Академический Документы
Профессиональный Документы
Культура Документы
Pharmacotherapy For Obsessive-Compulsive Disorder PDF
Загружено:
dreamingИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pharmacotherapy For Obsessive-Compulsive Disorder PDF
Загружено:
dreamingАвторское право:
Доступные форматы
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
Official reprint from UpToDate www.uptodate.com 2013 UpToDate
Pharmacotherapy for obsessive-compulsive disorder Author Helen Blair Simpson, MD, PhD Disclosures All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Oct 2013. | This topic last updated: Dez 16, 2011. INTRODUCTION Obsessive-compulsive disorder (OCD) is characterized by recurrent, intrusive, and distressing thoughts, images, or impulses (ie, obsessions) and repetitive mental or behavioral acts that the individual feels driven to perform (ie, compulsions) to prevent or reduce distress. OCD can be effectively treated with serotonergic antidepressants as well as cognitive-behavioral therapy. However, patients frequently experience a partial response to treatment. A number of augmentation strategies have been studied. Pharmacotherapy for OCD in adults is discussed here. The epidemiology, clinical manifestations, and diagnosis of OCD are discussed separately. Psychotherapy for OCD, deep brain stimulation for OCD, and OCD in pregnant and postpartum women are also discussed separately. (See "Obsessive-compulsive disorder in adults: Epidemiology, pathogenesis, clinical manifestations, course, and diagnosis" and "Psychotherapy for obsessivecompulsive disorder" and "Obsessive-compulsive disorder in pregnant and postpartum women" and "Deep brain stimulation for treatment of obsessive-compulsive disorder".) MONOTHERAPY Efficacy Two classes of serotonergic antidepressants are strongly supported by randomized trials for OCD, while evidence for the third is weaker: Selective serotonin reuptake inhibitor (SSRI) antidepressants: Fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram, and escitalopram Clomipramine: A tricyclic antidepressant that inhibits the reuptake of serotonin and norepinephrine. Venlafaxine: a serotonin norepinephrine reuptake inhibitor (SNRI) antidepressant Selective serotonin reuptake inhibitors The SSRIs have been shown to be efficacious for OCD in large, multi-site randomized trials. A meta-analysis of 17 randomized trials with a total of 3097 patients with OCD found SSRIs to be more effective than placebo in reducing the symptoms of OCD [1]. No individual SSRI was found to be more efficacious than the other SSRIs for OCD. All of the SSRIs except citalopram and escitalopram have been approved for the treatment of OCD by the Food and Drug Administration (FDA) in the United States (US). Clomipramine A meta-analysis of seven randomized trials of 392 patients with OCD found clomipramine to reduce symptoms of OCD compared to placebo [2]. A tricyclic antidepressant, clomipramine inhibits the reuptake of serotonin and norepinephrine. Clomipramine is generally less well tolerated than the SSRIs or SNRIs. (See 'Side effects' below.) Head-to-head comparisons between clomipramine and several of the SSRIs (fluoxetine, fluvoxamine, paroxetine, and sertraline) have not shown either to be superior for OCD [3-9]. Some meta-analyses of randomized trials that did not directly compare clomipramine to SSRIs have suggested that clomipramine has a greater effect size than the SSRIs [10]. However, the studies of SSRIs generally occurred in an era later than the clomipramine trials, and thus likely included more patients who had previously responded inadequately to another agent. Section Editor Murray B Stein, MD, MPH Deputy Editor Richard Hermann, MD
1 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
