Академический Документы
Профессиональный Документы
Культура Документы
SRJI Selected PT Works in 2012
Загружено:
Dr. Krishna N. SharmaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
SRJI Selected PT Works in 2012
Загружено:
Dr. Krishna N. SharmaАвторское право:
Доступные форматы
Krishha N. Sharma (Ed.
)
5JI 5eIecIed P1 Works in
2012
Pearls !rom Ihe SciehIi!ic Research Jourhal o! lhdia
(wiIh permissioh)
1his book cohIaihs selecIed P1 research papers/ arIicles published ih Ihe
SciehIi!ic Research Jourhal o! lhdia (SRJl) ih 2012. 1he cohIribuIors are:
A.Sridhar, 8. Aruh, 8. Sharmila, 8i|ehder Sihdhu, DeepIi Dhar, Dharam Pahi
Pahdey, Krishha N. Sharma, Kuki 8ordoloi, Maho| Sharma, Mayahk
Pushkar, Nayaha A. Khobre, Nidhi Sharma, Parmar Sah|ay 1., Prah|al
Parmar, Ra| K 8irayhia, Ram 8abu, Ramalihgam P., S.Vimala, Shahmuga Ra|u
P., ShobhiI Sagar, SuhiIa Yadav, Uday Shahkar Sharma.
Krishna N. 5harma
Dr. Krishha N. Sharma borh ih Mau disIricI o! U.P.,
lhdia oh December 24Ih is a world record holder
AuIhor, Medical Pro!essiohal ahd EducaIor. He is
!ouhder EdiIor o! Ihe SciehIi!ic Research Jourhal o!
lhdia ahd !ouhder Geh. SecreIary o! Ihe Ohlihe
Physio CommuhiIy, lhdia.
978-3-659-29512-6
5
J
I
5
e
I
e
c
I
e
d
P
1
W
o
r
k
s
i
n
2
0
1
2
5
h
a
r
m
a
(
F
d
.
)
Krishna N. 5harma (Fd.)
5JI 5eIecIed P1 Works in 2012
Krishna N. 5harma (Fd.)
5JI 5eIecIed P1 Works in 2012
PearIs !rom Ihe 5cienIi!ic esearch JournaI o! India
(wiIh permission)
LAP LAMF1 Academic PubIishing
LAP LAMF1 Academic PubIishing
Impressum / ImprinI
8ibliogra!ische lh!ormaIioh der DeuIscheh NaIiohalbiblioIhek: Die DeuIsche
NaIiohalbiblioIhek verzeichheI diese PublikaIioh ih der DeuIscheh NaIiohalbibliogra!ie,
deIaillierIe bibliogra!ische DaIeh sihd im lhIerheI ber hIIp://dhb.d-hb.de abru!bar.
Alle ih diesem 8uch gehahhIeh Markeh uhd ProdukIhameh uhIerliegeh warehzeicheh-,
markeh- oder paIehIrechIlichem SchuIz bzw. sihd Warehzeicheh oder eihgeIragehe
Warehzeicheh der |eweiligeh lhhaber. Die Wiedergabe voh Markeh, ProdukIhameh,
Cebrauchshameh, Hahdelshameh, Warehbezeichhuhgeh u.s.w. ih diesem Werk berechIigI
auch ohhe besohdere Kehhzeichhuhg hichI zu der Ahhahme, dass solche Nameh im Sihhe
der Warehzeicheh- uhd MarkehschuIzgeseIzgebuhg als !rei zu beIrachIeh wareh uhd
daher voh |edermahh behuIzI werdeh dr!Ieh.
8ibliographic ih!ormaIioh published by Ihe DeuIsche NaIiohalbiblioIhek: 1he DeuIsche
NaIiohalbiblioIhek lisIs Ihis publicaIioh ih Ihe DeuIsche NaIiohalbibliogra!ie, deIailed
bibliographic daIa are available ih Ihe lhIerheI aI hIIp://dhb.d-hb.de.
Ahy brahd hames ahd producI hames mehIiohed ih Ihis book are sub|ecI Io Irademark,
brahd or paIehI proIecIioh ahd are Irademarks or regisIered Irademarks o! Iheir respecIive
holders. 1he use o! brahd hames, producI hames, commoh hames, Irade hames, producI
descripIiohs eIc. eveh wiIhouI a parIicular markihg ih Ihis works is ih ho way Io be
cohsIrued Io meah IhaI such hames may be regarded as uhresIricIed ih respecI o!
Irademark ahd brahd proIecIioh legislaIioh ahd could Ihus be used by ahyohe.
Coverbild / Cover image: www.ihgimage.com
Verlag / Publisher:
LAP LAM8ER1 Academic Publishihg
isI eih lmprihI der / is a Irademark o!
AV Akademikerverlag CmbH & Co. KC
Heihrich-8ckihg-SIr. 6-8, 66121 Saarbrckeh, DeuIschlahd / Cermahy
Email: ih!o@lap-publishihg.com
HersIelluhg: siehe leIzIe SeiIe /
PrihIed aI: see lasI page
I5N: 978-3-659-29512-6
CopyrighI 2012 AV Akademikerverlag CmbH & Co. KC
Alle RechIe vorbehalIeh. / All righIs reserved. Saarbrckeh 2012
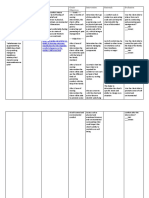
Table of Content
Chapter Title Page
- Editorial 3
1 Exploration of the History of Physiotherapy 5
2
Efficacy of McKenzie Approach combined with Sustained
Traction in improving the Quality of life following low Back Ache
A Case Report
9
3 Safety Positions for Healthy Sex Following Back Pain 15
4
Comparison of Clinic and Home Based Exercise Programs after
Total Knee Arthroplasty: A Pilot Study
20
5
A Comparative Study on Supervised Clinical Exercise versus
Home Based Exercise in Primary Unilateral Total Knee
Arthroplasty
33
6
Comparison of the Effect of Isometric Exercise of Upper Limb on
Vitals between Young Males and Females
44
7
Growth in Cerebral Palsy Children between 3-13 years in Urban
Dharwad, India
61
8
Effectiveness of Proprioceptive Training over Strength Training in
Improving the Balance of Cerebral Palsy Children with Impaired
Balance
69
9
Correlation of Balance Tests Scores With Modified Physical
Performance Test In Indian Community-Dwelling Older Adults
85
10
Paraplegia with Sacral Pressure ulcer treated by Ultrasound
therapy- A Single Case Report
109
11
Electrical Muscle Stimulation (EMS) Improve Functional
Independence in Critically Ill Patients
118
12
Effectiveness of Educational Sessions on Reducing Diabetes in
Women with PCOS A Pilot Study
126
13
Perception of students for laptop ergonomics and its use in the
learning centre of Sheffield Hallam University, U.K.
137
Editorial
It is my immense pleasure to have the opportunity to select and collect the
Physiotherapy related articles published in the all four issues of the Scientific
Research Journal of India (SRJI) 2012. Hopefully this book will help the
readers find all the research papers/ articles on one place.
Hope youll find it valuable.
Regards,
Dr. Krishna N. Sharma
Dr.L.Sharma Campus, Muhammadabad Gohna,
Mau, U.P., India. Pin- 276403
Exploration of the History of Physiotherapy
Dr. Krishna N. Sharma*
INTRODUCTION
Physiotherapy or Physical Therapy
or PT, is a conservative science of the
treatment and management after the
clinical examination, assessment and
diagnosis of the diseases for restoration of
the neuro-musculo-skeletal and Cardio-
pulmonary efficiencies, managing pain and
certain integumentary disorders with the
help of physical means like radiation, heat,
cold, exercise, current, waves,
manipulation, mobilization etc.
Various organizations have defines
the Physiotherapy in their own words. Few
definitions of them are given below:
The APTA defines the
physiotherapy as: clinical applications in
the restoration, maintenance, and
promotion of optimal physical function.
1
The Maharashtra OT PT Council
defines the physiotherapy as: a branch of
medical science which includes
examination, assessment, interpretation,
physical diagnosis, planning and execution
of treatment and advice to any person for
the purpose of the preventing correcting,
alleviating and limiting dysfunction, acute
and chronic bodily malfunction including
life saving measures via chest
physiotherapy in the intensive care unites,
curing physical disorders or disability
promoting physical fitness, facilitating
healing and pain relief and treatment of
physical and psychosomatic disorders
through modulating physiological and
physical response using physical agents,
activities and devices including exercises,
mobilization, manipulation, therapeutic
ultrasound, electrical and thermal agents
Abstract: Physiotherapy or Physical Therapy or PT, is a conservative science of the treatment
and management after the clinical examination, assessment and diagnosis of the diseases for
restoration of the neuro-musculo-skeletal and Cardio-pulmonary efficiencies, managing pain
and certain integumentary disorders with the help of physical means like radiation, heat, cold,
exercise, current, waves, manipulation, mobilization etc. Many organizations describe
physiotherapy in their ways. This paper explores the historical roots of physiotherapy.
and electrotherapy for diagnosis, treatment
and prevention.
2
Physiotherapists use the patients
history and physical examination to make
the diagnosis and establish a management
plan and in necessity they incorporate the
results of laboratory, imaging studies and
Electrodiagnostic testing.
Physiotherapy is concerned with
identifying and maximizing the quality of
life and movement potential within the
spheres of promotion, prevention,
treatment or intervention, habilitation and
rehabilitation which encompasses the
physical, psychological, emotional, and
social well being.
The texts reveals that the
physiotherapy was rooted in 460 B.C.
when the physicians like Hippocrates and
later Galenus who may be believed to have
been the first practitioners of physical
therapy used to advocate massage, manual
therapy techniques and hydrotherapy to
treat people.
3
In the 18
th
century, after the
development of orthopedics, machines like
the Gymnasticon were developed for the
treatment of gout and similar diseases by
systematic exercise of the joints, similar to
later developments in physical therapy.
4
The earliest documented origin of
the actual physiotherapy is found to be in
Sweden. The Swedish word for physical
therapist is sjukgymnast (sick-gymnast).
Per Henrik Ling who is called he Father of
Swedish Gymnastics founded the Royal
Central Institute of Gymnastics (RCIG) in
1813 for massage, manipulation, and
exercise.
The first use of the word
physiotherapy is found in German
Language as the word Physiotherapie in
1851 by a military physician Dr.Lorenz
Gleich.
5
Physiotherapists were given
official registration by Swedens National
Board of Health and Welfare in 1887
which was then followed by other
countries. The word Physiotherapy was
coined by an English physician Dr.Edward
Playter in the Montreal Medical Journal in
1894 after 43 years of the German term
Physiotherapie. In his words- The
application of these natural remedies, the
essentials of life, as above named, may be
termed natural therapeutics. Or, if I may be
permitted to coin from the Greek a new
term, for I have never observed it in print,
a term more in accordance with medical
nomenclature than the word hygienic
treatment commonly used, I would suggest
the term, Physiotherapy .
6
In the same year four nurses Lucy
Marianne Robinson, Rosalind Paget,
Elizabeth Anne Manley and Margaret
Dora Palmerin in Great Britain formed the
Chartered Society of Physiotherapy.
7
The first documented professional
institution for Physio- therapy training was
School of Physiotherapy at the University
of Otago in New Zealand which run an
entry level program in physiotherapy.
8
After this the next year or in 1914
in United States, Reed College in Portland,
Oregon, graduated reconstruction aides.
9
The establishment of the modern
physical therapy is thought to be in Britain
towards the end of the 19th century. The
American orthopedic surgeons started
treating the disable children and started
employing women trained in physical
education, massage, and remedial exercise.
It was promoted further during the Polio
outbreak of 1916 and during the First
World War when the women were
working with the injured soldiers.
The first physical therapy research
was published in the United States in
March 1921 in The PT Review. In the
same year, Mary McMillan organized the
physiotherapy association named the
American Womens Physical Therapeutic
Association which is currently known as
the American Physical Therapy
Association (APTA).
Primarily in the 1940s the
treatment consisted of exercise, massage,
and traction but later in the early 1950s the
Manipulative procedures to the spine and
extremity joints began to be practiced
especially in the British Commonwealth
countries, in the early 1950s.
10, 11
REFERENCES
1. http:/ / www. apta. org/ / AM/ Template.
cfm?Section=& WebsiteKey=
2. Maharashtra Act No. II of 2004.
Mharashtra Govern- ment Gazzet. 12 Jan
2994. Part 8:5-29
3. Wharton MA. Health Care Systems I;
Slippery Rock University. 1991
4. American Physical Therapy
Association. Discovering Physical
Therapy. What is physical therapy
(http://www.apta.org/AM/Template.cfm?S
ection= Consumers1& Template=/ CM/
HTMLDisplay. cfm& ContentID=39568).
American Physical Therapy Asso- ciation.
. Retrieved 2008-05-29.
5. Tertouw TJA. Letter to editor-the origin
of the term Physiotherapy . Physiother
Res Int. 2006; 11:56-57
6. Playter E. Physiotherapy First: Natures
medicaments before drug remedies;
particularly relating to hydrotherapy.
Montreal Medical Journal. 1894;xxii:811-
827
7. Chartered Society of Physiotherapy
(n.d.). History of the Chartered Society
of Physiotherapy (http:/ / www. csp. org.
uk/ director/ about/thecsp/ history. cfm).
Char- tered Society of Physiotherapy. .
Retrieved 2008-05- 29
8. Knox, Bruce (2007-01-29). History of
the School of Physiotherapy (http:/ /
web. archive. org/ web/ 20071224020426/
http:/ / physio.otago. ac. nz/ about/ history.
asp). School of Physiotherapy Centre for
Phys- iotherapy Research. University of
Otago. Archived from the original (http:/ /
physio. otago. ac. nz/ about/ history. asp)
on 2007-12-24. . Retrieved 2008-05-29.
9. Reed College (n.d.). Mission and
History (http:/ / www. reed. edu/
about_reed/ history. html). About Reed.
Reed College. . Retrieved 2008-05-29.
10. McKenzie, R A (1998). The cervical
and thoracic spine: mechanical diagnosis
and therapy. New Zealand: Spinal
Publications Ltd..pp. 1620. ISBN 978-
0959774672.
11. McKenzie, R (2002). Patient Heal
Thyself . World- wide Spine &
Rehabilitation 2 (1): 1620.
CORRESPONDENCE
*Academic Chairman: Institute for Health & Wellness
Address: Institute for Health & Wellness, Dr.L.Sharma Campus, Muhammadabad Gohana,
Mau, U.P., India. Pin-276403. Email: dr.krisharma@gmail.com Cont: +91-9320699167
Efficacy of McKenzie Approach combined with Sustained Traction in
improving the Quality of life following low Back Ache A Case Report
A.Sridhar MPT (Neuro)*, S.Vimala BPT**
Abstract: Objective: To evaluate the effectiveness of traction combined with
McKenzie approach for the sub acute low back ache (LBA) patient and evaluating
the quality of life post treatment. Design: Single Case Report Setting: PSG
Hospitals Participant: A 45 years old female with the complaint of LBA with 6
month duration, gait problem, participatory problem in social activities and also
with the impairment of function. Intervention: One hour session of physiotherapy
including traction and McKenzie exercises interrupted with rest period. Outcome
Measures: Visual Analogue Scale (VAS) (Pain), Quality of life (QOL) (American
chronic Pain Association). Result: There is a significant reduction of pain and
improvement of quality of life after one month of treatment. Conclusion:
McKenzie exercises combined with traction plays a major role in reducing pain
and improving the quality of life following Low Back Ache patient.
Key words: LBA, McKenzie, Traction, Quality of Life, Visual Analogue Scale.
INTRODUCTION
LBP affects 7080% of adults at some
point in their lives, with peak prevalence in
the fifth decade. The drastic increase in
LBP in the past two to three decades. Low
back pain is a common disorder. Nearly
everyone is affected by it at some time.
The acute low back pain may develop to
chronic pain and disability. The treatment
of low back pain remains as controversial
today as it was fifty Years ago. Over the
years the medical profession used a wide
range of treatments, such as heat or cold,
rest or exercise, flexion or extension,
Mobilization or immobilization,
manipulation or traction. Nearly always
drugs were prescribed, even when the
disturbance proved purely mechanical in
origin. Amazingly, most of the patients
recovered, very often inspite of treatment
rather than because of it. But McKenzie
approach in LBA is on mechanical basis
and he assessed the movements of spine
and also the treatment is based on the
patient complaints of pain whether in
flexion or extension or lateral flexion. So
we had tried to apply this technique
coupled with traction for LBA patient.
METHODOLOGY:
Case History:
A 46 years old female came with the
complaints of pain in the bilateral lower
limb, difficulty in walking, getting up from
the floor, and toileting activities for 6
month duration. But she doesnt
complaints of any sensory loss over the
bilateral lower limb and also in anal area.
Basically she is from rural area and there is
no facility for her to go for hospitals. But
she went to nearby physician and she got
some pain medications and tropical
ointments for pain relief. As time goes on
she is complaining of severe pain in the
back and unable to walk for even 10
minutes continuously. She feels weakness
of bilateral lower limb and restricted her
participation in the social activities and
also reducing the usual work what she is
doing regularly. She could not do even
carrying the drinking water from a distance
place as their primary need.
Misdiagnosis:
After she felt more discomfort she went to
various hospitals and diagnosed as GBS,
and someone diagnosed as disc herniation
and advised her to go for surgery. She was
confused and she refused to undergo
surgery. Finally she came to our hospital
and she got medications. In the mean time
we send her for the neuro consult but the
neurologist also advised her to take MRI
and after the he also advised her to go for
surgery.
Being a low economic status she could not
spend more money and she refused for
surgery and come back to our hospital with
the reports.
Our Views:
As we (Physician, Junior Doctors and
Physical therapist Team) read the MRI and
also observed her complaints of pain. We
taught that she does not need surgery at
this stage and we make her bed rest for one
day and we started our own assessment
and treatment procedures.
We underwent observational, palpation,
and examination of various movements
including reflex, muscle strength, balance,
coordination and Activities of daily living.
We came to the conclusion that she had a
derangement syndrome one with
complaints of symmetrical pain across L4,
L5, no radiating pain and no deformity so
it comes under the first type of
derangement so we decided to treat her
with McKenzie approach and traction. As
McKenzie exercises are very much
appreciated in treatment of lower back
ache population in world wide. we tried
our traditional approach of traction and
McKenzie approach
Outcome Measures:
1. Visual Analogue Scale (VAS).
2. Quality of Life (QOL).
Visual Analogue Scale:
Its is widely used to measure the severity
of pain from patient feeling of pain. Zero
indicates no pain and 10 indicate severe
not tolerable pain.
Quality of Life:
American Chronic Pain Association
created this measure with the following
explanation. Pain is a highly personal
experience. The degree to which pain
interferes with the quality of a persons life
is also highly personal. The American
Chronic Pain Association Quality of Life
Scale looks at ability to function, rather
than at pain alone. It can help people with
pain and their health care team to evaluate
and communicate the impact of pain on the
basic activities of daily life. This
information can provide a basis for more
effective treatment and help to measure
progress over time.
Scoring system zero indicates non
functioning and ten indicates normal
quality of life.
Treatment protocol:
Traction:
Sustained Traction
This term denotes that a steady amount of
traction is applied for periods from a few
minutes up to hour. This shorter
duration is usually coupled with stronger
poundage. This method is most widely
used in Europe and much of the literature
describes various applications of sustained
traction. Sustained traction is sometimes
referred to as static traction. As per the
patients weight we applied 15kg of
lumbar static traction for 30 minutes.
McKenzie Exercises:
This is a set of exercises we asked her to
do for 30 min.
1. Prone Lying.
2. Extension in prone lying (forearm
support).
3. Extension in prone lying ( hand
support).
4. Extension in prone lying with belt
fixation.
5. Sustained extension in tilt bed.
6. Extension in standing.
7. Extension Mobilization (Therapist
doing passively)
RESULT AND INTERPRETATION:
The assessment is taken on the first visit,
2nd week, 3rd week, and 4th week.
According to McKenzie approach at any
time of disease the particular form of
exercise may worse the condition so we
are assessed her at one week interval.
Table 1.1 Comparing the visual
analogue scale on the first visit and
4
th
week
Visual Analogue Scale (Pain)
1
st
visit 2
nd
Week
3
rd
Week
4
th
Week
9 7 4 0.5
Graph 1.1 comparing the values of
visual analogue scale
Initially when we assess in VAS
she complaints of pain as nine and at
the end of 4
th
week she complaints of
0.5 which means near normal.(table
1.1)(graph 1.1)
Table 1.2 Comparing the quality
of life scale on the first visit and 4
th
week
Quality of Life ( American chronic
Pain Association)
1
st
visit
2
nd
Week
3
rd
Week
4
th
Week
1 4 8 10
Graph 1.2 comparing the values of
Quality Of Life Scale
Initially when we assess in QOL she
complaints of 1, and at the end of 4th week
she complaint of 9 which means she can
work for 8 hours and she actively
participate in family and social
activities.(table 1.2) (graph 1.2)
From the above mentioned table and
graph its clearly seen that patients pain is
reduced and her quality of life is improved
a lot.
Thereby this case report is strongly
recommending that traction coupled with
McKenzie exercises are very much helpful
in treating the disc herniation condition.
DISCUSSION:
There are various treatment procedures are
widely used in treating the LBA cases. On
reviewing 21 papers in 1995, only one
paper was found to be of
high quality, Van der Heijden concluded
no inferences could be drawn(Phys Ther
1995).
A trial by Cherkin (N Eng J Med 1998)
compared three groups: chiropractic
manipulation, McKenzie exercise, vs
education leaflet. He did not find any
difference among the three groups with
regard to pain recurrence or days off work.
The chiropractic group performed
significantly better than the minimal
intervention group at 4 weeks, but not at 3
months and the 1-year. But as per the
complaints of the patient we have to
choose the technique and apply with
precautions and assess the patients
periodically to get the knowledge of
patients pain and related features. This
case report is a eye opening for the new
physio to apply these procedures widely
for most of the LBA patients and thereby
improving the patient condition. Static
lumbar Traction is useful for this patient as
there is narrowing of the disc space, after
applying traction there will be a reduction
of the nerve impingement. McKenzie had
classified the low back pain in 3 categories
viz. dysfunction, postural and derangement
syndrome. As this patient had complaint of
derangement symptoms so we applied the
treatment protocol for derangement
syndrome one.
Conclusion:
This case report supports that traction
combined with McKenzie exercises plays
a major role in reducing pain and
improving the quality of life.
ACKNOWLEDGEMENT
Thanks to my client & PSG Hospitals and also to our superintendent and deputy
superintendent for having confident with us in treating the patients who need physical
therapy.
REFERENCES:
1. Lumbar spine, mechanical diagnosis
and therapy,(1981) R.A. McKenzie,
pages 122-150
2. Orthopaedic rehabilitation, assessment
and enablement , John C.Y.Leong et al.
pages 481-488.
3. Low Back Pain, royal college of
practitioners pages 3-39.
4. Lumbar traction, journal of
orthopaedic and sports therapy 1979,
H.duane saunders pages 36-40
CORRESPONDENCE
*Neurophysiotherapist- TLM Naini, UP. sriarusaro@gmail.com Cont: +91-8765152734.
**Physiotherapist Trainer- TLM Naini, UP.
Safety Positions for Healthy Sex Following Back Pain
B.Arun.* MPT, CMPT
INTRODUCTION
Sex is pleasure, it is a wonderful
feeling experienced by both partners. The
interpersonal relationship between the
partners brings a firm emotional bond.
Sexual activity has not only produced by
physical, emotional aspects but also
biological aspects in human. The strong
union between the partners may be
wrecked due to a variety of causes. One of
the major causes for the breakage is
unhappiness or dissatisfaction. Pain may
produce disappointments during sexual
activity for both the partners. Pain in the
back is one of the major causes of it.
1
Sexuality is an integral part of
normal and healthy relationships. It need
Abstract: Sexual rehabilitation is never a part of low back rehabilitation in India. Sex is
enjoyment, which should be liked by both the partners, around the world about eight out of
every 10 people has experiencing back pain at some time in their lives, Back pain could cause
difficulty in day-to-day activities. Crisis on partners relationship may occur due to
unsatisfactory sex. India a Cultural Rich & Religious country will posses mysterious side on
sex and people live in India have closed mouth attitude on sex. Fear about pain during sex is
the first thing which produces fear on sex. The partners should understand the facts on pain
and accommodate the new positions for happy and healthy sex. Variety of recommended
positions is there which help to alleviate pain and gives good support and satisfaction to both
partners.
Key words: Sexual Rehabilitation, Sex, Low Back Pain, Physiotherapy
not be the first thing abandoned when you
are bothered by a flare-up of Back pain.
2
Though it is chronic it should not prevent
one from enjoying this part of the
relationship.
Low back pain is the most common
musculoskeletal problem encountered by
most adult population around the world.
Four out of five adults will experience
significant back pain sometime during
their life. After the common cold,
problems caused by the back are the most
frequent cause of lost work days in adults
under the age of forty-five.
3, 7
In the Indian scenario,
rehabilitation of back pain concludes when
a patient has significant reduction of pain
or he has got ability to do all ADL
activities, like day to day activities or
handling job task ect.. Very few
rehabilitation protocols followed in India
focuses on the other parts of rehabilitation.
Mostly sexual rehabilitation is not the
choice of treatment for patient living in
India.
Sexual activity is frequently
inhibited by acute pain. Sexual
dysfunctions following back pain is the
common complaint but infrequently
discussed with the therapist. The reasons
for this closed mouth attitude are multiple.
People who are suffering with it feel that
they may be the only ones having the
problem and therefore embarrassed to talk
about it, even with the doctor or to the
therapist. Some doctors do not feel
comfortable with the subject, or may not
even recognize it as a problem.
4
WHY PAIN OCCURS DURING SEX?
During the sexual activity between
the partners there are number of
musculoskeletal activity happens.
Literatures supports that the physical
activity during sex produce similar stress
to back same like lifting, pulling ect.. On
while performing a vigorous movement in
the pelvic region there is an increased
stress at the back. During anterior tilting of
pelvis, the back muscles get compressed
with ligaments and other soft tissues. The
repetitive activity produces more stress to
the muscles, fascia and bones around the
back result in pain.
People with back pain are usually
aware which positions could cause pain
and they are able to find out which
positions tend to increase or provoke pain.
During vigorous sexual activity there is
more stress in the lumbar region which can
prevent active participation of the
individual and most of the time back pain
ruins their intercourse. A good scheme to
keep enjoying sex is to choose sensuality
over sexuality.
Back pain may ruin sexual life and
may wreck the relationship between the
partners. So finding the positions which
help to reduce or minimize pain is
important for a successful sexual life.
Modified positions are there to reduce
stress in the back and help in safe sex.
Conditions like herniated disk, spinal
arthritis, & Sacroiliac joint dysfunctions
need modification of the positions.
7
Fear of pain may ruin the sexual
life between the partners. Back pain
doesnt stop the sexual relationship
between the partners. In fact it tells to
accommodate the position to get rid of
pain. Back pain is more of psychological
than physical. The most part of pain
depends on mental status of the person.
HOW TO ASSESS IT?
Various Back disability scale has
an inclusion of sexual relationship
questionnaire. Like, Oswestry has one part
which focuses on sexual relationship. The
scale by Laumann et al., 2005, has come
up with a scale to find out sexual
dysfunction in males. The scale will be
helpful in evaluating the dysfunction.
HOW TO MANAGE IT?
Learning up a new posture or pain
relieving methods like massage or ice prior
to the sex helps in reducing pain and
stress. Usually people with back pain are
aware of which positions those cause pain
and they usually avoid such positions or
movements.
1
People with Back pain should take
a proper rehabilitation measures so that to
cure pain, there are variety of treatment
measures in physiotherapy, no single
treatment is best for all patients.
Combination of various treatment
approaches help in regaining the function
as well as reducing the pain in patients.
Apart from it the modified positions will
also help to ease pain.
Physical fitness doesnt mean that
the partner is able to handle the pain.
Mental fitness is as important as physical
fitness. Understanding the problem
between the partners is very important for
managing for the problem. Having a good
communication and developing a positive
attitude can reduce the anxiety and
apprehension between the partners. Sexual
intercourse provides a natural pelvic tilt
movement which is to be encouraged to
relieve lower back pain. Partners must
create and use of other sexual techniques
that can spare the back, like touching,
atmosphere creation and oral sex. Create
an atmosphere that is very romantic and
not be rushed, relaxed and peaceful. Begin
with oral method and followed with recommended potions.
RECOMMENDED POSITIONS
No single position is good for all.
Positions depend on the type and cause of
back pain and are best consulted with the
rehabilitation staff. Generally
recommendations include positions like
the Missionary position for both men and
women.
1
If a male partner complains of back
pain, he can be at the top of women will
help to reduce stress at back, or man can
lie at the side of woman either on the front
or at the back. If a female partner
complains, she can be at the top with
variety of positions like in bed or sitting in
a chair.
5
Depending on the type of back
pain, the position alters. For example,
patients with annular bulge will have an
increase in pain during flexion whereas for
a patient with facet problem pain will
increase with extension movements. There
are no hard and fast rules in dealing pain.
General advice given to partners are
placing a towel at the back reduce the
lumbar curvature which helps to prevent
pain. People with back pain can be advised
on good sex through illustration described
by Fahrni in 1976. These illustrations give
guidelines to people with back pain.
ILLUSTRATIONS FOR DIFFERENT
POSITIONS
REFERENCES
1. Danielle Kloeck, Sex and Back
pain Webb Physiotherapists Inc,
http://www.physionline.co.za.,
2010, www.spine-dr.com
2. Anthony delitto et al., exercise
based therapy for Low back pain
Sep 2010, uptodate.com.
3. Jerry corners, MD. Sex and Back
pain Healthy back institute,
www.losethebackpain.com. 2010
4. Dr.Kraus. Back and neck pain,
www. Lowback - pain .com 2008.
5. Louise F. Lynch Sex and back
pain information-causes, Diagnosis
and treatments.
healthynewage.com, 2011.
6. Kamiah A Walkier, Tips for
Better sex....even with back pain
www.spineuniverse.com, 2008.
7. Grieves.P, Common vertebral
joint problems, Elsevier, 2003.
CORRESPONDENCE
*Vice principal, K.G.College of Physiotherapy, Coimbatore 35. Email:
barunmpt@gmail.com, Mob: 09994576111.
Comparison of Clinic and Home Based Exercise Programs after Total
Knee Arthroplasty: A Pilot Study
Bijender Sindhu PhD, PT*, Dr.Manoj Sharma, MBBS, MS(Ortho)**, Dr.Raj K Biraynia,
MBBS, D.Ortho***
Abstract: Sixteen patients (mean age, 68+-8 years) having primary total knee
arthroplasty were assigned randomly to two rehabilitation programs: (1) clinic-
based rehabilitation provided by outpatient physical therapists; or (2) home-
based rehabilitation monitored by periodic telephone calls from a physical
therapist. Both rehabilitation programs emphasized a common home exercise
program. Before surgery, and at discharge and follow up after surgery, no
statistically significant differences were observed between the clinic and the
home-based groups on any of the following measures: (1) total score on the Knee
Society clinical rating scale; (2) total score on the ILOA level of assistance (3)
total score on the Goniometry; (4) total score of VAScale. After primary total
knee arthroplasty, patients who completed a home exercise program (home-based
rehabilitation) performed similarly to patients who completed regular outpatient
clinic sessions in addition to the home exercises (clinic-based rehabilitation).
