Академический Документы
Профессиональный Документы
Культура Документы
Anca Vasculitits
Загружено:
atul_desai_3Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Anca Vasculitits
Загружено:
atul_desai_3Авторское право:
Доступные форматы
mini review
http://www.kidney-international.org & 2013 International Society of Nephrology
Antineutrophil cytoplasm antibodyassociated vasculitis: recent developments
Shunsuke Furuta1 and David R.W. Jayne1
1
Lupus and Vasculitis Clinic, Addenbrookes Hospital, Cambridge University Hospitals, Cambridge, UK
Antineutrophil cytoplasm antibody (ANCA)associated vasculitis (AAV) is a group of vasculitides characterized by small-to-medium-sized blood vessel vasculitis and the presence of ANCA. Although our understanding of the causes of AAV remains limited, new information supporting an autoimmune basis is emerging. This review highlights recent progresses in etiology, pathogenesis, classification, and treatment. A genome-wide association study has confirmed a role for genetic susceptibility in AAV, and links between environmental factors and AAV induction through abnormal neutrophil extracellular traps has been demonstrated. Ongoing international consensus initiatives have revised approaches to the classification of vasculitis that has been enhanced by the analysis of large-scale prospective clinical data sets. New autoantibodies to human lysosomeassociated membrane protein-2 antibody, moesin, and plasminogen have been detected in AAV sera and a prognostic classification of renal biopsies developed. Clinical trial networks have extended the evidence base for the treatment of AAV, and rituximab has emerged as an alternative to cyclophosphamide for remission induction. Long-term outcomes following current treatment strategies have been determined and increased risks for cardiovascular and malignant disease reported.
Kidney International (2013) 84, 244249; doi:10.1038/ki.2013.24; published online 20 February 2013 KEYWORDS: ANCA-associated vasculitis; classification; granulomatosis with polyangiitis; microscopic polyangiitis; treatment
Antineutrophil cytoplasm antibody (ANCA)associated vasculitis (AAV) is a grouping of multisystem diseases characterized by a pauci-immune small-vessel vasculitis and the presence of circulating autoantibodies. AAV has an annual incidence of 20 per million. Its outcomes are often poor with a mortality of 25% at 5 years. Renal involvement is frequently seen and is strongly associated with outcomes.
CLASSIFICATION OF VASCULITIS
Correspondence: Shunsuke Furuta, Lupus and Vasculitis Clinic, Addenbrookes Hospital, Cambridge University Hospitals, Hills Road, Cambridge CB2 0QQ, UK. E-mail: shunsuke.furuta@addenbrookes.nhs.uk Received 26 September 2012; revised 25 October 2012; accepted 8 November 2012; published online 20 February 2013 244
The nomenclature of the primary systemic vasculitis syndromes was defined by the 1994 Chapel Hill Consensus Conference (CHCC). The American College of Rheumatology (ACR) had previously proposed classification criteria for seven vasculitis syndromes including Wegeners granulomatosis (WG), ChurgStrauss syndrome (CSS), and polyarteritis nodosa (PAN) on the basis of analysis of a large retrospective cohort. The ACR criteria were developed before widespread ANCA testing, and PAN and microscopic polyangiitis (MPA) were not differentiated. The CHCC definitions were based on the expert opinion in order to standardize the nomenclature and were based on the predominant size of blood vessel involvement in tissue biopsies. MPA and PAN were defined as two different vasculitides, a small-to-medium-sized blood vessel vasculitis and a medium-sized blood vessel vasculitis, respectively. An association between WG, CSS, MPA, and ANCA due to the common finding of a pauci-immune microscopic vasculitis was emphasized. These three syndromes were subsequently grouped together as AAV. Application of the ACR criteria alone results in frequent overlaps between syndromes of WG, CSS, and PAN, and the CHCC system was limited by its requirement for histology resulting in many unclassified cases. The absence of MPA in the ACR criteria has led to the use of the ACR criteria and the CHCC definitions in parallel. Resolving these problems, European Medicines Agency developed a stepwise algorithm for diagnosing AAV and PAN in patients with suspected vasculitis in 2007. This algorithm categorizes cases with suspected vasculitis using the ACR and Lanham criteria for CSS, surrogate markers for WG and renal vasculitis, and the CHCC definitions. The deficiencies in these systems and the need for newer approaches to the classification and diagnosis of vasculitis were reviewed by the European League Against Rheumatism/ACR working group in 2010.1 This led to the launch of a large, prospective, observational study, Diagnosis
Kidney International (2013) 84, 244249
S Furuta and DRW Jayne: AAV: recent developments
mini review
and Classification of Vasculitis Study, to develop both revised classification criteria and a validated set of diagnostic criteria. The CHCC definitions were revised in 2012 to take an account of recent advances, to cover a more complete spectrum of vasculitis, and to begin the replacement of eponyms with descriptive titles for vasculitis syndromes (Table 1).2 New categories included single-organ vasculitis and variable-vessel vasculitis. In the 2012 CHCC system, small-vessel vasculitis was subdivided into AAV and immune complex small-vessel vasculitis. An AAV was officially defined as a group of necrotizing vasculitides with few or no immune deposits, predominantly affecting small vessels, associated with ANCA. AAV included MPA, granulomatosis with polyangiitis (GPA) renamed from WG, and eosinophilic granulomatosis with polyangiitis (EGPA), renamed from CSS. The CHCC definitions are based on histology and clinical manifestations, but newer insights for classification have emerged from large cohort and genetic studies. Mahr et al.3 using a cluster analysis approach demonstrated the importance of ANCA subtypes, myeloperoxidase (MPO)/ proteinase 3 (PR3)-ANCA, in deriving novel subgroups. Lyons et al.4 demonstrated in their genome-wide association study that associations with the particular genes were primarily aligned with ANCA subtypes rather than diagnostic subgroups. Their results have suggested the classification of AAV into MPO-ANCA-positive angiitis and PR3-ANCA-positive angiitis.
