Академический Документы
Профессиональный Документы
Культура Документы
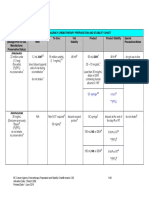
IVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.
Загружено:
Marc Imhotep Cray, M.D.Оригинальное название
Авторское право
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
IVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.
Загружено:
Marc Imhotep Cray, M.D.Авторское право:
HEMATOLOGY/ONCOLOGY SUMMARY
A companion to PowerPoint IVMS Hematology-Blood Physiology and Pathology Overview | Review
Terms Platelet
Macrophage
Eosinophils
Basophils
Mast cell
Factor XII
Definitions - contains dense granules (ADP, calcium) and -granules (vWF, fibrinogen) - approximately 1/3 of the body's platelet pool is stored in spleen - life span of 8-10 days - vWF receptor: GpIb - Fibrinogen receptor: GpIIb/IIIb - Phagocytoses bacteria, cell debris, and senescent red cells and scavenges damaged cells and tissues - long life in tissues - activated by -interferon - can function as APC via MHC II - CD14 surface marker - bilobate nucleus - packed with large eosinophilic granules of uniform size - highly phagocytic for Ag-Ab complexes - produces histamine and arylsulfatase (help limit reaction following mast cell degranulation) - causes of eosinophilia: neoplasia, asthma, allergic processes, collagen vascular diseases, parasites - mediates allergic reactions - bilobated nucleus - densely basophilic granules contain: heparin (anticoagulant), histamine (vasodilator), and other vasoactive amines, and leukotrienes (LTD4) - found in blood - mediates allergic reaction - degranulation - histamine, heparin, and eosinophil chemotatic factors - can bind the Fc portion of IgE to membrane - structurally and functionally similar to basophils - involved in type I hypersensitivity reactions - found in tissue - first step of the intrinsic pathway - activated by collagen, basement membrane, activated platelets, and HMWK (bradykinin precursor) - activates factor XI and converts prokallikrein to kallikrein
Page 1 of 16
Hematology-Oncology Summary /mic-12-13
Kallikrein
Bradykinin
Common coagulation pathway Factors effected by Vitamin K deficiency
Antithrombin
Protein C
tPA platelet plug formation
Aggregation balance
- activated by factor XII - converts HMWK to bradykinin (kinin cascade) - converts plasminogen to plasmin (degrades fibrin) - part of Kinin cascade, activated by intrinsic coagulation pathway - vasodilation - permeability - pain - X (+V) II (aka thrombin) Fibrin aggregation (by XIII and Ca2+) - both extrinsic and intrinsic pathways convert on factor X Factor II (thrombin, common pathway) Factor VII (extrinsic pathway) Factor IX (intrinsic pathway) Factor X (common pathway protein C protein S - vit K activated by epoxide reducatase cofactor in maturation of II, VII, IX, X, C, and S from precusors - activated by heparin - inhibits thrombin and: factor VII (extrinsic) factor IX (intrinsic) factor X (common) factor XI (intrinsic) factor XII (intrinsic) - Protein C is activated by thrombomodulin from endothelial cells - protein S assist activated protein C in the cleavage and inactivation of Va and VIIIa - activates plasmin, which degrades fibrin - used as a thrombolytic - injury: vWF binds to exposed collagen - adhesion: platelets bind vWF via GpIb receptor and release ADP and Ca2+ (necessary for coagulation cascade) - ADP: helps platelets adhere to endothelium, ADP binding to receptor induces GpIIb/IIIa expression at platelet surface aggregation: fibrinogen binds GpIIb/IIIa receptors and links platelets - Pro-aggregation factors: TXA2 (released by platelets) blood flow and platelet aggregation
Page 2 of 16
Hematology-Oncology Summary /mic-12-13
Drugs that disrupt thrombogenesis
Erythrocyte sedimentation rate
Pathologic RBC forms: acanthocyte Pathologic RBC forms: basophilic stippling
Pathologic RBC forms: Elliptocyte Pathologic RBC forms: macro-ovalocyte Pathologic RBC forms: ringed sideroblasts Pathologic RBC forms: schistocyte Pathologic RBC forms: spherocyte Pathologic RBC forms: teardrop cell Pathologic RBC forms: target cells
- Anti-aggregation factors: PGI2 and NO (released by endothelial cells) blood flow and platelet aggregation - aspirin: cyclooxygenase ( TXA2 synthesis) - Ticlopidine and clopidogrel: inhibits ADP-induced expression of GpIIb/IIIa (platelets can't cross link) - Abciximab: inhibits GpIIb/IIIa directly - acute-phase reactants in plasma can cause RBC aggregation, thereby RBC sedimentation rate - ESR: infections, inflammatory diseases, malignany neoplasms, GI disease, pregnancy - ESR: polycythemia, sickle cell anemia, CHF, microcytosis, hypofibrinogenemia (AKA: spur cell) - liver disease - abetalipoproteinemia - Thalassemia - Anemia of chronic disease - Iron deficiency - Lead poisoning - hereditary elliptocytosis - megaloblastic anemia (also hypersegmented PMNs) - marrow failure - sideroblastic anemia - DIC - TTP/HUS - traumatic hemolysis - hereditary spherocytosis - autoimmune hemolysis - bone marrow infiltration - HbC disease - Asplenia - Liver disease - Thalassemia - oxidation of iron from ferrous to ferric form leads to **denatured hemoglobin precipitation and damage to RBC membrane - -thalassemia - G6PD deficiency
