Академический Документы
Профессиональный Документы
Культура Документы
JNatScBiolMed41134-3785895 103058 PDF
Загружено:
scaindrianie29030 оценок0% нашли этот документ полезным (0 голосов)
12 просмотров0 страницmedical
Оригинальное название
JNatScBiolMed41134-3785895_103058.pdf
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документmedical
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
12 просмотров0 страницJNatScBiolMed41134-3785895 103058 PDF
Загружено:
scaindrianie2903medical
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 0
134 Journal of Natural Science, Biology and Medicine | January 2013 | Vol 4 | Issue 1
Prevention of post-partum hemorrhage by rectal
Misoprostol: A randomized clinical trial
Abstract
Background: Post-partum hemorrhage (PPH) is a common cause of maternal mortality in developing countries. This trial was
conducted to study the effectiveness and safety of rectal misoprostol for PPH. Aim: To assess the effectiveness and safety of
misoprostol and comparing with oxytocin for prevention of PPH. Materials and Methods: Women were randomized to receive
either two 200 mg rectal misoprostol tablets (study group) or 20 units oxytocin in 1000 cc normal saline intravenously (control group).
The outcomes were incidence of PPH, amount of blood loss, duration of labor, incidence of side effects, pre- and post-delivery
hemoglobin, and use of additional uterotonics. Finding: The incidence of PPH was 12% in the study group and 10% in the control
group (P>0.05). No signifcant difference was observed between the groups hematocrit (P>0.05). Other variables including
severe PPH and duration of the third stage of labor were similar in both groups. Conclusion: Rectal misoprostol was as effective
as intravenous oxytocin for preventing postpartum hemorrhage with the same incidence of side effects and is recommended to
be use as an uterotonic agent to manage third stage of labor routinely.
Key words: Active management, misoprostol, oxytocin, postpartum hemorrhage, third stage
Mozhgan Firouzbakht,
Azadeh Kiapour
1
,
Shabnam Omidvar
2
Department of Nursing and Midwifery,
1
Basic Science, Babol Branch, Islamic Azad University,
2
Nursing
and Midwifery, Babol Medical Sciences University, Babol, Iran
Address for correspondence:
Dr. Shabnam Omidvar, Department of Nursing and midwifery, Babol Medical Sciences University,
Babol, Iran. E-mail: shomidvar@yahoo.com
INTRODUCTION
A major cause of maternal mortality is post-partum
hemorrhage (PPH). The incidence of PPH has been
reported from <5% to >10%. These fgures remain at
least 100 times higher than those in developed countries.
[1]
The World Health Organization estimates that 20
million morbidities are consequences of PPH every
year, (accounting for one-third of maternal deaths).
[2]
The
causes of death are multi-factorial, and prevention requires
a multi-disciplinary response.
[3]
The primary cause of PPH is uterine atony. The third
stage of labor is potentially the most dangerous for the
mother, and active management is necessary. Active
management of the third stage of labor is composed of
immediate administration of an uterotonic, controlled cord
traction for placental delivery, and uterine massage. This
procedure is internationally recognized as an evidence-based
intervention that reduces PPH caused by uterine atony
up to 60%.
[2]
Conventional oxytocic agents used include
oxytocin, the ergot alkaloids ergonovine (ergometrine) and
methylergonovine (methylergometrine), syntometrine (which
consists of 5 IU oxytocin [Syntocinon] and 0.5 mg
ergometrine), and prostaglandins such as carboprost.
[4-7]
Moreover, oxytocins is an injectable uterotonic, that is
unstable at high temperature, and requires cold storage
and skills that birth attendants, who do not practice
active management of the third stage of labor, might not
possess.
[2,4,8]
Several side effects may occur with the use of
these agents including nausea, vomiting, elevated blood
pressure, headache, tachycardia, and bronchospasm.
