Академический Документы
Профессиональный Документы
Культура Документы
Pelvic 11
Загружено:
ticponyАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pelvic 11
Загружено:
ticponyАвторское право:
Доступные форматы
CLINICAL OBSTETRICS AND GYNECOLOGY Volume 52, Number 2, 250255 r 2009, Lippincott Williams & Wilkins
Obstetric Ultrasonography in Low-income Countries
JOSEPH D. SEFFAH, MD and RICHARD M. K. ADANU, MD Department of Obstetrics and Gynaecology, University of Ghana Medical School, Accra, Ghana
Abstract: The major issues in obstetric practice in developing countries are the high rates of maternal and perinatal mortality. In most low-income countries health financing systems are not well established so most people pay for health services at the service delivery points. This causes cost-related issues to be of major concern. The main questions that therefore need to be addressed about obstetric ultrasonography in low-income countries is whether the practice improves maternal and neonatal outcomes and whether the service is within the means of most people in these countries. The indications for obstetric ultrasound, guidelines for the use of obstetric ultrasound and the benefits of obstetric ultrasound in low-income countries are discussed and the future of obstetric ultrasound in developing countries is also briefly considered. Key words: obstetric ultrasonography, low income countries, perinatal mortality
Introduction
Ultrasonography has become established as an essential part of modern obstetric practice. Obstetric ultrasound has been in
Correspondence: Joseph D. Seffah, MD, Department of Obstetrics and Gynaecology, University of Ghana Medical School, PO Box 4236, Accra, Ghana. E-mail: jseffah@yahoo.co.uk
CLINICAL OBSTETRICS AND GYNECOLOGY /
use for almost 40 years and there has been no documented adverse effect on the mother or fetus.1 Equipment used in ultrasound examinations have evolved from static machines through real time 2 dimensional (2D) machines until we now have 3 dimensional and 4 dimensional (4D) machines. Although not all modern ultrasound machines are available in all low-income countries, there are reports from countries where 3 dimensional and 4D machines are available.2 The major issues in obstetric practice in developing countries are the high rates of maternal and perinatal mortality. In most low-income countries health financing systems are not well established so most people pay for health services at the service delivery points. This causes costrelated issues to be of major concern. The main questions that need to be addressed about obstetric ultrasonography in lowincome countries is whether the practice improves maternal and neonatal outcomes and whether the service is within the means of most people in these countries.
VOLUME 52 / NUMBER 2 / JUNE 2009
250 | www.clinicalobgyn.com
Obstetric Ultrasonography in Low-income Countries
251
Obstetric ultrasound services in low-income countries are generally provided by obstetricians, radiologists, and general duty medical officers. Owing to the shortage of specialists there have been program in developing countries that are aimed at training general duty medical officers in obstetric ultrasonography.3 These training program are usually short courses and are combined with the provision of ultrasound machines in district and regional hospitals.3 Training and certification may not be as adequate, standardized and rigorous as obtained in developed countries. Ultrasound services are provided in both public and private facilities. Most of the ultrasonographers in low-income countries perform basic ultrasound surveys. This involves routine scanning for pregnancy dating, fetal life, and placental location.1 Skill for targeted scanning which are scans by experts in maternal and perinatal sciences aimed at detecting anomalies1 is not very common. The absence of training program for maternalfetal medicine as a subspecialty in many developing countries is probably a major contributor to this situation. There has not been much research into obstetric sonography in developing countries and this could be due to lack of funding and motivation. Customized growth charts are often not available and the program and software may depend on the American, European or Japanese values depending on where the machine was purchased. There have been some uncoordinated attempts to derive some growth curves but these are limited to small localities and are not national or regional in outlook. The health care delivery in developing countries also faces a lot of challenges including the frequent power outages that have tremendous impact on the life span of the machines.
