Академический Документы
Профессиональный Документы
Культура Документы
HTTP ::racodelallum - Blogspot.com - Es:2013:11:Respuestas Contrasentidos Historicos y 5.HTML
Загружено:
edmundo_mr3888Исходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
HTTP ::racodelallum - Blogspot.com - Es:2013:11:Respuestas Contrasentidos Historicos y 5.HTML
Загружено:
edmundo_mr3888Авторское право:
Доступные форматы
Aesth Plast Surg (2013) 37:11941201 DOI 10.
1007/s00266-013-0213-2
ORIGINAL ARTICLE
EXPERIMENTAL/SPECIAL TOPICS
Economic Analysis and Review of the Literature on ImplantBased Breast Reconstruction With and Without the Use of the Acellular Dermal Matrix
Jonathan Bank Nicole A. Phillips Julie E. Park David H. Song
Received: 1 May 2013 / Accepted: 29 August 2013 / Published online: 3 October 2013 Springer Science+Business Media New York and International Society of Aesthetic Plastic Surgery 2013
Abstract Background Use of the acellular dermal matrix (ADM) in two-stage implant-based breast reconstruction has been widely adopted. Despite an increasing focus on health care costs, few reports have addressed the nancial implications of ADM use. This study sought to examine the costs of the two-stage technique with and without ADM, concentrating on the direct variable costs of patient care during the expansion process. Methods A retrospective review of a prospectively maintained database was conducted. Data were collected on 132 cases resulting in a second-stage exchange for a permanent implant. The ndings showed that AlloDerm was used in 61 reconstructions and Strattice in 23 reconstructions. The primary outcome was the number of lls required to achieve the nal expander ll volume. The cost of subsequent patient encounters for expansion was estimated using institutional cost data. Results The number of lls required to achieve the nal volume was higher in the non-ADM group (6.5 1.7) than in the ADM group (3.6 1.4) (p \ 0.0001). No signicant difference was found in the small ll volumes (\350 ml; 5.3 vs. 3.7; p [ 0.05). The difference was signicant in the larger ll volumes ([500 ml; 8.3 vs. 3.7; p \ 0.05). Relative to non-ADM reconstruction, with AlloDerm at
current prices, the cost increase ranged from $2,727.75 for large reconstructions to $3,290.25 for small reconstructions ($2,167.75$2,739.25 with Strattice). Conclusion The use of ADM in two-stage reconstruction reduces the number of visits required for reconstructions with 350 ml or more. However, at current pricings, the direct cost of ADM use does not offset the cost savings from the reduced number of visits. Level of Evidence IV This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266. Keywords Economics Breast reconstruction Acellular dermal matrix
J. Bank J. E. Park D. H. Song (&) Department of Surgery, Section of Plastic and Reconstructive Surgery, University of Chicago Medical Center, 5841 South Maryland Avenue, Chicago, IL 60637, USA e-mail: songd@uchicago.edu; dsong@surgery.bsd.uchicago.edu N. A. Phillips Division of Plastic Surgery, Department of Surgery, Brigham and Womens Hospital, Boston, MA, USA
Implant-based breast reconstruction is the most common form of breast reconstruction after mastectomy. Of 96,277 breast reconstructions in the United States in 2011, 69,916 (72.6 %) were performed in two stages, with initial tissue expander placement followed by exchange for a permanent implant [1]. This two-stage approach has undergone revisions in recent years, including dual-plane positioning [24] over total submuscular prosthetic placement, the advent of the acellular dermal matrix (ADM), and the incorporation of ADM into the initial stage of alloplastic breast reconstruction. These techniques have been widely adopted by many reconstructive surgeons [3, 59]. The use of ADM provides support for the prosthesis and its coverage, limiting muscle dissection and resulting in decreased postoperative pain [10]. Further benets include reduced migration of the pectoralis major and stabilization of the prosthetic device itself [3, 11]. In addition,
123
Aesth Plast Surg (2013) 37:11941201
1195
incorporation of ADM allows for creation of a larger submuscular pocket and potentially greater expansion at the initial reconstruction time [3, 59]. However, signicant economic factors are associated with the use of ADM, including the cost of the material itself, operating times, physician fees, and the management of related complications. Despite an increasing focus on health care costs, only been a handful of reports have addressed the nancial implications of ADM use [1214]. Two recent studies [13, 14] have concluded that the most cost-effective option is single-stage implant (SSI) reconstruction with ADM. A third study has concluded that onestage reconstruction using AlloDerm (LifeCell Corporation, Branchburg, NJ, USA) does not differ signicantly in terms of cost from two-stage reconstruction without AlloDerm [12]. However, many patients are not candidates for SSI reconstruction [13]. Currently, only 10 % of all breast reconstructions are performed in one stage [1]. It is therefore relevant to examine the costs of the two-stage technique with and without the addition of ADM. To date, no published study has examined these two reconstructive options alone, and no previous studies have analyzed the direct variable costs of patient care during the expansion process. Intuitively, the greater initial expansion allowed by ADM reconstruction would result in fewer clinic visits and, consequently, decreased direct variable health care costs. Global costs, incorporating indirect costs such as patient time off work, would possibly be decreased as well. Our study aimed to evaluate formally the aspect of direct variable costs associated with the use of ADM in two-stage, implant-based breast reconstruction.
