Академический Документы
Профессиональный Документы
Культура Документы
5405 CR 4
Загружено:
Narendra BhattaraiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
5405 CR 4
Загружено:
Narendra BhattaraiАвторское право:
Доступные форматы
C ase R eport
Singapore Med J 2013; 54(5): e105-e107 doi: 10.11622/smedj.2013066
Plasmacytoma of the pancreas: an unusual manifestation of multiple myeloma
Susan Swee Shan Hue1,
MBBS, PhD,
Rafay Azhar1,
MBBS, FRCPath
ABSTRACT Extramedullary plasmacytoma of the pancreas is a rare entity. Although this condition is uncommon, it
should be considered in the differential diagnosis of solid mass in the pancreas, especially in patients with underlying multiple myeloma. We report a case of pancreatic plasmacytoma in a 56-year-old woman with newly diagnosed multiple myeloma. We highlight this rare manifestation of multiple myeloma among other better recognised presentations.
Keywords: multiple myeloma, pancreatic tumour, plasmacytoma
I NTRO D U C TIO N
An entity in the spectrum of plasma cell neoplasms, extramedullary plasmacytoma is characterised by localised monoclonal plasma cell proliferation that forms a solitary lesion outside the bone marrow. The disease can occur as a manifestation of advanced multiple myeloma with extramedullary involvement, or as a true solitary plasma cell tumour without any bone marrow plasmacytosis.(1-3) We describe a rare case of pancreatic plasmacytoma diagnosed in a patient with newly discovered multiple myeloma.
1a
Pancreatic parenchyma
Tumour
CA S E R E P O R T
A 56 -year- old Chinese woman presented with right hypochondriac pain and unquantified weight loss over a period of one month. Her past medical history included diabetes mellitus and psoriasis. Radiologic evaluation revealed the presence of a solid mass measuring 3 cm in the midbody of the pancreas, which was suspicious for either a primary neuroendocrine tumour or pancreatic metastasis. An infiltrative, lytic, lower thoracic T9 vertebral lesion involving the right pedicle was noted, which was also thought to be metastatic. Serum cancer antigen 19-9 and chromogranin A were both within their respective normal limits. Biopsy of the vertebral bone lesion revealed the presence of a plasma cell myeloma, which corresponded with subsequent serological detection of monoclonal immunoglobulin (M protein). Haematological opinion was sought and the clinical impression was that the pancreatic mass was unlikely to be related to multiple myeloma. Fine needle aspiration of the pancreatic mass was then attempted on two separate occasions, which unfortunately did not yield any diagnostic material for evaluation. The pancreatic mass was subsequently excised for histological examination. Macroscopically, the specimen consisted of distal pancreas and spleen. There was a well-circumscribed, solid mass in the body of the pancreas measuring 5 cm 3.5 cm 3.5 cm. It had a homogeneous, tan-pink, firm-to-rubbery cut surface devoid of haemorrhage or necrosis. The patients spleen was not involved.
1
1b
Fig. 1 Photomicrographs show (a) par tial replacement of pancreatic parenchyma by an inf iltr ate of tumour cells (H aematox ylin & eosin, 2 . 5); a n d ( b) d i s c o h e s i v e p l a s m a c y t o i d c e l l s w i t h b a s o p h i l i c cy toplasm, eccentric nuclei and coarsely clumped chromatin (Haematoxylin & eosin, 20 0).
Histology showed sheet-like proliferation of predominantly immature plasma cells, with scattered mature plasma cells in the background (Fig. 1). On immunohistochemistry, the neoplastic cells were positive for CD138 (Fig. 2a), but negative for pan-cytokeratin marker, MNF116 (Fig. 2b). In situ hybridisation studies also demonstrated lambda light chain monotypia (Figs. 2c & d). A diagnosis of plasmacytoma of the pancreas was thus rendered.
Histopathology Department, Singapore General Hospital, Singapore
Correspondence : Dr Rafay Azhar, Consultant Pathologist, Histopathology Department, Singapore General Hospital, Outram Road, Singapore 169608. rafazhar@gmail.com
e105
C ase R eport
2a
2b
2c
2d
Fig. 2 Photomicrographs show tumour cells demonstrating (a) uniform and strong positivity for plasma cell marker CD138, in keeping with the diagnosis of myeloma; and (b) negative staining for pan-cytokeratin marker, MNF116. The monoclonal nature of the myeloma neoplasm is demonstrated by staining with (c) lambda and (d) kappa light chains (All immunoperoxidase stain, 2.5).
