Академический Документы
Профессиональный Документы
Культура Документы
Journal Atrophic Rhinits
Загружено:
Dion Satriawan Dhaniardi0 оценок0% нашли этот документ полезным (0 голосов)
37 просмотров0 страницatrophic rhinitis
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документatrophic rhinitis
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
37 просмотров0 страницJournal Atrophic Rhinits
Загружено:
Dion Satriawan Dhaniardiatrophic rhinitis
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 0
Atrophic Rhinitis and Its Surgical Management
Clinical Rhinology: An International Journal, September-December 2011;4(3):127-129
127
AIJCR
Atrophic Rhinitis and Its Surgical
Management
1
Vinit Kumar Sharma,
2
Rohit Sharma,
3
JP Purohit,
4
Sampan Vishth
1
Assistant Professor, Department of Otolaryngology, SRMS Institute of Medical Sciences, Bareilly, Uttar Pradesh, India
2
Associate Professor, Department of Otolaryngology, SRMS Institute of Medical Sciences, Bareilly, Uttar Pradesh, India
3
Professor and Head, Department of Otolaryngology, MLB Medical College, Jhansi, Uttar Pradesh, India
4
Resident, Department of Otolaryngology, MLB Medical College, Jhansi, Uttar Pradesh, India
Correspondence: Vinit Kumar Sharma, Assistant Professor, Department of Otolaryngology, SRMS Institute of Medical Sciences
Bareilly, Uttar Pradesh, India, e-mail: drvineetsharma@rediffmail.com
ORIGINAL ARTICLE
INTRODUCTION
Atrophic rhinitis is a chronic nasal disease characterized
by progressive atrophy of the nasal mucosa and underlying
bone of the turbinates and very roomy nasal cavity, the
formation of foul smelling thick black or greenish crust, to
which attributed the term ozaena.
1
The earliest complaint
is a feeling of dryness in the nose and headache commonly
described as an aching behind the eyes. Nasal myiasis occur
most commonly in Asia and less commonly in Africa. Nasal
myiasis, which is not uncommon in hot and humid climate
particularly in India, is also known as Peenash. It is a
demoralizing condition of infestation of the nasal cavities
by maggots, the larvae of fly (Diptera).
Myiasis can also affect the ear, mouth or larynx and
reach its peak in the months of March, April, September,
October and November. The majority of sufferers live in
bad hygienic conditions and have a source of offensive
decaying material, e.g. atrophic rhinitis, chronic sinusitis
or chronic suppurative otitis media, which provides a
suitable environment for the eggs of the fly to hatch into
larvae.
2
The patient complains of a diffuse swelling around
the nose and eyes, nasal obstruction, epistaxis or the
presence of maggots coming out of nose. Rhinoscopy
reveals a congested edematous mucosa, necrotic material
with embedded maggots, ulcerated mucosa or septal
perforations. The disease can spread to the paranasal sinuses
and via the nasolacrimal duct to lacrimal sac. In the late
stages, the nasal bones may be destroyed and death may
result from sepsis, meningitis or suicide.
Most of the surgical methods are aimed at reducing the
nasal airway. The drying effect of inspired air is a major
factor in causation or progression of the disease. Partial
obliteration of nasal cavity breaks this viscious cycle, which
causes atrophy of the mucosa and widening of the nasal
cavity. A review of various surgical treatments is given below:
1. Operation to narrow the nasal cavity
A. Nasal closure operation
i. Anterior nare closure
ii. Choanal occlusion
B. Implantation operation
i. Living tissue implants, like
(a) Autogenousdermofat, bone, cartilage
(b) Homogenousplacenta
(c) Heterogenousbioimplant
ii. Synthetic implants, like acrylic, silicone, teflon,
proplast
Objective: Clinical evaluation of atrophic rhinitis and comparative study of its surgical treatments.
Materials and methods: This study was carried out in the Department of ORL-HNS, MLB Medical College and Hospital, Jhansi and Department
of ORL-HNS, SRMS Institute of Medical Sciences, Bareilly, Uttar Pradesh, India from June 2006 to May 2011 including the cases of atrophic
rhinitis. A total of 40 patients of atrophic rhinitis were included in this study. Thirty-two patients had modified Youngs nostril closure and eight
patients had dermofat graft obliteration of nasal cavity. Preoperative and postoperative assessment of nasal mucociliary flow rate were also
assessed by saccharine test. Fifteen cases were kept in control group to compare the nasal mucociliary flow rate results.
