Академический Документы
Профессиональный Документы
Культура Документы
Phystx
Загружено:
jrubin83669Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Phystx
Загружено:
jrubin83669Авторское право:
Доступные форматы
CBC, Abnormalities of RBCs & WBCs
Compete Blood Count(CBC) Functions Detection & evaluation of anemia Detection of inflammatory & infectious processes Detection & evaluation of leukemia Evaluation of peripheral blood cell characteristics Detection & evaluation of polycythemia Red Blood Cell(RBC) Indices RBC Count Number of RBC's per unit volume Measured directly & given in millions per microliter Adult males-4.50-5.90 x 106/mm3 Adult females- 4.00-5.20 x 106/mm3 Hemoglobin (Hgb) Measured directly & given in grams per deciliter. Most useful measure of oxygen carrying capacity of blood Adult males 13.5-17.5 g/dL Adult females 12.0-16.0 g/dL Hematocrit (Hct) Calculated value RBC count x MCV Adult males 41.0-53.0 Adult females 36.0-46.0 Mean Corpuscular Volume (MCV) Measured directly; unit is femtoliter(fl) Measures size of RBC's Classifies anemias into "macrocytic" with higher than normal MCV &"microcytic" with low MCV. Normal 78-102 fl Mean Corpuscular Hemoglobin (MCH) Calculated Value Hgb RBC count Average mass of Hgb in an individual RBC; Unit is picogram(pg) Normal 26.0-34.0 pg/cell Mean Corpuscular Hemoglobin Concentration (MCHC) Hgb Hct Expressed g/dL Provides a measure of Hgb concentration in cells. Normal 31.0-37.0 g/dL RBC Distribution Width (RDW) Standard deviation of MCV Measure of anisocytosis, or variation in RBC size Normal 13.0( 11.5-14.5) Measured in femtoliters (fl). Reticulocyte Count (RC) Generated manually Peripheral smear stained with a supravital dye so number of reticulocytes can be enumerated. Given as a "corrected reticulocyte count" which compensates for falsely elevated RC with anemia: RC (corrected) = RC x (patient Hct 45). Normal RC 0.5-2.5 % RBCs Normal Values for WBCs Much less numerous than RBCs 1 WBC to 600 RBCs, or about 8,000 per cubic millimeter of blood, with a normal variation from 6,000 to 10,000 Under pathologic conditions, number may be greatly increased(leukocytosis) or reduced in number(leukopenia) Leukocytes identified by microscopic appearance on a stained blood smear.
WBCs may be identified based on their reactions to different dyes in stain Neutrophil Mean Cells/uL- 3650/ uL 95% Confidence Limits 1830-7250 cells/uL Percent total WBC 40-70% 9 to 10 days from myeloblast to cell death Pass from BM to peripheral blood & from peripheral blood to tissues Movement is not reversible AKA Polys, PMN, or segmented neutrophil Bands Percent total WBC 0-10% Lymphocyte Mean Cells/uL- 2500/uL 95% Confidence Limits 1500-4000 cells/uL Percent Total WBC 22-44 % RBC about 2/3 size of a normal lymphocyte. Monocyte Mean Cells/uL 430/uL 95% Confidence Limits 200-950 cells/uL Percent Total 4-11 % Kidney shaped Slightly larger than a lymphocyte & has a folded nucleus. Monocytes can migrate out of bloodstream & become tissue macrophages under influence of cytokines. Eosinophil Mean cells/uL 150 cells/uL 95% Confidence Limits 0-700 Percent Total WBC 0-8% Eosinophils can increase with allergic reactions & with parasitic infestations. Basophil Mean cells/uL 30/uL 95% Confidence Limits 0-150 Percent Total WBC 0-3% Lobed nucleus (like PMN's) & numerous coarse, dark blue granules in cytoplasm Platelet Count Included on routine CBC along with mean platelet volume (MPV) Platelets not true intact cells, but fragments of giant megakaryocyte Essential part of coagulation process, with direct or indirect influence on a variety of aspects of homeostasis & thrombosis Normal 150-350 x 103/mm3 < 50,000 may be considered a critical value in some situations & counts < 20,000 always considered critical Values > 1,000,000 may also be considered critical MPV with normal values 7.4 to 10.4 fL Larger platelets younger with better homeostatic function than older platelets With a normal platelet count(150,00 to 400,000), a field containing 200 RBCs should contain 6 to 18 platelets Giant Platelet Bleeding tendency significantly less with higher MPV values MPV correlates with bleeding tendency in patients with thrombocytopenia Normal RBC(Erythrocyte) 6 - 8 microns in diameter Appear as circular, homogeneous discs with a center that is paler than periphery Cells nearly uniform in size & shape. RBC about 2/3 size of a normal lymphocyte. Nucleated RBCs Precursors to mature RBCs & in healthy adult they are found only in bone marrow(BM) Occurrence in peripheral blood circulation when there is a increased demand on BM
Abnormalities of RBCs RBC Inclusions Basophilic Stippling Fine Basophilic Stippling Increased production RBCs Increased Reticulocytosis Coarse Basophilic Stippling Lead Poisoning Toxic BM damage Impaired Hgb synthesis Megaloblastic Anemia Myelodysplasia Thalassemia Cabot Rings RBC inclusion indicative of abnormal erythropoiesis Seen in severe hemolytic anemia Bluish, thread-like rings or convolutions(figure-of-eight, loop shaped) Howell-Jolly Bodies Small, round deeply basophilic nuclear chromatin remnant Seen when spleen is absent Also may be seen in Hyposplenism Megaloblastic anemia Hemolytic anemia Thalassemia Heinz Body Spherical inclusions of precipitated Hgb seen as a perimembranous blue dot after supravital staining Result from abnormal Hgb precipitation & may be a single large body or several small ones Not seen in normal individuals because they are removed by spleen Pappenheimer Body Multiple tiny iron-containing granules composed of mitrochondria & ribosomes resemble basophilic stippling Post-splenectomy Lead poisoning Iron overload Sideroblastic anemias Thalassemia Iron overload Multiple transfusions Plasmodium Infection Malaria With Plasmodium infection seen as "ring forms", stippling, & gametocytes, depending upon species PBS demonstrates several ring forms of Malaria (Plasmodium vivax) in RBCs Staining Hypochromia Cells with decreased MCH, typical of iron deficiency RBCs have less hemoglobin Central pale area becomes larger & paler, Hyperchromia Cells stain more deeply with less central pallor. Cells are larger & thicker Increased Hgb content (elevated MCH) Normal Hgb concentration (MCHC) Seen in megaloblastic anemia Polychromasia RBC that contain residual RNA stain with blue-gray tint
Indicates cell is immature & has only been in blood 1- 2 days. Increased polychromasia implies reticulocytosis or increased RBC production RBC Size & Shape Anisiocytosis-Variations in RBC Size Small cells imply a defect in hemoglobin synthesis caused by iron deficiency or abnormal hemoglobin genes Large cells imply delay in erythroid precursor DNA synthesis caused by folate or B12 deficiency or drug effect Microcytosis- Small RBCs RBC's are smaller than normal(microcytic) & have an increased zone of central pallor. Cells with decreased MCV, typical of iron deficiency anemia & thalassemia Macrocytosis-Large RBCs Cells with increased MCV, typical of megaloblastic anemias Note size of RBC's to lymphocyte Etiologies B 12/Folate deficiency Cancer chemotherapy Myelodysplastic syndromes Liver diseases Alcoholism Hypothyroidism Poikiocytosis-Variation in RBC shape Some variation in RBC shape normal. Increased variation in shape termed poikilocytosis. A variety of abnormal shapes seen & any abnormally shaped cell is referred as a poikilocyte. Anisiopoikiocytosis-Variation in RBC size & shape PBS from a patient with Hemoglobin H Disease showing target cells, microcytosis, hypochromia, & anisopoikilocytosis Spherocytosis Small, round dense cell without central pallor Decreased MVC & increased MCHC Hereditary Spherocytosis Suggests extravascular hemolysis in previously normal persons Immunohemolytic anemias Recent blood transfusion Size of many RBC's is small, with lack of central zone of pallor Spherocytes do not survive as long as normal RBC's & need for increased RBC production, Target cells Cell with central & peripheral staining with intervening pallor due to increased redundancy of RBC membrane When stained, a peripheral rim of Hgb seen with a dark, central Hgb-containing area, resembling a target Occurrence Obstructive jaundice S/P splenectomy Hypochromic anemia's Iron-deficiency anemia Thalassemia Hemoglobin C & Hemoglobin SC disease Hgb. C leads to formation of "target" cells--RBC's that have a central reddish dot. Curved, banana-shaped cell with pointed ends found in SC disease from aggregation of Hgb S Shows marked poikilocytosis PBS in Sickle Cell Crisis Hgb SS is prone to crystallization when O2 tension low, & RBC's change shape to long, thin sickle forms that sludge in capillaries, further decreasing blood flow & O2 tension
