Академический Документы
Профессиональный Документы
Культура Документы
93 Full
Загружено:
Yulinda PrimilisaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
93 Full
Загружено:
Yulinda PrimilisaАвторское право:
Доступные форматы
British Journal of Orthodontics/Vol.
26/1999/9396
Gingivitis ArtefactaA Case Report of a Patient Undergoing Orthodontic Treatment
R . J . S P E N C E R , B . D . S ., M . S C ., F . D . S . R . C . S ., M . O R T H . S . H A R I A , B . D . S ., M . S C ., F . D . S . R . C . S ., M . O R T H . R . D . E V A N S *, B . S C ., B . D . S ., M . S . C . D ., F . D . S . R . C . S ., M . O R T H .
Department of Orthodontics, Eastman Dental Hospital, 256 Grays Inn Road, London WC1X 8LD, UK Refereed Paper
Introduction Self-injurious behaviour (SIB) may be dened as that which results in the iniction of physical damage and, perhaps, pain upon oneself. Self-inicted injuries are not uncommon (Ayer and Levin, 1974), and range in severity from simple nail-biting to more extreme forms of mutilation, with oral trauma sometimes being the only presenting manifestation. Although the typical clinical features of oral SIB are well documented (Stewart, 1976; Blanton et al., 1977; Pattison, 1983), they often present a difcult diagnostic problem for the clinician and, even when recognized, the method of their development and their management are not clearly understood. Although many cases of self-inicted oral injuries have been reported since Neil (1958) rst reported a case involving self-mutilation of the tongue, there do not appear to be any reports of factitious oral injuries in a patient undergoing orthodontic treatment. The following case report describes gingivitis artefacta in a patient undergoing orthodontic treatment. Case Report An 11-year-old girl (L.K.) was assessed with a view to undertaking orthodontic treatment. Her medical history was uncomplicated. Her dental history, however, revealed that she had been referred to the department of paediatric dentistry at the age of 5 years, 6 months for the management of recession affecting the gingivae in the upper incisor region. At this time examination revealed that she had a healthy and intact dentition, except for an absent B|, but had severe gingival recession affecting the labial aspects of her remaining deciduous upper incisors. There were no signs of inammation or ulceration, and initial management was conservative. Follow-up a few weeks later showed that the permanent upper central incisors had erupted with a healthy gingival attachment except for an area of ulceration affecting the palatal aspect of the 1|. This lesion was thought to be traumatic in origin and SIB was suspected. The patient, however, denied this and the parents were unaware of any form of habitual trauma. This area of ulceration resolved in due course and there were no further episodes noted at her 6-monthly review appointments over the next 6 years.
*To whom correspondence should be addressed.
0301-228X/99/020000+00$02.00
Orthodontic assessment revealed that the patient presented in the permanent dentition with a Class I incisor relationship on a mild Skeletal III base. The 2| was absent with 3| and 1| in contact. There was a 3-mm midline diastema, and the buccal segment relationship was Class I on the left and Class II on the right. There was a left-sided unilateral crossbite, but no functional displacement. Radiographs conrmed the absence of 2| and all four third molars (Figure 1). It was decided to recreate the space for the absent 2|. Treatment was started with a removable appliance incorporating an expansion screw to simultaneously correct the crossbite and distalize 654|, supported with combination pull headgear. Compliance was good and treatment progressed uneventfully. Subsequently, a Quad-helix was tted to continue the upper arch expansion. This was used in conjunction with upper and lower pre-adjusted Edgewise xed appliances to localize space for the absent 2| and detail the occlusion. Three months after the placement of the xed appliances, a saucer-shaped area of ulceration affecting the labial gingival margin of the 1| was observed, which appeared to be traumatic in origin (Figure 2). Upon questioning, the patient readily admitted traumatizing her gingivae with her ngernail, and claimed that ever since the xed appliances had been tted she had an itchy feeling in the area involved and had an uncontrollable urge to scratch the area to gain some relief. The area of ulceration was shown to the patient. Her parents were also made aware of the problem and instructed to intercept any signs that she was continuing this habit. At review, 1 month later, it was noted that she had diverted her attention to the |2, where there was a keyholeshaped lesion at the gingival margin with some associated recession (Figure 3). The patient was, again, shown the damage she was causing and requested to stop. During this appointment, space opening was commenced between the 1| and 3| to allow for the replacement of 2|. At review 4 weeks later, the gingival tissues around the |2 had healed, albeit with some localized recession, but the patient continued to display SIB and was now damaging the area around the distal aspect of the 1| (Figure 4). This area had been attacked more vigorously than the other areas and there it was seen that 3 mm of cementum had been exposed. Advice was sought from the Department of Periodontology, and the patient was advised to carefully clean around this area with Corsodyl gel and to try wearing