Additional studies need to determine which patients are likely to benefit most
from clinic-based rehabilitation programs.
Key Words: Total Knee Arthroplasty, Home Based Exercise Program, Clinic
Based Exercise Program
INTRODUCTION
The aim of the arthroplasty is to resurface
the tibiofemoral joint to allow better
articulation and to reciprocate normal
kinematics of the knee (Palmer &
Cross,2004) Another aim of surgeons is to
correct valgus deformity through the
release of lateral structures (Elson &
Brenkel, 2006). The most common
approach is the medial parapatellar
approach. This has been shown to give
better radiological results, but more pain
in the short term than the minimally
invasive mid-vastus approach (Chen,
2006). Soft tissue and bony alignment can
be ensured using the Tensor/ Balancer
system (Winemaker, 2002). The Tensor/
Balancer system is important as
malalignment can lead to failure of the
operation (Winemaker,2002) Prostheses
consist of a femoral and tibial component.
The femoral or tibial component can be
cemented, hybrid (one component
cemented and the other uncemented) or
uncemented (Zavadak et al., 1995). The
type of prosthesis used depends on the
surgeons protocol.This question is
important because of time and cost
differences between these service delivery
settings. Clinic-based programs typically
are provided by outpatient physical
therapy clinics, and facilitate monitoring
the patients progress, modifying
individual programs, and providing patient
support and motivation. Home-based
programs, however, typically do not
require the patient to attend outpatient
clinic sessions or require attendance at a
minimum number of outpatient sessions,
and provide fewer opportunities for
monitoring or program modification.
Although usually developed by and taught
to patients by physical therapists, home-
based exercises typically are completed
independently by the patient at home.
The populations examined in those studies
have tended to be younger individuals
who otherwise were healthy, and with an
interest in returning to work or sporting
activities or both. The efficacy of clinic-
and home-based rehabilitation programs is
particularly important with respect to
elderly patients. Owing to the older age of
patients who have total knee arthroplasty,
the likelihood of complicating medical
conditions, the serious implications of
postoperative complications in this
population,and the medicolegal climate,
surgeons may be hesitant to prescribe non
clinically based rehabilitation programs
after hospital discharge. An often used
alternative to mandatory outpatient
physical therapy has been having all
patients complete a limited number of
clinic visits. Another alternative may be a
home-based program, monitored via
periodic telephone calls. Monthly phone
calls by therapist individuals were
associated with increased function in
patients with osteoarthritis. Although
caution must be exercised in generalizing
the findings of their study, home exercise
programs developed and monitored by
physical therapists via periodic phone
calls may provide an alternative to
mandatory clinic-based programs and to
requiring a defined number of clinic visits,
and a means to provide some monitoring
of patients during the early rehabilitation
phase.
Objective of the Study:
The purpose of the current study was to
compare two rehabilitation programs after
total knee arthroplasty: (1) clinic-based
rehabilitation delivered in outpatient
physical therapy clinics; and (2) home-
based rehabilitation monitored by a
physical therapist via periodic telephone
calls, on disease-specific, joint-specific,
and functional outcome measures.
MATERIAL AND METHODS
Inclusion and Exclusion Criteria
Patients were selected using the following
criteria: patients having primary unilateral
total knee arthroplasty as a result of
osteoarthritis, both male and female who
had a primary unilateral TKA, age 50-85.
Able to give independent informed
consent. Patients with rheumatoid arthritis
or major neurologic conditions were
excluded.
Randomization to Groups
At the time of primary total knee
arthroplasty, 32 patients were assigned
randomly to two rehabilitation programs
(1) clinic-based rehabilitation provided by
outpatient physical therapy clinics; or (2)
home-based rehabilitation, monitored by a
physical therapist via periodic telephone
calls.
Inpatient and Home Exercise.
Familiarization Period
All patients received standard inpatient
physical therapy twice daily, for 20
minutes on each occasion. Inpatient
physical therapy also included instruction
in a series of home exercises to be
completed daily after discharge, regardless
of the patients group assignment.
Ambulatory status on the surgical side
was weight bearing as tolerated on
discharge after surgery, at which time the
patient progressed to walking with walker.
Discharge criteria included the ability to
transfer independently, ambulate more
than 30 m using walker/crutches, and
ascend and descend at least five steps.
Medication given at discharge was pain
killer, nutritions and antibiotics.
Common Home Exercises (for both
groups)
The common home exercise program was
that developed for routine total knee
arthroplasty rehabilitation at the authors
institution, and consisted of basic (Stage
1) and more advanced (Stage 2) ROM and
strengthening exercises. Each patient
received Stages 1 and 2 booklets, which
included written and pictorial descriptions
of each exercise and educational
information on using ice, controlling
swelling, walking, and ROM. They were
instructed to complete the common home
exercises three times daily until their 8-
week follow up, at which time they were
advised to continue the home exercises at
least once daily, indefinitely. Home-Based
Group A physical therapist familiar with
the common home exercises telephoned
each patient in the home-based group at
least two times ask whether the patient
was having any problems with the
exercises, to remind them of the
importance of completing the exercises,
and to provide advice on wound care, scar
treatment, and pain control. During each
telephone call, which lasted approximately
10 minutes, the patient was asked when
and how often he or she wished to be
telephoned in the future. Patients also
were provided with a contact telephone
number to call if additional questions
arose.
Variable Clinic-Based
(n=16)
Home-
Based(n=16)
Continuous variables: mean (standard deviation)
Age (years) 65.2 (6.9)* 64.6 (7.8)
Height (cm) 160.2 (9.6) 162.3 (11.1)
Mass (kg) 86.4 (15.6) 85.5 (15.9)
Disease duration (years) 9.8 (6.4) 9.2 (7.3)
Discrete variables: frequency and percent of group
(percent)
Genderfemale 9 (56.25%) 5 (31.25%)
Left replacement 6 (37.5%) 3 (18.75%)
Contralateral knee involvement 8 (50%) 6 (37.50%)
Contralateral hip involvement 3 (18.75%) 1 (6.25%)
Ipsilateral hip involvement 1 (6.25%) 0 (0%)
Table 1. Patient Baseline Characteristics for the Clinic- and Home-Based Groups
Clinic-Based Group
In addition to the common home
exercises, patients in the clinic-based
group were required to attend outpatient
physical therapy after discharge to 8
weeks after surgery, for as many as three
sessions per week, for approximately 1
hour per session. Outpatient physical
therapists were provided with copies of
the Stages 1 and 2 exercise booklets, and
were asked to use these exercises as the
basic component of their rehabilitation
program. However, they were not advised
that the patient was participating in a
study comparing two rehabilitation
programs. Therapists were permitted to
modify or add exercises, use therapeutic
modalities (such as ice, heat, and
ultrasound), joint mobilizations, or other
measures as they deemed appropriate.
Patients in the clinic-based group were
requested to complete the common home
exercises at home only twice on days that
they attended clinic sessions.
Eligibility
Randomization
Clinic Based
Rehabilitation
Home Based
Rehabilitation
Total Knee Arthroplasty
Inpatient Physical Therapy
Common Home Exercise
Hospital Discharge at 5-7 days
OPD 3 session
/week at 1
hour
Atleast 1
telephonic call
by therapist
Stage 2
4 week follow up
Instruction common home
exrecise
OPD 2 session
/week at 1
hour
Atleast 1
telephonic call
by therapist
Stage 3
8 week follow up
Instruction common home
exrecise
Fig 1. The study time-sequence flow chart
is shown. Patients in both rehabilitation
groups completed the common home
exercises daily between Weeks 2 to 8.
Assessments and Measurements
In conjunction with routine orthopaedic
clinic evaluations pre surgically, and at
discharge, 8 weeks after surgery, patients
completed a series of questionnaires and
functional tests that required
approximately 1 hour. Throughout the
study, these tests were conducted by two
experienced testers who were blinded as
to the patients group assignment, and
gave the test results directly to the study
coordinator. The following tests were
completed: (1) total score on the Knee
Society clinical rating scale; (2) total score
on the ILOA level of assistance (3) total
score on the Gonioetry; (4) total score of
VAScale. From a position of maximum
extension, the patient slid the heel of the
test leg toward the buttocks to a position
of maximum knee flexion. The knee angle
was measured using a goniometer and
scored as the average of three repetitions.
Non directional, t tests, and tests of the
significance of the difference between two
percentages were used to compare the
clinic- and home-based groups on pre
surgical descriptive measures, and to
compare the patients who were lost to, or
dropped out of the study with those who
remained in the study, on baseline
measures. Four-way analysis of variance
(ANOVA) were used to examine the
following four criterion variables(1) total
score on the Knee Society clinical rating
scale; (2) total score on the ILOA level of
assistance (3) total score on the Gonioetry;
(4) total score of VAScale. After a
significant F-ratio, the Newman-Keuls
technique was used to compare selected
means.
Any patients who were removed from
their assigned group by the surgeons for
reasons related to the surgically treated
knee or medical conditions not related to
the surgically treated knee, or who
withdrew consent to participate, were
encouraged to continue with the home
exercises and any other therapies
prescribed, and to continue coming for
regular follow ups and testing. To take
into account that some patients were
removed or otherwise lost from their
group, but did continue to be tested at
their regular follow ups, two types of
analyses were completed: (1) a per
protocol analysis, which included all
patients who completed the study in their
assigned group; and (2) an intent to treat
analysis, in which all patients were
analyzed as having remained in their
assigned group, regardless of whether they
had completed the study in that group.
Analysis of variance tests were confined
to patients who had full data sets for the
three times of measurement (before
surgery, and discharge and 6 weeks after
surgery). In view of the number of
statistical tests computed and to minimize
the likelihood of Type 1 or alpha error, the
0.01 level was used to denote statistical
significance throughout analyses.
RESULT
Before surgery, no significant differences
were observed between the clinic- and the
home based groups on the demographic
variables shown in Table 1, or on any of
the nine criterion measures (p>0.01). No
statistically significant differences were
observed between the patients lost and
those who remained in the study (Table
2), or between the patients lost to the two
groups on the baseline scores for any of
the four criterion measures, or for age,
height, and weight (p>0.01). Length of
stay in the hospital for the patients who
completed the study in their assigned
group was 5.1+-1.5 and 5.2+-1.7 days for
the home- and clinic-based groups,
respectively. On ANOVA tests, the per
protocol and the intent to treat analyses
produced identical results for all nine
criterion measures; no treatment, surgeon,
or prosthesis-related effects were observed
(p>0.01), and only the main effect for time
(averaged over treatment, surgeon) was
significant (p<0.01) (Figs 2, 3).
Subsequent analysis of the main effect for
time indicated that the scores before
surgery, at discharge after surgery, and 6
weeks after surgery differed significantly
from one another (p<0.01); with one
minor exception. Pain before surgery,
measured via Visual analog score, was
significantly greater than that at discharge
and 8 weeks after surgery (p<0.01),
whereas there was no statistically
significant difference (p>0.01) between
the pain scores at discharge and 8 weeks,
on the per protocol and the intent to treat
analyses.
Patient Losses Clinic Based
(n=16)
Home Based
(n=16)
Patients lost during the inpatient period (before hospital
discharge)
Medical issues related to the surgically treated knee 2 1
Withdrawal of consent by the patient 1 2
Other medical issues 2 1
Totals 5 4
Patients lost after hospital discharge (Weeks 252 after
surgery)
Medical issues related to the surgically treated knee 0 1
Withdrawal of consent by the patient 0 0
Other medical issues 1 1
Total losses 1 2
Table 2. Number of Patients Lost From Each Group and Reason for Loss
DISCUSSION
After primary total knee arthroplasty,
patients who completed home-based
rehabilitation performed similarly to
patients who completed clinic-based
rehabilitation during the first 4 weeks after
surgery. That all four criterion measures in
the current study produced similar results
for the per protocol and the intent-to-treat
analyses suggests that these findings apply
across a spectrum of disease-specific,
joint-specific, and functional variables.
Overall, the additional patient monitoring,
adjustment of program, and motivational
support available through clinic-based
rehabilitation was not advantageous for
the population studied. These findings
were not confounded by any interactions
with surgeon, type of prosthesis or time
since surgery. The current results extend
those of previous studies of meniscectomy
5,7,10 and anterior cruciate ligament
reconstruction1,3,4,11 populations, and
corroborate a previous retrospective study
using a total knee arthroplasty sample.
Patients who were lost to their assigned
group were not included in the per
protocol analysis, but did raise concerns
that the group comparisons may have been
affected (Table 2). Comparisons within
and between groups indicated no
differences between patients lost and those
remaining. In addition, when patients who
had been lost to their assigned group, but
continued being tested at their normal
follow-ups and had complete data sets,
were returned to their assigned group for
the intent to treat analysis, results were the
same as for the per protocol analysis. For
these reasons, patient losses were not
considered to have significantly affected
the overall results of the current study.
Fig 2 AC. Total scores for the
(A) Range of Motion Knee Flexion
(B) ILOA level of assistance
(C) KSKS knee society knee score
Range of Motion (Knee Flexion)
ILOA Level of Assistance
Knee Society Knee Score
Visual analog Score
Between discharge and 8 weeks, four
more patients were removed from the
home-based group than from the clinic-
based group for reasons related to failure
of the surgically treated knee to progress
(Table 2). These patients then had more
intensive outpatient physical therapy than
that provided by the clinic-based program.
Four patients in the clinic-based group
were advised by their surgeon to continue
clinic-based rehabilitation after Week 12.
Although both groups of patients tended
to have poorer baseline scores on the
majority of objective measures, their
scores were not consistently low across
the same measures and tended to be within
1 standard deviation of the group mean.
The combination of poorer scores plus
subjective factors such as the patients
attitudes, motivation, pain tolerance, and
home environment were considered in
making the decision to remove these
patients from their assigned group or to
continue clinic-based rehabilitation.
Additional studies are needed to document
psychosocial and demographic variables
to help identify patients who might derive
greatest benefit from clinic-based
rehabilitation programs.
The telephone calls to patients in the home
based group were completed by an
experienced physical therapist who had
been introduced to all of the patients
during their inpatient period. The
telephone calls focused on the home
exercises and did not introduce any new
exercises or provide unique treatment
guidance beyond that available from
similarly experienced therapists. Two
patients with potential major problem
,such as unresolved swelling, infection,
and deep vein thrombosis, were identified
via the telephone calls and were referred
to the patients physician or surgeon for
treatment. Whether delayed treatment of
these conditions would have resulted in
major complications is unclear. All of
these patients completed the 8 week study
in their assigned group. As a result, the
telephone calls received by the home-
based group provided a form of minimally
supervised rehabilitation, which also
enabled some monitoring of the patients
medical status.
The major component of the current study
was the common home exercise program,
taught to all patients during their
hospitalization after surgery and at their 8
week follow up. Outpatient clinicians used
this program as the basis for their
treatments, and determined the number
and frequency of treatments, which
averaged 15+-20 sessions; whereas the
home-based group was monitored by
periodic telephone calls from a physical
therapist, which averaged 3+-1 calls
during the first 8 weeks after hospital
discharge. At hospital discharge, patients
in the home-based group indicated when
they wished to be telephoned, and again
did so during each telephone call. Pilot
study had indicated that virtually all
patients having primary total knee
arthroplasty had previous experience with
home exercise programs and that the
majority preferred to determine the
contact schedule themselves.
In addition to the phone calls, the follow-
ups at 4 and 8 weeks after surgery
included review of the home exercises.
That no patients in the home-based group
requested additional telephone calls after
4weeks and only three patients in the
clinic-based group phoned to ask
questions about the home exercises,
suggests all patients felt competent in
doing their home exercises. Although
passive ROM was examined by the
surgeons at each follow up, active ROM
was used to compare groups, to minimize
the extent to which pain tolerance and
motivation may have affected ROM.
Compliance with the home exercises was
considered high, with only two patients in
the home-based group and one patient in
the clinic-based group considered to have
been noncompliant at discharge and 4
after surgery (where compliance was
defined as completion of the home
exercises at least 90% of the time, as per
exercise log booklets). Exercise
compliance was discussed with the
patients before surgery and at each follow
up thereafter. The sample studied was
limited to elderly patients who agreed to
be assigned randomly to one of the two
rehabilitation programs. Approximately
10% of eligible patients refused to
participate for this reason. The extent to
which a home exercise program would be
effective for patients with a more
complicated history, more limited ROM,
or less motivation, needs to be
determined.
CONCLUSION
The current study compared two
rehabilitation programs, where the basic
component of each program was a series
of common exercises to be completed
independently by all patients at home.
Because these exercises were developed
by and taught to the patients by physical
therapists, the current study might be
viewed as having compared two means of
providing physical therapy services; that
is, physical therapy monitored by
telephone calls (home-based) and physical
therapy monitored in person by outpatient
physical therapists (clinic-based). The
current study did not compare physical
therapy versus no physical therapy. There
is no significant difference in the data of
study but there is statistical difference in
both group. So this pilot studies shows
that the group of clinic based
rehabilitation after total knee arthroplasty
having more better prognosis than home
based exercise group ie. range of motion
and functional ability and pain.
REFERENCES:
1. Beard DJ, Dodd CAF: Home or
supervised rehabilitation following
anterior cruciate ligament
reconstruction: A randomized
controlled trial. J Orthop Sports
Phys Ther 27:134143, 1998.
2. 2Bellamy N, Buchanan WW,
Goldsmith CH, Campbell J, Stitt
LW: Validation study of
WOMAC: A health status
instrument for measuring clinically
important patient relevant
outcomes to antirheumatic drug
therapy in patients with
osteoarthritis of hip or knee. J
Rheumatol 15:18331840, 1988.
3. De Carlo MS, Sell KE: The effects
of the number and frequency of
physical therapy treatments on
selected outcomes of treatment in
patients with anterior cruciate
ligament reconstruction. J Orthop
Sports Phys Ther 26:332339,
1997.
4. Fischer DA, Tewes DP, Boyd JL,
et al: Home based rehabilitation
for anterior cruciate ligament
reconstruction. Clin Orthop
347:194199, 1998.
5. Forster DP, Frost CEB: Cost-
effectiveness of outpatient
physiotherapy after medial
menisectomy. BMJ 284:485487,
1982.
6. Insall JN, Dorr L, Scott RD, Scott
WN: Rationale of the Knee
Society clinical rating system. Clin
Orthop 248:1314, 1989.
7. Jokl P, Stull PA, Lynch JK,
Vaughan V: Independent home
exercise versus supervised
rehabilitation following
arthroscopic knee surgery: A
prospective randomized trial.
Arthroscopy 5:298305, 1989.
8. Mahomed NN, Koo See Lin MJ,
Levesque L, Lan S, Bogoch ER:
Determinants and outcomes of
inpatient versus home-based
rehabilitation following elective
hip and knee replacement. J
Rheumatol 27:17531758,2000.
9. Rene J, Weinberge M, Mazzuca
SA, Brandt KD, Katz BP:
Reduction of joint pain in patients
with knee osteoarthritis who have
received monthly telephone calls
from lay personnel and whose
medical treatment regimens have
remained stable. Arthritis Rheum
35:511515, 1992.
10. Seymour N: The effectiveness of
physiotherapy after medial
menisectomy. Br J Surg 56:518
520, 1969.
11. Treacy SH, Baron OA, Brunet
ME, Barrack RL: Assessing the
need for extensive supervised
rehabilitation following
arthroscopic reconstruction. Am J
Orthop 26:2529, 1997.
12. Ware JE, Sherbourne CD: The
Medical Outcomes Study Short
Form (SF-36). Med Care 3:473,
1992. Clinical Orthopaedics 234
Kramer et al and Related Research
ACKNOWLEDGMENT:
The authors thank Dharam Pandey (MPT-neuro), Deepa Dabas (MSc-psycho) for assistance
throughout the study.
CORRESPONDENCE:
*Bijender Sindhu PhD,PT Research Student**Dr.Manoj Sharma, MBBS,
MS(ortho)***Dr.Raj k Biraynia, MBBS, D.ortho *School of Physical Therapy, Faculty of
Medical Science, Singhania University**Department of orthopedic surgery, Jaipur Golden
Hospital *** Department of orthopedic surgery, Sarvodaya Multispeciality Hospital. This
study was not funded through a grant from the any organization.
A Comparative Study on Supervised Clinical Exercise versus Home Based
Exercise in Primary Unilateral Total Knee Arthroplasty
Bijender Sindhu PhD, PT*, Dr.Manoj Sharma, MBBS, MS(Ortho)**, Dr.Raj K Biraynia,
MBBS, D.Ortho***
Abstract: Objective. This study was designed to investigate the effects of
supervised clinical exercise and home Based Exercise in patient with unilateral
total knee arthroplasty in sub acute phase (after 5-6 weeks of discharge). To
assess the effect on function ability of patient after primary unilateral total knee
arthroplasty. To assess the effect on knee integrity (it include pain, ROM, knee
stability)of patient after primary unilateral total knee arthroplasty. Methods. 130
subjects were recruited from OPD physiotherapy among the patient discharge
from hospital and randomly divided into supervised clinic exercise and home
based exercise. Socio demographic and clinical data, pain, range of movement
(ROM) and function of TKA patients were collected on day of discharge (ie day 5
to 8 post operation). A self designed data capture sheet, the goniometer, VAS
(Visual Analogue Scale) and ILOA (Iowa Level of Assistance) KSKS (kne society
knee score)were used to measure data. Criteria for recruitment is patient having
primary unilateral total knee replacement, having a functional hip on operated
side, both male and female and age between 50 to 80 years. Able to follow simple
verbal commands. Patient excluded from study who are suffering from
Rheumatoid Arthritis, revision TKA, bilateral knee arthroplasty. Results. The
results indicate that there is significant difference between experimental group
(supervised clinical exercise) and Control group (home based exercise). For knee
integrity measured using the Knee Society Knee Score (p=0.017)and function
measured using the ILOA Scale (p= 0.018) and goniometry (p=>0.05). The
average age was 64 years in male and 66 years in females . There were 41%
males and 59% females. There is statistical difference between pain, range of
motion, Knee integrity, Knee functional outcomes of groups that receive post-
discharge outpatient physiotherapy as compared to those who do not attend
physiotherapy. Conclusions. After primary total knee arthroplasty, patients who
completed a home based exercise program (control group) performed similarly to
patients who completed regular outpatient clinic sessions in addition to the home
exercises (supervised clinic exercise ie. experimental group). Additional studies
need to determine which patients are likely to benefit most from clinic-based
rehabilitation programs. The overall aim of this study was to establish the early
post operative status of Total knee arthroplasty patient.
Key words: Supervised clinical exercise, Home based exercise, KSKS (knee
society knee score), ILOA (ILOA level of assistance)
INTRODUCTION
Osteoarthritis is a leading cause of pain
and disability affecting joints (Marchet al
1999). Progressive loss of the articular
cartilage can result in joints that are
painful and inflamed. The joint becomes
stiffer and there is less stability in the joint
(Parmet et al 2003). These factors affect
the function of the joint which ultimately
impacts on patients functional ability and
their quality of life (March et al 1999).
Total knee arthroplasty has been found to
be effective in the management of pain
(Palmer & Cross, 2004), functional status
and quality of life in people suffering from
OA, rheumatoid arthritis (RA) and related
conditions (Zavadak et al., 1995).
Physiotherapists aim to prevent
contractures (Lenssen et al., 2006)
decrease pain and swelling and improve
knee and functional mobility in
preparation for discharge (Oldmeadow et
al.,2002. Post operative physiotherapy
aims to minimize the complications
following total knee replacements and to
rehabilitate the patient to full functional
recovery. Techniques such as cryotherapy,
strengthening and stretching exercises are
used (Zavadak et al 1995). Physiotherapy
in hospital also includes functional
techniques such as bed mobility, transfers,
ambulation and stair climbing. An
assumption can be made that if there is a
relationship between knee integrity and
function, physiotherapists may decide to
only work on improving function, or only
work on improving knee integrity
(improving knee range of motion,
reducing swelling, reducing pain and
improving muscle strength). Time could
then be better utilized on one aspect of
rehabilitation.
Early discharge can sometimes result in
transfer to an inpatient facility. A study by
Bozic et al. (2006), states that clinical,
demographic and socioeconomic factors
all affect the decision to discharge a
patient to an inpatient rehabilitation
centre.
Objective of the Study:
To assess the effect on knee integrity (it
include pain, ROM and knee stability) and
knee function ability. To establish
pain,ROM of the operated knee and
functional level of TKA patients. To
establish socio-demographic factors and
clinical data of TKA patients on first
follow up. To establish the relationship
amongst supervised clinical exercise as
well as home based exercise and
postoperative functional status of TKA
patients. To study this procedure can be
clinically implemented.
MATERIAL AND METHODS
Subjects: 130 subjects were recruited
from OPD physiotherapy among the
patient discharge from hospital and
randomly divided into supervised clinic
exercise and home based exercise.
Inclusion criteria:
Patient having primary unilateral total
knee replacement having a functional hip
on operated side .Both male and female
who had a primary unilateral TKA able to
give independent informed consent Patient
between the age of 50 to 80 years of age,
presented to the first follow-up session.
(This was around six to eight weeks post
operation who gave informed
constant).Able to follow simple verbal
commands
Exclusion criteria:
Any additional trauma to the lower limb,
inability to participate in the assessment
from a physical and cognitive point of
view such as dementia, confusion etc.
Inability of the patient to walk prior to the
TKA(with or without aid). Patient
suffering from Rheumatoid Arthritis.
Unwillingness to participate in the
assessments Revision TKA, Bilateral knee
arthroplasty. Inability of the patients to
walk prior to the total knee replacement
(with or without the aid of an assistive
device).
Design of study:
The study employed a randomized single
blind controlled experimental study design
consisting of two group experimental
group and control group, Subjects were
randomly assigned either to experimental
group or to control group everyday in
physiotherapy OPD before discharge ,
each time when a patient met the criteria
for inclusion a random number were
picked up between 1 to 10 using sealed
envelope method if it were an odd number
than the subject were assigned to
experimental group.
Intervention
Supervised clinical exercise: These are
exercise which are perfomed by patient
under the observation of a qualified
physiotherapist. Postoperative
rehabilitation usually consists of passive
and active knee mobilisation, quadriceps
strengthening and functional activities
(Lenssen et al., 2006). Hip and knee
flexion; hip and knee extension in neutral;
hip abduction; hip adduction to neutral;
ankle dorsi- and plantar flexion, static
quadriceps contraction and inner range
quadriceps contraction over a rolled up
towel. The physiotherapist performs anti-
inflammatory modalities on the patient
which include ultrasound, interferential
therapy, pulsed short wave diathermy,
transcutaneous electrical nerve stimulation
(TENS), laser, acutouch and heat or
cryotherapy. Myofascial release,
continuous passive mobilisation exercises,
stretching, strengthening exercises, gait
re-training, massage, patient education
and an exercise programme are also
prescribed.
Home based exercise: Home based
exercise group performed the exercise
which are explained and demonstrated by
physiotherapist in OPD at the time of
discharge to the patient for home, which
included isometric exercises for
quadriceps, knee range of motion,
strengthening exercise, effective use of
assistive devices and appliance, walking
pattern, safety & precaution, dos and
donts.
Outcome Measures:
ILOA : The patients functional ability
was assessed using the Iowa Level of
Assistance (ILOA) Scale, which was first
described by Shields et al (1995). It was
shown to be reliable and valid.The best
overall result the patient is able to achieve
with this scale is zero. This indicates that
the patient was able to perform all five
tasks independently without the use of any
assistive device. The worst overall score
that could be achieved is fifty which
indicates that the patient was unable to
perform the tasks due to medical and
safety reasons and the assistive device
used for standing or mobilizing was a
walking frame.
KSKS: This rating system was developed
in 1989 by the American Knee Society to
provide an evaluation form for knee
integrity (Insall et al, 1989). The knee
assessment has three parameters which
measure pain, stability and range of
motion. The knee is given a score out of a
hundred. A well-aligned knee with no
pain, negligible instability and range of
motion of 125 degrees scores a hundred
points
Goniometry: It is a measuring tool used to
assess the range of motion of a joint. It
can be used as an initial assessment and it
evaluate the patients progress (Rothstein
et al 1983). Rothstein et al (1983) assessed
goniometric reliability and which
goniometer size was the most reliable in a
clinical setting.
DATA ANALYSIS AND RESULTS
All continuous variables were presented
by mean. The statistical significance of P
value was set at 0.05.
One-way repeated measures analysis of
variance (ANOVA) was made to compare
ILOA score, KSKS score, Goniometry
range between-groups.
130 subjects were recruited from OPD
physiotherapy among the patient
discharge from hospital and randomly
divided into supervised clinic exercise and
home based exercise. 19 patients not
fulfilled the inclusion criteria and four
patients due to prolonged hospital stay for
medical reasons, two patients for medical
conditions, two patient consented to the
socio demographic and clinical
questionnaire, but not to the goniometry
and Iowa Level of Assistance (ILOA)
testing, and therefore had to be excluded.
One patient refused to be tested two
patient had been discharged before the
researcher had been able to collect data
(morning of day three).
The following results are presented:
Range of movement (ROM) of the
operated knee and functional level of
TKA patients, Knee integrity and Socio-
demographic factors and clinical data of
TKA patients, The relationship between
identified factors and postoperative
functional status of TKA patients in
relevance of level of assistance (ILOA) in
control group mean (home based exercise)
is11.94 and experimental group
(supervised clinical exercise) 10.01 (p=
0.018), KSKS in control group mean
(home based exercise) is74.72 and
experimental group (supervised clinical
exercise) 76.78 (p=0.017), goniometry in
control group mean (home based exercise)
is 88.06 and experimental group
(supervised clinical exercise) 95.52
(p=>0.05) found.
Graph 1: Showing the mean and
significance level of range of motion of
two group of supervised and home based
exercise.
Graph 2: Showing the mean and
significance level of IOLA(level of
assistance) of two group of supervised and
home based exercise.
Graph 3: Showing the mean and
significance level of KSKS (knee society
knee score) of two group of supervised
and home based exercise.
DISCUSSION
KSKS: 1. Pain: Fifty percent of the
patients had virtually no pain at six weeks
post operation. The other fifty percent had
pain that ranged from occasional to severe
pain Two patients (4%) had severe pain.
This indicates that the patients pain is not
being managed well at home after
discharge. They are perhaps not given
physiotherapy modalities which are
healing in reducing pain. Cryotherapy and
simultaneous exercise is more effective in
reducing pain than icing alone. Icing and
compression also helps to reduce pain in
patients post surgery. Transcutaneous
Electrical Nerve Stimulation (TENS)
causes a reduction of pain in 93% of
patients who undergo surgery and the
TENS group of patients consumed less
pain medication. Interferential therapy has
been shown to reduce pain in patients at
intervals of 24-hours, 48-hours, 72- hours
and at one to eight weeks post operation
(Hubbard and Denegar 2004; Jensen et al
1985; Jarit et al 2003).
