Академический Документы
Профессиональный Документы
Культура Документы
Current Concepts in Topical Therapy For Chronic Sinonasal PDF
Загружено:
yosi93Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Current Concepts in Topical Therapy For Chronic Sinonasal PDF
Загружено:
yosi93Авторское право:
Доступные форматы
REVIEW ARTICLE
Current Concepts in Topical Therapy for Chronic Sinonasal Disease
Richard J. Harvey, MD, Alkis Psaltis, MD, Rodney J. Schlosser, MD, and Ian J. Witterick, MD
ABSTRACT Introduction: There has been an explosion in the understanding of the mechanisms of chronic sinonasal inflammation. Multiple approaches to control and modify the inflammatory reaction in chronic rhinosinusitis have led to many new agents being introduced topically to the sinonasal cavities. This article aims to provide an evidence-based approach to the science behind topical management of sinonasal disease. Methods: The literature on delivery device, position, surgical state, and pharmaceutical and mechanical concepts of topical therapy to the paranasal sinuses is reviewed. Results: High-volume irrigation under positive pressure and in head-down positions is important for effective delivery and mechanical action of topical solutions. Unoperated paranasal sinuses appear to receive very limited topical therapy. Enhanced steroid therapy and surfactants appear to be the most promising pharmaceutical approaches. Future novel therapies may include enhancers of the innate immune system. The effect of antibiotic additives is difficult to establish as this might be treating a diseasemodifying state rather than the underlying pathology. Conclusions: Topical therapies, applied after surgery, are likely to represent the mainstay of future management for chronic inflammatory rhinosinusitis. SOMMAIRE Introduction: La compre hension des me canismes de linflammation nasosinusale chronique a fait des pas de ge ant. De nombreuses recherches visant a ` limiter et a ` modifier la re action inflammatoire dans la rhinosinusite chronique ont mene a ` le laboration de nombreux nouveaux agents a ` application topique dans les cavite s nasosinusales. Larticle vise a ` pre senter une approche fonde e sur des donne es probantes, a ` la science qui sous-tend le traitement topique des affections nasosinusales. Me thode: Nous avons passe en revue la documentation sur les dispositifs dadministration, la position de la te te, le tat du traitement chirurgical ainsi que les principes pharmaceutiques et me caniques du traitement topique des affections des sinus paranasaux. Re sultats: Une irrigation a ` grand volume, sous pression positive, et la te te en position de clive sont des facteurs importants dune administration efficace et de laction me canique des solutions topiques. Il semble que les sinus paranasaux non ope re s soient tre `s peu soumis au traitement topique. Lame lioration du traitement par les ste ro des et les agents de surface seraient les deux voies les plus prometteuses de la pharmacothe rapie. Les nouveaux traitements pourraient comprendre des stimulateurs du syste ` me immunitaire naturel. Enfin, leffet de ladjonction dantibiotiques est difficile a ` e valuer e tant donne que ces me dicaments pourraient agir sur un e tat modifiant le volution de la maladie pluto t que sur laffection sous-jacente. Conclusions: Les traitements topiques postope ratoires constitueront probablement, a ` lavenir, la clef de vou te de la prise en charge de la rhinosinusite inflammatoire chronique. Key words: antibiotic, biofilm, endoscopic sinus surgery, irrigation, sinusitis, steroid, surfactant, topical
Richard J. Harvey: Department of Otolaryngology/Skull Base Surgery, St Vincents Hospital, Darlinghurst, Sydney, NSW, Australia, and Department of OtolaryngologyHead and Neck Surgery, Royal Adelaide Hospital, Adelaide, SA, Australia; Alkis Psaltis: Department of OtolaryngologyHead and Neck Surgery, Royal Adelaide Hospital, Adelaide, SA, Australia; Rodney J. Schlosser: Department of OtolaryngologyHead and Neck Surgery, Medical University of South Carolina, Charleston, South Carolina; Ian J. Witterick: Department of Otolaryngology-Head and Neck Surgery, University of Toronto, Toronto, Ontario.
Address reprint requests to: Richard J. Harvey, MD, Department of Otolaryngology/Skull Base Surgery, St Vincents Hospital, Victoria Street, Darlinghurst, Sydney, NSW 2010, Australia; e-mail: richard@ richardharvey.com.au.
DOI 10.2310/7070.2009.090161
# 2010 The Canadian Society of Otolaryngology-Head & Neck Surgery
Journal of Otolaryngology-Head & Neck Surgery, Vol 39, No 3 (June), 2010: pp 217231
217
218
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
here has been a recent explosion in the understanding of the mechanisms of chronic sinonasal inflammation. Multiple approaches to control and modify the inflammatory reaction in chronic rhinosinusitis (CRS) have led to many new agents being introduced topically to the sinonasal mucosa. Current research into irrigation dynamics and delivery device has expanded over the past 3 years. A range of products have become available to deliver solutions topically to the nose (Table 1). There is a scientific basis behind topical delivery; however, it is often obscured by marketing information and commercial interests. Distribution research behind nebulizers, sprays, irrigations, and other delivery techniques has been performed. The general therapeutic goal of topical management may lie between potentially competing actions of mechanical and pharmaceutical intervention. The mechanical removal of mucus, antigen, pollutants, inflammatory products, and bacteria/biofilms is often targeted with topical approaches. These interventions often rely on highvolume positive pressure solutions to provide shearing forces with additives to alter air surface liquid (ASL) tension. However, the same approach may not be appropriate for delivery of pharmaceutical preparations. Complete sinus distribution, long mucosal contact time with local absorption, and minimal wastage are common desired properties. The over-the-counter (OTC) market for topical sinonasal treatments is likely to grow exponentially over the next few years. Increasingly, the pharmaceutical
options have also expanded. Antibiotics, such as mupirocin, and steroids are often added to solutions. The science, or lack thereof, behind many of the OTC agents and pharmaceutical additions to saline is not widely published. Potential adverse risks also need to be balanced with greater local intervention. The influence of pre- and postsurgical distribution efficacy is an important factor that significantly changes how these solutions should be used. This article aims to provide a systematic and evidence-based approach to the science behind the topical management of sinonasal disease.
Management Concepts for Topical Therapies
There are several mechanisms by which local topical irrigations may have effect. Saline alone has been thought to have several beneficial properties. 14 Additives in saline have all too easily been credited with therapeutic gain in uncontrolled studies, 5 but the efficacy may be due to saline or simply mechanical effects alone. Three main driving forces exist in CRS (Figure 1). There is an interacting triad of intrinsic mucosal inflammation, local infection, and mucociliary dysfunction. This includes multiple eosinophillic subtypes; systemic IgE, local IgE, aspirin-sensitive airways disease, leukotriene abnormalities, asthma, superantigen, and other T-cell-driven eosinophilic inflammation. Infection may be a primary event or opportunistic owing to ulcerated mucosa or dysfunctional mucociliary transport.6 Infection for many sufferers will be a diseasemodifying event rather than the primary driving pathology.6 Finally, mucociliary dysfunction is predominantly an acquired event. There are clinical correlates of a patient skewed to one mechanism. Mucoceles are generally without infection or inflammation. They may be an example of pure mucociliary dysfunction or simple obstruction without abnormal cilia but still impaired mucocilary clearance. Likewise, grade 4 polyps, presenting only with nasal obstruction very late in the clinical history with few other symptoms, is likely to be the result of an underlying immunologic abnormality with intrinisic mucosal inflammation and retained mucociliary function without infection. Finally, patients who respond solely to culture-directed antimicrobial therapy may have simple mucosal infection with limited or easily reversible mucociliary dysfunction without primary intrinsic mucosal inflammation. Within this framework, the majority of patients develop CRS from a combination of factors, and ostial obstruction is not the primary problem; thus, simply restoring ventilation is probably
Table 1. Summary of Delivery Techniques Delivery Pressure Positive pressure Delivery Volume High volume Squeeze bottle Pressurized sprays Pulsatile jet Bulb syringe Low volume Pump sprays Atomization High volume Nasal inhalation Neti pot Low volume Drops Nebulizer Catheter instillation
Negative or low pressure
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
219
Figure 1. The pathophysiologic interaction of intrinsic mucosal inflammation, microbial flora, and mucociliary dysfunction. Current topical therapies can affect all three interacting processes: the ability to substitute for loss of mucociliary clearance and alter mucus rheology, delivery of steroids to intrinsic mucosal inflammation, and antimicrobial therapies. Reproduced with permission from the Division of Rhinology, St Vincents Hospital.
of limited benefit. The majority of recalcitrant patients in our experience have aerated sinuses but persistent mucosal disease (Figure 2). Topical therapies may act by replacing mucociliary clearance, where deficient, and removing inflammatory mucus. They can prevent infection by protecting ulcerated and inflamed mucosa. Antiinflammatory and antibiotic additives are likely to further modify the disease triangle.
