Академический Документы
Профессиональный Документы
Культура Документы
Intraocular Pressure in An American Community: The Deover Dom Eye Study
Загружено:
Angkat Prasetya Abdi NegaraИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Intraocular Pressure in An American Community: The Deover Dom Eye Study
Загружено:
Angkat Prasetya Abdi NegaraАвторское право:
Доступные форматы
Investigative Ophthalmology & Visual Science, Vol. 33, No.
7, June 1992
Copyright Association for Research in Vision and Ophthalmology
Intraocular Pressure in an American Community
The Deover Dom Eye Study
Barbara E. K. Klein, Ronald Klein, and Karhryn L. P. Linron
The Beaver Dam Eye Study is a population-based study of age-related eye diseases in persons 43-86 yr of age. Applanation tonometry was done on all study subjects. Mean intraocular pressure (IOP) increased significantly with age. Mean IOP differed little between the sexes and was not significantly different after age adjustment (in right eyes of 2721 women, it was 15.5 mm Hg, and in right eyes of 2135 men, it was 15.3 mm Hg). There was an association of IOP with systolic and diastolic blood pressures, body mass index, hematocrit, serum glucose, glycohemoglobin, cholesterol level, pulse, nuclear sclerosis, season, and time of day of measurement. These data confirm that, in a general population, IOP is associated with important systemic and ocular characteristics. Those characteristics should be considered in further research on determinants of IOP. Invest Ophthalmol Vis Sci 33:2224-2228, 1992
Intraocular pressure (IOP) is an inherent physiologic characteristic of importance in maintaining structure and function of the eye. Correlates of this measurement include other important physiologic parameters that may need to be considered in investigating determinants of IOP. Because IOP is the ocular parameter that is associated most commonly with glaucoma,1"4 it may be important to evaluate these physiologic correlates of IOP; they may confound relationships between IOP and glaucoma. We briefly describe the distribution of IOP and investigate its correlates in the population participating in the Beaver Dam Eye Study. Materials and Methods A private census of Beaver Dam was done, and the procedures have been published elsewhere.5 In brief, 6612 households were identified, of which 3715 had at least one occupant 43-84 yr of age. Thereafter, each individual in the target age range was contacted for a study appointment. Three subjects were examined whose age was 86 yr at the time of testing. Their data are included in this report. Of the total of 5925
From the Department of Ophthalmology, University of Wisconsin Madison, Madison, Wisconsin. Supported by National Institutes of Health (Bethesda, Maryland) grant 5U10 EY 10 6594 (RK and BEKK). Presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Sarasota, Florida, April 28 to May 3, 1991. Submitted for publication: October 2, 1991; accepted December 21, 1991. Reprint requests: Barbara E. K. Klein, MD, MPH, Department of Ophthalmology, 600 Highland Avenue, Madison, WI 53792.
persons in the target age range, 4926 were evaluated (83.14%). Relevant parts of the study evaluation included the date of birth and a history of ocular trauma, surgery, medications, glaucoma, and diabetes. Most of the participants were white (99.4%). Blood pressure was measured according to the Hypertension Detection and Follow-up Program protocol.6 Height and weight were measured with a Health-o-Meter scale (Continental Scale Corp., Bridgewater, IL). The IOP was measured with a Goldmann applanation tonometer. A drop of Fluress (Armour, Kankakee, IL) was instilled in each eye. The tonometer was set at 10. The measurement was taken as the examiner viewed the mires through the prism. When the end point was reached, the examiner moved the slit lamp away from the eye and recorded the reading. The procedure was repeated for the other eye. The time of measurement was recorded. Iris pigmentation was evaluated and compared with three standard color 35-mm slides. The protocol specifies categories of pigmentation from a lightly pigmented iris (blue) through a heavily pigmented one (brown).7 After assessing anterior chamber depth, the pupils were dilated with one drop each of tropicamide 1% and phenylephrine 2.5%. When the pupils were dilated, a clinical assessment of the presence and severity of cataract was made, and photographs were taken with the illuminating beam at 45 to the viewing system.7 These photographs subsequently were graded by comparison with standard photographs according to the protocol.7 A blood specimen was obtained, and glucose and glycosylated hemoglobin were measured. The subjects were classified as having no diabetes if there was a negative history of
2224
No. 7
INTRAOCULAR PRESSURES IN DEAVER DAM / Klein er ol
2225
diabetes, blood glucose was less than 200 mg/dl, and glycosylated hemoglobin was within two standard deviations of the mean for the particular age-sex subgroup. Informed consent was obtained for each subject. We used the Statistical Analysis System (SAS, Cary, NC) to analyze the data.8 Because the distribution of IOP does not differ from normality, parametric tests were chosen where applicable. Univariate associations with IOP were detected by Student's t-test, and analysis of variance techniques were used for categoric factors, with Pearson correlation coefficients for continuous factors. Confidence intervals for the correlation coefficients were calculated using the method developed by Fisher.9 Results There was little difference between the mean IOP of right and left eyes (0.14 2.11 m m Hg) or their association s with other variables. Therefore, data for right eyes only are presented. The distribution of IOP in the right eye by sex and age is given in Table 1. There was a small but significant change in mean IOP with increasing age (P < 0.05). We found IOP greater than 21 mm Hg to be more frequent in older age groups (P < 0.01, by test for trends). Women had higher mean IOP than did men, but the difference was not great and was only borderline significant (P = 0.06) when adjusted for age (by multiple-linear regression). During the interview, the participants were asked whether they had glaucoma or were receiving medication for this disease. The mean IOP was significantly higher (20.1 mm Hg) in those with a positive compared with a negative history (15.3 mm Hg).