D I SCU S S IO N
Plasma cell neoplasms and other related immunosecretory disorders are clonal proliferations of immunoglobulin-secreting, heavy chain class-switched, terminally differentiated B cells. These typically secrete a single homogenous immunoglobulin usually detectable as M protein on serum or urine protein electrophoresis.(1) True plasma cell neoplasm includes multiple myeloma (also known as plasma cell myeloma), plasmacytoma and immunoglobulin deposition diseases, among others (Table I). Multiple myeloma is a bone marrow-based, multifocal plasma cell neoplasm associated with M protein in serum or urine.(1) In most cases of multiple myeloma, there is disseminated marrow involvement (diffuse myelomatosis), although the disease can also present as solitary myeloma of the bone or involve other organs secondarily in the form of extramedullary plasmacytoma.(1-3) The diagnosis of myeloma is made by a combination of clinical, morphologic, immunologic and radiographic information. The disease comprises 10%15% of haematologic malignancies and clinically ranges from asymptomatic to highly aggressive disease.(1) A plasmacytoma is a discrete but often solitary mass of neoplastic plasma cells that may occupy extramedullary sites.(4) However, primary extramedullary plasmacytomas are uncommon and account for about 5% of all plasma cell neoplasms.(3-5) They are commonly identified after the diagnosis of multiple myeloma, typically as a form of secondary involvement of extraskeletal organs. Rarely, there may be no evidence of bone marrow involvement (i.e. primary extramedullary plasmacytoma).(3) Although most commonly found in the upper respiratory tract, extramedullary plasmacytoma also occurs in the gastrointestinal
Table I. World Health Organizations classication of plasma cell neoplasms, adapted from McKenna et al.(1)
Types of plasma cell neoplasms Monoclonal gammopathy of undetermined signicance Multiple myeloma Subtypes Asymptomatic (smouldering) myeloma Nonsecretory myeloma Plasma cell leukaemia Solitary bone plasmacytoma Extraosseous (extramedullary) plasmacytoma Primary amyloidosis Systemic light and heavy chain deposition diseases
Plasmacytoma
Immunoglobulin deposition diseases Osteosclerotic myeloma (POEMS syndrome)
and genitourinary tracts, lungs, lymph nodes, skin and other locations.(6,7) Reports of extramedullary plasmacytoma affecting the pancreas are sparse, and to date, to the best of our knowledge, just over 20 cases of pancreatic plasmacytoma have been reported in the literature.(2,8-11) Most of these cases are associated with patients with underlying multiple myeloma. In our patient, the diagnosis of multiple myeloma was made before the diagnosis of plasmacytoma of the pancreas. Typical presentation of extramedullary plasmacytoma of the pancreas includes jaundice and abdominal pain, which are often related to obstruction of the biliary tree. Described as either a focal, multilobular, solid mass with homogeneous intravenous contrast enhancement on computed tomography (CT), or a heterogeneous focal mass (hypoechoic relative to normal
e106
C ase R eport
parenchyma) on ultrasonography, radiologic features ofextramedullary plasmacytoma are nonspecific.(12) These nonspecific features commonly resemble typical findings in other pancreatic neoplasms, including neuroendocrine tumours, carcinoma, lymphoma and metastases. Although diagnosis is usually made by CT-guided percutaneous fine needle aspiration (FNA) biopsy,(13) two attempts at FNA biopsy proved futile in obtaining diagnostic material in our case. In conclusion, pancreatic plasmacytoma should be considered in the differential diagnosis of a patient with multiple myeloma and a pancreatic mass. A correct diagnosis obviates unnecessary surgery, as surgical procedures (other than distal pancreatectomy necessary for isolated pancreatic tail involvement) are not commonly performed due to the often systemic nature of the disease and its good response to local radiotherapy.