ANCA AND OTHER ANTIBODIES
The major autoantigens of ANCA are MPO and PR3. MPOANCA is the predominant serotype in MPA patients, whereas PR3-ANCA is usually found in GPA. True dual positivity is rare and raises suspicion of a drug-induced vasculitis. In addition to being a diagnostic marker, a pathogenic role for ANCA is supported by experimental data and associations of ANCA with disease activity. However, vasculitis can occur in AAV without ANCA, and ANCA levels do not correlate well with disease activity. Differences in the functional effects of ANCA epitopes may explain differing clinical associations
but recently described autoantibodies in vasculitis may also be important. In 1995, Kain et al. found antihuman lysosomeassociated membrane protein-2 (hLAMP-2) antibody in 16 of 17 patients with pauci-immune focal necrotizing glomerulonephritis. They subsequently reported a higher prevalence in pauci-immune renal vasculitis (80/84 by immunofluorescence assay and 70/84 by ELISA), compared with ANCA (38/84 with MPO-ANCA and 39/84 with PR3-ANCA). LAMP-2 is a membrane protein in both the lysosome and cellular membrane; it is coexpressed in neutrophil granules with MPO and PR3, and it is also expressed in glomerular endothelial cells. Anti-hLAMP-2 antibodies activate neutrophils and induce apoptosis of human microvascular endothelium in vitro and cause renal vasculitis when injected into rats. There is cross-reactivity and 100% homology of LAMP-2 with the bacterial adhesion protein FimH. In 2012, Kain et al.5 showed a high prevalence again of 84% in 64 newly diagnosed, untreated AAV patients with three different methods, immunofluorescence, ELISA, and western blot. However, Roth et al.6 found only 21% of ANCA-positive renal vasculitis patients (n 329) and 28% of ANCA-negative patients (n 104) to have anti-hLAMP-2 as compared with 16% of controls with urinary tract infection (n 104). The rapid fall in anti-hLAMP2 antibody that appears to occur with the therapy and difference in subjects, assays, and the LAMP-2 substrates may explain differences in results between the studies. In 2011, a Japanese group revealed that MPO-ANCA activated glomerular endothelial cells directly in a murine model. They identified a new target antigen of MPO-ANCA, moesin, on the glomerular endothelium. Moesin has partial amino-acid sequence homology with an epitope of MPOANCA.7 They found a high prevalence of anti-moesin antibodies in MPA patients (not published). An increased prevalence of thromboembolic disease occurs in AAV, and autoantibodies have now been described to plasminogen and tissue plasminogen activator in the sera of one quarter of PR3-ANCA-positive AAV patients. The presence of antiplasminogen antibodies correlated with venous thrombosis and with the severity of renal vasculitis.8
Table 1 | Definitions of ANCA-associated vasculitis according to the Chapel Hill consensus conference in 2012
ANCA-associated vasculitis Necrotizing vasculitis, with few or no immune deposits, predominantly affecting small vessels (i.e., capillaries, venules, arterioles, and small arteries), associated with MPO-ANCA or PR3-ANCA. Not all patients have ANCA. Add a prefix indicating ANCA reactivity. e.g., PR3-ANCA, MPO-ANCA, and ANCA negative Necrotizing vasculitis, with few or no immune deposits, predominantly affecting small vessels (i.e., capillaries, venules, or arterioles). Necrotizing arteritis involving small and medium arteries may be present. Necrotizing glomerulonephritis is very common. Pulmonary capillaritis often occurs. Granulomatous inflammation is absent Necrotizing granulomatous inflammation usually involving the upper and lower respiratory tract, and necrotizing vasculitis affecting predominantly small to medium vessels (e.g., capillaries, venules, arterioles, arteries, and veins). Necrotizing glomerulonephritis is common Eosinophil-rich and necrotizing granulomatous inflammation often involving the respiratory tract, and necrotizing vasculitis predominantly affecting small to medium vessels, and associated with asthma and eosinophilia. ANCA is more frequent when glomerulonephritis is present
Microscopic polyangiitis
Granulomatosis with polyangiitis (Wegeners) Eosinophilic granulomatosis with polyangiitis (ChurgStrauss)
Abbreviations: ANCA, antineutrophil cytoplasm antibody; MPO, myeloperoxidase; PR3, proteinase 3. Quoted from the article by Jennette et al.
