Академический Документы
Профессиональный Документы
Культура Документы
The Utilization of Six Sigma and Statistical Process Control Techniques
Загружено:
drustagiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Utilization of Six Sigma and Statistical Process Control Techniques
Загружено:
drustagiАвторское право:
Доступные форматы
18
Journal for Healthcare Quality
The Utilization of Six Sigma and Statistical Process Control Techniques in Surgical Quality Improvement
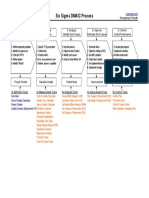
Jeffrey D. Sedlack Abstract: Surgeons have been slow to incorporate industrial reliability techniques. Process control methods were applied to surgeon waiting time between cases, and to length of stay (LOS) after colon surgery. Waiting times between surgeries were evaluated by auditing the operating room records of a single hospital over a 1-month period. The medical records of 628 patients undergoing colon surgery over a 5-year period were reviewed. The average surgeon wait time between cases was 53 min, and the busiest surgeon spent 29 1 2 hr in 1 month waiting between surgeries. Process control charting demonstrated poor overall control of the room turnover process. Average LOS after colon resection also demonstrated very poor control. Mean LOS was 10 days. Weibulls conditional analysis revealed a conditional LOS of 9.83 days. Serious process management problems were identified in both analyses. These process issues are both expensive and adversely affect the quality of service offered by the institution. Process control mechanisms were suggested or implemented to improve these surgical processes. Industrial reliability and quality management tools can easily and effectively identify process control problems that occur on surgical services. variance that occurs in any process. The techniques of Six Sigma management have only recently been applied to surgical quality improvement, and generally in single procedure high volume programs, such as for coronary artery bypass grafting. The cornerstone of Six Sigma is process management. This process management is accomplished using a five step technique known as DMAICDefine, Measure, Analyze, Improve, Control, which is based upon the scientific method, and heavily utilizes statistical analysis to determine causes of, and controls for, sources of variance within the overall process. The mainstay of this effort is referred to as statistical process control (Kumar & Steinebach, 2008; Shukla, Barreto, & Nadkarni, 2008). The techniques of statistical process control take the outcome of a process, and evaluate the effectiveness of that process in meeting a goal with as little variance as possible, while remembering that variability is inevitable. The steps involved require finding a measurable output, collecting the data, determining the statistical distribution for accurate analysis, then discovering the mean and degree of variation by determining control limits for the process, which, under Six Sigma, are the means, plus or minus three standard deviations (because Six Sigma refers to having process output within a span of six standard deviations, and quality improvement is reducing the standard deviation; Pyzdek, 2003). Another technique of reliability analysis of potential utility, particularly in the setting of a poorly controlled process, is the conditional statistic. These have been used in both medicine and surgery (Lorch et al., 2004; Silber et al., 2005, 2001) to identify process problems using length of stay (LOS) data. With this tool, the conditional LOS is determined, which is defined as that time at which a patient is as likely to stay in the hospital as to go home. The determination of conditional statistic is done using the Weibull distribution (Corporation, 2005), which is a refinement of the Hollander
Keywords
conditional length of stay quality improvement Six Sigma surgical Statistical Process Control
Journal for Healthcare Quality Vol. 32, No. 6, pp. 1826 & 2010 National Association for Healthcare Quality
Industrial and manufacturing concerns have long controlled and improved quality through rigorous identification of process, and then statistical control of the identified process (Gamm, Kash, & Bolin, 2007; Levett & Carey, 1999; Pyzdek, 2003). The overall goal of this mechanism is to identify, control, and reduce causes of variation within a given industrial process or system (Atkinson, 1994). Further modifications of these efforts to control variation include Six Sigma (attempting to reduce errors or defects to 3.4 per million opportunities), LEAN (attempting to identify and reduce system waste), Failure Modes Effects Analysis(identifying the likelihood and significance of potential errors in a process), and Statistical Process Control (statistical evaluation of outcomes, identification of statistical outliers, and defects analysis of the outliers to improve overall control over a process; Atkinson, 1994; Lagasse et al., 1995). Six Sigma in industrial quality control and improvement is a bottom line oriented, data driven approach to controlling the natural