Obstetric Ultrasound Service in Low-income Countries
Indications for Obstetric Ultrasound
Obstetric ultrasound examination is used in the following conditions:
DATING OF PREGNANCY
In cases where there is uncertainty about the date of the last menstrual period, an ultrasound examination is used to date the pregnancy. It has been shown that the date provided by ultrasound examination is more reliable when there is a discrepancy with the gestational age calculated from the last menstrual period.4,5 The first trimester ultrasonography enables a pregnancy to be confirmed and dating provided to a high degree of accuracy. In about 30% of women the last menstrual period is unknown or unreliable because of such factors as irregular menstrual cycles or the administration of oral contraceptive pill that interferes with the cycles. With the use of the transvaginal scan, the gestational sac is seen after 4 completed weeks, the yolk sac after 5 weeks, fetal pole with cardiac activity after 6 weeks, and a fetal pole with a separate amniotic sac and coelomic cavity with yolk sac after 7 weeks.6 In early pregnancy, chorionic villus sampling may be performed in advanced centers when a prenatal diagnosis for genetic disorder is indicated, but this facility is not available in many low-income countries. In the first 12 days the crown-rump length can be used and that gives an error of 3 to 5 days. In the second trimester the biparietal diameter, femur length, and abdominal circumference measurements could be carried out and the error is about 2 weeks. In the third trimester the error is about 3 weeks. In difficult cases the intercerebellar diameter can be useful as a reliable parameter.6 Early ultrasound examination alone for dating the pregnancy has been shown to be reliable. Using this method alone is www.clinicalobgyn.com
252
Seffah and Adanu second trimester.12 Thus it is helpful in cases where there are major malformations so that decisions can be taken about termination of pregnancy.
known to reduce the prevalence of prolonged pregnancies from 10% to 1.5%.7
DIAGNOSIS OF ECTOPIC PREGNANCY
The efficacy of using the ultrasound scan to diagnose unruptured ectopic pregnancy (EP) has been documented.8 The appearance of EP on transvaginal scan is variable. There may be a hyperechoic ring around the gestational sac in the adnexa or a small heterogeneous mass next to the ovary or any noncystic adnexal mass. This has been reported to have a positive predictive value of 96.3%, specificity of 98.9%, and sensitivity of 84.4%.9 Medical management of EP with methotrexate is about 71% to 100% successful and the success depends on the initial serum human chorionic gonadotropin levels.10 The laparoscopic approach has been shown to be better than laparotomy in the management of EP. The laparoscopic approach is associated with less hemorrhage and pain, and reduced hospital stay, and shorter recovery time.11 However in low-income countries where majority of EP is diagnosed after the tube has ruptured laparotomy is the norm in these patients who may be hemodynamically unstable. Here, ultrasound finding of fluid in the pouch of Douglas lends support to the diagnosis of ruptured EP. The level of effectiveness of the use of sonography in diagnosing EP might depend on the methodology used (transvaginal or transabdominal) in a particular center (Table 1) and the skill and knowledge of the sonographer.
CONGENITAL MALFORMATIONS
DIAGNOSIS OF MULTIPLE PREGNANCY
Ultrasound is more accurate than symphysio-fundal height measurement and palpation in determining the presence of multiple pregnancy. Ultrasound examinations also lead to knowledge about the chorionicity in cases of multiple pregnancy.
BLEEDING IN PREGNANCY
Vaginal bleeding at any stage of pregnancy requires an ultrasound examination. Obstetric ultrasound is helpful in differentiating between the different types of miscarriages and also in the diagnosis of placenta praevia.
FETAL PRESENTATION
Obstetric ultrasound late in the third trimester can be used to confirm the presentation of the fetus and thereby help in making decisions about the planned mode of delivery.
MONITORING OF FETAL GROWTH
Obstetric ultrasound performed in the latter part of the first trimester or early in the second trimester is able to detect fetal malformations. A recent publication from China has shown that it is possible there to diagnose some central nervous system or neck abnormalities in the first trimester and cardiac anomalies in the www.clinicalobgyn.com
When clinical examination shows a discrepancy between uterine size and dates, ultrasound examination could reveal the cause of the discrepancy. Ultrasound examination will reveal the presence of polyhydramnios, pelvic tumours or anything else that makes the uterus larger than expected. Fetal size can also be monitored through serial ultrasound scanning in cases of intrauterine growth restriction and the fetal weight can be estimated in cases where the fetus is thought to be bigger than expected. The use of fetal weight estimation by ultrasound is helpful also in planning for the delivery of women with a previous caesarean section.13
Obstetric Ultrasonography in Low-income Countries
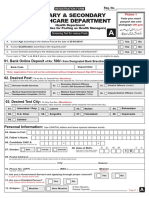
TABLE 1.