Kidney International (2013) 84, 244249
245
mini review
S Furuta and DRW Jayne: AAV: recent developments
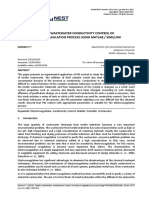
GENETICS AND THE ENVIRONMENT
Both genetic and environmental factors appear to contribute to the onset of AAV and the production of ANCA (Figure 1). Evidence for a genetic contribution in AAV has been increasing with familial associations and study of candidate genes, especially HLA DPB1*0401 in European GPA patients. The European Vasculitis Genetics Consortium has reported a genome-wide association study of 2687 Northern European Caucasian patients with GPA and MPA. Their results confirmed the distinct genetic difference between GPA and MPA. Associations with HLA-DP, SERPINA1, and PRTN3 were identified for GPA. SERPINA1 encodes for a-1 antitrypsin and PRTN3 encodes for PR3. An association with HLA-DQ was identified for MPA.4 Interestingly, the genetics were more strongly associated with ANCA specificity (MPO-/PR3-ANCA) than clinical diagnosis (MPA/GPA). Some previously reported associations with GPA, such as PTPN22 and CTLA-4, were not found, which might have been because of the sample size, which also limited the identification of further associations with MPA and of subgroup analyses. Associations with environmental factors, such as air pollutants, infections, and drugs, have also been investigated. Silica is a well-known air pollutant contributing to many autoimmune diseases including AAV. Peptides from Staphylococcus aureus have strong homology with peptides from complementary PR3, and Staphylococcus aureus infection has been associated with initiation and relapse of GPA. The anti-hLAMP-2 antibody also has 100% homology to FimH in Gram-negative bacteria. Cocaine use has caused several vasculitis syndromes including AAV, recently associated with contamination of cocaine by levamisole. Propylthiouracil (PTU) is the most frequent cause of drug-induced AAV (especially MPA).
The mechanism of drug-induced vasculitis is poorly understood. The finding of multiple autoantibodies is more common in drug-induced than primary AAV, suggesting a dysregulation of self-tolerance. Recently, Nakazawa et al.9 reported an association between PTU and neutrophil extracellular traps (NETs). NETs are a unique form of cell death seen with neutrophils, which is characterized by release of chromatin fibers and intracytoplasmic proteins, including MPO and PR3. ANCA has been shown to induce NETs in vitro, and NETs were detected in kidney biopsies from AAV patients. The shapes of the chromatin fibers in NETs were different between neutrophils treated with or without PTU and abnormal NETs induced by PTU were poorly digested by DNAaseI with persistent presence of MPO and PR3. Moreover, rats immunized with abnormal NETs induced by PTU produced MPO-ANCA and developed capillaritis. Their results not only explained a mechanism of PTU-induced MPA but also suggested a new model for the onset of AAV.
HISTOPATHOLOGY
Genetics HLA-DP, SERPINA1, PRTN3 (for GPA) HLA-DQ (for MPA) Others ... PTPN22?, CTLA4?
Environments Air pollutants ... Silica Infection ... S.aureus, E.coli Drug ........ Propylthiouracil, Cocaine Proinflammatory cytokine Complement system Alternative pathway C5a C5b ~ C9 (membrane attack complex)
Background
AAV often affects the kidneys and is the most common cause of rapidly progressive glomerulonephritis. Renal involvement is an important predictor of increased mortality risk and morbidity in AAV, and renal biopsy aids in both diagnosis and prognosis. An outcome-based classification of ANCAassociated glomerulonephritis histology has been developed to formalize the predictive value of the renal biopsy.10 In this classification, glomerular histology is classified into: Focal, Crescentic, Mixed, and Sclerotic classes according to the proportions of normal, cellular crescentic, and sclerotic glomeruli (Table 2). A validation study with 100 renal biopsies from AAV patients revealed that the classification was an independent predictor for estimated GFR after 1 year and 5 years. Although the Focal class showed good preservation of renal function and the Crescentic class a good chance for renal recovery, the Mixed and Sclerotic classes had, respectively, intermediate and high risks of progression to end-stage renal disease. In addition to glomerular lesions, T-cell tubulitis and tubular atrophy was reported in patients treated with rituximab in the RITUXVAS study.11 T-cell tubulitis was an independent predictor for estimated GFR after 12 months
Table 2 | Classification for ANCA-associated glomerulonephritis
Class Inclusion criteriaa X50% Normal glomeruli X50% Glomeruli with cellular crescents o50% Normal, o50% crescentic, o50% globally sclerotic glomeruli X50% Globally sclerotic glomeruli
T cells
B cells
Neutrophil PR3/MPO Priming ANCA, anti LAMP-2Ab? anti moesin Ab?