Journal for Healthcare Quality
Vol. 32 No. 6 November/December 2010
19
Proschan statistic used for reliability and warranty determinations in industry. It has been shown effective to use LOS greater than the conditional LOS as a marker for complications. Each of these quality improvement tools offers a perspective on any process, and with that perspective an opportunity to improve outcomes. These tools have, for a variety of reasons, been little used in the care of surgical patients (Atkinson, 1994; Moorman, 2005). A leading argument against the application of rigorous industrial process control mechanisms in surgical patients is the overall complexity of the human system, with dynamic ever-changing systems. Other issues include surgeon autonomy, lack of institutional commitment, the difficulty of establishing a rigorous quality program in a complex organization such as a hospital, and lack of Six Sigma trained personnel (Atkinson, 1994; Gallstones and Laparoscopic Cholecystectomy, 1992). That said, given the report of the Institute of Medicine on error rates in American hospitals (Havens & Boroughs, 2000), and the expenses associated with medical malpractice litigation in the United States, the high Costs of Poor Quality, in healthcare demonstrate a serious need to apply serious controls to reduce errors and variance. As a vivid example of how we, as surgeons, are accepting of a failure rate that would be unacceptable in any other endeavor, the National Institute of Health consensus conference in 1992 (National Institutes of Health Consensus Development Conference Statement on Gallstones and Laparoscopic Cholecystectomy, 1993) identified seven critical steps to the identification of the common bile duct during laparoscopic cholecystectomy. The surgical literature reports an incidence of bile duct injury during laparoscopic cholecystectomy of 1 per 1,500 surgeries (Khan et al., 2007). The current process of laparoscopic cholecystectomy therefore yields 95 defects per million opportunities (DPMO), and is operating at 5.25 sigma. Flying an airplane is also a system that has great variability such as weather, passenger weight, etc. A good rate of surgical mishap DPMO of 95 applied to airlines would result in approximately 20 commercial airline crashes per day in the United States. Six Sigma processes strive for a defect per million opportunities rate of 3.4 per million opportunities (Pyzdek, 2003). The airlines exceed
this rate. Our bile duct injury rate should be 1 per 45,000 surgeries. We must do better. Fortunately, modern process analysis and management methods can offer significant assistance in identifying and improving surgical processes. This study applies two such tools, Six Sigma and Statistical Process Control, to identify areas for potential quality improvement.
Study Design
In order to demonstrate the utility of Six Sigma and Statistical Process Control methodologies in the surgical setting, two areas were examined.
Surgeon Waiting Times
An evaluation of the process of utilizing operating rooms in one hospital was evaluated. The operating room logs of a single hospital were evaluated over the 1-month period of July 2006. The surgeon waiting times were calculated for each surgeon between consecutive scheduled cases. This time was calculated from the procedure end time to the next procedure start time in the operative logs. Total surgeon waiting time, and individual surgeon waiting times for the month were calculated, as was the cost of this lost time.
LOS After Colon Surgery
Outcomes for colon surgery at this institution were also evaluated. LOS has been used as an overall measure of quality of a process in several prior studies (Fry et al., 2009). The busiest general surgeons in this institution were surveyed as to their impression of the average LOS following the most commonly performed types of colon resection. The estimated averages conformed to the surgical literature as to average LOS reported for the various colon procedures. The LOS data were obtained from the hospital-computerized database for all colon surgery over the 5-year period from October 1, 2003 to November 30, 2008. The mean LOS and standard deviations were determined for all colon surgery patients combined and for several localized procedures by procedure code. In both cases, statistical process controls were developed after statistical analysis of the data to determine the nature of each individual distribution. In both cases, the data were analyzed using the industrial reliability/quality
20
Journal for Healthcare Quality
statistical software Weibull11s (Reliasoft Corporation&, Tucson, AZ, 2006).