Results: The results of both surgical modalities were compared at various intervals for 20 months.
Conclusion: The patients with history of nasal myiasis and septal perforation do better with partial nostril closure while patients, not having
history of maggots and septal perforations, had best results with dermofat graft operation. It was seen that after surgical treatment of atrophic
rhinitis, either by nostril closure or dermofat grafting, there was improvement in nasal mucociliary flow or, nearly, all patients were symptomatically
improved.
Keywords: Nasal myiasis, Atrophic rhinitis, Nasal mucociliary flow rate.
ABSTRACT
10.5005/jp-journals-10013-1091
Vinit Kumar Sharma et al
128
JAYPEE
2. Denervation operations
A. Sympathectomy
i. Cervical sympathectomy
ii. Stellate ganglion block
iii. Sphenopalatine ganglion block
B. Parasympathectomysection of greater superficial
petrosal nerve.
AIMS AND OBJECTIVES
1. To study the surgical treatments for atrophic rhinitis and
nasal myiasis and compare the follow-up results of
modified Youngs nostril closure and Girgis dermofat
graft implantation.
2. To compare the nasal mucociliary flow rates pre- and
postoperatively.
MATERIALS AND METHODS
This study was carried out in the Department of ORL-HNS,
MLB Medical College and Hospital, Jhansi and Department
of ORL-HNS, SRMS Institute of Medical Sciences, Bareilly,
Uttar Pradesh, India. The work was carried out from June
2006 to May 2011. This study included the cases of
atrophic rhinitis and some cases of nasal myiasis. A total of
40 patients were included in this study. Thirty-two patients
had modified Youngs nostril closure and eight patients had
dermofat graft obliteration of nasal cavity. They were
reexamined during follow-up at regular intervals and the
net outcomes of the above-mentioned modalities were
compared. The nasal mucociliary flow rate was also assessed
by saccharine test in which, a 0.5 mm sized particle was placed
approximately 1.0 cm behind the anterior end of inferior
turbinate in the sitting position with the head flexed about
10 to avoid the particle falling back in nasopharynx. The
subject was asked to swallow after every 50 seconds and not
to sniff or drink. He was asked to tell immediately, as he got
the sweet taste of saccharine. The time elapsing until the first
experience of sweet taste was recorded as nasal mucociliary
flow rate. Fifteen cases were also chosen as control group.
RESULTS
A. Dermofat graft implantation: The results of dermofat
graft implantation show that out of the eight operated
cases, one case did not come for follow-up after
6 months. Till 6 months, all the eight cases showed relief.
The remaining seven cases maintained good results up
to 1 year. After that three cases also lost follow-up in
18 months time, remaining cases maintained good results.
B. Modified Youngs operation: The results of 32 cases
operated showed that there was complete disappearance
of the crusting and foul smelling from the nose. All the
cases, during the follow-up periods, showed that patients
were relieved from the symptoms.
Patients operated, by either of the above methods,
showed significant improvement as assessed by
disappearance of visible crusting in nose, pharyngitis sicca
and olfactory disturbances. But as a comparative result of
the two methods, improvement in symptoms was found
better in patients who underwent dermofat graft implantation
as found in previous studies also (Table 1).
3
As mucociliary function is also disturbed as a sequelae
of atrophic rhinitis, we also assessed the outcome of these
two methods by assessing the nasal mucociliary flow rate
by saccharin test.
Nasal mucociliary rates as recorded pre- and post-
operatively are shown in Table 2. It was seen that there was
dramatic improvement in mucociliary flow rate confirming
the results of studies in past.
4
In control group, it was
approximately 12.5 minutes. All these patients showed
complete improvement in all symptoms.