Dysregulation of immune system
Interaction
NETs T effector cells Inflammation of small vessel Perforin ROS Activation
Cytotoxicity
Vascular endothelium
Focal Crescentic Mixed Sclerotic
Figure 1 | Mechanism of the onset of antineutrophil cytoplasm antibody (ANCA)associated vasculitis. LAMP-2, lysome-associated membrane protein-2; MPO, myeloperoxidase; NETs, neutrophil extracellular traps; PR3, proteinase 3; ROS, reactive oxygen species.
246
Abbreviation: ANCA, antineutrophil cytoplasm antibody. Quoted from the article by Berden et al. a Pauci-immune staining pattern on immunofluorescence microscopy (IM) and X1 glomerulus with necrotizing or crescentic glomerulonephritis on light microscopy (LM) are required for inclusion in all four classes. Kidney International (2013) 84, 244249
S Furuta and DRW Jayne: AAV: recent developments
mini review
and tubular atrophy was an independent predictor for estimated GFR after 12 months and 24 months. Other studies support the significance of T cells, especially CD4 T-helper cells, in AAV.12 Although B celltargeted therapy with rituximab is effective in renal vasculitis, these observations support the activated T cell as an alternative therapeutic target that may be superior in some patients. Another recent topic in histopathology is the involvement of the complement system, especially the alternative pathway. Xing et al.13 detected components of the alternative pathway, factor B, factor P, C3d, and membrane-attack complex, in glomeruli and small blood vessels in kidney biopsy specimens from AAV patients. This was supported by the absence of disease in a murine MPA model after factor B or factor C5 knockout. Those results have led to ongoing trials of complement inhibition in AAV.
TREATMENTS AND OUTCOMES
The current treatment for AAV has been optimized by randomized controlled trials performed over the last 20 years (Table 3). It is not curative but aims to control disease activity in a 3- to 6-month induction phase of high-dose glucocorticoid and daily oral or intravenous-pulsed cyclophosphamide that is effective in 8090%. Despite maintenance therapy of low-dose glucocorticoid and azathioprine or methotrexate, at least 10% of patients relapse each year. These treatment regimens are associated with early and late toxicities and fail to prevent an increased mortality risk and vital organ damage. A rationale for B celltargeted therapy in AAV has emerged from the presence of B cells at sites of inflammation,
Table 3 | Randomized controlled trials in AAV
Trial CYCLOPS NORAM MEPEX PE oral-CY PSL (n 70) RTX IV-CYx2doses PSL (n 33) RTX PSL (n 99) Induction CY PSL CY PSL IV-CY PSL IV-CY/MTX PSLETN mPSL pulse oral-CY PSL (n 67) IV-CY PSL (n 11) Oral-CY PSL (n 98) Maintenance (trial) AZA PSL (n 76) MMF PSL (n 76) MTX PSL (n 63) ETN (n 89) Induction (trial) IV-CY PSL (n 76) MTX PSL (n 49) Induction (control) Oral-CY PSL (n 73) Oral-CY PSL (n 46)
correlation of B-cell activation with disease activity in GPA, the efficacy of cyclophosphamide, which is a relatively B cellspecific immunosuppressant, and the contribution of ANCA to the pathogenesis. Several case series and small prospective studies highlighted the efficacy of the anti-CD20 B celldepleting monoclonal antibody, rituximab in refractory AAV. Subsequently, two randomized trials evaluated rituximab for remission induction in new and relapsing patients. Both the RAVE and RITUXVAS trials found similar remission rates for newly diagnosed patients between rituximab- and cyclophosphamide-based regimens when combined with high-dose glucocorticoid.14,15 The RAVE trial also demonstrated superiority of rituximab for the subgroup treated for relapsing disease. However, no differences in safety were observed between the treatment groups, suggesting that glucocorticoid rather than cyclophosphamide is the major treatment-related cause of toxicity in AAV. Rituximab is now indicated for relapsing AAV and newly diagnosed AAV when cyclophosphamide avoidance is desirable. There is uncertainty as to how long the remission maintenance therapy should be continued; a metaanalysis looking at glucocorticoid withdrawal suggested lower glucocorticoid dosing increased relapse rates.16 However, the ability of rituximab to safely permit lower glucocorticoid dosing has not been examined. The pathogenicity of ANCA has contributed to a therapeutic rationale for plasma exchange in AAV, although removal of other factors may also be important. A metaanalysis of plasma exchange trials suggests a beneficial effect on the risk for end-stage renal disease but no effect on mortality.17 Current practice recommends plasma exchange
Maintenance AZA PSL Oral-CY/MTX PSL AZA PSL
Brief results There was no difference in efficacy. Cumulative dose of CY was less in IV-CY MTX was less effective than control
There was no difference in mortality and safety. Renal survival was better in PE There was no difference in efficacy and safety
RITUXVAS
PSL/AZA PSL
RAVE
AZA without PSL
RTX showed similar efficacy with control. There was no difference in safety
Trial CYCAZAREM IMPROVE WEGENT WGET
Maintenance (control) Oral-CY PSL (n 79) AZA PSL (n 80) AZA PSL (n 63) AZA (n 91) Relapse rates were similar. AZA reduced cumulative dose of CY MMF was less effective and there was no difference in safety There was no difference in efficacy and safety There was no difference in efficacy and safety
Abbreviations: AZA, azathioprine; CY, cyclophosphamide; ETN, etanercept; IV, intravenous; MMF, mycophenolate mofetil; MTX, methotrexate; PE, plasma exchange; PSL, prednisolone; RTX, rituximab.
