Академический Документы
Профессиональный Документы
Культура Документы
A Cheaper Hospital in Five Days PDF
Загружено:
sweta_starОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A Cheaper Hospital in Five Days PDF
Загружено:
sweta_starАвторское право:
Доступные форматы
Get a Cheaper
(More Profitable)
Hospital in Five Days
A Special Report by Jay Arthur
It should come as no surprise that a faster, better hospital will be cheaper to operate and more
profitable. When youre not dealing with all of the delays in the ED-Admission-Discharge
process, fewer patients will be boarded in the ED, reducing diversion and LWOBS. More
patients can be seen more quickly, increasing revenue. When youre not dealing with the extra
costs of preventable falls, infections and medication errors, it will make the hospital more cost
effective and profitable.
Faster + Better = Cheaper and More Profitable!
And there are other opportunities. Most hospitals have too many problems with rejected,
appealed and denied claims costing millions! Lean Six Sigma can help reduce billing problems
among other operational problems. And the process is simple.
To reduce rejected, appealed and denied claims, use Six Sigma tools to focus the improvement
effort.
1. Analyze Claims using control charts and pareto charts
Rejected
Appealed
Denied
2010 KnowWare International Inc. 888-468-1537 1
info@qimacros.com
2. Analyze the Root Causes using the Dirty 30 process
3. Implement Countermeasures
4. Track Results
Reducing Denied Claims In Five Days
Denied claims mean no money for services rendered because the billing process failed in some
way. Non-payment drives up the cost of healthcare and pushes many hospitals toward
bankruptcy. In this case study, monthly denials were over $1 million (XmR chart).
Charges Coded as Denials
$2,552,122 UCL
CL $1,071,509
LCL $(409,103)
$(1,000,000)
$(500,000)
$-
$500,000
$1,000,000
$1,500,000
$2,000,000
$2,500,000
$3,000,000
10/02 11/02 12/02 01/03 02/03 03/03 04/03 05/03 06/03 07/03 08/03 09/03
2002-2003
C
h
a
r
g
e
s
Denials (E)
UCL
+2 Sigma
+1 Sigma
Average
-1 Sigma
-2 Sigma
LCL
2010 KnowWare International Inc. 888-468-1537 2
info@qimacros.com
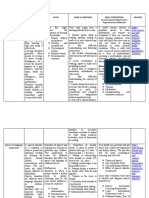
Using Pareto Charts of Denials
Using Excel PivotTables and the QI Macros, it was easy to narrow the focus to a few key areas
for improvement: Timely Filing (61%) and one insurer (67% of Timely Filling denials):
Denial-No Appeal Charges
$150
$109,813
$336,270
$750,766
$1,295,032
$2,516,508
$7,849,569
100%
99%
97%
91%
81%
61%
$-
$1,607,264
$3,214,527
$4,821,791
$6,429,054
$8,036,318
$9,643,582
$11,250,845
$12,858,109
Timely Filing Medical
Necessity
No Auth Partial Auth Invalid Auth ET ES
Memo Code
A
m
o
u
n
t
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=12858108.93
Denials for Timely Filing by Insurer
1 1 1 4 4 7 11 14 15 18
24 24 27
45
81
501
100% 100% 100%
99% 99%
98%
96%
94%
93%
90%
87%
84%
81%
75%
64%
0
97.25
194.5
291.75
389
486.25
583.5
680.75
778
Ins 1 Ins 2 Ins 3 Ins 4 Ins 5 Ins 6 Ins 7 Ins 8 Ins 9 Ins 10 Ins 11 Ins 12 Ins 13 Ins 14 Ins 15 Ins 16
Payer
N
u
m
b
e
r
o
f
D
e
n
i
a
l
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=778
2010 KnowWare International Inc. 888-468-1537 3
info@qimacros.com
Analyze Root Causes and Initiate Countermeasures
In a half-day root cause analysis session, the team identified ways to change the process
to work around the denials and change the contract process to 1) reduce delays that
contribute to timely filling denials and work with the insurer to resolve excessive denials.
Verify Results:
After implementing the process changes the following Monday, denied claims fell by $380,000
per month ($15 million/year). XmR chart below shows denials before and after improvement.
2010 KnowWare International Inc. 888-468-1537 4
info@qimacros.com
Reducing Rejected Claims In Five Days
In software we have a saying that finding a bug in a computer program is like finding a
cockroach in your hotel room. You dont say: Oh, theres a bug. You say: The place is infested.