Distribution of Topical Therapies
Surgery Distribution of topical solution to the unoperated sinuses is limited,7and in the setting of CRS with mucosal edema, it is
probably only in the order of , 2% of total irrigation volume.8 Nebulization is also ineffective with , 3% sinus penetration.9 A fundamentally held belief among those treating CRS patients is that endoscopic sinus surgery (ESS) improves the delivery of topical medications to the sinonasal mucosa,10,11 yet only recent evidence exists to support this claim.7,12 ESS is essential to effectively allow topical distribution to the sinuses. The frontal and sphenoid sinuses are essentially inaccessible prior to surgery7 (Figure 3), and an ostial size of 4+ mm is required to even begin seeing penetration to the maxillary sinus.12 For those with mucosal edema and chronic inflammation, distribution is probably worse.8 Additionally, there is a significant difference in the way in which ESS is delivered across institutions as some post-ESS cavities are opened widely, whereas others practice techniques to simply dilate or create very conservative
220
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
Figure 2. Postsurgical disease (A and B). Rarely is lack of ventilation a major factor. Most refractory patients have air in the sinus, and ostial patency is a poor measure of success. Objective evidence of inflammatory resolution and symptom improvement are better outcomes. These patients often result in a dramatic improvement (C and D) with topical therapy. Reproduced with permission from the Division of Rhinology, St Vincents Hospital.
sinusotomies (Figure 4). A heterogeneous group of surgical comparisons makes evaluating locally delivered therapies difficult to assess,13 and the pracitce of minimal techniques have populated without consideration of many of these factors.14 In medically managing CRS, the use of expensive and time-wasting topical therapies is probably not supported prior to surgery.
Device Nebulizers poorly penetrate the sinuses even after maximal ESS,15 and large-volume squeeze bottles appear to have the best efficacy post-ESS.7,1517 Presurgery, the distribution to the sinuses is extremely limited regardless of the device,7,8,12 and sprays are the least effective of all7 (see
Figure 3. Sprays have almost no sinus distribution prior to surgery. Mean sinus dispersion of radiographic contrast is extremely limited without surgical exposure of the sinus mucosa. In the frontal and sphenoid sinuses, this is especially true. Reproduced with permission from the Division of Rhinology, St Vincents Hospital.
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
221
B
Figure 4. The right middle meatus as it will appear after (A) ostial dilatation and (B) formal endoscopic sinus surgery. The potential difference in assisting topical delivery to the sinus mucosa is great and thus makes studies into the efficacy of endoscopic scans surgery using a heterogeneous group of such patients very difficult to interpret.
Figure 3). Neti pots have some advantage in the unoperated sinus as head position and retrograde flow allow penetration.7 Postsurgery distribution is superior with high-volume positive pressure devices.7,12,18 Research into topical distribution often quantifies penetration and surface area covered but not volume, potential shearing action, or mucosal contact time. From intrasinus video observation within our own studies, there is a very significant difference in fluid dynamics between irrigation techniques that is difficult to quantify (Figure 5). Simple computed tomography studies or endoscopic grading do not take into account the increased hydrostatic forces seen with largevolume positive pressure devices, such as a squeeze bottle, when compared with large-volume, low-pressure devices, such as the Neti pot. In addition, it is unknown if these increased irrigation pressures are beneficial or not. Simple low-volume sprays and drops have very poor distribution and should be considered a nasal cavity treatment only, especially prior to ESS.7 Although multiple devices and head positions have been trialed, less than 50% of most lowvolume applications will reach the middle meatus.19
sinuses.7,1927 The majority of these studies involve assessing the distribution of dye around the middle turbinate with simple sprays and drops in presurgical patients. Many commercial products recommend a headdown, overthe-sink, noseto-the-ground position for irrigation (Figure 6). This is practical and makes runoff easy to collect. Evidence of the efficacy in delivery of drops to the middle meatus relative to head position demonstrated that the Mygind and Ragan (left lateral and supine positions) were superior to the Mecca and Head Back positions in one study28 but was inconclusive in others.19,27 The relevance of positioning with positive pressure application may be less significant. However, even with positive pressure high-volume irrigation, the headdown or lateral position may lead to better frontal distribution.7,29
Mechanical or Pharmaceutical Intervention?
There may be potential competing interests when it comes to topical therapies. Large-volume positive pressure irrigations appear to have the best distribution and would most likely remove mucus and inflammatory secretions. Unfortunately, they are also very inefficient at delivery of pharmaceutical agents to the sinuses. Our research into exposure and residual fluid remaining in the sinuses after
Position The are incomplete data on the most effective positioning for delivering fluid to the nasal cavity and paranasal
A B
Figure 5. Preendoscopic sinus surgery (ESS) high-volume positive pressure irrigation does allow some fluid to enter the maxillary sinus (A). However, the fluid only trickles in via the natural os (1), secondary ostium (2) and surgical antrostomy (3). Post-ESS fluid delivery is fast, with high shearing forces and the potential for mechanical removal of mucus (B).
222
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
changes of healthy respiratory mucosa, including ciliary loss, when exposed to hypotonic (0.3%) and hypertonic (3%) saline on electron microscopic study.33 These changes were not seen with isotonic saline. Host innate mucosal defenses may also be removed by irrigation.3436 However, there appears to be overwhelming support for symptom benefit rather than adverse effects. The Cochrane study did not demonstrate any serious adverse event in over 1650 patients in published trials.1 Enhanced Drug Delivery There is evidence of a synergistic effect of hypertonic saline and topical steroid delivery. Possible removal of the mucus blanket alone may allow better steroid absorption. Additionally, there is evidence that increased tight junction permeability of respiratory mucosa occurs with saline and is not seen with equivalent mannitol osmolarity.37 Does this lead to better intranasal steroid delivery? There is evidence to support a synergistic saline and steroid benefit from some clinical trials in rhinitis1,38 and from nebulized therapy in asthma.39,40 Mucociliary Clearance Mucociliary function is the combination of several factors. Ciliary beat frequency (CBF) is only part of the equation. Ciliary structure and orientation; areas of ciliary loss; changes in mucus rheology41 and to the gel and sol characteristics of the mucus blanket; and effective ciliary coupling with the gel layer42 will all be involved. Buffered isotonic and hypertonic (3%) saline decreases saccharine clearance time (SCT) by 24.1% and 39.6%, respectively.43,44 Additionally, 5% hypertonic saline reduced SCT, with no change in 0.9% and 3% solutions in a further study.45 All three of these studies were on healthy, normal adults. Saline, especially hypertonic, appears to improve SCT. It is unlikely to be a result of increased CBF. The reduced SCT is likely to be a result of increased ionic load to the sol layer46 with more favourable rheologic properties.47,48 Rehydration of the sol layer may change the viscoelastic properties of the mucus blanket and allow more efficient cilial action.47 Improved mucus transport has also been demonstrated with other substances, including nonionic solutions (glucose, mannitol, and urea).49 Effect on CBF Although data exist for a positive effect on mucocillary transport time,43,44 there is no direct evidence of enhanced
Figure 6. High-volume positive pressure squeeze bottle irrigation performed with retrograde flow in contralateral nose postendoscopic sinus surgery offers the best fluid distribution to the sinuses from recent fluid dynamic research. Reproduced with permission from the Division of Rhinology, St Vincents Hospital.
irrigation suggests that less than 5% of the solution will remain after standard squeeze bottle irrigation.30 With 96% of the irrigation going to waste, combining the mechanical and pharmaceutical aims of the therapy in one delivery may be suboptimal. In addition, even when post-ESS positive pressure irrigations reach the dependent sinuses, it is unclear exactly how long such irrigations and any pharmaceutical agents remain in the sinus cavity before being cleared by mucociliary transport or gravity alone.