Schistocytes Fragmented, irregularly shaped RBC A variant called a "helmet cell" appears cut in half Intravascular hemolysis Microangiopathic hemolytic anemia(DIC, TTP). Prosthetic heart valves or severe valvular diseases Burns Snakebites Elliptocyte Elongated, elliptical cell Up to 10% of RBCs in normal individuals may be elliptical; amounts above this are considered abnormal Hereditary Elliptocytosis-majority of RBCs are elliptocytes. Rouleaux Linear aggregation of RBC's that resembles a stack of coins & sediment more readily. Seen when surface charge is reduced with increased serum protein, particularly increased fibrinogen or globulin Sideroblast Non-nucleated RBC with stainable iron Spur Cells Hemolytic anemia with bizarre-shaped RBCs Occurs in some patients with severe hepatocellular disease, usually advanced Laennecs cirrhosis Tear Drop Cell Also called dacrocytes Tear shaped but may also be pear shaped with a blunt pointed projection Myelophthisis-(invasion of BM by tumor, fibrosis, granulomatous process) Myelofibrosis Polycythemia Thalassemia (homozygous type) Agglutinated RBCs in Cold Agglutinin Disease Cold active IgM antibodies react against RBC antigens Fresh blood specimens agglutinate during with drawl into a cooler syringe Etiology Infection( viral & Mycoplasma), Lymphoproliferative disorders(lymphoma) Idiopathic cold agglutinin disease Symptoms Due to vasoconstriction in cold-exposed regions of circulation
Artifactual Echinocytes (Crenated cells or Burr cells) Have regularly shaped, uniformly distributed spiny projections Occur as an artifact from smear preparation or in some disease states; uremia, RBC volume loss
Left Shift Absolute increase in neutrophils with an increase in bands, & sometimes an increase in immature forms such as metamyelocytes or myelocytes, or blasts Hypersegmented Neutrophil PMN leukocytes normally have 3 or 4 lobes, but 5, 6 or more lobes indicate hypersegmentation Seen most often with megaloblastic anemias, sometimes with myeloproliferative disorders, or following chemotherapy (methotrexate) Toxic Changes of Neutrophils Toxic Neutrophil & monocyte Refers to alterations in morphology of neutrophil in response to infection, inflammation, or stress Toxic Granulations Large darkly staining granules resulting from neutrophilic stimulation by foreign antigens Seen most often with bacterial infections & in association with cytoplasmic vacuolization Tend to cluster together Dhle Body
Pale or grayish, round or elongated bodies usually seen close to cell membranes Usually seen 1 to 3 days after an infection, burn, surgery, or other trauma & then disappear Vacuolation of the Cytoplasm Seen in infections: especially common in septic processes caused by bacteria or fungi Can be caused by phagocytosis of extracellular material Chediak-Higashi Syndrome Rare disorder with large neutrophilic granules representing abnormal lysosomes Pelger-Huet Anomaly Autosomal dominant condition with neutrophils that are mostly bilobed in heterozygote (normal function) & unilobate in homozygote (fatal) Atypical (Reactive) Lymphocytes Larger (more cytoplasm) & have nucleoli in their nuclei. Cytoplasm tends to be indented by surrounding RBC's. Nucleus may be eccentrically placed & may have irregular borders & indentations Cytoplasm contains areas that stain a darker blue due to their increased RNA content. Often associated IM Qualitative Abnormalities of WBCs Leukocytosis Increased amount Leukopenia Decreased amount Presence of immature forms in peripheral blood Erytroleukoblastic Blood Picture Leukemia's Leukemoid Reaction Causes of Neutrophilia Infections (localized and generalized) Inflammation Metabolic: uremia, gout, acidosis, poisoning Hemorrhage & acute hemolysis Myeloproliferative diseases Tissue necrosis Physiologic conditions Steroid administration Decreased/ineffective production Severe bacterial infections, sepsis, miliary TB, Zoonotic infections Viral infections (EBV, HepB, influenza, measles, rubella, psittacosis) Ricketsia infections Ionizing radiation Hematopoietic diseases Severe renal injury Causes of Neutropenia Drugs and chemicals Sulfonamides Antibiotics Analgesics Antithyroid drugs B12 or folic acid deficiency Myelodysplasia, anaplastic anemia, myelophthisis Conditions with decreased WBC survival Feltys syndrome, SLE, autoimmune neutropenia, splenic secquestration/hypersplenism Neonatal & Infantile causes Maternal Inborn defects of metabolism Immune defects Disorders of myeloid stem cell proliferation Benign chronic granulocytopenia in childhood
Pregnancy: progressive decrease. Causes of Leukemoid Reactions Myelocytic Infections (endocarditic, pneumonia, septicemia, leptospirosis) Burns Eclampsia Neoplasia (colon, kidney) Post treatment of Meg. Anemia Hemorrhage & hemolysis Lymphocytic Infectious mononucleosis Pertussis Varicella TB Carcinoma of stomach Carcinoma of breast Dermatitis (some types) Monocytic TB (miliary form) Leukoerythroblastic Reaction Similar to leukemoid reaction with addition of nucleated RBC/s & schistocytes, dacrocytes (tear dropped) Presence of precursor cells of myeloid & erythroid lineage. Anisocytosis, poikilocytosis, & polychromasia Giant platelets Causes of Leukoerythroblastosis Myelofibrosis Metastatic CA Breast Cancer Lung Cancer, Small Cell & Non-Small Cell Prostate Cancer: Metastatic and Advanced Disease Sarcoidosis Tuberculosis Lipid Storage disorders (Gaucher Disease) Causes of a Monocytosis Leukemias, particularly monocytic Malignant lymphomas Lipid storage diseases Post-splenectomy Protozoan, rickettsial & bacterial infections UC, Crohns disease, sprue Causes of Eosinophilia Allergic diseases Parasitic infestation Fungal & infectious diseases (some) Collagen-vascular diseases Hematopoietic diseases Immunodeficiency disorders Endocrine hypofunction Postradiation Others (tumors, hypereosinophilic syndrome, sarcoidosis, drugs) Causes of Basophilia Myeloproliferative disorders CML Polycythemia Hodgkins disease Chronic sinusitis Myxedema Nephrosis