We investigated the relationship between nuclear sclerosis and IOP (Table 2). There was a significant trend of increasing IOP with increasing severity of nuclear sclerosis. In those eyes that were either aphakic or had intraocular lens implants, the mean IOP was between the mean for those eyes in thefirsttwo categories of severity of nuclear sclerosis (Table 2). A history of other eye surgery or trauma was not associated with increased mean IOP. The participants were categorized as to definite, possible, or no history of diabetes. There was a significant difference between the IOP means among these groups (Table 2). There also was a seasonal effect on IOP; measurements during the summer months (July, August, and September) were significantly lower (15.2 mm Hg) than those during the winter months (January, March, and April; 15.7 mm Hg). There was no significant effect of iris color, refractive error, cigarette smoking, or alcohol consumption on IOP. A history of cardiovascular disease was not related to IOP. Table 3 describes the multiple linear-regression analysis for the variables significantly associated with IOP. Data for persons who reported receiving medicine for glaucoma or who had had surgery for glaucoma were excluded from this analysis. Systolic blood pressure, time of day of examination, body mass index, glaucoma history, refractive error, cholesterol level, hematocrit, female sex, month of examination, pulse rate, severity of nuclear sclerosis, diastolic blood pressure, and glycosylated hemoglobin were all selected in the stepwise analysis. Age did not enter as a significant factor when considered with the other variables.
Table 1. Percent distribution of intraocular pressure in right eyes by age and sex
IOP (mm Hg) Age (years) 43-49 50-54 55-59 60-64 65-69 70-74 75-79 80-86 TOTAL Sex F M F M F M F M F M F M F M F M F M N 448 385 340 327 347 287 348 325 391 299 340 233 276 168 231 111 2721 2135 0-12 21.9 22.9 21.8 24.2 23.6 16.4 17.8 15.1 12.5 20.1 15.3 15.9 16.3 19.6 18.2 22.5 18.5 19.6 13-15 35.5 37.4 33.2 39.1 29.4 40.8 28.5 32.9 29.4 32.4 32.7 36.1 31.2 30.4 36.8 31.5 32.0 35.4 16-18 32.6 31.2 32.4 24.2 34.9 27.2 38.2 36.0 39.4 30.8 32.9 31.8 31.5 32.7 29.4 33.3 34.2 30.5 19-21 6.9 6.2
9.7 9.5 7.5
22-24 2.7 1.3 2.7 2.1 4.3 2.4 3.2 4.0 4.9 4.7 3.5 5.6 6.2 6.0 3.5 2.7 3.8 3.4
25+ 0.5 1.0 0.3 0.9 0.3
1.1
Mean 15.0 14.7 15.1 14.9 15.1 15.4 15.6 15.8 16.0 15.4 15.9 15.6 15.9 15.8 15.5 14.9 15.5 15.3
SD 2.9 3.1 3.0 3.3 3.2 3.4 3.1 3.3 3.4 3.4 3.3 3.3 3.6 4.2 3.6 3.9 3.3 3.4
12.2 11.8 10.5 12.3 11.4 14.7 10.3 13.4 9.5 9.5 9.0 10.6 9.7
0.6 1.5 1.5 0.7 0.9 0.4 1.5 1.8 2.6 0.9 0.9 1.0
Twenty-seven "unreliable" and 43 "not obtainable" excluded from the analyses.