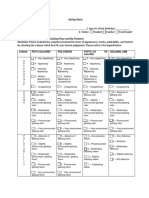
Table 1: Nasal mucociliary flow rates before and after
dermofat grafting
Total no of Dermofat grafting Modified Youngs
patients operation
40 8 32
DISCUSSION
In our series, we have done only eight cases of dermofat
grafting. This small number was due to choice of the patients
between dermofat grafting and nostril closure. We have
followed the techniques described by Girgis without any
modification, but in two cases, we approached the floor of
nasal cavity by incision in nasal vestibule instead of
sublabial approach. In the approach via nasal vestibule,
bleeding and time for surgery was reduced, because
dermofat grafting involves a major operation under general
anesthesia with a hospital stay. The immediate postoperative
period was quiet stormy in all the eight cases in which
sublabial approach was followed, they had swelling of face
and pyrexia, While in nasal vestibule approach, swelling of
face was minimum. The thigh wound did take time to heal
Table 2: Nasal mucociliary flow rates before and after
modified Youngs operation
Mean mucociliary flow time (min)
Dermofat grafting Modified Youngs
operation
Before surgery 50.4 51.2
After surgery 32.3 26.4
Control group12.5 minutes
Atrophic Rhinitis and Its Surgical Management
Clinical Rhinology: An International Journal, September-December 2011;4(3):127-129
129
AIJCR
up, and in one of our cases, there was wound dehiscence
and infection. It required cleaning and dressing for 1 month.
Scar on thigh was definitely a marked one, which one feels
to avoid as most of the patients are young females. The
shrinkage of the graft as stated by Girgis was due to
absorption of fat in 25% and, in some cases, up to 50% but,
in our series, shrinkage was not noticed as a major factor
during the follow-up.
5
All cases, during the 6 months follow-
up period, showed that the floor was raised adequately and
only in one case, it was not adequate, probably due to slight
shrinkage in graft. Graft rejection was not noticed in any
case. Even sloughing and fistula formation as experienced
by Girgis
6
were not seen.
In rest of the 32 cases, Youngs operation was done with
a slight modification by placing the incision little more
anteriorly and converting the technique in double layer
closure, i.e. modified Youngs operation. The added
advantages were safety avoidance of separate wound and
the patients satisfaction of breathing through the nose, and
one can perform anterior rhinoscopy with infant-sized ear
speculum through the hole. Bilateral operation could also
be performed in the same sitting without posing much
problems postoperatively and the problems of reopening
can be avoided. The operation appears technically a simple
one. One does not have to look out for external source or an
additional operation for materials for implantation. Most
of the cases, it can be performed under local anesthesia with
good sedation in adequate doses. Patient experiences mild
pain and swelling of the nose for 2 to 3 days. No serious
postoperative complications were observed by us. The
crusting disappears and the mucosa turns pink very quickly
after the closure. Perhaps nostril closure stands as an ideal
operation for those unfortunate patients who come with
history of maggots, and mutilation of turbinates and nasal
tissue by maggots with septal perforation. They do better
with partial nostril closure while patients not having history
of maggots and septal perforations had best result with
dermofat graft operation.
In all of the above-mentioned patients, there was great
improvement in nasal mucociliary flow rate after surgery
for atrophic rhinitis and all of them were relieved from their
symptoms.
Partial nostril closure was done in cases of septal
perforation. It is not possible to do another implant operation
like dermofat graft in these cases properly. In this series,
four patients who came with septal perforation with maggots
infestation were subjected to partial nostril closure. All are
showing good results inspite of septal perforation. Hence,
partial nostril closure stands unique as an ideal operation
where septal perforation is present. The partial nostril
closure does not pose any problem and is hardly noticeable.
In immediate postoperative days, the complaints of dryness
of mouth especially after a nights sleep by a few patients
were reported. It was due to mouth breathing and is relieved
by drinking water. They were also not found more prone to
suffer from upper respiratory tract infection. But surely, they
are disabled to some extent by the nasal tone of speech.
REFERENCES
1. Cook Gordon C, Zumla Alimuddin. Mansons Tropical Disease
(21st ed), 1600-04, 172732.
2. Warrell David A, Cox Timothy M, Fifth John. Oxford Text Book
of Medicine (4th ed), 853-54.
3. Taylor M, Young A. Studies on atrophic rhinitis. J Laryngol
Otol 1961;75:574-90.
4. Schonsted-Madsen U, Stoksted P, Christensen PH, Koch-
Henriksen N. Chronic headache related to nasal obstruction. J
Laryngol Otol Feb 1986;100(2):165-70.
5. Sinha SN, Sardana DS, Rajvanshi VS. Nine-year review of cases
of atrophic rhinitis and its management. J Laryngol Otol
1977;91:591-600.