Saline: The Basis of All Irrigations
Topical saline appears to improve symptom control in those patients with chronic sinonasal disease.1,31 Both rhinitis and rhinosinusitis have been included in these reviews together with pre- and postoperative patient selection. Based on our current understanding of topical distribution, this makes the results difficult to interpret. Symptom control may merely be a result of better mucus management in the nasal cavity or a potential therapeutic change to pathology. Nasal Mucosa: Protective or Cytopathic? Traditional thinking portrays a mucosal protective effect by saline irrigations, avoiding drying and excoriation. It has been speculated that improved trophism of mucosa, as a result of topical saline, would enhance mucosal defence by increased specific IgA mediated defense.32 However, in vitro observation has demonstrated deleterious morphologic
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
223
CBF with saline. On the contrary, ciliostasis has been observed with 3%, 7% and 14.4% saline solutions but not with isotonic saline.50,51 Even isotonic saline has demonstrated a reduction in CBF in some studies.51 Many authors have attempted to dispel these data as a result of sampling error or artificial exposure. In an attempt to reproduce a clinically relevant situation, Wabitz and colleagues exposed nasal mucosa to 3% and 0.9% saline in healthy individuals, in vivo, and then harvested.48 The assessment of CBF was made on the explanted mucosa. There was no significant enhancement in CBF. Nasal Provocation or Decongestion? There has been much speculation on the effect of hypertonic solutions as a nasal decongestant or to reduce edema.52 Many authors have suggested that an osmotic influence would improve nasal patency.53 The concept of buffered hypertonic as a decongestant44 has not been supported by scientific observation. In contrast, decreased airspace measurements on rhinometry have been shown after hypertonic saline exposure.54 At commonly used concentrations, no statistical difference was observed in rhinometric analysis of 0.9% and 3% saline solutions.43 Variable and inconsistent changes (6 100150%) in rhinomanometric assessment to 0.9% saline and varying tonicities of solutions have been demonstrated.55,56 No relationship was found in either study. Contrary to decongestion, hypertonic saline can act as a provocation to nasal mucosa. Additional secretions are first seen at 3.6% in healthy patients.56 At even lower tonicity, 2.7% solution, nasal pain and discomfort were elicited in healthy subjects.54 When solutions approach 5.4%, there is significant sensation of nasal obstruction and corresponding loss of airspace on acoustic rhinometry.54 Nebulized hypertonic saline of 4.5% and 7% is used in asthma provocation tests. The potential for saline to stimulate nasal pain, secretion, and vasodilatation increases with tonicity. Improvement in nasal patency is likely to be the result of clearance of secretions rather that an osmotic effect.54 With higher concentrations, provocation is likely with reduced airspace and increased sensation of obstruction. There will also be a wide individual variation in thresholds and tolerance.57 Mechanical Removal of Sinonasal Secretions, Antigens, or Biofilm The potential for sprays to remove debris, mucus, or antigen has always been implied. However, there is little
research to substantiate its effectiveness. There is only indirect evidence through reduced antigen-specific IgE levels in allergic rhinitis sufferers who used saline during the allergy season.58 High-volume solutions appear to be more effective in managing symptoms than simple sprays,59 but with mixed groups of pre- and post-ESS patients, the degree of benefit is still debatable. As a potential adverse effect, positive pressure irrigations may potentially seed antigens and inflammatory products throughout the paranasal sinuses as demonstrated on the positive pressure effects of nose blowing.60
The Additives
Mucoactive Agents: Surfactants Amphipathic molecules possess the ability to be soluble in both water and organic solutions. They form the basis of surfactants. This affects both the solution and remaining molecular load behaviour at airsurface interfaces.61 Pulmonary surfactant is the best known clinical example of the importance of these amphipathic molecules. Pulmonary surfactant greatly improves the efficiency of mucocilial clearance by reducing the adhesiveness of mucus to the respiratory epithelium. Acute respiratory distress of the newborn is the case example of the requirement of such agents in respiratory function. Surfactants can have both mucoactive properties and antimicrobial properties. Chemical surfactants can interfere with microbial cell membrane permeability and cause membrane disruption. These agents are often classified as cationic, anionic, or zwitterionic (possessing nonadjacent positive and negative charges) based on the charge of the hydrophilic domain present in these molecules. Cationic surfactants possess the most antimicrobial properties but are also the most irritating.62 There are many commercially produced surfactants. Synthetically produced detergents, soil wetting agents, paints, antifogging solutions, and ski wax are all examples. The combination of PEG-80 sorbitan laurate, cocamidopropyl betaine, and sodium trideceth sulphate (commonly known as Johnson & Johnson Baby Shampoo) has been shown to have both antibiofilm-forming properties at 1% solution and clinical efficacy in managing refractory CRS patients.62 Surfactants may not be a direct therapy for aggressive polypoid mucosal change that is dominated by inflammatory T-helper (Th)2 response but for treating crusting, thick mucus and chronic bacterial mucosal colonization.
224
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
Citric acid zwitterionic surfactant is currently under study for potential antimicrobial activity.63 This agent combines the calcium bridgedisrupting citric acid with the surfactant caprylyl sulsbetaine. It was effective at reducing bacteria-forming units within a sheep CRS model but not as effective as topical mupirocin.64 There are concerns regarding possible ciliary dysfunction from any synthetic additive, and future combination solutions are likely to lead to effective agents. Alteration to the Innate Immunity Components of the innate immune system are likely to play a significant role in the normal defense and function of sinus mucosa.34 High concentration of salt in this ASL is thought to impair the activity of airway antimicrobial factors and explain some of the pathogenesis in conditions such as cystic fibrosis (CF).65 Xylitol, a nonsoluble fivecarbon sugar, has been shown to reduce bacterial colonization in healthy controls.65 This compound lowers ASL salt osmolality, providing enhanced innate immunity (salt sensitive) but no direct antimicrobial effect. Reduced bacterial load has been demonstrated in a rabbit model on maxillary sinusitis.66 There is great promise for additives that enhance innate immunity, either directly or indirectly, but combinations of hypertonic salt solution and xylitol may potentially be counterproductive. Antimicrobials Until recently, only a paucity of studies existed examining the efficacy of topical antimicrobial agents in the treatment of CRS. With the emergence of bacterial biofilms as a possible inciting or perpetuating agent in the inflammatory process associated with CRS,67,68 interest in such treatments has been rekindled. The attractiveness of topical treatment lies in its theoretical ability to achieve much higher local, yet systemically tolerated concentrations, through the direct delivery of the agent to the site of infection and limited systemic absorption. The evidence for the efficacy of several of the more commonly used topical antimicrobials is reviewed below. Tobramycin The use of topical tobramycin in CRS has been an extension of its aerosolized use in the treatment of pseudomonal pulmonary infections in CF patients. The highest level of evidence to date, supporting its efficacy in CRS, was in a nonrandomized controlled study in CF patients with
sinusitis.69 In this study, both nasal polyposis and the need for revision surgery were significantly reduced in patients treated with tobramycin irrigations. Although such efficacy in symptomatic and endoscopic improvement has also been replicated in a small, doubleblind, randomized controlled trial (RCT), additional significant benefit over saline irrigation alone was not observed at recommended human clinical concentrations of 80 mg/mL.6,70 This finding is further supported by a recent animal sinusitis model, which reported equivalent evidence of histologic persistence of disease in sinuses treated with this concentration of tobramycin versus saline irrigation alone.71 Although the authors found that increasing tobramycin concentration to 400 mg/mL6 significantly reduced histologic inflammation, concerns have been raised about the possible adverse effects, including otoxicity encountered at such high concentrations. Amphotericin B The pathogenic role of fungus in CRS remains debated, with conflicting reports surrounding the efficacy of amphotericin B as a treatment modality. Despite level I evidence from a double-blind RCT by Ponikau and colleagues demonstrating a significant improvement in endoscopic, radiologic, and serologic findings in patients treated with 250 mg/mL amphotericin B irrigations,72 such findings have not been replicated by similar RCTs.73,74 A recent in vitro study examining the activity of various doses of amphotericin B against fungal organisms may help explain the discrepancy observed.75 This study demonstrated that nasal amphotericin B irrigation is ineffective in killing fungi in vitro at the Food and Drug Administration (FDA)-approved concentration of 100 mg/mL, with concentrations of 200 mg/mL or higher required for effective fungicidal activity. Recent phase III FDA (and unpublished) trials have failed to demonstrate a clinical improvement in these patients. It appears unlikely that current human studies will provide any further conclusions made about the safety or efficacy of amphotericin B irrigations at this stage. Mupirocin Mupirocins unique mechanism of action, low crossreactivity with other antibiotics, 100% stability in nasal secretions, and insignificant systemic absorption have made it the ideal theoretical choice for the management of Staphylococcus aureusrelated CRS treatment failures. Although no RCTs exist to date, in vitro laboratory,76 in vivo animal,77 and, more recently, human cohort
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
225
