations of blood constituents in healthy adults: practical application of blood specimen collection procedures recommended by the Scandinavian Committee on Reference Values. Scand J Clin Lab Invest 1980;40(7):615-21. 34. Kjeldsen SE, Eide I, Leren P, Foss OP. Effects of posture on serum cholesterol fractions, cholesterol ratio and triglycerides. Scand J Clin Lab Invest 1983;43(2):119-21. 35. Hagan RD, Upton SJ, Avakian EV, Grundy S. Increases in serum lipid and lipoprotein levels with movement from the supine to standing position in adult men and women. Prev Med 1986;15(1):18-27. 36. The Stationary Office. Health Survey of England, Cardiovascular disease. Volume 1: Findings; Volume 2: Methodology & Documentation. 1999. Available from: URL:http://www.officialdocuments.co.uk/document/doh/survey98/hse98.htm 37. U.S. Department of Health and Human Services. National Health and Nutrition Examination Survey III, cycle 2 manual for medical techicians. 1992. Available from: URL:http://www.cdc.gov/nchs/about/major/nhanes/nhanes3/cdrom/NCHS/MANUALS/BLOOD.PDF 38. Gunter E, Lewis B, SM K. Laboratory Procedures Used for the Third National Health and Nutrition Examination Survey (NHANES III), 1988-1994. 1996. Available from: URL:http://www.cdc.gov/nceh/dls/labman.pdf 39. Junge B, Hoffmeister H, Feddersen HM, Rocker L. [Standardisation of obtaining blood samples: influence of tourniquet application on 33 constituents of blood and serum (author's transl)]. Dtsch Med Wochenschr 1978;103(6):260-5. 40. Naito HK. Reliability of lipid, lipoprotein, and apolipoprotein measurements. Clin Chem 1988;34(8B):B8494. 41. Crombie IK, Smith WC, Tavendale RT, Clark EC, Tunstall-Pedoe HD. Venous occlusion and estimation of serum constituents. Lancet 1987;2(8565):975. 42. Laboratory Methods Committee LRCP. Cholesterol and triglyceride concentrations in serum/plasma pairs.
www.thl.fi/publications/ehrm/product1/section5.htm 21/23
01/10/13
5. Lipids measurements
43. 44. 45. 46.
47. 48. 49. 50.
51. 52. 53.
54. 55.
56. 57.
58.
59. 60.
61.
Clin Chem 1977;23(1):60-3. Cloey T, Bachorik PS, Becker D, Finney C, Lowry D, Sigmund W. Reevaluation of serum-plasma differences in total cholesterol concentration. Jama 1990;263(20):2788-9. Tietz N. Clinical guide to laboratory tests. 3rd ed. Philadelphia: Saunders; 1995. Ono T, Kitaguchi K, Takehara M, Shiiba M, Hayami K. Serum-constituents analyses: effect of duration and temperature of storage of clotted blood. Clin Chem 1981;27(1):35-8. Belcher J, McNamara JR, Grinstead G, et al. Measurement of low density lipoprotein cholesterol concentration. In: Rifai N, Wernick G, editors. Methods for clinical laboratory measurements of lipid and lipoprotein risk factors. Washington DC: AACC Press; 1991. Evans K, Mitcheson J, Laker MF. Effect of storage at 4 degrees C and -20 degrees C on lipid, lipoprotein, and apolipoprotein concentrations. Clin Chem 1995;41(3):392-6. Bausserman LL, Saritelli AL, Milosavljevic D. High-density lipoprotein subfractions measured in stored serum. Clin Chem 1994;40(9):1713-6. Rehak NN, Chiang BT. Storage of whole blood: effect of temperature on the measured concentration of analytes in serum. Clin Chem 1988;34(10):2111-4. Shih WJ, Bachorik PS, Haga JA, Myers GL, Stein EA. Estimating the long-term effects of storage at -70 degrees C on cholesterol, triglyceride, and HDL-cholesterol measurements in stored sera. Clin Chem 2000;46(3):351-64. Lipid Research Clinics Program. Manual of