[4-5,7]
Misoprostol, a prostaglandin E
1
analogue, is used
orally to prevent or as treatment of gastric/duodenal
ulcers caused by using non-steroidal anti-infammatory
Access this article online
Quick Response Code:
Website:
www.jnsbm.org
DOI:
10.4103/0976-9668.107277
Ori gi nal Art i cl e
[Downloadedfreefromhttp://www.jnsbm.orgonWednesday,August28,2013,IP:111.95.130.79]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Firouzbakht, et al.: Prevention of postpartum haemorrhage
135 Journal of Natural Science, Biology and Medicine | January 2013 | Vol 4 | Issue 1
agents. Misoprostol has also been investigated for
preventing PPH, using either the oral or rectal route of
administration.
[4-5]
Misoprostol produces less serious side
effects, and gastrointestinal disturbances are less frequent.
The oral route has been associated with dose-related
shivering and pyrexia (temperature >38C). Some experts
believe that the rectal route may be advantageous because
it may lessen the gastrointestinal side effects. Thus,
misoprostol can be administered rectally to patients who
are vomiting or unable to take oral medications, those who
are under general anesthesia, or those with heavy vaginal
bleeding.
[6,8-10]
A study from Ghana, comparing the effects of rectal
misoprostol with intramuscular oxytocin for routine
management of the third stage of labor, it was confrmed
that administrating of 400 mg rectal misoprostol is as
effective as 10 IU intramuscular oxytocin to minimize blood
loss during the third stage of labor. Rectal misoprostol has
a lower incidence of side effects than the equivalent oral
dose. The study confrmed the utility of misoprostol as a
safe and effective uterotonic for use in rural and remote
areas of developing nations where other pharmacologic
agents may be less available.
Ayyad and Abu Omar (2004) determined that rectal
misoprostol is as effective as intravenous oxytocin for
preventing PPH with the same incidence of side effects
and recommended its use as a uterotonic agent for routine
management of the third stage of labor.
[11]
A recent Pakistani study, which was conducted to access
effectiveness and safety of rectal misoprostol for treating
PPH, demonstrated that misoprostol is an effective
treatment for PPH and that is might be an alternative
to parenteral prostaglandins. Given that misoprostol
is an inexpensive and stable drug, it has considerable
potential to reduce maternal mortality from PPH in
developing countries.
[2]
The effcacy of misoprostol for
preventing PPH has also been well demonstrated in trials
in Iran (2009), Afghanistan (2010), and Ethiopia (2010).
[12-14]
A meta-analysis provided consistent evidence to support a
recommendation for use of misoprostol to prevent PPH
when oxytocin is unavailable.
[15]
The aim of this study was to compare the effectiveness and
safety of oxytocin and rectal misoprostol for preventing
PPH.
MATERIALS AND METHODS
This study was a randomized clinical trial. The participants
were 100 patients who had a singleton, gestational age of
37 weeks or more and spontaneous vaginal delivery at
Imam Ali Hospital, Amol, Iran from March 15 to January
30, 2010. Exclusion criteria were patients undergoing
cesarean section, patients with hemoglobin <8 gm%,
pregnancy-induced hypertension, grand multiparity,
coagulation abnormalities, positive history of PPH,
or other medical disorders. Patient were randomly
divided into 2 groups to receive either two 200 mg rectal
misoprostol tablets (study group) or 20 units oxytocin
in 1000 cc normal saline intravenously (control group).
Baseline maternal characteristics included age and parity.
Signifcant obstetric history was recorded. Blood pressure
levels were noted before and after delivery. PPH was
defned as blood loss in excess of 500 cc or 10% drop in
Hb from admission to the time of mother discharge (12
hours after delivery). Blood loss was estimated in the third
stage of labor by placing a plastic pan under the patients
at the time of placental separation and the number,
and weight of soaked pads at the time of episiotomy
repair (volume in cc=weight in grams) were determined.
Blood loss was quantifed by the weight and number
of soaked towels or by changes in Hb concentration or
hematocrite value. The primary outcome was to objectively
estimate the amount of blood loss. The hemoglobin
concentration was recorded before delivery. A second Hb
was estimated before discharge (12 hours post-partum).