In general, SSRIs and clomipramine lead to improvement in 40 to 60 percent of people with OCD. On average, OCD patients who receive an adequate trial of one of these agents will experience a 20 to 40 percent reduction in their OCD symptoms [11,12]. Thus, they typically offer amelioration rather than elimination of symptoms. Serotonin-norepinephrine reuptake inhibitors Based on their mechanism and similarity to the SSRIs, we would expect the serotonin-norepinephrine reuptake inhibitors (SNRIs) to effectively treat OCD. There has been limited study of these medications in OCD, however, and they have not been approved by the US FDA for OCD [13-18]. One small, eight-week trial that randomly assigned 30 patients with OCD to either venlafaxine or placebo found no significant difference in OCD symptom reduction between the two groups [13]. The maximum dose of venlafaxine was limited to 225 mg/day. Two additional randomized trials compared higher doses of venlafaxine to SSRIs or clomipramine, finding similar rates of response among the agents [14,15]. However, these trials lacked a placebo control. Larger, placebo-controlled trials are needed. Duloxetine has not been studied in OCD in randomized trials. A case series reported on four patients with OCD treated with duloxetine (up to 120 mg/day) after having an inadequate response to an SSRI or clomipramine, three of whom experienced a reduction in OCD symptoms [17]. Side effects Common side effects of serotonergic antidepressants are described briefly below and in more detail separately. Serious adverse events, including serotonin syndrome and suicidality, are described separately. (See "Serotonin syndrome" and "Effect of antidepressants on suicide risk in adults".) Selective serotonin reuptake inhibitors SSRIs are generally well-tolerated. Potential side effects include gastrointestinal problems (eg, nausea or diarrhea), agitation, sleep disturbances (eg, insomnia, vivid dreams), increased tendency to sweat, and sexual side effects (eg, decrease in libido, trouble ejaculating, delayed orgasm). (See "Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects".) Clomipramine Some patients may not be able to tolerate the side effects of clomipramine, which include sedation, dry mouth, constipation, urinary delay, orthostatic hypotension, and cardiac conduction delay. (See "Tricyclic and tetracyclic drugs: Pharmacology, administration, and side effects", section on 'Clomipramine'.) Serotonin norepinephrine reuptake inhibitors SNRIs are generally well tolerated; the most common side effects include nausea, constipation, dizziness, insomnia, sedation and sexual side effects. Venlafaxine may cause elevated blood pressure and increases risk for gastrointestinal bleeding. (See "Serotonin-norepinephrine reuptake inhibitors (SNRIs): Pharmacology, administration, and side effects".) Medication selection When medication is used, we recommend SSRIs as first-line treatment. There is much greater support from randomized trials for SSRIs than for venlafaxine; the SSRIs have a superior side effect profile compared to clomipramine [19]. Because none of the individual SSRIs have shown an advantage in efficacy for OCD, the choice among the SSRIs can be made on the basis of prior treatment response, drug side effects and their acceptability to the patient, and the potential for drug interactions. (See 'Selective serotonin reuptake inhibitors' above and 'Serotonin-norepinephrine reuptake inhibitors' above and 'Clomipramine' above and 'Side effects' above.) A beneficial aspect of the serotonergic antidepressants for OCD is that these medications can provide effective treatment for several depressive and anxiety disorders that commonly co-occur with OCD (See 'Comparing pharmacotherapy and psychotherapy' below.) If an adequate trial of the SSRI results in no response, the patient should be given another trial of monotherapy, either with a second SSRI, clomipramine, or venlafaxine. It has been estimated that less than half of patients will benefit from switching from one SSRI to another, and the likelihood of response diminishes as the number of failed adequate trials increases [19]. If a trial of one of the serotonergic antidepressants results in a partial response, but the patient continues to experience clinically significant symptoms, we suggest augmentation of this agent. (See 'Augmentation' below.) Administration and course of treatment Most fixed-dose trials of the serotonergic antidepressants studied in OCD suggest that higher doses led to greater response rates and/or greater mean rates of improvement
2 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
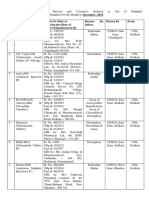