studies78,79 indicate promising results in relation to its efficacy against S. aureusrelated CRS. Indeed, the study by Uren and colleagues showed that twice-daily irrigations with 0.05% mupirocin resulted in a significant symptomatic and endoscopic improvement in more than threequarters of patients who had previously failed maximal medical and surgical management.78 Part of mupirocins efficacy in this subgroup of patients is thought to be mediated by its unique antibiofilm action.76 Manuka Honey Capiliano (Australia) and manuka (New Zealand) honeys, derived from the floral source in tea trees (Leptospermum spp), have antimicrobial properties,8082 and are the most widely studied. Other honeys also have therapeutic activity.80,83,84 Manuka honey has been used with success in managing infected wounds and ulcers. 8 5 8 8 Methylglyoxal (MGO) is a derivative from the manuka flowers and is thought to be significant in the antimicrobial activity of these honeys.89,90 The appropriate concentration is debatable. One in two dilution (50%) has shown good antistaphylcoccal and antipseudomonal activity to planktonic and biofilm bacteria.84 Lower concentrations (, 5%) still have activity against coagulasenegative staphylococci.91 With MGO isolated, there is a minimum inhibitory concentration of 1.1 mM MGO against Escherichia coli and S. aureus.89 This corresponds to a 15 to 30% dilution (1.11.8 mM of MGO) of manuka honey and would appear to represent an evidence-based concentration for researchers pursuing this therapy. Although the current evidence for the efficacy of topical antimicrobial use in the treatment of CRS appears promising, it is at best low level. Larger and better designed RCTs are needed before definitive conclusions can be made regarding the ideal dosing, safety, and efficacy profiles of such agents. Until then, it is likely that topical antimicrobial agents will remain out of the mainstream management of this condition, being reserved for those patients in whom all other treatment options have been exhausted. Antiinflammatories There is growing evidence that a predominant feature of CRS is a shift in mucosal immune response to a proinflammatory action, whether Th1 or Th2 dominated. This moves away from the normal mechanical and innate immunity that provides a stable healthy mucosa.6 The antiinflammatory action of corticosteroids would appear
to be the obvious solution to help suppress this response. Unfortunately, the evidence for the role of nasal steroid in the management of CRS is weak. Most studies include unoperated patients or a mixture of pre- and postsurgical populations. This raises greater questions of what mucosa we are actually treating in these studies. The potential for recording an action on secondary turbinate reactivity in CRS is great. Steroid sprays in unoperated patients lead to almost no sinus distribution.7,92 So it is not surprising that researchers using steroid postoperatively with direct application to sinus mucosa have demonstrated benefit9395 and those with a mixed or unoperated population found less benefit.96,97 Topical fluticasone and high-dose budesonide used in the postoperative period have the best evidence for use.98 Budesonide 0.5 mg/2 mL respules diluted in 240 mL squeeze bottle irrigation is the current treatment under most recent investigation (Figure 7). Budesonide 0.25 mg once daily was shown to improve quality of life as measured by SNOT-20 scores, with no adrenal suppression.99 Although high-dose steroid application has been shown to decrease polyps100 and is simple and easy to deliver, steroid irrigations have yet to be rigorously evaluated beyond safety and feasibility.99,101
Adverse Effects
Common adverse effects often overlooked include cost, preparation time, and delivery effort. These are substantial if nonreusable products are used and high-frequency regimens are recommended. All of our current research protocols rely on twice-daily or less delivery frequency. We believe that more frequent topical therapies or irrigations are simply not practical for managing a chronic disease. There will also be a subset of patients who will find the practice of nasal irrigation uncomfortable and have burning sensations, nausea, or eustachian tube symptoms, making tolerability low. The use of saline is commonly regarded as low risk, with minimal adverse effects. Its homeopathic background has allowed widespread use without reporting of potential unwanted side effects. A recent Cochrane Review summarized the reported side effects from trials.1 No overall risk ratio could be obtained from the published data; however, reported rates from 5 to 32% were recorded. Patient discomfort, itching, otalgia, sensation of nasal obstruction, and nausea were experienced. No major adverse events were noted in the trials. There was good tolerance and acceptability of irrigation among most participants.3,102
226
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
Figure 7. The postsurgical mucosal lining before (A and B) and after topical therapy (C and D). Prominent crusting and staphylococcal and pseudomonal colonization are present (A and B). High-dose steroid therapy in the setting of mucosal bacterial infection does not follow traditional concepts on bacterial management. However, the ability to downregulate a mucosa-damaging proinflammatory response and restore innate immunity might underlie efficacy.
Pain, Discomfort, and Provocation With saline solutions used for nasal provocation testing, it is not unexpected that a proportion of users will experience some degree of discomfort, nasal burning, or pain with their use. Hyperosmolar fluid generally induces a greater reaction. Nasal pain and discomfort were experienced in healthy subjects at 2.7% solutions in challenge testing.54 Clinically, hypertonic solutions also demonstrated greater burning and discomfort compared with isotonic saline when delivered to viral rhinosinusitis patients, 32% versus 13% (p , .05).53 Some commercial preparations contain a preservative, benzalkonium chloride. Benzalkonium chloride has been shown to induce short-term discomfort, but tolerance to this response was achieved with repeated exposure.103 Apart from the concerns of its effects on nasal mucosa, it appears to be well tolerated. An RCT of benzalkonium chloride versus placebo showed no difference in objective testing (mucociliary clearance time, rhinomanometry, smell test, and nasal secretion performance) or subjective tolerability over 4 weeks of use.104 Provocation Saline and hypertonic solutions have been shown to increase both ionic and mucinous secretions.105,106 At
higher concentrations, these solutions can induce both the sensation of nasal obstruction and a decrease in objective airway space.54 Nasal eosinophil degranulation and histamine release can also be induced with saline irrigation.57 Hypertonic (4.5%) saline solutions have demonstrated usefulness as a provocation tool in asthmatics.107 The concurrent existence of asthma and CRS raises the possible risk of exacerbation of hyperresponsive airway disease. Up to 20% of asthmatic children may demonstrate hyperresponsive effects to hypertonic saline when nebulized.108 Although there are concerns regarding induction of bronchospasm,109 knowledge of particle size and deposition dictates that little exposure to the lower respiratory tract is likely to occur.9 This is particularly so in sprays and irrigations. Mucosal Injury Hypotonic solutions risk local mucosal cell damage.33 Acute otitis media was reported in several participants in an abandoned water study.110 There is good evidence to suggest that water-based therapies be avoided. The preservative benzalkonium chloride has experimentally induced nasal mucosal lesions in rat nasal respiratory epithelium.111 Benzalkonium chloride, at concentrations used in commercial sprays, can possibly cause neutrophil inactivation.112 Mucociliary dysfunction
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
227
and nasal mucosal cell damage have also been reported with benzalkonium exposure.111,113,114 Speculation exists that natural immunodefense mechanism, lysozymes and secretatory immunoglobulins, will be removed with saline irrigation.36 However, the impact of this is unproven and, in the presence of active sinonasal inflammation, is difficult to assess. Innate immunity may already be lowered, resulting in the diseased state.115 Cross-infection The potential for bacterial contamination and sinus crossinfection has been a source of concern for those less enthusiastic about the routine use of nasal irrigations. Contamination of storage devices and solution source does occur. Bulb syringes and neti pots had moderate to many bacterial colonies growing in 19.5% and 7% of containers after 2 weeks.116 There was no statistical difference between pots and bulb syringes. Spray bottles are also not immune to the contamination. After 3 days of use, 90% of spray bottles had a bacterial growth. Nearly half of the colonies were S. aureus and Pseudomonas aeruginosa.117 The comparison group in this study was nasal drop bottles, which had only 15% growth after 3 days. The minimal direct contact with nasal drop bottles is likely to account for the lower rates. Contamination of the nasal lining by pathogens from palmar skin, originating from hand-based irrigation, has also been reported.118 Higher levels of gram-negative rods are also seen in patients using irrigations compared with controls.119 What role these bacterial species might have in the course of CRS is unclear. However, there is evidence of direct contamination of the sinuses by a Pseudomonas species that was confirmed in both nearby bottles and sinks.120 Sinusitis related to Pseudomonas contamination has been reported in both humans121 and animals.122 Similar outbreaks of Pseudomonas perichondritis from contamination were reported in patients who had ear piercings at a single shop with Pseudomonas colonies growing in the disinfectant bottle and sinks.123 Other aqueous environments, such as hydrotherapy pools124 and antifog solutions,125 have also lead to cross-infection. Especially in aqueous environments, the risk of container contamination with Pseudomonas is possible. How this might relate to pathologic significance in sinus cavities routinely growing Pseudomonas and other species is unclear. Systemic Absorption Systemic absorption of medication needs to be carefully predicted. Adrenal suppression from topical steroid has
been reported93 but appears to be uncommon even with high concentration irrigation.99 With only 2.5 6 1.5% of the solution retained in the sinuses after a squeeze bottle irrigation,30 there is only a 50 6 30 mg exposure of twicedaily 1 mg budesonide nasal irrigation. Mucosal absorption may vary greatly between compounds. Ototoxicity with topical tobramycin has been reported.126,127
Conclusion
Physicians are currently faced with a bewildering array of topical therapies available for their patients with rhinosinusitis. Topical therapies will continue to grow in popularity owing to their ease, efficacy, and targeted approach to the target organ in CRSthe sinonasal mucosa. There is currently little evidence to support the use of topical therapies delivered via low-volume devices, such as nebulizers or sprays. Additionally, most topical therapies used prior to ESS do not reach the paranasal sinuses to any significant extent and are simply treating nasal conditions, such as turbinate hypertrophy owing to allergic or nonallergic rhinitis. As our knowledge of the precise pathophysiology of the various subsets of CRS grows, it will enable us to tailor topical therapies that are specific for the type of CRS seen in each patient. The pharmacologic additives used must be selected with a purpose in mind, that is, targeted antimicrobials, antiinflammatories, surfactants, or mucociliary modulating agents, and one solution will likely not be the treatment of choice for all CRS patients. Otolaryngologists must have a comprehensive understanding of topical therapies that are available, when to use specific agents, and how to deliver them to provide maximal benefit to our patients.