Page 3 of 16
Pathologic RBC forms: Heinz bodies
Hematology-Oncology Summary /mic-12-13
Pathologic RBC forms: Howell-Jolly bodies Microcytic anemias
Normocytic, nonhemolytic anemias Hemolytic anemias intrinsic
Hemolytic anemias extrinsic
Megaloblastic anemias Macrocytic, nonmegaloblastic anemias
Iron deficiency anemia
-thalassemia
- basophilic nuclear remnants found in RBCs - due to functional hyposplenia or asplenia - Iron deficiency - Anemia of chronic disease (may initially present as normocytic anemia) - Thalassemias - Lead poisoning - Sideroblastic anemia - Anemia of chronic disease (progresses to microcytic) - Aplastic anemia - Kidney disease - RBC membrane defect: hereditary spherocytosis - RBC enzyme deficiency: G6PD, pyruvate kinase deficiency - HcC - Sickle cell anemia - Paroxysmal nocturnal hemoglobinuria - Autoimmune - Microangiopathic hemolytic anemia (MIHA) - Macroangiopathic hemolytic anemia (MAHA) - Infections - Folate deficiency - B12 deficiency - DNA synthesis is impaired -caused by liver disease, alcoholism, reticulocytosis MCV, metabolic disorders, congenital deficiencies of purine and pyrimidine synthesis and drugs (5-FU, zidovudine, hydroxyurea) - microcytic, hypochromic - iron heme synthesis - Plummer-Vinson: iron deficiency anemia, esophageal web, atrophic glossitis - Labs: serum iron transferrin or TIBC ferritin % transferrin saturation - microcytic, hypochromic - defect in -globin gene mutation -globin synthesis - prevalent in Asian and African populations - peripheral blood smear: basophilic stippling, target cells, Heinz bodies - 4 gene deletion = hydrops fetalis, (Hb Barts, 4)
Page 4 of 16
Hematology-Oncology Summary /mic-12-13
-thalassemia minor
-thalassemia major
HbS/-thalassemia heterozygotes Lead poisoning anemia
Sideroblastic anemia
- 3 gene deletion = HbH disease (4) - 1-2 gene deletion = no significant anemia - microcytic, hypochromic - point mutations in splice sites and promoter sequences globin synthesis - HbF (22) - peripheral smear: anisocytosis, poikilocytosis, target cells, schistocytes - seen in Mediterranean populations - minor = heterozygote - chain is underproduced - usually asymptomatic - Diagnosis confirmed by HbA2 (22) on electrophoresis - microcytic, hypochromic - point mutations in splice sites and promoter sequences globin synthesis - HbF (22) - seen in Mediterranean populations - major = homozygote - chain is absent severe anemia requiring blood transfusions - presents with marrow expansion skeletal deformities, Chipmunk facies - mild to moderat sickle cell disease depending on amount of globin production - microcytic, hypochromic - lead inhibits ferrochelatase and ALA dehydratase heme synthesis, protoporphyrin in blood - also inhibits rRNA degredation - presents with lead lining the epiphyses of long bones on x-ray, encephalopathy, erythrocyte basophilic stippling, abdominal colic, wrist/foot drop and sideroblastic anemia - adults: headache, memory loss, demyelination - treatment: Dimercaprol, EDTA, and succimer (for kids) - microcytic, hypochromic - defect in heme synthesis - Hereditary: x-linked defect in -aminolevulinic acid synthase gene - reversible etiologies: alcohol, lead - peripheral smear: ringed sideroblasts (from iron-laden mitochondria) - Labs: iron, normal TIBC, ferritin
Page 5 of 16
Hematology-Oncology Summary /mic-12-13
Folate Deficiency Megaloblastic anemia
B12 deficiency megaloblastic anemia
Intravascular hemolysis
Extravascular hemolysis
Anemia of Chronic Disease
aplastic anemia
Hereditary spherocytosis
- treatment: pyridoxine (B6) therapy - macrocytic - impaired DNA synthesis maturation of nucleus delayed - ineffective erythropoiesis pancytopenia - presents with hypersegmented neutrophils, glossitis, folate, homocyseine but normal methylmalonic acid - macrocytic - impaired DNA synthesis maturation of nucleus delayed - ineffective erythropoiesis pancytopenia - causes: insufficient intake, malabsorption, pernicious anemia, Diphyllobothrium latum (fish tapeworm) - presents with hypersegmented neutrophils, glossitis, B12, homocysteine, methylmalonic acid - Neurological symptoms: due to B12 involvement in fatty acid pathway peripheral neuropathy (sensorimotor), posterior column (vib/proprio), spasticity, dementia - haptoglobin (cleans up spilled heme, decrease means it is being used) - Lactate dehydrogenase - hemoglobin in urine - macrophages in spleen clears RBCs - LDH - unconjugated bilirubin jaundice - nonhemolytic, normocytic anemia - chronic inflammation hepcidin release of iron from macrophages - hepcidin - released by liver, binds ferroportin on intestinal mucosal cells and macrophages thus inhibiting iron transport - labs: iron, TIBC, ferritin - can become microcytic, hypochromic in long standing disease - nonhemolytic, normocytic anemia - failure or destruction of myeloid stem cells (radiation, drugs, viral, Fanconi's anemia, idiopathic) - pancytopenia, normal cell morphology but with hypocellular bone marrow (fatty infiltration) - presents with: fatigue, malaise, pallor, purpura, mucosal bleeding petechiae, infection - treatment: withdrawal cause, allogeneic marrow transplant, transfusion, granulocyte colony stimulating factor (G-CSF), GMCSF - intrinsic hemolytic, normocytic anemia