compared to lower doses [20-24]. A meta-analysis that supported this dose-response relationship also found that higher doses are associated with a higher proportion of dropouts due to side effects [25]. The suggest the following therapeutic-dose ranges for OCD [19]: SSRIs Fluoxetine 40 to 80 mg/day Fluvoxamine 200 to 300 mg/day Paroxetine 40 to 60 mg/day Sertraline 200 mg/day Citalopram up to 40 mg/day Escitalopram 20 to 40 mg/day Clomipramine 100 to 250 mg/day Venlafaxine 225 to 350 mg/day Patients should be started at a low dose to enhance tolerability (eg, fluoxetine 10 or 20 mg/day). The dose can be increased every week or every other week (as tolerated). The patient should be maintained at a dose within the therapeutic range for at least 6 weeks before concluding that he or she is resistant to the agent. This usually amounts to an 8 to 12 week trial overall, given usual titration schedules. An adequate trial of medication for OCD has been defined as the maximum dose tolerated for a minimum of 6 weeks [19]. It is important to explain to patients the 4 to 6 week delay in drug response, so that they do not prematurely stop the medication. (See "Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects".) Evidence is limited on the efficacy of higher-than-recommended dosing of SSRIs for OCD (eg, fluoxetine 120 mg/day). A trial randomly assigned patients with OCD who had not responded to 16 weeks of sertraline (titrated from 50 mg/day to 200 mg/day) to continue sertraline at 200 mg/day or to continue at an increased dose (averaging 357 mg/day) [26]. After 12 weeks of treatment, the higher dose group showed greater average improvement than the lower dose group. However, the difference was clinically modest. Both groups continued to have clinically significant symptoms and similar rates of adverse events. Thus, increasing SSRIs to higher than recommended doses may be effective for certain OCD patients, but this is not a highly effective strategy for all and can lead to more side effects. Duration of treatment Although clinical trials of current medications for OCD are mostly short-term, extended trials of SSRIs and clomipramine, which randomly assigned drug responders to continued medication treatment or to placebo, have generally found that patients who continue medication have a lower rate of relapse than patients on placebo [21,27-30]. Relapse rates have varied widely, in part due to methodological differences among studies. As a result, American Psychiatric Association practice guidelines suggest that OCD patients who respond to an adequate trial of a serotonergic antidepressant should stay on that medication for at least one to two years [19]. However, this needs further study. If the medication is discontinued, American Psychiatric Association practice guidelines recommend that it should be slowly tapered (eg, 10 to 25 percent every one to two months). Other medications as monotherapy There is a paucity of data supporting the use of other medications as monotherapy for OCD. No other drugs are approved for the disorder by the Food and Drug Administration in the US. Small, limited trials have suggested possible benefits of several other agents: mirtazapine (an antagonist at presynaptic alpha-2 adrenergic, 5-HT2, and 5-HT3 receptors) [31], tramadol (an agonist at the mu opioid receptor as well as a modulator of noradrenergic and serotonergic systems) [32], and stimulants (eg, D-amphetamine) [33-35]. All require further study with randomized trials to determine efficacy for OCD. There are no randomized trials of antipsychotic medications as monotherapy for OCD. Small, open trials have shown inconsistent results [36,37]. AUGMENTATION With many patients experiencing a partial response to a serotonergic antidepressant, there is considerable interest in strategies to augment these medications for OCD. Common approaches to augmentation
3 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