The same is true of rejected claims. Start with a line or control chart of rejects:
Use a series of Pareto charts to narrow your focus:
2010 KnowWare International Inc. 888-468-1537 5
info@qimacros.com
Rejected claims are the frequent type of error; appeals tie up accounts receivable, and denials
result in lost revenue. How can we use Lean Six Sigma? Start with rejected claims.
Categorize Rejected Claims
Rejects by Type
$364,234 $893,878 $917,622 $1,789,756 $1,941,177 $2,266,610
$3,098,585
$4,163,173
$5,440,543
$9,999,612
$19,993,417 $20,135,403 $20,410,036 $20,435,973
$40,418,050
100% 99%
99%
97%
96%
95%
93%
90%
86%
80%
67%
53%
40%
27%
$-
$19,033,508
$38,067,017
$57,100,525
$76,134,034
$95,167,542
$114,201,050
$133,234,559
$152,268,067
D
u
p
C
l
a
i
m
N
o
C
o
v
e
r
a
g
e
A
d
d
'
t
I
n
f
o
R
e
q
'
d
P
r
o
v
i
d
e
r
I
n
f
o
R
e
q
'
d
I
n
c
o
r
r
e
c
t
I
n
s
I
n
f
o
D
6
D
7
D
8
D
9
D
1
0
D
1
1
D
1
2
D
1
3
D
1
4
D
1
5
Type
A
m
o
u
n
t
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=152268067.28
Duplicate claims accounts for 27% of rejected claims. The next four bars of the pareto chart
combined with duplicate claims accounts for 80% of all rejected claims. Each of these five bars
of the pareto chart is an improvement story requiring root cause analysis. Lets take duplicate
claims down to the next level of pareto chart.
2010 KnowWare International Inc. 888-468-1537 6
info@qimacros.com
Duplicate Claims Verification
1 1 1 1 1 1 1
5
60
99%
97%
96%
94%
93%
92%
90%
83%
0
9
18
27
36
45
54
63
72
Medicare
Forward to
Secondary
Carrier
PTBAL billed for pt
portion after
insurance
pmt
billed
secondary
again after
primary
payment
Denied IC second bill
being sent
for pt portion
UK Unknown
C
l
a
i
m
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=72
In this example, secondary payments for Medicare patients accounts for 83% of the duplicate
claims. The team investigated 72 of these secondary payments and found that they had been
paid, but incorrectly coded in accounting. Simple process changes reduced duplicate claims by
$24 million.
Teams Continued With the Other Four Big Bars
No Coverage turned out to be caused by charges after policy termination (44%).
2010 KnowWare International Inc. 888-468-1537 7
info@qimacros.com
No Coverage by Code
1 1 2 3 3 5 5 5
10
14
21 22
26
34
106
202
100% 100% 99%
98%
98%
97%
96%
95%
92%
89%
85%
80%
74%
67%
44%
0
57.5
115
172.5
230
287.5
345
402.5
460
C
A
T
C
I
P
C
O
V
N
C
D
I
P
#
P
E
I
A
P
R
E
S
D
E
P
L
I
M O
D
E
P
E
N
D
N
S
C
C
B
T
N
F
S
T
U
C
l
a
i
m
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=460
DZ Codes
CAT Charges after Policy Termination
CIP Cannot Identify Patient
COV Coverage
COV Treatment not Covered
DEP Dependent
IAP Invalid Alpha Prefix
IP# Invalid Policy Number
LIM Limits Exceeded
NCD No Coverage for DOS
NF No Fault
NSC No Service Coverage
O Other
PE Presumptive Eligibility
Invalid Insurer info led to SSN incorrect and wrong primary insurer (51%).
Invalid Insurer Info
28
8 8 8 9
20
22 23
54
77
89%
86%
83%
80%
76%
68%
60%
51%
30%
0
32.125
64.25
96.375
128.5
160.625
192.75
224.875
257
SSI OIN VOU CAT CIP NAME ADR NCD PTB OTHER
Code
C
l
a
i
m
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=257
SSI - Social Security Incorrect
OIN - Other Insurer Primary
VOU - Voucher
CAT Charges after Policy Termination
CIP Cannot identify Patient
NAME - Correct Pts Name
ADR - Incorrect Ins Address
NCD - Treatment not Covered
PTB - No MCR Part B
Patient Info rejects led to analysis of Other Insurance (41%) and students missing from parents
insurance (39%).