Serum sickness Radiation Causes of Increased Plasma Cells Plasma cell leukemia, CLL, multiple myeloma Lymphomas & certain cancers Cirrhosis of liver Collagen-vascular diseases Bacterial infections (syphilis, TB) Parasitic infestation Viral infections Serum reaction Auer Rods in AML Very large, immature myeloblasts with many nucleoli. Distinctive feature of these blasts is a linear red "Auer rod" composed of crystallized granules. Acute Lymphoblastic Leukemia (ALL) Leukemic cells in characterized by round or convoluted nuclei, high nuclear/cytoplasmic ratio & absence of cytoplasmic granules. Chronic Myelocytic Leukemia(CML) Low Powered Leukocytosis with presence of precursor cells of myeloid lineage. Basophilia, eosinophilia, & thrombocytosis seen High Powered WBCs are present in all stages of maturation, with a characteristic predominance of segmented neutrophils & myelocytes ("myelocyte bulge"). Numbers of basophils & eosinophils) are increased. Chronic Lymphocytic Leukemia (CLL) PBS Patient presented with a WBC count of 130,000/ul. WBCs were nearly all mature appearing lymphocytes. Most of WBCs are small to medium-sized lymphocytes. Many smudged lymphocytes present. Hairy Cell Leukemia (HCL) PBS demonstrating lymphocytosis & absence of any other type of blood cell (pancytopenia). Characteristic cytoplasmic projections are already visible Normal Hemostasis Divided into primary & secondary components & is initiated when trauma, surgery, or disease disrupts vascular endothelial lining & blood is exposed to subendothelial connective tissue Primary Hemostasis Name given to process of platelet plug formation at sites of injury. It occurs within seconds of injury & is of prime importance in stopping blood loss from capillaries, small arterioles, & venules Major Events in Primary Hemostasis 1. Platelet adhesion, interaction of platelets with a non platelet surface 2. Platelet activation & secretion. 3. Platelet Aggregation binding of activated platelets to adherent monolayer Secondary Hemostasis Reactions of plasma coagulation system that result in fibrin formation. Requires several minutes for completion. Fibrin strands produced strengthen primary hemostatic plug. Particularly important in larger vessels & prevents bleeding from recurring hours or days after injury. Reactions are regulated by antithrombin, which forms complexes with all of coagulation protein serine proteases except factor VII, & Protein C & protein-S system, which inactivates factors V & VIII. Coagulation Pathways Two independent activation pathways Contact system or intrinsic system Tissue factor-mediated or extrinsic system.
Approach to the Bleeding Patient
Merge at point of factor X (Common Pathway) activation & lead to generation of thrombin, which converts fibrinogen into fibrin. Coagulation Cascade Hypothesis Intrinsic System Factor XII Prekallikren(PK) High-molecular weight kininogen(NK) Factor XI Factor VIII Factor IX Extrinsic System Factor VII Tissue factor Common Pathway Factor X Factor V Factor II Factor I(fibrinogen) Screening Tests for Bleeding Disorders Activated partial thromboplastin time(aPTT) Assesses coagulation proteins of intrinsic system & common pathway Mixture of a negatively charged surface, phospholipid, & plasma is incubated for a few minutes Calcium chloride added & time required for clot formation is measured Measures proteins of intrinsic system factor (XII, PK, HK, factor XI, factor IX & factor VIII) & proteins of common pathway(factors X, V, II, & fibrinogen) Normal 20-36 sec Differential Diagnosis of Prolonged aPTT Only Disorders associated with bleeding Factor VIII deficiency or defect is sex-linked & may be congenital or acquired. Congenital factor VIII deficiency(Hemophilia A) occurs only in males Factor IX deficiency(Hemophilia B) is sex linked Factor XI deficiency is autosomal recessive Disorders not associated with bleeding Factor XII deficiency is autsomal recessive & most common (prolonged aPTT) Deficiency of Prekallikren(PK) is a autosomal recessive (mildly prolonged aPTT) Deficiency of High-molecular weight kininogen( HK) is autosomal recessive & extremely rare Lupus anticoagulants- antiphospholipid antibodies that interfere with coagulation reactions Prothrombin Time(PT) Assesses coagulation proteins of extrinsic system & common pathway Tissue thromboplastin & plasma are incubated for a few minutes Plasma is recalcified & time required for clot formation is measured Prothrombin Time(PT): 10-12 sec-test International Normalized Ratio(INR): standardizes PT from lab to lab Measures extrinsic system activated factor VII(VIIa), & tissue factor & proteins of common pathway(factors X, V, II, & fibrinogen) Differential Diagnosis of Prolonged PT Only Usually indicates factor VII deficiency May also be seen in patients who have dysfibrinogenemia (abnormal fibrinogen) or a deficiency in coagulation factor X, V, or II Platelet count Used to exclude a quantitative platelet defect as cause of a bleeding disorder Platelet number(150,000-450,000) Bleeding time Forearm is scratched & time until bleeding stops is measured Assesses platelet number & function Bleeding time: Normal 2-9 minutes
Affected by ASA Thrombin clotting time (TCT) Purified thrombin is added to plasma to determine time for clot formation Direct measure of fibrinogen function Pathogenesis of Bleeding Disorders All bleeding disorders caused by one of three defects: 1. Plasma protein defects (defect in one or more plasma coagulation, fibrinolytic, or anticoagulant proteins) 2. Platelet abnormality( a defect in hemostatic cell fragment) 3 Defect in platelet-endothelial cell interactions( defect in adhesive interactions between platelets & vessel wall)` Platelet Abnormalities Quanitative Platelet Disorders Thrombocytopenia Decreased number of platelets & relatively common disorder Mechanisms Decreased production/ineffective production Increased destruction Sequestration in spleen Etiologies of Thrombocytopenia Decreased Production Aplastic Anemia Bone marrow hypoplasia Radiation Chemotherapy drugs Fanconi Syndrome- a genetic aplastic anemia Viral infections Thrombopoietin deficiency Leukemia Metastatic Carcinoma Ineffective Production Alcohol abuse Megoblastic conditions Severe iron deficiency anemias Paroxysmal nocturnal hemoglobinuria May-Hegglin, Wiskott-Aldrich, & Bernard-Soulier syndrome Increased Destruction/Loss Non-Immune processes Sepsis Extensive Burns DIC Severe hemorrhage with extensive transfusion Drugs Immune Processes Neonatal purpura Result of placental crossing of maternal antibodies directed against antigens on fetal platelets Post- transfusion purpura Immune thrombocytopenia purpura(ITP) Results from autoantibodies directed against platelets May be idiopathic or associated with SLE, lymphoma, or HIV May be acute or chronic disorder Platelet counts are typically < 50,000 with an increased number of large platelets IgG & less frequently IgA, & IgM Antibodies bound to surface of platelet can be demonstrated in most cases ITP Diagnostic Findings
CBC-thrombocytopenia(if < 20,000-may have spontaneous bleeding BM Aspirate & Biopsy: Normal with increased numbers of megakaryocytes Treatment(may not be needed unless platelet count < 20,000 or bleeding is occurring) A. Initial treatment: glucocorticosteroids B. Temporary Phagocytic blockade: IV immune globulin;anti-Rh-D, WinRo) May be given if steroids dont work Expensive and risk of hepatitis C C. Splenectomy 1. Performed if medical Rx. fails or patient extremely ill 2. Definitive Rx. for chronic ITP after initial control of disease Thrombotic thrombocytopenia(TTP) Etiology Associated with pregnancy, metastatic cancer, highdose chemotherapy & other drugs Abnormal increase in vWF activity & endothelial injury results in formation of widespread thrombi in microcirculation Clinical Findings TTP Classical pentad(40% ) Thrombocytopenia & purpura Hemolytic anemia with schistocytes Renal failure Neurologic problems (waxing and waning consciousness; transient, focal neurologic defects) Fever Triad of findings( 75%) Thrombocytopenia with purpura Neurologic defects Hemolytic anemia with schistocytes Treatment Delay in Rx may result in sudden death; mortality approaches 100% if not treated Exchange transfusion(removal of most of patients blood followed by transfusion of equal amount of donor blood) Intensive plasmapheresis(removal of plasma from patient) coupled with infusion of FFP Platelet transfusions are CONTRAINDICATED(will promote increased formation of platelet thrombi