include adding: Risperidone or another antipsychotic medication Cognitive-behavioral therapy (CBT) A low dose of clomipramine (to an SSRI or SNRI) Antipsychotic augmentation Antipsychotic drugs have been shown to be efficacious at further reducing OCD symptoms when added to an SSRI or clomipramine. Efficacy Meta-analyses of randomized trials have found risperidone and haloperidol to effectively augment the effects of SSRIs or clomipramine in patients with OCD who experienced incomplete response to the antidepressant alone, while studies of quetiapine and olanzapine have been mixed [38-44]. It is unclear whether varying responses found across antipsychotics reflect differences in efficacy or methodological issues specific to the trials. A 2006 meta-analysis of the augmentation of SSRIs or clomipramine with first or second-generation antipsychotic drugs identified 9 randomized trials of 278 patients with treatment-refractory OCD [60]. Patients who received antipsychotic augmentation were generally more likely to respond (defined as a 35-percent reduction in OCD symptoms) than patients who received placebo augmentation (32 versus 11 percent). The data supporting efficacy were strongest for risperidone and haloperidol. The authors estimated that about one-third of patients will have a meaningful treatment response to this strategy. A 2010 meta-analysis of augmentation of SSRIs or clomipramine with second-generation antipsychotics (SGA) differed methodologically somewhat from the 2006 meta-analysis [61]: a total of 396 patients with OCD from 11 randomized trials were studied, only second-generation antipsychotics were studied, inclusion was not limited to treatment-refractory OCD (one trial included non-refractory patients) [62], and the primary outcome (treatment response) was defined as a 25-percent reduction in OCD symptoms. However, the findings were generally congruent with the prior meta-analysis: Augmenting SSRIs or clomipramine with risperidone (four trials) resulted in a higher rate of treatment response than placebo augmentation. Low average doses (0.5 to 2.2 mg/day) of risperidone were used. Augmenting SSRIs or clomipramine with quetiapine (five trials) led to a response rate not significantly different than that of placebo augmentation. Quetiapine showed superiority to placebo in a secondary outcome, mean reduction in OCD symptoms. Olanzapine (two trials) augmenting SSRIs or clomipramine did not lead to a significantly different result than placebo augmentation. The efficacy of newer antipsychotics like aripiprazole remains unclear. Case reports and an open-label study suggest benefit in some patients [45,46], but randomized trials are needed. Side effects Side effects were incompletely reported across studies described above, but available data suggested that antipsychotic augmentation was associated with greater weight gain and/or sedation than SSRI or clomipramine monotherapy [47,48]. Side effects of antipsychotic drugs can include metabolic syndrome, extrapyramidal symptoms, tardive dyskinesia, and neuroleptic malignant syndrome [49]. Administration Given the delayed onset of action of SSRIs or clomipramine, the antipsychotic should be added only after the patient has not responded following a trial of at least 12-weeks at the maximal antidepressant dose tolerated [19]. Low antipsychotic doses appear effective (eg, 0.5 to 3 mg for risperidone or the equivalent). The antipsychotic should be terminated after one month if the patient does not show a clear benefit. This limits exposure to antipsychotics known risks. (See 'Side effects' above and "Second-generation antipsychotic medications: Pharmacology, administration, and comparative side effects" and "First-generation antipsychotic medications: Pharmacology, administration, and comparative side effects".) Efficacy trials of antipsychotic augmentation for OCD have examined short-term use only. One small retrospective study suggested a high risk of relapse when the antipsychotic was discontinued; 13 of 15 patients had a return of OCD symptoms when their antipsychotic was stopped [50]. Thus, patients who respond to antipsychotic augmentation are advised to continue the medication for up to six months before an attempt is made to gradually
4 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