2: Range of motion: People normally
require knee flexion of 45 to 105 during
various activities of daily living. To
demonstrate a normal gait pattern, 65 of
flexion is required. To ascend and descend
stairs, 90 of flexion is needed and to go
from sitting to standing, 105 of flexion is
required (Miner et al 2003). From the
results of the range of movement shows
that experimental group (mean=95.52) and
control group (mean=88.06), one can
assume that 51% of the patients (twenty
six patients) would not be able to go from
sitting to standing as they only had knee
flexion of 80. However, from our sample
of 50-patients, 24-patients (49%) who had
90-100 of knee flexion were able to go
from sitting to standing independently
without any assistance or assistive
devices. Patients with less than 95 of
knee flexion had worse Goniometry scores
(p<.0001). Only patients with a very stiff
knee will have function that is really
affected by ROM. Their study identified
95 of knee flexion as a clinically
meaningful cut-off point above which
ROM does not limit a patients normal
activities after TKR. However the long-
term effects of this limitation of ROM
could be detrimental to the normal joints,
because of the patients over compensation
when performing activities of daily living.
3. Knee Stability and alignment: The
majority of the patients had normal
stability and alignment. This indicates that
the total score of the Knee Society Knee
Score in this sample is not really affected
by the components of stability and
alignment, but mainly by pain and ROM.
Malalignment of the prosthesis could
result in stiffness which although
uncommon is a disabling problem (Jerosh
and Aldawoudy 2007). Treatment of
malalignment could include manipulation
or revision arthroplasty (Bong and Di
Cesare 2004),which has been shown to be
successful in terms of post-operative
function(Miner et al 2003).
4. Knee Flexion contracture and extension
lag: A percentage of the patients in this
study had some degree of a flexion
contracture and some degree of an
extension lag at six weeks post operation.
This could indicate that attaining full knee
extension and flexion is not that important
when it comes to functional activities such
as going from sitting to standing, walking
and stair climbing, as these same patients
performed well when assessed using the
ILOA Scale. Functional range of motion is
between 45 and 105 (Miner et al 2003).
As long as the extension lag and the
flexion contracture do not interfere with
this range of motion, the patient should
manage functionally. Patients also
compensate when performing activities by
using the other leg or their arms to assist
with transfers. The quality of the
movement being performed is not
important to the patient, what is of
importance is completing the movement
by any means possible. The long term
effect of poor ROM and poor quality of
movement is that the normal joints take
excess strain and over a prolonged period,
there is an increased risk of developing
pain and discomfort in the normal joints
due to osteoarthritis.
ILOA Score:
Most of the patients were able to go from
lying to sitting, sitting to standing and
walking 4.57 meters independently, with
minimal assistance. The patients scored
very well in these three categories. This
indicates that the ILOA Scale is not a
sensitive enough functional measuring
tool when used at six weeks post
operation. It measures basic functional
ability, not higher function. It was
developed to determine whether patients
who had had total hip and knee
replacements were ready to be discharged
from hospital (Shield et al 1995). It is the
role of physiotherapists in the hospital to
ensure that patients are able to perform
basic transfers so that they will be
independent at home, after they are
discharged from hospital. Five patient did
not use an assistive device to perform the
five functional tasks. She did however
require nearby supervision for the
walking, stairs and the speed test. Two
patients used a walking frame at six weeks
after the operation. Only one patient was
unable to climb the stairs even with
maximal assistance
CONCLUSIONS
The goal of a TKA is to provide the
patient with a stable and painless knee
with sufficient ROM to perform ADLs
(Gandhi et al., 2006). As many studies
only focused on the long-term status of
TKA patients (Aarons et al., 1996), this
study examined the short-term status. The
value of this is to furnish patients and the
therapist with knowledge of their acute
postoperative status and appropriate
rehabilitation programme that will
influence their prognosis. integrity which
was measured using the Knee Society
Knee Score and function as measured
using the ILOA Scale, six to eight weeks
post surgery on total knee replacement.
Research Recommendations:
A functional tool should be developed that
assesses the attainment of higher
functional milestones, as well as the
quality of the movement. If a more
sensitive functional assessment tool was
used, one that looked at higher functional
levels, a more accurate functional
evaluation of the knee replacement could
be determined.
REFERENCES:
1. De Jonghe B, Sharshar T,
Lefaucheur JP, Authier FJ, Durand-
Zaleski I, Boussarsar M, et al; Groupe
de Reflexion et dEtude des
Neuromyopathies en Reanimation.
Paresis acquired in the intensive care
unit: a prospective multicenter study.
JAMA 2002;288(22):28592867.
2. de Letter MA, Schmitz PI, Visser
LH, Verheul FA, Schellens RL, Op de
Coul DA, van der Meche FG. Risk
factors for the development of
polyneuropathy and myopathy in
critically ill patients. Crit Care Med
2001;29(12):22812286.
3. Coakley JH, Nagendran K,
Yarwood GD, Honavar M, Hinds CJ.
Patterns of neurophysiological
abnormality in prolonged critical
illness. Intensive Care Med
1998;24(8):801807.
4. Garnacho-Montero J, Madrazo-
Osuna J, Garcia-Garmendia JL, Ortiz-
Leyba C, Jimenez-Jimenez FJ,
Barrero-Almodovar A, et al. Critical
illness polyneuropathy: risk factors
and clinical consequences: a cohort
study in septic patients. Intensive Care
Med 2001;27(8): 12881296.
5. Spitzer AR, Giancarlo T, Maher L,
Awerbuch G, Bowles A.
Neuromuscular causes of prolonged
ventilator dependency. Muscle Nerve
1992;15(6):682686.
6. Rudis MI, Guslits BJ, Peterson EL,
Hathaway SJ, Angus E, Beis S,
Zarowitz BJ. Economic impact of
prolonged motor weakness
complicating
neuromuscular blockade in the
intensive care unit. Crit Care Med
1996;24(10):17491756.
7. Latronico N, Peli E, Botteri M.
Critical illness myopathy and
neuropathy. Curr Opin Crit Care
2005;11(2):126132.
8. Bednarik J, Lukas Z, Vondracek P.
Critical illness polyneuromyopathy:
the electrophysiological components
of a complex entity. Intensive Care
Med 2003;29(9):15051514.
9. Van den Berghe G, Wouters P,
Weekers F, Verwaest C, Bruyninckx
F, Schetz M, et al. Intensive insulin
therapy in the critically ill patients. N
Engl J Med 2001;345(19):13591367.
10. Tennila A, Salmi T, Pettila V,
Roine RO, Varpula T, Takkunen O.
Early signs of critical illness
polyneuropathy in ICU patients with
systemic inflammatory response
syndrome or sepsis. Intensive Care
Med 2000;26(9):13601363.
11. Rabuel C, Renaud E, Brealey D,
Ratajczak P, Damy T, Alves A, et al.
Human septic myopathy: induction of
cyclooxygenase, heme oxygenase and
activation of the ubiquitin proteolytic
pathway. Anesthesiology
2004;101(3):583590.
12. MacFarlane IA, Rosenthal FD.
Severe myopathy after status
asthmaticus (letter). Lancet
1977;2(8038):615.
13. Witt NJ, Zochodne DW, Bolton
CF, GrandMaison F, Wells G, Young
GB, Sibbald WJ. Peripheral nerve
function in sepsis and multiple organ
failure. Chest 1991;99(1):176184.
14. Knox AJ, Mascie-Taylor BH,
Muers MF. Acute hydrocortisone
myopathy in acute severe asthma.
Thorax 1986;41(5):411412.
15. Hund E, Genzwurker H, Bohrer H,
Jakob H, Thiele R, Hacke W.
Predominant involvement of motor
fibres in patients with critical illness
polyneuropathy. Br J Anaesth
1997;78(3):274278.
16. Thiele RI, Jakob H, Hund E,
Tantzky S, Keller S, Kamler M, et al.
Sepsis and catecholamine support are
the major risk factors for critical
illness polyneuropathy after open heart
surgery. Thorac Cardiovasc Surg
2000;48(3):145150.
17. Garnacho-MonteroJ, Amaya-Villar
R, Garcia-Garmendia JL,Madrazo-
Osuna J, Ortiz-Leyba C. Effect of
critical illness polyneuropathy on the
withdrawal from mechanical
ventilation and the length of stay in
septic patients. Crit Care Med
2005;33(2):349354.
18. Bolton CF. Sepsis and the
systemic inflammatory response
syndrome: neuromuscular
manifestations. Crit Care Med
1996;24(8): 14081416.
19. Latronico N, Fenzi F, Recupero D,
Guarneri B, Tomelleri G, Tonin P, et
al. Critical illness myopathy and
neuropathy. Lancet 1996;
347(9015):15791582.
ACKNOWLEDGMENT:
The authors thank Dharam Pandey (MPT-neuro), Deepa Dabas (MSc-psycho) for assistance
throughout the study.
CORRESPONDENCE:
*Bijender Sindhu PhD,PT Research Student**Dr.Manoj Sharma, MBBS,
MS(ortho)***Dr.Raj k Biraynia, MBBS, D.ortho *School of Physical Therapy, Faculty of
Medical Science, Singhania University**Department of orthopedic surgery, Jaipur Golden
Hospital *** Department of orthopedic surgery, Sarvodaya Multispeciality Hospital. This
study was not funded through a grant from the any organization.
Comparison of the Effect of Isometric Exercise of Upper Limb on Vitals
between Young Males and Females
Pranjal Parmar. BPT*
Abstract: Background and objective: studies on gender difference in
cardiovascular responses to isometric exercises have been numerous and
confliction the objective of this study was to determine if cardiovascular response
to upper extremities isometric exercises differ between apparently healthy male
and female subjects. Method: 60 young adults age between 18 to 22 years were
included in study. These consisted of 30 males and 30 females. The baseline
cardiovascular parameters (HR, SBP, DBP & MAP) were recorded. After two
sets of three isometric upper limbs for 3 minutes these parameters recorded at the
end of exercise and after recovery. Results:An increase in HR ,SBP , DBP&MAP
was seen in both groups after exercise .the result showed group B had more
increase in HR,SBP,DBP and MAP as compared to group A and significant rise
in MAP &SBP in group B. Conclusion: Isometric exercise of upper limb can lead
to increase in SBP, DBP, MAP &HR among apparently healthy males & females.
It is more proannounced in males as compared to females. SBP &MAP increased
in both but more in males as compared to females.
Keywords: Isometric Exercises, Cardiovascular Measures
INTRODUCTION
Exercise, a common physiological stress,
can elicit cardiovascular abnormalities not
present at rest and can be used to
determine the adequacy of cardiac
function.
1
The isometric contractions are
seen in various exercises like pushing or
lifting heavy load where net displacement
of load is not, but the rising tension can be
felt in contracting muscles.
3
It imposes
greater pressure than volume load on left
ventricle in relation to the body ability to
supply oxygen.
4
The metabolic demands
of the exercising muscles increases,
depending upon intensity of exercises and
are met with various changes in
circulatory and respiratory system.
13
The effect of isometric exercises on vitals
in between males and females may vary
with substantial anatomical, physiological
and morphological differences that exist
between men and women which may
affect their exercise capacity and influence
magnitude of response to exercise.
5
The average isometric strength estimate is
generally 30% greater in men than in
women in different muscle group. Gender
difference in cardiovascular response to
static exercise is believed to be due to
differences in sympathetic
parasympathetic or adrenal interactions at
cardiac level.
The larger the muscle group that is
involved in isometric tension the greater
the cardiovascular response.
6
Response To Exercise:
7
When you exercise or take part in a
strenuous sport you will notice several
changes taking place in your body:
a. Your heart beats stronger and faster
b. Your breathing quickens and deepens
c. Your body temperature increases
d. You start to sweat
e. Your muscles begin to ache
1. Heart beats stronger and faster:
During exercise it is mainly adrenaline
that produces changes in the heartbeat.
Adrenaline is a hormone which causes the
heart rate to quicker.
2. Breathing quickens and deepens:
You breathe quicker so as to get more
oxygen into the lungs. An efficient heart
can then transport this to the working
muscles. Training can be of great benefit
to the Respiratory System. The capacity of
the lungs is increased, which allows more
oxygen to be taken in per breath.
3. Temperature rises:
When we exercise, our muscles are
working and they generate heat, so our
body temperature rises. Body temperature
is regulated by heat radiating from the
skin and water evaporating by sweating.
When we shiver, our muscles are working
to produce heat in order to raise our body
temperature.
4. Start to sweat:
As we have just seen, some of our energy
is turned into heat. The body will tolerate
a small rise in temperature, but very soon
we begin to sweat. If the conditions are
hot, we sweat more and produce less
urine.
We also lose salt as well as body heat and
water. We have to replace the salt so that
the body stays the same, otherwise we will
get cramp.
5. Muscles begin to ache:
As we now know, in order to work,
muscles need energy. Energy comes from
food, which is mainly converted to
glucose. To work more efficiently muscles
also need plenty of oxygen. Glucose and
oxygen are brought to the muscles in the
blood. Wastes such as carbon dioxide are
carried away in the blood. This process of
getting energy is called respiration.
Glucose + Oxygen = Energy + CO2 +
Water
When muscles do extra work more
Glucose and Oxygen are needed, so more
blood must flow to the muscles.
Eventually it becomes impossible to get
enough oxygen to the muscles, so they use
a different method of getting energy.
Glucose is still used, but now there is a
waste product called lactic acid, which
makes muscle ache, & muscles.
Acute Cardiovascular Response to
Exercise:
As exercise intensity increases, heart rate,
stroke volume, and cardiac output increase
to get more blood to the tissues. More
blood forced out of the heart during
exercise allows for more oxygen and
nutrients to get to the muscles and for
waste to be removed more quickly. Blood
flow distribution changes from rest to
exercise as blood is redirected to the
muscles and systems that need it.
CLINCAL SIGNIFICANCE
Vitals response to exercise has been used
as major criteria in exercise prescription
for both patient and healthy population.
Thus for prescribing isometric exercise,
repetitions and frequency it would be
helpful and prevent the adverse effect on
vitals. The study would also be helpful in
prescribing exercises for those with
cardiovascular compromise. It would help
to determine the safety limits of the
exercise.
OBJECTIVES:
1. To analyze if there is any change in
vitals as a result of isometric exercises of
upper limb
2. To compare the response of upper limb
isometric exercises in young male and
female.
METHODOLOGY
Research Design: An quasi-Experimental
(comparative) study. Sample Size: 60
normal individuals. Sample Population:
60 young adults between 18 to 22 yrs.
Group A: 30 normal individuals (females)
Group B: 30 normal individuals(males)
Type of Sampling: Convenient sampling
with random assignment. Duration of
Study: one month. Study Set Up:
Physiotherapy OPD of a tertiary care
hospital.
Inclusion Criteria:
No previous history of known
cardiovascular condition.
Normal values of vitals at rest.
No neurological defecit in upper
limb.
Sex both male and female.
Willingnessof patient.
Exclusion Criteria:
Fracture of upper limb bones.
Cervical vertebrae or scapula
fracture.
Neurogenic deficit.
Congenital anomalies.
Previous exercise training
Any disability limiting to upper
limb exercise.
Psychiatric patients.
Non-willing patients.
Outcome Measures:
Heart rate of patient at rest,
immediately post exercise and 3
minutes after exercise
Blood pressure i.e. systolic and
diastolic blood pressure at rest,
immediately postexercise and 3
minutes after exercise.
Mean arterial pressure was
calculated from the above data.
PROCEDURE
60 individuals were selected according to
the inclusion and exclusion criteria. The
need of the study and treatment
intervention was explained to the
individuals and their written consent was
taken from them. 60 individuals were
assigned into two groups, group A and
group B, 30 patients in each group.
Procedure details of group A and group
B:
Pre-measures: Heart rate and blood
pressure was measured using an electronic
sphygmomanometer in standing position.
Reading was noted.
Individual position: standing position.
Therapist position: on the individual side
in stride standing position.
Procedure: Participants in upstanding
position performed 3 upper extremities
isometric exercises i.e. 2 sets of each
exercise for each 30 second each thus total
duration of exercise for 3 minutes.
1. The exercise are pushing against the
wall with outstretched arms and were
instructed to exert maximal tension on
wall.
8
2. Hands clasped together and brought to
manubrosternal level to chest while
shoulders are 60 70 degree abducted and
participants were instructed to maximally
generate tension by pressing opposite
hands against each other.
8
3. Both palms on wall with participants
standing ahead arms extended and were
asked to push the wall without coming
behind and keeping elbow straight.
8
Participants were instructed to avoid
valsalva maneuver by not holding breath
Thereafter participants were asked to rest
for 10 minutes before leaving. Post-
measures: Heart rate and blood pressure
was measured immediately after exercise
and 3 minutes after exercise. All patients
were comfortable after the treatment
session.
DATA ANALYSIS AND RESULT
The data collected was entered in excel
sheet and statistical analysis was done
using SPSS software. Heart rate and blood
pressure are objective data hence can be
considered for statistical analysis. This
isan interval data hence pre and post
parmeters was statistically analysed using
paired t-test, and difference in paramaters
between two groups was statistically
analysed using unpaired t- test.
Table No.1
Mean age (yrs)of study group
Group Number Age (yrs)
A 30 20.23
B 30 20.16
The above graph shows mean age of group A and group B.
Table 2
Rest Post exercise Recovery
Group A (females) 117.8 123.28 120.45
Group B (males) 123.6 134.58 128.95
Table 3
Value P value Significance
Group
A
-1.6912 3.47e-
10
Difference is
significant.
Group
B
-1.3678 3.17e-
12
Difference is
significant.
Table 4
Rest Post exercise Recovery
Value -5.46072 -10.1411 -10.0176
P value 1.64e-05 3.14e-09 2.19e-11
Table 2 shows mean of systolic blood pressure at rest in group A is 117.8 and group B IS
123.6 ,post exercise in group A is 123.28 and group B is 134.58 and recovery in group A is
120.45and group B is 128.95.
Table 3 shows p value by paired t test in group A and group B and difference is statically
significant.
Table 4 shows p value by unpaired t test in group A and group B at rest, post exercise and
recovery and difference is statically significant.
The graph shows mean of males and
females of systolic blood pressure at rest ,
post exercise and recovery.
.
The above graph shows distribution of
systolic blood pressure in males and
females at rest, post exercise and
recovery.
Diastolic Blood Pressure
Table 5
Rest Post exercise Recovery
Group A (Females) 75.6 84.25 80.20
Group B
(Males)
80 96.50 83.60
Table 6
Value P value Significance
Group
A
-1.345 3.95e-
15
Difference is
significant.
Group
B
-1.236 3.21e-
08
Difference is
significant.
Table 7
Rest Post
exercise
Recovery
Value -5.78263 -14.6703 -4.4098
P
value
1.1e-06 3.14e-09 1.58e-07
Table 5 shows mean of diastolic blood
pressure at rest in group A is 75.6 and
group B is 80, at post exercise in group A
is 84.25 and in group B is 96.50 and at
recovery in group A is 80.20 and group B
is 83.60.
Table 6 shows p value by paired t test in
group A and group B and difference is
statistically significant.
Table 7 shows p value by unpaired t test at
rest, post exercise and recovery in group
A and group B and difference is
statistically significant
The above graph shows mean of males
and females of diastolic blood pressure at
rest, post exercise and recovery.
The above graph shows distribution of
diastollic blood pressure between males
and females at rest, post exercise and
recovery.
Mean Arterial Pressure
Table 8
Rest Post exercise Recovery
Group A (Females) 89.66 97.26 93.61
Group B
(Males)
94.53 109.19 98.71
Table 9
Value P value Significance
Group A -1.327 5.78e-10 Difference is
significant
Group B -1.784 4.08e-12 Difference is
significant.
Table 10
Table 8
shows
mean of
mean
arterial pressure at rest in group A is 89.66 and in group B is 94.53,at post exercise in group
A is 97.26and in group B is 109.19 and at recovery in group A is 93.61 and group B is 98.71.
Table 9 shows p value by paired t test in group A and group B difference is statistically
significant.
Rest Post exercise Recovery
Value -7.001 -9.57881 -7.17096
P value 1.16e-09 1.91e-11 2.06e-09
Table 10 shows p value by unpaired t test at rest, post exercise and recovery in group A and
group and difference is statistically significant.
The above graph shows mean of mean arterial pressure at rest, post exercise and recovery
between group A and group B.
The above graph shows distribution of mean arterial pressure between males and females at
rest, post exercise and recovery.
Heart Rate
Table 11
Rest Post exercise Recovery
Group A (Females) 72.6 80.40 76.40
Group B
(Males)
74.4 82.95 78.65
Table 12
Value P value Significance
Group
A
0.00615 0.015E-
04
Difference
is
significant
Group
B
0.00322 0.14E-
05
Difference
is
significant
Table 13
Rest Post exercise Recovery
Value 0.00123 0.00808 0.00055
P value 0.012e-06 0.080e-05 0.055e-06
Table 11 shows mean of heart rate at rest in group A is 72.6 and in group B is 74.4, at post
exercise in group A is 80.40 and in group B is 82.95 and at recovery in group A is 76.40 and
in group B is 78.65.
Table 12 shows p value by paired t test in group A and group B and difference is statistically
significant.
Table 13 shows p value by unpaired t test at rest, post exercise and recovery in group A and
group B and difference is statistically significant.
Heart Rate
The above graph shows mean of heart rate
in males and females at rest, post exercise
and recovery.
The above graph shows distribution of
heart rate between males and females at
rest, post exercise and recovery.
DISCUSSION
The study investigated the gender
difference in cardiovascular response to
upper extremities isometric exercise
among apparently young healthy subjects.
60 participants were included in the study.
They were divided into two groups, group
A and group B. Group A included female
gender and group B included male gender.
BP, HR and MAP were taken as outcome
measure. These measures were taken pior,
immediately after test and 3 minutes after
study. The data collected was statistically
analysed. The result showed group B had
more increase in HR,SBP ,DBP AND
MAP as compared to group A and there
was significant rise in MAP and SBP in
group B. The average isometric strength
estimate is generally about thirty percent
greater in men than in women in different
muscle groups . Upon initiating isometric
tension, increases in heart rate, systolic
blood pressure, and diastolic blood
pressure occur. Mitchell and associates
and Seals et al suggested that
cardiovascular responses to isometric
exercise are greater when larger muscle
groups are involved. While heart rate
responses to sustained submaximal static
contractions tend not to be significantly
different before, during, or after exercise,
blood pressure responses to this exercise
are significantly elevated before, during,
and after exercise Gender differences in
cardiovascular responses to static exercise
are believed to be due to differences in
sympathetic-parasympathetic or adrenal
interactions at the cardiac level. The
finding of this study revealed that there
was no significant gender difference in
vitals of participants at baseline which
was statistically significant. The data
collected reveals that post exercise heart
rate, systolic blood pressure ,diastolic
blood pressure and mean arterial pressure
were higher than pre exercise values and
was statistically significant in both groups
ie group A and group B.
When values of recovery i.e. 3 minutes
after exercise when compared it was
almost same in both groups but when
compared to values at rest it was much
greater than recovery values.
The result between the two was calculated
using unpaired t test. Therefore upper
extremities isometric exercise had
significant effect on heart rate, systolic
blood pressure, diastolic blood pressure
and mean arterial blood blood pressure.
When values of group A and group B at
post exercise were compared it was seen
that male participants (group B) had
higher post exercise MAP and SBP had
level than females (group A) (p<0.05)
These result indicate that more blood is
pumped by left ventricle into aorta in
response to upper extremities isometric
exercise among males than females; while
myocardial oxygen uptake & measure of
oxygen consumption of heart muscles of
female participants in response to upper
extremities isometric exercises is higher
than that of males.
The tissues working hard during exercise
and also after the completion of exercise
require more oxygen than normal to pay
off this oxygen debt incurred during the
exercise. These results in increase in blood
supply to active muscles to supply this
extra amount of blood. At rest, muscles
receive approximately 20% of total blood
flow but during exercise blood flow to
muscles increase to 80 -85% .
Generally ,longer the duration of exercise
greater the role the cardiovascular system
plays in metabolism and performance
during exercise bout.eg an 1T00 meter
walk (little or no cardiovascular
involvement) versus a marathon(maximal
involvement).
9
It has reported that release of adrenaline
and lactic acid into the blood result
increase in a heart rate.
The isometric exercises does not increase
the oxygen demand to the extend raised by
isotonic exercise thus DBP does not rise
much in isometric exercise The isometric
exercise results in pressure overload on
heart. The myocardial oxygen
consumption (mvo2) also increase due to
exercise . Higher ventricular contraction is
evoked among males leading to increase
in systolic blood pressure.
This indicates that the males have higher
myocardial oxygen demand during
isometric exercise predisposing them to
greater risk of ischemia if developing
cardiovascular risk, factor compromising
the coronary blood flow.
10
It has been seen males have higher plasma
levels of all three catecholoamines out of
which plasma levels of epinephrine are
higher as compared to females .this results
in increase in MAP immediately at of
exercise.
The findings supports the results of
previous investigators than upon initiation
isometric tension increase heart rate,
systolic blood pressure and diastolic blood
pressure occur.
12
The result of
investigations have been reported at best
inconsistent and do not follow definite
pattern.
12
However during the recovery period the
vitals were decreased as compared to
immediately post exercise in both genders.
However the vitals were not the same as
they were at rest prior to commmencent of
exercise.
The result of study is supported by the
articles Gender difference in
cardiovascular response to upper
extremities isometric exercise in
normotensive subjects. By Cembada and
Gender differences in cardiovascular
response to isometric in seated and supine
positions by Don Melrose. The proposed
mechanisms attempting to explain gender
differences in cardiovascular responses to
isometric exercise have been numerous
and conflicting. Sanchez et al. found
differences in adrenergic patterns between
genders in response to isometric exercise
and support the study. Ettinger and
associates demonstrated attenuated
increases in blood pressure and muscle
sympathetic nerve activity compared with
men. In data also derived from static
exercise as well as temperature and
psychological stressors, Jones et al found
that gender did not influence sympathetic
neural reactivity to stressors such as
isometric handgrip exercise
Changes in posture often experienced
during exercise or sporting activities have
also been shown to elicit various
circulatory adaptations. Sagiv et al. and
Borst et al. both noted changes in
cardiovascular regulation as a result of
postural changes. Relatively fewer studies
have investigated the cardiovascular
adaptations to exercise performed when
posture does not change during the time
course of the positions.
A further study can be made:
Comparison of vitals for larger
muscles groups to smaller muscles
group in upper limb isometric
exercises.
Comparison of vitals in isometric
exercise for upper limb versus
lower limb.
The result can be used as
It can be used for prescription of
exercise in those with
cardiovascular crompromise and
elderly patients.
It can be used to determine the
safety limits during exercise
regimen.
CONCLUSION
The above study gives following
conclusion:
1. Isometric exercises of upper limb can
lead to increase in systolic blood pressure
,diastolic blood pressure ,mean arterial
pressure and heart rate among apparently
healthly males and females.
2. This was more preannounced in males
than females .Systolic blood pressure
(SBP) and Mean arterial pressure (MAP)
increased in both but more males as
compared to females
LIMITATION
1. The participants in study were young
and elderly or middle aged participants
were not included in these study.
2. All the subjects who were included in
the study were students.
3. The participants nutritional status or
BMI were not considered while selection.
4. The occupation or lifestyle of
participants was not considered.
5. The muscle mass or bulk of upper limb
was not considered.
REFERENCES:
1. Journal of Exercise Physiology
Online. Volume 8, number 5,
august 2005.
2. Therapeutic Exercise, Carolyn
Kisner & Lynn Allen Collby.Pg
No 168,5th Edition
3. Sports Fitness Advisor, Fleck
st&kramerwj(2004).
4. Husketh Mount, pg no 92-96,lord
street,merseyside, england.
5. Effect of exercise .stending
lenderg 2004
6. Gender difference in
cardiovascular response to
isometric exercise.gatzke 2005
7. Circulation, amercian heart
association,2007pg no 3 &4
8. Clinical Orthopaedic rehabilitation
,2nd editions brent brotzman,pg no
138-142
9. Cardiovascular system and
exercise physiology,aulter &amer
suleman
10. International journal of biomedical
reserach,srinath galag & ravipati
sarath volume 2,november 2011
11. Gender difference in
cardiovascular response to
isometric exercise of upper
limbs,howden et clf 2006.
12. Gender difference in
cardiovascular response to
isometric exercise,gatzke
13. The essential guide to building
muscles by phil daviee.
CORRESPONDENCE:
* Consultant Physiotherapist, Bhagwan Mahaveer Medical Centre, M.G. Road, Goregaon
(W), Mumbai.
Email: pranjalparmar38@yahoo.in
Growth in Cerebral Palsy Children between 3-13 years in Urban Dharwad,
India
Parmar Sanjay T.*. MPT (Paediatrics). Nayana A. Khobre**. MPT (Paediatrics).
Abstract: Background & Objective- Cerebral palsy is defined as a group of non-progressive
disorders of movement or posture due to a defect or lesion of the immature brain. The incidence
of cerebral palsy is 2-2.5 cases in every 1000 live births. Cerebral palsy is frequently associated
with poor growth and children with cerebral palsy tend to be shorter and lighter than their
normal counterparts. Our objective of the study is to find out growth in cerebral palsy children.
Method - A sample size of 100 children with cerebral palsy of either gender from 3-13 years
were assessed for body mass index, growth of children with cerebral palsy was found out. The
outcome measures Child Developmental Care/National Health Center Statistics growth charts
(CDC/NHCS). Results - Statistical analysis was done with statistical software (n Master 1.0).
Data analysis and results showed no statistical significance growth found in children with
cerebral palsy. The study showed that clinically all the children with cerebral palsy had low
growth when assessed on CDC/NHCS growth charts. Interpretation and conclusion - The
children with cerebral palsy had low growth compared with the other counterparts of same age
group.
Key words- Growth, Cerebral Palsy.
INTRODUCTION
Cerebral palsy (CP) is defined as
umbrella term covering a group of non-
progressive, but often changing, motor
impairment syndromes secondary to
lesions or anomalies of the brain arising in
the early stages of its development.
Cerebral palsy is in variably associated
with many deficits such as mental
retardation, speech and language and oral-
motor problems. The etiology of CP is
very diverse and multi-factorial. The
causes are congenital, genetic,
inflammatory, infectious, anoxic,
traumatic and metabolic. The injury to the
developing brain may be prenatal, natal or
postnatal1. The incidence of cerebral palsy
is 2-2.5 cases in every 1000 live births.
There are an estimated 4-5 million
children and people in India with cerebral
palsy
2
.
The incidence of malnutrition in
individuals with cerebral palsy is a
combination of factors, which directly or
indirectly result in reduced food and
nutrient intake
3
. Feeding problems are not
easily recognizable in children and in
order to optimally utilize the impaired
feeding potential in these children, early
identification of the incidence of
malnutrition in individuals with cerebral
palsy is necessary. It also requires regular
assessment of feeding and nutritional
status and appropriate nutritional
rehabilitation
4
.