Results
Surgeon waiting time: the operating room records and schedules for 1 month, July 2006, were reviewed. This midsized community teaching hospital has 14 functioning operating rooms. The schedules were reviewed for instances of consecutive scheduled cases for individual surgeons. There were 283 such instances during that month. The operating room logs were then examined to determine procedure stop timethat is when the surgeon completed one case, and the next procedure start timethat is the surgeon made the incision on the next case. The difference in these times was the surgeon wait timeor time between completing one surgery and starting another. We also calculated the efficiency use of surgeon time as a percentage of time spent actually operating versus total time spent that day in the operating room. The curve fit histogram of operating room waiting times is shown in Figure 1. Statistical analysis of the distribution showed best fit with a g or Erlangs distribution, rather than a normal distribution because of the leftward skew of the data. Interestingly, the Erlang curve is used for queuing statistics, which, appropriately, is really what this waiting time represents. With this g distribution, there was a mean wait time of 51.35 min (s18.71 min). Assuming a
normal distribution, the mean was 51.92 min, with a s of 19.52 min, which was not significantly different. Wait times were totaled for each surgeon for the entire month. The data are summarized for the five busiest surgeons in Table 1. In 1 month, the busiest surgeon in the hospital spent 1,769 min (29 hr, 29 min) waiting for his next scheduled case to start, and, only 53.5% of the time spent in the operating rooms for scheduled cases was actually performing surgery. For the entire operating room, total waiting time in 1 month was 19,679 min (331 hr, 19 min), representing significant lost productivity, both for the surgeon and for the hospital. Statistical process control charts were then constructed using an upper control limit of 107.48 min. The upper control limit is defined as the mean plus three standard deviations. This process control chart is shown in Figure 2, which demonstrates that there were only four instances in which there were special or unusual causes of variance at play. The fact that the upper control limit is so high, suggests that the process is out of control, that the standard deviation of the data is excessively long; there are excessive common causes of variance, leading to a very prolonged and unpredictable wait between scheduled surgeries.
Colon Surgery LOS
A total of 628 patients underwent colon resection in one institution over the 5-year period
Figure 1. Surgeon Waiting Times Histogram
F/S Histogram
0.030
0.024
0.018 Value 0.012 0.006 0.000
Period
Vol. 32 No. 6 November/December 2010
21
Table 1. Surgeon Waiting Times Between Scheduled, Consecutive CasesThe Five Busiest Surgeons
# Cases 40 34 30 28 25 Average Wait Time (min) 51.85 68.64 59.2 57 43.38 Standard Deviation 34.38 9.66 18.68 25.81 11.13 Total Minutes Operating 2,038 2,658 1,829 1,176 812 Total OR (min) 3,807 4,547 3,287 2,537 1,882 OR Efficiency 53.5 58.5 55.6 46.4 43.1 Nonproductive (min) 1,769 1,889 1,458 1,361 1,070
Surgeon A B C D E
from October 1, 2003 to November 30, 2008. The five surgeons performing the majority of the colon surgeries at this institution were also polled as to their best estimate of average LOS after colon surgery of various types, before their knowledge of data from this study. These survey data are summarized in Table 2. The LOS data of the patient set was then studied both as a group and by procedure using the tools of statistical process analysis. For each procedure, the LOS histograms were developed with curve analysis. The representative histogram for right colectomy is shown as Figure 3. In this case, the data more clearly show the leftward skew of LOS data, and distribution analysis again best fit with the g or Erlangs distribution. In fact, for right hemicolectomy, mean and standard deviation calculated using the g distribution were 9.69 and 5.96 days, respectively, whereas under a normal distribution, they were 11.54 and 8.52 days, respec-
tively, and overall calculations for each procedure are summarized in Table 3. Statistical process control graphs were then constructed for each procedure. The representative graph for right colectomy is shown in Figure 4. The process of colectomy throughput is also out of statistical control at this institution based upon the large standard deviations, the longer than estimated mean LOS, and, because of the long standard deviation, the very high statistical upper control limit. Under the current process for colectomy, there is not a significant variance in LOS until the patient has stayed in the hospital for more than 4 weeks. The conditional LOS was also calculated for patients undergoing each type of colectomy using the Weibull/Hollander 5 Proschan statistic. The Weibull curve is calculated as the discharge rate as a percentage of the remaining patients. The conditional statistic is the
Figure 2. Process Control Chart for Surgeon Wait Times
22
Journal for Healthcare Quality
Table 2. Survey Results of Surgeon Perceived LOS after Colon Surgery, by Procedure
Estimated LOS After Colon Surgery Procedure A Total abdominal colectomy Abdominal perineal resection Open cecectomy Right colectomy Transverse colectomy Left hemicolectomy Sigmoid colectomy Low anterior resection
LOS, length of stay.