Qualitative Disorders of Platelet Function May be hereditary or acquired Occur as a primary process or secondary to another condition Suspect in a patient presenting with easy bruising, nose bleeds, menorrhagia, or other bleeding tendencies, but yielding a platelet count that is within or very near normal reference range & abnormal bleeding time Tests of Platelet Function Bleeding Time (ref. range 2-9 minutes) Time required for a wound of standardized length & depth to stop bleeding, simple test sensitive to abnormalities of both number & function, but primarily used in evaluation of platelet adhesion
Prolonged in thrombocytopenia, von Willebrands disease, severely decreased or absent fibrinogen, & other platelet disorders von Willebrand Factor Assay von Willebrand factor (vWF) functions to assist in platelet aggregation Platelet Factor Assays Platelet factor III (PF3) activity which measures ability of platelets to provide a surface for factor binding Platelet factor IV (PF4) - beta - thromboglobulin (protein in alpha-granules that can bind heparin) Platelet Aggregation Test Standardized concentration of an aggregating substance (e.g., ADP, epinephrine, thrombin, ristocetin regent) is added to a substance of platelet - rich plasma & changes in light transmission are measured Useful aid in DD between hereditary & acquired disorders of platelet function Functional Abnormalities of Platelets Defects of platelet adhesions Uremia DIC Defects in platelet aggregation Seen in conditions where fibrinogen is absent or reduced & where glycoprotein complexes are absent or insufficient in number Afibrinogenemia Glanzmanns thrombasthenia Platelet release defects Primary Storage pool disease Wiskott-Aldrich Syndrome Secondary Uremia Aspirin Alcohol Acquired Defects of Platelet Function Medications Aspirin NSAIDs Dipyridamole Heparin Penicillin, esp Carbenicillin, Ticarcillin Alcohol Disease process Vitamin B 12 or folate deficiencies Myeloproliferative disorders Uremia Cirrhosis Dysproteinemias DIC Myelodysplastic syndromes Von Willebrands Disease(vWD) Most common inherited bleeding disorder: 1/800-1/1000 people affected Deficiency or decreased function of Von Willebrand factor(vWF) results in decreased platelet function & decreased factor VIII activity vWF attaches platelets to injured endothelium & carries factor VIII in plasma Diagnostic Findings Decreased plasma vWF concentration & activity Prolonged bleeding time Decreased plasma factor VIII activity Prolonged aPTT Because of decreased factor VIII
Intrinsic coagulation pathway affected Variants Type 1: most common;autosomal dominant inheritance; mild to moderate decrease in vWF level Type 2: vWF does not function properly Type 3: no vWF; extremely rare Bleeding Manifestations Excessive bleeding after minor surgical procedures Mucocutaneous bleeding with normal platelet count Superficial brusing (common) Petechiae(rare) Gingivial bleeding Epistaxis Mennorhagia GI mucosal bleeding Immediate bleeding after dental extraction Postpartum hemorrhage Spontaneous hemarthrosis rare; usually in type 3 Treatment Factor VIII concentrates with high molecular weight vWF multimers (Humate-P); up to 10 bags bid for 48-72 h depending on severity of bleeding Desmopressin (DDAVP): a vasopressin analogue-increases level of vWF; given intranasally for pts with type I vWD (mild-moderately severe disease) Cryoprecipitate: plasma product rich in factor VIII containing vWF Disorders of Intrinsic Coagulation System Hereditary(single factor deficiency) Hemophilia A: factor VIII deficiency Overview Most common of the hemophilia with an incidence of 1-2 cases per 10,000 male births Genetics Inherited as a sex-linked recessive disorder Sons of a hemophilic man & a normal woman do not inherit paternal hemophilia(XY) All daughters of such a union are obligate carriers (XXh). A carrier has equal chances of having a normal (XY) or hemophilic (XhY) son & a normal daughter or a daughter who carries hemophilia gene on one of her X chromosomes XXh) Of newly diagnosed patients with factor VIII deficiency, 30% have no family history of hemophilia because there is an inherent de novo spontaneous mutation rate of that portion of X chromosome Bleeding symptoms of factor VIII deficiency may be expressed in females Turner Syndrome(XhO) Double heterozygote for factor VIII deficiency(XhXh)-daughter of a mother who is a carrier of factor VIII deficiency & a father who has hemophilia A Clinical Presentation Severe Disease(< 1% factor VIII activity) Presents shortly after birth as cephalohematoma or profuse bleeding at circumcision; may present with spontaneous soft tissue or joint bleeding when child crawls or walks Moderate disease(1-5% factor VIII activity) Presents when child walks or crawls with spontaneous hemarthrosis or soft tissue bleeding; may present with extensive bleeding after moderate trauma Mild disease( > 5% factor VIII activity) Presents in adolescence or young adulthood(e.g. as unexplained bleeding during tooth extraction) infrequent bleeding; usually secondary to trauma Bleeding Manifestations in Hemophilia Bleeding after circumcision Delayed oozing from deep lacerations Protracted bleeding after dental extractions IM hematomas Intraarticular hemorrhage
CNS bleeding Hematuria Laboratory Evaluation Hemophilia A Factor VIII levels < 30% can be reliably detected using the aPTT as a screening test Routine aPTT screening alone misses some patients with hemophilia because aPTT is not always prolonged with mildly decreased factor VIII levels(i.e.,25%-49%) PT, bleeding time & thrombin clotting time(TCT) are normal in factor VIII deficiency Treatment of Hemophilia A Factor VIII concentrate (recombinant or highly purified) Cryoprecipitate factor VIII activity as FFP in 1/10 the original volume Used if factor VIII concentrate is not available Factor IX deficiency (Hemophilia B) Overview Account for 10% of hereditary coagulation factor deficiencies Incidence is 1 in 30,000 live male births Along with factor VIII deficiency, is most severe bleeding state that allows for normal gestation & delivery Genetics X-linked recessive disorder, although 30% of patients may have no other affected family members but instead carry a spontaneous new mutation Clinical Presentation Identical to those of factor VIII deficiency Diseases are indistinguishable without specific factor assays Laboratory evaluation Levels of factor IX below 50% result in prolonged aPTT Specific factor assay for factor IX is diagnostic PT, thrombin clotting time & bleeding time normal Treatment Factor IX concentrate (recombinant or highly purified) FFP Plasma fraction enriched in prothrombin complex proteins Factor XI deficiency (Hemophilia C) Overview Rare, occurring in 1 of 100,000 persons Genetics Incompletely recessive autosomal trait High predilection in Ashkenazi Jews of eastern European descent(50% of cases) Clinical Presentation Bleeding symptoms are less severe than in moderate or severe factor VIII or IX deficiency 50% of patients bleed after surgery or trauma; remainder have relatively minor symptoms & are identified only by an abnormal PTT Symptomatic patients typically have spontaneous nosebleeds, hematuria, & mennorhagia Bleeding with dental extractions and urological procedures Clinical symptoms tend to be similar within affected family members Laboratory Evaluation aPTT is prolonged PT, thrombin clotting time & bleeding time are normal Reduced factor XI is diagnostic Bleeding is most likely to occur in individuals with levels below 10% Disorders of the Common Pathway: Factors V, X, & II Overview Deficiencies of these proteins are rare disorders of autosomal recessive inheritance Incidence is < 1 in 1 million Clinical Presentation Patients present with soft tissue and spontaneous bleeding. Only severe factor V and X deficiencies are associated with hemarthrosis