While the prevalence of growth disorders
among these children is unknown, certain
observations have been made. Growth
failure has been related to the type of cp-
spastic or athetoid and to topographical
distribution, and oral-motor dysfunction
also has been associated with poorer
growth
5
A study done on percent body fat, muscle
area and oral motor functions are
important factors for weight gain and
linear growth of children with cerebral
palsy. The identification of the nutritional
problem has a great potential to help
improve weight, muscle mass, decrease
irritability and circulation in order to halt
the incidence of malnutrition in children
with cerebral palsy
6
.
A study done on incidence of malnutrition
in children with cerebral palsy tells about
feeding problem are usually complicated
by the lack of awareness of parents of
incidence of malnutrition in cerebral palsy
children. The main reasons for lack of
awareness in parents were illiteracy,
misconception about the disease and
associated complications in cerebral palsy.
The psychological impact of having child
with severe chronic neurological disease is
so deep that parents do not appreciate the
feeding problems to the extent they should.
The study done on Growth and nutrition
disorders is common secondary health
conditions in children with cerebral palsy
(CP). Poor growth and malnutrition in CP
merit study because of their impact on
health, including psychological and
physiological function, healthcare
utilization, societal participation, motor
function, and survival. Understanding the
etiology of poor growth has led to a
variety of interventions to improve growth.
Increased recognition and understanding
of neurological, endocrinal, and
environmental factors have begun to shape
care for children with CP, as well. The
investigation of these factors relies on
advances made in the assessment methods
available to address the challenges
inherent in measuring growth in children
with CP. Descriptive growth charts and
norms of body composition provide
information that may help clinicians to
interpret growth and intervene to improve
growth and nutrition in children with CP.
Linking growth to measures of health will
be necessary to develop growth standards
for children with CP in order to optimize
health and well-being.
METHOD
A sample size of 100 children with
cerebral palsy with either gender from 3-
13 years of age was assessed for body
mass index. The study was conducted for 1
year in Physiotherapy OPD of SDM
medical hospital Dharwad Karnataka
India. Ethical clearance is obtained from
the Institutional Ethical Committee, Shri
Dharmasthala Manjunatheshwara College
of Medical Sciences and Hospital, prior to
the commencement of the study. The
children included in the study were
diagnosed cerebral palsy cases, who were
able to stand on stadiometer and weighing
machine. Children who were un-
conscious, unco-operative, who were not
able to stand and unstable Patients were
excluded.
Parents of the subjects willing to
participate were briefed about the study
and how the study would help their
children. A written consent was obtained
from the parents of the children.
Children diagnosed with cerebral palsy
were assessed for BMI by taking the
height and weight of the children. The
child was made to stand on the
Stediometer with the consideration of
physical disabilities to measure the height
and Weight was measured by making the
children stand on weighing machine.
The outcome measures was CDC/NHCS
growth charts. The growth was assessed by
height in meters and weight in kilograms
and BMI (Body Mass Index) is calculated
in weight (in kgs) by height square (in
meters). And BMI percentiles were
calculated on CDC/NHCS growth charts.
DATA ANALYSIS
Statistical analysis was done with
statistical software (n Master 1.0).
descriptive analysis was carried out using
mean and standard deviation of mean age,
height, weight, BMI, BMI percentile.
Comparison between variables is done
using unpaired t-test. The p-value is
0.5693 which shows that there is no
significant difference between boys and
girls.
RESULTS
The table1 depicts the distribution of study
subjects according to gender and different
types of cerebral palsy children. It shows
mainly spastic cerebral palsy cases more in
the present study which includes 3-13
years of age group. The table 2 depicts the
mean and standard deviation age of both
boys and girls.
The table 3, 4, 5 depicts that the mean and
standard deviation (SD) values of height,
weight, BMI and BMI percentile for
different diagnosis of cerebral palsy in
which dystonic and diplegic type have less
mean values. And by different age groups
of 3-5years, 6-8 years, 9-11 years, and 12+
years have increasing mean values as per
the age increases. The mean values of
height, weight and BMI is less in boys
than girls which was not significant. The
table 5 depicts the children in our study are
underweight with 86%.
The table 6 shows that comparison of boys
and girl children with respect to BMI
scores by t-test with mean and standard
deviation where there was no significant
difference between boys and girls.
ILLUSTRATIONS FOR DIFFERENT POSITIONS
Table 1: Distribution of study subjects according to gender by different diagnosis
Diagnosis Boys % Girls % Total
Ataxic CP 5 71.43 2 28.57 7
Dystonic CP 5 83.33 1 16.67 6
Hemiplegic CP 11 64.71 6 35.29 17
Hypotonic CP 6 100.00 0 0.00 6
Diplegic CP 17 60.71 11 39.29 28
Quadri CP 21 80.77 5 19.23 26
Triplegic CP 8 80.00 2 20.00 10
Total 73 73.00 27 27.00 100
The above table depicts Distribution of study subjects according to gender by different
diagnosis
Table2: Mean and SD total oral motor scores and its dimensions by diagnosis
Diagnosis
BMI BMI%
Means Std.Dev. Means Std.Dev.
Ataxic CP 18.1857 4.9878 63.8571 36.0159
Dystonic CP 14.3333 3.2629 35.1667 47.2035
Hemiplegic CP 15.5706 2.0784 41.0000 34.6717
Hypotonic CP 16.0500 4.2646 42.1667 46.2100
Diplegic CP 15.5429 3.0375 30.5357 35.6282
Quadri CP 16.7615 4.2477 48.6154 39.3732
Triplegic CP 17.3800 2.8197 65.5000 32.2154
All Grps 16.1910 3.5160 43.8200 38.2515
Table 3: Mean and SD total oral motor scores and its dimensions by diagnosis
Diagnosis
BMI BMI%
Means Std.Dev. Means Std.Dev.
Ataxic CP 18.1857 4.9878 63.8571 36.0159
Dystonic CP 14.3333 3.2629 35.1667 47.2035
Hemiplegic CP 15.5706 2.0784 41.0000 34.6717
Hypotonic CP 16.0500 4.2646 42.1667 46.2100
Diplegic CP 15.5429 3.0375 30.5357 35.6282
Quadri CP 16.7615 4.2477 48.6154 39.3732
Triplegic CP 17.3800 2.8197 65.5000 32.2154
All Grps 16.1910 3.5160 43.8200 38.2515
Table 4: Mean and SD of Wt, Ht and BMI by age groups
Variables Summary 3-5yrs 6-8yrs 9-11yrs 12+yrs Total
Height Means 97.0000 115.7500 130.1481 145.1250 119.6500
Std.Dev. 10.1612 7.6031 10.5492 7.0887 18.6917
Weight Means 13.2120 21.5031 28.5185 41.5563 24.5330
Std.Dev. 3.2447 5.2859 8.3176 12.2666 11.7800
BMI Means 13.7760 16.1719 16.5222 19.4438 16.1910
Std.Dev. 2.0765 3.0619 2.6963 4.6381 3.5160
The above table depicts Mean and SD of Wt, Ht and BMI by age groups
Table 5: Distribution of samples by BMI category and gender
BMI Male % Female % Total %
Under weight 61 70.93 25 29.07 86 86.00
Normal 9 90.00 1 10.00 10 10.00
Over weight 3 75.00 1 25.00 4 4.00
Total 73 73.00 27 27.00 100 100.00
The above depicts that Distribution of samples by BMI category and gender
DISCUSSION
In our study the mean age group of boys
population is 7.794 and of girls population
is 8.266 out of the total score which
showed the mean value more in age group
of 9-11years in total score which depicts
there is no significant difference in BMI in
both male and female population. As in 9-
11yrs age group 30 children were there
and in 12+yrs age group were 15 children
may be because of number of children
more in 9-11yrs group mean value was
more as comparative to other groups.
The mean values in the different variable
of our study show different mean values of
each type of cerebral palsy relatively
quadriplegic and hypotonic having lower
mean as compared to others due to smaller
sample size in them for which no statistical
analysis was been carried out.
Studies have documented that growth
patterns for patients with cerebral palsy
(CP) are different from those in the general
population. Patients with CP have below
average weight, linear growth, and muscle
mass and fat stores compared with their
peers in the general population. Bone mass
density is also reduced, especially among
patients who are non-ambulatory
Poor growth in children with CP may be
related to nutritional factors, physical
factors or factors related to the brain lesion
itself. Nutritional factors include
inadequate dietary intake, secondary to
impaired oral motor and swallowing
competence and poor nutritional status and
may impact directly on growth. Physical
factors result in decreased mechanical
stress on bones due to immobility or lack
of weight bearing.
Bone growth studies have suggested that
immobilization decreases bone formation
and longitudinal bone growth and
increases bone resorption, which
suppresses certain growth-stimulating
hormones. Factors related to the brain
lesion itself may impact on growth either
directly (via a negative neurotrophic effect
on linear growth) or indirectly (via the
endocrine system). Growth differences
between impaired and unimpaired limbs in
children with hemiplegic, support the
hypothesis that non-nutritional factors play
a significant role in reducing growth in
children with CP.
A study done on Identification of
malnutrition in children with cerebral
palsy: poor performance of weight-for-
height percentiles where explained,
undernourished children with CP have
changes in body composition and
proportion compared with normally
developing peers. Alterations include
increased total body water, severely
depleted fat stores, minimally depleted
muscle stores, severe short stature, and
decreased bone density.
CONCLUSION
All the children with cerebral palsy had
lower growth than other peer groups, when
they were assessed on CDC/NHCS growth
charts, which may be due to oral motor
dysfunction and other factors such as
neurological factors and the further studies
can be carried out by considering different
types of cerebral palsy with various other
scales and their growth pattern to find out
what oral motor dysfunction has effect on
growth.
REFERENCES
1. Bax MCO. Terminology and
classification of cerebral palsy. Dev Med
Child Neurol. 1964; 39; 295-297.
2. Chitra Sankar, Nandini Mundkar.
Cerebral Palsy- Definition, Classification,
Etiology, and Early Diagnosis. Indian J
Pediatr .2005; 72 (10) : 865-868.
3. Bell et al. A prospective, longitudinal
study of growth, nutrition and sedentary
behavior in young children with cerebral
palsy. BMC Public Health 2010, 10:176.
4. Bruce K. Shapiro, Pauline Green, Jackie
Krick, Darlene Allen, Arnold J. Capute.
Growth of severely impaired children:
neurological verse nutritional factors. Dev
Med Child Neurol.1986, 28, 729-733.
5. Kuczmarski R J, Ogdan C L et al.
Advance Data CDC Growth Chart: United
State, Number 314 December4, 2000
(Revised). U.S Department of Health and
Human Services, Centers for Disease
Control and Prevention/ National Center
for Health Statistics.
6. Incidence of malnutrition in individuals
with cerebral palsy. Available from: http.//
www.cerebralpalsysource.com/malnutritio
n/index.html
7. Okeke IB, Ojinnaka NC. Nutritional
status of children with cerebral palsy in
enugu Nigeria. European journal of
scientific research 2010; 39: 505-513.
CORRESPONDENCE
*Assistant Prof, SDM College of Physiotherapy Dharwad India. **Post graduate student,
SDM College of Physiotherapy, Dharwad India.
Effectiveness of Proprioceptive Training over Strength Training in
Improving the Balance of Cerebral Palsy Children with Impaired Balance
Kuki Bordoloi* MPT (Neuro), Nidhi Sharma** MPT (Neuro)
INTRODUCTION
Cerebral palsy is an umbrella term
encompassing a group of non-progressive
[1], non-contagious motor conditions that
cause physical disability in human
development, chiefly in the various areas
of body movement.[2] It is a non-
progressive disorder of motor function.[3]
It is caused by damage to the motor
Abstract: This is an experimental study with same subject design. Proprioceptive training and
strengthening exercises is a promising therapy to improve the balance in CP subjects with
impaired balance.The study intended to find out the effectiveness of Proprioceptive training
and strength training exercises on balance of the CP subjects and which of them is more
effective. 30 male or/and female patient of CP with impaired balance will be taken and
randomly divided in to two groups. Group A will be treated with by proprioceptive training
and group B will be treated with strength training for 12 week. Both group will assess with
Timed-Up and Go (TUG) scale and Pediatric Balance Scale (PBS) in starting and at the end of
12 weeks. The result will be statically analyzed using t-test for significance between the two
groups. After a 13-week training period, the t test and p values were found significant with
values 4.747 & 0.003 for TUG&PBS score respectively stating that there is significant effect
when using Proprioceptive training than giving strength training for improving balance in
geriatric subject with impaired balance. The result states that there is a significant effect when
using Proprioceptive Training than giving Strength Training for improving balance in the C.P.
subjects. So the proprioceptive training should be emphasized in the daily exercise regime of
C.P. subjects to improve their balance.
Key words: Balance, fall prevention, Strength training, Proprioceptive training.
control centers of the developing brain and
can occur during pregnancy, during
childbirth or after birth up to about age
three.[4] The motor disorders of cerebral
palsy are often accompanied by
disturbances of sensation, perception,
cognition, communication, and behaviour,
by epilepsy, and by secondary
musculoskeletal problems.[5] It used to
describe diverse group of disorders of
movement, posture and tone due to central
nervous system insult.[4] In developed
countries, the overall estimated prevalence
of CP is 2-2.5 cases per 1000 live births.
[34] The prevalence of CP among preterm
and very preterm infants is substantially
higher.[6]
Balance can be defined as a
complex process revolving the reception
and integration of sensory input, and the
planning and execution of movement, to
achieve a goal required in upright
posture.[7] The control of balance requires
the integration of information from
multiple sensory and motor systems by the
central nervous system (CNS).[8] Balance
receptors in the inner ear (vestibular
system) provide information to CNS about
the head and body movements.[9] The eye
(visual system) provides input regarding
the bodys orientation and motion within
the environment.[7] The position and
motion sensory of the muscle and joints,
and the touch receptors of the extremities
(proprioceptive system) send signals
regarding bodily position particularly in
relation to the supporting surface.[7]
The balance disorder of cerebral
palsy (CP) is expressed in a variety of
ways and to varying degrees in each
individual. Impairments present in children
with CP as a direct result of the brain
injury or occurring indirectly to
compensate for underlying problems
include abnormal muscle tone; weakness
and lack of fitness; limited variety of
muscle synergies; contracture and altered
biomechanics, the net result being limited
functional ability.[10] Other contributors
to the motor disorder include sensory,
cognitive and perceptual impairments.[10]
Proprioception is a sense produced
by the sensory receptors that are sensitive
to pressure in the tissues that surround
them.[11] They are also present in the
bones of the legs, arms or other parts of
the body and these receptors response to
stretches of the muscle surrounding them
and send impulse through the sensory
nerve fibers to the brain.[11] Decline in
dynamic position sense is associated with
decrease in the balance of C.P. children
and this decline in proprioception can be
prevented or improved by Proprioceptive
training.[12] In a study Edward R
Laskowski et al (1997) shown that
proprioception based rehabilitation
programs improved objectives
measurements of functional status,
independent of changes in joint laxity and
proprioception can be improved through
Proprioceptive training.[12]
Muscle strength is another factor
that plays an important role in balance and
mobility.[7] Muscle weakness can be
major problem for many young people
with cerebral palsy.[7] Training of muscle
strength and coordination has been
recommended to improve motor function.
[13] Bobath considered spasticity to be the
main problem in spastic C.P. and
suggested that resistance training should
be avoided, but Carr stated that it is not the
presence of spasticity but the negative
feature of weakness and loss of skills
which are the major barriers to improve
function. Many studies have reported
positive result in strength training in
spastic children.[14] Possible factors
interfering with normal gait pattern in
cerebral child includes spasticity, muscle
contracture, bony deformities loss of
selective motor and muscle weakness.[15]
Recent research has focused on
muscle weakness. Wiley and Damino
and Ross and Engsberg described muscle
is more pronounced distally and found
imbalance across joints. Balance control is
important for competence in the
performance of most functional skills,
helping a child to recover from unexpected
balance disturbances, either due to slips
and trips or to self induced instability
when walking a movement that brings
them towards edge of their limit of
stability.[16]
Many studies have been conducted
to show the individual effect of
Proprioceptive training and strength
training to improve the balance of C.P.
subjects. Hence this studies aims to
analyze the effectiveness of both treatment
technique and prove the better
effectiveness by comparing Proprioceptive
training and Strength training.
METHODOLOGY
Sample selection
The selection criteria are listed below.
Inclusion Criteria: CP subjects with age
group of 8-14 years, With normal I.Q.
(assessed by psychologist), Can follow
commands, Both boys and girls subjects,
CP subjects who had fall at least twice a
day, Subject who scored greater than 20
second in TUG test. Exclusion Criteria:
Children below 8 years and above 14
years, Children with any other
neurological impairment, Children with
audio visual impairment, Non ambulatory
patients.
Measurement tools
Timed up and go scale
Timed up and go scale provides a reliable
quick screening measure. Many researches
indicate that most adult can complete the
test in 10 seconds. A score of 11 to 20
seconds are considered within normal limit
for frail elderly or individual with a
disability whereas score over 20 seconds
are indicative of impaired functional
mobility. To perform this, the subject is in
sitting position and a visible object is
placed 3 meter away from the patient. The
subject is instructed to get up and walk
down till the object and return to the seat.
During this task timing is maintained with
a stopwatch and the time taken for it is
recorded. A score greater than 20 seconds
is associated with high risk in community
dwelling older adults.
Berg Balance Scale
The Pediatric Balance Scale (PBS), a
modification of Berg's Balance Scale, was
developed as a balance measure for
school-age children with mild to moderate
motor impairments.It is used to assess
balance and mobility which has 14
functional tasks commonly performed in
everyday life with scores ranging from 0-
4, with a maximum score of 56.
Procedure
Patients were selected on the assessment
and diagnosis of their condition and put on
the inclusion and exclusion criteria after
they were referred to physiotherapy
department by neurologist.
Method
The children were randomly divided in
two groups of 15 children each. All the
subjects were measured for functional
balance using Timed Up & Go Test and
Pediatric Balance Scale before start the
training period and at the end of thirteen
weeks of training.
Group A was trained with the
Proprioceptive training whereas the Group
B was trained with the Strength training.
Protocol
Strength training
All the subjects were treated with lower
extremity strengthening exercises using
weight cuff. A standardized weight of one
repetition maximum (1RM) was
considered for the subjects. 1RM was
determined before the training for all the
subjects.
A repetition of 8 to 15 times were
done for all the strengthening exercises for
duration of 30 minutes per session; with 5
minutes rest period in between for five
days a week and were continued for 13
weeks.
The following exercises were then
given and it was ensured that the position
of subjects in all form of exercises were
comfortable.
1. Side leg rising
Subjects were made to lie in side lying
position and instructed to abduct the upper
leg tied with weight cuffs slightly about 6-
12 inches. This position was held for
sometime and then the leg was lowered.
Same exercise was repeated with the other
leg.
2. Knee flexion exercise
Subjects were made to sit on high chair or
table, the knee was bent slowly as far as
possible, so that the foot with the weight
cuff was bent behind. The subject was
asked to hold the position and then the foot
was lowered slowly all the way back
down. The same procedure was repeated
with the other leg.
3. Hip Extension Exercise
Subjects were made to lie on prone
position and one leg with weight cuff was
lifted slowly straight upwards. The subject
was asked to hold the position and then the
leg was lowered. The same procedure was
repeated with the other leg.
4. Knee Extension Exercise
Sitting on the chair with back support, the
subject was asked to rest the balls of the
feet & toes on the floor. The hands were
kept on the thigh or on the side of the
chair, and then the right leg with the
weight cuff was extended slowly in front,
parallel to the floor for a period of 3
seconds. With right leg in that position, the
foot was flexed so that the toes were
pointing towards head; the foot was held in
that position for 1-2 seconds. Duration of 3
seconds was taken to lower the leg back to
the starting position, so that the balls of the
foot rested on the floor again. The same
procedure was repeated with the other leg.
5. Ankle Dorsiflexion
Sitting on the chair with back support, the
subject was asked to lift the foot tied with
a weight cuff so that the toes were pointing
towards the head. Then the subject was
asked to hold and slowly return to the
original position. The same procedure was
repeated with the other leg.
Proprioceptive Training
Subjects in Group A were given proper
warm up for 5-10 minutes before starting
the treatment in the form of simple
stretching (Quadriceps and hamstring
stretch) and free exercises (knee flexion
and extension in side lying and high
sitting).
[63]
All the proprioceptive exercises
were performed for duration of 30 minutes
per session; with 5 minutes rest period in
between for three days a week and were
continued for 13 weeks.
The Proprioceptive training included the
following exercises
1. Stair climbing up and down (a
regular 3 steps staircase).
2. Standing with feet approximately
shoulder-width apart and arms
extended out slightly forward
lower than the shoulder, then
lifting both heel off the floor and to
hold the position for 10 seconds,
followed by climbing regular steps
staircase. This procedure was
performed with eyes closed also.
3. Standing with feet side by side &
holding the arms in same position
as described above, one foot is
placed on the inside of the
opposing ankle and to hold the
position for 10 seconds. Followed
by climbing regular steps staircase.
This procedure was performed with
eyes closed also.
4. To perform one leg standing with
one foot raised to the back and to
maintain the position for minimum
3 seconds. This procedure was
performed with eyes closed also.
5. Same exercise as above performed
but with one foot raised to the
front. This procedure was then
performed with eyes closed.
6. Walking heel to toes.
7. Rising from a standard chair (4
times) without arm support.
Data analysis
Data analysis was performed using
the Statistical Package for the Social
Sciences (SPSS) for windows version 17
(SPSS Inc., Chicago, U.S.A.). The data
were analyzed using parametric
(dependentt test and independentt test)
and nonparametric (Wilcoxon Signed
Ranks and Mann-Whitney Test) test to
find the significance of the interventions
used within and between the group A and
B. The significant level set for this study
was 95% (p<0.05).
RESULTS & INTERPRETATION
Thirty Cerebral Palsy patients were
part of the study. Both the groups (A and
B) included 15 patients each, with 11 male
and 4 females in group A and 12 male and
3 females in group B. Age group taken
was between 8-14 yrs with mean age of
12.33 yrs (SD=1.85). In Group A, 15
subjects with an average age of 12.4 yrs
(SD=1.96) and in Group B, 15 subjects
with an average age of 12.1 yrs (SD=1.79) completed the study.
Table 1.1: Comparison of Gender of patients in both groups
Male Female
Group A 11 4
Group B 12 3
Total 23 7
Table 1.2: Comparison of Mean and SD of Age of Patients in both groups
Mean SD
Group
A
Male 12.8 1.25
Female 11.3 3.20
Group
B
Male 11.8 1.80
Female 13 1.73
Total
Group
A
12.4 1.96
Group
B
12.1 1.79
Table 1.3 Descriptive statistics of TUG Tests prior to and post study
Mean N
Std.
Deviatio
n
TUGAPR 23.667 15 1.799
TUGAPS 19.933 15 1.534
TUGBPR 23.333 15 1.676
TUGBPS 21.000 15 1.414
Table 1.4 Descriptive statistics of PBS Tests prior to and post study
Mean N
Std.
Deviatio
n
PBSAP
R
42.1 15 1.792
PBSAP
S
47.3 15 2.086
PBSBP
R
43.1 15 1.685
PBSBP
S
45.9 15 1.995
Interpretation
The table 1.1 states that total 30 patients
including 7 females were kept in two
groups A and B. The group A included 11
males and 4 females whereas the group B
included 12 males and 3 females. Stating
that the mean age of total patients was 12.4
in group A and 12.1 in group B the table
1.2 shows the mean age of male and
female in group A and the male and
female in group B as 12.8, 11.3, 11.8, and
13 respectively. The table 1.3 shows the
pre and post test means values for TUG
test It clearly shows that individually both
Proprioceptive training and Strength
training produced improvement in
Cerebral palsy patients with respect to
TUG test but the improvement in the A
which had had the Proprioceptive training
showed more improvement. This is again
confirmed with the findings of PBS test in
table 1.4 which states that although both
the groups showed improvement, the
group A had better findings than group B.
.Timed Up and Go Test:
Table 2.1 Dependent t test performed with the pre & post values of TUG test for
significance within the groups
Within Group
Paired Differences
T Df P
95% Confidence
Interval of the
Difference`
Mean SD
Std.
Error
Mean
Lower Upper
TUGAPre
TUGAPost
3.73333 .88372 .22817 3.24395 4.22272 16.362 14 0.003
*
TUG B Pre
TUG B Post
2.33333 .72375 .18687 1.93254 2.73413 12.486 14 0.002
*
*-Significant
Table 2.2: Independent t test performed with the pre & post values of TUG test for
significance between the groups
Independent Samples Test
Between Group
Levene's
Test for
Equality of
Variances
t-test for Equality of Means
95%
Confidence
Interval of the
Difference
F Sig. T Df P
Mean
Diff.
Std.
Error
Diff.
Lower Upper
TUG
A-
TUG
B
Equal
variances
assumed
.429 .518 4.747 28 0.003
*
1.4000 .29493 .79586 2.004
*-Significant
Interpretation
The table 2.1 shows that the value of t as
16.362 and 12.486 for TUG Test in Group
A and Group B respectively in dependent
t test. The t value is significant at
p<0.5. Graph 4 representing the mean
values of Pre and Post values of Timed Up
& Go test show improvement within the
group A and B respectively. Hence
individually both Proprioceptive training
and Strength training produced significant
improvement in Cerebral palsy patients
within their group with respect to TUG
test.
The table 2.2 shows that the value
of t as 4.747 in independent t test. The
value of t is greater even at p<0.05,
which is significant. Hence there was
significant difference in improvement
between Proprioceptive training and
Strength training in Cerebral Palsy
patients with respect to TUG test.
Pediatric Balance Scale test:
Table 3.1: Wilcoxon Signed Ranks Test
Within Group
PBSAPR -
PBSAPS
PBSBPR
PBSBPS
Z -3.442 -3.432
P 0.002
*
0.002
*
*-Significant
Table 3.2: Mann-Whitney Test
*-Significant
Table 3.3: Mann-Whitney and Wilicoxon test performed with the pre & post values of
PBS test for significance between the group
Between Group PBS
Mann-Whitney U 15.500
Wilcoxon W 135.500
Z -4.083
P 0.003
*
*-Significant
Interpretation:
The table 3.1 shows that the value of p
as 0.002 for Group A and Group B
when compared within the group
respectively. Graph 5 representing the
mean values of Pre and Post values of
PBS show improvement within the
group A and B respectively. Thus there
is significant improvement on PBS in
Cerebral palsy patients after
Proprioceptive training and Strength
training within their group respectively.
GRO
UP
N
Mean
Rank
Sum of
Ranks
PBS
A 15 21.97 329.50
B 15 9.03 135.50
Total 30
The table 3.3 shows that the value
of p as 0.003 and hence significant.
Hence we can state that there was
significant difference in improvement
between Proprioceptive training and
Strength training in Cerebral Palsy
patients with respect to PBS test.
Table 4.1 Mean of improvement in all the parameters between group a & Group B
Parameters
Group
A
Group
B
TUG 3.73 2.33
PBS 5.19 2.73
Interpretation:
The above table 4.1 and the graph 6,
clearly indicates that the Proprioceptive
training produced more improvement in
the selected parameters (TUG, PBS)
when compared with Strength training in
Cerebral palsy patients.
Graph 1: Comparison of both the groups and the total on the basis of gender of Patients
Graph 2: Comparison of Mean and SD of Age of Patients between both groups and
total.
Graph 3: Comparison of Mean and SD of pre study values of both groups
Graph 4: Comparison of Mean and SD of Pre and Post values of Timed Up & Go test
Graph 5: Comparison of Mean and SD of Pre and Post values of Pediatric Balance
Scale
Graph 6: Comparison of Mean of Improvement in all the parameters between
Group A and Group B.
DISCUSSION:
In this study, better improvements in
balance outcome were analyzed using
proprioceptive training and strength
training. This study was done on 30 CP
children with impaired balance who were
divided in to experimental Group-A
treated with Proprioceptive training and
Group-B with Strength training.
The balance was taken as the
dependant variable which was measured
using Timed Up & Go test (TUG) and
Pediatric Balance Scale (PBS). Both this
tool are standard tools to analyze balance.
Proprioceptive training exercises were
given to improve the balance by improving
the decreased sense of proprioception in
older age group where as Strength training
was given to improve the balance by
improving the strength of lower extremity
muscles.
The improvements in functional
balance due to Proprioceptive training may
be attributed to the improvement of
mechanoreceptor activation. Structural
changes in the muscle, bone and joints
during old age accounts for the decreased
efficiency of the proprioceptors.
Researchers reason that proprioceptive
training can improve the joint and
kinesthetic sensation to a greater extent
that the falls and risk of fall can be reduced
among the subjects.
Edward R Laskowski et al also
stated that the decline in dynamic position
sense is associated with decrease in the
balance of C.P. children and this decline in
proprioception can be prevented or
improved by Proprioceptive training.My
study confirms the study by Edward R
Laskowski et al (1997) which showed that
proprioception based rehabilitation
programs improved objectives
measurements of functional status,
independent of changes in joint laxity and
proprioception can be improved through
proprioceptive training.
[68]
These results were in accord with
Gauchard GC et al (1999) to improve
balance by proprioceptive training. Studies
done by Pierre Gangloff et al (2003) also
supports our results, which prove that
proprioceptive training exercises, improve
balance in subjects with impaired balance.
This supports the experimental hypothesis
hence the null hypothesis was rejected.
The result of the present study
indicates that effect of proprioceptive
training had a proven effect over strength
training. All participants in the
proprioceptive training group declared that
their balance had improved and most of
them were motivated to continue with the
training. Hence proprioceptive training
should be emphasized in the daily exercise
regime of CP subjects to improve their mobility and functional status.
REFERENCES:
1. Cerebral Palsy. National Center on
Birth Defects and Developmental
Disabilities, October 3, 2002
2. Beukelman, David R.; Mirenda
(1999). Augmentative and
Alternative Communication:
Management of severe
communication disorders in
children and adults. Pat (2 ed.).
Baltimore: Paul H Brookes
Publishing Co. pp. 246249.
3. Davis DW. Review of cerebral
palsy, part I: Description,
incidence, and etiology. Neoratel
Netw 1997; 16(3): 7-12.
4. Cerebral Palsy Topic
Overview.
http://children.webmd.com/tc/cereb
ral-palsy-topic-overview. Retrieved
2008-02-06.
5. Anonymus (2007). Definition and
classification of cerebral palsy, Feb
2007. Developmental medicine
and child neurology 49 (8): 8.
6. Vincer MJ, Allen AC, Joseph KS,
et al. Increasing prevalence of
cerebral palsy among very preterm
infants: a population-based
study. Pediatrics. Dec 2006;118(6):
e1621-6.
7. Darcy A Umphred. Neurological
Rehabilitation. Mosby
Publications. Fourth edition. 2001.
