Академический Документы
Профессиональный Документы
Культура Документы
Assess Extrinsic Pathway (Tissue Factor Pathway) Prothrombin Time / PT Test / INR
Загружено:
Kristin DouglasИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Assess Extrinsic Pathway (Tissue Factor Pathway) Prothrombin Time / PT Test / INR
Загружено:
Kristin DouglasАвторское право:
Доступные форматы
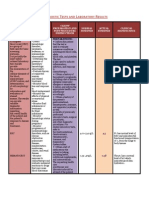
HIS 11,12 - Anticoagulant Drugs Compare and contrast the different types of blood clotting tests.
Both require blood that is freshly drawn or stored in an appropriate anti-coagulant (EDTA, Citrate, ACD or thrombin inhibitors such as hepatin)
1. Assess Extrinsic Pathway (Tissue factor pathway)
i. Prothrombin time / PT test / INR Whole blood in glass tube would result in clotting in 5-11 minutes Whole blood in a vaccutainer w/ anti-coagulant it would not clot However, you can also add back Ca++ to overcome anticoagulant If you also add tissue factor, it will clot very fast (12-14 seconds this is refered to as the Prothrombin time or PT = extrinsic pathway of CC) Time will determine if blood clots properly. Since PT varies, the prothrombin ratio (PR) is the PT of patient / PT of normal pooled plasma, 0.8-1.2 is considered normal. Recombinant human proteins are used to calculate the International Normalised ratio (INR) which is the reference of PR and can be effected by smoking, alcohol, drugs, illness (liver disease), stress, and climate.
2. Assess Intrinsic Pathway
i.
Activated partial thromboplastin time
Anti-coagulated whole blood and calcium, phospholipid, silica, celite, kaeolin or ellagic acid, (Partial because NO TF), the clot forms within 33 s = activated partial thromboplastin time (aPTT)
ii.
D-Dimer test D-dimer is a specific degradation fragment of cross-linked fibrin. Produced naturally as part of the wound healing process by plasmin degradation
of thrombus (Long half-life) Measurement used to aid diagnosis of systemic thrombosis A positive D-dimer result may indicate the presence of an abnormally high level of fibrin degradation products (Recent thrombotic event)
Explain common disorders of coagulation, their diagnosis and treatment.
Too little coagulation Inherited Disorders: Haemophilia A: Factor VIII, B: Factor IX Give purified/recombinant Factor VII Aquired Disorders Liver disease (Alcoholic liver disease) or Vitamin K deficiency (Haemorrhagic disease of newborn) Give vitamin K supplement Too much coagulation: Venous Disorders: Caused by artificial surfaces, prolonged stasis (post-surgery), arterial fibrillation, deficiency in reg factors, smoking, cancer, obesity Oral Anti-coagulants Warfarin (Vitamin K antagonist) Injectable Anti-coagulants Heparin (acts as an anti Thrombin)
Arterial Thrombosis Induced Disorders MI, angina, stroke, peripheral artery disease Excessive demand of coagulation - Severe wounds Prevention: antiplatelet drugs New drug: NOVA 7, functions where TF Treatment: Thrombolytic drugs: tissue present at wound site, plasminogen activator (tPA), streptokinase
Summarize the different classes of anti- coagulant drugs, their mode of administration and side effects.
Many drugs are vitamin K antagonists which inhibit coagulation cascade from proceeding at (II, VII, IX, X) Warfarin and other Coumarins o Treatment of venous thrombosis (long flight, or immobile hospital patient) or secondary prophylaxia (individuals who have already formed a blood clot to prevent future blood clots) o Admin'd orally but takes a long time (8h to 4 days) to deplete stores in body o 99% plasma protein bound (Can interact with other drugs and their activity) o Metabolized by cytochrome P450 in liver. o Warfarin dosage needs careful monitoring by (PT) test Vitamin K is necessary for coagulation and is synthesized by bacteria in the gut.
Compare and contrast Intravenous anticoagulants: Heparin and lowmolecular weight heparins with oral anticoagulants: warfarin and the newer (oral) anti-coagulants: direct thrombin inhibitors Dabigatrin.
Warfarin Oral, very slow onset/offset Long term use, cheap Careful monitoring by INR Treats: venous thrombosis Heparin (LMWH) Intravenous, immediate onset of action Short term use, cheap Careful monitoring by aPTT and HIT Treats: DVT, Pul embolism, acute MI Dabigatrin Direct thrombin inhibitor, prodrug, does not need careful monitoring, more expensive No antidote for it but allows predictable anticoagulation.
Explain the role of intact endothelium in regulating haemostasis.