R E FE R E N C E S
1. McKenna RW, Kyle RA, Kuehl WM, et al. Plasma cell neoplasms. In: Swerdlow SH, Campo E, Harris NL, et al, eds. WHO Classifications of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed. Lyon: IARC, 2008: 200-13. 2. Leake PA, Coard KC, Plummer JM. Extramedullary plasmacytoma of the
pancreas as an uncommon cause of obstructive jaundice: a case report. J Med Case Rep 2009; 3:8785. 3. Kremer M, Ott G, Nathrath M, et al. Primary extramedullary plasmacytoma and multiple myeloma: phenotypic differences revealed by immunohistochemical analysis. J Pathol 2005; 205:92-101. 4. Nolan KD, Mone MC, Nelson EW. Plasma cell neoplasms: Review of disease progression and report of a new variant. Surg Oncol 2005; 14:85-90. 5. Hirata S, Yamaguchi K, Bandai S, et al. Secondary extramedullary plasmacytoma involving the pancreas. J Hepatobiliary Pancreat Surg 2002; 9:111-15. 6. C, Kau RJ, Dietzfelbinger H, et al. Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer 1999; 85:2305-14. 7. Corwin J, Lindberg R. Solitary plasmacytoma of bone vs. extramedullary plasmacytoma and their relationship to multiple myeloma. Cancer 1979; 43:1007-13. 8. Wilson TE, Korobkin M, Francis IR. Pancreatic plasmacytoma: CT findings. AJR Am J Roentgenol 1989; 152:1227-8. 9. Fischer A, Suhrland MJ, Vogl SE. Myeloma of the head of the pancreas. A case report. Cancer 1991; 67:681-3. 10. Olson MC, Kalbhen CL, Posniak HV. Pancreatic plasmacytoma in a patient with multiple myeloma: CT and ultrasound findings. Abdom Imaging 1993; 18:323-4. 11. Hiller N, Goitein O, Ashkenazi YJ. Plasmacytoma of the pancreas. Isr Med Assoc J 2004; 6:704-5. 12. Balliu E, Casas JD, Barluenga E, Guasch I. Multifocal involvement of the pancreas in multiple myeloma :sonographic, CT and MR imaging findings. AJR Am J Roentgenol 2003; 180:545-6. 13. Mitchell DG, Hill MC. Obstructive jaundice due to multiple myeloma of the pancreatic head: CT evaluation. J Comput Assist Tomogr 1985; 9:1118-9.
e107
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Your Consequences WorksheetДокумент10 страницYour Consequences WorksheetThe Center for Motivation and ChangeОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The JFK AutopsyДокумент6 страницThe JFK AutopsysithusoemoeОценок пока нет
- Lecciones Basicas en Control de Calidad.2008 Bio-Rad InglesДокумент62 страницыLecciones Basicas en Control de Calidad.2008 Bio-Rad InglesPili Gabriel67% (3)
- Basics of Stem Cell TransplantationДокумент46 страницBasics of Stem Cell TransplantationNarendra Bhattarai100% (5)
- CholecystectomyДокумент5 страницCholecystectomyRachelle Maderazo CartinОценок пока нет
- Motorcycle DiariesДокумент9 страницMotorcycle DiariesGelo De Guzman100% (1)
- Platelet IndicesДокумент17 страницPlatelet IndicesNarendra Bhattarai0% (1)
- Cephalometric Evaluation and Measurement of The Upper Airway PDFДокумент13 страницCephalometric Evaluation and Measurement of The Upper Airway PDFSoe San KyawОценок пока нет
- Calcaneum Fractures: Jensen Joseph GMC KannurДокумент104 страницыCalcaneum Fractures: Jensen Joseph GMC KannurAmel VnairОценок пока нет
- History of MicrobiologyДокумент3 страницыHistory of MicrobiologyAngeli ButedОценок пока нет
- 01 Bone Tumors DR SSDДокумент17 страниц01 Bone Tumors DR SSDNarendra BhattaraiОценок пока нет
- Jiwan Thursday Breast Lump FnaДокумент47 страницJiwan Thursday Breast Lump FnaNarendra BhattaraiОценок пока нет
- Anti Thyroglobulin FATG200 Multilingual E 23 0106 06Документ0 страницAnti Thyroglobulin FATG200 Multilingual E 23 0106 06Narendra BhattaraiОценок пока нет
- 03 - Head Neck - I - DR SVKДокумент31 страница03 - Head Neck - I - DR SVKNarendra BhattaraiОценок пока нет
- GCLP HandbookДокумент28 страницGCLP HandbookaloediyahОценок пока нет
- RBC MorphologyДокумент7 страницRBC MorphologyNarendra Bhattarai100% (1)
- Terumo DДокумент2 страницыTerumo DNarendra BhattaraiОценок пока нет
- Bethesda Tiroides PDFДокумент8 страницBethesda Tiroides PDFSebastian Sarutte RoselloОценок пока нет
- Clinical Use of Blood Blood Productsreplacement Fluid RUNAДокумент37 страницClinical Use of Blood Blood Productsreplacement Fluid RUNANarendra BhattaraiОценок пока нет
