Академический Документы
Профессиональный Документы
Культура Документы
Revascularization of The Anterior Cerebral Artery.38
Загружено:
Andreea GiovaniИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Revascularization of The Anterior Cerebral Artery.38
Загружено:
Andreea GiovaniАвторское право:
Доступные форматы
TECHNICAL CASE REPORTS
REVASCULARIZATION OF THE ANTERIOR CEREBRAL ARTERY WITH AN A3A3 ANASTOMOSIS AND A SUPERFICIAL TEMPORAL ARTERY BYPASS USING AN A3-RADIAL ARTERY GRAFT TO TRAP A GIANT ANTERIOR COMMUNICATING ARTERY ANEURYSM: TECHNICAL CASE REPORT
Tomohiro Inoue, M.D.
Department of Neurosurgery, Showa General Hospital, Tokyo, Japan
Kazuo Tsutsumi, M.D.
Department of Neurosurgery, Showa General Hospital, Tokyo, Japan
Hiroyasu Ohno, M.D.
Department of Neurosurgery, Showa General Hospital, Tokyo, Japan
Munehisa Shinozaki, M.D.
Department of Neurosurgery, Showa General Hospital, Tokyo, Japan Reprint requests: Kazuo Tsutsumi, M.D., Department of Neurosurgery, Showa General Hospital, 2-450 Tenjinn-cho, Kodaira-shi, Tokyo 187-8510, Japan. Email: k.tsutsumi-md@nifty.com Received, April 19, 2004. Accepted, January 13, 2005.
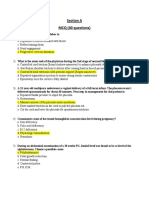
OBJECTIVE AND IMPORTANCE: How to manage the distal anterior cerebral artery (ACA) circulation in the treatment of a giant anterior communicating artery aneurysm or a giant azygous A2 aneurysm is still controversial. CLINICAL PRESENTATION: We are reporting the case of a 70-year-old man who presented with an evolving giant thrombosed anterior communicating artery aneurysm. INTERVENTION: He was successfully treated by trapping the aneurysm in conjunction with an A3A3 side-to-side anastomosis and a superficial temporal artery bypass using an A3-radial artery graft. The postoperative angiography showed an excellent filling of all the bilateral distal ACA area through the bypass. CONCLUSION: In cases in which direct clipping to preserve distal ACA flow is quite difficult, the bilateral ACA revascularization described here should be considered as another possibility.
KEY WORDS: A3A3 anastomosis, Giant anterior communicating artery aneurysm, Radial artery graft, Revascularization
Neurosurgery 57[ONS Suppl 1]:ONS-207, 2005
DOI: 10.1227/01.NEU.0000163682.31075.28
iant anterior communicating artery (AComA) aneurysms are rare and difficult to remove from circulation while preserving distal anterior cerebral artery (ACA) flow. We successfully treated a 70-year-old man who presented with a giant thrombosed AComA aneurysm by trapping and revascularizing the ACA through a bypass. The details of the operation are presented and discussed.
CASE REPORT
A 70-year-old man presented at our hospital with complaints of hesitant speech and forgetfulness. The neurological examination did not show any focal deficit. The only important note regarding his past medical history was hypertension, which had been medically controlled at another hospital. He underwent magnetic resonance imaging
(MRI) to exclude lacunar stroke. The MRI scan revealed a large frontal mass with flow void and thrombus consistent with a thrombosed giant AComA aneurysm (Fig. 1, A and B). He was admitted and underwent angiography. The left internal carotid angiogram showed a 27 21-mm AComA aneurysm projecting superiorly with a delayed filling of the bilateral distal ACA compared to the middle cerebral artery on the same side (Fig. 1, C and D). The right internal carotid angiogram did not show filling of the aneurysm, although a Matas test revealed the existence of very hypoplastic right A1, which did not fill the aneurysm either. Considering the operative risk and the comparatively minor symptoms, close observation with serial MRI scans was chosen and the patient was discharged. However, 2 months later, another MRI scan revealed an enlargement of the aneurysm. After thorough discussion, it was decided that we would con-
NEUROSURGERY
VOLUME 57 | OPERATIVE NEUROSURGERY 1 | JULY 2005 | ONS-E207
INOUE
ET AL.