Laboratory Evaluation PT and a PTT are both prolonged in deficiencies of these factors Thrombin clotting time is normal Disorders of the Extrinsic Coagulation System: Factor VII Deficiency Genetics Inherited in an autosomal recessive pattern Heterozygous individuals are usually asymptomatic Clinical Presentation Factor VII levels < 1% are associated with severe spontaneous hemorrhage and intraaticular bleeding Factor VII levels as low as 10% seem to protect against severe bleeding symptoms Laboratory Evaluation Factor VII deficiency is the only cause of an isolated prolonged PT aPTT, bleeding time, and thrombi clotting time are normal Disorders of Fibrinogen Hereditary afibrinogenemia Rare disorder with only 150 cases reported Autosomal recessive No clotting or antigenic fibrinogen is detected Hereditary hypofibrinogenemia More common than afibrinogenemia Some cases are actually dysfibrinogenemia with normal amounts of fibrinogen but functionally abnormal Clinical Presentation Prolonged umbilical stump bleeding Intracranial hemorrhage Intraarticular bleeds GI and mucosal bleeding frequent Most patients with dysfibrinogenemia are asymptomatic & diagnosed during lab screening If concentration of normal fibrinogen is greater than 100 mg/dL there is a decreased tendency to hemorrhage Laboratory Evaluation PT, aPTT, & thrombin clotting time are all markedly abnormal in afibrinogenemia,& to a lesser extent in hypofibrinogenemia In dysfibrinogenemia, PT aPTT, & thrombin clotting time are variably prolonged with PT & thrombin clotting time being most sensitive screening test Acquired Disorders of Blood Coagulation Most common forms of bleeding encountered in practice Often result of medical treatment or a manifestation of an underlying disease state rather than specific abnormalities of the hemostatic system Usually cause prolongation of PT, PTT or both Causes Anticoagulation defects Occur in patients who are taking anticoagulant agents to treat venous thrombosis, MI,CVA, & others Management of these pts involves achieving a balance between preventing thrombosis & preventing excessive bleeding Usually interfere with PT & aPTT but do not prolong the bleeding time Medications that interfere with coagulation proteins Heparin Carbohydrate polymer that forms complexes with antithrombin & other plasma protease inhibitors Complexes inhibit major enzymes of hemostatic system: thrombin, factor Xa, & to a lesser extent factors IXa, XIa, XII & kallikren Prolongs aPTT to a greater degree than PT Does not dissolve clots Low-molecular-weight heparin (LMWH) Smaller more highly purified carbohydrate polymer
Directed primarily at factor Xa Some preparations also inhibit activity of thrombin At most therapeutic doses, these preparations do not prolong the PT or aPTT Warfarin (Coumadine) Vitamin K antagonist of 2 enzymes that are essential for carboxylation reactions of certain amino acids in coagulation factors VII, IX, X,& II & proteins C, S & Z Prolongs PT more significantly than aPTT Vitamin K Deficiency Impairs production of factors II(prothrombin), VII, IX, & X Co-factor in carboxylation of glutamate residues or prothrombin complex proteins Major source of vitamin K is dietary(esp, green vegetables), with minor production by gut bacteria Etiology Inadequate dietary intake especially when associated with antibiotic therapy (kills GI bacteria which make Vit K) Intestinal malabsorption Cirrhosis (liver makes bile acids to absorb Vit K) Laboratory features Elevation of PT & aPTT Treatment Vitamin K 10 mg IM or slow IV FFP if hemorrhage is occuring(has all coagulation factors) Liver Disease Liver synthesizes all coagulation proteins &clears activated products of coagulation Results in deficiencies of all clotting factors except VIII May be factor also in Vit K deficiency Structural manifestation of liver disease also promote bleeding(portal HTN, varices, gastritis & hemorrhoids) Lab Features Elevated PT Normal or elevated PTT Treatment FFP Cryoprecipitate DIC Clinicopathologic syndrome of activated coagulation Causes bleeding or thrombosis because of loss of balance between clot promoting and clot-lysing systems in vivo Clinical spectrum ranges from a bleeding state to a prothromic state Not a specific diagnosis; it always indicates underlying disease Bleeding associated with DIC is usually result of excessive fibrinolysis Thrombosis associated with DIC is result of excess thrombin formation Characterized by presence of thrombin plasmin Etiologies of Acute DIC Infectious Causes Most common cause is sepsis Gram-positive & gram-negative septicemia Typhoid fever Rocky Mountain spotted fever Viremia Parasites Obstetric Causes Abruptio placentae Amniotic fluid embolism Hypertonic saline abortion Eclampsia Hemolytic transfusion reaction Acute promyelocytic leukemia
Major Trauma Burns Head injury GSW Frost bite Crush injuries Heat stroke Snakebite Fresh water drowning Miscellaneous Homozygous protein C & S deficiency Factor V Leiden Severe liver disease Heparin induced thrombocytopenia & thrombosis syndrome Necrotizing enterocolitis Renal homograft rejection Dissecting aortic aneurysm Etiologies of Subacute DIC Usually a prothrombic condition resulting from increased thrombin formation Malignant Mucinous adenocarcinoma that may manifest as trousseau syndrome (migratory thrombophlebitis, marantic endocarditis (fibrin on heart valves), and arterial embolization Obstetric Retained dead fetus Vascular Connective disease disorders Giant cavernous hemangioma Chronic renal disease Venous thrombosis Pulmonary embolus Clinical Presentation of DIC Acute May be explosive & life threatening Most pts: extensive bleeding in skin & mucous membranes; hemorrhage from surgical incisions, venipuncture, or catheter sites; mouthorgan failure may occur Subacute or Chronic More typical in cancer patients Can become symptomatic with surgery or chemotherapy Thrombosis my dominate clinical picture Diagnostic Findings in DIC Mechanical fragmentation of RBC Formation of schistocytes Hemolytic anemia Consumption of platelets, coagulation factors & fibrinogen: Thrombocytopenia Prolonged PT & aPTT Decreased fibrinogen Fibrinolysis (degradation of fibrin clots) Increased fibrin degradation(or split) products:FDP(or FSP) Increased dimers Laboratory Evaluation of DIC Screening include PT, aPTT, platelet count & fibrinogen level (1) If the findings of two of these tests are abnormal, DIC is a possible diagnosis (2) If the findings of three of these tests are abnormal, DIC is a probable diagnosis (3) If the findings of all these tests are abnormal, the diagnosis is considered to be DIC until another diagnosis is established Confirmatory tests for DIC are the D-dimer, fibrin degradation products (FDP), and fibrin monometer assays D-Dimer Assay