Differences in the Hb values before and after delivery
were estimated in each group. Other variables included
agents used for augmentation of labor, mode of delivery,
and birth weight. Secondary outcomes were the length of
labor and the length of the third stage of labor, the need
for additional agents to control vaginal bleeding, and the
need for a blood transfusion.
The side effects of each medicine such as nausea, vomiting,
diarrhea, shivering, and headache were noted.
Data were analyzed on an intent-to-treat basis by
parametric (t- test and chi-sq test) and non-parametric
tests (MannWhitney U-test), using SPSS version 15
analytical software, (SPSS, Inc., Chicago, IL, USA).
A P <0.05 was considered as signifcant.
RESULTS
A total of 100 women were enrolled and randomized
to receive either rectal misoprostol (n = 50) or infusion
oxytocin (n=50) during the study period. In present study,
no signifcant differences were observed between the
groups regarding baseline characteristics [Table 1].
No signifcant differences were observed between the
groups for changes in Hb concentration. (P = 0.80).
[Downloadedfreefromhttp://www.jnsbm.orgonWednesday,August28,2013,IP:111.95.130.79]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Firouzbakht, et al.: Prevention of postpartum haemorrhage
136 Journal of Natural Science, Biology and Medicine | January 2013 | Vol 4 | Issue 1
No signifcant differences were observed between the
groups for the length of the first, second, and third
stages of labor (P=0.54, P=0.59, P=0.98), respectively.
The estimated blood loss during the third stage in the
misoprostol group decreased signifcantly (P = 0.003),
but no signifcant difference was observed for blood loss
after birth, length of the third stage, or need for a blood
transfusion. No other women required an operative
intervention (such as manual removal of placenta,
dilatation and curettage, laparotomy, or hysterectomy)
or had estimated blood loss >1000 ml. No difference
was observed for additional uterotonics between the two
groups (P=0.737) [Table 2].
The incidence of shivering was 14% in the misoprostol
group compared with 4% in the oxytocin group. Our
observations elicited that the incidence of other side effects
such as nausea, vomiting, and headache were essentially
similar [Table 3].
DISCUSSION
This study confrmed the utility of rectal misoprostol
for routine management of the third stage of labor.
Misoprostol (400 mg) administered rectally was effective
for minimizing blood loss when utilized to actively manage
the third stage of labor, as measured by changes in Hb
concentration before and 12 hours after delivery. This dose
and route of administration are well tolerated, and usual
side effects such as shivering and increasing temperature
were not prevalent. Karkanis et al. reported that No
difference in Hb was observed between the groups of
women who randomly received 400 (mg) rectal misoprostol
after delivery of the infant or 5 units of parenteral oxytocin
or 10 units oxytocin intramuscularly with delivery of the
anterior shoulder.
[16]
The duration of the third stage of
labor was not different between the two groups. Bugalh
et als. observation also confrmed similar results.
[17]
Nasr
et al. conducted a randomized trial with 514 women to
receive either 400 (mg) rectal misoprostol or one ampoule
of syntometrin. The results showed that the incidence of
PPH, duration of third stage of labor, and the drop in Hb
were similar between the two groups.
[12]
Ayyad and Abu
Omar also reported rectal misoprostol to be effective to
stop severe delivery-induced hemorrhage after failure of
syntocinon.
[11]
These studies provide further evidence for the utility
of misoprostol as an effective uterotonic that provides
a simple therapeutic option for health care providers in
developing nations to use against obstetric hemorrhage.
PPH is regarded as one of the major causes of maternal
mortality and morbidity in developing countries.
Consequently, active management of the third stage of
labor should be practiced by routinely use of intravenous
oxytocin. Misoprostol was chosen as a substitute for
oxytocin to prevent PPH because it has similar advantages
to oxytocin but with minimal side effects.
[11]
Misoprostol
is an inexpensive medicine, which is easily available.
It is easy to use and does not require special storage
conditions (i.e., can be stored easily at room temperature;
is thermo-stable and light stable; does not require specifc
conditions for transfer) and has a shelf life of several years.