Page 6 of 16
Hematology-Oncology Summary /mic-12-13
Mean Cell Volume (MCV)
Mean cell hemoglobin concentration (MCHC)
Red cell distribution width (RDW)
G6PD deficiency
Pyruvate kinase deficiency
HbC defect
- extravascular hemolysis - defects in ankyrin, band 3, protein 4.2, or spectrin which are involved in cytoskeleton and membrane integrity - less membrane spherocytes premature removal by spleen - labs: MCHC, RDW - presents with splenomegaly, aplastic crisis (B19 infections), positive osmotic fragility test - treat with splenectomy - Average **size of red blood cells - Normal range: 80-100 fL (1 fL = 10-15 L) - Differentiates between microcytic (MCV < 80) normocytic (MCV 80-100) macrocytic (MCV >100) anemias - Concentration of Hgb RBC - expresses coloration** - Normal range: 32-36 g/dL - Differentiates between hypochromic (MCHC < 32) and normochromic (MCHC 32-36) anemias - normochromic cells have a "zone of central pallor" (that white dot in the middle of the cell) that is no more than 1/3 the diameter of the red cell. - Hypochromic red cells have just a thin rim of hemoglobin. - Standard deviation of the MCV - Tells you how much the RBC differ from each other in size. Anisocytosis - If they are all pretty similar in size, the RDW is low. - If some are little and some are big, the RDW is high. - Normal range = 12-13.5% - intrinsic hemolytic, normocytic anemia - intravascular and extravascular hemolysis - x-linked - hemolytic anemia follows oxidative stress - presents with back pain and hemoglobinuria a few days later - intrinsic hemolytic, normocytic anemia - extravascular hemolysis - autosomal recessive - defect in pyruvate kinase ATP rigid RBCs pyruvate kinase catalyzes pyruvate to lactate - hemolytic anemia in newborns - intrinsic hemolytic, normocytic anemia - glutamic acid-to-lysine mutation at position 6 in chain mutation
Page 7 of 16
Hematology-Oncology Summary /mic-12-13
Paroxysmal nocturnal hemoglobinuria
Sickle cell anemia
autoimmune hemolytic anemia
Erythroblastosis fetalis
Direct Coomb's test Indirect Coomb's test Microangiopathic anemia
Macroangiopathic anemia
Hemochromatosis
- patients with HbSC (1 of each mutated gene) have milder disease than do HbSS patients - intrinsic hemolytic, normocytic anemia - intravascular hemolysis - complement-mediated RBC lysis - impaired synthesis of GPI anchor/decay-accelerating factor in RBC membrane - urine hemosiderin - complication: thrombosis - point mutation on -chain (glutamic acid valine at position 6) - sickling from low O2 or dehydration - complications: aplastic crisis (Parvovirus B19), autosplenectomy, splenic sequestration crisis, salmonella osteomyelitis, painful crisis (dactylitis [painful hand swelling], acute chest syndrome), renal papillary necrosis, microhematuria - treatment: hydroxuria (HbF), bone marrow transplant - extrinsic hemolytic, normocytic anemia - warm agglutination (IgG) - chronic anemia seen in SLE, CLL, or with certain drugs - cold agglutination (IgM) - acute anemia triggered by cold, seen in CLL, Mycoplasma pneumonia infections, or mononucleosis - usually Coomb's test positive - seen in newborns due to Rh or other blood antigen incompatibility - mother's Ab attack fetal RBCs - anti-Ig antibody added to patient's RBCs agglutinate if RBCs are coated with Ig - normal RBCs added to a patient's serum agglutinate if serum has anti-RBC surface Ig - extrinsic hemolytic, normocytic anemia - intravascular hemolysis - RBCs are damaged when passing through obstructed or narrow vessel lumina - seen in DIC, TTP-HUS, SLE, and malignant hypertension - schistocytes on blood smear - extrinsic hemolytic, normocytic anemia - intravascular hemolysis - prosthetic heart valves and aortic stenosis may also cause hemolytic anemia, mechanical destruction - schistocyte on peripheral smear - labs:
Page 8 of 16
Hematology-Oncology Summary /mic-12-13
Acute intermittent porphyria
Porphyria cutanea tarda
PT (prothrombin time)
aPTT (Partial Thromboplastin Time) Hemophilia
Platelet disorders
Bernard-Soulier disease
Glanzmann's thrombasthenia