Fig. 1 Case inclusion
Materials and Methods A retrospective review of a prospectively maintained database was conducted in accordance with the University of Chicago Medical Center institutional review board. Data were collected on 176 consecutive postmastectomy breast reconstructions performed by the senior author (D. H. S.) between July 2002 and November 2011 (Fig. 1). The study included 132 cases (80 %) managed in two stages. Among the reconstructions in these cases, 48 were executed without the use of ADM (beneath the pectoralis major and the serratus anterior without elevation of the rectus abdominis). The remainder of the cases involved the use of ADM as an adjunct to the initial reconstruction, with 61 reconstructions performed using AlloDerm and 23 reconstructions using Strattice (LifeCell Corporation). Patient selection into the two groupsthose with reconstruction using ADM and those who had reconstruction without ADMlargely reects a shift in the senior authors reconstructive algorithm. No patients in our study had reconstruction with ADM before March 2005. The patients from 2002 to 2005 were included to make up a sufcient number of comparison cases by the same surgeon. After a period during which the materials and techniques associated with ADM use in breast reconstruction gained popularity and became more widely available and during which the senior author gained prociency with this technique, the majority of patients received ADM unless it was contraindicated or deemed unnecessary in the setting of ample soft tissue and muscular coverage. Currently, breast reconstruction with ADM is the standard of care in
123
1196
Aesth Plast Surg (2013) 37:11941201
our institution, and since 2010, all patients have undergone reconstruction using ADM as part of a standard protocol. The study excluded 11 cases that failed to meet the inclusion criteria or to achieve adequate follow-up evaluation. Subsequently, 33 cases that involved something other than a normal exchange were excluded from the analyses to allow accurate comparison of a single set of variable costs. The primary outcome examined was the number of tissue expander lls required to achieve the nal expander ll volume, a proxy for the number of clinic visits required to achieve this volume. All lls were via 50-ml increments in both study groups. Expander size, shape, and type were consistent throughout the entire study period for both groups. Additional variables assessed were patient age, percentage of bilateral cases, and initial and nal ll volumes of the tissue expander. Variables were analyzed two ways. First, the cases were divided into three study arms (AlloDerm, Strattice, and non-ADM). Analyses comparing age, number of bilateral cases, initial ll volume, number of lls, and nal ll volume showed no signicant differences between AlloDerm and Strattice (p [ 0.05 for all comparisons). Therefore, it was deemed appropriate to combine these cases (AlloDerm and Strattice) into one study arm (ADM). A second set of analyses involving the same variables then was performed using two study arms (ADM vs. nonADM). In addition, the primary outcome was studied with reference to the nal ll volume, subdivided arbitrarily into small-(\350 ml), medium-(350500 ml), and large([500 ml) volume reconstructions. Again, this was performed for both the three-armed study (AlloDerm vs. Strattice vs. non-ADM) and the two-armed analysis (ADM vs. non-ADM). Statistical analyses of patient age, initial ll volume, number of lls required to achieve the nal ll volume, and the average ll volume per clinic visit were carried out using analysis of variance (ANOVA). Post hoc comparisons among the study arm means used the Tukey procedure to control for the family-wise error rate of 0.05. Comparison of the percentage of bilateral cases and the nal ll volume distribution among the study arms was carried out using Chi square tests. A p value lower than 0.05 was considered statistically signicant. Previously published analyses on this topic have used presumed Medicare reimbursement rates and projected costs associated with expected complication rates to study the nancial implications of ADM use [13, 14]. For the purposes of our study, the total cost of each clinic encounter was estimated using expenditure data from our own institution. Calculations encompassed facility fees, labor costs, and miscellaneous variable costs (e.g., material
costs) associated with each clinic visit. The net present value calculation at the time of manuscript preparation was $187.50 per clinic visit. For the purposes of limiting confounding variable costs, including physician professional time, our methodology focused on the variable costs associated with expansion and held xed costs of health care delivery the same for these visits.