2226
INVESTIGATIVE OPHTHALMOLOGY & VISUAL SCIENCE / June 1992
Vol. 33
Table 2. Mean intraocular pressure in right eyes by subject characteristics
Variable Nuclear sclerosis <Stdl <Std2 <Std3 <Std4 >Std4 GC Aphakic or IOL Glaucoma Hx No Yes Diabetes status No Hx, but no meds/symptom Yes Trends test. N 847 1790 1251 625 25 64 258 4743 113 4418 55 383 Mean (mm Hg) 15.0 15.2 15.7 15.9 16.0 16.5 15.1 15.3 20.1 15.3 16.1 16.0 SD 3.0 3.2 3.3 3.7 3.3 3.8
3.9
J
P value*
<0.0001
3.2 1 4.4 3.3 1 4.0
<0.0001
0.0003
3.6 J
Discussion The Beaver Dam Eye Study is a current large population-based study in American adults. It provides information about ocular and systemic parameters. Thus, it is possible to evaluate independent relationships of other physiologic features with IOP. In the future, such data will provide the opportunity to determine whether the other characteristics also influence or confound the relationship of IOP to disease (eg, glaucoma, altered retinal sensitivity, and decreased contrast sensitivity). There was a small positive relationship of age and IOP in the adults in Beaver Dam, Wisconsin. Positive correlations of age and IOP in America and Europe have been reported in most studies of this relationship.10"16 Both black and white Americans participated in the Health and Nutrition Examination Survey. A positive relationship was found in both groups. A negative association between these variables was seen in Japanese studies.1718 Whether this difference is related directly to specific ocular characteristics that
differ between ethnic groups o mental effect is not known. Eye color was defined according to a scale of increasing pigmentation in the Beaver Dam Eye Study. Standard 35-mm slide photographs were used by the examiner for comparison with the subject's iris. No relationship was seen between the degree of pigmentation and IOP. Although pigmentary glaucoma may be related to mechanical obstruction from pigment in the trabeculum, there is no evidence in these analyses to suggest that iris pigment plays a role in the height of the IOP level in the absence of characteristics of pigmentary glaucoma. Others reported an effect of iris color on IOP.19 The difference between our findings and theirs may reflect differences in ethnicity between the study populations or chance. The severity of nuclear sclerosis was based on gradings of slit-lamp photographs according to the study protocol.7'20 It was correlated with a higher mean IOP. The finding that mean IOP in aphakic eyes or those with lens implants was similar to that found in those with less severe nuclear sclerosis is compatible with
Table 3. Multiple regression analysis for intraocular pressure in right eyes
Variable
Coefficient 0.019 -0.001 3.883 8.791 -0.107 0.004 0.075 0.473 -0.053 0.019 0.172 0.018 0.074
P value 0.0001 0.0001 0.0001 0.0001 0.0001 0.0007 0.0001 0.0001 0.0002 0.0157 0.0016 0.0014 0.0162
Partial R2 0.039 0.024 0.007 0.006 0.006 0.005 0.004 0.005 0.003 0.002 0.002 0.002 0.001
Total R2
Systolic blood pressure (mm Hg) Time of day of exam (hr) Body mass index Glaucoma history (yes/no) Refractive error (diopters) Cholesterol (mg/dl) Hematocrit (mm) Sex (F) Month of exam (1-12) Pulse (beats/min) Nuclear sclerosis Diastolic blood pressure (mm Hg) Glycosylated hemoglobin (%)
0.104
No. 7
INTRAOCULAR PRESSURES IN DEAVER DAM / Klein er ol
2227
the hypothesis that there is a mechanical effect if a larger lens compromises aqueous outflow; this would be relieved by lens removal. Such an interpretation was suggested by some authors who observed amelioration of phacomorphic glaucoma after cataract surgery.21 An alternative explanation may be that cataract surgery influences the aqueous physiology and leads to lower IOP. A history of diabetes and medications to lower blood sugar was elicited during the study interview. Those who said they had diabetes or were suspected of having it had a significantly higher mean IOP than those without diabetes. The IOP among the study participants in the Wisconsin Epidemiologic Study of Diabetic Retinopathy were slightly higher than the mean of a nondiabetic comparison group evaluated at the same time.13 Other investigators have found an increased frequency of elevated IOP in people with diabetes.2223 Although a physiologic explanation is unclear, the health care implication is that persons with diabetes may be at increased risk of glaucoma, and ophthalmologists who follow such persons should be evaluating the patient for the possible development of glaucoma. Other systemic factors may influence IOP. Blood pressure has been found in several studies to be associated significantly with 1OP.121319-31 There may be a direct effect of systolic blood pressure on ultrafiltration and, through this mechanism, on IOP.1827 Body mass index, a measure of obesity, was correlated positively with IOP. Others found a similar relationship of obesity with IOP.25 Because corticosteroid secretion is increased in obese persons, this may explain this relationship.30 Mechanically, it has been suggested that orbital pressure from excess fat may cause a rise in episcleral venous pressure and decreased outflow facility.18*27 Diurnal IOP variation could not be assessed in our study; the participants only underwent one study examination. The time of the appointment depended only on scheduling concerns. Nevertheless, a pattern emerged of mean IOP tending to be higher earlier in the day. This finding was compatible with the report on the Bedford Glaucoma Survey;32 positive screenings for glaucoma were more likely to occur in the morning. This relationship has important implications for those who treat people with glaucoma and who tailor this treatment to the IOP level. The pulse rate was found to be correlated to IOP in earlier studies.12-27 An association of IOP with cholesterol level also was reported previously.12-30 In addition, we found hematocrit was significantly related to IOP; similarly, hemoglobin and erythrocyte count were associated with IOP in another study.25 The biologic importance of the association of these cardiovas-
cular risk variables with IOP is unclear, but they appear to be more universal than just an ethnic variation. Seasonal variations were reported by others,28'33 with slightly higher pressures found in the winter months. We found a similar pattern in Beaver Dam. From these earlier studies, we might question whether this represents a response of people from a northern European ethnic background or is related to the northern latitudes. However, one of these studies was conducted in Israel.34 The seasonality may be related to the light, temperature, and humidity changes. There are other annual rhythms affecting physiologic systems.33 The variation in IOP may be a result of these other physiologic changes or may be intrinsic to the regulatory systems in the eye. The relationships reported emphasize the physiologic interdependence of the eye with other organ systems. These relationships and the influence of external environmental conditions indicate that these too must be considered when studying IOP and its relationship to eye disease. Key words: intraocular pressure, epidemiology, Beaver Dam Eye Study, age-related eye diseases Acknowledgments
The authors thank the community of Beaver Dam, Wisconsin, and their health care providers for their enthusiastic cooperation throughout all phases of the study; Moneen Meuer and Sarah Baumgart for project coordination; Stacy Meuer for photograph management; Barbara Houser for data management; Ann Varda, Anik Ganguly, and Karl Jensen for programming and computing; Yvonne M. Bellay, Dayna S. Dalton, Norma Dorn, Kathy Peterson, and Kathryn Burke for examining all subjects; Michael Neider for photography training and equipment design; Carol Hoyer, Deborah Reiderer, Maria Swift, and A. Jeffrey Whitehead for photograph grading; Helen Soldner for reception; David L. DeMets for statistical advice; and Julie K. Olson, Kristine A. Tway, and Luann Soule for manuscript preparation.