6. Girgis IH. Surgical management of ozaena by dermofat graft. J
Laryngol Otol 1966;80:615-27.
Вам также может понравиться
- UntitledДокумент6 страницUntitledangela cañariОценок пока нет
- Rhinomanometric Assessment of Nasal Airflow in Deviated Nasal SeptumДокумент2 страницыRhinomanometric Assessment of Nasal Airflow in Deviated Nasal SeptumRia Tutkey-MelmambessyОценок пока нет
- Inferior Turbinectomy For Nasal Obstruction Review of 75 CasesДокумент4 страницыInferior Turbinectomy For Nasal Obstruction Review of 75 CasesMeilina Elin WardhaniОценок пока нет
- TURKEY Tonimer GelДокумент12 страницTURKEY Tonimer Geldenisp1987Оценок пока нет
- A Comparative Study Between Two Monitoring TechniqДокумент22 страницыA Comparative Study Between Two Monitoring TechniqSanketNandaniОценок пока нет
- Effects of Surgical Treatment PDFДокумент6 страницEffects of Surgical Treatment PDFAssifa RidzkiОценок пока нет
- Asha Annie 2014Документ4 страницыAsha Annie 2014Ratna Puspa RahayuОценок пока нет
- The Impact of Allergic Rhinitis On Symptom Improvement in Pediatric Patients After AdenotonsillectomyДокумент6 страницThe Impact of Allergic Rhinitis On Symptom Improvement in Pediatric Patients After AdenotonsillectomyBayu PrakosoОценок пока нет
- Conclusions Discussion ResultsДокумент1 страницаConclusions Discussion ResultsAldy PratamaОценок пока нет
- Endoscopic Sinus Surgery: Indications and Complications: February 2020Документ7 страницEndoscopic Sinus Surgery: Indications and Complications: February 2020husnul khatimahОценок пока нет
- A Prospective Study of Sinonasal and Nasopharyngeal Pathology in Chronic Otitis MediaДокумент5 страницA Prospective Study of Sinonasal and Nasopharyngeal Pathology in Chronic Otitis MediaAmalia OkvitariandariОценок пока нет
- Evolvingmaterials Andtechniquesfor Endoscopicsinus SurgeryДокумент20 страницEvolvingmaterials Andtechniquesfor Endoscopicsinus Surgerydisk_la_poduОценок пока нет
- Internal Nasal ValveДокумент6 страницInternal Nasal ValveAmmar EidОценок пока нет
- Bishnoi2020 Article EvaluationOfFactorsDeterminingДокумент6 страницBishnoi2020 Article EvaluationOfFactorsDeterminingAlvaro Andres Flores JimenezОценок пока нет
- Jur Nal Reading FixДокумент30 страницJur Nal Reading FixArum DiannitasariОценок пока нет
- PARS Reader's Digest - June 2013Документ8 страницPARS Reader's Digest - June 2013info8673Оценок пока нет
- TurbinoplastyДокумент7 страницTurbinoplastyNeena GuptaОценок пока нет
- EnsДокумент6 страницEnsAlwi Qatsir AlyaОценок пока нет
- Anesthesia Challenge in Dental Abscess Induced Trismus: A Case ReportДокумент4 страницыAnesthesia Challenge in Dental Abscess Induced Trismus: A Case ReportesraОценок пока нет
- Evaluation of Prednisolone and Prednisolone Sodium Succinate Concentrations in Human Plasma and Inner Ear Perilymph During Cochlear Implantation 24 HДокумент7 страницEvaluation of Prednisolone and Prednisolone Sodium Succinate Concentrations in Human Plasma and Inner Ear Perilymph During Cochlear Implantation 24 HRafael BaybayОценок пока нет
- Doppler Ultrasonographic Anatomy of The Midline Nasal DorsumДокумент6 страницDoppler Ultrasonographic Anatomy of The Midline Nasal DorsumKerlida SantosОценок пока нет
- PAFMJ DecДокумент5 страницPAFMJ DecAhmed BazilОценок пока нет
- Trans-Septal Suture Method Versus Intranasal Silicone Splint in SeptoplastyДокумент7 страницTrans-Septal Suture Method Versus Intranasal Silicone Splint in SeptoplastyInternational Jpurnal Of Technical Research And ApplicationsОценок пока нет