discontinue. If symptoms recur or worsen during the taper, then the antipsychotic can be restarted for a longer period provided that the patient is not experiencing long-term adverse effects of the antipsychotic. Augmentation with CBT Two randomized controlled trials have demonstrated the benefit of adding cognitivebehavioral therapy (CBT), consisting of exposure and response prevention, to the treatment of patients with OCD that have partially responded to a serotonergic antidepressant [51,52]. (See 'Comparing pharmacotherapy and psychotherapy' below and 'Combining pharmacotherapy and psychotherapy' below.) In one trial, 96 patients who completed three months of medication (paroxetine or venlafaxine) for OCD were randomized to a 6 month continuation of the medication alone or with the addition of exposure and response prevention (18 45-minute sessions over six months [51]). The augmentation of the antidepressant with exposure and response prevention modestly increased the proportion of patients achieving remission compared to continued medication alone. The mean reduction in OCD symptoms did not significantly differ between the two groups. In a second trial, 108 patients who continued to experience clinically significant symptoms of OCD despite 12 weeks of a therapeutic dose of a serotonergic antidepressant were randomly assigned to exposure and response prevention or to stress management therapy (17 90-minute sessions over eight weeks), while continuing the medication [52]. After 8 weeks, patients who received exposure and response therapy plus the medication experienced a greater decrease in OCD symptoms, a higher rate of treatment response (74 versus 22 percent) and a greater proportion with mild to minimal symptoms (33 versus 4 percent) compared to patients who received stress management therapy plus the antidepressant. Other pharmacologic augmentation Although not systematically studied, we have used low doses of clomipramine (10 to 50 mg/day) to augment an SSRI or SNRI in cases of OCD responding partially to the antidepressant. Higher doses can result in markedly increased levels of clomipramine, and should ideally be used in conjunction with monitoring serum levels of the drug and its metabolites [53]. Other medications have been tested in augmentation of serotonergic antidepressants in OCD. Although promising in case reports or open trials, several did not show clear efficacy in small randomized trials, including lithium, buspirone, clonazepam, L-triiodothyronine, pindolol, and desipramine [19]. Other strategies that have shown promise but need further study in randomized controlled trials include: adding topiramate [54,55], morphine sulfate [56], d-amphetamine or caffeine [57], or ondansetron [58,59]. Novel medications Because of the limitations of current medications for OCD, medications that affect other brain neurotransmitter systems continue to be studied. Medications thought to modulate the glutamate system have shown some promise as an adjunct to SSRIs in case reports or open-label studies [60], including N-acetylcysteine (an amino-acid derivative that has glutamate-modulating properties) [61], memantine (a noncompetitive NMDA receptor antagonist) [62-66], riluzole (an agent thought to modulate glutamate both by reducing neuronal release and increasing glial reuptake) [67], and minocycline (an agent thought to modulate glutamate by enhancing glial glutamate transport) [68]. COMPARING PHARMACOTHERAPY AND PSYCHOTHERAPY Available evidence suggests that cognitivebehavioral therapy may be more effective than treatment with serotonergic antidepressants for non-comorbid OCD. The type of cognitive-behavioral therapy commonly used for OCD uses exposure and response prevention (ERP), sometimes with adjunctive cognitive restructuring. A 12-week randomized trial compared ERP (provided intensively for 4 weeks followed by 8 weekly maintenance sessions), clomipramine (200 to 250 mg/day), ERP plus clomipramine, and pill placebo in 122 patients with OCD [69]. A greater proportion of patients responded to ERP compared to clomipramine or placebo (62 versus 42 and 8 percent, respectively). Mean OCD symptom reduction was greater in the group receiving ERP compared to patients receiving clomipramine or placebo. In OCD comorbid with major depression or other anxiety disorders, the serotonergic antidepressants have the additional benefit of being an effective treatment for several of these disorders (See "Obsessive-compulsive disorder in adults: Epidemiology, pathogenesis, clinical manifestations, course, and diagnosis", section on 'Epidemiology'.) COMBINING PHARMACOTHERAPY AND PSYCHOTHERAPY CBT and clomipramine or SSRIs Combined therapy with medication and CBT may be more effective than monotherapy for some, but not all, patients with OCD. Studies suggest that how CBT and serotonergic