Kidney International (2013) 84, 244249
247
mini review
S Furuta and DRW Jayne: AAV: recent developments
for those with severe renal disease or alveolar hemorrhage, although the evidence base in the latter indication is weak. The PEXIVAS trial is examining the effect of plasma exchange on patients with a GFR below 50 ml/min or with severe alveolar hemorrhage. Following control of features of vasculitis activity, the maintenance therapy aims to prevent vasculitis returning. The WEGENT trial aimed to demonstrate the superiority of methotrexate over azathioprine, but adverse event rates were similar and relapse rates at 36 months were 50 and 47%, respectively. The IMPROVE trial found mycophenolate mofetil was less effective compared with azathioprine for prevention of relapse, 55% vs. 38% after 39 months, with similar adverse event rates. Consequently, azathioprine or methotrexate, with or without low-dose glucocorticoid, is the preferred maintenance agents. Recently, Smith et al.18 published a retrospective study, which revealed that a 2-year fixed interval routine rituximab therapy reduced relapse rate in relapsing AAV patients treated with rituximab. This subject will be further studied in the ongoing RITAZAREM trial. EGPA has been excluded from most AAV trials. Recently, a French group examined the response to glucocorticoids in nonsevere EGPA and glucocorticoids, as well as cyclophosphamide in severe EGPA. Relapse rates in nonsevere EGPA are high if treated with glucocorticoids alone and studies of combinations with other immunosuppressants are needed. Similarly, only anecdotal data exist for the role of rituximab in EGPA. Two, small, open-label studies of an antiinterleukin-5 antibody, mepolizumab, have reported good effects in EGPA. Longer follow-up of induction trials have led to revision of the original conclusions. Patients with nonsevere AAV treated with methotrexate in the NORAM trial had similar survival and adverse events after a median of 6 years to those treated with initial cyclophosphamide, but required more subsequent glucocorticoid and cyclophosphamide because of a higher relapse rate.19 In long-term follow-up (median 4.3 years) of the CYCLOPS trial, an intravenous-pulsed cyclophosphamide based induction therapy, with 50% less cumulative cyclophosphamide exposure, was associated with a higher relapse risk compared with an oral cyclophosphamidebased induction therapy. However, that was not associated with increased mortality or long-term morbidity.20 Long-term outcome studies by the European Vasculitis Society cohort with 535 AAV patients with a median of 5.2-year follow-up reported cumulative survival rates at 1 and 5 years of 88 and 78%, respectively. Frequent causes of death within the first year were infection (48%) and active vasculitis (19%), and those after 1 year were cardiovascular disease (26%), malignancy (22%), and infection (20%).21 In the same cohort, 38% of 535 patients experienced a relapse, and the relapse was more common in PR3-ANCA-positive patients.22 Cardiovascular events were seen in 14% of patients, and, in addition to established risk factors, MPO-ANCA or negative ANCA status was independently
248
associated with higher risk.23 As to malignancy, only the risk of nonmelanoma skin cancer was increased in this cohort (sex- and area-standardized incidence ratio; 2.78).24 The low increases in cancer risk compared with previous studies might reflect short follow-up or lower exposure to cyclophosphamide in current protocols. Indeed, the French Vasculitis Study Group also showed similar results in their study for urotoxic adverse events.25 The risk of bladder cancer in AAV was low in an intravenous-pulsed cyclophosphamide group and a group diagnosed after 1998. Longer follow-up is necessary because of the late development of malignancy. Of newer therapeutic agents, the proteasome inhibitor bortezomib has demonstrated a stronger effect on autoantibody production than cyclophosphamide in experimental models. The immunosuppressive agent gusperimus proved efficacy in controlling disease activity in two nonrandomized trials of refractory or relapsing GPA. Compassionate use of the anti-CD52 pan lymphocytedepleting antibody, alemtuzumab, has led to sustained treatment-free remissions in AAV, but it is strongly immunosuppressive and is associated with severe adverse events in the elderly and those with renal failure. As an induction agent mycophenolate mofetil has compared well with cyclophosphamide in small studies of MPA. A larger induction study with mycophenolate mofetil in AAV, the MYCYC trial, will provide further information.
CONCLUSIONS
The classification of vasculitis has been further revised and new genetic associations are likely to drive more changes in how vasculitis is subgrouped. The discovery of newer autoantibodies raises the potential for newer biomarkers of clinical utility, as well as inspiring pathogenetic studies. Rituximab is now firmly established in the treatment of ANCA vasculitis, and further innovations permitting reduced immunosuppressive and glucocorticoid exposure are in development. Much of the recent progress has developed from the creation of international collaborative networks permitting consensus approaches and large-scale clinical studies.