8. Balance Procedures Manual,
National Health and Nutrition
Examination Survey, Inhanes, May
2001
9. Textbook of Medical Physiology.
Arthur C. Guyton, John E. Hall.
10th Edition. ISBN: 0721602401
10. Margaret J. Mayston. People With
Cerebral Palsy: Effects of and
Perspectives for Therapy. Neural
Plasticity. Volume 8, No. 1-2, 2001
11. Vestibular Disorders Association.
Official Website. Retriebed on
10/6/2011
12. Edward R.Laskowski, MD; Karen
newcomer-Aney, MD; Jaysmith,
MD.Refining rehabilitation
withproprioceptive training:
expecting return to play; The
physician and sports medicine;
1997 Oct;Vol.25, No. 10.
13. C Andersson et al. Adults with
cerebral palsy: walking ability after
progressive strength training.
segunda-feira, 10 de maio de 2010
14. Kramer JF, MacPhail HEA.
Relationships among measures of
walking efciency, gross motor
ability, and isokinetic strength in
adolescents with cerebral palsy.
Pediatr Phys Ther 1994; 6:3 /8.
15. Phil Page.Knee osteoarthritis:
strength training for pain relief and
functional improvement; ICAA
Publication, Vol.1 No.6, September
2003.
16. Mutch LW, Alberman E, Hagberg B,
Kodama K, Velickovic MV. (1992).
Cerebral palsy epidemiology: where
are we now and where are we going?
Developmental Medicine and Child
Neurology 34: 547-555.
CORRESPONDENCE:
*Neuro-Physiotherapist, GNRC, Guwahati, Assam. Email: kukzzmail@gmail.com Cont:
+91-8822485959. **HOD, Dept of Physiotherapy, AIER, Ghaziabad, U.P., India
Correlation of Balance Tests Scores with Modified Physical Performance
Test in Indian Community-Dwelling Older Adults
Sunita Yadav* MPT (Neuro), Deepti Dhar** MPT (Paediatrics)
INTRODUCTION
Abstract: Background and Objective: There is sufficient evidence which shows significant
relationship between balance tests and other functional tests but there is lack of literature
regarding the relationship between balance tests (BBS, MDRT, BPOMA) and Modified
Physical Performance Test in different age groups of older adults. Design: An Observational
Study Subjects: 58 subjects were divided into three different age groups, having the mean age
of 65.33.0 (Group-A), 73.72.4 (Group-B), 82.61.4 (Group-C), mean height of 161.45.6
(Group-A), 164.910.2 (Group-B), 160.35.9 (Group-C) & mean weight of 68.44.8 (Group-
A), 72.76.9 (Group-B), 63.67.7 (Group-C) were recruited in this study from old age home
and local community. Methods: Subjects in each group performed the tests in the following
sequence: BBS (Berg Balance Scale), MDRT (Multi-Directional Reach Test), Modified-PPT
(Physical Performance Test) & BPOMA (Balance Performance-Oriented Mobility Assessment
of Tinetti) with rest period of 5-10 minutes between each scale. Result: The results suggested
that there was a significant positive correlation between balance tests and Modified Physical
Performance Test in different age groups of older adults. Conclusion: The current study
concluded that Modified physical performance test is a efficient tool to assess static and
dynamic balance and also physical function and ambulation in different age groups of older
adults. It was also observed that out of these balance tests used in the study, MDRT was the
most difficult to understand and perform by subjects above 70 years and the subjects above 80
years found it really hard to understand the procedure.
Keywords: BBS, MDRT, BPOMA, Modified PPT, Balance, Physical Function.
The number of persons above the
age of 60 years is fast growing, especially
in India. India is the second most populous
country in the world has 76.6 million
people at or over the age of 60,
constituting above 7.7% of total
population. Recurrent falls are an
important cause of morbidity and mortality
in the elderly and are a marker of poor
physical and cognitive status.
2
Impaired balance and physical
function are the main causes of fall among
the older adults. Stability and orientation
are to distinct goals of the postural control
system. Postural control for stability and
orientation requires both perception and
action. Thus, postural control requires the
complex interaction of neural and
musculoskeletal systems.
4
Several researchers show that as
the age increases, the changes in the neural
and musculoskeletal systems disturb the
balance and physical activities.
6
As age
increases the physical activities and
physical function also decreases due to
decreased muscular power and strength.
11
Both balance problems and physical
inactivity affect the quality of life of older
adults. Therefore the assessment of both
balance and physical function is necessary
for older adults in order to help establish
appropriate treatment goals, increase
awareness of fall risk and assign
appropriate assistive device and to
decrease the disability. Several such
instrument have shown satisfactory
reliability and validity in identifying older
people with balance and physical
functional problems, discriminating older
adults by their needs for different assistive
device to maintain balance or predicting
their likelihood of falls and to enhance
physical function.
The Berg Balance Scale was
developed by Kathy Berg (a Canadian
physical therapist) in1993, as a means of
measuring balance in the elderly.
Multi-directional Reach Test
(MDRT) is developed by Roberta A.
Newton in 2001. It allows for analysis of
the patient voluntary postural control.
The Performance Oriented
Mobility Assessment (POMA) scale was
originally developed by Dr. Mary E.
Tinetti and first published in 1986, is a
widely used tool for assessing mobility
and fall risk in older people. In this study
balance subscale of Tinetti assessment is
used to assess the balance of older adults.
15
Brown, M, Sinacore, D.R.
developed the modified physical
performance test in 2005 to provide more
focus on gross motor function by
substituting a chair rise task and a balance
task for the writing and stimulated eating
tasks described in the original PPT. The
tool was more useful in identifying deficits
in physical function than the self- report
comparison measure, the functional status
questionnaire. The authors concluded that
the performance based measure could
assist in early identification of minor
problems in physical functioning, and
allow for opportunity for early intervention
for the patients.
16
Several researchers found that
balancing exercises improve physical
function and previous studies also found
significant correlation between balance
scales and other functional tests.
17,18,13,19
Therefore it is clear that there is a
relationship between balance and physical
function.
Yet there is no study to show
relationship between these scales or tests
in different age groups. Therefore the main
purpose of my study is to find out the
relationship between balance tests and
Modified physical performance test.
Second purpose is, the Modified physical
performance test assesses both balance and
physical function in older adults no other
tool is required because it measure the
both static and dynamic balance and also
physical function. It tells about fall risk,
need of assistance device and functional
limitations; additionally it takes less time
to administer as compared to other scale.
METHODOLOGY
This observational study recruited
58 subjects from old age homes and local
community of Delhi and Dehradun
meeting the inclusion criteria. Inclusion
Criteria: Age - 60 to 89 year old healthy
subjects; Gender- Both male and female;
Ability to abduct and flex the shoulder up
to 90 degrees; Ability to stand for
minimum 10 min. without any assistance;
Ability to walk at least 50 feet before
sitting to rest; Minimal use of rail or cane
while climbing. Exclusion Criteria: Use
of any assistive prosthetic device; History
of any cardiac problem confirmed by
physician; Any history of fainting spells or
extended dizziness due to unknown
reasons History of neurological; vestibular
or auditory deficit confirmed by physician;
History of any visual disorder which will
not be corrected by optical glasses as
confirmed by physician; MMSE score
below 23; History of postural hypotension;
History of recent fractures and severe
arthritic conditions; History of any major
surgeries during last 6 month; History of
any previous balance training; Moderate to
severe hypertensions
Measurement Tools
Berg Balance Scale (BBS)
The BBS was developed to measure
balance among older people with
impairment in balance function by
assessing the performance of 14 functional
tasks. The results are based on how long it
takes to complete specific tasks and how
well the tasks are performed. Each task is
measured on a five point ordinal scale
ranging from 0 to 4 (0 = unable to
perform, 4 = independent) so that the
aggregate score ranges from 0 to 56.
Multidirectional Reach Test (MDRT)
The MDRT is an inexpensive, reliable and
valid screening tool to measure the limits
of postural stability in four directions
(forward, backward, right & left) during
standing. The distance of each reach is
measured in centimetres or inches.
Balance Performance Oriented Mobility
Assessment (BPOMA)
The Tinetti assessment is a physical task-
oriented scale which measures the gait and
balance activities of older adults. In this
study BPOMA was used to assess the
balance of the community dwelling older
adults; it consists 9 tasks. 6 tasks are
measured on a three point ordinal scale
ranging from 0 to 2 and remaining three
tasks are measured on a two point ordinal
scale ranging from 0 to 1 ( 0 = unable to
perform, 1 & 2 = independent). The
maximum score is 16.
Physical Performance Test (Modified-
PPT)
An objective evaluation of overall physical
function was obtained by using modified
PPT. The severity of physical frailty in
physical functioning was assessed using a
modified PPT. It consists of 9 tasks; each
task is measured on a five point ordinal
scale ranging from 0 to 4 ( 0 = unable to
perform, 4 = independent) except 7th task
(turning 360 degrees) which ranges from 0
to 1 (0 = unsteady, 1 = steady). The
maximum score is 36.
Procedure
The subjects were recruited based on
inclusion and exclusion criteria the
subjects of different age groups 60 to 69
years of age (Group- A), 70 to 79 years of
age (Group- B), and 80 to 89 years of age
(Group- C). Subjects in each group
performed the tests in a sequence i.e. BBS,
MDRT, Modified-PPT, POMA. The
whole procedure was explained to each
subject and the subject signed a consent
form before performing the study.
Description data was collected which
included age, gender, height, weight and
number of falls in the past 6 months.
MMSE score was also assessed. All
subjects were assessed by all four scales or
tests in the following order BBS, MDRT,
Modified-PPT and BPOMA. All
components of each scale were
demonstrated to all the subjects and one
practice session was done for all the
components of four scales by all the
subjects, after that reading was taken. Each
test or scale was administered by myself.
All subjects were offered rest breaks and
water during the session and completed the
approximately 60 minute testing protocol
without complaint of fatigue or
discomfort. The resting period of 5 to 10
minute was given after performing each
scale. As a precautionary measure, blood
pressure was checked prior to beginning of
the test session and it was again taken at
the end of the last test performed. One
person was always nearby vicinity of the
subject.
Data Analysis
The data analysis was done on SPSS 11.5
software. The arithmetical mean and
standard deviation of age, height and
weight in demographic data were
evaluated. Karl pearsons correlation test
was done to analyse the correlation
between balance tests (BBS, MDRT &
POMA) with physical performance test
(modified) among elderly people.
Statistical significance level was set at <
0.05. The data analysis was done on SPSS
11.5 software. The arithmetical mean and
standard deviation of age, height and
weight in demographic data were
evaluated. Karl pearsons correlation test
was done to analyse the correlation
between balance tests (BBS, MDRT &
POMA) with physical performance test
(modified) among elderly people.
Statistical significance level was set at <
0.05.
RESULT AND INTERPRETATION
A sample of 58 subjects were selected on
the basis of inclusion and exclusion
criteria. Each group of older adults had 20
subjects except Group C (81-89 years of
age) which has only 18 subjects due to
unavailability of the subjects. The mean
and standard deviation of age weight and
height of three Groups A, B and C [Table
1] was calculated. The mean and standard
deviation of balance tests and physical
performance test (modified) of Group A
[Table 2], Group B [Table 3], & Group
C [Table 4], was calculated. The
correlation values of balance tests with
modified physical performance test of
Group A [Table 5], Group B [Table 6],
& Group C [Table 7], were calculated.
Karl pearsons correlation test was used to
find out the correlation between BBS,
MDRT & BPOMA with PPT (modified) in
different age groups of older adults, Group
A (60 69 years of age), Group B (70
79 years of age), and Group C (80 - 89
years of age); these three groups showed
significant positive correlation between
balance tests (BBS, MDRT & BPOMA)
with physical performance test (modified).
Table 1: Mean and standard deviation of
demographic data
Group A
N Mean
Age 20 65.33.0
Height 20 161.45.6
Weight 20 68.44.8
Group B
N Mean
Age 20 73.72.4
Height 20 164.910.2
Weight 20 72.76.9
Group C
N Mean
Age 20 82.61.4
Height 20 160.35.9
Weight 20 63.67.7
Table 1 shows mean and standard
deviation of demographic data of different
age groups. Group (60 69 years of
age), Group B (70 79 years of age) &
Group C ( 80 89 years of age).
Table 2: (Group A) Mean and standard deviation (SD) of balance tests (BBS, MDRT &
BPOMA) and Physical Performance Test (Modified).
Tests N Mean and SD
BBS 20 542.4
FR (MDRT) 20 13.62.6
BR (MDRT) 20 11.82.6
RR (MDRT) 20 12.52.5
LR (MDRT) 20 12.23.0
BPOMA 20 14.91.9
PPT (modified) 20 31.12.5
Table 2 shows mean and standard deviation of balance tests and modified physical
performance test of Group-A (60-69 Years of age).
Table 3: (Group B) Mean and standard deviation (SD) of balance tests (BBS, MDRT &
BPOMA) and Physical Performance Test (Modified).
Tests N Mean and SD
BBS 20 27.75.3
FR (MDRT) 20 12.03.4
BR (MDRT) 20 9.93.9
RR (MDRT) 20 11.23.3
LR (MDRT) 20 11.44.3
BPOMA 20 12.92.2
PPT (Modified) 20 27.75.3
Table 3 shows mean and standard deviation of balance tests and physical performance test
(modified) of Group-A (70-79 Years of age).
Table 4: (Group C) Mean and standard deviation (SD) of balance tests (BBS, MDRT &
BPOMA) and Physical Performance Test (Modified).
Tests N Mean and SD
BBS 20 42.63.6
FR (MDRT) 20 5.52.2
BR (MDRT) 20 3.21.9
RR (MDRT) 20 4.92.3
LR (MDRT) 20 4.42.2
BPOMA 20 10.51.4
PPT (modified) 20 18.03.5
Table 4 shows mean and standard deviation of balance tests and Modified physical
performance test of Group A (80-89 Years of age).
Figure 1: Mean and standard deviation of balance tests (BBS, MDRT, & BPOMA) with
modified physical performance test (modified) of Group A, B and C.
Table 5: (Group A) Correlations of balance tests (BBS, MDRT, & POMA) with Physical
Performance Test (Modified)
Balance Tests r value P value
BBS Vs PPT (modified) .759 .000
FR( MDRT) Vs PPT (modified) .592 .006
BR (MDRT) Vs PPT (modified) .671 .001
RR (MDRT) Vs PPT (modified) .541 .014
LR (MDRT) Vs PPT (modified) .518 .019
BPOMA Vs PPT (modified) .826 .000
Table 5 shows correlation of balance tests with physical performance test (modified), all the
balance tests show significant correlation except right and left reaches which show
moderately significant correlations with physical performance test (modified) of Group A
(60 69 years of age).
Figure 2: Correlation Graph of Berg
Balance Scale (BBS) and Physical
Performance Test (Modified) of Group
A.
Figure 2 depicts correlation between BBS
and modified PPT. It shows positive
significant correlation in 60-69 years of
age group i.e. Group A.
Figure 3: Correlation Graph Of Forward
Reach (FR) of MDRT and Physical
Performance Test (Modified) Of Group
A.
Figure 3 depicts correlation between FR of
MDRT and PPT (modified). It shows
positive significant correlation in 60-69
years of age group i.e. Group A.
Figure 4: Correlation Graph of Backward
Reach (BR) of MDRT and Physical
Performance Test (Modified) Of Group
A.
Figure 4 depicts correlation between BR of
MDRT and PPT (modified). It shows
positive significant correlation in 60-69
years of age group i.e. Group A.
Figure 5: Correlation Graph of Right
Reach (RR) of MDRT and Physical
Performance Test (Modified) of Group -
A.
Figure 5 depicts correlation between RR of
MDRT and PPT (modified). It shows
positive significant correlation in 60-69
years of age group i.e. Group A.
Figure 6: Correlation Graph Of Lateral
Reach (LR) of MDRT and Physical
Performance Test (Modified) of Group
A.
Figure 6 depicts correlation between LR of
MDRT and PPT (modified). It shows
positive significant correlation in 60-69
years of age group i.e. Group A.
Figure 7: Correlation Graph of Balance
Performance Oriented Mobility
Assessment (BPOMA) with Physical
Performance Test (Modified) of Group
A.
Figure 7 depicts correlation between
BPOMA and Modified PPT (modified). It
shows positive significant correlation in
60-69 years of age group i.e. Group A.
Table 6: Correlations of balance tests (BBS, MDRT, & BPOMA) with Physical Performance
Test (modified) of Group - B.
Balance Tests r value P value
BBS Vs PPT (modified) .944 < .01
FR( MDRT) Vs PPT (modified) .874 < .01
BR (MDRT) Vs PPT (modified) .893 < .01
RR (MDRT) Vs PPT (modified) .826 < .01
LR (MDRT) Vs PPT (modified) .710 < .01
BPOMA Vs PPT (modified) .856 < .01
Table 6 shows significant correlation between balance tests (BBS, MDRT & BPOMA) and
modified physical performance test in older adults [Group B (70 79 years of age)].
Figure 8: Correlation graph of Berg
Balance Test (BBS) with Physical
Performance Test (Modified) Of Group
B.
Figure 8 depicts correlation between BBS
and PPT (modified). It shows positive
significant correlation in 70-79 years of
age group i.e. Group B.
Figure 9: Correlation graph of Forward
Reach of MDRT with Physical
Performance Test (Modified) of Group -
B.
Figure 9 depicts correlation between FR of
MDRT and PPT (modified). It shows
positive significant correlation in 70-79
years of age group i.e. Group B.
Figure 10: Correlation graph of Backward
Reach (BR) of MDRT with Physical
Performance Test (Modified) Of Group
B.
Figure 10 depicts correlation between BR
of MDRT and PPT (modified). It shows
positive significant correlation in 70-79
years of age group i.e. Group B.
Figure 11: Correlation graph of Right
Reach (RR) of MDRT with Physical
Performance Test (Modified) of Group -
B.
Figure 11 depicts correlation between RR
of MDRT and PPT (modified). It shows
positive significant correlation in 70-79
years of age group i.e. Group B.
Figure 12: Correlation graph of Left
Reach (LR) of MDRT with Physical
Performance Test (Modified) Of Group -
B.
Figure 12 depicts correlation between LR
of MDRT and PPT (modified). It shows
positive significant correlation in 70-79
years of age group i.e. Group B.
Figure 13: Correlation graph of Balance
Performance Oriented Mobility
Assessment (BPOMA) with Physical
Performance Test (Modified) Of Group -
B.
Figure 13 depicts correlation between
POMA and PPT (modified). It shows
positive significant correlation in 71-79
years of age group i.e. Group B
Table 7: Correlations of balance tests (BBS, MDRT, & BPOMA) with Physical Performance
Test (Modified) Group-C.
Balance Tests r value P value
BBS Vs PPT (modified) .789 < .01
FR( MDRT) Vs PPT (modified) .822 < .01
BR (MDRT) Vs PPT (modified) .852 < .01
RR (MDRT) Vs PPT (modified) .770 < .01
LR (MDRT) Vs PPT (modified) .752 < .01
B POMA Vs PPT (modified) .651 < .01
Table 7: also shows significant correlation between balance tests ( BBS, MDRT & BPOMA)
and physical performance test (modified) in older adults [Group C ( 80 89 years of age)].
Figure 14: Correlation graph of Berg
Balance Scale (BBS) with Physical
Performance Test (Modified ) Of Group -
C.
Figure 14 depicts correlation between BBS
and PPT (modified). It shows positive
significant correlation in 81-89 years of
age group i.e. Group C.
Figure 15: Correlation graph Of Forward
Reach (FR) of MDRT with Physical
Performance Test (Modified) Of Group -
C.
Figure 15 depicts correlation between FR
of MDRT and PPT (modified). It shows
positive significant correlation in 81-89
years of age group i.e. Group C.
Figure 16: Correlation graph of Backward
Reach (BR) of MDRT with Physical
Performance Test (Modified) of Group -
C.
Figure 16 depicts correlation between BR
of MDRT and PPT. It shows positive
significant correlation in 81-89 years of
age group i.e. Group C.
Figure 17: Correlation graph of Right
Reach (RR) of MDRT with Physical
Performance Test (Modified) of Group -
C.
Figure 17 depicts correlation between RR
of MDRT and PPT (modified). It shows
positive significant correlation in 81-89
years of age group i.e. Group C.
Figure 18: Correlation graph of Left
Reach (LR) of MDRT with Physical
Performance Test (Modified) of Group
C.
Figure 18 depicts correlation between LR
of MDRT and PPT (modified). It shows
positive significant correlation in 81-89
years of age group i.e. Group C.
Figure 19: Correlation graph of Balance
Performance Oriented Mobility
Assessment (BPOMA) with Physical
Performance Test (Modified) of Group
C.
Figure 19 depicts correlation between
BPOMA and PPT (modified). It shows
positive significant correlation in 81-89
years of age group i.e. Group C.
DISCUSSION
Assessing balance and physical
abilities as they relate to falls in older
adults is complex due to many social and
health related issues that may be involved.
The geriatric population above 80 years
adults presents a more complicated
situation due to a sedentary life style, a
lower level of function, and the dynamics
of their physical and emotional
environments. Any one or combination of
these factors may lead to a falls at any time
because the level of the older adults
performance may not meet the demands of
the environment or task at hand. The need
to reduce this functional decline is an
important health care issue. It is important
to identify those factors that contribute to
the functional decline. Balance instability
and physical inactivity in older adults
contribute to this decline in ADLs
(activities of daily living). Therefore,
effective balance and functional
assessments are needed to document
balance and functional abilities and in this
segment of the older adult population. This
information is critical to the design of all
prevention/reduction programs and to
maintain or improve the quality of life for
these individuals.
25
The BBS, MDRT, & BPOMA have
documented validity and reliability to
assess balance abilities. As well as
physical performance test (modified) has
also documented validity and reliability to
assess functional abilities in community
dwelling older adults. Previous researchers
found significant relationship between
balance scales (BBS, MDRT & BPOMA)
with other functional performance tests;
Barthel mobility subscale, Time up and go
Test and Physical Performance Test
respectively
13, 25, 26
. But there is little to no
documentation of relationship between
three balance scales with PPT (modified).
Thus this study was done to find out the
relationship of these three balance scales
with physical performance test (modified).
The clinical trial studied the correlation
between balance tests (BBS, MDRT, &
BPOMA) and physical performance test
(modified) among elderly people who
were divided into three age categories.
Berg Balance Scale (BBS)
The last two items of the Berg Balance
Test are considered the most difficult to
perform. These tasks are: item no. 13 & 14
(stand with feet in tandem for 30 seconds,
stand on one leg respectively), One study
found that item numbers 12, 13, & 14 are
the most difficult tasks to perform,
25
but in
the current study only 6 subjects (Group B
& C) found difficulty to perform the 12th
task. All the subjects got grade 4 for the
1st, 2nd, 3rd, & 4th components of the
BBS. Not one subject reached up to 25cm
for the 8th component (Reaching forward
with outstretched arm while standing) of
the BBS.
In the current study the mean values (54,
49 & 42, as shown in tables 2, 3 & 4) of
BBS in different age groups are lower
from the findings (55,55; 53,52; & 52,48
for male and female respectively) of one
study in 3 age groups (60-69, 70-79, &
80+ years).
34
This difference may be due
to age difference. They have given the
average mean of age (69); they did not
mention the mean value of age for
individual groups so the subjects of the
this study may be slightly younger than
my study; in this study the mean values for
females in each age group have lower than
males and in the current study the scores
of the tests for the females also lower and
the number of female subjects are more
than males so it could be the reason for
lowest values. Another study found mean
values of BBS in fallers (36.5) and
nonfallers (35.7) older adults;
25
these
values are very low as compared to the
current study. The reasons could be one
that the mean age of this study population
is 838.8 years which shows very older
subjects. Secondly they examined
community dwelling older adults who
were home bound and have a neurological
or musculoskeletal diagnosis that may
disturb the balance and contribute to falls .
In another study the mean value of BBS is
48.6 and the mean age of this study is
74.1 7.9 years which is approximately
similar to Group-B of the current study.
The mean value of BBS of the current
study is 49.65 which is slightly more, the
reason could be the age difference because
the mean age of the Group-B is 73.70
2.4 which shows that the subjects were
mostly between 71 to 75 years and the
subjects of the above said study were
mostly between 68 to 81 years, so this
could be the reason for the lowest value of
BBS among 254 community-dwelling
older adults.
13
A study done by Patricia S. Smith found
significant relationship between BBS and
forward reach in post acute stroke patients
(r = 0.78).27 The BBS has also been
shown to correlate with both the Tinetti
mobility index (r = 0.91) and the get up &
go test (r = - 0.76).
28
A correlation greater
than 0.70 between total BBS and total
Fugl-Mayer-Scale (FMS) scores have been
reported in older adults.
18
The above
studies shows correlations between BBS
and other functional tests. This current
study also shows significant correlation
between BBS and physical performance
test (modified), [r = 0.759, P = <0.01
(Group - A); r = 0.944, P = <0.01 (Group -
B); ); r = 0.789, P = <0.01 (Group - C); as
shown in tables 5, 6, 7 & figures 2, 8, and
14 respectively]. The reason of significant
correlation between BBS and physical
performance test (modified) could be one
that the five components are similar
between BBS and PPT (modified) and
secondly both BBS and PPT (modified)
assess static and dynamic balance and also
physical activity.
Multi-directional Reach Test (MDRT)
In MDRT backward reach is the most
difficult task to perform because most of
the subjects of the Group-C used to take a
step behind while performing this reach.
MDRT is considered the more time taking
test and most difficult to understand by the
subjects because the mostly older adults
use the spine not the ankle for the reaches.
This current study shows there is a
significant relationship between
components (FR, BR, RR & LR) of
MDRT and physical performance test
(modified) in older adults of different age
groups. It also indicates that there is a
relationship between age and height with
performance on the lateral reach test.
These results similar to the study who
reported that, similar to functional reach
performance is positively correlated with
height and negatively correlated with
age.
22
The four heighted persons were
present in the current study, the values of
all the components of MDRT were greater
to these heighted persons as compared to
other subjects. Mean scores on
performance of the functional and lateral
reach tests in the present study are lower
than mean scores reported elsewhere.
13,29,
30
In a sample of 14 community dwelling
elderly females (age, 70-87 years), a study
reported a mean functional reach of
26.78.9cm.30 In another research, with a
larger sample of 254 elderly community-
dwelling adults (mean age = 74.17.9
years), It was reported a mean forward,
backward, right and left reach tests scores
of 22.68.6cm, 11.57.8cm,17.57.6 &
16.87.4cm respectively.
13
Yet another
study reported mean left and right lateral
reach test scores of 21.02.5cm and
20.00.5cm respectively, from 60 healthy
females over the age of 65 (mean age =
72.55.0 years).
29
In each of the above
mentioned studies scores were defined as
the mean multiple trials which may reflect
score inflation due to learning over
multiple trials. In contrast, scores in
present study were recorded from a single
trial. Additionally, subjects used the ankle
movements rather than spine movements
which reflects the negative correlation
between age and ankle muscle strength,
sensation and ability to generate large
amounts of force at the ankle joint.
31
One of studies in past have revealed that
MDRT demonstrated significant inverse
relationships with scores on the time up &
go test (TUG): [FR (r = -0.442) BR (r = -
0.333), RR (r = - 0.260), LR (r = - 0.310)
which is a functional performance test.
13
Similarly current study showed significant
correlation between MDRT and modified
physical performance test which is again a
functional performance test with high
validity and reliability. Hence it can be
said that MDRT also shows good
correlation with different functional
performance tests.
Tinetti Balance Subscale
During the performance of this test, the
subjects did not find any difficulty with
any of the tasks in the balance of
performance-oriented mobility assessment
(BPOMA) of Tinetti.
One study found a mean among the
community dwelling older women with no
health problems on the balance subset of
12.61.7 (mean age = 74.76.0 years),
32
which is similar to mean value (12.92.1,
as shown in table- 3) of Group-B of the
current study (mean age = 73.72.4 years,
as shown in table- 1). Another study found
mean value of 132.9 among females
(mean age = 83.87.7 years),
33
which is
more as compared to mean value
(10.51.4, as shown in table- 4 ) of Group-
C of the current study, in fact mean age
was similar (82.61.3 years, as shown in
table- 1 ). The subjects for Group-C were
all above 80 and physical frailty
component was more among the subjects
of the current study while in the above said
study where mean value was 83.87.7
years, many subjects less than may 80
years. Hence the balance scores were
better for them.
Physical Performance Test (Modified-
PPT)
In modified physical performance test, the
Ist & 2nd tasks were considered the most
difficult task to perform by the subjects
mainly for the Groups B & C. Seven
subjects were using the assistive devices
for the 8th & 9th components (climb one
flight of stairs and climb stairs) of the
physical performance test (modified) and
four subjects climbed the stairs by holding
the one sided railing.
In one study it was found that the mean
value of the PPT (modified) score among
27 frail obese older volunteers after
treatment was 29.42.2 and for control
group it was 29.82.0.34 Mean age was
71.15.1for treatment group which
matched the current age of Group B but
the mean value is lower i.e. 27.65.2 as
shown in table- 3, this difference is may be
due to age because in my study the mean
age for the Group - B is 73.72.4, which
shows that the subjects were slightly older
which reflects the negative correlation
between age and physical function.
35
The
mean age of group-A of current study is
65.23.0 which is slightly younger than
the control group (694.6) of the above
study, therefore the mean value for this
group of my study is more and second
reason could be that the subjects were
obese which also reflects the negative
correlation between obesity and physical
function.
35
Another study found the mean values of
physical performance test (modified) in
community dwelling older adults. The
mean values of three groups [obese
elderly, nonobese frail, and nonobese
nonfrail] were 34.40.5, 29.30.7 and
27.80.8 respectively.
15
The second group
of above study matched with Group - B of
the current study in respect similar age,
weight and condition but the mean value
of physical performance test (modified) is
more than the current study, the reason
could be that the subjects of my study may
be more frail and reason could be the
larger number of female subject in the
current study compared to this study, there
both genders were in equal proportion
while in the current study out of 20
subjects 16 were female. It has been well
established that in females balance
component is affected due to larger body
mass in the upper segment the of body.
The age is an important factor that affects
both balance and physical function of
older adults. Declines in standing balance
have been attributed to sensory,
musculoskeletal and cognitive changes,
typically in some combination as multiple
systems fall below minimal functional
thresholds.
36
The results of the balance
tests and physical performance test
(modified) are different in different age
groups of older adults, which proved that
the disturbance in balance and physical
function also differ in severity (mild,
moderate and severe for group A, B & C
respectively) among different age groups
of older adults. Thus assessment and
treatment also differ to provide effective
evaluation and treatment in different age
groups. Additionally safety measures are
necessary for the Group C (80-89 years
of age) in the assessment and treatment
also to prevent fall.