Acknowledgement
Financial disclosure of authors: No external funding was received. Dr. Schlosser receives grant support from the Flight Attendant Medical Research Institute, NeilMed, and Xoran. Dr. Schlosser is a consultant for BrainLAB, Medtronic Xomed, Gyrus, and Schering-Plough and serves on the speakers bureau for GlaxoSmithKline. Dr. Harvey has served on an advisory board for Schering-Plough and has received grant support from NeilMed. Dr. Witterick is on Advisory Boards for Schering-Plough and Abbott Laboratories and a consultant for Alcon and Pharmascience Inc. Dr. Psaltis has nothing to declare. Financial disclosure of reviewers: None reported.
228
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
References
1. Harvey R, Hannan SA, Badia L, et al. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 2007;(3):CD006394. 2. Brown CL, Graham SM. Nasal irrigations: good or bad? Curr Opin Otolaryngol Head Neck Surg 2004;12:913. 3. Rabago D, Barrett B, Marchand L, et al. Qualitative aspects of nasal irrigation use by patients with chronic sinus disease in a multimethod study. Ann Fam Med 2006;4:295301. 4. Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope 2000;110:118993. 5. Ferguson BJ. Antifungal nasal washes for chronic rhinosinusitis: whats therapeuticthe wash or the antifungal? J Allergy Clin Immunol 2003;111:11378. 6. Kern RC, Conley DB, Walsh W, et al. Perspectives on the etiology of chronic rhinosinusitis: an immune barrier hypothesis. Am J Rhinol 2008;22:54959. 7. Harvey RJ, Goddard JC, Wise SK, et al. Effects of endoscopic sinus surgery and delivery device on cadaver sinus irrigation. Otolaryngol Head Neck Surg 2008;139:13742. 8. Snidvongs K, Chaowanapanja P, Aeumjaturapat S, et al. Does nasal irrigation enter paranasal sinuses in chronic rhinosinusitis? Am J Rhinol 2008;22:4836. 9. Hyo N, Takano H, Hyo Y. Particle deposition efficiency of therapeutic aerosols in the human maxillary sinus. Rhinology 1989;27:1726. 10. Olson D, Rasgon B, Hilsinger R. Radiographic comparison of three methods for nasal saline irrigation. Laryngoscope 2002;112: 13948. 11. Wormald P, Cain T, Oates L, et al. A comparative study of three methods of nasal irrigation. Laryngoscope 2004;114:22247. 12. Grobler A, Weitzel EK, Buele A, et al. Pre- and postoperative sinus penetration of nasal irrigation. Laryngoscope 2008;118:207881. 13. Dijkstra MD, Ebbens FA, Poublon RM, et al. Fluticasone propionate aqueous nasal spray does not influence the recurrence rate of chronic rhinosinusitis and nasal polyps 1 year after functional endoscopic sinus surgery. Clin Exp Allergy 2004;34: 1395400. 14. Chiu AG, Kennedy DW. Disadvantages of minimal techniques for surgical management of chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg 2004;12:3842. 15. Valentine R, Athanasiadis T, Thwin M, et al. A prospective controlled trial of pulsed nasal nebulizer in maximally dissected cadavers. Am J Rhinol 2008;22:3904. 16. Wormald P-J, Cain T, Oates L, et al. A comparative study of three methods of nasal irrigation. Laryngoscope 2004;114:22247. 17. Olson DEL, Rasgon BM, Hilsinger RL. Radiographic comparison of three methods for nasal saline irrigation. Laryngoscope 2002; 112:13948. 18. Miller TR, Muntz HR, Gilbert ME, et al. Comparison of topical medication delivery systems after sinus surgery. Laryngoscope 2004;114:2014. 19. Merkus P, Ebbens FA, Muller B, et al. The best method of topical nasal drug delivery: comparison of seven techniques. Rhinology 2006;44:1027. 20. Kayarkar R, Clifton NJ, Woolford TJ. An evaluation of the best head position for instillation of steroid nose drops. Clin Otolaryngol Allied Sci 2002;27:1821.
21. Karagama YG, Lancaster JL, Karkanevatos A, et al. Delivery of nasal drops to the middle meatus: which is the best head position? Rhinology 2001;39:2269. 22. Homer JJ, Raine CH. An endoscopic photographic comparison of nasal drug delivery by aqueous spray. Clin Otolaryngol Allied Sci 1998;23:5603. 23. Homer JJ, Maughan J, Burniston M. A quantitative analysis of the intranasal delivery of topical nasal drugs to the middle meatus: spray versus drop administration. J Laryngol Otol 2002;116:103. 24. Aggarwal R, Cardozo A, Homer JJ. The assessment of topical nasal drug distribution. Clin Otolaryngol Allied Sci 2004;29:2015. 25. Tsikoudas A, Homer JJ. The delivery of topical nasal sprays and drops to the middle meatus: a semiquantitative analysis. Clin Otolaryngol Allied Sci 2001;26:2947. 26. Cannady SB, Batra PS, Citardi MJ, et al. Comparison of delivery of topical medications to the paranasal sinuses via vertex-tofloor position and atomizer spray after FESS. Otolaryngol Head Neck Surg 2005;133:73540. 27. Benninger MS, Hadley JA, Osguthorpe JD, et al. Techniques of intranasal steroid use. Otolaryngol Head Neck Surg 2004;130:5 24. 28. Karagama YG, Lancaster JL, Karkanevatos A, et al. Delivery of nasal drops to the middle meatus: which is the best head position? Rhinology 2001;39:2269. 29. Beule A, Athanasiadis T, Athanasiadis E, et al. Efficacy of different techniques of sinonasal irrigation after modified Lothrop procedure. Am J Rhinol Allergy 2009;23:8590. 30. Harvey RJ, Debnath N, Srubiski A, et al. Fluid residuals and drug exposure in nasal irrigation. Otolaryngol Head Neck Surg 2009 [In press]. 31. Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg 2007;133:111520. 32. Passali D, Damiani V, Passali FM, et al. Atomized nasal douche vs nasal lavage in acute viral rhinitis. Arch Otolaryngol Head Neck Surg 2005;131:78890. 33. Kim CH, Hyun Song M, Eun Ahn Y, et al. Effect of hypo-, isoand hypertonic saline irrigation on secretory mucins and morphology of cultured human nasal epithelial cells. Acta Otolaryngol (Stockh) 2005;125:1296300. 34. Ooi EH, Wormald P-J, Tan LW. Innate immunity in the paranasal sinuses: a review of nasal host defenses. Am J Rhinol 2008;22:139. 35. Psaltis AJ, Bruhn MA, Ooi EH, et al. Nasal mucosa expression of lactoferrin in patients with chronic rhinosinusitis. Laryngoscope 2007;117:20305. 36. Berry YJ. Negative side of nasal saline sprays: they can be harmful. Arch Otolaryngol Head Neck Surg 2003;129:1352. 37. Hogman M, Mork AC, Roomans GM. Hypertonic saline increases tight junction permeability in airway epithelium. Eur Respir J 2002;20:14448. 38. Slapak I, Skoupa J, Strnad P, et al. Efficacy of isotonic nasal wash (seawater) in the treatment and prevention of rhinitis in children. Arch Otolaryngol Head Neck Surg 2008;134:6774. 39. Rogers DF. Mucoactive agents for airway mucus hypersecretory diseases. Respir Care 2007;52:117693; discussion 937. 40. Daviskas E, Anderson SD. Hyperosmolar agents and clearance of mucus in the diseased airway. J Aerosol Med 2006;19:1009.