These advantages make it a useful medicine for reducing
the incidence of PPH in developing countries. The rectal
route was chosen because of ease of administration,
and because it avoids gastrointestinal side effects such as
nausea, vomiting, and diarrhea; therefore, it can be given
to women who have nausea and vomiting.
[11]
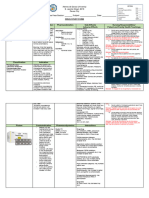
Table 1: Demographic characteristics
Characteristics Misoprostol
N=50
Oxytocin
N=50
P
Maternal age (year) 24.34.3 24.9 5 0.539
Parity
Nulipar 26 (52%) 27 (54%) 0.99
Multipar 21 (42%) 22 (44%)
Gestational age (week) 38.71.8 392.3 0.645
Weight of baby (kg) 3.420.49 3.30.41 0.78
Predelivery hemoglobin (gr/dl) 12.61.12 12.31.28 0.206
Mode of delivery
Spontaneous delivery 11 (22%) 10 (20%) 0/803
Episiotomy 33 (66%) 29 (58%) 0/67
Laceration 6 (12%) 11 (22%) 0/709
Length of labor
1
st
stage (hours) 11.196.02 10.84.7 0/54
2
nd
stage (minutes) 29.620.02 25.918.3 0/59
Data are presented as meanSD
Table 2: Primary and secondary outcomes
Characteristics Misoprostol
N=50
Oxytocin
N=50
P
Vaginal bleeding500 cc 6 (12%) 5 (10%) 0/828
Average blood loss (ml) 436.621404 415.06227.2 0/069
Average blood loss in
third stage
136111.3 162.4115.2 0/003
Average blood loss in
post-partum
143.3122.7 105.0886 0/017
Change in Hb (gr/dl) 1.151.28 1.411.3 0.0468
Post partum Hb 11.81.03 11.531.34 0.28
Length 3
rd
stage (minute) 5.083.07 5.492.45 0.198
Additional utrotonic agent 3 (6%) 4 (8%) 0.523
Data are presented as meanSD
Table 3: Medication side effects
Characteristics Misoprostor 50 (%) Oxytocin 50 (%) P
Nausea 5 (10) 3 (6) 0/42
Vomiting 2 (4) 0 (0) 0/52
Shivering 10 (20) 5 (10) 0/035
Headache 3 (6) 2 (4) 0/29
[Downloadedfreefromhttp://www.jnsbm.orgonWednesday,August28,2013,IP:111.95.130.79]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Firouzbakht, et al.: Prevention of postpartum haemorrhage
137 Journal of Natural Science, Biology and Medicine | January 2013 | Vol 4 | Issue 1
CONCLUSION
Rectal misoprostol seems to be safe and effective for
preventing PPH and is recommended for use to manage
the third stage of labor.
ACKNOWLEDGMENTS
The authors would like to thank all of the pregnant women that
participated in this study. Special thanks go to Mrs. Raee and
Mortazavie for their cooperation in collecting data.
REFERENCES
1. Walley RL, Wilson JB, Crane JM, Mathews K, Sawyer E, Hutchens D.
A doubleblind placebo controlled randomised trial of misoprostol
and oxytocin in the management of the third stage of labour. BJOG
2000;107:11115.
2. Mobeen N, Durocher J, Zuberi N, Jahan N, Blum J, Wasim S, et al.
Administration of misoprostol by trained traditional birth atendants
to prevent postpartum haemorrhage in homebirths in Pakistan:
A randomised placebocontrolled trial. BJOG 2010;118:35361.
3. Celenza MT, Brassil ML, Code H. Obstetrical hemorrhage:
Development of a team approach. J Obstet Gynecol Neonat Nurs
2011;40:S467.
4. Cunningham F, Kenneth Leveno K, Bloom S, Hauth J, Rouse D, Spong C.
Williams obstetrics. 23
th
ed. New York: McGrawHill Companies; 2010.