Author TIMOR-T NYBERG BROWN ILOABACHIE PICAUD
253
Effectiveness of Using Ultrasonography for the Diagnosis of Ectopic Pregnancy
Year 1989 1991 1991 1990 Country USA USA Nigeria Gabon Sensitivity 100 94 84.4 71 98 Specificity 98 50 98.9 81 97 Positive Predictive Value 99 46 96.3 83 84 Negative Predictive Value 100 97 94.8 65 98
INTRAUTERINE FETAL DEMISE
Obstetric ultrasound is the best way of confirming intrauterine fetal demise. Making such a diagnosis based simply on the absence of fetal movements or the absence of fetal heart tones is not acceptable in modern obstetric practice.
Routine Obstetric Ultrasound Scanning
Routine ultrasound scanning has been defined as obstetric ultrasound scanning performed in the absence of any clinical condition that indicates the need for ultrasound scanning.7,14,15 Routine ultrasound scanning could be either early (before 24 wk gestation) or late (after 24 wk).7,15 A meta-analysis of early routine ultrasound scanning showed that although the practice did not improve maternal or perinatal outcomes, it provided better dating of pregnancies with fewer inductions for postdate pregnancies.7 Studies on routine ultrasound scanning in low income16,17 have provided the same results and have also raised questions about the cost of such a service. Routine late ultrasound scanning has however not been shown to be of any benefit when it is used.15 Routine early scanning is associated with greater detection of multiple pregnancy [twins undiagnosed at 26 wk, odds ratio (OR); 0.08; 95% confidence interval (CI) 0.04-0.16].7 It also reduces the induction of labor for postterm pregnancy (OR; 0.61, 95% CI 0.320.72).7
However there were no differences in perinatal outcomes such as perinatal mortality (OR; 0.86: 95% CI 0.67-1.12) and in situations where the screening was to determine fetal anomaly this resulted in more terminations of pregnancy.7 The practice is fast becoming established in obstetric practice in low-income countries and there is need for research into effectiveness, overuse, and abuse.
Frequency of Ultrasound Scanning in Pregnancy
There is still no universally accepted schedule for ultrasound scanning in pregnancy. Whereas some authorities recommend at least 4 ultrasound scans in an uncomplicated pregnancy, others recommend a single ultrasound scan between 20 and 24 weeks gestation.1 The schedule when 4 ultrasound scans are performed is to perform the first scan between 10 and 14 weeks to document fetal life, date the pregnancy, and for possible detection of anomalies.1 The second scan between 18 and 22 weeks is for a complete anomaly scan and confirmation of dating.1 The third scan between 30 and 34 weeks is to assess fetal growth whereas the fourth between 36 and 38 weeks focuses on fetal weight and position to aid decision on the optimal mode of delivery.1 Studies have not shown the superiority of either of these scanning schedules. Reports from Vietnam2 show a trend, which the authors describe as comodification of obstetric ultrasound. In this report some women had more than 10 ultrasound examinations in normal pregnancies. www.clinicalobgyn.com
254
Seffah and Adanu ing the practice of potentially dangerous procedures such as the double set up examination in diagnosing placenta praevia.
Cost of Ultrasound Services
The only paper that addresses the issue of cost of ultrasound scanning in low-income countries reports the cost to be US$1.30 for a 2D scan and about US$20 for a 4D scan.2 This reported cost of the 2D scan is similar to the cost in some West African countries. The corresponding cost of a 2D obstetric ultrasound scan in developed countries is US$200. Developing countries can afford to provide ultrasound services at such apparently low prices for several reasons. One reason is the large number of pregnant women so that service providers are still able to make a profit. Another reason is the low level of remuneration for service providers in developing countries results in such charges having a very small labor component. Also very few people could afford to pay the price charged for the service in developed countries.
Benefits of Obstetric Ultrasonography in Developing Countries
Although the use of obstetric ultrasound does not result in reduction of maternal mortality or perinatal mortality, the service is still useful for low-income countries. The use of routine early obstetric ultrasound in developing countries has showed a significant reduction in the referral of women to tertiary centers.16 Accurate dating of pregnancies and the ability to monitor fetal growth also prevents premature clinical intervention in the progress of the pregnancy. Ultrasound scanning helps in diagnosing fetal anomalies and therefore enables the obstetrician to take the decision to terminate a pregnancy.18 The diagnosis of postdatism is made more accurate and therefore the rate of induction of labor is reduced.18 The diagnosis of the cause of antepartum hemorrhage also reduces the amount of unnecessary time spent by women on admission in addition to preventwww.clinicalobgyn.com
The report from Vietnam2 shows the danger of abuse and overuse of ultrasound scanning in developing countries. In many developing countries private ultrasound scanning services are provided by obstetricians and other nonobstetricians who provide antenatal services. The danger in such cases is that requests, which are not clinically indicated, might be made to ensure extra income for such service providers. The presence of private ultrasound facilities couple with the fact that people pay for services out of pocket means that women can perform self referrals for ultrasound examinations for as many times as they can afford leading to overuse of the service. Chigbu et al19 working in Nigeria have shown the serious social and psychologic implications in the wrong assignment of fetal sex. This abuse calls for strict guidelines for sonographers practicing in developing countries.