References
1. Kolker AE and Hetherington Jr, editors: Becker-Shaffer's Diagnosis and Therapy of the Glaucomas, 5th ed. St. Louis, CVMosby, 1983, p. 59. 2. Leske MC: The epidemiology of open-angle glaucoma: A review. Am J Epidemiol 118:166, 1983. 3. Armaly MF, Krueger DE, Maunder L, et al: Biostatistical analysis of the collaborative glaucoma study: I. Summary report of theriskfactors for glaucomatous visualfielddefects. Arch Ophthalmol 98:2163, 1980. 4. Sommer A: Intraocular pressure and glaucoma. Am J Ophthalmol 107:186, 1989. 5. Campbell JA and Palit CD: Total digit dialing for a small area census by phone. In Proceedings of the Section on Survey Research Methods. Alexandria, VA, American Statistical Association, 1988, pp. 549-551. 6. Hypertension Detection and Follow-up Program Cooperative
2228
INVESTIGATIVE OPHTHALMOLOGY & VISUAL SCIENCE / June 1992
Vol. 33
7.
8. 9. 10. 11.
12. 13. 14. 15.
16. 17. 18.
19. 20.
Group. The hypertension detection and follow-up program. Prev Med 5:207, 1976. Klein BEK, Magli, YL, Neider MW, and Klein R: Wisconsin System for Classification of Cataracts from Photographs. Springfield, VA, National Technical Information Service. NTIS Accession No. PB90-138306, 1990, pp. 1-22. SAS Institute: SAS User's Guide: Statistics, version 5. Cary, NC, SAS Institute, 1985, pp. 403-506, 795-800. Snedecor GE and Cochran WG. Statistical Methods, 6th ed. Ames, I A, Iowa University Press, 1979, p. 185. Graham P: Epidemiology of simple glaucoma and ocular hypertension. Br J Ophthalmol 56:223, 1972. Hollows FC and Graham PA: Intraocular pressure, glaucoma and glaucoma suspects in a defined population. Br J Ophthalmol 50:570, 1966. Klein BEK and Klein R: Intraocular pressure and cardiovascular risk variables. Arch Ophthalmol 99:837, 1981. Klein BEK, Klein R, and Moss SE: Intraocular pressure in diabetic persons. Ophthalmology 91:1356, 1984. Seddon JM, Schwartz B, and Flowerdew G: Case-control study of ocular hypertension. Arch Ophthalmol 101:891, 1983. Goedbloed J, Schappert-Kimmijser J, Donders PC, et al: Frequency distribution of the intraocular pressure in the Netherlands. Ophthalmologica 141:481, 1961. Armaly MF: On the distribution of applanation pressure in the normal eye. Arch Ophthalmol 78:187, 1967. Kurokawa M: Studies on the normal intraocular pressure. Nippon Ganka Gakkai Zasshi 73:112, 1969. Shiose Y and Kawase Y: A new approach to stratified normal intraocular pressure in a general population. Am J Ophthalmol 101:714, 1986. Hiller R, Sperduto RD, and Krueger DE: Race, iris pigmentation, and intraocular pressure. Am J Epidemiol 115:674, 1982. Klein BEK, Klein R, Linton KLP, et al: Assessment of cataracts from photographs in the Beaver Dam Eye Study. Ophthalmology 97:1428, 1990.
21. Jaffe NS, Jaffe MS, and Jaffe GF: Cataract Surgery and Its Implications, 5th ed. St. Louis, CV Mosby, 1990, pp. 385-411. 22. Traisman HS, Alfano JE, Andrews J, and Gatti R: Intraocular pressure in juvenile diabetics. Am J Ophthalmol 64:1149, 1967. 23. Carel RS, Korczyn AD, Rock M, et al: Association between ocular pressures and health parameters. Ophthalmology 91:311, 1984. 24. Christiansson J: Intraocular pressure in diabetes mellitus. Acta Ophthalmol (Copenh) 39:155, 1961. 25. Shiose Y: The aging effect on intraocular pressure in an apparently normal population. Arch Ophthalmol 102:883, 1984. 26. Leske MC and Podgor MJ: Intraocular pressure: Cardiovascular risk variables and visual field defects. Am J Epidemiol 118:280, 1983. 27. Bulpitt CJ, Hodes C, and Everitt MG: Intraocular pressure and systemic blood pressure in the elderly. Br J Ophthalmol 59:717, 1975. 28. Bengtsson B: Some factors affecting the distribution of intraocular pressure in a population. Acta Ophthalmol (Copenh) 50:33, 1972. 29. McLeod SD, West SK, Quigley HA, and Fozard JL: A longitudinal study of the relationship between intraocular and blood pressure. Invest Ophthalmol Vis Sci 31:2361, 1990. 30. Schteingart DE: Characteristics of increased adrenocortical function observed in many obese persons. Ann N Y Acad Sci 131:388, 1965. 31. Kahn LA, Leibowitz HM, Ganley JP, et al: The Framingham Eye Study: 2. Association of ophthalmic pathology with single variables previously measured in the Framingham Heart Study. Am J Epidemiol 106:33, 1977. 32. Perkins ES: The Bedford Glaucoma Survey II: Rescreening of normal population. Br J Ophthalmol 57:186, 1973. 33. Blumenthal M, Blumenthal R, Peritz E, and Best M: Seasonal variation in intraocular pressure. Am J Ophthalmol 69:608, 1970.