through the STA radial artery A3A3 bypass. We then proceeded anteriorly and exposed the giant anterior communicating aneurysm. At the same time, the temporary clip was proximally replaced step-by-step. Finally, the permanent clip was placed on the left A1 and bilateral A2 just distal to the aneurysm. The right hypoplastic A1 was left patent to allow flow to the hypothalamic perforators, since confirming its existence intraoperatively would cause more harm than good when considering the size of the aneurysm. Postoperatively, the patient showed a slight disorientation, which gradually disappeared. The postoperative angiogram revealed no filling of the aneurysm for both the internal and the right external carotid (Fig. 2, A and B). The angiogram also showed there was excellent distal ACA flow through the bypass (Figure 2, C and D). Follow-up examinations with the patient have been in outpatient settings, and he has been living an independent life. After 1.5 years, the donor STA continues to provide very good pulsation and follow-up MRI scans have shown a remarkable shrinkage of the aneurysm and clear flow void of the radial artery graft in a T2-weighted image without any evidence of distal ACA area infarction.
DISCUSSION
FIGURE 1. A and B, preoperative axial T1-weighted MRI scan (A) and coronal T2-weighted MRI scan (B) showing the frontal mass suggestive of a thrombosed giant AComA aneurysm. C and D, left carotid angiograms (anteroposterior [C] and lateral [D] views) showing the giant AComA aneurysm.
Managing the distal ACA circulation on both sides in the treatment of a giant AComA aneurysm (6) or giant azygous artery aneurysm (10) is still controversial. Although direct clipping of the aneurysm with preservation of the parent
duct operative therapy to trap the aneurysm, preceded by revascularization of the distal ACA. A bicoronal skin incision was made, and a large bifrontal craniotomy on the right side over the superior sagittal sinus (SSS) and a small craniotomy near the parasylvian area were carried out. Simultaneously, approximately 15 cm of the right radial artery was prepared for an interposing graft. Because the bridging vein in the left frontal area drained into the SSS more posteriorly than to the right side, we entered the interhemispheric space from the left side up to the falx after ligation of the SSS and division of the falx at the anterior border. After a sharp dissection of the interhemispheric fissure, with minimal retraction of the right frontal lobe over the SSS and falx, we obtained wide exposure of the bilateral A3 just distal to the genu. First, the A3A3 side-to-side anastomosis was performed with 10-0 nylon. The occlusion time was 50 minutes. Then, the right A3, just proximal to the A3A3 bypass, was trapped with a temporary clip for an end-to-side A3 radial artery anastomosis. A radial artery graft was passed through the subdural space and at the parasylvian craniotomy, the proximal end was anastomosed to the superficial temporal artery (STA) end-to-end. The two anastomoses were conducted using 8-0 nylon. Finally, a temporary clip was placed on each A3, just proximal to the A3A3 and A3 radial artery anastomoses. We used Doppler ultrasonography to confirm that there was excellent distal ACA flow on both sides
FIGURE 2. A and B, postoperative right (A) and left (B) carotid angiograms showing nonfilling of the giant AComA aneurysm. C and D, right external carotid angiograms (anteroposterior [C] and lateral [D] views) demonstrating good bilateral ACA flow through the bypass.