2010 KnowWare International Inc. 888-468-1537 8
info@qimacros.com
Patient Info Required Rejects
3 3
6
9
10
59
63
98%
96%
92%
86%
80%
41%
0
19.125
38.25
57.375
76.5
95.625
114.75
133.875
153
Other Insurance Students Other Other
Dependents
Babies Auto Demographic
C
l
a
i
m
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=153
Results
Half-day root cause analysis sessions for each of the big bars on these pareto charts and
subsequent improvements resulted in dramatic improvement in first pass yield of insurance
claims.
72% reduction in ED billing errors
60% reduction in impacted charges
2010 KnowWare International Inc. 888-468-1537 9
info@qimacros.com
Reducing Appealed Claims in Five Days
Delayed payments caused by appealed claims can put a hospital in a financial crunch. In 2003,
appealed claims spiked due to Medicare Part B changes. The recent healthcare reform legislation
and subsequent changes will most likely cause further spikes.
Reject Appeals Chart
$15,045,583 UCL
CL $8,363,312
LCL $1,681,040
$1,681,040
$3,681,040
$5,681,040
$7,681,040
$9,681,040
$11,681,040
$13,681,040
$15,681,040
$17,681,040
10/02 11/02 12/02 01/03 02/03 03/03 04/03 05/03 06/03 07/03 08/03 09/03
Date/Time/Period
R
e
j
e
c
t
A
p
p
e
a
l
s
Reject Appeals
UCL
+2 Sigma
+1 Sigma
Average
-1 Sigma
-2 Sigma
LCL
2010 KnowWare International Inc. 888-468-1537 10
info@qimacros.com
Use Pareto Charts to Analyze Appealed Claims:
There is a number of ways to analyze appeals data: by patient and appeal type:
Reject Appeals
$19,441 $32,456 $33,063 $243,241
$906,352 $1,077,005 $1,346,122 $1,361,097
$13,997,941
$81,343,021
100% 100% 100% 100%
99%
98%
96%
95%
81%
$-
$12,544,967
$25,089,935
$37,634,902
$50,179,869
$62,724,837
$75,269,804
$87,814,771
$100,359,739
ED-
InPatient
1 2 3 4 5 6 7 8 9
FC
C
h
a
r
g
e
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=100359738.510001
Reject Appeals
$3,256
$8,149,240
$12,302,541
$15,341,703
$64,562,998
100%
92%
80%
64%
$-
$12,544,967
$25,089,935
$37,634,902
$50,179,869
$62,724,837
$75,269,804
$87,814,771
$100,359,739
Auth Precert
Notification
Medical Necessity No Cert/Recert for days Timely Filing FC
Type
A
m
o
u
n
t
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=100359738.51
2010 KnowWare International Inc. 888-468-1537 11
info@qimacros.com
From these pareto charts, authorization and pre-certification of admissions from the ED are the
most common and costly appeals. Root cause analysis required team members from the ED and
Time
admissions to identify and reduce Auth/Precert appeals.
Reducing Appealed Claims Cycle
Appeals Delays
0
5000
10000
15000
20000
25000
30000
35000
40000
0 -
180
180 -
360
360 -
540
540 -
720
720 -
900
900 -
1,080
1,080
-
1,260
1,260
-
1,440
1,440
-
1,620
1,620
-
1,800
1,800
-
1,980
1,980
-
2,160
2,160
-
2,340
2,340
-
2,520
2,520
-
2,700
Days
N
u
m
b
e
r
o
f
A
p
p
e
a
l
s
Auth/Precert Appeals by Patient Type
7
105
266
309
429
1543
2839
100%
98%
93%
88%
80%
52%
0
687.25
1374.5
2061.75
2749
3436.25
4123.5
4810.75
5498
In Out S V R E F
Patient Type
N
u
m
b
e
r
o
f
F
B
M
e
m
o
s
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
n=5498
2010 KnowWare International Inc. 888-468-1537 12
info@qimacros.com
Using the simple tools of Lean (Post-it Notes), it was possible to redesign the appeals process to:
Reduce touches per account from 21 down to 11
Minutes per touch (16 minutes)
2.97 hours saved per account
Accelerate payment by 50 days
Other Examples
In 2002, rural hospital, Thibodaux Regional Medical Center, used Lean Six Sigma to reduced
discharged not final billed from $3.3 million to $600,000. They also reduced net accounts
receivable from 73 days to 62 days resulting in an increased cash flow of $2 million per year. A
In 2 6 a to reduce oncology
billing errors (missing charges) from 50 percent to only 2.5 percent. This resulted in increased
rev o reduced turnaround time for charge entry from 3.7 to
2.4 days and DOS-to-billing from 13.6 days to 6.8 days. The biggest factor in timely filing of
bills acy:
second wave of projects saved an addition $489,000 per year in inventory costs.