Вам также может понравиться
- Biophysical Properties in Glaucoma: Diagnostic TechnologiesОт EverandBiophysical Properties in Glaucoma: Diagnostic TechnologiesIngrida JanulevicieneОценок пока нет
- What Is NTGДокумент4 страницыWhat Is NTGSonia RogersОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)От EverandComplementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)Оценок пока нет
- BR J Ophthalmol 2005 Hashemi 652 7Документ7 страницBR J Ophthalmol 2005 Hashemi 652 7masmedicaОценок пока нет
- AssociationsДокумент8 страницAssociationsSelfima PratiwiОценок пока нет
- Retinopathy DiabeticДокумент5 страницRetinopathy DiabeticMagnaОценок пока нет
- The Prevalence of OpenДокумент17 страницThe Prevalence of OpenShaney_flОценок пока нет
- Jurnal HighlightДокумент4 страницыJurnal HighlightStrangersОценок пока нет
- Glaucoma and Diabetes - Is There An Association? Jain Shashi, Lakhtakia Sujata, Tirkey Eva Rani, Jain Sheel ChandraДокумент5 страницGlaucoma and Diabetes - Is There An Association? Jain Shashi, Lakhtakia Sujata, Tirkey Eva Rani, Jain Sheel ChandranjmdrОценок пока нет
- Clinical and Epidemiology: Relationship Between Age and Intraocular Pressure: The Blue Mountains Eye StudyДокумент3 страницыClinical and Epidemiology: Relationship Between Age and Intraocular Pressure: The Blue Mountains Eye StudyPutri YingОценок пока нет
- Metabolic Syndrome Components and Age-RelatedДокумент8 страницMetabolic Syndrome Components and Age-RelatedOki LambeОценок пока нет
- Clinical Characteristics of CyclodeviationДокумент7 страницClinical Characteristics of Cyclodeviationcarlosalladoa0% (1)
- Risk Factors For Primary Open Angle Glaucoma in Japanese Sub 101911Документ7 страницRisk Factors For Primary Open Angle Glaucoma in Japanese Sub 101911marwicuteОценок пока нет
- Research ArticleДокумент6 страницResearch Articlenaufal12345Оценок пока нет
- An Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Документ6 страницAn Objective Approach To DED Severity Sullivan Et Al IOVS 12-2010Meyva HannaОценок пока нет
- Landmark Studies in GlaucomaДокумент53 страницыLandmark Studies in GlaucomaDrEknathPawarОценок пока нет
- Role of Flicker Perimetry in Predicting Onset of Late-Stage Age-Related Macular DegenerationДокумент10 страницRole of Flicker Perimetry in Predicting Onset of Late-Stage Age-Related Macular DegenerationHarold Estiven MarinОценок пока нет
- Relationship Between Intraocular Pressure and Obesity in JapanДокумент0 страницRelationship Between Intraocular Pressure and Obesity in JapanAngkat Prasetya Abdi NegaraОценок пока нет
- Am J Ophthalmol 2004 - p401Документ6 страницAm J Ophthalmol 2004 - p401Abrilia OctafijayantiОценок пока нет
- A Correlational Study of Systemic Blood Pressure and IOP HL SITHOLEДокумент6 страницA Correlational Study of Systemic Blood Pressure and IOP HL SITHOLESurya Nirmala DewiОценок пока нет
- Pressure Fluctuations in GlaucomaДокумент6 страницPressure Fluctuations in GlaucomaTushar BatraОценок пока нет
- +ijam 2016+Документ5 страниц+ijam 2016+Syane TitaleyОценок пока нет
- RF GlaucomaДокумент6 страницRF Glaucomamaandre123Оценок пока нет
- DM Dan GlaukomaДокумент5 страницDM Dan GlaukomaYandhie RahmanОценок пока нет
- A Review of Optic NeuritisДокумент5 страницA Review of Optic NeuritissatrianiОценок пока нет
- Comparison of Visual Outcomes in Coats' Disease A 20-Year ExperienceДокумент9 страницComparison of Visual Outcomes in Coats' Disease A 20-Year ExperienceMuhammad Ihsan AuliaОценок пока нет
- Brjopthal00019 0027Документ4 страницыBrjopthal00019 0027Fernando CortesОценок пока нет
- Prospective Evaluation of Acupuncture As Treatment For GlaucomaДокумент10 страницProspective Evaluation of Acupuncture As Treatment For Glaucoma16.11Hz MusicОценок пока нет
- Jurnal Reading GlaucomaДокумент6 страницJurnal Reading GlaucomawidyawirapОценок пока нет
- Jurnal Mata 3Документ4 страницыJurnal Mata 3Ami AntariksawatiОценок пока нет
- Full Paper. Clinical Profile of Cyclocryotherapy Patients in Yap Eye HospitalДокумент4 страницыFull Paper. Clinical Profile of Cyclocryotherapy Patients in Yap Eye HospitalSeravina Adila IzzatiОценок пока нет