5. Glmezoglu AM, Forna F, Villar J, Hofmeyr GJ. Prostaglandins for
preventing postpartum haemorrhage. Cochrane Database Syst Rev
2007;3:CD000494.
6. Hofmeyr GJ, Glmezoglu AM, Novikova N, Linder V, Ferreira S,
Piaggio G. Misoprostol to prevent and treat postpartum haemorrhage:
A systematic review and metaanalysis of maternal deaths and
doserelated efects. Bull World Health Organ 2009;87:66677.
7. Khan RU, ElRefaey H. Pharmacokinetics and adverseefect profle
of rectally administered misoprostol in the third stage of labor.
Obstet Gynecol 2003;101:96874.
8. Elati A, Elmahaishi MS, Elmahaishi MO, Elsraiti OA, Weeks AD.
The efect of misoprostol on postpartum contractions: A randomised
comparison of three sublingual doses. BJOG 2010;118:46673.
9. Anbreen F. Efcacy of Rectal Misorpostol when Combined with
Standard Oxytocin to Treat Postpartum Hemorrhage. Gomal J Med
Sci 2010;8:279.
10. Mansouri H, Alsahly N. Rectal versus oral misoprostol for active
management of third stage of labor: A randomized controlled trial.
Arch Gynecol Obstet 2011;283:9359.
11. Ayyad I, Jordan R. Prevention of post partum haemorrhage by rectal
misoprostol: A randomised controlled trial. Middle East J Fam Med
2004;5:16.
12. Nasr A, Shahin AY, Elsamman AM, Zakherah MS, Shaaban OM.
Rectal misoprostol versus intravenous oxytocin for prevention of
postpartum hemorrhage. Int J Gynecol Obstet 2009;105:2447.
13. Sanghvi H, Ansari N, Prata NJ, Gibson H, Ehsan AT, Smith JM.
Prevention of postpartum hemorrhage at home birth in Afghanistan.
Int J Gynecol Obstet 2010;108:27681.
14. Prata N, Gessessew A, Abraha AK, Holston M, Pots M. Prevention of
postpartum hemorrhage: Options for home births in rural Ethiopia.
Afr J Reprod Health 2010;13:8795.
15. Langenbach C. Misoprostol in preventing postpartum hemorrhage:
A metaanalysis. Int J Gynecol Obstet 2006;92:108.
16. Karkanis SG, Caloia D, Salenieks ME, Kingdom J, Walker M,
Mefe F, et al. Randomized controlled trial of rectal misoprostol
versus oxytocin in third stage management. J Obstet Gynaecol Can
2002;24:14954.
17. Bugalho A, Daniel A, Fandes A, Cunha M. Misoprostol for
prevention of postpartum hemorrhage. Int J Gynecol Obstet
2001;73:16.
How to cite this article: Firouzbakht M, Kiapour A, Omidvar S. Pre-
vention of post-partum hemorrhage by rectal Misoprostol: A randomized
clinical trial. J Nat Sc Biol Med 2013;4:134-7.
Source of Support: Nil. Confict of Interest: None declared.