serum iron transferrin ferritin % transferrin saturation - defective heme synthesis that leads to accumulation of heme precursors - affected enzyme: porphobilinogen deaminase - accumulation of porphobilinogen, - ALA, uroporphyrin - presents with painful abdomen, red wine colored urine, polyneuropathy, psychological disturbance, precipitated by drugs - treat with glucose and heme - defective heme synthesis that leads to accumulation of heme precursors - affected enzyme: Uroporphyrinogen decarboxylase - accumulation of uroporphyrin - blistering cutaneous photosensitivity - most common porphyria - tests the extrinsic pathway - factor VII (also I, II, V, and X) - defect leads to increased time - tests the intrinsic pathway - all factors except VII and XIII - defect leads to increased time - aPTT - A: deficiency in VIII - B: deficiency in IX - macrohemorrhage, hemarthroses, easy bruising - defect in platelet plug formation bleeding time - platelet abnormalities microhemorrhages, mucous membrane bleeding, epitaxis, petechiae, purpura, bleeding time, possible platelet count - Bernard-Soulier disease, Glanzmann's thrombathenia, idiopathic thrombocytopenic purpura (ITP), Thrombotic thrombocytopenic purpura (TTP) - defect in platelet plug formation - GpIb defect in platelet to collagen adhesion - platelet count - Bleeding time - defect in platelet plug formation - GpIIb/IIIa defect in platelet to platelet aggregation - bleeding time, blood smear shows no platelet clumping
Page 9 of 16
Hematology-Oncology Summary /mic-12-13
Idiopathic thrombocytopenic purpura (ITP)
Thrombotic thrombocytopenic purpura (TTP)
von Willebrand's disease
DIC
Factor V Leiden
Prothrombin gene mutation Antithrombin deficiency
Protein C or S deficiency
Blood transfusion therapy: packed RBCs Blood transfusion therapy: platelets
- platelet survival - anti- GpIIb/IIIa antibodies peripheral platelet destruction - megakaryocytes - bleeding time - platelet count - platelet survival - deficiency of ADAMTS 13 degradation of vWF multimers platelet aggregation and thrombosis - Labs: schistocytes, LDH - presents with pentad of neurologic and renal symptoms, fever, thrombocytopenia, and microangiopathic hemolytic anemia - platelet count - bleeding time - vWF carries and protects factor VIII, connects GpIb of platelet to collagen - defect of intrinsic pathway, vWF may see aPTT - defect of platelet adhesion to collagen bleeding time - mild, but most common bleeding disorder - treatment: desmopressin (releases vWF stored in epithelial cells) - wide spread activation of clotting leads to a deficiency in clotting factors bleeding state - caused by sepsis (G (-)), trauma, obstetric complications, acute pancreatitis, Malignancy, Nephrotic syndrome, Transfusion - Labs: schistocytes, fibrin split product (D-dimer), fibrinogen, factors V and VII - production of mutant factor V that cannot be degraded by protein C - most common cause of inherited hyprcoagulability - leads to hypercoagulable state - mutation in 3' untranslated region associated with venous clots - leads to hypercoagulable state - inherited deficiency of antithrombin - reduced in PTT after administration of heparin - leads to hypercoagulable state - ability to inactivate factors V and VIII - risk of thrombotic skin necrosis with hemorrhage following administration of warfarin - Hb and O2 carrying capacity - acute blood loss and severe anemia - platelet count - usually given in 6 platelet units for therapeutic effect
Page 10 of 16
Hematology-Oncology Summary /mic-12-13
Blood transfusion therapy: Fresh frozen plasma Blood transfusion therapy: cryoprecipitate Blood transfusion risks
Hodgkin's lymphoma
Non-Hodgkin's lymphoma
Nodular sclerosing Hodgkin's lymphoma
Mixed cellularity Hodgkin's lymphoma
Lymphocyte predominant
- stop significant bleeding (thrombocytopenia, qualitative platelet defects) - coagulation factor levels by about 20% - treats DIC, cirrhosis, warfarin over-anticoagulation - contains fibrinogen, factor VIII, factor XIII - treats coagulation factor deficiencies involving fibrinogen and factor VIII - infection - reactions - iron overload - hypocalcemia - citrate is a calcium chelator - hyperkalemia - RBCs may lyse in older blood units - Reed-Sternberg cells (CD30+/CD15+) - localized to single group of nodes - contiguous spread - constitutional signs/symptoms - low-grade fever, night sweats, weight loss - mediastinal lymphadenopathy - 50% of cases associated with EBV - bimodal age distribution - more common in men except the nodular sclerosing type (lacunar variant of RS cells) - good prognosis = lymphocytes, RS cells - may be associated with HIV and immunosuppression - multiple peripheral nodes - extranodal involvement common - noncontiguous spread - majority involve B cells (except for those of lymphoblastic T cell origin) - fewer constitutional signs/symptoms - peak incidence for certain subtypes at 20-40 years - most common type (65-75%) - variant type RS cells - increased # of lymphocytes - excellent prognosis - collagen banding, women >men, primarily young adults - lots of RS cells - increased lymphocytes - intermediate prognosis - 25% of Hodgkin's lymphoma cases - seen in males under 35