- tmp1617 TMPДокумент7 страницtmp1617 TMPFrontiersОценок пока нет
- Steriod Cataract PDFДокумент4 страницыSteriod Cataract PDFLisa IskandarОценок пока нет
- S00219150nbdfcyh10X00065 S0021915009009964 MainДокумент6 страницS00219150nbdfcyh10X00065 S0021915009009964 MainFiqih Andrian IlmansyahОценок пока нет
- Ibyt 13 I 4 P 659Документ10 страницIbyt 13 I 4 P 659Sadhira GitaОценок пока нет
- 7 Geriatric Ophthalmology: MethodsДокумент26 страниц7 Geriatric Ophthalmology: Methodsadibashafique_214280Оценок пока нет
- Journal Reading SepoДокумент30 страницJournal Reading Seposeptian_tjayaОценок пока нет
- Jurnal KDMДокумент8 страницJurnal KDMFhietry Idrus ScaftweeОценок пока нет
- Diabetes and Risk of Fracture: The Blue Mountains Eye StudyДокумент6 страницDiabetes and Risk of Fracture: The Blue Mountains Eye Studymuhammad subhanОценок пока нет
- Epidemiology and Clinical Characteristics of Patients With Glaucoma: An Analysis of Hospital Data Between 2003 and 2012 Original ArticleДокумент7 страницEpidemiology and Clinical Characteristics of Patients With Glaucoma: An Analysis of Hospital Data Between 2003 and 2012 Original Articlesyntacs skОценок пока нет
- 11 Shailaja EtalДокумент4 страницы11 Shailaja EtaleditorijmrhsОценок пока нет
- Normal Tension GlaucomaДокумент7 страницNormal Tension GlaucomaSonia RogersОценок пока нет
- Co-Relation Between Body Mass Index and Intraocular Pressure in AdultsДокумент4 страницыCo-Relation Between Body Mass Index and Intraocular Pressure in AdultsAngkat Prasetya Abdi NegaraОценок пока нет
- gt0513 LandmarkДокумент5 страницgt0513 Landmarkjoe lopasoОценок пока нет
- The Association Between Intraocular Pressure and Predictors of Coronary Heart Disease Risk in KoreansДокумент4 страницыThe Association Between Intraocular Pressure and Predictors of Coronary Heart Disease Risk in KoreansAngkat Prasetya Abdi NegaraОценок пока нет
- Epidemiology of Angioid Streaks-Associated Choroidal Neovascular Membranes in The United KingdomДокумент20 страницEpidemiology of Angioid Streaks-Associated Choroidal Neovascular Membranes in The United KingdomCureusОценок пока нет
- Papers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsДокумент3 страницыPapers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsDanil Anugrah JayaОценок пока нет
- 10mridula EtalДокумент7 страниц10mridula EtaleditorijmrhsОценок пока нет
- Normal-Tension (Low-Tension) GlaucomaДокумент13 страницNormal-Tension (Low-Tension) GlaucomaFidela OliviaОценок пока нет
- The Influence of Diabetes Mellitus On Lenticular Thickness: KeywordsДокумент4 страницыThe Influence of Diabetes Mellitus On Lenticular Thickness: KeywordssuhasОценок пока нет
- VT For TBI (Ciuffreda Optomety 2010)Документ5 страницVT For TBI (Ciuffreda Optomety 2010)Synapgen ArticlesОценок пока нет
- Social Approach To Diabetic Retinopathy in NigeriaДокумент14 страницSocial Approach To Diabetic Retinopathy in NigeriaEmmanuel OgochukwuОценок пока нет
- 641 FullДокумент6 страниц641 FullLider Olmen PanggabeanОценок пока нет
- Glaucoma OHTSДокумент13 страницGlaucoma OHTSJose Antonio Fuentes VegaОценок пока нет
- Diabetes Mellitus and Refractive ChangesДокумент3 страницыDiabetes Mellitus and Refractive ChangesKhairunnisa0% (2)
- AteroscleroticДокумент5 страницAteroscleroticPutri PurnamaОценок пока нет
- Axial Myopia and Low HbA1c Level Are Correlated AnДокумент8 страницAxial Myopia and Low HbA1c Level Are Correlated AnGeert SmoldОценок пока нет
- Corneal Biomechanical Changes and Intraocular Pressure in Patients With Thyroid OrbitopathyДокумент5 страницCorneal Biomechanical Changes and Intraocular Pressure in Patients With Thyroid Orbitopathykevin_jawanОценок пока нет
- Crosstalk Between Nafld and CKD and Its Effect On EgfrДокумент5 страницCrosstalk Between Nafld and CKD and Its Effect On EgfrIJAR JOURNALОценок пока нет
- The Changing Profile of Astigmatism in Childhood The NICER StudyДокумент9 страницThe Changing Profile of Astigmatism in Childhood The NICER Studyforumuser123Оценок пока нет
- Judika-Sampai AkhirДокумент1 страницаJudika-Sampai AkhirAngkat Prasetya Abdi NegaraОценок пока нет
- Book 1Документ13 страницBook 1Semba Anggen RachmaniОценок пока нет