Results No statistically signicant differences were found between the study group arms when patient age or percentage of bilateral reconstructions was compared (p [ 0.05) (Tables 1, 2). When initial ll volume was examined, AlloDerm was found to have a mean initial ll volume of 235.7 ml, whereas Strattice had a mean ll volume of 278.3 ml. These initial ll volumes, although not signicantly different from one another (p [ 0.05), were each signicantly higher than the mean initial ll volume for the non-ADM group (84.2 ml). We therefore combined these two sets of patients into one study arm (ADM). Comparing ADM with non-ADM, we found that the ADM group had a
Table 1 Statistics by age in year of surgery n Three arms Non-ADM AlloDerm Strattice Two arms Non-ADM ADM
a
Mean SD
p valuea
48 61 23 48 84
44.4 9.5 47.9 11.1 44.7 9.1 44.4 9.5 47.0 10.6
0.1617
0.1603
SD standard deviation, ADM acellular dermal matrix Analysis of variance comparing study arm means
Table 2 Percentage of bilateral cases n (%) Three arms Non-ADM AlloDerm Strattice Two arms Non-ADM ADM ADM acellular dermal matrix
a
p value
22 (45.8) 61 (47.5) 11 (47.8) 22 (45.8) 40 (47.6)
0.9804
0.8434
Chi square test comparing percentages of bilateral cases among the study arms
123
Aesth Plast Surg (2013) 37:11941201
1197
signicantly higher initial ll mean (247.3 ml) than the non-ADM group (84.2 ml) (p \ 0.0001) (Table 3). A comparison of nal ll volumes between the three categories of size stratication showed no signicant difference in the nal ll volume distribution between the AlloDerm and Strattice groups (p [ 0.05), thus permitting a comparison between the combined non-ADM group and the ADM group. This showed a signicant difference in the nal ll volume distributions (p = 0.0137) (Table 4). In analyzing our primary outcome (the mean number of lls required to achieve nal ll volume), we found a signicant difference between the study group arms (p \ 0.0001) (Table 5). AlloDerm and Strattice, although not signicantly different from each other (p [ 0.05), each had a signicantly lower mean number of lls than the nonTable 3 Statistics on the initial ll (in ml) n Three arms Non-ADM AlloDerm Strattice Two arms Non-ADM ADM
a
ADM group. After these patient sets were combined into one study arm (ADM), comparison with the non-ADM group showed a signicantly lower mean number of lls (p \ 0.0001). The nal ll volume differed signicantly from the mean number of required lls in the comparison of nonADM and ADM within the size stratication (p = 0.0132) (Table 6). Among the patients whose nal ll volumes were considered medium (350500 ml) or large ([500 ml), the number of lls required to achieve the nal expander ll volume differed signicantly between the ADM and non-ADM groups (p \ 0.05). This difference
Table 5 Primary outcome: Statistics on the no. of lls n Three arms Mean SD p valuea
Mean SD
p valuea
Non-ADM AlloDerm Strattice Two arms Non-ADM ADM
a b
48 61 23 n 48 84
6.5 1.7c 3.7 1.4d 3.3 1.3d Average 6.5 1.7 3.6 1.4
c d
\0.0001b
48 61 23 n 48 84
84.2 65.9b 235.7 89.5a 278.3 118.5a Average 84.2 65.9b 247.3 99.4
a
\0.0001b
p valuea \0.0001b
p valuea \0.0001b
SD standard deviation, ADM acellular dermal matrix Analysis of variance Indicates a signicant difference in the nal ll volume distributions among the study arms c,d The letter designations (a,b) are assigned to denote differences. The study arms connected with the same letter do not differ signicantly (p [ 0.05)
SD standard deviation; ADM acellular dermal matrix Analysis of variance comparing mean initial ll among the study arms
Indicates that at least one study arm has a signicantly different mean initial ll (p \ 0.05)
a,b