Page 11 of 16
Hematology-Oncology Summary /mic-12-13
Hodgkin's lymphoma
Lymphocyte depleted Hodgkin's lymphoma
Burkitt's lymphoma
Diffuse large B-cell lymphoma
Mantle cell lymphoma
Follicular lymphoma
Adult T cell lymphoma
Mycosis fungoides/Sezary syndrome
Multiple myeloma
- some RS cells, lymphocytes - excellent prognosis - 6% of Hodgkin's lymphoma cases - slight increase in lymphocytes - RS high relative to lymphocytes - seen in older males with disseminated disease - poor prognosis - non-Hodgkin's lymphoma - seen in young adults - genetics: t(8;14) c-myc gene moves next to heavy-chain Ig gene - "starry-sky" appearance - sheets of lymphocytes with interspersed macrophages - EBV - Jaw lesion most common, pelvis or abdomen in sporadic form - non-Hodgkin's lymphoma - usually seen in older adults, 20% in kids - most common NHL - may be of mature T cell origin (20%) - non-Hodgkin's lymphoma, B cell - seen in older males - genetics: t(11;14) overexpression of cyclin D regulatory gene - CD5+ - poor prognosis - non-Hodgkin's lymphoma, B cell - seen in adults - genetics: t(14;18) bcl-2 expression inhibits apoptosis - difficult to cure, indolent course - non-Hodgkin's lymphoma, T cell - seen in adults - caused by HTLV-1 - adults present with cutaneous lesions - especially effects populations in Japan, West Africa, and the Caribbean - aggressive - non-Hodgkin's lymphoma, T cell - seen in adults - adults present with cutaneous patches/nodules - indolent CD4+ - monoclonal plasma cell (fried egg appearance) cancer that arises from the marrow and produces large amounts of IgG (55%) or IgA (25%)
Page 12 of 16
Hematology-Oncology Summary /mic-12-13
MGUS
Leukemias
ALL - Acute lymphoblastic leukemia/lymphoma
SLL - small lymphocytic lymphoma/CLL - chronic lymphocytic leukemia
Hairy cell leukemia
AML - Acute myelogenous leukemia
- most common 1 tumor arising within bone in the elderly - intracytoplasmic inclusions containing Ig - CRAB: hyperCalcemia Renal insufficiency Anemia Bone lytic lesions Back pain (distinguish from Waldenstrom's macroglobulinemia M spike = IgM, and no lytic bone lesions) - monoclonal gammopathy of undetermined significance - monoclonal plasma cell expansion without symptoms of multiple myeloma - unregulated growth of leukocytes in bone marrow - or number of circulating leukocytes in blood and marrow failure - anemia, infections, & hemorrhage - leukemic cell infiltrates in liver, spleen, and lymph nodes are possible - usually seen < 15 y/o - may present with BM involvement in children or mediastinal mass in adolescent males - BM replaced by lymphoblasts - TdT+ (marker of pre-T/B cells) - CALLA+ - most responsive to therapy - may spread to CNS or testes - genetics: t(12;21) - usually seen > 60 y/o - often asymptomatic - smudge cells in peripheral smear - warm antibody autoimmune hemolytic anemia - SLL is same as CLL except CLL has peripheral blood lymphocytes - seen in adults - Mature B cell tumor in elderly - cells have filamentous hairlike projections - stain TRAP (tartrate-resistant acid phosphatase) positive - seen in 60 y/o - Histo: Auer rods in cytoplasm - circulating myeloblasts on peripheral smear - genetics: t(15;17) M3 AML (acute promyelocytic leukemia)
Page 13 of 16
Hematology-Oncology Summary /mic-12-13
CML - Chronic myelogenous leukemia
Auer bodies
Langerhans cell histiocytosis (LCH)
Polycythemia vera
Essential thrombocytosis
Myelofibrosis
responds to all-trans retinoic acid (vitamin A), which induces differentiation of myeloblasts - DIC is common presentation - 30-60 y/o - Philadelphia chromosome - t(9;22), bcr-abl - JAK2 mutation? - myeloid stem cell proliferation - presents with RBC, neutrophils, metamyelocytes, basophils, platelets; splenomegaly - may accelerate and transform to AML or ALL (blast crisis) - very low leukocyte alkaline phosphatase due to immature granulocytes - treat with imatinib - peroxidase-positive cytoplasmic inclusions in granulocytes and myeloblasts - commonly seen in acute promyelocytic leukemia (M3) - treatment of AML M3 can release Auer rods DIC - proliferative disorder of dendritic (langerhans) cells from monocyte lineage - etiology unknown - cells are functionally immature and do not efficiently stimulate T lymphocytes - cells express S-100 and CD1a - Birbeck granules (look like tennis rackets on EM) - chronic myeloproliferative disorders - abnormal clone of hematopoietic stem cells are increasingly sensitive to growth factor - RBCs ( plasma volume, RBC mass) - WBCs - platelets - genetics: JAK2+ - chronic myeloproliferative disorders - similar to polycythemia vera, but specific for megakaryocytes - platelets - genetics: JAK2+ (30-50%) - chronic myeloproliferative disorders - fibrotic obliteration of BM - teardrop cells in blood smear - RBCs - variable amounts of WBCs - variable amounts of platelets