DISCLOSURE
All the authors declared no competing interests.
ACKNOWLEDGMENTS
We acknowledge support from the Cambridge Biomedical Research Center. DRWJ has received research grant support from Roche/ Genentech and Viforpharma.
REFERENCES
1. Basu N, Watts R, Bajema I et al. EULAR points to consider in the development of classification and diagnostic criteria in systemic vasculitis. Ann Rheum Dis 2010; 69: 17441750. Jennette J, Falk R, Bacon P et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 2012; 65: 111. Mahr A, Katsahian S, Varet H et al. Revisiting the classification of clinical phenotypes of anti-neutrophil cytoplasmic antibody-associated vasculitis: a cluster analysis. Ann Rheum Dis 2012 (e-pub ahead of print).
Kidney International (2013) 84, 244249
2.
3.
S Furuta and DRW Jayne: AAV: recent developments
mini review
4. 5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
Lyons PA, Rayner TF, Trivedi S et al. Genetically distinct subsets within ANCA-associated vasculitis. N Engl J Med 2012; 367: 214223. Kain R, Tadema H, McKinney EF et al. High prevalence of autoantibodies to hLAMP-2 in anti-neutrophil cytoplasmic antibody-associated vasculitis. J Am Soc Nephrol 2012; 23: 556566. Roth AJ, Brown MC, Smith RN et al. Anti-LAMP-2 antibodies are not prevalent in patients with anti-neutrophil cytoplasmic autoantibody glomerulonephritis. J Am Soc Nephrol 2012; 23: 545555. Nagao T, Suzuki K, Utsunomiya K et al. Direct activation of glomerular endothelial cells by anti-moesin activity of anti-myeloperoxidase antibody. Nephrol Dial Transplant 2011; 26: 27522760. Berden AE, Nolan SL, Morris HL et al. Anti-plasminogen antibodies compromise fibrinolysis and associate with renal histology in ANCAassociated vasculitis. J Am Soc Nephrol 2010; 21: 21692179. Nakazawa D, Tomaru U, Suzuki A et al. Abnormal conformation and impaired degradation of NETs induced by propylthiouracil: Implication of disordered NETs in MPO-ANCA-associated vasculitis. Arthritis Rheum 2012; 64: 37793787. Berden AE, Ferrario F, Hagen EC et al. Histopathologic classification of ANCA-associated glomerulonephritis. J Am Soc Nephrol 2010; 21: 16281636. Berden AE, Jones RB, Erasmus DD et al. Tubular lesions predict renal outcome in antineutrophil cytoplasmic antibody-associated glomerulonephritis after rituximab therapy. J Am Soc Nephrol 2012; 23: 313321. Abdulahad WH, Lamprecht P, Kallenberg CG. T-helper cells as new players in ANCA-associated vasculitides. Arthritis Res Ther 2011; 13: 236. Xing GQ, Chen M, Liu G et al. Complement activation is involved in renal damage in human antineutrophil cytoplasmic autoantibody associated pauci-immune vasculitis. J Clin Immunol 2009; 29: 282291. Stone JH, Merkel PA, Spiera R et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med 2010; 363: 221232.
15. 16.
17.
18.
19.
20.
21. 22.
23.
24.
25.
Jones RB, Tervaert JW, Hauser T et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med 2010; 363: 211220. Walsh M, Merkel PA, Mahr A et al. Effects of glucocorticoid therapy on relapse rate in antineutrophil cytoplasmic antibody-associated vasculitis: A meta-analysis. Arthritis Care Res 2010; 62: 11661173. Walsh M, Catapano F, Szpirt W et al. Plasma exchange for renal vasculitis and idiopathic rapidly progressive glomerulonephritis: a meta-analysis. Am J Kidney Dis 2011; 57: 566574. Smith RM, Jones RB, Guerry MJ et al. Rituximab for remission maintenance in relapsing ANCA-associated vasculitis. Arthritis Rheum 2012; 64: 37603769. Faurschou M, Westman K, Rasmussen N et al. Long-term outcome of a clinical trial comparing methotrexate to cyclophosphamide for remission induction of early systemic ANCA-associated vasculitis. Arthritis Rheum 2012; 64: 34723477. Harper L, Morgan MD, Walsh M et al. Pulse versus daily oral cyclophosphamide for induction of remission in ANCA-associated vasculitis: long-term follow-up. Ann Rheum Dis 2012; 71: 955960. Flossmann O, Berden A, de Groot K et al. Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis 2011; 70: 488494. Walsh M, Flossmann O, Berden A et al. Risk factors for relapse of antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2012; 64: 542548. Suppiah R, Judge A, Batra R et al. A model to predict cardiovascular events in patients with newly diagnosed wegeners granulomatosis and microscopic polyangiitis. Arthritis Care Res 2011; 63: 588596. Heijl C, Harper L, Flossmann O et al. Incidence of malignancy in patients treated for anti-neutrophil cytoplasm antibody-associated vasculitis: follow-up data from European Vasculitis Study Group trials. Ann Rheum Dis 2011; 70: 14151421. Guenno GL, Mahr A, Pagnoux C et al. Incidence and predictors of urotoxic adverse events in cyclophosphamide-treated patients with systemic necrotizing vasculitides. Arthritis Rheum 2011; 63: 14351445.