Post hoc pairwise comparisons of means were carried out using the Tukey adjustment procedure with control for the family-wise error rate at 0.05. The study arms connected with the same letter do not differ signicantly
Table 6 Average number of lls per case by nal ll volume category Average of number of lls
Table 4 Final ll volume distribution Small (\350 ml) n (%) Three arms Non-ADM AlloDerm Strattice Two arms Non-ADM ADM
a
Small (\350 ml) Large ([500 ml) n (%) p valuea Three arms Non-ADM AlloDerm 0.0156b Strattice Two arms Non-ADM ADM 0.0137b 5.3 3.7
b b
Medium (350500 ml)
Large ([500 ml)
Total
Medium (350500 ml) n (%)
5.3b 3.7
b
6.3c 3.6 3.4 6.3 3.5
b b
8.3c 4.1 3.1 8.3 3.7
b b
6.5c 3.7b 3.3b Total 6.5c 3.6b
9 (18.8) 3 (4.9) 0 (0) 9 (18.8) 3 (3.6)
31 (64.6) 50 (82.0) 16 (69.6) 31 (64.6) 66 (78.6)
8 (16.7) 8 (13.1) 7 (30.4) 8 (16.7) 15 (17.9)
NA
c b
c b
ADM acellular dermal matrix
a
ADM acellular dermal matrix Chi square test comparing the nal ll volume distributions among the study arms
Indicates a signicant difference in the nal ll volume distributions among the study arms
This table should be read vertically. No statistical comparisons have been made among the nal ll volume categories within a study arm. Statistical comparisons among the study arms are made within each nal ll volume category only b,c The letter designations (a,b) are assigned to denote differences. The study arms connected with the same letter do not differ signicantly (p [ 0.05)
123
1198
Aesth Plast Surg (2013) 37:11941201
was not seen among the patients whose nal ll volume was considered small (\350 ml). Overall, the non-ADM cases required 6.5 1.7 visits, whereas the ADM cases required 3.6 1.4 visits to complete the expansion (Table 5). This difference was accentuated in the cases with a larger nal ll volume (8.3 for non-ADM vs. 3.7 for ADM) (Table 6). The smaller nal ll volumes showed a smaller difference in the number of visits (5.3 vs. 3.7). More patients in the ADM group achieved higher ll volumes (15 in the ADM group vs. 8 in the non-ADM group), and fewer cases in the ADM group had small volumes (3 vs. 9). Therefore, to normalize for nal ll volume distribution, we calculated the number of additional visits expected for non-ADM patients to achieve a comparable nal ll distribution. On the average, non-ADM patients would be expected to return an additional 0.42 times (95 % condence interval, 0.1780.655) to achieve the nal ll volume reected in the distribution seen in ADM cases. Accordingly, 40 % of nonADM patients would have one or more additional visits if the nal ll volume were normalized to the comparator group (ADM) using our standard 50-ml ll per visit. Table 7 shows the direct variable costs incurred by the visits required to achieve the nal ll volumes for the nonADM and ADM cases. Small nal ll volumes required fewer visits to achieve the nal ll, and there was less difference in the number of visits between the non-ADM
and ADM groups. Concordantly, the corrected cost differential was lower than that of the higher nal ll volume groups ($378.75). The higher the nal ll volume, the more ll visits were required, raising the variable cost per case. Relatively more visits were required for the non-ADM group than for the ADM group, resulting in an average additional cost of $941.25 to achieve the nal ll volume (Table 7). The market price of a 6 9 16-cm piece of thick AlloDerm in 2012 was $3,669. The price of a pliable 6 9 16cm piece of Strattice in 2012 was $3,109. The corrected costs for additional visits (0.42 additional visits per nonADM case) to normalize the nal ll volume distribution are shown as well. The nal corrected cost difference is highlighted.