Laboratory Operations: Lipid and lipoprotein analysis. DHEW Publication NIH 75-628. Bethesda MD: National Institutes of Health; 1974, 1st revised 1982. Warnick GR, Nguyen T, Albers AA. Comparison of improved precipitation methods for quantification of high- density lipoprotein cholesterol. Clin Chem 1985;31(2):217-22. Sugiuchi H, Uji Y, Okabe H, Irie T, Uekama K, Kayahara N, Miyauchi K. Direct measurement of highdensity lipoprotein cholesterol in serum with polyethylene glycol-modified enzymes and sulfated alphacyclodextrin. Clin Chem 1995;41(5):717-23. Lopes-Virella MF, Stone P, Ellis S, Colwell JA. Cholesterol determination in high-density lipoproteins separated by three different methods. Clin Chem 1977;23(5):882-4. Bachorik PS, Walker RE, Virgil DG. High-density-lipoprotein cholesterol in heparin-MnCl2 supernates determined with the Dow enzymic method after precipitation of Mn2+ with HCO3. Clin Chem 1984;30(6):839-42. Bergmeyer H, Grassl M, editors. Methods of enzymatic analysis. Metabolites 3: Lipids, amino acids and related compounds, 3rd edition. Weinheim: Wiley-VCH; 1990. Kattermann R, Jaworek D, Moller G, Assmann G, Bjorkhem I, Svensson L, Borner K, Boerma G, Leijnse B, Desager JP, et al. Multicentre study of a new enzymatic method of cholesterol determination. J Clin Chem Clin Biochem 1984;22(3):245-51. Benlian P, Cansier C, Hennache G, Khallouf O, Bayer P, Duron F, Carrat F, Couderc R, Chazouilleres O, Bardet J, Bouchard P, Poupon R, Masliah J, Bereziat G. Comparison of a new method for the direct and simultaneous assessment of LDL- and HDL-cholesterol with ultracentrifugation and established methods. Clin Chem 2000;46(4):493-505. Hirany S, Li D, Jialal I. A more valid measurement of low-density lipoprotein cholesterol in diabetic patients. Am J Med 1997;102(1):48-53. McNamara JR, Cole TG, Contois JH, Ferguson CA, Ordovas JM, Schaefer EJ. Immunoseparation method for measuring low-density lipoprotein cholesterol directly from serum evaluated. Clin Chem 1995;41(2):232-40. Myers GL, Cooper GR, Winn CL, Smith SJ. The Centers for Disease Control-National Heart, Lung and Blood Institute Lipid Standardization Program. An approach to accurate and precise lipid measurements.
22/23
www.thl.fi/publications/ehrm/product1/section5.htm
01/10/13
5. Lipids measurements
62. 63.
64.
65. 66.
Clin Lab Med 1989;9(1):105-35. U.S. Department of Health and Human Services. Manual of instructions and protocols for laboratory quality control in the Lipid Research Clinics Program. Atlanta GA: Centers for Disease Control; 1978. Kuulasmaa K, Tunstall-Pedoe H, Dobson A, Fortmann S, Sans S, Tolonen H, Evans A, Ferrario M, Tuomilehto J, for the WHO MONICA Project. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet 2000;355(9205):675-87. Tolonen H, Kuulasmaa K, Ruokokoski E, for the WHO MONICA Project. MONICA Population Survey Data Book. (2000). Available from: URL:http://www.thl.fi/publications/monica/surveydb/title.htm, URN:NBN:fi-fe20001206 Erkelens DW. Cholesterol consensus in The Netherlands. Consensus Preparatory Committee. Eur J Clin Nutr 1989;43(2):89-96. Sempos CT, Cleeman JI, Carroll MD, Johnson CL, Bachorik PS, Gordon DJ, Burt VL, Briefel RR, Brown CD, Lippel K, et al. Prevalence of high blood cholesterol among US adults. An update based on guidelines from the second report of the National Cholesterol Education Program Adult Treatment Panel. Jama 1993;269(23):3009-14. Previous (Section 4.) Next (Section 6.)