1999 British Orthodontic Society
94
R. J. Spencer et al.
Clinical Section
BJO Vol 26 No. 2
(a) FIG. 1 Pretreatment photograph.
(b)
(c)
FIG. 2
Lesion 1|.
FIG. 5
Lesion 1| at the time of removal of xed appliances.
FIG. 3
Lesion |2.
FIG. 6
Patient after placement of resin retained bridge 2|.
FIG. 4
Initial lesion 1|.
(Figure 6). When the patient attended for the adjustment of her retainers she was not only traumatizing the 1|, but also the |1. Later during the retention period, her attention turned to the 3| and the patient admitted that this was occurring during school lessons. The fact that these episodes had continued well into the retention period, when no active tooth movement was being undertaken, meant that it was felt that this behaviour was perhaps more deep-seated than originally thought. However, an assessment with a clinical psychologist was declined and at the next review, 3 months later, the trauma was seen to have stopped. The patient is still under long-term review.
gloves to bed in an attempt to stop this habit. The push coil in place (31|) was not reactivated in an attempt to minimize the forces acting on this tooth, in case this was the aggravating factor. Despite this, over subsequent appointments, the recession around this tooth worsened (Figure 5) and this was associated with a degree of sensitivity, which only served to perpetuate the situation. Following xed appliance removal, an upper removable retainer was tted to maintain the space for the 2|. After 4 months, a resin-bonded bridge was tted to replace the absent 2|, but due to poor communication, the patient did not re-attend to have her retainer adjusted, which allowed some relapse of the rotation previously affecting the |1
Discussion A review of the literature reveals that self-inicted oral injuries are not uncommon and since the late 1950s there have been more than 55 reported cases. Although the gingivae is the most commonly targeted tissue, no structure in the oral cavity is immune from the effects of this type of behaviour. Amongst the more extreme examples reported are auto-extraction (Plesset, 1959; Altom and DiAngelis, 1989) and a fractured mandible (Goldstein and Dragon, 1967). Oral self-mutilation is a well recognized feature of
BJO June 1999
Clinical Section
Gingivitis Artefacta
95
certain neurological conditions, most notably Lesch Nyhan Syndrome, but also De Georges Syndrome, autism, and congenital indifference to pain (LaBanc and Epker, 1981) Most case reports suggest that the method of producing injury is by picking or scratching the tissues with ngers or ngernails. Other objects have also been reported to have been used including knives, toothpicks, and even hair (Golden and Chosak, 1964; Blanton et al., 1977; Groves, 1979), although this case appears to be the rst where this type of behaviour has been diagnosed in a patient undergoing orthodontic treatment. In the case reported by Beckett et al. (1995), although the habit was apparently active during orthodontic treatment, this was not recognized until some time after treatment had been completed. Stewart (1976) has divided self-injurious behaviour affecting the gingival tissues into gingivitis artefacta minor and major. Gingivitis artefacta minor was recognized as being more common and thought to be provoked by a preexisting locus of irritation. In this form, the habit was claimed to respond readily to simple treatment that removed the underlying source of irritation. In contrast, the injuries suffered in gingivitis artefacta major were said to be more widespread, so that several areas of the mouth could be affected simultaneously. This type of behaviour also differed in being more resistant to conventional forms of treatment and was probably associated with an emotional disorder. In the present case, it seems almost certain that the gingival recession noted when the patient was 5 years old was the result of self-inicted trauma. Stewart (1976) has previously reported gingivitis artefacta associated with exfoliating primary teeth and found that the habit ceased once the offending tooth had been removed, presumably indicating that the exfoliating tooth was the source of irritation that triggers the traumatic habit. This rst episode of self-injury ceased with the eruption of the permanent incisors. Upon the placement of xed orthodontic