Measures plasmin-cleaved insoluble cross-linked fibrin which is formed when thrombin cleaves fibrinogen and leaves a soluble fibrin monomer. Plasmin cleaves the insoluble cross-linked monometer to liberate the D- dimer Fibrin degradation products assay Measures plasmin-cleaved soluble or insoluble fibrinogen or fibrin Fibrin monomer assay Measures thrombin-cleaved fibrinogen only Least reliable test for DIC and often produces false negative results Treatment of DIC Treat underlying disorder first Antibiotics for sepsis Delivery of placenta & fetus when cause is obstetrical catastrophe Supportive blood component therapy FFP Platelet concentrates Cryoprecipitate Heparin My be useful for those patients who have acral cyanosis, & digital ischemia, purpura fulminans, a retained dead fetus, migratory thrombophlebitis, or acute leukemia Massive transfusion(dilutional coagulopathy) Infusion of more than 1.5 times patients blood volume in 24 hours Acquired coagulopathy can occur as a result of dilution of plasma & platelets, increased concentration of anticoagulant sodium citrate dextrose, & depletion of calcium Acquired coagulopathy can be prevented by administering 1 unit of FFP for every 4-6 units of packed RBCs. In addition one ampule of calcium for every 4-6 units of transfused RBCs or FFP is administered to overcome the anticoagulant effect of sodium citrate Dysfibrinogenemias Usually found in patients who have acquired liver disease as a result of alcoholism or immunologic, toxic, or viral causes PT, aPTT & thrombin time is prolonged Hypergammaglobulinemic states multiple myeloma Waldenstrom macroglobulinemia Systemic amyloidosis Inhibitors to factors X, V, II and fibrinogen Heparinoids, or heparin-like anticoagulants, may be produced in patients who have an underlying malignancy Factitious bleeding disorders most often occur in an individual who is a health care professional & fakes medical illness by self-administering an anticoagulant, usually heparin or warfarin Defect in platelet-endothelial cell interactions Defect in the adhesive interactions between platelets and blood vessel wall Many causes Hemostatic Disorders due to Blood Vessel Wall Defects Aging Drugs Glucocorticoids(chronic therapy) Penicillin's Sulfonamides Vitamin C deficiency TTP Hemolytic Uremic Syndrome Henoch-Schonlein purpura Paraproteinemias Hereditary hemorrhagic telangiectasia(Osler-Rendu-Weber disease) Differential Diagnosis of Prolonged aPTT & PT Acquired Medical Conditions
Transfusion & Pheresis Therapy
DIC, liver disease, vitamin K deficiency, use of anticoagulants (heparin, warfarin), & massive transfusion Dysfibrinogenemia Occurs when abnormal fibrinogen molecules do not participate properly in coagulation reactions Coagulation protein defects of common pathway (factor X, V, or II) -Rare cases DDx. of Prolonged Bleeding Time with Normal platelet count Von Willebrand factor Platelet function defect Quantitative decrease in platelet count(< 100,000) will increase bleeding time Rare connective tissue disorders, including pseudoxanthoma elasticum, Ehlers- Danlos syndrome, & scurvy DDx of Bleeding with no abnormality in screening tests Factor XIII deficiency May be congenital or acquired. Patients bleed excessively as a result of surgery or trauma Alpha 2 Antiplasmin deficiency Absence of major serine protease inhibitor. Patients have a bleeding disorder that is caused by hyperfibrinolytic state, with lysis of any clots that are formed. Can be acquired as a result of consumption in DIC Plasminogen activator inhibitor-1 deficiency Deficiency in major serpin inhibitor of plasminogen activators. Causes increased activation of plasminogen . A profibrinolytic state occurs as a result Blood Bank Testing Tests Performed 1. Determination of blood type with a crossmatch 2. Screening for antibodies that may produce adverse effects if transfused 3. Screening for possible infectious agents that could be transmitted with transfusion Tests Performed on all Blood Collected for Transfusion ABO group & Rh type Screening for blood-group antibodies Serologic test for syphilis*** Serologic tests for human retroviruses HIV-1 antibody HIV-2 antibody HIV p24 antigen HTLV I antibodies Serologic tests for hepatitis Hepatitis B surface antigen (HBsAg) Hepatitis B core antibody (HBcAb) Hepatitis C antibody Transfusion Transmitted Diseases Hepatitis B Transmitted through parenteral & sexual exposure. Incubation time -mean of 90 days( range of 30- 180 ) Donor blood is routinely tested for HBsAg & HBcAb Risk of transmission (RT) = 1/66,000 to 1:200,000 Hepatitis C Route of transmission is parenteral, with sexual transmission uncommon Mean incubation time is 6 -8 weeks Blood Bank testing for HCV started in 1990. At present, only testing for hepatitis C antibody available. Risk of transmission (RT) = 1/121,000 Human Immunodeficiency Virus (HIV) First testing of blood products for HIV started in 1985 detects presence of antibody directed against HIV. Testing for HIV p24 antigen mandated in 1996. Risk of transmission = 1/563,000 to 1/825,000 Human T-lymphocytotrophic Virus (HTLV-1).
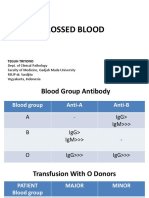
Retrovirus endemic in Japan & Caribbean. Implicated as causing adult T-cell leukemia/lymphoma & neurological disorder similar to MS. Blood is routinely screened for antibodies to HTLV-1. Risk of transmission = 1/641,000 (but only 1-3 % of seropositive individuals will develop disease Cytomegalovirus (CMV) Prevalence of CMV antibody ranges from 50 to 80% of population. Blood contaminated with CMV can cause problems in neonates or immunocompromised patients. Potential problems in selected patient populations can be prevented by transfusing CMV negative blood or frozen, deglycerolized RBC's. Donor blood is not routinely tested for CMV. Malaria Rarely transmitted by RBC products, although # of transfusion associated cases of malaria is at an all-time high. There are no practical laboratory tests available to test donor blood, so donors travelling to high risk malaria areas are excluded from donating blood for six months. Others Additional diseases which are rarely transmitted by blood products, but for which no routine costeffective laboratory testing is available include: Babesiosis Lyme disease Chagas' disease Blood Compatibility Testing (Crossmatch) Definitions Alloantigen -an antigen that occurs in some, but not in other members of same species. Alloantibodies -an antibody specific for an alloantigen Front type" Determines which antigens ("flags") in ABO blood group system are on patient's RBCs Back type Identifies isohemagglutinin (naturally occurring antibody) in patient's serum & should correspond to antigens found on RBCs In addition, RBC's are Rh typed & identified as "D" positive or negative. Type A A antigen only on RBCs; Anti B antibody in serum Type B B antigen only on RBCs; Anti A antibody in serum Type AB Both A & B antigens on RBCs Neither Anti A or Anti B antibody in serum Type O Neither A or B antigen on RBCs Has both anti A & anti B antibodies in serum Screen Looks for unexpected red cell alloantibodies which may form following pregnancy or prior transfusions. If screen + antibody is identified & 2 units lacking corresponding antigen are crossmatched for patient. Antibody identification can be complicated & take more than a day to complete. Type & Cross Determines compatibility between patient serum & donor RBCs A full crossmatch procedure takes about 45 minutes to complete Units refrigerated until used. Unit of blood must be properly labeled & label MUST be checked before use. Every unit crossmatched is removed from general inventory reserved for patient for 72 hours. Blood will ordinarily not be released for transfusion until compatibility testing is completed. Units which are crossmatched unnecessarily will deplete Blood Bank inventories & can result in blood shortages, such as those which occurred in California after earthquake. Blood shortages can result in cancellation of elective surgical procedures. Type & Cross in Emergencies Blood products may be released without a crossmatch if patient is in danger of dying if transfusion delayed.