Kidney International (2013) 84, 244249
249
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- EDUC 201 Facilitating Learner-Centered TeachingДокумент12 страницEDUC 201 Facilitating Learner-Centered TeachingCrizel MaeОценок пока нет
- Annotated Chess GameДокумент3 страницыAnnotated Chess Gameatul_desai_3100% (1)
- Nrneph 2013 232Документ11 страницNrneph 2013 232atul_desai_3Оценок пока нет
- Alekhine 1Документ1 страницаAlekhine 1atul_desai_3Оценок пока нет
- Clinical Trials in LNДокумент19 страницClinical Trials in LNatul_desai_3Оценок пока нет
- Costimulatory BlockadeДокумент11 страницCostimulatory Blockadeatul_desai_3Оценок пока нет
- Kasparov Vs IvanchukДокумент1 страницаKasparov Vs Ivanchukatul_desai_3Оценок пока нет
- Therapy of LN Lessons LearntДокумент8 страницTherapy of LN Lessons Learntatul_desai_3Оценок пока нет
- 3 Hepatmon 12 11 7359Документ9 страниц3 Hepatmon 12 11 7359atul_desai_3Оценок пока нет
- Anca VasculitisДокумент12 страницAnca Vasculitisatul_desai_3100% (2)
- 2028 Full PDFДокумент8 страниц2028 Full PDFdhineyОценок пока нет
- Hou YifanДокумент1 страницаHou Yifanatul_desai_3Оценок пока нет
- Game 2Документ2 страницыGame 2atul_desai_3Оценок пока нет
- Chess GameДокумент3 страницыChess Gameatul_desai_3Оценок пока нет
- Power of Passed PawnДокумент2 страницыPower of Passed Pawnatul_desai_3Оценок пока нет
- Clinical Trials in Lupus NephritisДокумент19 страницClinical Trials in Lupus Nephritisatul_desai_3Оценок пока нет
- Diag.1 Diag.2 Diag.3: Find The Move For Black, and Calculate The Response of White To It Blacks Response?Документ2 страницыDiag.1 Diag.2 Diag.3: Find The Move For Black, and Calculate The Response of White To It Blacks Response?atul_desai_3Оценок пока нет
- Calcium MetabolismДокумент51 страницаCalcium Metabolismatul_desai_3Оценок пока нет
- Laszlo Vs Geller Find Moves For BlackДокумент2 страницыLaszlo Vs Geller Find Moves For Blackatul_desai_3Оценок пока нет
- Approach Hypophosphatemic RickeДокумент1 страницаApproach Hypophosphatemic Rickeatul_desai_3Оценок пока нет
- DIET in Chronic Kidney DiseaseДокумент3 страницыDIET in Chronic Kidney Diseaseatul_desai_3Оценок пока нет
- Update On Cystatin CДокумент9 страницUpdate On Cystatin Catul_desai_3Оценок пока нет
- Permaeability Factor in FSGSДокумент4 страницыPermaeability Factor in FSGSatul_desai_3Оценок пока нет
- Obesity-Related Cardiorenal DiseaseДокумент13 страницObesity-Related Cardiorenal Diseaseatul_desai_3Оценок пока нет
- Complicated Urinary Tract InfectionsДокумент39 страницComplicated Urinary Tract InfectionsAndreas IoannouОценок пока нет
- Association of Dialysate Bicarbonate Concentration With Mortality in The Dialysis Outcomes and Practice Patterns Study (DOPPS)Документ9 страницAssociation of Dialysate Bicarbonate Concentration With Mortality in The Dialysis Outcomes and Practice Patterns Study (DOPPS)atul_desai_3Оценок пока нет
- Living Kidney DonationДокумент2 страницыLiving Kidney Donationatul_desai_3Оценок пока нет
- Renal Artery Stenosis-Predicting Responses To RevascularizaДокумент1 страницаRenal Artery Stenosis-Predicting Responses To Revascularizaatul_desai_3Оценок пока нет
- Renal Cancer in Von Hippel-Lindau DiseaseДокумент10 страницRenal Cancer in Von Hippel-Lindau Diseaseatul_desai_3Оценок пока нет
- Atypical Haemolytic Uraemic Syndrome With UnderlyingДокумент14 страницAtypical Haemolytic Uraemic Syndrome With Underlyingatul_desai_3Оценок пока нет
- Virtual Reality in Tourism: A State-Of-The-Art ReviewДокумент39 страницVirtual Reality in Tourism: A State-Of-The-Art ReviewMegi VisiОценок пока нет
- Risk Assessment of Jetty-Less LNG Transfer System For Onshore LNG TerminalДокумент335 страницRisk Assessment of Jetty-Less LNG Transfer System For Onshore LNG TerminalMuhammad AdlanieОценок пока нет