Page 14 of 16
Hematology-Oncology Summary /mic-12-13
Drug: Cytarabine
Drug: Dactinomycin/ Actinomycin
Drug: Busulfan
Drug: Tacrolimus
Drug: Azathioprine
Muromonab
Pernicious anemia
- neoplastic drug, antimetabolite - pyrimidine analog inhibition of DNA polymerase - S-phase specific - treats: AML, ALL, high-grade non-Hodgkin's lymphoma - toxicity: leukopenia, thrombocytopenia, megaloblastic anemia - antitumor antibiotics - intercalates in DNA - treats: Wilms' tumor, Ewing's sarcoma, rhabdomyosarcoma - used for childhood tumors - toxicity: myelosuppression - alkylating agent - alkylates DNA - Treats: CML - also used to ablate patient's bone marrow before bone marrow transplant - toxicity: pulmonary fibrosis, hyperpigmentation - binds to FK-binding protein, inhibiting secretion of IL-2 and other cytokines - similar to cyclosporine - potent immunosuppressant used in organ transplant - Toxicity: nephrotoxicity, peripheral neuropathy, hypertension, pleural effusion, hyperglycemia - antimetabolite precursor of 6-mercaptopurine that interferes with the metabolism and synthesis of nucleic acids - toxic to proliferating lymphocytes - used for kidney transplantation and autoimmune disorders (glomerulonephritis and hemolytic anemia) - Toxicity: BM suppression - Active metabolite mercaptopurine is metabolized by xanthine oxidase, toxic effects by allopurinol - AKA: OKT3 - monoclonal antibody that binds CD3 on the surface of T cells - blocks cellular interaction with CD3 protein responsible for T cell signal transduction - used for immunosuppression after kidney transplant - Toxicity: cytokine release syndrome, hypersensitivity reaction - type II hypersensitivity reaction - autoantibodies against proton pump in parietal cells (85-90%), antibodies that block binding of vitamin B12 to intrinsic factor (60-75%), antibodies that prevent binding of B12-IF complexes to ileal receptors (30-50%)
Page 15 of 16
Hematology-Oncology Summary /mic-12-13
- presents with achlorhydria (lack of gastric acid) due to parietal cell destruction, chronic gastritis, increased risk of gastric carcinoma, elevated serum gastrin, and signs of vitamin B12 deficiency
Hematology-Oncology Summary /mic-12-13
Page 16 of 16
Вам также может понравиться
- UW (Step 1) Renal - Educational Objectives PDFДокумент50 страницUW (Step 1) Renal - Educational Objectives PDFDrbee10Оценок пока нет
- Medical Student Amnesia USMLE Step 1 - Flash Cards by CueFlashДокумент13 страницMedical Student Amnesia USMLE Step 1 - Flash Cards by CueFlashMuhammad Farhan KhaliqОценок пока нет
- Flashcards FinalДокумент272 страницыFlashcards FinalMarie SantoroОценок пока нет
- Usmle 1Документ36 страницUsmle 1Suruchi Jagdish SharmaОценок пока нет
- Goljan Transcripts - Nts MODIFIED With SLIDES 5Документ91 страницаGoljan Transcripts - Nts MODIFIED With SLIDES 5Divya KondaveetiОценок пока нет
- Micro Buzz Words - KEY WordsДокумент8 страницMicro Buzz Words - KEY WordsKris GulleyОценок пока нет
- SURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1От EverandSURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1Рейтинг: 5 из 5 звезд5/5 (2)
- Comquest NotesДокумент58 страницComquest NotesBhumiShahОценок пока нет
- Hematology & Oncology FirecrackerДокумент91 страницаHematology & Oncology FirecrackerMiri PravdaОценок пока нет
- Renal SystemДокумент76 страницRenal SystemDaNy ChiriacОценок пока нет
- Combank NotesДокумент7 страницCombank NotesVee MendОценок пока нет
- Online Med Ed NotesДокумент12 страницOnline Med Ed NotessonОценок пока нет
- 269 First Aid Plus U WorldДокумент25 страниц269 First Aid Plus U WorldHoney HoneyОценок пока нет
- Genetic Conditions For USMLEДокумент2 страницыGenetic Conditions For USMLEkcxieОценок пока нет
- Micro Cheat Sheet #1 For PASS ProgramДокумент10 страницMicro Cheat Sheet #1 For PASS ProgramOJOSAZULESAK100% (1)
- Internal Medicine NBME Form 3 ExplanationsДокумент11 страницInternal Medicine NBME Form 3 ExplanationssasghfdgОценок пока нет
- NBME 1 RatioДокумент87 страницNBME 1 RatioBugs Caslib100% (1)
- Medical Triads, Tetrads, and PentadsДокумент10 страницMedical Triads, Tetrads, and PentadsAyessa BandalОценок пока нет
- Problem-based Approach to Gastroenterology and HepatologyОт EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisОценок пока нет
- USMLE Most CommonДокумент3 страницыUSMLE Most Commonkohinoor81525650% (2)
- Amboss Hemolytic AnemiaДокумент16 страницAmboss Hemolytic AnemiaAhmed Ali100% (2)
- 'Aliah's Physio NotesДокумент30 страниц'Aliah's Physio NotesLuqman Al-Bashir FauziОценок пока нет
- 2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksДокумент25 страниц2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksRushi ShahОценок пока нет
- Hematology Slides Step 1 UsmleДокумент1 страницаHematology Slides Step 1 Usmlenreena aslamОценок пока нет
- Second Aid - USMLE MnemonicsДокумент21 страницаSecond Aid - USMLE MnemonicsKgerbОценок пока нет