Contents
www.thl.fi/publications/ehrm/product1/section5.htm
23/23
Вам также может понравиться
- Inked CultureДокумент90 страницInked Culturemar phisОценок пока нет
- INTP Parents - 16personalitiesДокумент4 страницыINTP Parents - 16personalitiescelinelbОценок пока нет
- Floret Fall Mini Course Dahlia Sources Updated 211012Документ3 страницыFloret Fall Mini Course Dahlia Sources Updated 211012Luthfian DaryonoОценок пока нет
- Figure 1: Basic Design of Fluidized-Bed ReactorДокумент3 страницыFigure 1: Basic Design of Fluidized-Bed ReactorElany Whishaw0% (1)
- PulpectomyДокумент3 страницыPulpectomyWafa Nabilah Kamal100% (1)
- CD005425 AbstractДокумент3 страницыCD005425 AbstractokisutartoОценок пока нет
- Study of Lipid Profile in Coronary Heart Disease Patients in LibyaДокумент9 страницStudy of Lipid Profile in Coronary Heart Disease Patients in LibyaInternational Medical PublisherОценок пока нет
- Analysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Документ9 страницAnalysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Aleksa CopicОценок пока нет
- Fasting and Nonfasting LDL Cholesterol: To Measure or Calculate?Документ5 страницFasting and Nonfasting LDL Cholesterol: To Measure or Calculate?OKTAFIRANI AL SASОценок пока нет
- Association Between Fluid Overload and SOFA Score Kinetics in Septic Shock Patients: A Retrospective Multicenter StudyДокумент18 страницAssociation Between Fluid Overload and SOFA Score Kinetics in Septic Shock Patients: A Retrospective Multicenter StudydaliaОценок пока нет
- Pi Is 1499267115008965Документ6 страницPi Is 1499267115008965Nefri ArshintaОценок пока нет
- Plasma Lipids: Optimal Levels for HealthОт EverandPlasma Lipids: Optimal Levels for HealthAmerican Health FoundationОценок пока нет
- Effects of High Flavonol Dark Chocolate On Cardiovascular Function and Platelet AggregationДокумент9 страницEffects of High Flavonol Dark Chocolate On Cardiovascular Function and Platelet AggregationAnindya MMОценок пока нет
- Case Study 2. Lipid AbnormalitiesДокумент3 страницыCase Study 2. Lipid AbnormalitiesBryan Christian MadeloОценок пока нет
- High Prevalence of Undiagnosed Diabetes Mellitus in Southern Germany: Target Populations For Efficient Screening. The KORA Survey 2000Документ8 страницHigh Prevalence of Undiagnosed Diabetes Mellitus in Southern Germany: Target Populations For Efficient Screening. The KORA Survey 2000Novia ChrisnawatiОценок пока нет
- Nutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsДокумент15 страницNutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsMutiara Putri UtamiОценок пока нет
- Comparison of The Relationships of Alcoholic and Nonalcoholic Fatty Liver With Hypertension, Diabetes Mellitus, and DyslipidemiaДокумент7 страницComparison of The Relationships of Alcoholic and Nonalcoholic Fatty Liver With Hypertension, Diabetes Mellitus, and DyslipidemiaNurul MaulidaОценок пока нет
- Dyson LineДокумент10 страницDyson LineSharly DwijayantiОценок пока нет
- The Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsДокумент6 страницThe Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsjoelОценок пока нет
- Sdarticle1 La HoreДокумент20 страницSdarticle1 La HoreLuis Eduardo SantosОценок пока нет
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsДокумент9 страницThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaОценок пока нет
- Efficacy and Safety of Inositol Ate in Diabetic DyslipidemiaДокумент10 страницEfficacy and Safety of Inositol Ate in Diabetic DyslipidemiavanigvОценок пока нет