- KLP1 Jurnal IlmiahДокумент8 страницKLP1 Jurnal IlmiahArya KusumaОценок пока нет
- Cyclosporine Reduces Reperfusion InjuryДокумент3 страницыCyclosporine Reduces Reperfusion InjuryAngkat Prasetya Abdi NegaraОценок пока нет
- Nilai RemediДокумент21 страницаNilai RemediAngkat Prasetya Abdi NegaraОценок пока нет
- 2965 CONSORT+2010+ChecklistДокумент2 страницы2965 CONSORT+2010+ChecklistsongsiriОценок пока нет
- Critical Appraisal of Epidemiological Study PDFДокумент11 страницCritical Appraisal of Epidemiological Study PDFYessy Dwi OktaviaОценок пока нет
- Nilai Normal Laboratorium Pada AnakДокумент6 страницNilai Normal Laboratorium Pada AnakMaharani Primastuti ArganistОценок пока нет
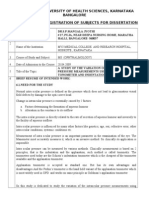
- Rajiv Gandhi University of Health Sciences, Karnataka Bangalore Proforma For Registration of Subjects For DissertationДокумент5 страницRajiv Gandhi University of Health Sciences, Karnataka Bangalore Proforma For Registration of Subjects For DissertationAngkat Prasetya Abdi NegaraОценок пока нет
- Review Article: Today and Future of Age-Related Macular DegenerationДокумент9 страницReview Article: Today and Future of Age-Related Macular DegenerationAngkat Prasetya Abdi NegaraОценок пока нет
- Nilai Normal Vital PediatriДокумент4 страницыNilai Normal Vital PediatriEkaPutri AzizОценок пока нет
- Pengendalian Emosi Pasien Hipertensi Dengan Terpai MusikДокумент5 страницPengendalian Emosi Pasien Hipertensi Dengan Terpai MusikAngkat Prasetya Abdi NegaraОценок пока нет
- Correlation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsДокумент1 страницаCorrelation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsAngkat Prasetya Abdi NegaraОценок пока нет
- B82 FDD 01Документ24 страницыB82 FDD 01Angkat Prasetya Abdi NegaraОценок пока нет
- Correlation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsДокумент1 страницаCorrelation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsAngkat Prasetya Abdi NegaraОценок пока нет
- Original ArticleДокумент5 страницOriginal ArticleAngkat Prasetya Abdi NegaraОценок пока нет
- BMC Genetics: Intraocular Pressure in Genetically Distinct Mice: An Update and Strain SurveyДокумент15 страницBMC Genetics: Intraocular Pressure in Genetically Distinct Mice: An Update and Strain SurveyAngkat Prasetya Abdi NegaraОценок пока нет
- D4 AF0 D 01Документ11 страницD4 AF0 D 01Angkat Prasetya Abdi NegaraОценок пока нет
- Eeb05036 767 772Документ6 страницEeb05036 767 772Angkat Prasetya Abdi NegaraОценок пока нет
- B82 FDD 01Документ24 страницыB82 FDD 01Angkat Prasetya Abdi NegaraОценок пока нет
- Association of Life-Style With Intraocular Pressure in Middle-Aged and Older Japanese ResidentsДокумент8 страницAssociation of Life-Style With Intraocular Pressure in Middle-Aged and Older Japanese ResidentsAngkat Prasetya Abdi NegaraОценок пока нет
- Height and Its Relationship To Refraction and Biometry Parameters in Singapore Chinese ChildrenДокумент6 страницHeight and Its Relationship To Refraction and Biometry Parameters in Singapore Chinese ChildrenAngkat Prasetya Abdi NegaraОценок пока нет
- D 01Документ10 страницD 01Angkat Prasetya Abdi NegaraОценок пока нет
- 2011 02 Obese Women GlaucomaДокумент1 страница2011 02 Obese Women GlaucomaAngkat Prasetya Abdi NegaraОценок пока нет
- 257 EEd 01Документ4 страницы257 EEd 01Angkat Prasetya Abdi NegaraОценок пока нет
- 6187 DD 01Документ4 страницы6187 DD 01Angkat Prasetya Abdi NegaraОценок пока нет
- 265 901 2 PBДокумент5 страниц265 901 2 PBAngkat Prasetya Abdi NegaraОценок пока нет
- International Journal of Biomedical and Advance ResearchДокумент4 страницыInternational Journal of Biomedical and Advance ResearchAngkat Prasetya Abdi NegaraОценок пока нет
- Intraocular Pressure: Harry Murgatroyd BSC MB CHB (Hons) Jane Bembridge MB CHB (Hons) FrcaДокумент4 страницыIntraocular Pressure: Harry Murgatroyd BSC MB CHB (Hons) Jane Bembridge MB CHB (Hons) FrcaAngkat Prasetya Abdi NegaraОценок пока нет
- New KitДокумент195 страницNew KitRamu BhandariОценок пока нет
- B1 Editable End-of-Year TestДокумент6 страницB1 Editable End-of-Year TestSyahira Mayadi50% (2)