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
229
41. Quraishi MS, Jones NS, Mason J. The rheology of nasal mucus: a review. Clin Otolaryngol Allied Sci 1998;23:40313. 42. Sleigh MA. Ciliary adaptations for the propulsion of mucus. Biorheology 1990;27:52732. 43. Keojampa BK, Hoang Nguyen M, Ryan MW. Effects of buffered saline solution on nasal mucociliary clearance and nasal airway patency. Otolaryngol Head Neck Surg 2004;131:67982. 44. Talbot AR, Herr TM, Parsons DS. Mucociliary clearance and buffered hypertonic saline solution. Laryngoscope 1997;107:5003. 45. Homer JJ, Dowley AC, Condon L, et al. The effect of hypertonicity on nasal mucociliary clearance. Clin Otolaryngol Allied Sci 2000;25:55860. 46. Daviskas E, Anderson SD, Gonda I, et al. Inhalation of hypertonic saline aerosol enhances mucociliary clearance in asthmatic and healthy subjects. Eur Respir J 1996;9:72532. 47. Middleton PG, Geddes DM, Alton EW. Effect of amiloride and saline on nasal mucociliary clearance and potential difference in cystic fibrosis and normal subjects. Thorax 1993;48:8126. 48. Wabnitz DA, Wormald PJ, Wabnitz DAM, et al. A blinded, randomized, controlled study on the effect of buffered 0.9% and 3% sodium chloride intranasal sprays on ciliary beat frequency. Laryngoscope 2005;115:8035. 49. Wills PJ, Hall RL, Chan W, et al. Sodium chloride increases the ciliary transportability of cystic fibrosis and bronchiectasis sputum on the mucus-depleted bovine trachea. J Clin Invest 1997;99:913. 50. Min YG, Lee KS, Yun JB, et al. Hypertonic saline decreases ciliary movement in human nasal epithelium in vitro. Otolaryngol Head Neck Surg 2001;124:3136. 51. Boek WM, Keles N, Graamans K, et al. Physiologic and hypertonic saline solutions impair ciliary activity in vitro. Laryngoscope 1999;109:3969. 52. Olson DEL, Rasgon BM, Hilsinger RL Jr. Radiographic comparison of three methods for nasal saline irrigation. Laryngoscope 2002;112:13948. 53. Adam P, Stiffman M, Blake RL Jr. A clinical trial of hypertonic saline nasal spray in subjects with the common cold or rhinosinusitis. Arch Fam Med 1998;7:3943. 54. Baraniuk JN, Ali M, Naranch K. Hypertonic saline nasal provocation and acoustic rhinometry. Clin Exp Allergy 2002;32: 54350. 55. Haavisto L, Sipila J, Suonpaa J. Nonspecific nasal mucosal reactivity, expressed as changes in nasal airway resistance after bilateral saline provocation. Am J Rhinol 1998;12:2758. 56. Cassano P, Latorre F. Il test di provocazione nasale con soluzioni iperosmolari: dati normativi. Boll Soc Ital Biol Sper 1991;67:3118. 57. Krayenbuhl MC, Hudspith BN, Brostoff J, et al. Nasal histamine release following hyperosmolar and allergen challenge. Allergy 1989;44:259. 58. Subiza JL, Subiza J, Barjau MC, et al. Inhibition of the seasonal IgE increase to Dactylis glomerata by daily sodium chloride nasalsinus irrigation during the grass pollen season. J Allergy Clin Immunol 1999;104:7112. 59. Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg 2007;133:111520. 60. Gwaltney JM Jr, Hendley JO, Phillips CD, et al. Nose blowing propels nasal fluid into the paranasal sinuses. Clin Infect Dis 2000; 30:38791.
61. Van Hamme JD, Singh A, Ward OP. Physiological aspects. Part 1 in a series of papers devoted to surfactants in microbiology and biotechnology. Biotechnol Adv 2006;24:60420. 62. Chiu AG, Palmer JN, Woodworth BA, et al. Baby shampoo nasal irrigations for the symptomatic postfunctional endoscopic sinus surgery patient. Am J Rhinol 2008;22:347. 63. Desrosiers M, Myntti M, James G. Methods for removing bacterial biofilms: in vitro study using clinical chronic rhinosinusitis specimens. Am J Rhinol 2007;21:52732. 64. Le T, Psaltis A, Tan LW, et al. The efficacy of topical antibiofilm agents in a sheep model of rhinosinusitis. Am J Rhinol 2008;22: 5607. 65. Zabner J, Seiler MP, Launspach JL, et al. The osmolyte xylitol reduces the salt concentration of airway surface liquid and may enhance bacterial killing. Proc Natl Acad Sci U S A 2000;97: 116149. 66. Brown CL, Graham SM, Cable BB, et al. Xylitol enhances bacterial killing in the rabbit maxillary sinus. Laryngoscope 2004;114:20214. 67. Psaltis AJ, Ha KR, Beule AG, et al. Confocal scanning laser microscopy evidence of biofilms in patients with chronic rhinosinusitis. Laryngoscope 2007;117:13026. 68. Harvey RJ, Lund VJ. Biofilms and chronic rhinosinusitis: systematic review of evidence, current concepts and directions for research. Rhinology 2007;45:313. 69. Vaughan WC. Nebulization of antibiotics in management of sinusitis. Curr Infect Dis Rep 2004;6:18790. 70. Desrosiers MY, Salas-Prato M. Treatment of chronic rhinosinusitis refractory to other treatments with topical antibiotic therapy delivered by means of a large-particle nebulizer: results of a controlled trial. Otolaryngol Head Neck Surg 2001;125:2659. 71. Antunes MB, Feldman MD, Cohen NA, et al. Dose-dependent effects of topical tobramycin in an animal model of Pseudomonas sinusitis. Am J Rhinol 2007;21:4237. 72. Ponikau JU, Sherris DA, Weaver A, et al. Treatment of chronic rhinosinusitis with intranasal amphotericin B: a randomized, placebo-controlled, double-blind pilot trial. J Allergy Clin Immunol 2005;115:12531. 73. Weschta M, Rimek D, Formanek M, et al. Topical antifungal treatment of chronic rhinosinusitis with nasal polyps: a randomized, double-blind clinical trial. J Allergy Clin Immunol 2004;113:11228. 74. Ebbens FA, Scadding GK, Badia L, et al. Amphotericin B nasal lavages: not a solution for patients with chronic rhinosinusitis. J Allergy Clin Immunol 2006;118:114956. 75. Shirazi MA, Stankiewicz JA, Kammeyer P. Activity of nasal amphotericin B irrigation against fungal organisms in vitro. Am J Rhinol 2007;21:1458. 76. Ha KR, Psaltis AJ, Butcher AR, et al. In vitro activity of mupirocin on clinical isolates of Staphylococcus aureus and its potential implications in chronic rhinosinusitis. Laryngoscope 2008;118: 53540. 77. Dalpiaz A, Gavini E, Colombo G, et al. Brain uptake of an antiischemic agent by nasal administration of microparticles. J Pharm Sci 2008;97:4889903. 78. Uren B, Psaltis A, Wormald PJ. Nasal lavage with mupirocin for the treatment of surgically recalcitrant chronic rhinosinusitis. Laryngoscope 2008;118:167780. 79. Solares CA, Batra PS, Hall GS, et al. Treatment of chronic rhinosinusitis exacerbations due to methicillin-resistant
230
Journal of Otolaryngology-Head & Neck Surgery, Volume 39, Number 3, 2010
80.