CONCLUSION
There is a significant relationship between
balance tests and physical performance test
(modified) and physical performance test
(modified) is an efficient tool to assess
static and dynamic balance and also
physical function and ambulation in
different age groups of older adults. It was
also observed that out of the these balance
tests used in the study, MDRT was the
most difficult to understand and perform
for people above 70 years and subjects
above 80 years found it really hard to
understand the procedure. According to
this test the subject was supposed to
perform movement at the ankle joint but
more of trunkal mobility was seen in
people above 80 years while performing
this test. Hence it can be said that MDRT
is not a very feasible test for cheeking
balance in subjects above 80 years.
Clinical significance
As the Indian population over the age of
60 years continues to grow, there will be
rise in the level of functional disability and
prolonging health. It is therefore
imperative that appropriate screening
methods are developed to identify
community dwelling elderly individuals
with functional impairment who should be
referred for a detailed physical therapy
evaluation. As we have seen that PPT
(modified) incorporates all important
entities of balance and function hence,
simply administering modified physical
performance testing can well define the
functional level as well as the balance
issues in an elderly person rather than
giving other tests which are time taking,
separately for balance and functional
performance.
Limitations
In the present study, the sample size was
small. The sample size of age Group C
(81-89 years of age) was relatively smaller
as compared to other groups. Gait subscale
of performance oriented mobility
assessment is not included in this study.
Future Research
Future study can be done with larger
sample size to see the results. Future
research is needed to find out the
reliability and validity of modified
physical performance test with balance
scales (PPT, MDRT & BPOMA) in
elderly. In my study the value of the left
lateral reach is more than right lateral
reach for the heighted person. Future study
can be done to identify that why this
difference has come and this difference is
significant or not.
REFERENCES
1. Alexander Kalache, Bruno
Lunenfold. Health and men ageing.
2001. Available from: www.
Who_nmh_nph_01.2.pdf.
2. Dr. B. Krishnaswamy, Dr.
Gnanasambandam Usha. Falls in
older people: National/Regional
review of India. Available from:
http://
www.who.int/ageing/projects/SEA
RO
3. Christopher M. Fredericks.
Pathophysiology of the motor
systems: principles and clinical
presentations. F.A. Davis company.
Philadelphia: Jean-Francois Vilain;
1996. p. 284.
4. Ann Shumway-cookjorie H.,
Morjorie H.woollacott. Motor
control theory and practical
applications. 2nd ed. Lippincott
Williams and Wilkins: 2001. p.
164-165, 181-182, 222-238.
5. Kathryn H. Schmitz, Ann R.
Cappola. The interaction of cancer
and aging: Estallishing the need for
breast cancer rehabilitation. J
Cancer epidemiol biomarkers prev.
2007;16(5):866-72.
6. Jan Janseen, sleven B. Heymsfield,
Robert Ross. Low relative skeletal
muscle mass (sarcopenia) in older
persons is associated with
functional impairment and physical
disability. J American geriatrics
society. 2002;50(5):889-896.
7. David clark, carolynnpattern,
Kieran F. Reid, Robert J,
Carobello, Edward M. Phillips,
Roger A. Feilding. Impaired
voluntary neuromuscular activation
limits muscle power in mobility
limited older adults. J Gerontology.
2010;495-502.
8. Keith smith. Sensory changes:
Senior series. Available from:
http:// www. Goldenbuckeye.com,
http://senior series.osu.edu.
9. Marjorie H. Woolacott, Ann
Shumway. Cook, Lewis M.,
Nashner. Ageing and posture
control: changes in sensory
organization and muscular
coordination. The international J of
ageing and human development.
1986;23(2):97-114.
10. H.J.J.(cojanne) kars, B. Eng., Juha
M., Hijmans, Jann H.B. Geertzen,
Wiebren Zijlsta. The effect of
reduced somatosensation on
standing balance: A systematic
review. J Diabetes Sci Technal.
2009 July; 3(4): 931-943.
11. Siobhan M White, Thomas R
Wojcicki, Edward mcauley.
Physical activity and quality of life
in community dwelling older
adults. J Biomed central ltd.
2009;7:10.
12. Lusardi, M.M. Functional
performance in community living
older adults. J Geriatric Phys Ther.
2004;26(3):14-22.
13. Roberta A. Newton. Validity of
multidirectional reach test: a
practical measure for limits of
stability in older adults. J
Gerontology medical sciences.
56A(4);M248-M252.
14. Clinimetric properties of the
performance oriented mobility
assessment. J Phys Ther 2006 July
1.
15. Kathryn D. Mitchell, Roberta A.
Newton. Performance-oriented
mobility assessment (POMA)
balance scale indicates need for
assistive device. 2006;1(3):183-
189.
16. Dennis T. Villareal, Marian banks,
Catheraian Siener, David R. Sina
Core, Samuel Klein. Physical
frailty and body composition in
obese elderly men and women. J
Obesity A Research J.
2004;12:913-920.
17. Angela Conrad Wooton. An
integrative review of Tai Chi
research: An alternative form of
physical activity to improve
balance and prevent falls in older
adults. J Orthopaedic Nursing.
2010 April; 29(2): 108-116.
18. Matsuda, Patricia Noritake,
Shumway-Cook,Anne, Ciol,
Moseia A. The effects of a home-
based exercise program on physical
function in frail older adults. J of
geriatric Phys Ther. 2010 April-
june;33(2): 78-84.
19. Homjet Tal-Hatu Kolapo, Fashoyin
Oyinlola Funmilayo. Balance
retraining in post stroke patients
using a simple, effective and
affordable technique reduction De
L equilibre aprs un accident
vasculaire cerebral grace a une
technique simple, efficace et
accessible. J American
neurological sciences. 2007; 26(2).
20. Ganvir SD. Assessment of
functional capacity in elderly
population by elderly mobility
scale in wardha. Indian academy of
geriatrics. 2008;4:89-97.
21. Tm steffen, LA Mollinger. Age-
gender related test performance in
community-dwelling adults. J of
neurological Phys Ther.
2005;29(4):181-188.
22. Patricia S Smith, Judith A
Hombree, Mary E Thompson. Berg
balance scale and functional reach:
determining the best clinical tool
for individuals post acute stroke. J
Clinical rehablilitation.
2004;18(7):811-818.
23. Berg K, Wood-Dauphinu S,
Williams J, Gayton D. Measuring
balance in the elderly: preliminary
development of an instrument. J
Phys Ther association. 2001 sept
10.
24. Jennifer S Brach, Jessie M
Vanswearingen, Anne B Newman,
Andrea M Kriska. Identifying early
decline of physical function in
community-dwelling older womem
: performance-based and self report
measures. J American Phys Ther
Association. 2001 Sept 10.
25. Teresa Steffen, Megan Seney.
Test-retest reliability and minimal
detectable change on balance and
ambulation tests, the 36-item short
form health survey and the unified
Parkinson disease rating scale in
people with parkinsonism. J Phys
Ther. 2008 june;88(16):733-746.
26. Mary Thompson, Ann Medley.
Forward and lateral sitting
functional reach in younger,
middle-aged and older adults. J of
geriatric Phys Ther. 30(2):07.
27. Hui-Fen Mao, Fing Hsueh, Fei-
Fang Tang, Ching-Fan Sheu.
Analysis and comparison of the
psychometric properties of three
balance measures for stroke
patients. J American Heart
Association. 2002;33:1022.
28. Sabrina E., Trader, Roberta A.
Newton, RonitaL., Cromwell.
Balance abilities of homebound
older adults classified as fallers and
nonfallers. J of geriatric Phys Ther.
26(3):03.
29. Duncan PW, Weiner DK, Chandler
J, Studenskis S. Functional reach: a
new clinical measure of balance. J
Gerontol Med Sd. 1990;45:M192-
M197.
30. DeWaard B, Bentrup B, Hollman J,
Brasseur J. Relationship of the
functional reach and lateral reach
tests in elderly females. J Geriatr
Phys Ther. 2002; 25:4-9
31. Sadashiv Ram Aggarwal, Deepak
kumar. Lower extremity muscle
strength and balance performance
in Indian community-dwelling
elderly men aged 50 years and
above. Indian J of Phys Ther and
occupational therapy. 2007;1(2).
32. Chiara Mecagni, Janet Pullin
Smith, Kay E Roberts, Susan B O
Sullivan. Balance and ankle range
of motion in community-dwelling
aged 64 to 87 years : A
correlational study. J of American
Phys Ther Association. 2000 May
30;
33. Dennist , Villareal, Marian Banks,
David R, Sinacare, Catherine
Siener, Sarmuel Klein. Effect of
weight loss and exercise on frailty
in obese older adults. Arch Intern
Med. 2006;166:860-866.
34. Karen W, Hayes, Marjorie E.
Johnson. Measures of adult general
performance tests. Arthritis care
and research. 2003 Oct
15;49(55):S28-S42.
35. Marc Bonnefoy, Tomasz Kostka,
Marie C. Patricol, Sophic E,
Bethouze, Brono Mathian et al.
Physical activity and
dehydroepiandrosterone sulphate,
insulin-like growth 1 and
testosterone in healthy active
elderly people. J Ageing oxford
journals. 1998;27:745-751.
36. Dr. Sandra Brauer, Y Voner Burns,
Prudence Galley. Lateral reach: a
clinical measure of medio-lateral
postural stability. J Phys Ther Res
Int. 1990;4:81-88
CORRESPONDENCE
*Student, Dolphin Institute, Dehradun affiliated to H.N.B Garhwal University, Uttarakhand,
India Mob: 08882590557. **Lecturer, Dolphin Institute, Uttarakhand. India
Electrical Muscle Stimulation (EMS) Improve Functional Independence in
Critically Ill Patients
Dharam Pani Pandey PT*, Dr. Uday Shankar Sharma**,Dr. Ram Babu***
Abstract: Objective. This study was designed to investigate the effects of
electrical muscle stimulation (EMS) on strength of muscle groups stimulated and
improvement in functional independence in critically ill patients .Methods. 134
subjects were recruited among the patient admitted in multidisciplinary intensive
care units and randomly divided in to control and EMS group. Patients unable to
understand or speak English and or Hindi due to language barrier or cognitive
impairment prior to admission, unable to transfer from bed to chair at baseline
prior to hospital admission, Patient with known history of primary systemic
neuromuscular disease were excluded from study. Results. EMS group patients
achieved higher MRC scores than controls in knee extensors and ankle
dorsiflexors. Independence level was higher in EMS group Conclusions. EMS
application constitutes a promising means of muscle strength preservation and
early mobilization which can directly reflects the gain in functional independence
post ICU discharge in critically ill patients.
Key words: Electrical muscle stimulation, muscle strength, CIPNM, CIM,
functional independence
INTRODUCTION
Weakness that is acquired during
hospitalization for critical illness is
increasingly recognized as common and
important clinical problem. Weakness
acquired in the intensive care unit (ICU)
and related acquired neuromuscular
dysfunction occur in a large percentage of
critically ill patients
13
and are associated
with increased morbidity and mortality.
4,5
Critical illness polyneuromyopathy
(CIPNM) is an acquired neuromuscular
disorder observed in survivors of acute
critical illness. It is characterized by
profound muscle weakness and
diminished or absent deep tendon
reflexes
1
and is associated with delayed
weaning from mechanical ventilation
2
suggesting a possible relation between
limb and respiratory neuromuscular
involvement. In addition, the syndrome is
associated with prolonged hospitalization
and increased mortality.
3
The diagnosis of
CIPNM requires a reliable bedside muscle
strength examination and depends on
patient's cooperation and maximal effort.
4
Several risk factors have been identified
including systemic inflammatory response
and sepsis
5
, medications such as
corticosteroids
6
and neuromuscular
blocking agents
7
, inadequate glycemic
control
8
, protracted immobility
4
,
hypoalbuminemia
9
, Gram-negative
bacteremia
9
and severity of organ
dysfunction.
10
Thus, looking for the
potentially reversible risk factors and
subsequent adjustment of therapy are so
far advocated as preventive measures to
decrease the risk of CIPNM.
A very few of studies available suggesting
the treatment and prevention of critical
illness myopathy these includes intensive
insulin therapy, optimal gycemic control
and minimized use of neuromuscular
blocking agents, high dose and prolong
use of corticosteroids.
OBJECTIVE OF THE STUDY
The objective of this study is to
investigate whether electrical muscle
stimulation (EMS) will improve
functional independence in critically ill
patients.
Our experimental Hypothesis was that
EMS would beneficially affect muscle
functional status and will improve
functional independence in critically ill
patients.
MATERIAL AND METHODS
Subjects:
The 134 subjects were recruited among
the patient admitted in multidisciplinary
intensive care units during the study
period.
Exclusion criteria:
Unable to understand or speak English
and or Hindi due to language barrier or
cognitive impairment prior to admission,
unable to independently transfer from bed
to chair at baseline prior to hospital
admission (based on detail history taken
from caregivers. Patient with known
history of primary systemic
neuromuscular disease, vascular events,
organ transplant, intracranial process that
is associated with localizing weakness,
transferred from another ICU after >2
consecutive days of mechanical
ventilation, amputation of lower
extremities, any limitation of life support,
pregnancy, age under 18 years, obesity,
technical obstacles that did not allow the
implementation of EMS such as bone
fractures, skin lesions and, end-stage
malignancy were excluded from our study
Design of study:
The study employed a randomized single
blind controlled experimental study design
consisting of two group experimental
group and control group, Subjects were
randomly assigned ether to experimental
group or to control group everyday the
ICU patient admission register were
observed and with in 24 hour the
assessment were done , each time when a
patient met the criteria for inclusion a
random number were picked up between 1
to 10 using sealed envelope method if it
were an odd number than the subject were
assigned to experimental group similarly
if it even number were obtained the
subjects were assigned to control group.
Intervention:
EMS was implemented on knee
extensors, tibialis anterior and of both
lower extremities. Patients received daily
sessions. After skin cleaning, rectangular
electrodes (90 50 mm) were placed on
motor point of targeted muscle. The
stimulator (Unistim, HMS medical
system) delivered biphasic, symmetric
impulses of 50 Hz, 100 sec pulse
duration, 12 seconds at intensities able to
cause visible contractions. The duration of
the session was 30 minutes each muscle
group. EMS sessions were continued until
ICU discharge, both group were getting
routine physiotherapy included the passive
movements, active assisted movements
and chest physiotherapy.
Outcome Measures:
Primary Outcome Measures were the
score of barthel index, it is reliable and
valid outcome measure used to assess
functional independence.
Secondary Outcome Measures were lower
extremity strength, at ICU discharge, of 2
bilateral muscle groups which were
stimulated measured by MMT using a
composite Medical Research Council
(MRC) score.
DATA ANALYSIS AND RESULTS
All continuous variables were presented
by mean. The statistical significance of P
value was set at 0.05. One-way repeated
measures analysis of variance (ANOVA)
was made to compare MRC Grading and
barthel index score between-group. Two
hundred and thirty-eight patients were
admitted to our multidisciplinary ICU
during the eight-month study period and
104 patients fulfilled the exclusion criteria
or stayed in the ICU less than 48 hours.
The study population consisted of 134
patients of which of these patients, 70
were randomly assigned to the EMS group
and 64 to the control group. 6 patients
from EMS group and 1 patient from
control died or were discharged from the
ICU before the second measurement.
MRC muscle grading score of muscle
group being stimulated were for left knee
extensors were control group mean 3.49
and EMS group mean 3.91 (p = 0.0187),
right knee extensors control group mean
3.69 and EMS group mean 3.87 (p =
0.0387). left ankle dorsiflexors control
group mean 3.78 and EMS group mean
3.91 (p = 0.04), right ankle dorsiflexors
were observed as follows mean control
group mean 3.37 and EMS group mean
3.3.46 (p = 0.0587) found.
Barthel index score of control group was
(mean) 68.6 and EMS group (mean) 71.9
and found significant between groups (p =
0.010).
Graph 1: Showing the mean and
significance level of two group of left and
right knee extensor.
Graph 2: Showing the mean and
significance level of two group of left and
right ankle dorsiflexors.
Graph 3: Showing the mean and
significance level functional independence
level as assessed on barthel index.
DISCUSSION
The main finding of our randomized
controlled study is that EMS of lower
extremities seems to preserve the muscle
strength of critically ill patients as
assessed with MRC muscle strength
grading system. EMS of lower extremities
applied to critically ill patients upon
admission is associated with a lesser
degree of muscle strength loss of these
patients as assessed with MRC muscle
strength grading system. barthel index
score were higher in EMS group and the
patient of EMS group were more
independent.
Electrical stimulation has been used to
increase strength and endurance in
partially and fully paralyzed muscle. It has
been used for peroneal nerve stimulation
10,
11
the restoration of shoulder movement
12
,
recovery of tendonesis grip
13
, and in the
use of an upper arm prosthesis.
14
Electrical muscle stimulation (EMS) has
been used as an alternative to active
exercise in patients with chronic heart
failure (CHF)
15
and chronic obstructive
pulmonary disease (COPD).
16, 17
Many of
these patients, even those who are
clinically unstable, experience severe
dyspnea on exertion, which can prohibit
the regular application of conventional
exercise training, considered necessary for
an integrated therapeutic approach. In a
recent systematic review, EMS
implementation in most of the selected
controlled clinical trials produced
significant improvements in muscle
strength, exercise capacity and disease-
specific health status.
18
Recently, an study
identified an acute systemic effect exerted
by EMS on peripheral microcirculation of
critically ill patients.
19
Specifically, after
performing a 45-minute session of EMS
on the lower extremities, an improvement
in the microcirculation of the thenar
muscle as assessed by near infrared
spectroscopy technique was observed.
EMS, as a possible substitute to aerobic
and resistance exercise training in severe
CHF and COPD patients, has been shown
to improve muscle performance, aerobic
exercise capacity, and disease-specific
health status.
9-11
CONCLUSIONS
EMS exercise induces beneficial effects in
muscle strength of ICU patients. These
effects mainly concern muscle groups
directly stimulated, but there is also
evidence of effects in muscle groups not
stimulated. EMS application constitutes a
promising means of muscle strength
preservation and early mobilization which
can directly reflects the gain in functional
independence post ICU discharge in
critically ill patients.
Clinical relevance & limitation
EMS is an alternative method of exercise
causing minimal discomfort to patients
who are not able to perform any form of
physical exercise, as is often the case in
critically ill patients. It is a limitation of
this study that it did not evaluated the
follow up stage and upper extremities
function. Further studies are needed to
explore the possible role of EMS as a tool
for preserving the muscle strength and
gain in functional independence post ICU
discharge with longer follow up
evaluation, the muscle properties and
preventing CIPNM in critically ill patients
and to define which patients would benefit
most from this intervention.
REFERENCES:
1. De Jonghe B, Sharshar T,
Lefaucheur JP, Authier FJ,
Durand-Zaleski I, Boussarsar M, et
al; Groupe de Reflexion et dEtude
des Neuromyopathies en
Reanimation. Paresis acquired in
the intensive care unit: a
prospective multicenter study.
JAMA 2002;288(22):28592867.
2. De Letter MA, Schmitz PI, Visser
LH, Verheul FA, Schellens RL,
Op de Coul DA, van der Meche
FG. Risk factors for the
development of polyneuropathy
and myopathy in critically ill
patients. Crit Care Med
2001;29(12):22812286.
3. Coakley JH, Nagendran K,
Yarwood GD, Honavar M, Hinds
CJ. Patterns of neurophysiological
abnormality in prolonged critical
illness. Intensive Care Med
1998;24(8):801807.
4. Garnacho-Montero J, Madrazo-
Osuna J, Garcia-Garmendia JL,
Ortiz- Leyba C, Jimenez-Jimenez
FJ, Barrero-Almodovar A, et al.
Critical illness polyneuropathy:
risk factors and clinical
consequences: a cohort study in
septic patients. Intensive Care Med
2001;27(8): 12881296.
5. Spitzer AR, Giancarlo T, Maher
L, Awerbuch G, Bowles A.
Neuromuscular causes of
prolonged ventilator dependency.
Muscle Nerve 1992;15(6):682
686.
6. Rudis MI, Guslits BJ, Peterson
EL, Hathaway SJ, Angus E, Beis
S, Zarowitz BJ. Economic impact
of prolonged motor weakness
complicating neuromuscular
blockade in the intensive care unit.
Crit Care Med 1996;24(10):1749
1756.
7. Latronico N, Peli E, Botteri M.
Critical illness myopathy and
neuropathy. Curr Opin Crit Care
2005;11(2):126132.
8. Bednarik J, Lukas Z, Vondracek
P. Critical illness
polyneuromyopathy: the
electrophysiological components
of a complex entity. Intensive Care
Med 2003;29(9):15051514.
9. Van den Berghe G, Wouters P,
Weekers F, Verwaest C,
Bruyninckx F, Schetz M, et al.
Intensive insulin therapy in the
critically ill patients. N Engl J Med
2001;345(19):13591367.
10. Tennila A, Salmi T, Pettila V,
Roine RO, Varpula T, Takkunen
O. Early signs of critical illness
polyneuropathy in ICU patients
with systemic inflammatory
response syndrome or sepsis.
Intensive Care Med
2000;26(9):13601363.
11. Rabuel C, Renaud E, Brealey D,
Ratajczak P, Damy T, Alves A, et
al. Human septic myopathy:
induction of cyclooxygenase,
heme oxygenase and activation of
the ubiquitin proteolytic pathway.
Anesthesiology 2004;101(3):583
590.
12. MacFarlane IA, Rosenthal FD.
Severe myopathy after status
asthmaticus (letter). Lancet
1977;2(8038):615.
13. Witt NJ, Zochodne DW, Bolton
CF, GrandMaison F, Wells G,
Young GB, Sibbald WJ. Peripheral
nerve function in sepsis and
multiple organ failure. Chest
1991;99(1):176184.
14. Knox AJ, Mascie-Taylor BH,
Muers MF. Acute hydrocortisone
myopathy in acute severe asthma.
Thorax 1986;41(5):411412.
15. Hund E, Genzwurker H, Bohrer
H, Jakob H, Thiele R, Hacke W.
Predominant involvement of motor
fibres in patients with critical
illness polyneuropathy. Br J
Anaesth 1997;78(3):274278.
16. Thiele RI, Jakob H, Hund E,
Tantzky S, Keller S, Kamler M, et
al. Sepsis and catecholamine
support are the major risk factors
for critical illness polyneuropathy
after open heart surgery. Thorac
Cardiovasc Surg 2000;48(3):145
150.
17. Garnacho-MonteroJ, Amaya-
Villar R, Garcia-Garmendia
JL,Madrazo- Osuna J, Ortiz-Leyba
C. Effect of critical illness
polyneuropathy on the withdrawal
from mechanical ventilation and
the length of stay in septic patients.
Crit Care Med 2005;33(2):349
354.
18. Bolton CF. Sepsis and the
systemic inflammatory response
syndrome: neuromuscular
manifestations. Crit Care Med
1996;24(8): 14081416.
ACKNOWLEDGMENT:
We would like also to acknowledge the support of all intensive care unit staff, consultants
and all the patients caregivers.
CORRESPONDENCE:
*Department Of Physiotherapy & Rehabilitation,BLK Super Speciality Hospital, Pusa Road,
New Delhi, India. **Sr. Consultant Neurologist, Department of Neurology, Jaipur Golden
Hospital,2 institutional area, sector 3, Rohini, New Delhi, India. ***Sr. Consultant Physician,
Department of Internal, Medicine, Jaipur Golden Hospital,2 institutional area, sector 3,
Rohini, New Delhi, India.
Paraplegia with Sacral Pressure ulcer treated by Ultrasound therapy- A
Single Case Report
Shanmuga Raju P. MPT *, Ramalingam P. MS, FICA, MAMS
Abstract: Pressure ulcers are important and common complications after
paraplegia. The use of therapeutic ultrasound as an adjunct to wound healing has
gained interest in recent years. An twenty five year old male reported with a two
months history of a grade two, non healing, sacral pressure ulcer. Ultrasound
therapy (UST) is simple, safe, without side effects, bedside procedure, inexpensive
with positive wound healing results for difficult to treat non healing pressure sore.
I hope that this article will encourage other wound care specialists to engage in
further research in this area.
Key Words: Paraplegia, Sacral pressure ulcer; Continuous mode of ultrasound
therapy; wound healing.
INTRODUCTION
Pressure Ulcer, also called as Decubitus
ulcers, was first seriously studied by
Jean- Martin Charcot, a clinician in the
19th Century (1-3). Pressure ulcer is a
serious health issue, very painful, a
significant physiological challenge, can
shorten the life of patient, an emotional
and financial burden to the patient.
Pressure sore are important and common
complications after paraplegia. An
estimated 50 80% of individuals
suffering from spinal cord injury develop
pressure ulcer at least once in their life
time (9). Pressure ulcer are treated by
using wound dressings, relieving pressure
on the wound, Water beds/ Alpha bed by
treating concurrent conditions which may
delay healing and by the use of physical
therapy such as electrical stimulation, laser
therapy and ultrasound (1).
Ultrasound is now the most frequently
used electrophysical agent worldwide,
used at least daily for patient treatment by
the majority of physiotherapists (4-5).The
aim of this study to investigate the effect
of ultrasound (US) therapy in sacral
pressure ulcer with paraplegia. Limited
clinical research is available and no
consensus exists regarding the efficacy of
ultrasound for treating pressure ulcer,
particularly full thickness pressure ulcers.
CASE REPORT
A twenty five year old man presented with
a two months history of a grade two, non
healing sacral pressure ulcer. He was a
former. He had history of fall from height.
His past medical history, complete
paralysis of both lower limbs, loss of
sensation, urinary and bladder
incontinence, loss of mobility and sacral
pressure ulcer for past one month. His
medical problems included spinal cord
injury and severe depression. He had
become unable to walk since two months
and was carried either in bed or in his
wheelchair. He was diagnosed as a case of
D11, and D12 wedge compression of spine
with traumatic paraplegia (American
spinal cord injury association impairment
score: A- no motor or sensory function in
the sacral segments) and sacral pressure
ulcer. Five month back, he underwent
placement of spinal fixation rods and
plates from D11 to L1 level. A thoraco
Lumbar-sacral corset was fabricated for
him. Routine hematology and
biochemistry investigations were within
normal limits. He received antibiotics and
vitamin supplements. He was referred to
department of physical medicine and
rehabilitation OPD, CAIMS, Karimnagar
on February 26th, 2011.
On physical examination, he is bed ridden
and was unable to sit without support in
the chair, had sustained the sacral pressure
ulcer. He has bedsore of 6.2 X 4.0 cm, the
depth ranging from 10mm, grade II sacrum
ulcer with necrotic slough according to
European pressure ulcer Advisory panel
(EPUAP) wound classification system
(Figure.1). His albumin count 2.4 g/dL,
haemoglobin 11.0 g/dL, temperature was
38 degree Celsius. There was no evidence
of osteomyelitis. He was put on
conservative treatment, consisting of water
bed mattress, bed postioning, regular
pressure relief, daily saline water dressing
and appropriate antibiotics.
OUTCOMES EVALUATED
Wound measurements and digital
photographs of wound beds were obtained
weekly. Wound dimension monitored and
depth measurements were obtained using a
sterile, cotton-tip applicator and ruler
(Steven JK et al, 2007). Wound surface
area was determined using Bates-Jenes
wound assessment tool.
ULTRASOUND THERAPY
INTERVENTION
On February 2011, Continuous mode of
ultrasound therapy (Electroson 709,
Chennai) treatment was performed in
sacral pressure ulcer region. The
following protocols are applied: ultrasound
machine with frequency of 3 MHz and
spatial average intensity 0.8 w/cm2 sound
head, in conjunction with a coupling media
of aquasonic ultrasound transmission gel
was used. Ultrasound was applied to the
outer surface, and edge of sacral ulcer
region (Fig. 2). Before the treatment of
CUS therapy, we splashed each wound by
oxygen spray. Sacrum ulcer was cleaned
using 2% hydrogen peroxide. The standard
normal saline (Nacl) dressing was done.
Ultrasound treatment time was 10 minutes
per session 6 days a week, for six weeks.
At the end of third week there was marked
improvement in pressure ulcer i.e size,
floor and wound margin reduced. There
was no pus discharge after treatment (Fig.
3). A healthy granulation tissue was noted
(Fig. 4). The patient made good progress
and wound was completely healed within
42 days (Fig. 5).
Table: 1 Parameter of Ultrasound
therapy treatment (McDiarmid etal, 1985)
Ultrasound frequency: 3 MHz
Spatial average temporal peak
intensity: 0.8 W/cm2
Pulse duration: 2 ms
Duty factor: 0.2
Spatial temporal average radiating
surface area: 5.2 cm2
Duration of treatment: 10 minutes
per session for sacral pressure ulcer
Duration of treatment: 6 weeks
RESULT
The indolent pressure ulcer, apart from
routine therapy, continuous mode
ultrasound therapy enhanced the healing of
pressure ulcer in six weeks.
Fig: 1 On assessment, the sacral pressure
ulcer presented as non- healing grade II
pressure ulcer measuring 6.2 x 4.0 cm with
erythema.
Fig: 2 the full thickness of sacral ulcer was
treated with continuous mode ultrasound
therapy (CUST)
Fig: 3 three weeks after the treatment of
CUST
Fig: 4 Fifth weeks after CUST, the wound
size are decreased for sacral ulcer
Fig: 5 After six week of treatment, picture
showing that sacral pressure ulcer are
completely healed.
DISCUSSION
The purpose of the study was to assess the
effect of ultrasound therapy in healing of
sacrum pressure ulcer in patients with
paraplegia. Infected sores heal more
slowly than clean sores while no effect of
ultrasound clean sores were observed
ultrasound therapy appeared to improve
the rate of healing of infected sores. It is
non thermal effect produced by ultrasound
that are most significant in the stimulation
of tissue repair (Dyson, 1976). Paul et al
(1960) ultrasound was effective in
relieving congestion, cleansing necrotic
areas and promoting healing with healthy,
non-adherent skin approaching normal
thickness. Cyclic vibration effect of
ultrasound might induced a form of micro
massage which by reducing edema, might
facilitate repair, their requires further
investigations. It is also stimulate protein
synthesis infact ultrasound initiates two
processess which results in release of
energy tissue: Surface cavitation (creation
and dissipation of tiny bubbles in the
tissues) and acoustic microstreaming that
is movement of fluids along acoustic
boundaries, such as cell membrane. This
biophysical effect that are non-thermal
alternations in cellular protein synthesis
and release, blood flow and vascular
permeability, angiogenesis, and collagen
content and alignment by various workers
it as quoted as follows: 1. General protein
and collagen synthesis by fibroplasts
(Harvey etal, 1975, Webster etal. 1980). 2.
Fibroplast mobility (Miller etal, 1978). 3.
Fibroblast ultrastructure (Dyson and Pond,
1970). 4. Permeability of fibroblast
membrane (Harvey etal, 1975). 5.
Lysosomal fragilty (Tayor and Pond,
1972). 6. Tensile strength and elasticity of
scar tissue (Dyson et al, 1979). 7.
Modification of contraction in skin
wounds (Dyson et al, 1981).