00 , North Shore Long Island Jewish Health System used Six Sigm
enue of $4 million per year. They als
: missing information. Biggest culprit, pharm
2010 KnowWare International Inc. 888-468-1537 13
info@qimacros.com
How to Get a Cheaper Hospital in Five Days
From working with teams in various industries, Ive developed a simple method for achieving
breakthrough improvement on transactional processes like billing. I call it the Dirty Thirty
Process. I used it in the case study presented in this white paper.
The Dirty 30 Process for Better Billing
The secret is to:
1. Quantify the cost of correcting these rejected, appealed and denied transactions
2. Understand the pareto pattern of rejected, appealed and denied transactions
3. Analyze 30-50 rejected, appealed or denied transactions to determine the root cause
4. Revise the process and system system to prevent the rejected, appealed or denied claim.
to understand each error. Detailed analysis of 30 errors in each of the top error buckets (i.e.,
all
1. Focus: Determine which rejected, appealed or denied error buckets to analyze first for
revent the
3. Sustain: Track the rejected, appealed and denied claims after implementation of the changes.
4. Honor: Recognize and reward team members
Process: Typical root cause analysis simply does not work because of the level of detail required
The Dirty Thirty) led to a breakthrough in understanding of how errors occurred and how to
prevent them. Simple checksheets allowed the root cause to pop out from analysis of this sm
sample. As expected, the errors clustered in a few main categories. The Dirty Thirty process has
four steps:
maximum benefit. (This analysis takes 2 to 3 days.)
2. Improve: Use the Dirty Thirty approach to analyze root causes (4 hours per error type
facilitator with team) and determine process and system changes necessary to p
problem.
2010 KnowWare International Inc. 888-468-1537 14
info@qimacros.com
Insights
Using the basic tools of Six Sigma, anyone can learn to use what I call The Dirty Thirty Process
in a day or less to find the root causes of transaction errors. Once a team has found the root
causes of these errors, its just a matter of changing the processes and systems to eliminate these
errors.
Hundreds of people spend their lives fixing the fallout from these rejected, appealed and denied
fixing things that shouldnt be
wrong to begin with.
get to where you can prevent errors, every system could benefit from a simple, yet
the data required to implement it is collected by most systems automatically. Then all it takes is 4
each error.
ance?
ent
ur, the KnowWare Man, works with hospitals that want to get faster, better and cheaper
claims. And they all think theyre doing meaningful work, not just
Conclusion
Until you
rigorous approach to analyzing and eliminating errors. The Dirty Thirty process is ideal because
to 8 hours of analysis to identify the root cause of
Need Guid
The first project may seem scary, but we can facilitate your improvement teams to achieve
breakthroughs in patient flow. Once youve learned how, youll find it easy to continue. Hav
you waited long enough to get a faster hospital in five days or less?
Jay Arth
in a matter of days using the proven methods of Lean Six Sigma. Jay is the author of Lean Six
Sigma Demystified and the QI Macros SPC Software for Excel. Jay has worked with healthcare
companies to reduce denied claims by $3 million per year, appealed claim turnaround time and
lab turnaround times by 30-70 percent.
ospital in five days, call: Jay Arthur at 888-468-1537
Email: jay@qimacros.com
To get a faster h
Web: www.qimacros.com
Mail: KnowWare International, Inc. 2696 S. Colorado Blvd., Suite 555 Denver, CO 80222
2010 KnowWare International Inc. 888-468-1537 15
info@qimacros.com
Вам также может понравиться
- Accenture Emerging Market EntryДокумент16 страницAccenture Emerging Market EntryPrateek JainОценок пока нет
- Interest Based Negotiations Presentations Armenda DayeДокумент31 страницаInterest Based Negotiations Presentations Armenda Dayesweta_starОценок пока нет
- Roasted or FriedДокумент16 страницRoasted or Friedsweta_starОценок пока нет
- 2013-01-08 JPMorgan ZerhouniДокумент41 страница2013-01-08 JPMorgan Zerhounisweta_starОценок пока нет
- SPSS TutorialДокумент10 страницSPSS Tutorialsweta_starОценок пока нет