Surgeon B 8 10 4 5 6 6 5 5 C 6 7 6 6 6 7 7 7 D 7 7 6 6 6 7 7 7 E 7 8 4 5 5 6 6 7 Average 6.8 8 5.4 5.4 5.6 6.6 6.4 6.6
6 8 7 5 5 7 7 7
point at which the patient is as likely to continue in the hospital as to be discharged. The Weibull curve for right colectomy is shown as Figure 5, and the conditional LOS for each procedure is summarized in Table 4.
Discussion
These tools of statistical process control are very heavily utilized in industry, particularly in the field of reliability analysis (Corporation, 2005). Reliability analysis is used to determine everything from warranties, to whether an electronic part should be burned in before sale, or should be sold new. The author believes that
the tools of reliability analysis have direct application to surgery and to surgeons. The author applied Six Sigma and Statistical Process Control methodologies to two distinct areas of concern for general surgeons: how effectively a surgeons time is used by the hospital, and how effectively colon surgery patients are managed by the care process at one hospital.
Surgeon Waiting Times
In the area of time utilization, the wait time between finishing one surgery and starting the next consecutive scheduled operation was evaluated. In a 1-month audit, a surgeon in this
Figure 3. Colon Surgery Length of Stay Histogram
F / S Histogram 0.070
0.056
0.042 Value 0.028 0.014 0.000 Period
Vol. 32 No. 6 November/December 2010
23
Table 3. Actual Patient Length of Stay after Colon Surgery, by Procedure
Procedure All colons Total abdominal colectomy Abdominal perineal resection Open cecectomy Right colectomy Transverse colectomy Left hemicolectomy Sigmoid colectomy Low anterior resection
UCL, upper control limit.
n 628 15 15 23 189 32 77 175 78
Mean 10.04 11.41 12.38 12.13 9.69 11.94 12.26 9.3 7.77
s 6.21 10.13 7.56 8.35 5.96 8.13 7.09 5.5 3.39
Process UCL 28 42 34 37 27 36 33 25 17
Success 603 15 14 23 178 36 74 169 71
Failure 25 0 1 0 11 0 3 6 7
institution spent an average of 51 min waiting to start the next scheduled procedure. There was also very wide variability in the data indicating that the process was not only prolonged, but that it was also under poor control. One busy general surgeon spent 29 1 2 hr waiting to operate in 1 month. Overall, this institution had 331 hr of nonproductive time between scheduled procedures, and surgeons in this institution spent 51% of their time in the operating room operating. From a financial standpoint, these findings are of concern. Operating room time in this institution is costs US$16/min. This finding represents wastage of US$314,864 in 1 month. In addition, as more surgeons are hospital employees, this wasted time is also expensive. For example, if all surgeons were employed at this institution, and the average surgeon is paid US$150/hr, then these data would also show
US$49,500 in wasted wages per month for employed surgeons. Finally, for surgeons in private practice who can choose what hospital at which to operate, there can be no excuse for a hospital causing a customer to their operating rooms to wait 29 hr a month in the physician lounge. Quality improvement for this particular process under Six Sigma methods calls for application of the DMAIC cycle, that is to define the process, to measure the outcomes at each step, to analyze and improve these steps in the process, and then to apply control mechanisms to allow for continued measurement and improvement. During the course of this analysis, the process mapping identified several steps required to successfully have a patient, anesthesia, OR staff, and surgeon in the room in a timely fashion. Problems were identified in the preparation of patients, which
Figure 4. Process Control Chart for Colon Surgery Length of Stay (LOS)
24
Journal for Healthcare Quality
Figure 5. Weibull Analysis of Colon Surgery Length of Stay
Probability - Weibull 99.000 90.000
50.000 Unreliability, F (t)
10.000 5.000
1.000 1.000
10.000 Time, (t)
100.000
led to delay, in the availability of surgeons, which led to delay, and, finally, in the utilization process for the operating rooms. There was a chokepoint identified in the system in that operating room availability, rather than staff or surgeon availability, was used as the rate-limiting step in this process. Several specific improvement suggestions for this process were then made, that included: (1) process improvements in patient preparation, including timely return of preoperative laboratories and consents, skin preparation and site identification in the holding area, and improved preoperative patient education; (2) a carrot and stick approach to surgeon availability. Improved waiting time results
in reduced wandering off by the surgeons. It was thought unreasonable to expect a surgeon waiting an average of 51 min between surgeries to spend that entire time waiting in the surgeon lounge. In addition, there was increased involvement of the surgeon in the preparation process in the holding area, again improving patient preparation effectiveness; (3) it was proposed that the traditional surgeon block scheduling time be eliminated, and instead, because there was excess operating room capacity in this facility, that surgeon and staff availability be used as the bottleneck, and that operating rooms be made available on an industrial just in time basis. This proposal has been under study at this institution.