5 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
antidepressants are combined (specifically the dose of each treatment and the timing of when they are combined) can influence the effectiveness of this strategy. As examples: In the aforementioned trial, the effects of exposure and response prevention (ERP) did not differ from that of ERP plus clomipramine for OCD [69]. This trial studied OCD patients who were relatively free of comorbid depression, and ERP was delivered in an intensive format (daily sessions for four weeks). Moreover, the CBT and clomipramine were started at the same time, such that the full effects of clomipramine were not yet realized during the CBT treatment. (See 'Comparing pharmacotherapy and psychotherapy' above.) In contrast, in the two trials discussed above of effective CBT augmentation of serotonergic antidepressants, patients were already stable on a serotonergic antidepressant, and the CBT was delivered less frequently. (See 'Augmentation with CBT' above.) CBT and D-cycloserine D-cycloserine, a partial agonist at the N-methyl-D-aspartate receptor, may speed up the time to response to ERP in OCD [70]. Specifically, three small randomized trials have compared ERP to exposure augmented by D-cycloserine [71-73]. In two of the studies, D-cycloserine reduced the time to response but did not result in an increased response by the end of the trial [71,73]. D-cycloserines proposed mechanism of action is to enhance extinction learning in exposure therapy. D-cycloserine has been found to enhance fear extinction in animal models. SUMMARY AND RECOMMENDATIONS We recommend that patients with obsessive-compulsive disorder (OCD) be treated with cognitivebehavioral therapy (CBT), a selective serotonin reuptake inhibitor (SSRI) medication, or both ( Grade 1A) We suggest use of exposure and response prevention (a type of CBT) rather than medication as first-line treatment of non-comorbid OCD (Grade 2B). An SSRI can be used in patients who prefer medication to psychotherapy, or when CBT is not available. (See 'Comparing pharmacotherapy and psychotherapy' above and "Psychotherapy for obsessive-compulsive disorder".) Higher doses of antidepressants have generally been found to be more effective for OCD. As an example, fluoxetine can be gradually titrated to 40 to 80 mg/day. The medication should be continued within the therapeutic range for at least six weeks before concluding that the drug is ineffective. (See 'Administration and course of treatment' above.) In patients with a severe, comorbid disorder that responds to SSRI treatment, we suggest treatment of OCD with an SSRI. (Grade 2C). (See 'Monotherapy' above and 'Medication selection' above.) If an adequate trial of the SSRI results in no response, we suggest treatment with a second SSRI, clomipramine, or venlafaxine (Grade 2C). (See 'Monotherapy' above and 'Medication selection' above.) If a trial of an SSRI or SNRI results in a partial response, but the patient continues to experience clinically significant symptoms, we suggest augmenting the antidepressant with CBT or an antipsychotic medication (eg, risperidone 0.5 to 3 mg/day) (Grade 2B). Another approach with less supporting evidence is the addition of clomipramine (10 to 50 mg/day). (See 'Augmentation' above.) SSRIs and clomipramine generally lead to improvement in 40 to 60 percent of people with OCD. When patients have an adequate response, practice guidelines recommend that they be maintained on the medication for at least one to two years, though more research is needed on this issue. (See 'Duration of treatment' above.) ACKNOWLEDGMENT The editorial staff at UpToDate, Inc. would like to acknowledge Drs. Wayne Katon and Paul Ciechanowski, who contributed to an earlier version of this topic review. Use of UpToDate is subject to the Subscription and License Agreement.
6 de 7
02/12/2013 05:06