ONS-E207 | VOLUME 57 | OPERATIVE NEUROSURGERY 1 | JULY 2005
www.neurosurgery-online.com
A3A3 ANASTOMOSIS
AND
SUPERFICIAL TEMPORAL ARTERY BYPASS
The bonnet bypass was first reported by Spetzler et al. (8). Since then, ACA revascularization for the treatment of ACA occlusive disease, free STA (5) and saphenous vein (9) have been used as an interposing graft between donor (STA) and recipient (ACA). Considering the availability in the same surgical field, free STA graft harvested from the contralateral side could have a benefit, the length and size would be restricted. Although, according to a recent report, the long-term patency of a saphenous vein graft in the reconstruction of the internal carotid artery is acceptable (7), we did not use this graft given the size discrepancy between a saphenous vein graft and an ACA or STA. To establish all the revascularization throughout the bilateral ACA area, the radial artery free graft has several advantages. There is enough length to FIGURE 3. Schematic diagram depicting the flow after establishing the A3A3 anastomointerpose it between the A3 and STA main trunk, sis. A, during A3-radial artery graft-STA anastomosis; B, replacing the temporary clip which can provide for a more robust flow than the proximally; C, completion of the trapping. frontal or parietal STA branch. It also provides a good free graft and recipient (or donor) ratio, and it has a reduced tendency toward redundancy or kinking when compared with a vein graft. Although there is artery is preferable, it is not always possible because of a wide no cumulative data for ACA reconstruction with a radial neck or thrombus. In some cases, special techniques, including artery graft, reliable long-term patency has been documented temporary clipping, evacuation of the intraluminal thrombus, in the reconstruction of a carotid artery with a radial artery and tandem or fenestrated clipping are needed (6). There are graft (2). The technical details of an A3A3 side-to-side anassome reported successful cases which had tolerated the proxtomosis were first and well described by Ito (4). Since then, imal ligation of dominant A1 well because of excellent leptothis procedure has rarely been discussed in the literature (3), meningeal collateral circulation (6). In the presence of a giant probably because it is rare to have a case where this technique AComA aneurysm with concomitant delayed filling of distal is required. However, this technique is still valuable when we ACA in the angiogram, the potential for robust leptomeninneed to reconstruct bilateral ACA, as with the present case. geal collateral vessels following A1 occlusion could be high (1, With appropriate temporary clip application and enough ex6). In addition, the endovascular occlusion of the A1 might be posure of the surgical field, the method illustrated here can be the alternative approach, if the patient tolerated trial balloon performed safely and should be considered in the treatment of occlusion. However, there is no established method to detera giant AComA aneurysm. mine which cases can tolerate proximal ligation or endovascular occlusion without ischemic complications in the distal ACA area in the acute phase as well as in long-term follow-up. In this patient, we accomplished the successful trapping of REFERENCES a giant AComA aneurysm in conjunction with distal ACA revascularization. The key issue was that the occlusion time of 1. Drake CG, Peerless SJ, Ferguson GG: Hunterian proximal arterial occlusion the distal ACA occurred during the A3A3 anastomosis profor giant aneurysms of the carotid circulation. J Neurosurg 81:656665, 1994. 2. Houkin K, Kamiyama H, Kuroda S, Ishikawa T, Takahashi A, Abe H: Long cedure. It is difficult to preoperatively evaluate those cases term patency of radial artery graft bypass for reconstruction of the internal with insufficient leptomeningeal collateral flow and safely carotid artery. J Neurosurg 90:786790, 1999. guarantee that an ischemic insult during the A3A3 anasto3. Ikeda A, Okada T, Shibuya M, Noda S, Sugiura M, Iguchi I, Gonda T, mosis procedure will not occur. After the A3A3 anastomosis, Kageyama N: Revascularization of the anterior cerebral artery: Report of the circulation of all the distal ACA area was secured during two cases. J Neurosurg 62:603606, 1985. 4. Ito Z: A new technique of intracranial interarterial anastomosis between the establishment of a radial artery interposition until the distal anterior cerebral arteries (ACA) for ACA occlusion and its indication trapping of the aneurysm was accomplished (Fig. 3). Tempo[in Japanese]. Neurol Med Chir (Tokyo) 21:931939, 1981. rary clips divided the anterograde flow through A1 and the 5. Iwata Y, Mizuta T, Takemoto O, Shimizu K, Nakatani S: An interposed distal bypass flow (Fig. 3), which prevented an early occlusion superficial temporal artery graft bypass for anterior cerebral artery ischemia. Microsurgery 9:1417, 1988. of the anastomosis site by the impact of both flows. Ligation of 6. Lownie SP, Drake CG, Peerless SJ, Ferguson GG, Pelz DM: Clinical presenthe SSS and the division of the falx at its anterior border tation and management of giant anterior communicating artery region contributed to opening up an excellent working space requiraneurysms. J Neurosurg 92:267277, 2000. ing less brain retraction. Depending on the distribution of the 7. Morgan MK, Ferch RD, Little NS, Harrington TJ: Bypass to the intracranial frontal bridging vein, this might not always be possible. internal carotid artery. J Clin Neurosci 9:418424, 2002.