- Nejmoa 032782Документ10 страницNejmoa 032782elvinegunawanОценок пока нет
- Implications of The United Kingdom Prospective Diabetes StudyДокумент5 страницImplications of The United Kingdom Prospective Diabetes StudyAgustin MendezОценок пока нет
- Glycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsДокумент15 страницGlycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsLisiane PerinОценок пока нет
- ANNALS DyslipidemiaДокумент16 страницANNALS Dyslipidemiaewb100% (1)
- Hypertension Prevalence, Awareness, Control and Association With Metabolic Abnormalities in The San Marino Population: The SMOOTH StudyДокумент7 страницHypertension Prevalence, Awareness, Control and Association With Metabolic Abnormalities in The San Marino Population: The SMOOTH StudyIndah SundariОценок пока нет
- Nutrition, Metabolism & Cardiovascular Diseases: B.A. Kappel, N. Marx, M. FedericiДокумент9 страницNutrition, Metabolism & Cardiovascular Diseases: B.A. Kappel, N. Marx, M. Federicirachel0301Оценок пока нет
- Artigo - Uva e Compostos FenólicosДокумент12 страницArtigo - Uva e Compostos Fenólicospedrovanderley13Оценок пока нет
- Monitoring The Metabolic Side-Effects of Atypical AntipsychoticsДокумент6 страницMonitoring The Metabolic Side-Effects of Atypical AntipsychoticsAdina OlteanuОценок пока нет
- Remnant Cholesterol As A Causal Risk Factor For Ischemic Heart DiseaseДокумент10 страницRemnant Cholesterol As A Causal Risk Factor For Ischemic Heart DiseaseIonuț CozmaОценок пока нет
- Perspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsДокумент7 страницPerspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsHania Asmarani RahmanitaОценок пока нет
- Lipid Profile: 1 Components 3 ImplicationsДокумент3 страницыLipid Profile: 1 Components 3 ImplicationsZiedTrikiОценок пока нет
- Habitual Chocolate Consumption and The Risk of Incident Heart Failure Among Healthy Men and WomenДокумент13 страницHabitual Chocolate Consumption and The Risk of Incident Heart Failure Among Healthy Men and WomenxiuhtlaltzinОценок пока нет
- Chapter Five AbdokafiДокумент3 страницыChapter Five AbdokafiibrahimОценок пока нет
- Metabolic ControlДокумент9 страницMetabolic ControlRommanah AzmiОценок пока нет
- Prevention of Hypertension in Patients With Pre-Hypertension: Protocol For The PREVER-prevention TrialДокумент7 страницPrevention of Hypertension in Patients With Pre-Hypertension: Protocol For The PREVER-prevention TrialhahahaОценок пока нет
- Journey in Guidelines For Lipid Management: From Adult Treatment Panel (ATP) - I To ATP-III and What To Expect in ATP-IVДокумент9 страницJourney in Guidelines For Lipid Management: From Adult Treatment Panel (ATP) - I To ATP-III and What To Expect in ATP-IVNiluh putu Satria maharaniОценок пока нет
- 2010-Fasting For Haematological TestДокумент6 страниц2010-Fasting For Haematological Testpedro vargasОценок пока нет
- Prevalence of Metabolic Syndrome and Its Associated Factors Among Thai Police Officers - A Population-Based StudyДокумент10 страницPrevalence of Metabolic Syndrome and Its Associated Factors Among Thai Police Officers - A Population-Based StudyRonald WiradirnataОценок пока нет
- Jurnal InggrisДокумент8 страницJurnal InggrisEry ShaffaОценок пока нет
- The Relationship Between Hba1C and Lipid Profile in Type 2 Diabetic Saudi PatientsДокумент6 страницThe Relationship Between Hba1C and Lipid Profile in Type 2 Diabetic Saudi PatientsnaxxxОценок пока нет