Discussion An estimated 230,480 new cases of breast cancer were diagnosed in the United States in 2011 [15], and more women are electing to proceed with prophylactic mastectomies [16]. With the multitude of reconstructive options available, the number of patients affected by breast cancer, and the current economic climate, it is imperative that reconstructive surgeons be aware of the costs incurred by these procedures. However, as noted by de Blacam et al. [13], the balance between aesthetic outcome and nancial burden is not necessarily determined easily. Multiple authors have documented the aesthetic benets of two-stage breast reconstruction incorporating ADM, most notably the greater denition of the inframammary and lateral mammary folds achieved with ADM use [3, 5 9]. A recent systematic review by Jansen and Macadam [10] compared outcomes in studies examining the use of ADM in two-stage breast reconstruction with those in studies surveying non-ADM alloplastic reconstruction. Minor acute complication rates were determined to be comparable between the two groups, and lower rates of capsular contracture have been reported for reconstructions performed with ADM [7, 10]. Previous analyses determining the nancial impact of ADM use have calculated expenses based on direct health care costs incurred by procedures and hospital stays including operating room cost, anesthesia time, hospital fees, and stafng costs [1214]. Furthermore, they have calculated expected complication rates based on previously published reports, applying these costs to their overall analyses [13, 14]. De Blacam et al. [13] conducted a cost analysis of breast reconstruction comparing traditional two-stage implant-based reconstruction with two-stage reconstruction using ADM and with single-stage (directto-implant) reconstruction also using ADM. This study
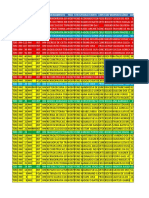
Table 7 Cost of ll visits per case by nal ll volume category (in $) Small (\350 ml) Three arms Non-ADM AlloDerm Strattice Difference Two arms Non-ADM Corrected cost ADM Difference Corrected difference Difference including AlloDerm Difference including Strattice 993.75 1072.5 693.75 -300 -378.75 3,290.25 1,181.25 1,260 656.25 -525 -603.75 3,065.25 1,556.25 1,635 693.75 -862.5 -941.25 2,727.75 1,218.75 1,297.5 675 543.75 -622.5 3,046.5 993.75 693.75 NA 300 1,181.25 675 637.5 506.25 1,556.25 768.75 581.25 787.5 1,218.75 693.75 618.75 525 Medium (350500 ml) Large ([500 ml) Total
2,730.25
2,505.25
2,167.75
2,486.5
ADM acellular dermal matrix, NA not available
123
Aesth Plast Surg (2013) 37:11941201
1199
calculated Medicare reimbursement for each procedure and incorporated probable additional costs incurred by complications. Presumed complication rates were based on a literature review examining reported outcomes per procedure. The most expensive procedure at baseline was found to be tissue expander/implant (TE/I) reconstruction with ADM ($11,255.78) followed by TE/I alone ($10,934.18) and SSI with ADM ($5,423.02). Higher complication rates were expected for procedures involving ADM, leading to an incremental rise in the cost of those procedures. The additional cost associated with ADM use was attributed to extended operating room time and greater material costs. In their calculations, these authors did not use the wholesale cost of ADM or the hospital fee charged for its use because of institutional and national variability, assuming that the relative difference in procedure cost incurred by the use of ADM would be similar if actual costs were used. Jansen and Macadam [14] published a similar cost analysis using a decision analytic model, calculating baseline and expected costs using assigned outcomes probabilities. These authors compared two-stage TE/I non-ADM reconstruction with SSI using ADM. Expected costs were calculated based on the Canadian payer structure and included direct medical costs associated with the procedures. A 6 9 16-cm sheet of AlloDerm was presumed to be the ADM graft material. The ndings showed that SSI with ADM was less expensive than the two-stage non-ADM procedure in both baseline noncomplicated cases (in Canadian dollars, $10,240 vs. $10,584) and in expected cost incorporating potential complications ($10,734 vs. $11,251). With a smaller ADM sheet (6 9 12 cm), the expected cost of SSI decreased to $9,673. However, these calculations assumed similar operative times for both methods. When a longer operative time for the single-stage technique was taken into account, the expected cost of SSI with ADM rose to $11,784. The investigators also performed a sensitivity analysis to examine the effect of presumed capsular contracture rates but found that changing these rates had little effect on the overall cost of either procedure. In focusing the discussion on direct costs and expected direct costs associated with complication probabilities, these studies underestimated the broader scope of the nancial burden covered in other analyses such as that recently published by Damen et al. [17]. These investigators in Holland performed a medium-term cost analysis of breast reconstruction options encompassing medical costs beyond the scope of the procedure itself, including consultations with other physicians, in-home nursing care, and physical therapy costs. Whereas these factors may not be pertinent to each type of reconstruction, other incorporated costs such as patient travel and productivity burdens are broadly applicable and can have a deep impact on the overall nancial burden of a chosen reconstructive option.