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessОт EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanОценок пока нет
- Uwise HYДокумент3 страницыUwise HYJack GuccioneОценок пока нет
- Revised PPClues - 3-3-08Документ16 страницRevised PPClues - 3-3-08jeffjohnson909100% (2)
- Second Aid USMLE Mnemonics PDFДокумент19 страницSecond Aid USMLE Mnemonics PDFTony Lǎo Hǔ ChenОценок пока нет
- DO Student Write Up 265 780Документ3 страницыDO Student Write Up 265 780aloverofdanceОценок пока нет
- Medical MnemonicsДокумент256 страницMedical MnemonicssitalcoolkОценок пока нет
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsОт EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsОценок пока нет
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Multiple Choice Questions for Haematology and Core Medical TraineesОт EverandMultiple Choice Questions for Haematology and Core Medical TraineesОценок пока нет
- Kochar's Clinical Medicine for Students: Sixth EditionОт EverandKochar's Clinical Medicine for Students: Sixth EditionОценок пока нет
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- IVMS-Hematology-Oncology Terminology Summary TableДокумент16 страницIVMS-Hematology-Oncology Terminology Summary TableMarc Imhotep Cray, M.D.Оценок пока нет
- Robbins Pathology Chapter 14 - RBCsДокумент7 страницRobbins Pathology Chapter 14 - RBCsscorpiosphinx79100% (10)
- Microcytic Hypochromic Macrocytic Normochromic Normocytic: Anemia HematocritДокумент7 страницMicrocytic Hypochromic Macrocytic Normochromic Normocytic: Anemia Hematocritjjjj31Оценок пока нет
- Hematology Board Review 2Документ33 страницыHematology Board Review 2Edwin OkonОценок пока нет
- SGL 2 (Hemolytic Anemia & Hemoglobinopathies)Документ53 страницыSGL 2 (Hemolytic Anemia & Hemoglobinopathies)raman mahmudОценок пока нет
- HP Pathologies SummaryДокумент10 страницHP Pathologies SummaryMiki AberaОценок пока нет
- Drug-Drug Interactions (DDIs)Документ63 страницыDrug-Drug Interactions (DDIs)Marc Imhotep Cray, M.D.100% (3)
- Molecular and Cell Biology of The Endocrine SystemДокумент78 страницMolecular and Cell Biology of The Endocrine SystemMarc Imhotep Cray, M.D.Оценок пока нет
- Host Defense and Microbial PathogenesisДокумент72 страницыHost Defense and Microbial PathogenesisMarc Imhotep Cray, M.D.Оценок пока нет
- Prepared and Presented by Marc Imhotep Cray, M.DДокумент30 страницPrepared and Presented by Marc Imhotep Cray, M.DMarc Imhotep Cray, M.D.100% (1)
- HIV and AIDSДокумент75 страницHIV and AIDSMarc Imhotep Cray, M.D.100% (1)
- Endocrine System Pathology PPT Lecture SeriesДокумент285 страницEndocrine System Pathology PPT Lecture SeriesMarc Imhotep Cray, M.D.100% (6)
- Drug Metabolism and Drug InteractionsДокумент52 страницыDrug Metabolism and Drug InteractionsMarc Imhotep Cray, M.D.100% (1)
- Pneumonia and Lung AbscessДокумент50 страницPneumonia and Lung AbscessMarc Imhotep Cray, M.D.Оценок пока нет
- Gram Positive RodsДокумент15 страницGram Positive RodsMarc Imhotep Cray, M.D.Оценок пока нет
- Renal Pathology Lectures - PPT SeriesДокумент267 страницRenal Pathology Lectures - PPT SeriesMarc Imhotep Cray, M.D.100% (12)
- Clinical History and Examination of Patients With Infectious DiseaseДокумент43 страницыClinical History and Examination of Patients With Infectious DiseaseMarc Imhotep Cray, M.D.Оценок пока нет
- Mechanisms of Antibiotic ActionДокумент15 страницMechanisms of Antibiotic ActionMarc Imhotep Cray, M.D.Оценок пока нет
- Pulmonary Tuberculosis, With Leprosy and HIV-Tuberculosis CoinfectionДокумент74 страницыPulmonary Tuberculosis, With Leprosy and HIV-Tuberculosis CoinfectionMarc Imhotep Cray, M.D.Оценок пока нет
- Gastrointestinal Physiology-A Global OverviewДокумент76 страницGastrointestinal Physiology-A Global OverviewMarc Imhotep Cray, M.D.Оценок пока нет
- 4-Pharmacokinetics IДокумент88 страниц4-Pharmacokinetics IMarc Imhotep Cray, M.D.Оценок пока нет
- Drugs Used in Disorders of The Gastrointestinal SystemДокумент201 страницаDrugs Used in Disorders of The Gastrointestinal SystemMarc Imhotep Cray, M.D.Оценок пока нет
- 6-Pharmacokinetics and Pharmacokinetics SynopsisДокумент60 страниц6-Pharmacokinetics and Pharmacokinetics SynopsisMarc Imhotep Cray, M.D.100% (2)
- General Principles of Pharmacology - Approach To Learning PharmacologyДокумент65 страницGeneral Principles of Pharmacology - Approach To Learning PharmacologyMarc Imhotep Cray, M.D.Оценок пока нет
- Renal Insufficiency - Dialysis, Urinary Incontinence - CalculiДокумент27 страницRenal Insufficiency - Dialysis, Urinary Incontinence - CalculiMarc Imhotep Cray, M.D.Оценок пока нет
- Pharmacodynamics II Dose Response RelationshipsДокумент35 страницPharmacodynamics II Dose Response RelationshipsMarc Imhotep Cray, M.D.Оценок пока нет
- Definitions, Basic Principles and Pharmacodynamics IДокумент28 страницDefinitions, Basic Principles and Pharmacodynamics IMarc Imhotep Cray, M.D.100% (1)