Pharmacotherapy for obsessive-compulsive disorder Topic 14629 Version 2.0
http://www.uptodate.com/contents/pharmacotherapy-for-obsessive-com...
7 de 7
02/12/2013 05:06
Вам также может понравиться
- Treatment of Acute Stress Disorder PDFДокумент4 страницыTreatment of Acute Stress Disorder PDFdreamingОценок пока нет
- Psychotherapy For Specific Phobia in Adults PDFДокумент6 страницPsychotherapy For Specific Phobia in Adults PDFdreamingОценок пока нет
- Psychotherapy For Obsessive-Compulsive Disorder PDFДокумент9 страницPsychotherapy For Obsessive-Compulsive Disorder PDFdreamingОценок пока нет
- Generalized Anxiety Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFДокумент7 страницGeneralized Anxiety Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFdreaming100% (1)
- Psychotherapy For Panic Disorder PDFДокумент9 страницPsychotherapy For Panic Disorder PDFdreaming100% (2)
- Pharmacotherapy For Social Anxiety Disorder PDFДокумент8 страницPharmacotherapy For Social Anxiety Disorder PDFdreamingОценок пока нет
- Pharmacotherapy For Panic Disorder PDFДокумент8 страницPharmacotherapy For Panic Disorder PDFdreamingОценок пока нет
- Co-Occurring Anxiety Disorders and Substance Use Disorders - Epidemiology, Clinical Manifestations, and Diagnosis PDFДокумент7 страницCo-Occurring Anxiety Disorders and Substance Use Disorders - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreamingОценок пока нет
- Pharmacotherapy For Generalized Anxiety Disorder PDFДокумент16 страницPharmacotherapy For Generalized Anxiety Disorder PDFdreaming100% (1)
- Obsessive-Compulsive Disorder in Pregnant and Postpartum Women PDFДокумент6 страницObsessive-Compulsive Disorder in Pregnant and Postpartum Women PDFdreamingОценок пока нет
- Comorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFДокумент24 страницыComorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreaming0% (1)
- Obsessive-Compulsive Disorder in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, and Diagnosis PDFДокумент9 страницObsessive-Compulsive Disorder in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, and Diagnosis PDFdreamingОценок пока нет
- Pharmacotherapy For Specific Phobia in Adults PDFДокумент4 страницыPharmacotherapy For Specific Phobia in Adults PDFdreamingОценок пока нет
- Treatment of Acute Procedure Anxiety in Adults PDFДокумент7 страницTreatment of Acute Procedure Anxiety in Adults PDFdreaming100% (1)
- Combat Operational Stress Reaction PDFДокумент12 страницCombat Operational Stress Reaction PDFdreamingОценок пока нет
- Panic Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFДокумент10 страницPanic Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFdreamingОценок пока нет
- Agoraphobia in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, and Diagnosis PDFДокумент8 страницAgoraphobia in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, and Diagnosis PDFdreamingОценок пока нет
- Psychotherapy For Social Anxiety Disorder PDFДокумент6 страницPsychotherapy For Social Anxiety Disorder PDFdreaming100% (1)
- Psychotherapy For Generalized Anxiety Disorder PDFДокумент9 страницPsychotherapy For Generalized Anxiety Disorder PDFdreamingОценок пока нет
- Acute Stress Disorder - Epidemiology, Clinical Manifestations, and Diagnosis PDFДокумент6 страницAcute Stress Disorder - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreaming100% (1)
- Acute Procedure Anxiety in Adults - Course, Screening, Assessment, and Differential Diagnosis PDFДокумент4 страницыAcute Procedure Anxiety in Adults - Course, Screening, Assessment, and Differential Diagnosis PDFdreamingОценок пока нет
- Posttraumatic Stress Disorder - Epidemiology, Pathophysiology, Clinical Manifestations, Course, and Diagnosis PDFДокумент10 страницPosttraumatic Stress Disorder - Epidemiology, Pathophysiology, Clinical Manifestations, Course, and Diagnosis PDFdreamingОценок пока нет
- Treatment For Specific Phobias of Medical and Dental Procedures PDFДокумент8 страницTreatment For Specific Phobias of Medical and Dental Procedures PDFdreamingОценок пока нет
- Deep Brain Stimulation For Treatment of Obsessive-Compulsive Disorder PDFДокумент6 страницDeep Brain Stimulation For Treatment of Obsessive-Compulsive Disorder PDFdreamingОценок пока нет