Costs associated with the expansion process have been largely excluded from previously published economic analyses of ADM use in breast reconstruction, except for a brief mention by Colwell et al. [12], who noted that the inclusion of extramural factors such as patient time off work would have resulted in a cost savings for SSI reconstruction. We began with the hypothesis that the direct and indirect costs incurred during the expansion process play a signicant role in the overall economics of alloplastic breast reconstruction. This hypothesis was not borne out by our results. Among the patients whose nal ll volumes were considered medium (350500 ml) or large ([500 ml), the ndings showed a statistically signicant difference in the number of lls required to achieve the nal expander ll volume between the ADM and non-ADM groups (Table 6). However, an average cost difference of roughly $3,000 remained if AlloDerm was used in the reconstruction ($2,500 with Strattice). The cost differences were lower when the reconstructions were larger (more expansion visits required). It should be noted that the calculations performed were based on general pricings of LifeCell products and not on specic contract pricings with any particular surgical practice. In theory, break-even calculations could be derived from the data presented in Table 7. No signicant difference was found between the study arms in terms of patient age, percentage of bilateral cases, or average ll volume achieved per outpatient clinic visit. However, statistically signicant differences were noted regarding initial ll volume and nal ll volume between the ADM and non-ADM group (Tables 3, 4). The difference in initial ll volume was expected because one primary advantage of the ADM technique over the traditional two-stage method is the greater initial expansion allowable due to the larger pocket. The higher percentage of patients in the non-ADM group who had a small nal ll volume (\350 ml; 18.8 vs. 3.6 % in the ADM group; p = 0.0137) could have been due to several factors. Because most reconstructions aim to restore the original breast size and shape, it is likely that these patients were expected to need less volume expansion and less prosthetic coverage. Therefore, they may have been selected for non-ADM reconstruction due to their anatomy. It also is possible that greater volume expansion was not appropriate for some patients, although 64.6 % of the patients in the non-ADM group achieved a medium nal ll volume (350500 ml), and 16.7 % achieved a large nal ll volume ([500 ml). The limitations of this study included those inherent to a single-center, single-surgeon study. The patient population factors in this study may not be applicable to all practice settings, and the gain of experience over time may inuence the results achieved with the same procedure.
123
1200
Aesth Plast Surg (2013) 37:11941201
Time as an independent variable also is specically relevant to this study. No patients in our study had reconstruction with ADM before March 2005. Because the materials and techniques associated with ADM use in breast reconstruction gained popularity and became more familiar, more patients in our study underwent this type of reconstruction. Currently, it is the standard of care in our institution, and the patients who underwent reconstruction in the later period of the study had reconstruction with ADM as part of a standard protocol. Based on our study, no cost advantage is associated with the use of ADM. Therefore, our continued decision to offer two-stage reconstruction using ADM is based on clinical criteria, and all patients are offered this form of reconstruction unless it is contraindicated or deemed unnecessary in the setting of ample soft tissue and muscular coverage. Prior studies [13, 14] have highlighted the fact that the costs associated with complications not only add to the overall cost associated with each type of reconstruction; they also complicate cost calculations. This study was a small, nonrandomized, retrospective investigation. We purposefully excluded from our study cases that involved anything other than a normal exchange of tissue expander for a permanent implant, designing our study to compare cost differences in noncomplicated cases so we would have an accurate comparison of a single set of variable costs. We recognize that costs incurred by the complications associated with each reconstructive option can be signicant. A prospective, randomized casecontrol study is indicated to address not only the economic burden of these reconstructive options but also the aesthetic and functional benets of ADM use and its associated complication and revision rates. Our study was specically designed to address the variable costs associated with the expansion process as it applies to two-stage reconstruction, currently the most common form of alloplastic breast reconstruction performed. However, because previous studies examining the nancial burden of ADM use in breast reconstruction have included single-stage reconstructions in their analyses [12 14], it would be interesting to compare all reconstructive options while taking the costs of the expansion process into account. Other factors to be considered in future economic studies analyzing the use of ADM in alloplastic breast reconstruction include the lower revision and capsular contracture rates reported in several studies [7, 10].
for women expected to reach nal ll volumes of at least 350 ml. However, the cost savings of reduced clinic visits do not offset the direct cost of ADM at the current pricings of the products used in this study. The economics of the expansion process should be included in further discussions on the nancial implications of ADM use in alloplastic breast reconstruction.