- Jurnal EbmДокумент10 страницJurnal EbmdeasyОценок пока нет
- Fungal Otitis Externa As A Cause of Tympanic Membrane Perforation: A Case SeriesДокумент6 страницFungal Otitis Externa As A Cause of Tympanic Membrane Perforation: A Case Serieszerin_atinОценок пока нет
- Subannular T Tube For The Treatment of Adhesive OtitisДокумент6 страницSubannular T Tube For The Treatment of Adhesive OtitisTeuku Ahmad HasanyОценок пока нет
- Functional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueДокумент10 страницFunctional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueHendra SusantoОценок пока нет
- Maxillary Sinus Function After Sinus Lifts For The Insertion of Dental ImplantsДокумент4 страницыMaxillary Sinus Function After Sinus Lifts For The Insertion of Dental Implantsyortu1982Оценок пока нет
- Miiringotomi OMEДокумент7 страницMiiringotomi OMEamaliaОценок пока нет
- Otorhinolaryngology: Inferior Turbinectomy: What Is The Best Technique?Документ2 страницыOtorhinolaryngology: Inferior Turbinectomy: What Is The Best Technique?Ramya KamathОценок пока нет
- Tracheostomy and Intubation Related DysphagiaДокумент25 страницTracheostomy and Intubation Related DysphagiaVikashОценок пока нет
- Case Report Dr. Frenky RSKДокумент12 страницCase Report Dr. Frenky RSKTHT KLОценок пока нет
- 1574-Article Text-2641-1-10-20181107Документ5 страниц1574-Article Text-2641-1-10-20181107Faraz HaiderОценок пока нет
- Endoscopic Insertion of Tympanostomy Tube in ChildrenДокумент5 страницEndoscopic Insertion of Tympanostomy Tube in ChildrenInternational Jpurnal Of Technical Research And ApplicationsОценок пока нет
- March 2015 266-269 PDFДокумент4 страницыMarch 2015 266-269 PDFEsha PradnyanaОценок пока нет
- Chronic Rhinosinusitis - An Overview: N.V Deepthi, U.K. Menon, K. MadhumitaДокумент6 страницChronic Rhinosinusitis - An Overview: N.V Deepthi, U.K. Menon, K. MadhumitaMilanisti22Оценок пока нет
- Medip,+15 59 1 CEДокумент7 страницMedip,+15 59 1 CEKabir Ahmed LaskarОценок пока нет
- The Advantages of External DR PDFДокумент13 страницThe Advantages of External DR PDFalitОценок пока нет
- Airway and Class II Div 1Документ9 страницAirway and Class II Div 1jayashreeОценок пока нет
- Respirador BucalДокумент8 страницRespirador Bucalyessenia armijosОценок пока нет
- Juvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyДокумент3 страницыJuvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyGiiszs AlvarezОценок пока нет
- Original Article: 360 Degree Subannular Tympanoplasty: A Retrospective StudyДокумент7 страницOriginal Article: 360 Degree Subannular Tympanoplasty: A Retrospective StudyAkanshaОценок пока нет
- Sinus Radiography: Is Water'S View Helpful in The Management of Chronic Maxillary Sinusitis?Документ4 страницыSinus Radiography: Is Water'S View Helpful in The Management of Chronic Maxillary Sinusitis?Ardhito BudhijuwonoОценок пока нет
- Emergency Medicine:: Pediatric Deep Neck Space Abscesses: A Prospective Observational StudyДокумент6 страницEmergency Medicine:: Pediatric Deep Neck Space Abscesses: A Prospective Observational StudyG Virucha Meivila IIОценок пока нет
- Cystic Hygroma An Anesthesiologist ChallengeДокумент2 страницыCystic Hygroma An Anesthesiologist ChallengeAlbertina L TebayОценок пока нет
- Ijhs 12577+883 892Документ10 страницIjhs 12577+883 892hai1Оценок пока нет
- Nasolaryngoscopy: Scott E. MoserДокумент5 страницNasolaryngoscopy: Scott E. Moserriski novitaОценок пока нет