Table 4. Analysis of Conditional Length of Stay (LOS) Statistic for Colon Surgery, by Procedure
Procedure All colons Total abdominal colectomy Abdominal perineal resection Open cecectomy Right colectomy Transverse colectomy Left hemicolectomy Sigmoid colectomy Low anterior resection Conditional LOS (days) 9.87 15.2 12.12 10.61 9.94 10.7 12.11 9.1 8.27
Vol. 32 No. 6 November/December 2010
25
Colon Surgery
Five years of colon surgery patients were then examined from this institution, and evaluated for LOS. It is important to note that LOS does not follow a normal distribution, but rather follows a g or Erlangs statistical distribution (Corporation, 2005). The mean and standard deviations of LOS are more accurately calculated using this distribution. Such distribution analysis can be easily performed using commercially available reliability analysis software, and should allow for more accurate comparison of data. The actual mean LOS (10.4 days) was significantly longer than was estimated by the surgeons (6.35 days), or that reported in the literature (7.25 days; Mahmoud et al., 2009). These data suggest that surgeon perception of performance is unrealistic, and that the process is poorly controlled. Statistical process controls then demonstrated that the process for colon surgery has wide variability and is under poor control. In fact, for most colon surgery in this institution, there is so much variability that the patient does not have a statistical problem using the typical statistical method of upper control limits (mean13s) until they have been in the hospital for more than 4 weeks. The conditional LOS was therefore used as a starting point for the evaluation of variance, and in the establishment of a statistically controlled process for the care and management of colon surgery patients in this institution. The average cost per day of hospitalization in this institution is US$1,147. The LOS statistics for this institution imply a 3.15 day average excess LOS, or US$3,614.05 wasted hospital cost per patient, or US$2,268,995.40 lost over this 5-year period as a result of excess LOS for colon surgery at this institution. Process analysis of colon surgery revealed several interesting findings. First, the institution does not have a fast track program, or designed, controlled process, for colon surgery. Fast track programs have been developed for colon surgery and reported from around the country (Ishiguro et al., 2008; Melbert et al., 2002; Uchiyama et al., 2002), and have been shown to be effective in reducing LOS (Dy et al., 2005). In reality, these fast track programs, or critical pathways, as they used to be called (Bradshaw, Liu, & Thirlby, 1998), are process maps designed to move a patient through a specific program of recovery after surgery.
The most effective of these care plans are institution specific, and tailored to the specific traits of an institution (Dy et al., 2005), but with control mechanisms in place, fast tracks represent a Six Sigma DMAIC-controlled process of care. This institution has not, to date, had a defined process for caring for colon surgery patients. Several quality improvement suggestions were made for this institution based upon these findings using Six Sigma DMAIC methodology: (1) process mapping should be done to define the current process of care for colon surgery at this institution; (2) a clinical pathway or fast track, should be established at this institution based upon current practices, and with development of effective measurement indices beyond LOS; (3) once these indices are developed, there should be rigorous education and dissemination of this information to process stakeholders, in order to eliminate the current disconnect between perceived and actual performance as shown with LOS; (4) There is currently no quality control monitoring mechanism for colon surgery at this institution. It was recommended that, because the current process is not under valid statistical control, that hospital stays in excess of conditional LOS statistic (9.67 days) be used as an automatic identifier for review of the care for complications.
Conclusion
This study examined the utility of Six Sigma methods of statistical process control in identification and management of two areas of surgical care. These methods were used to identify very prolonged waiting times with poor process control and inefficiency in utilization of surgeon time in the operating room, and to identify great variability in LOS after colon surgery in one institution that was remarkably at odds with the surgeons surveyed perceptions regarding this performance. Statistical process control, adopted from industry represents an effective, datadriven approach to quality improvement in surgery.