- Urban-Rural Disease Its Factors: Differences in The Prevalence of Coronary Heart and Risk in DelhiДокумент8 страницUrban-Rural Disease Its Factors: Differences in The Prevalence of Coronary Heart and Risk in DelhiputiridhaОценок пока нет
- WHO - Haemoglobin Level For Anemia 2011Документ6 страницWHO - Haemoglobin Level For Anemia 2011Adhi SanjayaОценок пока нет
- Lyon Diet Heart Study - de Lorgeril 1994Документ6 страницLyon Diet Heart Study - de Lorgeril 1994acolpoОценок пока нет
- JURNAL ANEMIA PADA CKD P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Документ7 страницJURNAL ANEMIA PADA CKD P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Arv IraОценок пока нет
- Metabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismДокумент7 страницMetabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismMaria Alice BourneufОценок пока нет
- Fibrin GenДокумент7 страницFibrin GenGarawee AliОценок пока нет
- Euu 2Документ10 страницEuu 2Johanna GalvisОценок пока нет
- ADA Scientific 2000Документ6 страницADA Scientific 2000Rahmah Gadis Wartania PutriОценок пока нет
- Clinica Chimica Acta: SciencedirectДокумент6 страницClinica Chimica Acta: SciencedirectIndra AjaОценок пока нет
- A Nutraceutical Combination Improves Insulin Sensitivity in Patients With Metabolic SyndromeДокумент7 страницA Nutraceutical Combination Improves Insulin Sensitivity in Patients With Metabolic SyndromegiannidietОценок пока нет
- Lipid Profile PatternДокумент5 страницLipid Profile PatternPhrycilia LimenОценок пока нет
- Medicina 55 00687 v2 PDFДокумент16 страницMedicina 55 00687 v2 PDFAwatiful AzzaОценок пока нет
- Applied-A Correlative Study of Hypertension-Raksha GoyalДокумент8 страницApplied-A Correlative Study of Hypertension-Raksha GoyalImpact JournalsОценок пока нет
- Cohort Profile: The Japan Diabetes Complications Study: A Long-Term Follow-Up of A Randomised Lifestyle Intervention Study of Type 2 DiabetesДокумент9 страницCohort Profile: The Japan Diabetes Complications Study: A Long-Term Follow-Up of A Randomised Lifestyle Intervention Study of Type 2 DiabetesPutri HakimОценок пока нет
- IJC - Smokingcessationmanuscript - Accepted VersionДокумент18 страницIJC - Smokingcessationmanuscript - Accepted VersionUnderdog EsportОценок пока нет
- Labcomp FДокумент23 страницыLabcomp Fking peaceОценок пока нет
- 1 s2.0 S0022316622105067 MainДокумент7 страниц1 s2.0 S0022316622105067 MainqixiadeyouxiangОценок пока нет
- tmp7639 TMPДокумент6 страницtmp7639 TMPFrontiersОценок пока нет
- DZ Tip II CancerДокумент7 страницDZ Tip II CancerAndreeaGheorgheОценок пока нет
- Prevalence, Patterns, and Associations of Dyslipidemia Among Sri Lankan Adults-Sri Lanka Diabetes and Cardiovascular Study in 2005-2006Документ8 страницPrevalence, Patterns, and Associations of Dyslipidemia Among Sri Lankan Adults-Sri Lanka Diabetes and Cardiovascular Study in 2005-2006Rekha NirwanОценок пока нет
- Lab 9 (Biochemical Test) - Edited PDFДокумент2 страницыLab 9 (Biochemical Test) - Edited PDFrzhrsОценок пока нет
- Hba1C: Predictor of Dyslipidemia and Atherogenicity in Diabetes MellitusДокумент3 страницыHba1C: Predictor of Dyslipidemia and Atherogenicity in Diabetes MellitusPramod Reddy EvuriОценок пока нет
- Association Between Protein Intake and Mortality in Hypertensive Patients Without Chronic Kidney Disease in The OLD-HTA CohortДокумент14 страницAssociation Between Protein Intake and Mortality in Hypertensive Patients Without Chronic Kidney Disease in The OLD-HTA Cohortluis Gomez VallejoОценок пока нет