appliances, however, the patient resumed the habit. She claimed that her gums felt itchy and she therefore scratched them to obtain some relief, a description previously reported by other authors (Golden and Chosack, 1964; Hasler and Schultz, 1968). She eventually concentrated her efforts on the gingival margin at the distal aspect of the 1|, where a signicant amount of orthodontic tooth movement was occurring to open space for the replacement of the absent lateral incisor. It may therefore be reasonable to hypothesis that the orthodontic forces acted as a source of irritation which led to the re-establishment of her SIB. In the case reported by Beckett et al. (1995) the patient had the habit of inserting the sharp end of a pin into the gingival crevice on the palatal aspect of an upper incisor tooth during orthodontic treatment and it is therefore possible that orthodontic treatment may act as trigger to this sort of behaviour in susceptible patients. Should a patient demonstrate such behaviour, the orthodontist is faced with a difcult problem not normally encountered during other types of conventional dental treatment. The clinician must weigh up the advantages of completing treatment with the potential disadvantages of abandoning treatment midway and so lessening any impact of SIB. If it is decided to continue treatment, there is also a
dilemma between the need for regular appointments for appliance adjustments and the need to almost ignore SIB. It is believed that patients exhibiting SIB crave attention and the regular visits necessary for appliance adjustments may only serve to reinforce the pattern of behaviour (Ayer and Levin, 1974; Rodd, 1995). In the case presented here, the initial gingival recession associated with the exfoliating deciduous incisors was localized and resolved once the teeth were shed naturally, and so may reasonably have been classied as a case of gingivitis artefacta minor. When the condition reappeared, many factors pointed to this also being another episode of gingivitis artefacta minor. The lesions were known to be of traumatic origin, were associated with a locus of irritation, and did not appear simultaneously. However, the fact that the lesions varied in location and continued to appear after orthodontics had ceased, and that the condition had reappeared some 6 years after the rst episode, suggests that this type of behaviour is perhaps deeply entrenched, and may be a case of gingivitis artefacta major. It is therefore difcult to denitely classify this patients condition as either gingivitis artefacta minor or major at this time, and the patient will therefore be kept under long-term review to monitor her for any further signs of similar behaviour. Despite the fact that the chance to be referred to a clinical psychologist was refused, it is not the role of the clinician to try and explore the reasons for such behaviour as they do not have the necessary training or skills (Rodd, 1995).
References
Altom, R. L. and DiAngelis, A. J. (1989) Multiple autoextractions: oral self mutilation reviewed, Oral Surgery Oral Medicine Oral Pathology, 67, 271274. Ayer, A. A. and Levin, M. P. (1974) Self-mutilating behaviours involving the oral cavity, Journal of Oral Medicine, 29, 47. Beckett, H., Buxey-Softley, G. and Gilmour, G. A. (1995) Self-inicted gingival injury (letter), British Dental Journal, 178, 246. Blanton, P. L., Hurt, W. C. and Largent, M. D. (1977) Oral factitious injuries, Journal of Periodontology, 48, 3337. Golden, S. and Chosack, A. (1964) Oral manifestations of an psychological problem, Journal of Periodontology, 35, 349350. Goldstein, I. C. and Dragon, A. I. (1967) Self-inicted oral mutilation in a psychotic adolescent: report of a case, Journal of the American Dental Association, 74, 750751. Groves, B. J. (1979) Self-inicted periodontal injury, British Dental Journal, 147, 244246. Hasler, J. F. and Schultz, W. F. (1968) Factitial gingival traumatism, Journal of Periodontology, 39, 362363. LaBanc, J. and Epker, B. N. (1981) LeschNyhan Syndrome: surgical treatment in a case of lip chewing, Journal of Maxillofacial Surgery, 9, 6467. Neil, J. G. (1958) Self-mutilation of the tongue, Journal of Laryngology and Otology, 72, 947950. Pattison, G. L. (1983) Self-inicted gingival injuries: literature review and case report, Journal of Periodontology, 54, 299304.