81.
82.
83.
84.
85.
86.
87.
88. 89.
90.
91.
92.
93.
94.
95.
96. 97.
Staphylococcus aureus with mupirocin irrigations. Am J Otolaryngol 2006;27:1615. Lee H, Churey JJ, Worobo RW. Antimicrobial activity of bacterial isolates from different floral sources of honey. Int J Food Microbiol 2008;126:2404. Lusby PE, Coombes AL, Wilkinson JM. Bactericidal activity of different honeys against pathogenic bacteria. Arch Med Res 2005; 36:4647. Allen KL, Molan PC, Reid GM. A survey of the antibacterial activity of some New Zealand honeys. J Pharm Pharmacol 1991; 43:81722. Mullai V, Menon T. Bactericidal activity of different types of honey against clinical and environmental isolates of Pseudomonas aeruginosa. J Altern Complement Med 2007;13:43941. Alandejani T, Marsan J, Ferris W, et al. Effectiveness of honey on Staphylococcus aureus and Pseudomonas aeruginosa biofilms. Otolaryngol Head Neck Surg 2009;141:1148. Visavadia BG, Honeysett J, Danford M. Manuka honey dressing: an effective treatment for chronic wound infections. Br J Oral Maxillofac Surg 2008;46:6967. Cooper RA, Molan PC, Krishnamoorthy L, et al. Manuka honey used to heal a recalcitrant surgical wound. Eur J Clin Microbiol Infect Dis 2001;20:7589. Gethin G, Cowman S. Manuka honey vs. hydrogela prospective, open label, multicentre, randomised controlled trial to compare desloughing efficacy and healing outcomes in venous ulcers. J Clin Nurs 2009;18:46674. Chambers J. Topical manuka honey for MRSA-contaminated skin ulcers. Palliat Med 2006;20:557. Mavric E, Wittmann S, Barth G, et al. Identification and quantification of methylglyoxal as the dominant antibacterial constituent of manuka (Leptospermum scoparium) honeys from New Zealand. Mol Nutr Food Res 2008;52:4839. Adams CJ, Manley-Harris M, Molan PC. The origin of methylglyoxal in New Zealand manuka (Leptospermum scoparium) honey. Carbohydr Res 2009;344:10503. French VM, Cooper RA, Molan PC. The antibacterial activity of honey against coagulase-negative staphylococci. J Antimicrob Chemother 2005;56:22831. Hwang PH, Woo RJ, Fong KJ. Intranasal deposition of nebulized saline: a radionuclide distribution study. Am J Rhinol 2006;20: 25561. DelGaudio JM, Wise SK. Topical steroid drops for the treatment of sinus ostia stenosis in the postoperative period. Am J Rhinol 2006;20:5637. Lavigne F, Cameron L, Renzi PM, et al. Intrasinus administration of topical budesonide to allergic patients with chronic rhinosinusitis following surgery. Laryngoscope 2002;112: 85864. Mastalerz L, Milewski M, Duplaga M, et al. Intranasal fluticasone propionate for chronic eosinophilic rhinitis in patients with aspirin-induced asthma. Allergy 1997;52:895900. Qvarnberg Y, Kantola O, Salo J, et al. Influence of topical steroid treatment on maxillary sinusitis. Rhinology 1992;30:10312. Parikh A, Scadding GK, Darby Y, et al. Topical corticosteroids in chronic rhinosinusitis: a randomized, double-blind, placebocontrolled trial using fluticasone propionate aqueous nasal spray. Rhinology 2001;39:759.
98. Kanowitz SJ, Batra PS, Citardi MJ. Topical budesonide via mucosal atomization device in refractory postoperative chronic rhinosinusitis. Otolaryngol Head Neck Surg 2008;139:1316. 99. Sachanandani NS, Piccirillo JF, Kramper MA, et al. The effect of nasally administered budesonide respules on adrenal cortex function in patients with chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg 2009;135:3037. 100. Kang IG, Yoon BK, Jung JH, et al. The effect of high-dose topical corticosteroid therapy on prevention of recurrent nasal polyps after revision endoscopic sinus surgery. Am J Rhinol 2008;22:497 501. 101. Bhalla RK, Payton K, Wright ED. Safety of budesonide in saline sinonasal irrigations in the management of chronic rhinosinusitis with polyposis: lack of significant adrenal suppression. J Otolaryngol Head Neck Surg 2008;37:8215. 102. Rabago D, Pasic T, Zgierska A, et al. The efficacy of hypertonic saline nasal irrigation for chronic sinonasal symptoms. Otolaryngol Head Neck Surg 2005;133:38. 103. Storaas T, Andersson M, Persson CG, et al. Effects of benzalkonium chloride on innate immunity physiology of the human nasal mucosa in vivo. Laryngoscope 2000;110:15437. 104. Lange B, Lukat KF, Bachert C. Local tolerability of a benzalkonium chloride-containing homeopathic nasal spray. Allergologie 2004;27:10210. 105. Greiff L, Andersson M, Wollmer P, et al. Hypertonic saline increases secretory and exudative responsiveness of human nasal airway in vivo. Eur Respir J 2003;21:30812. 106. Middleton PG, Pollard KA, Wheatley JR. Hypertonic saline alters ion transport across the human airway epithelium. Eur Respir J 2001;17:1959. 107. Anderson SD, Brannan JD, Chan HK. Use of aerosols for bronchial provocation testing in the laboratory: where we have been and where we are going. J Aerosol Med 2002;15: 31324. 108. Riedler J, Reade T, Dalton M, et al. Hypertonic saline challenge in an epidemiologic survey of asthma in children. Am J Respir Crit Care Med 1994;150:16329. 109. Karadag A, Kurtaran H, Tekin O, et al. Isotonic saline or hypertonic saline: which is best for sinusitis? J Fam Pract 2004;53:637. 110. Wendeler HM, Muller J, Dieler R, et al. Nasal irrigation using isotonic Emser salt solution in patients with chronic rhinosinusitis. Otorhinolaryngol Nova 1997;7(56):2548. 111. Cho JH, Kwun YS, Jang HS, et al. Long-term use of preservatives on rat nasal respiratory mucosa: effects of benzalkonium chloride and potassium sorbate. Laryngoscope 2000;110:3127. 112. Boston M, Dobratz EJ, Buescher ES, et al. Effects of nasal saline spray on human neutrophils. Arch Otolaryngol Head Neck Surg 2003;129:6604. 113. Bernstein IL. Is the use of benzalkonium chloride as a preservative for nasal formulations a safety concern? A cautionary note based on compromised mucociliary transport. J Allergy Clin Immunol 2000;105:3944. 114. McMahon C, Darby Y, Ryan R, et al. Immediate and short-term effects of benzalkonium chloride on the human nasal mucosa in vivo. Clin Otolaryngol Allied Sci 1997;22:31822. 115. Psaltis AJ, Wormald P-J, Ha KR, et al. Reduced levels of lactoferrin in biofilm-associated chronic rhinosinusitis. Laryngoscope 2008;118:895901.
Harvey et al, Current Topical Therapy for Chronic Sinonasal Disease
231
116. Heatley DG, McConnell KE, Kille TL, et al. Nasal irrigation for the alleviation of sinonasal symptoms. Otolaryngol Head Neck Surg 2001;125:448. 117. Brook I. Bacterial contamination of saline nasal spray/drop solution in patients with respiratory tract infection. Am J Infect Control 2002;30:2467. 118. Johannssen V, Maune S, Erichsen H, et al. [How does postoperative endonasal mucosa care affect the nasal bacterial flora? A study of two rinsing techniques using saline solution after paranasal sinus surgery.] Laryngorhinootologie 1996;75:5803. 119. Nadel DM, Lanza DC, Kennedy DW. Endoscopically guided cultures in chronic sinusitis. Am J Rhinol 1998;12:23341. 120. Faden H, Britt M, Epstein B, et al. Sinus contamination with Pseudomonas paucimobilis: a pseudoepidemic due to contaminated irrigation fluid. Infect Control 1981;2:2335. 121. Bert F, Maubec E, Bruneau B, et al. Multi-resistant Pseudomonas aeruginosa outbreak associated with contaminated tap water in a neurosurgery intensive care unit. J Hosp Infect 1998;39:5362.