- Social Anxiety Disorder - Epidemiology, Clinical Manifestations, and Diagnosis PDFДокумент7 страницSocial Anxiety Disorder - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreamingОценок пока нет
- Pharmacotherapy For Posttraumatic Stress Disorder PDFДокумент6 страницPharmacotherapy For Posttraumatic Stress Disorder PDFdreamingОценок пока нет
- Psychotherapy For Posttraumatic Stress Disorder PDFДокумент9 страницPsychotherapy For Posttraumatic Stress Disorder PDFdreamingОценок пока нет
- Treatment of Co-Occurring Anxiety Disorders and Substance Use Disorders PDFДокумент9 страницTreatment of Co-Occurring Anxiety Disorders and Substance Use Disorders PDFdreamingОценок пока нет
- Specific Phobia in Adults - Epidemiology, Clinical Manifestations, Course and Diagnosis PDFДокумент10 страницSpecific Phobia in Adults - Epidemiology, Clinical Manifestations, Course and Diagnosis PDFdreamingОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Effective Home Remedies With HerbsДокумент23 страницыEffective Home Remedies With HerbsAlexandru Vasile100% (1)
- The Teacher's Guide ToДокумент90 страницThe Teacher's Guide ToKellyn KlapaskaОценок пока нет
- CyclophosphamideДокумент3 страницыCyclophosphamideChen Boon TeyОценок пока нет
- Teva PharmaceuticalДокумент17 страницTeva PharmaceuticalGanesh VedhachalamОценок пока нет
- Syringe Pump ReportДокумент6 страницSyringe Pump ReportzulayieОценок пока нет
- Utility Validations - Review: Hvac Explain HVAC QualificationДокумент64 страницыUtility Validations - Review: Hvac Explain HVAC Qualifications lavanya100% (1)
- 6-Gingerol ArecolineДокумент8 страниц6-Gingerol Arecolineapi-327826901Оценок пока нет
- Various Drugs Used in Paediatric DentistryДокумент56 страницVarious Drugs Used in Paediatric DentistryPo PowОценок пока нет
- Quality Assurance,: A Systemic Approach For Effective ComplianceДокумент73 страницыQuality Assurance,: A Systemic Approach For Effective ComplianceHemanth PanasaОценок пока нет
- Royal Surgical April 2018 Outward Sales ReportДокумент6 страницRoyal Surgical April 2018 Outward Sales ReportManoj SharmaОценок пока нет
- Dissolution Testing of Poorly Soluble Compoundsolution TestingДокумент7 страницDissolution Testing of Poorly Soluble Compoundsolution TestingArranee ChotikoОценок пока нет
- Communication and Ethics in Pharmacy Practice: What Is To BeДокумент23 страницыCommunication and Ethics in Pharmacy Practice: What Is To BeMuhammad RezaОценок пока нет
- Brochure IIPRD 2012Документ6 страницBrochure IIPRD 2012satyadev_IIPRDОценок пока нет
- Zambia Health Shop GuidelinesДокумент18 страницZambia Health Shop Guidelinesdavies100% (1)
- Patient Medication Adherence PDFДокумент5 страницPatient Medication Adherence PDFAlexandrahautaОценок пока нет
- Poster PresentationДокумент1 страницаPoster PresentationsjОценок пока нет
- Puente PiedraДокумент6 страницPuente PiedraBotica Super FarmaОценок пока нет
- EtosuksimidДокумент14 страницEtosuksimidMaharani IndriatyОценок пока нет
- Receptors and PharmacodynamicsДокумент78 страницReceptors and PharmacodynamicsMuhammad Bilal Bin Amir100% (1)
- ECA Biological Raw Materials ExcipientsДокумент6 страницECA Biological Raw Materials ExcipientsBiopharma GuruОценок пока нет
- The High Cost of Prescription Drugs CausesДокумент5 страницThe High Cost of Prescription Drugs Causesjuddy avottОценок пока нет
- Hyoscine ButylbromideДокумент2 страницыHyoscine ButylbromideKepslock StahpОценок пока нет
- Group MembersДокумент28 страницGroup MembersBlackjack100% (1)
- Kiran Mazumdar ShawДокумент11 страницKiran Mazumdar ShawraghavmehraОценок пока нет
- Document (12) 1Документ7 страницDocument (12) 1Fazal JalalОценок пока нет
- PCP Regulations For Pharm.D ProgramДокумент21 страницаPCP Regulations For Pharm.D ProgramAdil YousafОценок пока нет
- DIS IPD Ceftriaxone KonsulДокумент28 страницDIS IPD Ceftriaxone KonsulTriana MaulidyahОценок пока нет
- Drug Alert For The Month of December 2016Документ3 страницыDrug Alert For The Month of December 2016amit545Оценок пока нет
- APEC Product Security Supply Chain Management SystemДокумент32 страницыAPEC Product Security Supply Chain Management SystemRenzo FernandezОценок пока нет
- Role of Echinocandins in Invasive Fungal InfectionsДокумент63 страницыRole of Echinocandins in Invasive Fungal Infectionsbanteng wibisonoОценок пока нет