[Downloadedfreefromhttp://www.jnsbm.orgonWednesday,August28,2013,IP:111.95.130.79]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Veterans Affairs Presumptive Service Connection and Disability CompensationДокумент33 страницыVeterans Affairs Presumptive Service Connection and Disability CompensationChuck Achberger100% (1)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- RN MedSurgДокумент685 страницRN MedSurgArgyll Baye Ansuas100% (4)
- Test Bank Health Assessment in Nursing 6th Edition Weber KelleyДокумент9 страницTest Bank Health Assessment in Nursing 6th Edition Weber KelleyPhyllis Vandenberge100% (25)
- Precision Medicine OncologyДокумент18 страницPrecision Medicine Oncologyaminudinrahman100% (1)
- CHC33015-Sub 1 AssessmentДокумент102 страницыCHC33015-Sub 1 AssessmentMaimuna100% (8)
- Metabical CBДокумент31 страницаMetabical CBKumar AbhishekОценок пока нет
- Pil 13082Документ2 страницыPil 13082raul sinatoОценок пока нет
- HayalllДокумент41 страницаHayalllchalie tarekegnОценок пока нет
- VAW ToT Caribbean May 2019 DAY 1Документ77 страницVAW ToT Caribbean May 2019 DAY 1NITU SHARMAОценок пока нет
- Valproate SodiumДокумент2 страницыValproate SodiumKhairul KhairulОценок пока нет
- Renal Drug StudyДокумент3 страницыRenal Drug StudyRiva OlarteОценок пока нет
- CDP 2011 20 Final Chapter 2 Matrix of Local Development IndicatorsДокумент7 страницCDP 2011 20 Final Chapter 2 Matrix of Local Development Indicatorswassila boutaaОценок пока нет
- Hexco November December 2023 NC - ND Final Timetable PDFДокумент28 страницHexco November December 2023 NC - ND Final Timetable PDFlionelngoveОценок пока нет
- Air in The Urinary Tract: Images in Clinical MedicineДокумент1 страницаAir in The Urinary Tract: Images in Clinical MedicineSamira LizarmeОценок пока нет
- Vilas County News-Review, March 14, 2012 - SECTION BДокумент10 страницVilas County News-Review, March 14, 2012 - SECTION BNews-ReviewОценок пока нет
- Animal Research As A Basis For Clinical Trials: FocusДокумент5 страницAnimal Research As A Basis For Clinical Trials: FocusIuliana MogaОценок пока нет
- Reading Material - Case - Studies - in - Occupational - Health - and - Safety - ManagementДокумент11 страницReading Material - Case - Studies - in - Occupational - Health - and - Safety - ManagementJoker KingОценок пока нет
- Poster Sindh 2-01-2024Документ11 страницPoster Sindh 2-01-2024FM Printers111Оценок пока нет
- Reviewer Micp Midterms 1Документ29 страницReviewer Micp Midterms 1Shiro KagomeОценок пока нет
- Meperidine Hydro ChlorideДокумент4 страницыMeperidine Hydro Chlorideapi-3797941Оценок пока нет
- Obsessive Compulsive Disorder (OCD) : DefinitionДокумент3 страницыObsessive Compulsive Disorder (OCD) : Definitionapi-295297012Оценок пока нет
- The Ancestral Human Diet: What Was It and Should It Be A Paradigm For Contemporary Nutrition?Документ6 страницThe Ancestral Human Diet: What Was It and Should It Be A Paradigm For Contemporary Nutrition?Alec LiuОценок пока нет
- RH BillДокумент23 страницыRH BillArah Obias CopeОценок пока нет
- 6 Respectful Baby Sleep Solutions Freebie 21fe39a1 A163 4d22 b5f2 9d5261e10772Документ4 страницы6 Respectful Baby Sleep Solutions Freebie 21fe39a1 A163 4d22 b5f2 9d5261e10772Jamie AsuncionОценок пока нет
- Faktor Resiko Infeksi SCДокумент11 страницFaktor Resiko Infeksi SCAlberto BrahmОценок пока нет
- Soal PAS BIG Xi, SMT 3, OnlineДокумент10 страницSoal PAS BIG Xi, SMT 3, OnlineRivaldi Lukman HakimОценок пока нет
- Tutor: Dr. Vera Dr. Haerani: Skenario Problems Learning Objectives Main Map ReferensiДокумент36 страницTutor: Dr. Vera Dr. Haerani: Skenario Problems Learning Objectives Main Map ReferensiAdeLia Nur FitrianaОценок пока нет
- NOFRNCompetencies Updated March2016 PDFДокумент63 страницыNOFRNCompetencies Updated March2016 PDFamandeep kaurОценок пока нет
- The Vaccine Adverse Event Reporting System (VAERS)Документ21 страницаThe Vaccine Adverse Event Reporting System (VAERS)Kraft DinnerОценок пока нет
- Review: Tinea Corporis: An Updated ReviewДокумент22 страницыReview: Tinea Corporis: An Updated ReviewMade SetiadjiОценок пока нет