- Growth Kinetic Models For Microalgae Cultivation A ReviewДокумент16 страницGrowth Kinetic Models For Microalgae Cultivation A ReviewJesús Eduardo De la CruzОценок пока нет
- Alan Freeman - Ernest - Mandels - Contribution - To - Economic PDFДокумент34 страницыAlan Freeman - Ernest - Mandels - Contribution - To - Economic PDFhajimenozakiОценок пока нет
- Deep Sea 500 Ats ManДокумент18 страницDeep Sea 500 Ats ManLeo Burns50% (2)
- Enzymatic Hydrolysis, Analysis of Mucic Acid Crystals and Osazones, and Thin - Layer Chromatography of Carbohydrates From CassavaДокумент8 страницEnzymatic Hydrolysis, Analysis of Mucic Acid Crystals and Osazones, and Thin - Layer Chromatography of Carbohydrates From CassavaKimberly Mae MesinaОценок пока нет
- Rfis On Formliners, Cover, and EmbedmentsДокумент36 страницRfis On Formliners, Cover, and Embedmentsali tahaОценок пока нет
- Jurnal KORELASI ANTARA STATUS GIZI IBU MENYUSUI DENGAN KECUKUPAN ASIДокумент9 страницJurnal KORELASI ANTARA STATUS GIZI IBU MENYUSUI DENGAN KECUKUPAN ASIMarsaidОценок пока нет
- Ingres in ReproductionДокумент20 страницIngres in ReproductionKarlОценок пока нет
- Actara (5 24 01) PDFДокумент12 страницActara (5 24 01) PDFBand Dvesto Plus CrepajaОценок пока нет
- English 8 q3 w1 6 FinalДокумент48 страницEnglish 8 q3 w1 6 FinalJedidiah NavarreteОценок пока нет
- 4.9 Design of Compression Members: L 4.7 UsingДокумент22 страницы4.9 Design of Compression Members: L 4.7 Usingctc1212100% (1)
- Interceptor Specifications FinalДокумент7 страницInterceptor Specifications FinalAchint VermaОценок пока нет
- 3114 Entrance-Door-Sensor 10 18 18Документ5 страниц3114 Entrance-Door-Sensor 10 18 18Hamilton Amilcar MirandaОценок пока нет
- Detailed Lesson Plan in Mathematics (Pythagorean Theorem)Документ6 страницDetailed Lesson Plan in Mathematics (Pythagorean Theorem)Carlo DascoОценок пока нет
- MBA 2nd Sem SyllabusДокумент6 страницMBA 2nd Sem SyllabusMohammad Ameen Ul HaqОценок пока нет
- All About History History of Communism - 4th Edition 2022Документ148 страницAll About History History of Communism - 4th Edition 2022Duke100% (1)
- Comparison of Multi-Coil and Diaphragm Spring ClutchesДокумент3 страницыComparison of Multi-Coil and Diaphragm Spring Clutchesmasb_994077Оценок пока нет
- Jurnal Direct and Indirect Pulp CappingДокумент9 страницJurnal Direct and Indirect Pulp Cappingninis anisaОценок пока нет
- Astm C119-16Документ8 страницAstm C119-16Manuel Antonio Santos Vargas100% (2)
- Major Stakeholders in Health Care SystemДокумент5 страницMajor Stakeholders in Health Care SystemANITTA S100% (1)
- Green ProtectДокумент182 страницыGreen ProtectLuka KosticОценок пока нет
- Review On Antibiotic Reidues in Animl ProductsДокумент6 страницReview On Antibiotic Reidues in Animl ProductsMa. Princess LumainОценок пока нет
- Pinterest or Thinterest Social Comparison and Body Image On Social MediaДокумент9 страницPinterest or Thinterest Social Comparison and Body Image On Social MediaAgung IkhssaniОценок пока нет
- Exam Ref 70 483 Programming in C by Wouter de Kort PDFДокумент2 страницыExam Ref 70 483 Programming in C by Wouter de Kort PDFPhilОценок пока нет
- The Story of An Hour QuestionpoolДокумент5 страницThe Story of An Hour QuestionpoolAKM pro player 2019Оценок пока нет
- Internship (1) FinalДокумент12 страницInternship (1) FinalManak Jain50% (2)
- Malaybalay CityДокумент28 страницMalaybalay CityCalvin Wong, Jr.Оценок пока нет
- 3 HVDC Converter Control PDFДокумент78 страниц3 HVDC Converter Control PDFJanaki BonigalaОценок пока нет
- Tech SharmitДокумент16 страницTech SharmitRishu SinhaОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningОт EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningРейтинг: 4 из 5 звезд4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Оценок пока нет
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerОт EverandGut: the new and revised Sunday Times bestsellerРейтинг: 4 из 5 звезд4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingОт EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingРейтинг: 4 из 5 звезд4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassОт EverandTroubled: A Memoir of Foster Care, Family, and Social ClassРейтинг: 4.5 из 5 звезд4.5/5 (26)