26
Journal for Healthcare Quality
References
Atkinson, S. (1994). Applications of statistical process control in health care. Managed Care Quarterly, 2, 5769. Bradshaw, B. G., Liu, S. S., & Thirlby, R. C. (1998). Standardized perioperative care protocols and reduced length of stay after colon surgery. Journal of the American College of Surgeons, 186, 501506. Corporation, R. (2005). Reliasoft life data analysis reference: Weibull117. Tuscon, AZ: Reliasoft Corporation. Dy, S. M., Garg, P., Nyberg, D., Dawson, P. B., Pronovost, P. J., Morlock, L., et al. (2005). Critical pathway effectiveness: Assessing the impact of patient, hospital care, and pathway characteristics using qualitative comparative analysis. Health Service Research, 40, 499516. Fry, D. E., Pine, M., Jones, B. L., & Melmban, R. J. (2009). Adverse outcomes in surgery: Redefinition of postoperative complications. American Journal of Surgery, 197, 479484. Gallstones and laparoscopic cholecystectomy. NIH Consensus Statement (1992) 10, 128. Gamm, L., Kash, B., & Bolin, J. (2007). Organizational technologies for transforming care: Measures and strategies for pursuit of IOM quality aims. Journal of Ambulatory Care Management, 30, 291301. Havens, D. H., & Boroughs, L. (2000). To err is human: A report from the Institute of Medicine. Journal of Pediatric Health Care, 14, 7780. Ishiguro, S., Yamamoto, S., Fujita, S., Akasu, T., Kobayashi, Y., & Moriya, Y. (2008). Effect of a clinical pathway after laparoscopic surgery for colorectal cancer. Hepatogastroenterology, 55, 13151319. Khan, M. H., Howard, T. J., Fogel, E. L., Sherman, S., Watkins, J. L., Canal, D. F., et al. (2007). Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: Experience at a large tertiary referral center. Gastrointestinal Endoscopy, 65, 247252. Kumar, S., & Steinebach, M. (2008). Eliminating US hospital medical errors. International Journal of Health Care Quality Assurance, 21, 444471. Lagasse, R. S., Steinberg, E. S., Katz, R. J., & Sauberman, A. J. (1995). Defining quality of perioperative care by statistical process control of adverse outcomes. Anesthesiology, 82, 11811188. Levett, J. M., & Carey, R. G. (1999). Measuring for improvement: From Toyota to thoracic surgery. Annals of Thoracic Surgery, 68, 353358; discussion 3746. Lorch, S. A., Zhang, X., Rosenbaum, P. R., Evan-Shoshan, O., & Silber, J. H. (2004). Equivalent lengths of stay of
pediatric patients hospitalized in rural and nonrural hospitals. Pediatrics, 114, e400e408. Mahmoud, N. N., Turpin, R. S., Yang, G., & Saunders, W. B. (2009). Impact of surgical site infections on length of stay and costs in selected colorectal procedures. Surgical Infection (Larchmt). Melbert, R. B., Kimmins, M. H., Isler, J. T., Billingham, R. P., Lawton, D., Salvadalena, G., et al. (2002). Use of a critical pathway for colon resections. Journal of Gastrointestinal Surgery, 6, 745752. Moorman, D. W. (2005). On the quest for Six Sigma. American Journal of Surgery, 189, 253258. National Institutes of Health Consensus Development Conference Statement on Gallstones and Laparoscopic Cholecystectomy. American Journal of Surgery (1993) 165, 390398. Pyzdek, T. (2003). The Six Sigma handbook (2nd ed.). New York, NY: McGraw Hill and Co. Shukla, P. J., Barreto, S. G., & Nadkarni, M. S. (2008). Application of Six Sigma towards improving surgical outcomes. Hepatogastroenterology, 55, 311314. Silber, J. H., Rosenbaum, P. R., Trudeau, M. E., EvenShoshan, O., Chen, W., Zhang, X., et al. (2001). Multivariate matching and bias reduction in the surgical outcomes study. Medical Care, 39, 10481064. Silber, J. H., Rosenbaum, P. R., Trudeau, M. E., Chen, W., Zhang, X., Kelz, R. R., et al. (2005). Changes in prognosis after the first postoperative complication. Medical Care, 43, 122131. Uchiyama, K., Takifuji, K., Tani, M., Onishi, H., & Yamaue, H. (2002). Effectiveness of the clinical pathway to decrease length of stay and cost for laparoscopic surgery. Surgical Endoscopy, 16, 15941597.