If patient's blood type is not known, then group O Rh negative (O neg) blood can be released without compatibility testing. In cases in which patient's blood type is reliably known, type-specific blood or RBC's of same ABO & Rh group may be released Blood Preservation & Storage Blood is collected as whole blood Blood can be stored as whole blood (with all plasma present) or, much more commonly, as packed PRBC's in which about 70% of plasma has been removed. Both whole blood & PRBC's can be stored for up to 42 days at 1 - 6 degrees C. Plasma can be centrifuged heavily a second time to separate platelet rich plasma Supernatant plasma can be expressed into a third bag & stored as fresh frozen plasma (FFP). Remaining platelet rich plasma is utilized as a platelet pack Types of RBC Products Whole blood Packed red blood cells (PRBC's) Leukocyte depleted RBC's: Obtained by filtering blood through leukocyte-specific filters. Frozen, deglycerolized RBCs Transfusion Reactions Hemolytic Reactions Occur when recipient's serum contains antibodies directed against corresponding antigen found on donor RBCs Can be an ABO incompatibility or an incompatibility related to a different blood group antigen. Complications-DIC, renal failure, & death Most common cause is a clerical error, such as a mislabeled specimen sent to blood bank, or not properly identifying patient to whom you are giving blood. Allergic Reactions to Plasma Proteins Can range from complaints of hives & itching to anaphylaxis. Febrile Reactions Caused by patient antibodies directed against antigens present on transfused lymphocytes or granulocytes. Symptoms usually consist of chills & a temperature rise > 1 degree C. Transfusion related acute lung injury (TRALI) Caused when plasma contains HLA or granulocyte specific antibodies which correspond to antigens found on donor WBC's. Granulocyte enzymes are released, increasing capillary permeability & resulting in sudden pulmonary edema. Most often occurs with administration of blood products with plasma, such as FFP. Bacterial Contamination Can occur during collection Bacteria can grow during storage at room temperature & during refrigeration (psychrophilic organisms). Transfusing a contaminated unit can result in septic shock & death. Circulatory Overload Can occur with administration of blood or any IV fluid, particularly in patients with diminished cardiac function. RBC transfusions & Alloimmunization Can expose patient to RBC antigens not recognized as self. If an antibody is produced, future transfusions can be delayed because extended donor blood typing will be required to identify compatible units. O negative blood released uncrossmatched in emergencies could result in a hemolytic transfusion reaction if patient has an alloantibody produced after a previous transfusion. Platelet Transfusions & Alloimmunization Contain HLA & A & B antigens. Prior exposure to non-self HLA antigens (from WBC contamination of red cell products) can result in antibodies that will render future platelet transfusions useless Graft Versus Host Disease (GVHD) Transfused lymphocytes engraft & multiply in immunocompromised patients (BM transplant patients). Newly engrafted lymphocytes attack host tissues
Uniformly fatal & untreatable. Prevented by gamma-irradiating blood products to be transfused Therapeutic Apheresis Components of whole blood are separated Plasma (plasmapheresis) Platelets (plateletpheresis) Leukocytes (leukapheresis) Purpose is to remove a component of blood which contributes to a disease state. Whole blood is introduced into a chamber that is spinning, & blood separates into components by gravity along wall of chamber. Component to be removed can be selected Plasmapheresis Plasma contained antibodies & antigen-antibody complexes present that may contribute to deleterious effects of autoimmune diseases Removal of plasma (& replacement with saline solution) will help to reduce circulating antibodies & immune complexes. Hyperviscosity states(Wladenstroms macroglobulinemia TTP Immune-complex and autoantibody disorders (Goodpastures syndrome, rapidly progressive glomerulonephritis, myasthenia gravis; possibly Guillain-Barre, SLE, ITP)*** Cold agglutinin disease, cryoglobulinemia Leukapharesis Removal of WBCs Most often used in acute leukemia, -AML in cases complicated by marked elevation(>100,000/uL) of peripheral blast count Lowers risk of leukostasis(blast-mediated vasoocclusive events resulting in CNS or pulmonary infarction, hemorrhage) Used to harvest hematopoietic stem cells from peripheral blood of cancer pts Such cells are then used to promote hematopoietic reconstitution after high-dose myeloablative therapy Plateletpheresis Used in some pts with thrombocytosis associated with myeloproliferative disorders with bleeding & /or thrombotic complications Removal of platelets can help to avoid complications of thrombosis & bleeding. Also use to enhance platelet yield from blood donors Blood Donation Whole blood is collected from healthy donors who are required to meet strict criteria concerning Medical history Physical health Possible contact with transfusion-transmissible infectious diseases, including a history of Sexual behavior Drug use Travel to areas of endemic disease (e.g., malaria) Potential donor Be in good health &feeling well on day of donation. Be on no prescribed medication that would cause donor a problem when donating or that would affect recipient Have a Hgb level which meets established U.S. FDA standard. Wait 56 days before giving another donation of whole blood. Autologous Donation Occurs when a person donates his or her own blood for personal use. Use of pts own stored blood avoids hazards of donor blood Useful in pts with multiple RBC antibodies Pace may be accelerated using erythropoietin(50-150 U/kg SC 3x week in setting of normal iron stores Since blood is not be used for anyone else, units positive for infectious agents & units with irregular blood group antibodies are acceptable If an autologous unit is collected but not used by patient-donor, then it is destroyed. Because of potential risk for a clerical error with mistransfusion of an autologous unit in inventory, units positive for hepatitis B (HBsAg) & human immunodeficiency virus (HIV) are not allowed into Blood Bank.