- Jiwan Lymphoma CytoДокумент51 страницаJiwan Lymphoma CytoNarendra BhattaraiОценок пока нет
- WHO Platelet and Leukocyte CountДокумент8 страницWHO Platelet and Leukocyte CountNarendra BhattaraiОценок пока нет
- Lymphatic SystemДокумент4 страницыLymphatic SystemNarendra BhattaraiОценок пока нет
- J Clin Pathol 2011 Bain 373 9Документ8 страницJ Clin Pathol 2011 Bain 373 9Narendra BhattaraiОценок пока нет
- Function of EndocrineДокумент11 страницFunction of EndocrineNarendra BhattaraiОценок пока нет
- Inflammation: A Complex Protective ReactionДокумент24 страницыInflammation: A Complex Protective ReactionNarendra BhattaraiОценок пока нет
- Icmi ChartsДокумент35 страницIcmi ChartsMohit JainОценок пока нет
- Thymic CystДокумент6 страницThymic CystNarendra BhattaraiОценок пока нет
- Basics of CPRДокумент8 страницBasics of CPRNarendra BhattaraiОценок пока нет
- Approach To Thrombocytopenia PDFДокумент7 страницApproach To Thrombocytopenia PDFNarendra BhattaraiОценок пока нет
- Action Potential in Cardiac Muscle 2003Документ11 страницAction Potential in Cardiac Muscle 2003Narendra BhattaraiОценок пока нет
- Compliance of Lung 2003Документ13 страницCompliance of Lung 2003Narendra Bhattarai100% (1)
- Cardiac Cycle 2003Документ27 страницCardiac Cycle 2003Narendra BhattaraiОценок пока нет
- Report - NCP SakhuwasabhaДокумент15 страницReport - NCP SakhuwasabhaNarendra BhattaraiОценок пока нет
- Resume 2019Документ1 страницаResume 2019api-316723361Оценок пока нет
- Relaxation TechniquesДокумент13 страницRelaxation TechniquesBhakti Joshi KhandekarОценок пока нет
- Clinical Rehabilitation: Does Electrical Stimulation Reduce Spasticity After Stroke? A Randomized Controlled StudyДокумент9 страницClinical Rehabilitation: Does Electrical Stimulation Reduce Spasticity After Stroke? A Randomized Controlled StudyArkar SoeОценок пока нет
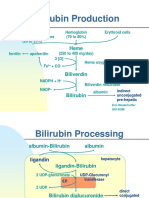
- Bilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Документ5 страницBilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Daffa Samudera Nakz DoeratipОценок пока нет
- Philips Respironics Bipap ST Niv Noninvasive VentilatorДокумент2 страницыPhilips Respironics Bipap ST Niv Noninvasive Ventilatorsonia87Оценок пока нет
- District Sales Manager in Los Angeles CA Resume Ronald FoxДокумент2 страницыDistrict Sales Manager in Los Angeles CA Resume Ronald FoxRonaldFoxОценок пока нет
- Hydralazine For Severe PIHДокумент4 страницыHydralazine For Severe PIHYwagar YwagarОценок пока нет
- Masterlist SummaryДокумент6 страницMasterlist Summarykentclark03Оценок пока нет
- Abigail BДокумент3 страницыAbigail BbjhilarioОценок пока нет
- Introduction To Dosage FormДокумент3 страницыIntroduction To Dosage FormkbnarkhedeОценок пока нет
- PG Physician Guide 03 Eng1Документ88 страницPG Physician Guide 03 Eng1hüseyin vururОценок пока нет
- Diagnostic Report SummaryДокумент5 страницDiagnostic Report SummaryShalini Rakesh JunejaОценок пока нет
- Monnal t75 Air Liquide Ventilator PDFДокумент10 страницMonnal t75 Air Liquide Ventilator PDFFederico DonfrancescoОценок пока нет
- Psychological Point of ViewДокумент3 страницыPsychological Point of ViewForam PatelОценок пока нет
- Wave One Brochure 0Документ18 страницWave One Brochure 0Shivendra Nath TripathiОценок пока нет
- 00-30juni 2023 Data Stok FLДокумент98 страниц00-30juni 2023 Data Stok FLSunaryo AryandaОценок пока нет
- ق 4Документ36 страницق 4Zainab HasanОценок пока нет
- Hybrid Hyrax Distalizer JO PDFДокумент7 страницHybrid Hyrax Distalizer JO PDFCaTy ZamОценок пока нет
- Pelvic Floor Exercises in The Elderly Irmina Nahon1Документ34 страницыPelvic Floor Exercises in The Elderly Irmina Nahon1Anonymous C7H7wS6Оценок пока нет
- Sound Transduction EarДокумент7 страницSound Transduction Earhsc5013100% (1)
- Scio Four Gas Module Family: Reliable and Flexible Gas AnalysisДокумент2 страницыScio Four Gas Module Family: Reliable and Flexible Gas AnalysisNasr Eldin AlyОценок пока нет
- Iryu.4 Team - Medical.Dragon.E09.720p.Web ENGДокумент45 страницIryu.4 Team - Medical.Dragon.E09.720p.Web ENGcintoyОценок пока нет
- Joint InfectionsДокумент10 страницJoint InfectionsJPОценок пока нет