Authors Biography
Jeffrey D. Sedlack, MD, Department of General Surgery, The Belfast Group, 116 Northport Avenue, Belfast, ME 04915.
For more information on this article, contact Jeffrey D. Sedlack at jsedlack@wchi.com.
Вам также может понравиться
- APG Design and Development 2015Документ7 страницAPG Design and Development 2015John RajeshОценок пока нет
- Leanmap FREE Six Sigma Tool OverviewДокумент2 страницыLeanmap FREE Six Sigma Tool OverviewdrustagiОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- SDC Course OutlineДокумент3 страницыSDC Course OutlinedrustagiОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- New Blank TemplateДокумент11 страницNew Blank TemplateAmine MoutaqiОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Lean Vs Six SigmaДокумент23 страницыLean Vs Six SigmaSiddharth ChakkarwarОценок пока нет
- Scrum Master Certification (SMC™) Course OutlineДокумент1 страницаScrum Master Certification (SMC™) Course OutlinedrustagiОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Appreciation Cards v.1.0Документ2 страницыAppreciation Cards v.1.0drustagiОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Top Questions Asked About SAFe ExamsДокумент2 страницыTop Questions Asked About SAFe ExamsdrustagiОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Create the future storyboardДокумент1 страницаCreate the future storyboarddrustagiОценок пока нет
- SMC Class ScheduleДокумент1 страницаSMC Class ScheduledrustagiОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Agile Scrum at Glance BaselineДокумент1 страницаAgile Scrum at Glance BaselinedrustagiОценок пока нет
- Six Sigma Fact SheetДокумент4 страницыSix Sigma Fact SheetMarcus Skookumchuck VanniniОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Change Log TemplateДокумент3 страницыChange Log TemplatedrustagiОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Permanent Change and Temporary Deviation Request FormДокумент1 страницаPermanent Change and Temporary Deviation Request FormdrustagiОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Set Project Priorities - ToCДокумент4 страницыSet Project Priorities - ToCdrustagiОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- 6 Six Sigma Roadmap RevДокумент20 страниц6 Six Sigma Roadmap RevJuan PabloОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Updated Agile - KanbanДокумент25 страницUpdated Agile - Kanbandrustagi100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Leanmap FREE Six Sigma DMAIC ProcessДокумент1 страницаLeanmap FREE Six Sigma DMAIC ProcessdrustagiОценок пока нет
- A Solution Template To Help in Hypothesis TestingДокумент3 страницыA Solution Template To Help in Hypothesis TestingdrustagiОценок пока нет
- MAW KitДокумент3 страницыMAW KitdrustagiОценок пока нет
- PDSA History Ron MoenДокумент9 страницPDSA History Ron MoenAli Shah100% (1)
- FBD, Fmea, ParetoДокумент5 страницFBD, Fmea, ParetodrustagiОценок пока нет
- Quality Management Gurus TheoriesДокумент6 страницQuality Management Gurus TheoriesSyafiqah RedzwanОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- A Solution Template To Help in Hypothesis TestingДокумент3 страницыA Solution Template To Help in Hypothesis TestingdrustagiОценок пока нет
- PDSA History Ron MoenДокумент9 страницPDSA History Ron MoenAli Shah100% (1)
- The Benefits of PDCAДокумент2 страницыThe Benefits of PDCAdrustagiОценок пока нет
- Quality Management Gurus TheoriesДокумент6 страницQuality Management Gurus TheoriesSyafiqah RedzwanОценок пока нет
- Sample Chartered Accountant ResumeДокумент5 страницSample Chartered Accountant ResumedrustagiОценок пока нет
- Who Are The TOP Quality GurusДокумент8 страницWho Are The TOP Quality GurusdrustagiОценок пока нет