- Renal Physiology and Regulation of Water and Inorganic IonsДокумент73 страницыRenal Physiology and Regulation of Water and Inorganic IonsMarc Imhotep Cray, M.D.67% (3)
- From Enzyme Kinetics To Drug Receptor InteractionsДокумент20 страницFrom Enzyme Kinetics To Drug Receptor InteractionsMarc Imhotep Cray, M.D.Оценок пока нет
- Clinical Pharmacology of Drugs Used To Affect Renal FunctionДокумент117 страницClinical Pharmacology of Drugs Used To Affect Renal FunctionMarc Imhotep Cray, M.D.Оценок пока нет
- Bacterial Pneumonia PharmacologyДокумент70 страницBacterial Pneumonia PharmacologyMarc Imhotep Cray, M.D.Оценок пока нет
- Pulmonary Tuberculosis PharmacologyДокумент48 страницPulmonary Tuberculosis PharmacologyMarc Imhotep Cray, M.D.Оценок пока нет
- Basic Pharmacology of DiureticsДокумент46 страницBasic Pharmacology of DiureticsMarc Imhotep Cray, M.D.100% (3)
- BP, The Kidneys and Diuretics As Anti-HTN AgentsДокумент18 страницBP, The Kidneys and Diuretics As Anti-HTN AgentsMarc Imhotep Cray, M.D.Оценок пока нет
- Drugs Used in Disorders of The Respiratory SystemДокумент100 страницDrugs Used in Disorders of The Respiratory SystemMarc Imhotep Cray, M.D.Оценок пока нет
- Respiratory Pathology and Pathophysiology-Global OverviewДокумент90 страницRespiratory Pathology and Pathophysiology-Global OverviewMarc Imhotep Cray, M.D.100% (1)
- GoldenretrieverДокумент6 страницGoldenretrieverTobias-Andreas DietzelОценок пока нет
- UC San Diego: Independent Study ProjectsДокумент21 страницаUC San Diego: Independent Study ProjectsSoha ShahidОценок пока нет
- DOPR Vision 2030Документ36 страницDOPR Vision 2030Hendi HendriansyahОценок пока нет
- Aldrine Ilustricimo VS Nyk Fil Sjip Management IncДокумент11 страницAldrine Ilustricimo VS Nyk Fil Sjip Management Inckristel jane caldozaОценок пока нет
- Fat Soluble VitaminsДокумент20 страницFat Soluble VitaminsWati WindayaniОценок пока нет
- Infective Endocarditis (IE)Документ76 страницInfective Endocarditis (IE)Mahesh RathnayakeОценок пока нет
- 1.11 ANATOMY - The Nose and Paransal SinusesДокумент4 страницы1.11 ANATOMY - The Nose and Paransal SinusesPaolo NaguitОценок пока нет
- Acid Base PhysiologyДокумент1 страницаAcid Base PhysiologyHAMMYER ALROKHAMIОценок пока нет
- Muscles of Mastication Saurav 2Документ79 страницMuscles of Mastication Saurav 2FourthMolar.comОценок пока нет
- Music Therapy in Nursing HomesДокумент7 страницMusic Therapy in Nursing Homesapi-300510538Оценок пока нет
- A Sonographic Sign of Moderate ToДокумент5 страницA Sonographic Sign of Moderate ToDivisi FER MalangОценок пока нет
- Menstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleДокумент6 страницMenstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- CHED DOH JMC No. 2021 004Документ31 страницаCHED DOH JMC No. 2021 004Miguel PAlmaresОценок пока нет
- QB BT PDFДокумент505 страницQB BT PDFنيزو اسوОценок пока нет
- DR Bagus Ari - Cardiogenic Shock KuliahДокумент28 страницDR Bagus Ari - Cardiogenic Shock KuliahrathalosredОценок пока нет
- Riddhi Perkins College ResumeДокумент3 страницыRiddhi Perkins College Resumeapi-3010303820% (1)
- Polydactyly of The Foot A Review.92Документ10 страницPolydactyly of The Foot A Review.92mamyeu1801Оценок пока нет
- BioInformatics Quiz1 Week14Документ47 страницBioInformatics Quiz1 Week14chahoub100% (4)
- 13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsДокумент36 страниц13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsAzam DanishОценок пока нет
- Tendonitis Guide - Causes, Symptoms and Treatment OptionsДокумент6 страницTendonitis Guide - Causes, Symptoms and Treatment OptionsSylvia GraceОценок пока нет
- Hemorrhoid - Pathophysiology and Surgical ManagementA LiteratureДокумент7 страницHemorrhoid - Pathophysiology and Surgical ManagementA LiteratureIndra YaniОценок пока нет
- 10a General Pest Control Study GuideДокумент128 страниц10a General Pest Control Study GuideRomeo Baoson100% (1)
- Adult Failure To ThriveДокумент5 страницAdult Failure To Thriveasmika danaОценок пока нет
- Operator MGC Ultima PFX - English - 142152-001rCДокумент65 страницOperator MGC Ultima PFX - English - 142152-001rCEvangelosОценок пока нет
- GIEEE TGMP Policy Terms For 2022-23Документ5 страницGIEEE TGMP Policy Terms For 2022-23Janardhan Reddy TОценок пока нет
- Conduction Blocks in Acute Myocardial Infarction: A Prospective StudyДокумент6 страницConduction Blocks in Acute Myocardial Infarction: A Prospective StudyJack JacksonОценок пока нет
- Biology Viral DiseasesДокумент11 страницBiology Viral DiseasesPrasoon Singh RajputОценок пока нет
- Chemo Stability Chart AtoK 1jun2016Документ46 страницChemo Stability Chart AtoK 1jun2016arfitaaaaОценок пока нет
- ANIOSPRAY QUICK-Fiche Technique-00000-ENДокумент2 страницыANIOSPRAY QUICK-Fiche Technique-00000-ENGustea Stefan AlinОценок пока нет
- Nightinale Paper 400 WordsДокумент4 страницыNightinale Paper 400 WordsAshni KandhaiОценок пока нет