Dangers of Obstetric Ultrasound Scanning in Developing Countries
Applications for Low-income Countries
Women receiving antenatal care should have a routine early ultrasound examination performed between 20 and 24 weeks. This examination will be able to accurately date the pregnancy, diagnose congenital malformations, and multiple pregnancy and also to localize the placenta. Subsequent ultrasound examination should be based on clinical indications. In places where ultrasound machines are not available, practitioners can still manage women adequately by using clinical examinations and referring women for ultrasound examination only when a clinical indication arises.
Obstetric Ultrasonography in Low-income Countries
255
Future Direction for Obstetric Ultrasonography in Low-income Countries
Obstetric ultrasonography has developed into a specialized field. The future development of this field in developing countries will depend on the establishment of local training programs in maternal-fetal medicine and the establishment of centers where the skill for levels 2 and 3 scanning is available. This would also lead to increase in ultrasound-guided procedures such as amniocentesis and chorionic villus sampling.
References
1. Papp Z, Fekete T. The evolving role of ultrasound in obstetrics/gynecology practice. Int J Gynaecol Obstet. 2003;82: 339346. 2. Gammeltoft T, Nguyen HT. The commodification of obstetric ultrasound scanning in Hanoi, Viet Nam. Reprod Health Matters. 2007;15:163171. 3. Jumah KB, Brakohiapa MO, Obajimi JO, et al. Training of non radiologist medical doctors in ultrasound in Ghana. Ghana Med J. 2001;35:6668. 4. Dietz PM, England LJ, Callaghan WM, et al. A comparison of LMP-based and ultrasound-based estimates of gestational age using linked California livebirth and prenatal screening records. Paediatr Perinat Epidemiol. 2007; 21(suppl 2):6271. 5. Thorsell M, Kaijser M, Almstrom H, et al. Expected day of delivery from ultrasound dating versus last menstrual periodbstetric outcome when dates mismatch. BJOG. 2008;115:585589. 6. Warren WB, Timot-Tritsch I, Peisner DB, et al. Dating the early pregnancy by sequential appearance of embryonic structures. Am J Obstet Gynecol. 1989; 161:831833. 7. Neilson JP. Ultrasound for Fetal Assessment in Early Pregnancy. The Cochrane Library, Issue 1. Chichester: John Wiley & Sons Ltd; 2006.
8. Seffah JD. Ultrasonography and ectopic pregnancy-a review. Int J Gynaecol Obstet. 2000;71:263264. 9. Brown DL, Doubilet PM. Transvaginal sonography for the diagnosis of ectopic pregnancy: positivity criteria and performance characteristics. J Ultrasound Med. 1994;13:259266. 10. Parker J, Bists A, Droietto AM. A systematic review of single dose intramuscular methotrexate for the treatment of ectopic pregnancy. Aust N Z J Obstet Gynaecol. 1998;38:145150. 11. Mol BW, Hajenius PJ, Engelsbel S, et al. An economic evaluation of laparoscopy and open surgery in the treatment of tubal pregnancy. Acta Obstet Gynecol Scand. 1997;76:596600. 12. Qiuming L, Buyun G, Dongzhi L. Detection of fetal structural abnormalities by early pregnancy ultrasound in China. Int J Gynaecol Obstet. 2007;100:277278. 13. Adanu RM, McCarthy MY. Vaginal birth after cesarean delivery in the West African setting. Int J Gynaecol Obstet. 2007;98:227231. 14. Skupski DW, Chervenak FA, McCullough LB. Routine obstetric ultrasound. Int J Gynaecol Obstet. 1995;50:233242. 15. Bricker L, Nielson JP. Routine Ultrasound in Late Pregnancy (After 24 Weeks Gestation). Cochrane Database of Systemic Reviews. Chichester: John Wiley & Sons; 2000. 16. Geerts L, Theron AM, Grove D, et al. A community-based obstetric ultrasound service. Int J Gynaecol Obstet. 2004;84: 2331. 17. Geerts LT, Brand EJ, Theron GB. Routine obstetric ultrasound examinations in South Africa: cost and effect on perinatal outcomea prospective randomised controlled trial. Br J Obstet Gynaecol. 1996;103:501507. 18. van Dyk B, Motto JA, Buchmann EJ. Routine second-trimester ultrasound for low risk pregnancies in a South African community. Int J Gynaecol Obstet. 2007; 98:257258. 19. Chigbu CO, Odugu B, Okezie O. Implications of incorrect determination of fetal sex by ultrasound. Int J Gynaecol Obstet. 2008;100:287290.