- Role of Surgery in Isolated Concha Bullosa: Clinical Medicine Insights: Ear, Nose and ThroatДокумент7 страницRole of Surgery in Isolated Concha Bullosa: Clinical Medicine Insights: Ear, Nose and ThroatPinandhito LatukolanОценок пока нет
- Surgical Management of Turbinoplasty LO MEJOR DE LO MEJORДокумент10 страницSurgical Management of Turbinoplasty LO MEJOR DE LO MEJORDavid CáceresОценок пока нет
- Aesthetic Surgery Journal: Components of The Nasal ExaminationДокумент6 страницAesthetic Surgery Journal: Components of The Nasal ExaminationdoctorbanОценок пока нет
- Nitte University Journal March 2012-37-41Документ5 страницNitte University Journal March 2012-37-41Monna Medani LysabellaОценок пока нет
- Adenoid Radiologic MeasurementДокумент5 страницAdenoid Radiologic MeasurementfantamerahОценок пока нет
- A Comparative Study of Endoscopic Versus Conventional Septoplasty An Analysis of 50 CasesДокумент6 страницA Comparative Study of Endoscopic Versus Conventional Septoplasty An Analysis of 50 CasesDay LightОценок пока нет
- Otitie Media Adhesiva JMCM - Volume 9 - Issue 1 - Pages 108-112Документ5 страницOtitie Media Adhesiva JMCM - Volume 9 - Issue 1 - Pages 108-112Teuku Ahmad HasanyОценок пока нет
- Thirty Years of Submental Intubation: A Review: Review Paper Oral SurgeryДокумент5 страницThirty Years of Submental Intubation: A Review: Review Paper Oral SurgeryUmer HussainОценок пока нет
- Arya PDFДокумент26 страницArya PDFRahmawati JuliaОценок пока нет
- Journal of Otology: Gendi Yin, Jingqian Tan, Peng LiДокумент5 страницJournal of Otology: Gendi Yin, Jingqian Tan, Peng LiKevanОценок пока нет
- Basics and modern practice of nasal high-flow therapyОт EverandBasics and modern practice of nasal high-flow therapyРейтинг: 5 из 5 звезд5/5 (1)
- Normal and Pathological Bronchial Semiology: A Visual ApproachОт EverandNormal and Pathological Bronchial Semiology: A Visual ApproachPierre Philippe BaldeyrouОценок пока нет
- Postlaryngectomy voice rehabilitation with voice prosthesesОт EverandPostlaryngectomy voice rehabilitation with voice prosthesesОценок пока нет
- Hordeolum & ChalazionДокумент22 страницыHordeolum & ChalazionDion Satriawan Dhaniardi100% (1)
- Time License Pla Terminal SIM Card Tracker Sta Vehicle Sta Alarm Speed (Km/Mileage (K Used FuelДокумент2 страницыTime License Pla Terminal SIM Card Tracker Sta Vehicle Sta Alarm Speed (Km/Mileage (K Used FuelDion Satriawan DhaniardiОценок пока нет
- Time License Pla Terminal SIM Card Tracker Sta Vehicle Sta Alarm Speed (Km/Mileage (K Used FuelДокумент2 страницыTime License Pla Terminal SIM Card Tracker Sta Vehicle Sta Alarm Speed (Km/Mileage (K Used FuelDion Satriawan DhaniardiОценок пока нет
- Letters Subject Object Question in Words Would You Be My Girlfriend? (22 - 11 - 15)Документ1 страницаLetters Subject Object Question in Words Would You Be My Girlfriend? (22 - 11 - 15)Dion Satriawan DhaniardiОценок пока нет
- Brief Negative Symptom Scale: Scoresheet: I. AnhedoniaДокумент1 страницаBrief Negative Symptom Scale: Scoresheet: I. AnhedoniaDion Satriawan DhaniardiОценок пока нет
- The Expression of Platelet Serotonin Transporter (SERT) in Human ObesityДокумент8 страницThe Expression of Platelet Serotonin Transporter (SERT) in Human ObesityDion Satriawan DhaniardiОценок пока нет
- Validation of Fluorescence in Situ Hybridization Using AnДокумент6 страницValidation of Fluorescence in Situ Hybridization Using AnDion Satriawan DhaniardiОценок пока нет