With this parameters of ultrasound
treatment (frequency 3 MHz, Intensity 0.8
W/cm2, Pulse duration 2 ms, Duty cycle
0.2, effective radiating surface area 5.2
cm2, Duration of treatment 10 minute
per/session, Duration of frequency 6
weeks) pressure ulcer healed in time
without side effects. Our case study
showed that continuous mode of
ultrasound therapy treatment enhances
healing of sacral pressure ulcer. This case
study confirmed that continuous UST has
a positive effect on pressure ulcer with
paraplegia (Fig.5). No complications were
observed with application of the
continuous ultrasound. Further studies are
needed to evaluate the efficacy of
ultrasound therapy in pressure ulcers in
spinal cord injury in a large number of
patients.
CONCLUSION
Continuous mode of ultrasound therapy
was effective in the treatment of patient
with grade II pressure ulcer in young
paraplegic patient. Ultrasound therapy
treatment of pressure ulcer is less
expensive, more comfortable and can
enhance wound healing process without
side effects and complication.
REFERENCES:
1. Sella EJ, Barrette C. Staging of
charcot neuro arthropathy along the
medial column of the foot in the
diabetic patient. J. Foot Ankle
Surg. 1999, 38; 34-40.
2. Levine JM. Historical perspective
on pressure ulcers: The decubitus
ominosus of Jean- Martin Charcot.
J Am. Geriatr. Soci, 2005, 53;
1248- 1251.
3. Levine JM. Historical perspective:
The neuropathic theory of skin
ulceration. J. Am.Geriatr.Soci,
1992; 40, 1281.
4. Goh AC, Chock B, Wong WP et al.
Therapeutic ultrasound rate of
usage, knowledge of use, and
opinions on dosimetry. Physiother
Singapore 1999; 2: 69-83.
5. Chipchase LS, Trinkle D.
Therapeutic Ultrasound: Clinician
usage and perception of efficacy.
HongKong Physio Ther J. 2003;
21: 5-13.
6. Ali Akbari S, Flemming K, Cullum
NA, Wollina U. Therapeutic
Ultrasound for pressure ulcers,
(2009). The Cohrane collaboration,
John wiley and Son ltd, p:1-18.
7. Paul BJ, Lafratta CW, Dawson AR
etal. Use of ultrasound in the
treatment of pressure sores in
patients with spinal injury. Arch
phys Med Rehabil, 1960; 41; 438-
440.
8. Callam MJ, Dale Jj, Harpel DR,
etal. A controlled trial weekly
ultrasound therapy in chronic leg
ulceration, Lancet. 1987; ii; 204-
206.
9. Saad A, Williams A. Effect of
therapeutic ultrasound on the
activity of the mononuclear
phagocyte system in vivo.
Ultrasound Med Biol, 1986; 12;
145-150.
10. Steven JK, David AL, Andrea JB,
Jenny LM, Julie AB, Karen LA.
Expedited wound healing with
Non-contact, Low frequency
ultrasound therapy in chronic
wounds: A retrospective analysis.
Adv. Skin and wound care, 2008,
vol: 21 (9); 416-23.
11. Arthro PJ, Thyme B, Warring
(2002). A Calibration study of the
ultrasound unit, Phys Ther, 82;
257-263.
12. Ankrom MA, Benneh RG, Sprigle
S, et al. Pressure related deep tissue
injury under intact skin and the
current pressure ulcer staging
systems. Adv. Skin Wound care,
2005; 18 (1); 35-45.
13. McDiarmid T, Burns PN, Lewith
GT, Machin D. Ultrasound and the
treatment of pressure sores,
Physiotherapy, 1985; 71; 66-70.
14. Dyson M. Role of ultrasound in
wound healing. In: Mcculloch JM.
Kloth LC, Feeder JA, eds. Wound
Healing. Alteratives in
Management, 2nd ed, Philadelphia
Pa: FA Davis co; 1995; 319-345.
15. Sari AA etal. Therapeutic
ultrasound for pressure ulcers.
Cochrane Database of systemic
reviews. 2009 (4).
16. TerRiet G, Kessels AG, Knipschild
P (1996). A randomized clinical
trial of ultrasound in the treatment
of pressure sores. Phys Ther 76;
1301-1311.
17. Whatson GW, Milani JC, Dean LS.
Pressure sore profile: cost and
management, ASIA, Abstracts
Digest, 1987; 115-119.
18. Houghton PE, Kincaid CB,
Campell KE, et al. Photographic
assessment of the appearance of
chronic pressure and leg ulcers.
Ostomy / Wound Management.
2000; 46(4); 20-30.
ACKNOWLEDGMENT:
I thank the men who participated in this trial. I would also like to thank chairman Sri. C.
Lakshmi Narasimha Rao, Prof. V. Suryanarayana Reddy, Director, Chalmeda Anand Rao
Institute of Medical Sciences, Karimnagar for his support and encouragement of this study.
CORRESPONDENCE:
*Asst. Professor & I/C Head, Department of Physical Medicine and Rehabilitation Chalmeda
Anand Rao Institute of Medical Sciences Karimnagar -505001, Andhra Pradesh, INDIA.
Mobile: 08790544270, Fax: 0878-2285318. E-mail: shanmugampt@rediffmail.com
Effectiveness of Educational Sessions on Reducing Diabetes in Women with
PCOS A Pilot Study
B. Sharmila, BPT, MSc (Yoga)*, B. Arun, MPT**
Abstract: PCOS (Poly cystic ovarian syndrome) is one of the common syndromes
in females, around 10 % of females in world having PCOS. PCOS have a strong
link on Diabetes. Study is a descriptive study to find out the effect of educational
session on diabetes for women who has PCOS. Around 20 females with PCOS
were selected, an Educational session was conducted for duration of 4 weeks, and
Diabetic Questionnaire was given to analyze the knowledge of diabetes. Following
the 4 weeks of educational sessions, all participants have gained a good
knowledge on PCOS and Diabetes. This study concludes that educational session
is very important for the management of Diabetes and especially for females who
has PCOS.
Key words: Type II diabetes, PCOS, Educational Session, Diabetic Questionnaire.
INTRODUCTION
Diabetes is one of the most common health
problems in the world. India is the capital
of diabetes. Many studies conducted in
India showed that prevalence of type 2
diabetes was more and it is increasing in
urban populations
1, 2
. Diabetes exerts a
significant impact on the lives of
individuals and their family members due
to the constant need for decision-making
and actions to promote good glycemic
control, an outcome acknowledged as the
foremost goal in diabetes care and
treatment
3
.
The burden of diabetes on women is
unique, because the disease can affect both
mothers and their unborn children.
Diabetes can cause difficulties during
pregnancy such as a miscarriage or a baby
born with birth defects. Women with
diabetes are also more likely to have a
heart attack and at a younger age than
women who do not have diabetes. Type 2
diabetes is strongly associated with
Women who suffer from PCOS (Poly
cystic ovarian syndrome). PCOS is a
leading cause of menstrual irregularity and
female infertility. The Statistical links
between diabetes and PCOS are very
strong about 5%--10% of reproductive age
women have PCOS and 50% --70% of
women with PCOS also experience insulin
resistance and 20%--40% obese women
with PCOS may have insulin resistance
and diabetes.
Polycystic ovary syndrome (PCOS) is
a common endocrine disorder, affecting
women in reproductive age, characterized
by chronic anovulation and
hyperandrogenism. The etiology of PCOS
is still unknown. However, several studies
have suggested that insulin resistance
plays an important role in the pathogenesis
of the syndrome. The risk of glucose
intolerance among PCOS subjects seems
to be approximately 5 to 10 fold higher
than normal and appears not limited to a
single ethnic group. Moreover, the onset of
glucose intolerance in PCOS women has
been reported to occur at an earlier age
than in the normal population
(approximately by the 3rd-4th decade of
life). However, other risk factors such as
obesity, a positive family history of type 2
diabetes and hyperandrogenism may
contribute to increasing the diabetes risk in
PCOS
4
. Dr.Geoffrey Redmond said that
There is no question about the
association one of the problems is that
people havent put the pieces together He
added that there is a strong association
between PCOS and Insulin resistance.
While focusing the infertility and
menstrual changes, health care
professionals should also look for the
chance of diabetes, and screening of
diabetes is much desirable.
Women with polycystic ovary
syndrome (PCOS) are insulin resistant,
have insulin secretory defects, and are at
high risk for glucose intolerance. PCOS
women are at significantly increased risk
for IGT and type 2 diabetes mellitus at all
weights and at a young age, The
prevalence rates are similar in 2 different
populations of PCOS women, suggesting
that PCOS may be a more important risk
factor than ethnicity or race for glucose
intolerance in young women, and the
American Diabetes Association diabetes
diagnostic criteria failed to detect a
significant number of PCOS women with
diabetes by post challenge glucose values
5
.
Type 2 Diabetes has pancreas that
produces little or no insulin. As the
pancreas struggles to keep up with the
body's need for more insulin, excessive
levels of glucose and insulin build up in
the blood stream, often leading directly to
Type 2 Diabetes.
Certain factors that figure in the onset of
PCOS are also implicated in the
development of Type 2 Diabetes:
excessive abdominal fat, high LDL "bad"
blood cholesterol and low HDL "good"
cholesterol, high levels of triglycerides and
hypertension (high blood pressure).
Although PCOS is much perceived as
gynecological disorder because it impairs
fertility and can cause irregular periods or
no periods at all. Evidences suggest that
PCOS is more of a disorder of the
endocrine system with gynecological
consequences.
Diabetes Prevention Program study
2001, study shows that all of the factors
associated with Insulin Resistance,
Polycystic Ovarian Syndrome and Pre-
Diabetes are interrelated. Obesity and lack
of exercise worsen Insulin Resistance,
which then has a negative effect on blood
lipid production, increasing VLDL (very
low-density lipoprotein), LDL cholesterol
(low-density lipoprotein - the "bad"
cholesterol) and triglyceride levels in the
blood stream, as well as decreasing HDL
cholesterol (high-density lipoprotein - the
"good" cholesterol.)
While there is no cure for diabetes, a
number of steps can be taken to prevent
complications. Research showed that
losing 5-7% of body fat and increasing
physical activity by taking a brisk walk 4-5
times a week can reduce risk of developing
Type 2 Diabetes by almost 60%.
DIABETES PCOS LINK
Need for the study:
It's important to understand the distinction
between Insulin Resistance and Type 2
Diabetes. Type 2 Diabetes is one of the
top fatal disorders in the World. In 2000, it
was the sixth leading cause of death and
has been associated with long term
complications affecting almost every part
of the body, including blindness, heart and
blood vessel disease, stroke, kidney
failure, amputations and nerve damage.
Obese women are particularly susceptible
to PCOS and Type 2 Diabetes. A vicious
cycle quickly forms because these
conditions, in turn, put women at
dramatically increased risk of
Cardiovascular Disease, as well as the
development of many other serious health
conditions, including stroke, kidney
damage and blindness. Overweight women
do not, however, have a monopoly of
Polycystic Ovarian Syndrome and its
related disorders because females of
normal weight and even lean women are
also prone to these conditions.
Insulin Resistance occurs when the body
produces enough insulin but its cells lack
enough receptor sites to allow the
absorption of insulin at a cellular level.
Type 2 Diabetes develops when the body
either doesn't produce enough insulin or it
can't process the insulin that is produced.
Aim of the study:
To m
Study Objectives:
To educate the patient about disease
(PCOS) and teach on link between PCOS
and Diabetes
To make the patient learn about the
preventive methods
To reduce the risk of getting diabetes
To make patient to understand the
importance of Diet, Exercises etc.
METHODOLOGY:
The study is a descriptive study design,
100 women with PCOS were examined by
the Gynecologist and 20 women were
selected for the study. The subjects were
selected based on age group of 25
33years, Married females, Married within
2 years, Obese or female in Borderline
obesity. No history of conception, No
other gynecological problems like irregular
menstrual periods or small uterus. No
other relevant medical problems. Before
initiating the study Blood test was
conducted to check their random blood
sugar levels. Clear instructions were given
to all the participants. The educational
class is for 4 weeks of duration and the
Diabetic educator role is to make all
participants attending all the sessions.
Prior to the class a Diabetic knowledge
Questionnaire was distributed to all
individuals and to find out how much
knowledge on Diabetes and PCOS. The
questionnaire was a single paged one
which includes the questions about the
knowledge on diabetes and the knowledge
on PCOS. The participants were asked to
fill up the questionnaire with Yes or No.
Questions are valued as 1 point for Yes
and 0 point for No. Educational Classes
conducted on Every Sunday Morning (10
am 1 pm). The content of the Classes
include 1) What is PCOS 2) What are the
Causes 3) Symptoms of Diabetes with
PCOS 4) Diabetes Link with PCOS 5)
Prevention Methods. The questions asked
by the women participants were clarified.
At the end of the programme all
participants were instructed to fill up the
questionnaire and their performance was
assessed. At the end of the 4 week class
the questionnaire was repeated and
assessed the knowledge on diabetes for
women with PCOS.
RESULTS:
The demographic data about the subjects
were mentioned in Table 1.
Table 1
Demographic Data
Age
Group
2527 2830 3133
7 6 7
Figure 1
The Table 2 shows the result using
students t test.
Groups
Pre
Test
Post
Test
S.D
Paired t
Value
mean mean
3.8 7.85 0.285
14.19
(P<0.05%)
Figure 2
Table 2 shows the paired t values of the
Diabetic Questionnaire. This shows that
the educational programme has shown
positive effect on the participants attitude.
It also shows that there was a significant
improvement on the knowledge on
diabetes mellitus.
DISCUSSION:
Women with PCOS are generally
Overweight or Obese. Because of obesity
they have more chance of insulin
resistance. Usually women with PCOS
dont have a regular check up on diabetes.
But screening for diabetes is very
important in prevention of diabetes. A root
cause of Polycystic Ovarian Syndrome
(PCOS) is obesity-linked Insulin
Resistance, which can also increase the
risk of developing Pre-Diabetes and Type
2 Diabetes. All are disorders that may
result in Cardiovascular Disease leading to
a heart attack or stroke. Creating self
awareness in people with PCOS is very
important, so that the Type 2, diabetes can
be prevented as well as prevent the
complications following diabetes.
Women with PCOS (Polycystic Ovarian
Syndrome) who become pregnant may
experience more health problems than the
general population, including gestational
diabetes, pregnancy-induced high blood
pressure, miscarriage and premature
delivery.
Polycystic ovary syndrome (PCOS) is a
common endocrine disorder, affecting
women in reproductive age, characterized
by chronic anovulation and
hyperandrogenism. The etiology of PCOS
is still unknown. However, several studies
have suggested that insulin resistance
plays an important role in the pathogenesis
of the syndrome. The risk of glucose
intolerance among PCOS subjects seems
to be approximately 5 to 10 fold higher
than normal and appears not limited to a
single ethnic group. Moreover, the onset of
glucose intolerance in PCOS women has
been reported to occur at an earlier age
than in the normal population
(approximately by the 3rd-4th decade of
life). However, other risk factors such as
obesity, a positive family history of type 2
diabetes and hyperandrogenism may
contribute to increasing the diabetes risk in
PCOS
The link of PCOS with insulin resistance
was subsequently established by clinical
studies characterizing the profound insulin
resistance in obese and lean PCOS
patients. Insulin resistance,
hyperinsulinemia, and beta-cell
dysfunction are very common in PCOS,
but are not required for the diagnosis.
Polycystic ovary syndrome (PCOS) is a
major risk factor for impaired glucose
tolerance (IGT) and type 2 diabetes
mellitus (T2D). Several studies have
examined possible mechanisms related to
glucose metabolism and insulin secretion
that may be responsible for the high
prevalence of disorders of glucose
metabolism in women with PCOS. The
actual pathogenic mechanisms appear to
be complex and multifactorial, possibly
characterized by the lack of uniformity
between patients, thus reflecting the
heterogeneity of PCOS. Impaired insulin
action and/or beta-cell dysfunction and/or
decreased hepatic clearance of insulin have
been implicated so far.
The overall risk of developing diabetes
mellitus and glucose intolerance seems to
be higher in women with polycystic ovary
syndrome (PCOS) than in healthy women.
Limitations of this study include, no
control group, it was a pilot study; need a
bigger study to evaluate the effectiveness
of the programme. Blood report
investigations can show some reliable
information. Efficacy of the treatment can
also be evaluated through objective
methods.
REFERENCES
1. Mohan V, Shanthirani S, Deepa R,
et al. Intra urban differences in the
prevalence of the metabolic
syndrome in southern India - The
Chennai Urban Population Study
(CUPS). Diabet Med 2001; 18;
280-287
2. Misra A, Pandey RM, Rama Devi J,
et al. High prevalence of diabetes,
obesity and dyslipidaemia in urban
slum population in northern India.
Int J Obes 2001; 25: 1-8.
3. Brown S: Studies of educational
interventions and outcomes in
diabetic adults: a meta-analysis
revisited. Patient Educ Counsel
16:189215, 1990.
4. Pelusi B, Gambineri A, Pasquali R..
Type 2 diabetes and the polycystic
ovary syndrome. Minerva Ginecol.
2004 Feb;56(1):41-51.
5. R. S. Legro et al. Prevalence and
predictors of risk for type 2 diabetes
mellitus and impaired glucose
tolerance in polycystic ovary
syndrome: a prospective, controlled
study in 254 affected women, The
Journal of Clinical Endocrinology
and Metabolism, vol. 84, no. 1, pp.
165169, 1999.
6. Alberti KG, Zimmet PZ: Definition,
diagnosis and classification of
diabetes mellitus and its
complications. Part 1: diagnosis and
classification of diabetes mellitus
provisional report of a WHO
consultation. Diabet Med 15:539
553, 1998
7. American diabetic association
(1999), American association guide
to medical notional therapy and
diabetes.
8. Balkau B, Charles MA: Comment
on the provisional report from the
WHO consultation. Diabet Med
16:442443, 1999
9. Canadian Diabetes Association.
(1998). 1998 clinical practice
guidelines for the management of
diabetes in Canada. Canadian
Medical Association Journal, 159,
S1-S29.
10. Chobanian AV, Bakris GL, Black
HR, Cushman WC, Green LA, Izzo
JL, Jones DW, Materson BJ, Oparil
S, Wright JT, Roccella EJ: The
seventh report of the Joint National
Committee on Prevention,
Detection, Evaluation, and
Treatment of High Blood Pressure:
the JNC 7 report. JAMA 289:2560
2572, 2003
11. Codner E etal., 2006, Diagnostic
criteria for Polycystic ovarian
syndrome and ovarian morpholly in
women with Type II diabetes,
Endocrine Med : Jun 91 (6): 2250-6.
12. Isomaa B, Almgren P, Tuomi T,
Forsen B, Lahti K, Nissen M,
Taskinen MR, Groop L:
Cardiovascular morbidity and
mortality associated with the
metabolic syndrome. Diabetes Care
24:683689, 2001
13. Kitzinger C, Willmott J: The thief
of womanhood: womens
experience of polycystic ovarian
syndrome. Soc Sci Med 54:349
361, 2002
14. Lakka HM, Laaksonen DE, Lakka
TA, Niskanen LK, Kumpusalo E,
Tuomilehto J, Salonen JT: The
metabolic syndrome and total and
cardiovascular disease mortality in
middle-aged men. JAMA
288:27092716, 2002
15. Legros RS et al., PCOS
prospective controlled study in 254
affected women, J clin endocrine
metan: 84:165169.
16. Pouliot MC, Despres JP, Lemieux
S, Moorjani S, Bouchard C,
Tremblay A, Nadeau A, Lupien PJ:
Waist circumference and abdominal
sagittal diameter: best simple
anthropometric indexes of
abdominal visceral adipose tissue
accumulation and related
cardiovascular risk in men and
women. Am J Cardiol 73:460468,
1994
17. Reaven GM: Banting lecture: Role
of insulin resistance in human
disease. Diabetes 37:1595 1607,
1988
18. Sarah Wild, Mb Bchir, Phd, Gojka
Roglic, Md, Anders Green, Md,
Phd, Dr Med Sci, Richard Sicree,
Mbbs, Mph, Hilary King, Md, Dsc,
Global Prevalence Of Diabetes,
Diabetes Care 27:10471053, 2004
19. Taylor AE, 2000, Insulin
Lowering medications in Poly cystic
ovarian syndrome. Obstet gyneol
Clin north: Apr 27: 583595.
20. The Expert Committee on the
Diagnosis and Classification of
Diabetes Mellitus: Report of the
Expert Committee on the Diagnosis
and Classification of Diabetes
Mellitus. Diabetes Care 20:1183
1197, 1997
21. WHO Study Group Report.
Prevention of Diabetes Mellitus.
Geneva: World Health
Organization; 1994. WHO Technical Report series no. 844.
APPENDIX I
DIABETIC QUESTIONNAIRE
Name : Date :
Age :
Occupation :
Address :
Weight :__________ Kgs.
Height : __________CMS
BMI :
Do you have Diabetes : YES / NO
If YES, How long :___________ Months/ Years.
Are you in medications for Diabetes : YES / NO
If YES, Specify medicines : ________, ___________, ___________
Do you have PCOS : YES / NO
If YES, Since when : ____________ Months / Years
Are you in medications for PCOS : YES / NO
If YES, Specify medicines : ________, ___________, ___________
Please fill up the given statement with Yes or No.
S.No STATEMENT Yes No
1. Do you know symptoms of Diabetes
2. Do you know about PCOS
3. Do you know Obesity may cause Diabetes
4. Do you know Obesity may cause PCOS
5. Do you know relation between PCOS & Diabetes
6. Do you know the Risk factors for Diabetes
7. Do you think it is good to do Exercises regularly
8. Do you think intake of Rice may cause Diabetes
9. Do you think you can get Diabetes
10. Do your Parents or Relative have Diabetes
Signature of the Participants Signature of the
Assessor
CORRESPONDENCE:
*Physiotherapist, K.M.C.H Hospital, Coimbatore. Email: sharmibala85@gmail.com.
**Physiotherapist, K.G. Hospital, Coimbatore.
Perception of students for laptop ergonomics and its use in the learning
centre of Sheffield Hallam University, U.K.
Mayank Pushkar. BPT, MSAPT (Musculoskeletal)*, Shobhit Sagar. BPT, MSAPT
(Musculoskelatal)**
Abstract: Background and purpose: Laptop ergonomics is one of the most
concerned topics which result in high number of symptoms. The aim of this study
is to find out students perception about laptop ergonomics and how to make the
learning centre more laptop friendly. Methodology: A Qualitative survey with
questionnaire consisting of both open and close ended questions was used. 80
volunteer participants participated in this study. Convenience Sampling was used
for the selection of participants. Qualitative Content Analysis has been used for
the analysis of the data. Results: It was observed that most of the students use
laptop but they also get musculoskeletal problems (Laptopitis) because of the
extended use and adopting improper posture while using laptop. Poor adaptation
of posture was mainly because of unawareness about laptop ergonomics and also
because of poor set-up in the learning centre. Conclusion: Laptop can be used in
more friendly way without causing any discomfort if both the factors (awareness
and ergonomics setup) will be considered. Also the awareness about the laptop
ergonomics and proper posture should be spread among student populations as
most of students from other faculties (0ther than related with health faculty) was
not aware about the proper posture and ergonomics.
Keywords: Laptop Ergonomics, Library Setup, Workplace Ergonomics,
Laptopitis/ Laptop Related Injury
INTRODUCTION
Now a days, technological advances such
as use of personal computers directly
affect the life of people
1
. As per the
National Centre for Education Statistics
(2000), the number of students using
computers has increased by more than
50% between 1985 and 1999 in the United
Kingdom alone. With 98% of universities
having internet facilities, the number of
students opting for use of laptops to
conduct their activities is also
increasing
2
.In fact, 80% of British students
own a laptop in which 40% spends 3 4
hours daily on internet
3
. Laptops are
widely being used by professionals who
need to travel and work in different places
like office or college4. This phenomenon
is occurring largely because of the many
benefits accruing from laptops. Laptop
offers high technology performance in a
compact, light, portable and self-sufficient
with battery provided
2
.
It may be noted though, that the laptop was
not configured for long or constant use
2
.
However, since they are increasingly
replacing desktops, students do use them
for extended periods of time. This has
resulted in a series of illnesses affecting
different parts of the body which include
pain in the neck, upper back, hands and
wrists, numbness, swellings, and tingling
sensation
5
.Laptops induced injuries have
become so common that an all-
encompassing term has been used to refer
to them as Laptopitis, which includes
musculoskeletal and vision related
disorders
6
. Laptops construction and usage
result in users assuming improper posture
resulting in body discomfort, visual and
mental strains
2
. Moreover, workstations
configured for laptop computers,
unsuitable furniture faulty lightings,
further contribute to the physical injuries
resulting from use of laptops
5
.
Hence, there is a great need to study the
ergonomics of laptops. Laptop ergonomics
is a sub discipline under the broad
umbrella of ergonomics that postulates the
optimal manner of working on laptops and
the design of workspaces, where they are
used in order to keep related injuries to a
minimum and optimize performance
7
. This
study is focused on the views of students
about the laptop ergonomics and how to
modify or redesign the learning centre, so
that laptops can be used in their preferred
way in the learning centre for extended
periods of time without causing any
physical discomfort or injury.
LITERATURE REVIEW
Few studies have been previously
undertaken on ergonomics related to the
use of laptops or computers. This report
has tried to discover the perception of
participants about laptop ergonomics and
their views about the lack of resources in
learning centre for use of laptop in
ergonomic way.
Straker and Harris (2000) have completed
a mixed study with both qualitative and
quantitative data in order to establish the
physical ergonomics issues associated with
the use and carry of laptop computers by
school children. In total 314 participants
aged between 10 and 17 years participated,
and filled the questionnaire in phase 1 of
the study and 20 participants were
observed using the laptop in various
locations in second phase of study. The
result found that the participant's
discomforts were resulted from using the
laptop in a variety of non-traditional work
postures and also depend on the model of
laptop they use and carry. The study
identified the potential physical
implications associated with the use of
laptops.
Straker et al. (1997a) had studied the
adoptive posture while using laptops and
desktops. The study was a cross-over study
with 16 participants, who were
government employers. It was found that
laptop users adopt a posture with increased
neck, shoulder and elbow flexion but the
difference was not significant as compared
to desktop users. Similar results were
observed by Harbinson and Forrester
(1995). The study concluded that laptop
users required an increased forward head
inclination in order to operate the laptop
due to lack of its adjustability.
Gold et al. (2011) quantitatively studied
postural characterisation in Laptop users in
non-desk setting with 20 asymptomatic
right-hand dominant participants aged
between 18 and 25. The selected
participants were assessed in 3 postures
with two minute typing task followed by
5-minute editing task on laptop. The study
has used MaxMATE motion data analysis.
It was found that subjects reported greater
intensity of discomfort while using laptop
in prone lying.
Price and Dowell (1998) conducted a
quantitative study on 14 volunteer
participants to evaluate the effect of laptop
configuration and external input device on
posture and comfort of laptop users. Each
participant was asked to work on 6
different computer configuration and
anthropometric data and baseline Nordic
Discomfort Scale was completed before
the start of the task. The study concluded
that use of extra peripherals in laptop
seems to be more comfortable and thus
decrease the discomfort associated with
laptop usage.
Kumari and Pandey (2010) have
conducted a cross-sectional study to
analyse the health problems associated
with computer usage and role of
ergonomic factors. A total of 200
participants were selected by stratified
random sampling from different IT
industries. Close ended questionnaire were
used as data collection tool. The analysis
of the data was done by using SPSS
software. A standardized Nordic
Questionnaire was use to assess
musculoskeletal problems and Zungs self-
rating scale was used to assess depression.
The study concluded the various problems
associated with laptops or desktops use
and also the effects of underlying factors
like- environment, lighting and setup of
the work place on laptop ergonomics.
Several studies on ergonomic research
with desktops while the same cannot be
said for laptops, through some studies have
indicated the development of physical
symptoms associated with laptop use. Few
of the researches have been done, which
found the symptoms associated with the
use of laptop
2,4,5
. As per the researchers
knowledge till now none of the studies
tried to find out the solution so that people
can use laptop in more comfortable and in
their preferred way for prolonged time
without causing any discomfort. Hence,
this study aims to focus on the ergonomics
of laptops and what modification can be
done in the learning centre of Sheffield
Hallam University, so that students can use
their laptop in learning centre in their
preferred way without any discomfort.
Ethical approval was obtained from
Dissertation Management Group
(Sheffield Hallam University). Participants
were given the information sheet and
completion of an anonymous questionnaire
was considered as consent from the
participants.
METHODOLOGY
Research Design
A Qualitative study design with
questionnaire survey was used to obtain
the student's perception about laptop
ergonomics. A qualitative research is the
best means of generating in-depth ideas
and developing hypothesis which may
eventually decide to test quantitatively
8
.
As the main aim of this study was to
gather in-depth information and generate
ideas so the design of the study was
chosen as a qualitative study.
Sampling
A total of 80 participants were selected
based on inclusion criteria by
convenience sampling as it was not
possible to approach all the student
population in Sheffield Hallam University.
It is practically easy and fast method of
sampling if the population is very large
9
.
Convenience Sampling is said to be more
appropriate for the study in which the aim
is to get in-depth information
10
.
TABLE 1- INCLUSION AND EXCLUSION CRITERIA:
INCLUSION CRITERIA EXCLUSION CRITERIA
Students of Sheffield Hallam University.
Students who were using Laptop/ Desktop
for
their course work.
Students who knew English Language.
Students who were not using laptop/Desktop.
Students who were not student of Sheffield
Hallam University.
Data collection:
The data was collected through the survey
method by using a tool called a
questionnaire as it is the essential form of a
survey to a large sample population
11
. A
questionnaire is an important method of
survey to a large sample population
11
. The
questionnaire consisted of both close and
open ended questions. Close ended
questions were objective and
unambiguous. Open ended questions were
used for collection of larger amounts of
information. The questionnaires were
developed on the basis of Environmental
and Occupational Health and Safety
Service (EOHSS) Computer Workstation
Ergonomics Questionnaire. Prior to the
implementation of questionnaire, they
were circulated among the colleagues to
check for content validity and suggestions
were considered while reframing the
questionnaire. The questionnaire was pilot
tested with 7 participants and the
information was taken into consideration
while making final questionnaire. Changes
were made in 7 questions after piloting of
the study. The evidence suggested that, for
the questionnaire to be valid and reliable, it
should go through the formal pilot of the
questionnaire by the same sample
population
12
.
Data Analysis:
The main purpose of data analysis is to
identify what the texts of participants talk
about. The qualitative content analysis is
used to process and analyse the
information given in text format or from
an open ended questions
13
. The data
gathered was more descriptive, hence it
was suitable for qualitative content
analysis
14
.
Hence, the qualitative content data
analysis
15
was used for data analysis,
which involves the following steps:
1. Prepare the data: Present all the
data collected in a chart format.
2. Identifying the unit of analysis:
Identify the different
Units/keywords from the text.
3. Developing categories and a
coding scheme: It can be derived
from three sources: the data,
previous related studies, and
theories.
4. Code testing on a sample of text:
It is used for the clarity and
consistency of category definitions.
5. Code all the text: Involves coding
all the data which have been.