Acknowledgments This study was conducted with an unrestricted educational grant from LifeCell Corporation. The senior author was a paid consultant for LifeCell. Conicts of interest interest to disclose. The remaining authors have no conicts of
References
1. Report of the plastic surgery statistics (2011). http://www. plasticsurgery.org/Documents/news-resources/statistics/2010statisticss/Top-Level/2010-US-cosmetic-reconstructive-plasticsurgery-minimally-invasive-statistics2.pdf. Accessed 25 May 2012 2. Spear SL, Carter ME, Ganz JC (2006) The correction of capsular contracture by conversion to dual-plane positioning: technique and outcomes. Plast Reconstr Surg 118(7 Suppl):103S113S discussion 114S 3. Spear SL, Parikh PM, Reisin E, Menon NG (2008) Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg 32: 418425 4. Spear SL, Pelletiere CV (2004) Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants. Plast Reconstr Surg 113:20982103 5. Breuing KH, Colwell AS (2007) Inferolateral AlloDerm hammock for implant coverage in breast reconstruction. Ann Plast Surg 59:250255 6. Breuing KH, Warren SM (2005) Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg 55:232239 7. Rawlani V, Buck DW II, Johnson SA, Heyer KS, Kim JY (2011) Tissue expander breast reconstruction using prehydrated human acellular dermis. Ann Plast Surg 66:593597 8. Salzberg CA (2006) Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 57:15 9. Zienowicz RJ, Karacaoglu E (2007) Implant-based breast reconstruction with allograft. Plast Reconstr Surg 120:373381 10. Jansen LA, Macadam SA (2011) The use of AlloDerm in postmastectomy alloplastic breast reconstruction: part I. A systematic review. Plast Reconstr Surg 127:22322244 11. Bindingnavele V, Gaon M, Ota KS, Kulber DA, Lee DJ (2007) Use of acellular cadaveric dermis and tissue expansion in postmastectomy breast reconstruction. J Plast Reconstr Aesthet Surg 60:12141218 12. Colwell AS, Damjanovic B, Zahedi B, Medford-Davis L, Hertl C, Austen WG Jr (2011) Retrospective review of 331 consecutive immediate single-stage implant reconstructions with acellular dermal matrix: indications, complications, trends, and costs. Plast Reconstr Surg 128:11701178 13. de Blacam C, Momoh AO, Colakoglu S, Slavin SA, Tobias AM, Lee BT (2012) Cost analysis of implant-based breast reconstruction with acellular dermal matrix. Ann Plast Surg 69: 516520
Conclusion The use of ADM in two-stage reconstruction reduces the number of clinic visits required between the initial operation and the second operation for tissue expander exchange
123
Aesth Plast Surg (2013) 37:11941201 14. Jansen LA, Macadam SA (2011) The use of AlloDerm in postmastectomy alloplastic breast reconstruction: part II. A cost analysis. Plast Reconstr Surg 127:22452254 15. Cancer facts and gures 2011 from the American Cancer Society (2012). http://www.cancer.org/acs/groups/content/@epidemiolo gysurveilance/documents/document/acspc-029771.pdf. Accessed 25 May 2012
1201 16. Wood WC (2009) Should the use of contralateral prophylactic mastectomy be increasing as it is? Breast 18(Suppl 3):S93S95 17. Damen TH, Wei W, Mureau MA et al (2011) Medium-term cost analysis of breast reconstructions in a single Dutch centre: a comparison of implants, implants preceded by tissue expansion, LD transpositions, and DIEP aps. J Plast Reconstr Aesthet Surg 64:10431053
123
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Money Tooth BookДокумент41 страницаMoney Tooth BookVizi Adrian0% (2)
- Ref Des Medicaments Cnops 2014Документ770 страницRef Des Medicaments Cnops 2014doxydnitro67% (6)