- 1 GhunnaДокумент4 страницы1 GhunnaAmr WagihОценок пока нет
- Cleft Rhinoplasty CMEДокумент13 страницCleft Rhinoplasty CMENaveed KhanОценок пока нет
- Connotative Vs DenotativeДокумент4 страницыConnotative Vs DenotativeSyeda WaniyaОценок пока нет
- Muthia Sani (Daftar Pustaka)Документ5 страницMuthia Sani (Daftar Pustaka)tttttОценок пока нет
- Hello + How Are You BobbyДокумент7 страницHello + How Are You BobbyMai ĐỗОценок пока нет
- Anatomi Dan Fisiologi HidungДокумент51 страницаAnatomi Dan Fisiologi HidungVania GirsangОценок пока нет
- Average: Dina FatmawatiДокумент2 страницыAverage: Dina FatmawatiregyanaОценок пока нет
- 23 Sur Deviated Nasal SeptumДокумент3 страницы23 Sur Deviated Nasal SeptumSardar jiОценок пока нет
- Pmfadj20 EastДокумент2 страницыPmfadj20 EastEdwin Barazorda VillegasОценок пока нет
- SGD 11 - Zayyina Chamaladina - 30101900210Документ8 страницSGD 11 - Zayyina Chamaladina - 30101900210Anonymous iTstegX2Оценок пока нет
- 6 EpistaxisДокумент19 страниц6 EpistaxissuciОценок пока нет
- Disease of Nasal Septum and SeptoplastyДокумент21 страницаDisease of Nasal Septum and SeptoplastyHolly ReedОценок пока нет
- Anterior Rhinoscopy-Hanan BakriДокумент15 страницAnterior Rhinoscopy-Hanan BakriMadalina DutanОценок пока нет
- Modul Rinologi - 1. Benda Asing HidungДокумент13 страницModul Rinologi - 1. Benda Asing HidungPutri DamayantiОценок пока нет
- Nasal ObstructionДокумент6 страницNasal Obstructionjoal510Оценок пока нет
- Rating Sheet Part I. Personal Information: Criteria Puto Galiang Polvoron Galiang JamДокумент2 страницыRating Sheet Part I. Personal Information: Criteria Puto Galiang Polvoron Galiang JamNanette A. Marañon-SansanoОценок пока нет
- Deviated Nasal SeptumДокумент17 страницDeviated Nasal SeptumsksbashaОценок пока нет
- Otorhinolaryngology: Inferior Turbinectomy: What Is The Best Technique?Документ2 страницыOtorhinolaryngology: Inferior Turbinectomy: What Is The Best Technique?Ramya KamathОценок пока нет
- Clinical Case Reports - 2022 - Amin - Short Duration Phantosmia Changes in A Post COVID 19 Patient in BangladeshДокумент4 страницыClinical Case Reports - 2022 - Amin - Short Duration Phantosmia Changes in A Post COVID 19 Patient in BangladeshArsyaka InaraОценок пока нет
- Digital Scent TechnologyДокумент13 страницDigital Scent TechnologyRahul Maravi0% (1)
- Assessing The Nose and SinusesДокумент2 страницыAssessing The Nose and SinusesAccey RamirezОценок пока нет
- RSKJikesiДокумент9 страницRSKJikesivonnyОценок пока нет
- Sense of SmellДокумент11 страницSense of SmelltarebentinaОценок пока нет
- OlfactionДокумент12 страницOlfactionbakex645Оценок пока нет
- 11 Nasal Cavity and Paranasal Sinuses-Dr - GosaiДокумент41 страница11 Nasal Cavity and Paranasal Sinuses-Dr - GosaiDr.B.B.GosaiОценок пока нет
- Data Isoman 24 Juni SD 5 Juli 2021Документ57 страницData Isoman 24 Juni SD 5 Juli 2021Nita ZahriОценок пока нет
- Stanford PulmicortДокумент1 страницаStanford Pulmicortcbr plansОценок пока нет
- Nose - Is The Sense Organ For Smelling.: (Traditional)Документ1 страницаNose - Is The Sense Organ For Smelling.: (Traditional)Kenneth Delos SantosОценок пока нет
- Childhood Nasal Foreign Bodies: Analysis of 1724 CasesДокумент4 страницыChildhood Nasal Foreign Bodies: Analysis of 1724 Caseshelda dwianaОценок пока нет
- Assessing The Nose and SinusesДокумент2 страницыAssessing The Nose and SinusesJo Hn VengzОценок пока нет