- Chartered Accountant Resume Sample - Best FormatДокумент4 страницыChartered Accountant Resume Sample - Best FormatdrustagiОценок пока нет
- Harrington JMP Working RemotelyДокумент83 страницыHarrington JMP Working RemotelyCEO CEOОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- PMV TrainingДокумент8 страницPMV TrainingBill BriegerОценок пока нет
- Religious Attendance, Spirituality, and Major Depression in Canada: A14-Year Follow-Up StudyДокумент9 страницReligious Attendance, Spirituality, and Major Depression in Canada: A14-Year Follow-Up StudyCatarina C.Оценок пока нет
- CDM Sample Resume 1Документ4 страницыCDM Sample Resume 1Rahul SОценок пока нет
- Understanding Randomised Controlled TrialsДокумент5 страницUnderstanding Randomised Controlled TrialsWafiy AkmalОценок пока нет
- Template Consent FormДокумент5 страницTemplate Consent FormAlexandru ComanОценок пока нет
- Detectionof Cotton Plant DiseseДокумент20 страницDetectionof Cotton Plant DiseseAdarsh ChauhanОценок пока нет
- Laplace Transforms PDFДокумент32 страницыLaplace Transforms PDFShubham GuptaОценок пока нет
- Quiz 2Документ22 страницыQuiz 2araceliОценок пока нет
- Brownsville Learn Phase ReportДокумент28 страницBrownsville Learn Phase ReportJennifer LeeОценок пока нет
- Scope of Agriculture ExtensionДокумент3 страницыScope of Agriculture Extensionhasnain183533Оценок пока нет
- Mitchell and Jolley-Research Design Explained-359-381Документ23 страницыMitchell and Jolley-Research Design Explained-359-381Gaby Fitria BahriОценок пока нет
- IBM Big Data and Analytics PDFДокумент24 страницыIBM Big Data and Analytics PDFSameer ParadkarОценок пока нет
- Breadth RequirementsДокумент2 страницыBreadth RequirementsJulian ChoОценок пока нет
- VDCA Guideline SrilankaДокумент31 страницаVDCA Guideline SrilankaVinay PathakОценок пока нет
- Charotar University of Science & Technology (Charusat) Research Scholar's Progress Report Review FormДокумент4 страницыCharotar University of Science & Technology (Charusat) Research Scholar's Progress Report Review Formmanali_thakarОценок пока нет
- Hoyos y Narayan. (2011)Документ25 страницHoyos y Narayan. (2011)yelida blancoОценок пока нет
- Lesson 3 Lab ManagementДокумент17 страницLesson 3 Lab ManagementSAMUEL REYESОценок пока нет
- Activity For Central TendencyДокумент3 страницыActivity For Central TendencyJessel TagalogОценок пока нет
- F&B Waste Management QuestionnaireДокумент3 страницыF&B Waste Management QuestionnairePranav Kakà Harmilapi70% (27)
- Enterprise Agility: Buzz or Business Impact?Документ19 страницEnterprise Agility: Buzz or Business Impact?Melissa Salaverry CamposОценок пока нет
- Sucrose Gradient Separation ProtocolДокумент16 страницSucrose Gradient Separation ProtocolBalaОценок пока нет
- Research Paper FinalДокумент45 страницResearch Paper FinalEricson B. PetagaraОценок пока нет
- Fyp BriefingДокумент12 страницFyp BriefingsalahОценок пока нет
- Anyanwu & Amaechi-Chijioke, 2022Документ5 страницAnyanwu & Amaechi-Chijioke, 2022Mohamed hanyfouadОценок пока нет
- Jane DissertationДокумент147 страницJane DissertationAsdasОценок пока нет
- Louis de Vorsey (1978) Amerindian Contributions To The Mapping of North AmericaДокумент9 страницLouis de Vorsey (1978) Amerindian Contributions To The Mapping of North AmericatiagokramerОценок пока нет
- Sciencensw4 ch00Документ9 страницSciencensw4 ch00ryan.mundanmany58Оценок пока нет
- Exploring Space Project MercuryДокумент16 страницExploring Space Project MercuryBob Andrepont100% (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesОт EverandThe Ultimate Guide To Memory Improvement TechniquesРейтинг: 5 из 5 звезд5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementОт EverandTechniques Exercises And Tricks For Memory ImprovementРейтинг: 4.5 из 5 звезд4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОценок пока нет