- An Energy Saving Guide For Plastic Injection Molding MachinesДокумент16 страницAn Energy Saving Guide For Plastic Injection Molding MachinesStefania LadinoОценок пока нет
- BKM 10e Ch07 Two Security ModelДокумент2 страницыBKM 10e Ch07 Two Security ModelJoe IammarinoОценок пока нет
- TCJ Series: TCJ Series - Standard and Low Profile - J-LeadДокумент14 страницTCJ Series: TCJ Series - Standard and Low Profile - J-LeadgpremkiranОценок пока нет
- Power Divider and Combiner: EE403-Microwave Engineering MTC, EE Dep., Electromagnetic Waves GroupДокумент52 страницыPower Divider and Combiner: EE403-Microwave Engineering MTC, EE Dep., Electromagnetic Waves GroupHabibat El Rahman AshrafОценок пока нет
- As Level Chemistry Practical Paper 3 - GCE GuideДокумент1 страницаAs Level Chemistry Practical Paper 3 - GCE GuideJamal AldaliОценок пока нет
- Geography - Development (Rural - Urban Settlement)Документ32 страницыGeography - Development (Rural - Urban Settlement)jasmine le rouxОценок пока нет
- Coarse DispersionsДокумент35 страницCoarse Dispersionsraju narayana padala0% (1)
- 2015 12 17 - Parenting in America - FINALДокумент105 страниц2015 12 17 - Parenting in America - FINALKeaneОценок пока нет
- Measurement of Bioreactor K AДокумент18 страницMeasurement of Bioreactor K AAtif MehfoozОценок пока нет
- Aakanksha ProjectДокумент32 страницыAakanksha ProjectAakash murarkaОценок пока нет
- BCA2006 BCA GuideДокумент507 страницBCA2006 BCA GuidePatrick LiaoОценок пока нет
- Plumbing Breakup M 01Документ29 страницPlumbing Breakup M 01Nicholas SmithОценок пока нет
- SSP 465 12l 3 Cylinder Tdi Engine With Common Rail Fuel Injection SystemДокумент56 страницSSP 465 12l 3 Cylinder Tdi Engine With Common Rail Fuel Injection SystemJose Ramón Orenes ClementeОценок пока нет
- Rajivgandhi University of Health Sciences Bangalore, KarnatakaДокумент19 страницRajivgandhi University of Health Sciences Bangalore, KarnatakaHUSSAINA BANOОценок пока нет
- Public Conveyances: Environments in Public and Enclosed Places"Документ1 страницаPublic Conveyances: Environments in Public and Enclosed Places"Jesse Joe LagonОценок пока нет
- Tcu Module Pe1 Lesson 1Документ7 страницTcu Module Pe1 Lesson 1Remerata, ArcelynОценок пока нет
- He 3 Basic Types of Descriptive Research MethodsДокумент2 страницыHe 3 Basic Types of Descriptive Research MethodsRahul SarinОценок пока нет
- Lesson Plan PPEДокумент3 страницыLesson Plan PPEErika Jean Moyo ManzanillaОценок пока нет
- Boeco BM-800 - User ManualДокумент21 страницаBoeco BM-800 - User ManualJuan Carlos CrespoОценок пока нет
- Powerful Communication Tools For Successful Acupuncture PracticeДокумент4 страницыPowerful Communication Tools For Successful Acupuncture Practicebinglei chenОценок пока нет
- Chapter One - FiveДокумент118 страницChapter One - FivePrecious AnthonyОценок пока нет
- BR Interlock Pallet Racking System 2009 enДокумент8 страницBR Interlock Pallet Racking System 2009 enMalik Rehan SyedОценок пока нет
- Aromatic Electrophilic SubstitutionДокумент71 страницаAromatic Electrophilic SubstitutionsridharancОценок пока нет
- Tackling Food Inflation: Ashwinkumar Kokku - 67 Malcolm Pinto - 89 Samir Vele - Nitin JadhavДокумент9 страницTackling Food Inflation: Ashwinkumar Kokku - 67 Malcolm Pinto - 89 Samir Vele - Nitin JadhavMalcolm PintoОценок пока нет
- People of The Philippines V. Crispin Payopay GR No. 141140 2003/07/2001 FactsДокумент5 страницPeople of The Philippines V. Crispin Payopay GR No. 141140 2003/07/2001 FactsAb CastilОценок пока нет