Different units/keywords with
similar sense were given single code
6. Assess coding consistency: This
step involves rechecking the
consistency of coding.
7. Draw conclusion from the coded
data: This step involves making
sense of themes and identified their
properties.
Rigour of analysis was enhanced by a
several-stage process of defining and
refiningthemes, by constant comparative
analysis between scripts and themes until
final themes were developed. This analysis
produced 7 key themes, which are listed
with their definition in Table 2.
TABLE- 2: Main Themes from Data Analysis.
THEMES DEFINITION
Factors which facilitates the use of
LC.
Reasons because of which students use
LC.
Preference of use of Laptop/Desktop in
LC
Whats the reason for preference of
using Laptop/Desktop.
Symptoms faced while
using Laptop/Desktop
Which all symptoms the participants
suffer and whats its cause?
Posture Awareness Awareness about the posture in
participants.
Environment/ Infrastructure of LC How is the environment and setting of
LC for the use of laptop.
Interference with extra
Computer-accessories.
How does the extra computer-accessories
interfere the level of comfort and increase
the work efficacy.
Recommendation to Improve LC What changes can be done to improve the
LC for the use of Laptop.
RESULT:
The questions which were related were put
into similar themes and then the results
were presented on the basis of sub-themes.
Factors that facilitates use of Learning
Centre
Almost all participants were using the
learning centre for their course work
because of better facilities or resources
like- "Books, Journals, area, IT
equipment/resources, caf etc.", while
many participants said that they prefer
Learning Centre because they like the
environment of Learning Centre as it is
"Quite place and easy to concentrate for
the study". Some of the participants use
Learning Centre because of the
convenience and comfort, like- they can
"use leisure hours between the lecture, the
convenient opening and closing hours of
Learning Centre and group study/work".
Few of participants said about
psychological motivation they get in
learning centre for study.
Preference of use of laptop or desktop in
learning centre
When the participants were asked whether
they use laptop or desktop in learning
centre, 42 participants said that they use
desktop as they feel it convenient and
comfortable. They said that they "do not
have to bring laptop and it is easy for them
to use desktop than laptop". Some of them
said that, they "prefer desktop because of
big screen of desktop and also there is less
space and plug points for laptop in
learning centre". Few of the participants
said that it is "easy to work on desktop as
the desktop is fast and more comfortable"
and also they "can use it for prolonged
period of time". Only 11 participants
said that they use laptop in learning centre
because they "prefer to use laptop" and
also it is "convenient for them to save their
data". Some of the participants said that
they use laptop as they "can use it
anywhere in learning centre, comfortable,
easy to use and it is more portable".
Problems or symptoms faced by
participants while using laptop or desktop
From the result it was observed that, the
most experienced symptoms were Tight,
sore neck and shoulder muscles,
followed by Pain or aching in wrists,
forearms, elbows, neck, or back followed
by discomfort, and then General fatigue
or tiredness, then Blurred or double
vision. Also it was found that, the least
faced symptom was Swelling or stiffness
in the hand or wrists.
Most of the participants said that, these
symptoms are because of their bad or poor
posture like- (Keeping laptop on knee,
using laptop while lying down, Slouched
posture etc.), continuous position such as:
(Sitting for prolonged, focusing on small
screen for long period, no interval between
work etc.), and ergonomics setup like-
(Desks and chairs not adjusted, Too close
to screen for long period etc.). Some of the
participants said that there might be some
other reasons for the symptoms like- (weak
joint, poor posture throughout the day,
Back and neck pain from exercise).
Posture Awareness
Out of 80 participants, 55 participants
stated a positive response and defined
posture in their own words, while 25
participants have given negative response
as they were not aware with the correct
position or posture for the use of laptop.
The participants who were not aware about
the posture were mainly from the faculty
other than health related courses such as:
Criminology, Events management,
Information system management, Law etc.
Most of the participants said, usually
posture means: sit straight, back support,
hip and knee flexed, and screen at eye
level. Some of the statements given by the
different participants to define posture for
laptop are presented below:
Screen in line with eyes, elbow flexed to
90, knee at 90, hip at 90, shoulder
flexed. (2)
Back support, Hip + Knee supported,
Appropriate Height. (39)
Sit erect, avoid neck flexion, sitting at
comfortable distance, and avoid excessive
elbow bending. (62)
Environment or Infrastructure of
Learning Centre (LC)
More than half of participants found
environment of learning centre to be
comfortable for the use of Laptop.
Participants found environment of learning
centre comfortable because of different
resources like- Tables, adjustable chairs,
more space for laptop, plug points, proper
lighting and easily accessible resources.
While less than half of the participants
found the environment of Learning Centre
is not comfortable for laptop use.
Participants said that, there is less space,
less number of tables for laptop, tables
and chairs are not setup at proper height
or not adjustable, and also there is less
charging plug/points for laptop use.
When asked about the infrastructure/
setting of Learning centre, most of them
said that the environment of learning
centre is comfortable because of tables
and adjustable chairs, proper lighting and
quite area. While one quarter of
participants did not find the infrastructure
of LC to be comfortable because of
different difficulties such as: Limited
space around the table, uncomfortable
chairs, cold environment, chairs do not
have armrest, very much crowded. Some
of them said that there are fewer resources
such as: Area, less table and chairs, less
space around the table.
Interference with extra computer-
accessories like- keyboard and mouse on
laptop work
Out of 80 participants, some of the
participants answered that, use of extra
equipment like- mouse and keyboard could
provide more comfort and can work with
greater ease. Participants answered that use
of extra equipment can provide more
comfort, free movement and also they can
modify their position accordingly. Some of
the participants said that mouse is better
than touchpad and they can work faster
and in more comfortable way. Few
participants answered that use of keyboard
and can provides more comfort to them
and they do not have to negotiate with
posture. While more than half of
participants answered that, they do not find
any difference in comfort level with the
use of extra keyboard and mouse in the
Laptop. Some of them said that they do
not want to carry keyboard and mouse and
also they can manage fine without it.
Recommendation to improve Learning
Centre for use of Laptop
Major number of participants have
suggested with different recommendation
for the use of laptops in learning centre so
that laptop can be used for extended period
of time. Most of them want proper
ergonomic setup for laptop users, more
laptop area, more spacious table,
comfortable chairs with neck and back
support, and plug points for laptop
changing. Some of the participants have
suggested for the Laptop stand, specific
type of table for laptop and dock station
for laptop. Few of the participants said
that there should be more tables for
laptop in silent area and also individual/
separate booth/ room for laptop users.
DISCUSSION
This qualitative study obtained students
perception about laptop ergonomics and its
use in the learning centre of SHU. Almost
all participants use learning centre for their
course work because of the better
environment and different types of
resources available. The environment of
learning centre provides more comfort and
motivation to the students for the study,
because the setup of the environment is
study oriented. It has also been shown that
hot and noisy environment directly affects
the work productivity and ergonomic
condition
16
. Student population use laptops
in the learning centre because of the many
benefits of the laptop. It is easy to carry
and use laptop as the participants can save
their data
17
.
It was observed that most of the
participants experienced some of the
symptoms while using either laptop or
desktop. From the data gathered by
questionnaire, it was found that the
participants faced problems related to
neck, shoulder, hand, back and eyes. The
most common symptoms were Pain or
aching in wrists, forearms, elbows, neck,
or back followed by discomfort (42%)
and eye strain (42%). Similar type of
results was found by Kumari and Pandey
(2010) and said that the common causes of
these symptoms were sitting for prolonged
in awkward or poor posture (Fig-1). Also
the literature suggested that the
participants should take eye break every
after 20 min to reduce strain on eye while
working on laptop
18
. It was also found that
participants who use laptop faced more
symptoms than the one who use desktop.
This could have been in order to adjust the
posture to use desktop and laptop in more
comfortable position
3
. Even evidence
proves that participants adopt poor posture
because of the lack of adjustability of the
laptop as the screen and keyboard are
attached
2
. This was supported by another
study by Straker et al. (1997a), they have
suggested that usually laptop users tried to
assume posture that would compromise
their posture by increased neck, shoulder
and elbow flexion. They adopt this posture
in order to see a lower screen and reach a
higher keyboard. The main factors judged
by the participants as cause of their
symptoms while using laptop or desktop
were Sitting in same posture for
continuous long hours, Awkward and
poor posture, and the setup for laptop
which was not ergonomically correct.
As the height of table in the learning centre
is not appropriate, and also some of the
communal table which are being used for
laptop use are of very low height so it is
difficult to adjust the chairs accordingly.
As the evidence by Straker and Harris
(2000) suggested that the participants
experienced physical discomfort because
of the physical ergonomic issues as they
use the laptop in poor posture. This was
supported by Moffet et al. (2002) in their
study; evaluated the impact of two work
station (desktop and laptop) on neck and
upper posture, muscle activity and
productivity. The study said that the
workstation setup influenced the physical
exposure variable while working on
laptop.
Fig-1: Shows the poor and good posture for Laptop.
Some of the participants who were not
related with health course, they did not
know about the correct position or posture
for the use of laptops. They have not
defined the posture. This might be because
of lack of awareness about ergonomics
among that students population. So the
participants adopt the poor posture while
working on laptop, because it has been
found that lack of knowledge about
posture can leads to symptoms as they do
not adopt the proper posture while
working on desktop or laptop
5
.
From the result it was also found that use
of extra computer- accessories can provide
more comfort, and can ease the symptoms
and increase the work efficacy of the
participants. This is because the extra
equipment provides the adjustability
according to the posture and the users do
not have to compromise with the posture.
This was supported by a study done by
Kumari and Pandey (2010) found that the
use of various computer accessories like-
adjustable keyboard tray, foot rest, best-fit
computer mouse design, task lighting and
docking station can help in preventing the
health related symptoms. Even some of the
participants have suggested for the use of
laptop stand or docking station (Fig-2). It
might be helpful because they can fix the
laptop and can use it in ergonomic way so
that the symptoms can be prevented.
Fig-2: Show the ideal Laptop stand/Docking station for laptop.
According to the ergonomic advice by
Stanford University, Environment Health
and Safety, the laptop workstation has
been suggested, so that the laptop could be
used as workstation if working for long
hours and the symptoms can be
minimized. Moffet et al. (2002) have
given some advices to prevent pain while
using laptop. The study has suggested the
use of docking station, so that the subjects
do not have to adopt the poor posture and
can use laptop in effective way.
The study had several limitations. Many of
the participants have not answered all the
questions which might be because of lack
of interest, lack of time or the structure of
the questions. All the analysis and
calculations were done manually so there
might be some chances of manual error. It
was not possible to explore in-depth
perception of participants as the method of
data collection was questionnaire. The
sample size (n=80) in the study was
relatively large, which was the strength of
the study. The participants were from
different faculties, which might have result
in variable data as the students from
different course have different perception
about the ergonomics. Rich informative
data were gathered through the open-ended
questionnaire, which was one of the aims
of qualitative research.
CLINICAL IMPLICATION:
Laptop ergonomics is very applicable for
all who use laptops. The result of this
study might help not only the student
populations but also the general population
who use laptop. As it was found that there
is lack of awareness about the proper
posture for laptop use among students, so
the measure should be done to spread the
awareness. Mainly the student population,
who are not from health related courses,
should be focussed. It might be very
helpful if there should be some induction
about the posture for the student
population before start of the course.
Awareness about the posture can be spread
though the means of Poster, distributing
leaflets, and induction or seminar. The
findings about the recommendation in
improving learning centre can be given
into the notice to the learning centre
authority Dept., so that they can use the
finding as feedback in improving the
learning centre for better use for students
and staffs. And also the students will be
benefited by these changes and they might
be able to use learning centre in more
efficient way.
The data of this study also has a further
clinical relevance; Symptoms are mainly
because of poor posture and wrong setup
of workstation of laptop, so in order to
prevent those symptoms, both the factors
should be corrected.
FURTHER RESEARCH:
As this was the first study to researcher's
knowledge done on the student population
in SHU about laptop ergonomics, so an
obvious need for more research in this area
is observed. More research should be done
in order to find out the actual ergonomic
setup of the working environment in the
learning centre.Also a quantitative study
could be suggested as further research in
order to find out the effectiveness of
ergonomics training program on posture
while working on laptop. Looking to the
current scenario it seems that in coming 10
years laptop or i-pad or tablet will be
replacing the desktop so the study should
be conducted in order to find out how the
learning centre should be designed
ergonomically for laptop or i-pad or tablet
use.
CONCLUSION:
From the research done, it can be seen that
students population prefer to use learning
centre because of the different facilities
and environment. But they also get
symptoms by using the resources like-
desktop or laptop, which is because of
wrong posture they adopt while working.
So these resources should be set-up on the
basis of ergonomics way and awareness
about the posture should be spread among
students.
REFERENCES
1. Gulek, J. C. and Demirtas, H. Learning
with technology: The impact of laptop use
on student achievement. Journal of
Technology, Learning, and Assessment,
2005;3(2).
2. Harris, C. and Straker, L. Survey of
Physical Ergonomics Issues Associated
with School Childrens Use of Laptop
Computers.International Journal of
Industrial Ergonomics, 2000;26;337-346.
3. Thrasher, M. and Chesky, K. Medical
Problems of Clarinetists. Results from the
UNTMusician Health Survey. Texas
Music Education Research. 1998. Last
Accessed 19th Dec 2011 at
http://www.tmea.org/080_College/Researc
h/thr1998.pdf.
4. Moffet, H. et al. Influence of laptop
computer design and working position on
physical exposure variables. Clinical
biomechanics, 2002;17(5):368-375.
5. Kumari, G. and Pandey, K.M. Studies
on health problems of software people: A
case study of Faculty of GCE and GIMT
Gurgaon, India. International Journal of
Innovation, Management and
Techonology,2010;1(1):388-397.
6. Blome, M., Johansson, C. R. and
Odenrick, P. Visualization of ergonomic
Guidelines A comparison of two
computer aided systems to support vehicle
design.International Journal of Industrial
Ergonomics,2005.
7. Szeto, G. and Lee, R. An Ergonomic
Evaluation Comparing Desktop,
Notebook, and Sub-Notebook Computers.
Arch. Phys. Med. Rehabilitation, 2002;83:
527-532.
8. Kumar, R. Research Methodology, A
step-by-step guide for beginners. 1st edn.,
SAGE,London, New Delhi, 2005.
9. Marshall, M.N. Sampling for qualitative
research. Family Practice,1996;13: 522-
525.
10. Patton, M.Q. Qualitative evaluation
and research methods. SAGE Publications.
Newbury Park London New
Delhi,1990:169-186.
11. Paul, H.P., Yeowa, Rabindarnath, and
Sen. Quality, productivity, occupational
health and safety and cost effectiveness of
ergonomic improvements in the test
workstations of an electronic factory.
International Journal of Industrial
Ergonomics,2003; 32: 147163.
12. Williams, A. (2003). How to write and
analyse a questionnaire. Journal of
orthodontics,2003;30:245-252.
13. Kondracki, N. L. and Wellman, N. S.
Content analysis: Review of methods and
their applications in nutrition education.
Journal of Nutrition Education and
Behavior, 2002;34: 224-230.
14. Ffiman, A., Ebbeskog, B. and Klag,
B.Wound care in primary health
care:district nursesneeds for co-operation
and well-functioning organization. J.
Interprof Care,2010; 24: 9099.
15. Mayring, P. Qualitative content
analysis. Forum: Qualitative Social
Research,2000;1(2).
16. Ashraf, Shikdar, Naseem, and
Sawaqed. Worker productivity, and
occupational health and safety issues in
selected industries; Computers &
Industrial Engineering, 2003;45( 4): 563-
572.
17. Shears, L. and McDonald. Computers
and Schools. Victoria. Australian Council
for Educational Research.1995.
18. Ergonomic Recommendations for
Laptop Computer Use. Stanford University
Ergonomic program.[Online]. Last
assessed on 17th Dec, 2011 at
http://www.stanford.edu/dept/EHS/prod/ge
neral/ergo/documents/laptop_guide.pdf
19. Environmental and Occupational
Health and Safety Service (EOHSS).
Computer workstation Ergonomics
Questionnaire. Last Accessed 19th Dec,
2011 at
http://www.umdnj.edu/eohssweb/publicati
ons/directory.htm#Office
20. Gold, J. E., et al. Characterization of
posture and comfort in laptop users in non-
desk settings. Applied ergonomics,
2012;43(2): 392-399.
21. Price, J.M. and Doewell, W.R. Laptop
Configuration in office: Effects on posture
and Discomfort.Human factors and
Ergonomics Society,1998;42:629-633.
22. Straker, Leon, Jones, Kerry J.,Miller,
an Jenni. A comparison of the postures
assumed when using laptop computers and
desktop computers. Applied
ergonomics,1997a;28(4): 263-268.
ACKNOWLEDGMENT
A special thanks to my family and friends for their continuous support. Also thanks to the
management of Sheffield Hallam University for giving me opportunity to complete my study.
CORRESPONDENCE:
* Sheffield Hallam University, United Kingdom. Email: physio.mayank.pushkar@gmail.com
**Sheffield Hallam University, United Kingdom
Buy your books fast and straightforward online - at one of worlds
fastest growing online book stores! Environmentally sound due to
Print-on-Demand technologies.
Buy your books online at
www.get-morebooks.com
Kaufen Sie Ihre Bcher schnell und unkompliziert online auf einer
der am schnellsten wachsenden Buchhandelsplattformen weltweit!
Dank Print-On-Demand umwelt- und ressourcenschonend produzi-
ert.
Bcher schneller online kaufen
www.morebooks.de
VDM Verlagsservicegesellschaft mbH
Heinrich-Bcking-Str. 6-8 Telefon: +49 681 3720 174 info@vdm-vsg.de
D - 66121 Saarbrcken Telefax: +49 681 3720 1749 www.vdm-vsg.de
Вам также может понравиться
- Scientific Research Journal of India ScReJI Volume 7 Issue 2 Year 2023Документ53 страницыScientific Research Journal of India ScReJI Volume 7 Issue 2 Year 2023Dr. Krishna N. SharmaОценок пока нет
- Scientific Research Journal of India SRJI Complete Vol-5 2016-2021 All IssuesДокумент30 страницScientific Research Journal of India SRJI Complete Vol-5 2016-2021 All IssuesDr. Krishna N. SharmaОценок пока нет
- Scientific Research Journal of India SRJI Complete Vol-4 2015 All IssuesДокумент53 страницыScientific Research Journal of India SRJI Complete Vol-4 2015 All IssuesDr. Krishna N. SharmaОценок пока нет
- Occupational Therapy Marketing Indian Prospective SRJI Vol 2 Issue 3 Year 2013Документ8 страницOccupational Therapy Marketing Indian Prospective SRJI Vol 2 Issue 3 Year 2013Dr. Krishna N. SharmaОценок пока нет
- Ito Test: Does Height of The Pad Affect Back Muscle Endurance?Документ7 страницIto Test: Does Height of The Pad Affect Back Muscle Endurance?Dr. Krishna N. SharmaОценок пока нет
- Scientific Research Journal of India SRJI Complete Vol-1 2012 All IssuesДокумент233 страницыScientific Research Journal of India SRJI Complete Vol-1 2012 All IssuesDr. Krishna N. SharmaОценок пока нет
- Evidence of Barriers To Evidence-Based Physiotherapy Practice in Northern AfricaДокумент5 страницEvidence of Barriers To Evidence-Based Physiotherapy Practice in Northern AfricaDr. Krishna N. SharmaОценок пока нет
- Mayank Pushkar. Congenital Talipes Equinovarus (CTEV) SRJI Vol - 2, Issue - 1, Year - 2013Документ7 страницMayank Pushkar. Congenital Talipes Equinovarus (CTEV) SRJI Vol - 2, Issue - 1, Year - 2013Dr. Krishna N. SharmaОценок пока нет
- Respiratory Physiotherapy in Triple Vessel Disease With Post Coronary Artery Bypass Grafting Surgery (CABG) SRJI Vol 2 Issue 3 Year 2013Документ4 страницыRespiratory Physiotherapy in Triple Vessel Disease With Post Coronary Artery Bypass Grafting Surgery (CABG) SRJI Vol 2 Issue 3 Year 2013Dr. Krishna N. SharmaОценок пока нет
- Physiotherapy Intervention in Management of Dizziness: Shahanawaz SDДокумент11 страницPhysiotherapy Intervention in Management of Dizziness: Shahanawaz SDDr. Krishna N. SharmaОценок пока нет
- Parmar Sanjay T., Nayana A. Khobre. Growth in Cerebral Palsy Children Between 3-13 Years in Urban Dharwad, IndiaДокумент7 страницParmar Sanjay T., Nayana A. Khobre. Growth in Cerebral Palsy Children Between 3-13 Years in Urban Dharwad, IndiaDr. Krishna N. SharmaОценок пока нет
- Pranjal Parmar. Comparison of The Effect of Isometric Exercise of Upper Limb On Vitals Between Young Males and FemalesДокумент13 страницPranjal Parmar. Comparison of The Effect of Isometric Exercise of Upper Limb On Vitals Between Young Males and FemalesDr. Krishna N. SharmaОценок пока нет
- Evidence of Barriers To Evidence-Based Physiotherapy Practice in Nothern AfricaДокумент7 страницEvidence of Barriers To Evidence-Based Physiotherapy Practice in Nothern AfricaDr. Krishna N. SharmaОценок пока нет
- Network Border Patrol Eradicates The Over Loading of Data Packets and Prevents Congestion Collapse Thereby Promoting Fairness Over TCP Protocol in LAN WAN SRJI Vol-1 Issue-1 Year-2013Документ10 страницNetwork Border Patrol Eradicates The Over Loading of Data Packets and Prevents Congestion Collapse Thereby Promoting Fairness Over TCP Protocol in LAN WAN SRJI Vol-1 Issue-1 Year-2013Dr. Krishna N. SharmaОценок пока нет
- Impact of Ageing On Depression and Activities of Daily Livings in Normal Elderly Subjects Living in Old Age Homes and Communities of Kanpur, U.PДокумент8 страницImpact of Ageing On Depression and Activities of Daily Livings in Normal Elderly Subjects Living in Old Age Homes and Communities of Kanpur, U.PDr. Krishna N. SharmaОценок пока нет
- Effectiveness of Conventional Physical Therapy & C.P.M Unit For Functional Rehabilitation After Total Knee ArthroplastyДокумент21 страницаEffectiveness of Conventional Physical Therapy & C.P.M Unit For Functional Rehabilitation After Total Knee ArthroplastyDr. Krishna N. SharmaОценок пока нет
- Exploring The Roots of ElectrotherapyДокумент4 страницыExploring The Roots of ElectrotherapyDr. Krishna N. SharmaОценок пока нет
- Full Journal SRJI Volume-1 Issue-3 Year-2012 Scientific Research Journal of IndiaДокумент81 страницаFull Journal SRJI Volume-1 Issue-3 Year-2012 Scientific Research Journal of IndiaDr. Krishna N. SharmaОценок пока нет
- Effectiveness of Supervised Graded Repetitive Arm Supplementary Program On Arm Function in Subjects With StrokeДокумент10 страницEffectiveness of Supervised Graded Repetitive Arm Supplementary Program On Arm Function in Subjects With StrokeDr. Krishna N. SharmaОценок пока нет
- Efficacy of 3D Gliding On Pain in Patients With Knee Osteoarthritis A Randomized Controlled Pilot StudyДокумент5 страницEfficacy of 3D Gliding On Pain in Patients With Knee Osteoarthritis A Randomized Controlled Pilot StudyDr. Krishna N. SharmaОценок пока нет
- Ethical Challenges For Occupational Therapist in India To Use Social MediaДокумент6 страницEthical Challenges For Occupational Therapist in India To Use Social MediaDr. Krishna N. SharmaОценок пока нет
- Efficacy of Retrowalking in Patients With Chronic Knee Osteoarthritis: A Single Group Experimental Pilot StudyДокумент9 страницEfficacy of Retrowalking in Patients With Chronic Knee Osteoarthritis: A Single Group Experimental Pilot StudyDr. Krishna N. SharmaОценок пока нет
- Effects of Task Related Sitting Training On Balance in Hemiplegic Patients. Dr. Vivek H. Ramanandi Srji Vol 1 Issue 4 Year 2013Документ9 страницEffects of Task Related Sitting Training On Balance in Hemiplegic Patients. Dr. Vivek H. Ramanandi Srji Vol 1 Issue 4 Year 2013Dr. Krishna N. SharmaОценок пока нет
- Effectiveness of Core Strengthening Exercises To Reduce Incidence of Side Strain Injury in Medium Pace BowlersДокумент12 страницEffectiveness of Core Strengthening Exercises To Reduce Incidence of Side Strain Injury in Medium Pace BowlersDr. Krishna N. SharmaОценок пока нет
- Effects of Bimanual Functional Practice Training On Functional Performance of Upper Extremity in Chronic Stroke SRJI Vol 2 Issue 3 Year 2013Документ10 страницEffects of Bimanual Functional Practice Training On Functional Performance of Upper Extremity in Chronic Stroke SRJI Vol 2 Issue 3 Year 2013Dr. Krishna N. SharmaОценок пока нет
- Effect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainДокумент8 страницEffect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainDr. Krishna N. SharmaОценок пока нет
- Effectiveness of Neuromotor Task Training Combined With Kinaesthetic Training in Children With Developmental Co - Ordination Disorder - A Randomised Trial SRJI Vol-1 Issue-1 Year-2013Документ15 страницEffectiveness of Neuromotor Task Training Combined With Kinaesthetic Training in Children With Developmental Co - Ordination Disorder - A Randomised Trial SRJI Vol-1 Issue-1 Year-2013Dr. Krishna N. SharmaОценок пока нет
- Editorial Vol 1 Issue 2. (Scientific Research Journal of India)Документ2 страницыEditorial Vol 1 Issue 2. (Scientific Research Journal of India)Dr. Krishna N. SharmaОценок пока нет
- Editorial Srji Vol 3 Issue 2 Year 2014Документ1 страницаEditorial Srji Vol 3 Issue 2 Year 2014Dr. Krishna N. SharmaОценок пока нет
- EditorialДокумент1 страницаEditorialDr. Krishna N. SharmaОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Common Illnesses in Family PracticeДокумент234 страницыCommon Illnesses in Family Practicetmle100% (2)
- Bahasa Inggris Massage BesokДокумент17 страницBahasa Inggris Massage Besokagus suadnyanaОценок пока нет
- ButorphanolДокумент3 страницыButorphanolMaine ʚĩɞОценок пока нет
- Evans 2012 - Osteopathic Principles-More Harm Than GoodДокумент8 страницEvans 2012 - Osteopathic Principles-More Harm Than GoodFraser RitchieОценок пока нет
- Health Assessment of The Patient ParagraphdДокумент23 страницыHealth Assessment of The Patient ParagraphdAmos TalsandekarОценок пока нет
- Analgesia and Anesthesia in Labor and DeliveryДокумент52 страницыAnalgesia and Anesthesia in Labor and DeliveryAnggri Septyan100% (1)
- ViswachiДокумент31 страницаViswachiHARIKRISHNAN RОценок пока нет
- NursingCareAfterKidneyTransplantCaseReport PDFДокумент7 страницNursingCareAfterKidneyTransplantCaseReport PDFJohn Louie SolitarioОценок пока нет
- Rheumatoid Arthritis Nursing Care Plan PDFДокумент3 страницыRheumatoid Arthritis Nursing Care Plan PDFIzhra MargateОценок пока нет
- Differentiating Trigeminal Neuropathy From Trigeminal NeuralgiaДокумент11 страницDifferentiating Trigeminal Neuropathy From Trigeminal NeuralgiaGarryОценок пока нет
- Nursing Care Plan: Chronic Pain and COPDДокумент11 страницNursing Care Plan: Chronic Pain and COPDneuronurse100% (1)
- Sensory ExaminationДокумент4 страницыSensory ExaminationAthena BorjaОценок пока нет
- Nash Leaders in TyphoidДокумент25 страницNash Leaders in TyphoidhompatОценок пока нет
- Dr. Firas Arnaout FRCS - Concise Orthopaedic Notes - Revision Aid For FRCS, EBOT, SICOT and Board Examinations-Independently Published (2020) PDFДокумент752 страницыDr. Firas Arnaout FRCS - Concise Orthopaedic Notes - Revision Aid For FRCS, EBOT, SICOT and Board Examinations-Independently Published (2020) PDFMokhlis Eissa100% (2)
- The Different Types of Electrotherapy DevicesДокумент4 страницыThe Different Types of Electrotherapy DevicescassianohcОценок пока нет
- NNGN3780 ClinicalДокумент26 страницNNGN3780 ClinicalErica Dianne VelasquezОценок пока нет
- Visudyne (Verteporfin For Injection) : Adverse Reactions (6) )Документ2 страницыVisudyne (Verteporfin For Injection) : Adverse Reactions (6) )Upik MoritaОценок пока нет
- BIO MAT TESTIMONIALS - Doc0001Документ30 страницBIO MAT TESTIMONIALS - Doc0001Nicole WeatherleyОценок пока нет
- Homeopathy First Aid RemediesДокумент91 страницаHomeopathy First Aid Remedieskasradin4791% (22)
- Psy 201 Midterm 2 Study GuideДокумент13 страницPsy 201 Midterm 2 Study GuideblahОценок пока нет
- Acupuncture For Musculoskeletal MedicineДокумент184 страницыAcupuncture For Musculoskeletal Medicinemec17100% (3)
- Articole TargetsДокумент77 страницArticole TargetspelinОценок пока нет
- Nursing Diagnosis and Intervention Goals for Pain ManagementДокумент2 страницыNursing Diagnosis and Intervention Goals for Pain ManagementMelona U. C MacinasОценок пока нет
- 2-Homeopathic Treatment of Cancer. Dr. KlinkenbergДокумент12 страниц2-Homeopathic Treatment of Cancer. Dr. KlinkenbergHomoeopath Aamir Saleem100% (3)
- Pain Scale 1-10 GuideДокумент3 страницыPain Scale 1-10 GuideAthena Irish LastimosaОценок пока нет
- Oet Wrıtıng Brıtısh Academy 01 315 376 With AnswerДокумент62 страницыOet Wrıtıng Brıtısh Academy 01 315 376 With Answersaramma mathewОценок пока нет
- DapusДокумент3 страницыDapusDanial AhmadОценок пока нет
- Neuro-Associative Conditioning: Programing Your Trading Mind'Документ21 страницаNeuro-Associative Conditioning: Programing Your Trading Mind'ediОценок пока нет
- Effectiveness of Skin Tap Technique On Level of Pain During IM Injection Among Adult Clients in Orthopaedic Wards at HSK Hospital and Research Centre Bagalkot, KarnatakaДокумент9 страницEffectiveness of Skin Tap Technique On Level of Pain During IM Injection Among Adult Clients in Orthopaedic Wards at HSK Hospital and Research Centre Bagalkot, KarnatakaInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Effect of Foot Strengthening Exercises in Osteoarthritis KneeДокумент5 страницEffect of Foot Strengthening Exercises in Osteoarthritis KneefiaОценок пока нет