NEUROSURGERY
VOLUME 57 | OPERATIVE NEUROSURGERY 1 | JULY 2005 | ONS-E207
INOUE
ET AL.
8. Spetzler RF, Roski RA, Rhodes RS, Modic MT: The bonnet bypass: Case report. J Neurosurg 53:707709, 1980. 9. Tanaka K, Yonekawa Y, Kouno H, Katagiri K, Satou K: STA-ACA anastomosis with interposed vein graft: A case report [in Japanese]. No Shinkei Geka 20:171176, 1992. 10. Topsakal C, Ozveren F, Erol FS, Chiangiroglu M, Cetin H: Giant aneurysm of the Azygous pericallosal artery: Case report and review of the literature. Surg Neurol 60:524533, 2003.
COMMENTS
his case is an interesting example of the use of creative bypass techniques to treat complex intracranial aneurysms. The authors performed a side-to-side A3A3 anastomosis and then a radial artery graft between one of the A3s and the superficial temporal artery. After these bypasses, they performed a trapping of the aneurysm. An alternative approach to this case might have been to perform an endovascular trial occlusion of the left A1 segment. If the patient tolerated this occlusion, permanent endovascular occlusion of the left A1 might have been a much simpler therapy to accomplish the same goal. Robert A. Solomon New York, New York
he authors report a successful surgical strategy in the management of a very complicated giant anterior communicating artery aneurysm that was thrombotic. The authors concluded early on that the aneurysm would not be directly reconstructible and embarked upon a hunterian strategy with distal revascularization. A very important element of their strategy included the preservation of a hypoplastic A1 segment to hopefully provide supply to hypothalamic perforators coming from the complex. An A3A3 side-to-side anastomoses was performed, followed by a proximal superficial temporal artery-radial artery graft-A3 bypass. Subsequent to the construction of that revascularization, the aneurysm was trapped (with the exception of the right A1 segment). This was a very well thought out strategy in an elderly gentleman and had excellent clinical and radiographic results. We recently performed a double-barreled radial artery bypass into both A2 segments in an ischemic setting only to lose the graft in the postoperative period. In my view, our error in that case was to perform an aggressive angioplasty to dilate the radial artery. Our outflow system (both A2s) was simply not adequate to sustain flow to a conduit of that size. The authors have reported an innovative solution to a difficult surgical problem. H. Hunt Batjer Chicago, Illinois
ONS-E207 | VOLUME 57 | OPERATIVE NEUROSURGERY 1 | JULY 2005
www.neurosurgery-online.com
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Superficial Temporal Artery To Middle Cerebral.28Документ5 страницSuperficial Temporal Artery To Middle Cerebral.28Andreea GiovaniОценок пока нет
- Double Reimplantation Technique To Reconstruct.20Документ8 страницDouble Reimplantation Technique To Reconstruct.20Andreea GiovaniОценок пока нет
- A Novel Minimally Occlusive Microvascular.33Документ8 страницA Novel Minimally Occlusive Microvascular.33Andreea GiovaniОценок пока нет
- Microvascular Retractor A New Concept Of.34Документ4 страницыMicrovascular Retractor A New Concept Of.34Andreea GiovaniОценок пока нет
- Bilateral Internal Carotid To Anterior Cerebral.26Документ5 страницBilateral Internal Carotid To Anterior Cerebral.26Andreea GiovaniОценок пока нет
- In Situ Bypass in The Management of Complex.23Документ6 страницIn Situ Bypass in The Management of Complex.23Andreea GiovaniОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Conmed 5000 ESU - User ManualДокумент38 страницConmed 5000 ESU - User ManualdetschelОценок пока нет