- Proof of Performance Mobilith SHC 1500 Zahnradkupplung in Kohleminen EngДокумент1 страницаProof of Performance Mobilith SHC 1500 Zahnradkupplung in Kohleminen EngLaurent GuyotОценок пока нет
- Bsce Quarantine Reviewer Diagnostic Exams PDFДокумент27 страницBsce Quarantine Reviewer Diagnostic Exams PDFLaurence CervoОценок пока нет
- Understanding Factors in Second Language AcquisitionДокумент9 страницUnderstanding Factors in Second Language AcquisitionfatemehОценок пока нет
- Lecture Notes On CNCДокумент125 страницLecture Notes On CNCniteen_mulmule48580% (5)
- BHCS38523 AnomAlert Motor Anomaly Detector - R1 PDFДокумент2 страницыBHCS38523 AnomAlert Motor Anomaly Detector - R1 PDFZahid IrfanОценок пока нет
- Pedroso Probset 1Документ11 страницPedroso Probset 1Princess Niña B. PedrosoОценок пока нет
- Republic of The Philippines Carlos Hilado Memorial State College Talisay City, Negros OccidentalДокумент5 страницRepublic of The Philippines Carlos Hilado Memorial State College Talisay City, Negros OccidentalAbegail Marie LibresОценок пока нет
- Parramatta High School Year 9 Individual Research Project: ContextДокумент18 страницParramatta High School Year 9 Individual Research Project: ContextVikram BologaneshОценок пока нет
- Atmosphere Lesson PlanДокумент7 страницAtmosphere Lesson PlanJasmine DanaОценок пока нет
- Yulo, Brittany L. August 15, 2021 FS - 301 WEEK 4: Incised WoundsДокумент2 страницыYulo, Brittany L. August 15, 2021 FS - 301 WEEK 4: Incised WoundsBrittany YuloОценок пока нет
- Utilizing sludge to produce strong bricksДокумент7 страницUtilizing sludge to produce strong bricksSagirul IslamОценок пока нет
- 2018 Article 3585Документ14 страниц2018 Article 3585timosp1973Оценок пока нет
- Calamansi-Aloe Vera-Malunggay Organicantibacterial Hand SanitizerДокумент7 страницCalamansi-Aloe Vera-Malunggay Organicantibacterial Hand SanitizerELIZABETH MABIDA100% (2)
- Synthesis PowerpointДокумент31 страницаSynthesis PowerpointKara DОценок пока нет
- Prealgebra 2nd Edition Miller ONeill Hyde 007338447X Test BankДокумент16 страницPrealgebra 2nd Edition Miller ONeill Hyde 007338447X Test Bankmatthew100% (21)
- Co Op Housing Cover LetterДокумент6 страницCo Op Housing Cover Lettere7dhewgp100% (1)
- De HSG 60Документ8 страницDe HSG 60Phạm Trần Tiến KhánhОценок пока нет
- Textile Wastewater Conductivity Control of Electrocoagulation Process Using Matlab / SimulinkДокумент6 страницTextile Wastewater Conductivity Control of Electrocoagulation Process Using Matlab / SimulinkazerfazОценок пока нет
- General Tolerance (From ASME Y14.5M-2009) : Tolerances Can Be ExpressedДокумент12 страницGeneral Tolerance (From ASME Y14.5M-2009) : Tolerances Can Be ExpressedVivek PatelОценок пока нет
- Assignment 2 InstrumentationДокумент10 страницAssignment 2 InstrumentationDaneshSathaОценок пока нет
- ICS141: Discrete Mathematics For Computer Science IДокумент27 страницICS141: Discrete Mathematics For Computer Science IMahmoud Abdel-SalamОценок пока нет
- Geo Lab ReportДокумент12 страницGeo Lab ReportArivalagan Revichandran100% (1)
- 11.1 - Skill Acquisition: Assessment Statement Notes 11.1.1Документ3 страницы11.1 - Skill Acquisition: Assessment Statement Notes 11.1.1Alamedin SabitОценок пока нет
- General Specifications: Ph/redox and Temperature Sensor Model PH20 and FU20Документ8 страницGeneral Specifications: Ph/redox and Temperature Sensor Model PH20 and FU20HolicsОценок пока нет
- Examiners' Commentaries 2021: MN3141 Principles of Marketing Important NoteДокумент20 страницExaminers' Commentaries 2021: MN3141 Principles of Marketing Important NoteChandani FernandoОценок пока нет
- Failure Case Studies in Civil EngineeringДокумент135 страницFailure Case Studies in Civil Engineeringpratip_b100% (2)
- ITM Unit 2 - Tutorial Sheet - StudentsДокумент4 страницыITM Unit 2 - Tutorial Sheet - StudentsalexОценок пока нет