www.clinicalobgyn.com
Вам также может понравиться
- Air To Fluid RatioДокумент1 страницаAir To Fluid RatioticponyОценок пока нет
- PriSecHth FormAДокумент4 страницыPriSecHth FormAticponyОценок пока нет
- Ahmad Faraz Khan: ObjectiveДокумент2 страницыAhmad Faraz Khan: ObjectiveticponyОценок пока нет
- Matlab Lab ManualДокумент22 страницыMatlab Lab Manualticpony0% (1)
- Contact Us For All Medical Dvds - 03323959833: (List of Available Dvds at The End!)Документ25 страницContact Us For All Medical Dvds - 03323959833: (List of Available Dvds at The End!)ticponyОценок пока нет
- DR Nazim HussainДокумент5 страницDR Nazim HussainticponyОценок пока нет
- 1st TrimesterДокумент1 страница1st TrimesterticponyОценок пока нет
- 32 Critical UltrasoundДокумент1 страница32 Critical UltrasoundticponyОценок пока нет
- Under Estimation of Crown Ramp LenghДокумент1 страницаUnder Estimation of Crown Ramp LenghticponyОценок пока нет
- Fetal MeasurementДокумент1 страницаFetal MeasurementticponyОценок пока нет
- Cranium Is Absent Above The Orbit With Anencephaly As Seen in Above ImageДокумент1 страницаCranium Is Absent Above The Orbit With Anencephaly As Seen in Above ImageticponyОценок пока нет
- Routine Obstetric Sonography: Roy A. Filly, MDДокумент6 страницRoutine Obstetric Sonography: Roy A. Filly, MDticponyОценок пока нет
- Grstational AgeДокумент1 страницаGrstational AgeticponyОценок пока нет
- Abnormal A TiesДокумент1 страницаAbnormal A TiesticponyОценок пока нет
- Longitudinal ProbeДокумент1 страницаLongitudinal ProbeticponyОценок пока нет
- MachineДокумент1 страницаMachineticponyОценок пока нет
- First BasicДокумент1 страницаFirst BasicticponyОценок пока нет
- GainsДокумент1 страницаGainsticponyОценок пока нет
- Solid MassДокумент1 страницаSolid MassticponyОценок пока нет
- ArtifactДокумент1 страницаArtifactticponyОценок пока нет
- Chest RadiographДокумент1 страницаChest RadiographticponyОценок пока нет
- 1 Basic Notions of Critical UltrasoundДокумент1 страница1 Basic Notions of Critical UltrasoundticponyОценок пока нет
- Axial ScanДокумент1 страницаAxial ScanticponyОценок пока нет
- InterpretДокумент1 страницаInterpretticponyОценок пока нет
- Anterior Abdominal Wall Defects: Figures 22.1A and B: (A) Coronal View On The LipsДокумент1 страницаAnterior Abdominal Wall Defects: Figures 22.1A and B: (A) Coronal View On The LipsticponyОценок пока нет
- Fetal Anomaly Scan (FAS) at 20 To 24 WeeksДокумент1 страницаFetal Anomaly Scan (FAS) at 20 To 24 Weeksticpony100% (1)
- U T U P: Nderstanding and Eaching Ltrasound HysicsДокумент8 страницU T U P: Nderstanding and Eaching Ltrasound HysicsticponyОценок пока нет
- Routine Obstetric Sonography: Roy A. Filly, MDДокумент6 страницRoutine Obstetric Sonography: Roy A. Filly, MDticponyОценок пока нет
- Routine Obstetric Sonography: Roy A. Filly, MDДокумент6 страницRoutine Obstetric Sonography: Roy A. Filly, MDticponyОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- CP 101Документ4 страницыCP 101Jon EricОценок пока нет
- Maternal and Child Health Nursing 1Документ20 страницMaternal and Child Health Nursing 1Khibul Lim100% (1)
- NB 2 MDG UpdatesДокумент4 страницыNB 2 MDG UpdatesAliah DoroОценок пока нет
- Mortality and Morbidity CHNДокумент19 страницMortality and Morbidity CHNPamela Ria HensonОценок пока нет