- Basic Life Support (BLS) Primary Survey For Respiratory ArrestДокумент6 страницBasic Life Support (BLS) Primary Survey For Respiratory ArrestRifqi MuhammadОценок пока нет
- OBGYN 1st Round 2021 AnsweredДокумент14 страницOBGYN 1st Round 2021 AnsweredMuhammed Mostafa100% (4)
- IV InsertionДокумент9 страницIV InsertionSharmaine Grace FlorigОценок пока нет
- Ent History Taking and Examination-1Документ16 страницEnt History Taking and Examination-1Jyotirmayee100% (5)
- Oronasal SuctioningДокумент3 страницыOronasal SuctioningFRANCIS LOUIE CABADAОценок пока нет
- Surgical Informed Consent FormДокумент2 страницыSurgical Informed Consent FormMenGuitar100% (1)
- WOCN OCA Learning OutcomesДокумент3 страницыWOCN OCA Learning OutcomesNieva Portia Bunagan-DuriaОценок пока нет
- Emergency Neurological Life Support: Airway, Ventilation, and SedationДокумент50 страницEmergency Neurological Life Support: Airway, Ventilation, and SedationastrianamaulidianiОценок пока нет
- 418-M3-Cu14 Nursing Care of Clients in Emergency Situations 1 - AbcsДокумент9 страниц418-M3-Cu14 Nursing Care of Clients in Emergency Situations 1 - AbcsDanica FrancoОценок пока нет
- Profopol Vs KTMДокумент7 страницProfopol Vs KTMAuliaRusdiAllmuttaqienОценок пока нет
- Primary THA in DDH Crow's 2&3: Manor Hospital Walsall A Teaching Trust of University of BirminghamДокумент32 страницыPrimary THA in DDH Crow's 2&3: Manor Hospital Walsall A Teaching Trust of University of BirminghamDr Meenakshi ParwaniОценок пока нет
- Surgery OsceДокумент69 страницSurgery OsceRebecca BrandonОценок пока нет
- Master Degree in Plastic Surgery ThesisДокумент117 страницMaster Degree in Plastic Surgery ThesisMohamed Ahmed El-RoubyОценок пока нет
- Paramedic NREMTДокумент88 страницParamedic NREMTJadie Barringer III100% (2)
- Respiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)Документ14 страницRespiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)PkernОценок пока нет
- Open Cholecystectomy DictationДокумент4 страницыOpen Cholecystectomy DictationHassanОценок пока нет
- NRU HydroceleДокумент7 страницNRU HydroceleDyahFitriОценок пока нет
- Streeroga Paper 2 Part BДокумент94 страницыStreeroga Paper 2 Part BVYSHAK MOОценок пока нет
- BCSA Summative DOPySДокумент6 страницBCSA Summative DOPySMihaela BarbuОценок пока нет
- Journal of Pediatric Surgery Case Reports: Wandering Mesenteric CystДокумент4 страницыJournal of Pediatric Surgery Case Reports: Wandering Mesenteric CysthilalОценок пока нет
- Abdomen 2Документ22 страницыAbdomen 2carlosОценок пока нет
- Echocardiogram: Echocardiogram, Also Known As Echocardiography, or Heart Ultrasound Is AДокумент23 страницыEchocardiogram: Echocardiogram, Also Known As Echocardiography, or Heart Ultrasound Is AKarl RobleОценок пока нет
- 4 Ophthalmologists Cullman, AL: We Found NearДокумент2 страницы4 Ophthalmologists Cullman, AL: We Found NearSantosh Sharma VaranasiОценок пока нет
- 3 Intravenous-TherapyДокумент4 страницы3 Intravenous-TherapyMarie Louise Nicole TuvillaОценок пока нет
- Hand Injuries & Their ManagementsДокумент78 страницHand Injuries & Their ManagementsKuruОценок пока нет
- Importance of Percutaneous Gastrojejunostomy (PEG-J) in Advance Parkinson Disease TreatmentДокумент7 страницImportance of Percutaneous Gastrojejunostomy (PEG-J) in Advance Parkinson Disease TreatmentRoxana AndreeaОценок пока нет
- 1800 MCQ Revised VersionДокумент606 страниц1800 MCQ Revised VersionFarah FarahОценок пока нет
- Facial Feminization PDFДокумент2 страницыFacial Feminization PDFKimОценок пока нет
- Nys Molst FormДокумент4 страницыNys Molst FormDaniel_Taylor_4541Оценок пока нет