- Campbell Alliance - Recruiting - Why Campbell Alliance PDFДокумент8 страницCampbell Alliance - Recruiting - Why Campbell Alliance PDFsweta_starОценок пока нет
- (CAT) SyllogismsДокумент5 страниц(CAT) SyllogismsNishikanthОценок пока нет
- Autom ImmuneДокумент104 страницыAutom Immunesweta_starОценок пока нет
- Factor AnalysisДокумент3 страницыFactor Analysissweta_starОценок пока нет
- GK MaterialДокумент61 страницаGK Materialsweta_starОценок пока нет
- WikestudyДокумент11 страницWikestudysweta_starОценок пока нет
- Snap 2008 PaperДокумент29 страницSnap 2008 Papersanjay singh100% (4)
- TISS Sample PaperДокумент9 страницTISS Sample Papersweta_star100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- ERAS Protocols For Thyroid andДокумент9 страницERAS Protocols For Thyroid andOskar MartinezОценок пока нет
- Profile of Osteopathic Practice in Spain Results FДокумент11 страницProfile of Osteopathic Practice in Spain Results FBerenice LimarkОценок пока нет
- Age Is Just A Numbers Game PDFДокумент19 страницAge Is Just A Numbers Game PDFparthvarandaniОценок пока нет
- Assoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyДокумент8 страницAssoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyWindyanissa RecitaОценок пока нет
- Prilosec (Omeprazole) MoreДокумент3 страницыPrilosec (Omeprazole) MoreLuis Arturo Andrade CoronadoОценок пока нет
- Group DR - Script - Allergic Rhinitis (Peanut Allergy) Health EducationДокумент10 страницGroup DR - Script - Allergic Rhinitis (Peanut Allergy) Health EducationKyra Bianca R. FamacionОценок пока нет
- Food StampsДокумент80 страницFood StampsAnvitaRamachandranОценок пока нет
- PneumoconiosisДокумент19 страницPneumoconiosisgabriela.was.gabbbieОценок пока нет
- FEDIAF Nutritional Guidelines 2020 20200917Документ96 страницFEDIAF Nutritional Guidelines 2020 20200917luciana ribeiroОценок пока нет
- Hospital Pharmacy Communication - NewsletterДокумент5 страницHospital Pharmacy Communication - Newsletterjuveria nausheenОценок пока нет
- RLE-level-2-packet-week-12-requirement (SANAANI, NUR-FATIMA, M.)Документ26 страницRLE-level-2-packet-week-12-requirement (SANAANI, NUR-FATIMA, M.)Nur SanaaniОценок пока нет
- 2021 IWBF Classification Rules Version 202110 1Документ108 страниц2021 IWBF Classification Rules Version 202110 1Sebastian Alfaro AlarconОценок пока нет
- IMCI Chart BookletДокумент66 страницIMCI Chart Bookletnorwin_033875Оценок пока нет
- Fatima's CommissionДокумент7 страницFatima's CommissionSachie Daniela CheungОценок пока нет
- Fatal Airway Obstruction Due To Ludwig'sДокумент6 страницFatal Airway Obstruction Due To Ludwig'sRegina MugopalОценок пока нет
- Requirements Specification For Patient Level Information and Costing Systems (PLICS) Mandatory Collections Continued ImplementationДокумент40 страницRequirements Specification For Patient Level Information and Costing Systems (PLICS) Mandatory Collections Continued ImplementationAbidi HichemОценок пока нет
- AcupunctureДокумент10 страницAcupunctureAngel Iulian Popescu0% (2)
- PsikosomatikДокумент65 страницPsikosomatikHengki Permana PutraОценок пока нет
- Disability MatrixДокумент21 страницаDisability MatrixAngelika MendozaОценок пока нет
- Prescribing For Transgender Patients ELHEДокумент4 страницыPrescribing For Transgender Patients ELHEGe YgayОценок пока нет
- Antimicrobial ResistenceДокумент23 страницыAntimicrobial Resistencelayal mrowehОценок пока нет
- Improving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutДокумент1 страницаImproving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutUNICEF South SudanОценок пока нет
- Stress Management WorkbookДокумент19 страницStress Management WorkbookKATHYОценок пока нет
- Blood and Tissue Flagellates BSCДокумент27 страницBlood and Tissue Flagellates BSCSisay FentaОценок пока нет
- Bassam Osman ResumeДокумент4 страницыBassam Osman ResumeBassam OsmanОценок пока нет
- Organization and Management at State and District Level (GUJARAT)Документ26 страницOrganization and Management at State and District Level (GUJARAT)Akriti LohiaОценок пока нет
- Test AaДокумент55 страницTest AaKaye PatanindagatОценок пока нет
- Pres 2 PastpapersДокумент190 страницPres 2 PastpapersOdetteОценок пока нет
- StressДокумент4 страницыStressPinky Juntilla RuizОценок пока нет
- Pappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxДокумент5 страницPappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxVinoster ProductionОценок пока нет