- Studies in History and Philosophy of Science: Mary S. MorganДокумент12 страницStudies in History and Philosophy of Science: Mary S. Morganedmundo_mr3888Оценок пока нет
- Bates AS, Knepil GJ (Poster 65, Craniofacial) : ResultsДокумент1 страницаBates AS, Knepil GJ (Poster 65, Craniofacial) : Resultsedmundo_mr3888Оценок пока нет
- Gliding Mentoplasty PDFДокумент8 страницGliding Mentoplasty PDFedmundo_mr3888Оценок пока нет
- Torsoplasty PDFДокумент12 страницTorsoplasty PDFedmundo_mr3888Оценок пока нет
- AQCindecДокумент39 страницAQCindecedmundo_mr3888Оценок пока нет
- Coleman EsiteДокумент4 страницыColeman Esiteedmundo_mr3888Оценок пока нет
- Sports Vision G. JanssenДокумент35 страницSports Vision G. Janssenphilip davisОценок пока нет
- Abdominal "Signs" Table: Sign Diagnosis/ConditionДокумент1 страницаAbdominal "Signs" Table: Sign Diagnosis/ConditionMeg AmoonОценок пока нет
- Base 03 03 23Документ13 страницBase 03 03 23Jorge FilhoОценок пока нет
- Local Media577597190528174418Документ34 страницыLocal Media577597190528174418James Eugene CaasiОценок пока нет
- Quiz 3 MATERNAL BSN2 SFДокумент2 страницыQuiz 3 MATERNAL BSN2 SFElaiza Anne SanchezОценок пока нет
- Special Leave Benefits For Women PDFДокумент2 страницыSpecial Leave Benefits For Women PDFJoan CarigaОценок пока нет
- Medical Transcript FinishedДокумент6 страницMedical Transcript FinishedJason LeonaОценок пока нет
- Basic Anatomy: First YearДокумент10 страницBasic Anatomy: First YearRick DasОценок пока нет
- Mishermaliyani I11105026Документ49 страницMishermaliyani I11105026Dewi rafikaОценок пока нет
- Chest TraumaДокумент122 страницыChest TraumaMarina Maleș100% (1)
- ERBE PublicationДокумент240 страницERBE PublicationbenichiforОценок пока нет
- Periocular Hyaluronic Acid Fillers: Applications, Implications, ComplicationsДокумент6 страницPeriocular Hyaluronic Acid Fillers: Applications, Implications, ComplicationsLuis Fernando WeffortОценок пока нет
- 5 IV CannulationДокумент61 страница5 IV CannulationNursing Superintendent (SH)Оценок пока нет
- SH Catalogue - GynaecologyДокумент20 страницSH Catalogue - Gynaecologyمحمد خضير عليОценок пока нет
- Unitedhealthcare Dental Hmo Plan 2022 Summary of Benefits and CoverageДокумент9 страницUnitedhealthcare Dental Hmo Plan 2022 Summary of Benefits and CoverageAdam CliftonОценок пока нет
- EG-580UT Operation ManualДокумент112 страницEG-580UT Operation Manualkeng suttisangchanОценок пока нет
- Proliferative Vitreoretinopathy: Dr. Swati RamtekeДокумент22 страницыProliferative Vitreoretinopathy: Dr. Swati RamtekeSwati RamtekeОценок пока нет
- Aortic StenosisДокумент19 страницAortic StenosisPraveen RamasamyОценок пока нет
- Sentinel Lymph Node (SLN) Biopsy PDFДокумент5 страницSentinel Lymph Node (SLN) Biopsy PDFMDОценок пока нет
- PIIS0894731720307793Документ16 страницPIIS0894731720307793Shin Elcant Del BarçaОценок пока нет
- Wound Dressing ChecklistДокумент3 страницыWound Dressing ChecklistBUAHIN JANNA100% (1)
- 14 StomachДокумент24 страницы14 Stomachafzal sulemaniОценок пока нет
- HematotoraksДокумент15 страницHematotorakssafanj12Оценок пока нет
- Basal Cell Carcinoma Workup - Approach Considerations, Skin Biopsy, CytologyДокумент12 страницBasal Cell Carcinoma Workup - Approach Considerations, Skin Biopsy, CytologyyanuarrisaldiОценок пока нет
- Surgical IncisionДокумент35 страницSurgical IncisionJoshua SmithОценок пока нет
- Referat EndosДокумент29 страницReferat EndosShenaquitaIvandraОценок пока нет
- Implants in Esthetic ZoneДокумент10 страницImplants in Esthetic ZoneInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Debate ScriptДокумент5 страницDebate ScriptzahraumaiyaОценок пока нет