122. Watson PJ, Jiru X, Watabe M, et al. Purulent rhinitis and otitis caused by Pseudomonas aeruginosa in sheep showered with contaminated shower wash. Vet Rec 2003;153:7047. 123. Keene WE, Markum AC, Samadpour M. Outbreak of Pseudomonas aeruginosa infections caused by commercial piercing of upper ear cartilage. JAMA 2004;291:9815. 124. McGuckin MB, Thorpe RJ, Abrutyn E. Hydrotherapy: an outbreak of Pseudomonas aeruginosa wound infections related to Hubbard tank treatments. Arch Phys Med Rehabil 1981;62:2835. 125. Romney M, Sherlock C, Stephens G, et al. Pseudo-outbreak of Pseudomonas putida in a hospital outpatient clinic originating from a contaminated commercial anti-fog solutionVancouver, British Columbia. Can Commun Dis Rep 2000;26:1834. 126. Pai VB, Nahata MC. Efficacy and safety of aerosolized tobramycin in cystic fibrosis. Pediatr Pulmonol 2001;32:31427. 127. Scheinberg PA, Otsuji A. Nebulized antibiotics for the treatment of acute exacerbations of chronic rhinosinusitis. Ear Nose Throat J 2002;81:64852.
Copyright of Journal of Otolaryngology -- Head & Neck Surgery is the property of B.C. Decker Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Вам также может понравиться
- 1 Hidradenitis Suppurativa (HS) IsДокумент13 страниц1 Hidradenitis Suppurativa (HS) Isyosi93Оценок пока нет
- Effect of Myringotomy As An Office Procedure On The Clinical Course ofДокумент4 страницыEffect of Myringotomy As An Office Procedure On The Clinical Course ofyosi93Оценок пока нет
- Jurnal ReadingДокумент20 страницJurnal Readingyosi93Оценок пока нет
- Health Information for Travelers to IndonesiaДокумент3 страницыHealth Information for Travelers to Indonesiayosi93Оценок пока нет
- From Public Health PDFДокумент10 страницFrom Public Health PDFyosi93Оценок пока нет
- Ujian Ststus Bedah YosiДокумент61 страницаUjian Ststus Bedah Yosiyosi93Оценок пока нет
- J. Lipid Res.-1981-Abrams-323-38Документ16 страницJ. Lipid Res.-1981-Abrams-323-38yosi93Оценок пока нет
- Services MarketingДокумент55 страницServices MarketingTanmay SrivastavaОценок пока нет
- 1.jane Skok PDFДокумент3 страницы1.jane Skok PDFyosi93Оценок пока нет
- Letters To Editor PDFДокумент77 страницLetters To Editor PDFyosi93Оценок пока нет
- Current Concepts in Topical Therapy For Chronic Sinonasal PDFДокумент16 страницCurrent Concepts in Topical Therapy For Chronic Sinonasal PDFyosi93Оценок пока нет
- Conundrums and Controversies PDFДокумент6 страницConundrums and Controversies PDFyosi93Оценок пока нет
- 2 PDFДокумент7 страниц2 PDFyosi93Оценок пока нет
- Complaints PDFДокумент3 страницыComplaints PDFyosi93Оценок пока нет
- Conundrums and Controversies PDFДокумент6 страницConundrums and Controversies PDFyosi93Оценок пока нет
- MODUL KARDIOVASKULAR - Dr. MasinemДокумент6 страницMODUL KARDIOVASKULAR - Dr. Masinemyosi93Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- HESI Dosage Calculation Practice ExamДокумент24 страницыHESI Dosage Calculation Practice Exambhilligoss35Оценок пока нет
- Lots of Salt Causes Retention of WaterДокумент8 страницLots of Salt Causes Retention of WaterMarchant Lowry BleyОценок пока нет
- IVTДокумент11 страницIVTWilliam UrmanitaОценок пока нет
- Chapter 036Документ9 страницChapter 036Neverends201160% (5)
- Fluid Therapy: Route Advantages DisadvantagesДокумент3 страницыFluid Therapy: Route Advantages DisadvantagesAshref BelhajОценок пока нет
- Odisha State Medical Corporation Limited invites bids for supply of drugsДокумент125 страницOdisha State Medical Corporation Limited invites bids for supply of drugskahil sargwalОценок пока нет
- Management of Advanced Peritonitis PP TДокумент106 страницManagement of Advanced Peritonitis PP Tvedant kanadeОценок пока нет
- Solamente Amame (You Make Me Fe - Kathalee TruebaДокумент18 страницSolamente Amame (You Make Me Fe - Kathalee TruebaIvan BurgosОценок пока нет
- NSG122 Study Guide Exam V StudentДокумент5 страницNSG122 Study Guide Exam V StudentCarleetha SmithОценок пока нет
- MFAG Equipment According IMDG With Recent Code (IMO) When Dangerous Goods On BoardДокумент4 страницыMFAG Equipment According IMDG With Recent Code (IMO) When Dangerous Goods On BoardRosu AlexandruОценок пока нет
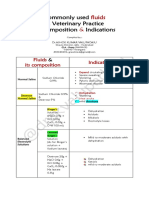
- Common IV Fluids at Composition & IndicationsДокумент2 страницыCommon IV Fluids at Composition & IndicationsNilesh SuryawanshiОценок пока нет
- MCQ Sick NewbornДокумент21 страницаMCQ Sick NewbornprabhatОценок пока нет
- IV Med NotesДокумент176 страницIV Med NotesRetno Nheeno R100% (1)
- Hydration by Subcutaneous InfusionДокумент11 страницHydration by Subcutaneous Infusionrene_smithОценок пока нет
- Major Intracellular and Extracellular IonsДокумент20 страницMajor Intracellular and Extracellular IonsTricia RestriveraОценок пока нет
- Fluids in Surgery 1 1Документ43 страницыFluids in Surgery 1 1محمد عماد عليОценок пока нет
- Remdesivir Injection 100 MG Pharmacy Manual v2 March 2020Документ15 страницRemdesivir Injection 100 MG Pharmacy Manual v2 March 2020Gurpreet SinghОценок пока нет
- SOP 6.3 - Ketamine Xylazine AnesthesiaДокумент2 страницыSOP 6.3 - Ketamine Xylazine AnesthesiaamelОценок пока нет
- Antibiotic Desensitization ProtocolsДокумент7 страницAntibiotic Desensitization ProtocolsMichael FreudigerОценок пока нет
- Fluid Managament by DR ShahabДокумент48 страницFluid Managament by DR ShahabShahabuddin ShaikhОценок пока нет
- PERFORMANCE EVALUATION CHECKLISTДокумент7 страницPERFORMANCE EVALUATION CHECKLISTJerika Shane MañosoОценок пока нет
- Nasal IrrigationДокумент16 страницNasal IrrigationMaya AnggrainiОценок пока нет
- Compatibility and Stability of Diazepam InjectionДокумент4 страницыCompatibility and Stability of Diazepam InjectionHanunОценок пока нет
- Practicum 1Документ4 страницыPracticum 1armin509Оценок пока нет
- Chapter 17 Sterile ProductsДокумент28 страницChapter 17 Sterile ProductsM Imran SajidОценок пока нет
- Elsiver NCLEX Critical CareДокумент112 страницElsiver NCLEX Critical CareHasan A AsFour100% (1)
- The Illusion of Viral Contagion - Scientific and Philosophical ReviewДокумент272 страницыThe Illusion of Viral Contagion - Scientific and Philosophical ReviewFlorin The GOATОценок пока нет
- Medication CardsДокумент65 страницMedication CardsMovaliya Ghanshyam80% (5)
- Type and Indication of IV Therapy 2Документ33 страницыType and Indication of IV Therapy 2Ruth Jazelle MendozaОценок пока нет
- IV dosage calculations overviewДокумент4 страницыIV dosage calculations overviewLuis RiveraОценок пока нет