96
R. J. Spencer et al.
Clinical Section
BJO Vol 26 No. 2
Plessett, D. N. (1959) Autoextraction, Oral Surgery Oral Medicine Oral Pathology, 12, 302303. Rodd, H. D. (1995) Self-inicted gingival injury in a young girl, British Dental Journal, 178, 2830.
Stewart, D. J. (1976) Minor self-inicted injuries to the gingivae, gingivitis artefacta minor, Journal of Clinical Periodontology, 3, 128132.
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Cracked Mirror, Karen KernbergДокумент10 страницThe Cracked Mirror, Karen Kernbergjuaromer100% (1)
- William S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Документ425 страницWilliam S. Breitbart - Meaning-Centered Psychotherapy in The Cancer Setting - Finding Meaning and Hope in The Face of Suffering (2017, Oxford University Press)Nicole Marie-Madeleine Alberto100% (2)
- University of The PhilppinesДокумент22 страницыUniversity of The PhilppinesFibi Pho0% (1)
- Cofer Pedoman UKMДокумент1 страницаCofer Pedoman UKMYulinda PrimilisaОценок пока нет
- Cause N Timing Delay BleedДокумент8 страницCause N Timing Delay BleedYulinda PrimilisaОценок пока нет
- Case Report Orto YP PDFДокумент6 страницCase Report Orto YP PDFYulinda PrimilisaОценок пока нет
- Tooth Ankylosis Follow UpДокумент6 страницTooth Ankylosis Follow UpYulinda PrimilisaОценок пока нет
- Clinical Dexa N TriamsinolonДокумент11 страницClinical Dexa N TriamsinolonYulinda PrimilisaОценок пока нет
- Guideline On Pediatric Oral SurgeryДокумент9 страницGuideline On Pediatric Oral SurgeryYulinda PrimilisaОценок пока нет
- Paradental CystДокумент7 страницParadental CystYulinda PrimilisaОценок пока нет
- Aging and The Periodontium: L-1 Blok STSДокумент10 страницAging and The Periodontium: L-1 Blok STSYulinda PrimilisaОценок пока нет
- 89 OmДокумент18 страниц89 OmFibrianti SeputriОценок пока нет
- An Assesment of Efectiveness EssixДокумент9 страницAn Assesment of Efectiveness EssixYulinda PrimilisaОценок пока нет
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Документ7 страницP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Yulinda PrimilisaОценок пока нет
- Class III Twin Blocks: A Case Series: Clinical SectionДокумент6 страницClass III Twin Blocks: A Case Series: Clinical SectionYulinda PrimilisaОценок пока нет
- Restoring Function and Esthetics in 2 Patients With Amelogenesis Imperfecta: Case ReportДокумент0 страницRestoring Function and Esthetics in 2 Patients With Amelogenesis Imperfecta: Case ReportYulinda PrimilisaОценок пока нет
- A Prospective Study of Cantilever Resin-Bonded Bridges: An Intial Repor TДокумент0 страницA Prospective Study of Cantilever Resin-Bonded Bridges: An Intial Repor TYulinda PrimilisaОценок пока нет
- Desquamatis GraftДокумент4 страницыDesquamatis GraftYulinda PrimilisaОценок пока нет
- 2012 KevinSextonMay2 BC Wound HealingДокумент40 страниц2012 KevinSextonMay2 BC Wound HealingYulinda PrimilisaОценок пока нет
- NecrosisДокумент41 страницаNecrosisYulinda PrimilisaОценок пока нет
- Static SpaceДокумент1 страницаStatic SpaceYulinda PrimilisaОценок пока нет
- Mikroabrasi Hidrokolid Dan Fosforik AsidДокумент13 страницMikroabrasi Hidrokolid Dan Fosforik AsidYulinda PrimilisaОценок пока нет
- Odontopediatria RestaurativaДокумент9 страницOdontopediatria RestaurativaAle DuarteОценок пока нет
- Dens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationДокумент4 страницыDens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationYulinda PrimilisaОценок пока нет
- IHS DentSpecResGuideCh10Документ71 страницаIHS DentSpecResGuideCh10Yulinda PrimilisaОценок пока нет
- Dens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationДокумент4 страницыDens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationYulinda PrimilisaОценок пока нет
- Dens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationДокумент4 страницыDens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationYulinda PrimilisaОценок пока нет
- Dens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationДокумент4 страницыDens Invaginatus, Clinically As Talons Cusp: An Uncommon PresentationYulinda PrimilisaОценок пока нет
- Dens EvaginatusДокумент32 страницыDens EvaginatusYulinda PrimilisaОценок пока нет
- Dr. Neeraj AgrawalДокумент4 страницыDr. Neeraj AgrawalYulinda PrimilisaОценок пока нет
- Down Screen Proposal For Health Screen at Thyrocare AmitДокумент19 страницDown Screen Proposal For Health Screen at Thyrocare AmitSwatiSuranaОценок пока нет
- Case Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)Документ4 страницыCase Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)john dave rougel ManzanoОценок пока нет
- Gynera: Coated TabletsДокумент67 страницGynera: Coated TabletsOdeke VascoОценок пока нет
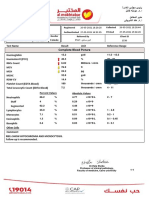
- Complete Blood Picture: 60 Year Female 23321506381Документ3 страницыComplete Blood Picture: 60 Year Female 23321506381SilavioОценок пока нет
- Tabel Severitas BPJS Tindakan JantungДокумент9 страницTabel Severitas BPJS Tindakan JantungTeduh ParamadinaОценок пока нет
- MBF7823423Документ425 страницMBF7823423Pete PetersОценок пока нет
- Corticosteroids 24613Документ33 страницыCorticosteroids 24613NOorulain HyderОценок пока нет
- Mock Congress Bill Research EssayДокумент9 страницMock Congress Bill Research Essayapi-302890064Оценок пока нет
- Surgery 37: Recent Advances inДокумент226 страницSurgery 37: Recent Advances inmudasir61Оценок пока нет
- Hip Resurfacing Expectations and LimitationsДокумент4 страницыHip Resurfacing Expectations and LimitationsCristian BenayОценок пока нет
- A Detailed Lesson Plan in Living ThingsДокумент23 страницыA Detailed Lesson Plan in Living ThingsclarisseОценок пока нет
- Question 1Документ87 страницQuestion 1hemihemaОценок пока нет
- Nurs 3020 Midterm EvaluationДокумент8 страницNurs 3020 Midterm Evaluationapi-372418362Оценок пока нет
- Kedaruratan THT I: Dr. Sri Utami Wulandari, SPTHT-KLДокумент24 страницыKedaruratan THT I: Dr. Sri Utami Wulandari, SPTHT-KLEvi Liana BahriahОценок пока нет
- Hemorrhagic Disease of The NewbornДокумент3 страницыHemorrhagic Disease of The NewbornDevi SuryandariОценок пока нет
- Resilient Health Care (2013)Документ297 страницResilient Health Care (2013)Pepi RamosОценок пока нет
- HipoglikemiaДокумент13 страницHipoglikemiaRC Ria Chairul100% (1)
- Report On Januvia DrugДокумент10 страницReport On Januvia DrugyogenaОценок пока нет
- Cytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesДокумент21 страницаCytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesIndah WahyuningtyasОценок пока нет
- Las - Mapeh - Health Module 1Документ5 страницLas - Mapeh - Health Module 1Analiza SantosОценок пока нет
- Acute Renal FailureДокумент1 страницаAcute Renal FailureSonia Letran Singson100% (1)
- Our Lady of Fatima University College of Nursing - Cabanatuan CityДокумент3 страницыOur Lady of Fatima University College of Nursing - Cabanatuan CityDanica FrancoОценок пока нет
- Introduction To Cerebral Palsy 2022Документ53 страницыIntroduction To Cerebral Palsy 2022Namakau MuliloОценок пока нет
- Organizing Patient CareДокумент16 страницOrganizing Patient CareDian Rosdiana100% (1)
- Pelayanan PaliatifДокумент43 страницыPelayanan PaliatifBety RindaОценок пока нет
- Pediatrics PDFДокумент33 страницыPediatrics PDFChellapandyaОценок пока нет
- M5L1 PPT Personal WellnessДокумент20 страницM5L1 PPT Personal WellnessWasif AzizОценок пока нет