Hemodilution Patient's blood is collected prior to surgery & replaced with a plasma expander. Theory is that any bleeding during surgery will lose fewer RBC's. Previously collected, higher HCT blood can be given back to patient following surgery. Cell Saver/Wound Drainage Device is used to collect blood in operative field during surgery, wash it, & return it with saline to patient. Will work as long as the operative field is not contaminated with bacteria or with malignant cells. Blood is collected from cavities & returned through a filter which removes big items like thrombi & tissue fragments, but does not remove inflammatory chemical mediators or cytokines Whole Blood Transfusions Indicated when acute blood loss is sufficient to produce hypovolemia Provides both oxygen-carrying capacity & volume expansion In acute blood loss, hematocrit may not accurately reflect degree of blood loss for 48 h until fluid shifts occur RBC Transfusion Indicated for symptomatic anemia unresponsive to specific therapy or requiring urgent correction One unit of packed RBCs raises Hgb by approximately 1 g/dL May be indicated in pts who are symptomatic from cardiovascular or pulmonary disease when Hgb is between 7 -9 g/dL If used instead of whole blood in setting of acute hemorrhage packed RBCs, FFP , & platelets in an approximate ratio of 3:1:10 units are an adequate replacement for whole blood Complications RBC Transfusion Transfusion reaction-immediate or delayed seen in 1-4% of transfusions-IgA-deficient pts at particular risk for severe reaction Circulatory overload Iron overload 1unit contains 200-250 mg iron; Hemochromatosis may develop after 100 U of RBC's in absence of blood loss Graft-versus-host disease Alloimmunization Reduce Risk of Complications Removal of leukocytes reduces risk of alloimmunization & transmission of CMV Washing to remove donor plasma reduces risk of allergic reactions Irridation prevents graft-versus-host disease in immunocompromised patients Iron chelation therapy with deferoxamine indicated to reduce risk of hemochromatosis in those at risk Platelet Transfusion Prophylactic transfusions usually for platelet count < 10,000/uL(< 20,000/uL in acute leukemia) 1 unit elevates count by about 10,000/uL if no platelet antibodies are present as a result of prior transfusions Efficacy assessed by 1-h & 24-h posttransfusion platelet counts HLA-matched single donor platelets may be required in pts with platelet antibodies Most common means for supplying HLA matched platelets to patients who have become HLA sensitized & require platelets from a single donor whose HLA type matches theirs. Transfusions of Plasma Components FFP Source of coagulation factors, fibrinogen, antithrombin, & protein C & S Used to correct coagulation factor deficiencies, DIC rapidly reverse warfarin effects & treat TTP Cryoprecipitate Source of fibrinogen, factor VIII, & von Willebrand factor May be used when recombinant factor VIII or factor VIII concentrates are not available
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Hyperliidemia Meds.Документ2 страницыHyperliidemia Meds.jrubin83669Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Pneumonia PDFДокумент3 страницыPneumonia PDFjrubin83669Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hematologic DisordersДокумент7 страницHematologic Disordersjrubin83669Оценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Cardiac Meds To MemorizeДокумент4 страницыCardiac Meds To MemorizekellyaeОценок пока нет
- Stud TabДокумент34 страницыStud Tabjrubin83669Оценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- PHM321Y Antibiotics: Amoxicillin Amoxicillin-ClavulanateДокумент3 страницыPHM321Y Antibiotics: Amoxicillin Amoxicillin-Clavulanatejrubin83669Оценок пока нет
- MI LABS ExplainedДокумент3 страницыMI LABS Explainedjrubin83669Оценок пока нет
- MI LABS ExplainedДокумент3 страницыMI LABS Explainedjrubin83669Оценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Review Notes 2000 - CardiologyДокумент58 страницReview Notes 2000 - Cardiologyeliaszavaleta100% (1)
- UA ResultsДокумент7 страницUA Resultsjrubin83669Оценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Blood Bank: Hospital Standards For Accreditation For AfghanistanДокумент15 страницBlood Bank: Hospital Standards For Accreditation For AfghanistanmahdaniОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Pre Transfusion TestingДокумент67 страницPre Transfusion TestingPaulino GarciaОценок пока нет
- Branham - Transfusion Medicine Instructional PlanДокумент12 страницBranham - Transfusion Medicine Instructional Planapi-610404410Оценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Blood Grouping & Transfusion: - DR Kaberi deДокумент22 страницыBlood Grouping & Transfusion: - DR Kaberi deSrishti GoenkaОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Association of Veterinary Hematology and Transfusion Medicine (AVHTM) Transfusion Reaction Small Animal Consensus Statement (TRACS) Part 2 - Prevention and MonitoringДокумент22 страницыAssociation of Veterinary Hematology and Transfusion Medicine (AVHTM) Transfusion Reaction Small Animal Consensus Statement (TRACS) Part 2 - Prevention and MonitoringLaboratório de Patologia ClínicaОценок пока нет
- Medsurg (112) Rle: Care of Patients With Problems of The Hematologic SystemДокумент5 страницMedsurg (112) Rle: Care of Patients With Problems of The Hematologic SystemChelsea Faith SarandiОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Advanced Workflow OperationДокумент21 страницаAdvanced Workflow OperationPatriciaОценок пока нет
- Venesection: Phlebotomy orДокумент20 страницVenesection: Phlebotomy orVera June RañesesОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Blood Grouping and Cross MatchingДокумент2 страницыBlood Grouping and Cross MatchinganupreetОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Blood: Chapter 10 - Human Anatomy and PhysiologyДокумент129 страницBlood: Chapter 10 - Human Anatomy and PhysiologyDjhica Nicolle TilosОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Uncrossed Blood: Teguh TriyonoДокумент15 страницUncrossed Blood: Teguh TriyonoHerlina InaОценок пока нет
- Assessment of Hiv Aids Among Intending DonorsДокумент48 страницAssessment of Hiv Aids Among Intending DonorsmubarakОценок пока нет
- GM.007 Crossmatch Anti IgG Gel CardДокумент10 страницGM.007 Crossmatch Anti IgG Gel CardKarl GutierrezОценок пока нет
- Bad Blood - Fatal Hospital Blood Transfusion InvestigationДокумент14 страницBad Blood - Fatal Hospital Blood Transfusion InvestigationMark J. RochesterОценок пока нет
- BB Book 2017Документ111 страницBB Book 2017Glens PineappleОценок пока нет
- Form Blood RequisitionДокумент2 страницыForm Blood Requisitionshubham kumar ram100% (1)
- In Practice Blood Transfusion in Dogs and Cats1Документ7 страницIn Practice Blood Transfusion in Dogs and Cats1何元Оценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- 2021 ISFM Consensus Guidelines On The Collection and Administration of Blood and Blood Products in CatsДокумент23 страницы2021 ISFM Consensus Guidelines On The Collection and Administration of Blood and Blood Products in CatsNurul Izzatul AnnisaОценок пока нет
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2018-2114)Документ97 страницMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2018-2114)Wiwik SundariОценок пока нет
- Blood Bank HarrДокумент7 страницBlood Bank HarrAhrisJeannine EscuadroОценок пока нет
- Hazards of Blood TransfusionДокумент2 страницыHazards of Blood TransfusionSakshi ShuklaОценок пока нет
- Blood Bank Case 1 KeyДокумент4 страницыBlood Bank Case 1 KeyGissele Palero75% (8)
- Study of The Ratio of Cross-Matching To Transfusio PDFДокумент7 страницStudy of The Ratio of Cross-Matching To Transfusio PDFampratikna 14Оценок пока нет
- Immuno Lab FinalsДокумент9 страницImmuno Lab FinalsJuzhley PerezОценок пока нет
- MCQ's Blood BankДокумент74 страницыMCQ's Blood BankAlireza Goodazri100% (2)
- DAV College For Girls BVOC MLTДокумент19 страницDAV College For Girls BVOC MLTgirdhargopal87Оценок пока нет
- Mtap BB 1Документ23 страницыMtap BB 1Jennie Grace MaloomОценок пока нет
- Cross MatchingДокумент3 страницыCross MatchingTP RMad100% (7)
- Blood Group Compatbility TestДокумент46 страницBlood Group Compatbility TestArslan ArshadОценок пока нет
- Blood Groups SystemsДокумент7 страницBlood Groups SystemsMir jaliesОценок пока нет