- PURBANCHAL UNIVERSITY - ReportДокумент29 страницPURBANCHAL UNIVERSITY - ReportAsh-i ShОценок пока нет
- Cervical Incompetence: Risk FactorsДокумент40 страницCervical Incompetence: Risk FactorsAriaPratamaОценок пока нет
- Common Obstetrics Case ScenariosДокумент10 страницCommon Obstetrics Case ScenariosPeter LeeОценок пока нет
- FHSIS Report Forms A1 M1 Q1 All ProgramsДокумент70 страницFHSIS Report Forms A1 M1 Q1 All ProgramsmynameissaiОценок пока нет
- Gauss Without AnswersДокумент115 страницGauss Without AnswersAshish R. JadhavОценок пока нет
- Exceptional Fetal Malformation Acardiac Headless TwinДокумент2 страницыExceptional Fetal Malformation Acardiac Headless TwinInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Leasson 4Документ11 страницLeasson 4DARLYN DAYANA GARCIA VASQUEZОценок пока нет
- A Prospective Randomized Study Comparing Two Commercially Available Types of Human Embryo Culture Media: G1-PLUS / G2-Plus Sequential Medium (Vitrolife) and The GL BLAST Sole Medium (Ingamed)Документ4 страницыA Prospective Randomized Study Comparing Two Commercially Available Types of Human Embryo Culture Media: G1-PLUS / G2-Plus Sequential Medium (Vitrolife) and The GL BLAST Sole Medium (Ingamed)meltwithsnow163.comОценок пока нет
- 2 PolyhydramniosДокумент8 страниц2 PolyhydramniosNovhy GanggutОценок пока нет
- Latent: From Onset of Uterine Contraction To Rapid Cervical Dilation. Contractions Are Mild and ShortДокумент18 страницLatent: From Onset of Uterine Contraction To Rapid Cervical Dilation. Contractions Are Mild and Shortlushxene84Оценок пока нет
- For PrintДокумент17 страницFor Printexample mailОценок пока нет
- Antenatal Examination According To WHOДокумент6 страницAntenatal Examination According To WHOManisha ThakurОценок пока нет
- Case Simulatio 115Документ6 страницCase Simulatio 115Dudong SasakiОценок пока нет
- Kode Icd ObgynДокумент4 страницыKode Icd ObgyndodiaryawanОценок пока нет
- HY ObgynДокумент52 страницыHY ObgynteapalmtreeОценок пока нет
- Tugas SC Vs Histerotomi Vs Laparotomi Ambil Anak Aji PatriajatiДокумент3 страницыTugas SC Vs Histerotomi Vs Laparotomi Ambil Anak Aji PatriajatiAji PatriajatiОценок пока нет
- Preeklampsia BeratДокумент5 страницPreeklampsia BeratmelatiigdОценок пока нет
- Thesis Hawa Last PDFДокумент58 страницThesis Hawa Last PDFMohamed AbdiОценок пока нет
- Safe Motherhood: Reproductive Health I Clinical Medicine ClassДокумент32 страницыSafe Motherhood: Reproductive Health I Clinical Medicine Classmoreen kipkemoiОценок пока нет
- Obstetrical EmergencyДокумент41 страницаObstetrical EmergencyDrPreeti Thakur ChouhanОценок пока нет
- 1a. Obstetric Emergencies Koros E.KДокумент225 страниц1a. Obstetric Emergencies Koros E.KSalman KhanОценок пока нет
- NCP Shoulder DystociaДокумент4 страницыNCP Shoulder DystociaTrishia CaroОценок пока нет
- Abortion KuliahДокумент38 страницAbortion KuliahElsa Hasibuan100% (1)
- The Structured Approach To Obstetric EmergenciesДокумент7 страницThe Structured Approach To Obstetric Emergencies'محمد علي' محمد لافيОценок пока нет
- Major Discourses With Their FormatДокумент16 страницMajor Discourses With Their FormatAthulОценок пока нет
- OBGYN 2022 + FM 122 PagesДокумент122 страницыOBGYN 2022 + FM 122 PagesDr. zesty anatomistОценок пока нет