Thrombomodulin is expressed on the surface of intact endothelial cells. Binds to thrombin and forms a 1:1 (TT) complex which functions to: o TT cannot activate fibrinogen o TT converts regulatory protein, Protein C, to its active form (APC) o APC and Protein S degrade Factors Va and VIIIa Heparan sulphate proteoglycans are synthesized by endothelial cells and expressed on the surface of intact cells. Enhances the inhibitory potency of Antithrombin III o AT-III weak inhibitor of thrombin, Combined w/ AT-III to be a more potent inhibitor (1000 fold) o Heparen and AT-III complex inhibits both Thrombin and Xa
Identify the drugs that impact on the thrombolytic pathway.
**IIa inhibitor include Dabigatran
Вам также может понравиться
- Medication Cheat Sheet For ClinicalДокумент4 страницыMedication Cheat Sheet For Clinicalanny100% (2)
- Group 3 Cardiovascular ProblemДокумент52 страницыGroup 3 Cardiovascular ProblemWARREN WILLIAM PERAN100% (3)
- Med-Surg Nusing BulletsДокумент65 страницMed-Surg Nusing BulletsHarley C. Tan100% (1)
- Hemostasis, Surgical Bleeding and TransfusionДокумент48 страницHemostasis, Surgical Bleeding and Transfusionaddelins100% (1)
- Slide Kuliah Transfusi DarahДокумент31 страницаSlide Kuliah Transfusi Darahfenti nurul khafifahОценок пока нет
- Warfarin LeafletДокумент2 страницыWarfarin LeafletchampbeeОценок пока нет
- AQUISEL Tubos Instrucciones-EnglishДокумент20 страницAQUISEL Tubos Instrucciones-Englishkukuh100% (1)
- Bleeding Time, Clotting Time PT and PTT2Документ41 страницаBleeding Time, Clotting Time PT and PTT2Qurrataini Ibanez100% (1)
- Pathology Outlines - Abnormal PT and PTT - CausesДокумент1 страницаPathology Outlines - Abnormal PT and PTT - CausesShane AranetaОценок пока нет
- 4 TH Hematology LectureДокумент13 страниц4 TH Hematology LectureneversighsОценок пока нет
- Drugs Affecting Coagulation ObjectivesДокумент14 страницDrugs Affecting Coagulation ObjectiveslouradelОценок пока нет
- Bleeding TimeДокумент47 страницBleeding Timechickenbacon34Оценок пока нет
- Bleeding in A NeonateДокумент36 страницBleeding in A NeonateDrBibek AgarwalОценок пока нет
- Cogulation Profile: Bleeding Time, Clotting Time, PT, and PTTДокумент49 страницCogulation Profile: Bleeding Time, Clotting Time, PT, and PTTDorin PathakОценок пока нет
- PHM - Hematologic DrugsДокумент3 страницыPHM - Hematologic DrugsJeanne Rodiño100% (3)
- Pharmacology - Hematologic DrugsДокумент51 страницаPharmacology - Hematologic DrugsBenjamin Joel Breboneria100% (1)
- Venous Thromboembolism (Vte) : Abdullah Al Dahbali, Mpharm, PHDДокумент23 страницыVenous Thromboembolism (Vte) : Abdullah Al Dahbali, Mpharm, PHDعزالدين الطيارОценок пока нет
- Bleeding DisorderДокумент56 страницBleeding DisorderPriya Singh100% (1)
- Coagulation DisordersДокумент20 страницCoagulation DisordersAnuj SharmaОценок пока нет
- Complex Process Terminates Blood Loss From The Intravascular SpaceДокумент25 страницComplex Process Terminates Blood Loss From The Intravascular SpaceDewi YukinohanaОценок пока нет
- Coagulation Cascade: Anticoagulant DrugsДокумент14 страницCoagulation Cascade: Anticoagulant Drugsabdo elbahrawyОценок пока нет
- Anti CoagulantsДокумент25 страницAnti Coagulantsshoaib106muhammadОценок пока нет
- CTBTДокумент45 страницCTBTimpi belindaОценок пока нет
- Coagulation TestДокумент5 страницCoagulation TestZahid HussainОценок пока нет
- Coagulation DisordersДокумент40 страницCoagulation DisordersDr. Shatdal Chaudhary100% (6)
- NCP-risk For BleedingДокумент3 страницыNCP-risk For BleedingAce Dioso Tubasco100% (2)
- Banua, Latigar, Rona - PCOL 2 - ReviewerДокумент61 страницаBanua, Latigar, Rona - PCOL 2 - ReviewerDiane BanuaОценок пока нет
- Coagulopathy in Cardiac Surgery1Документ63 страницыCoagulopathy in Cardiac Surgery1Mohammed Abdul ShafiОценок пока нет
- Hematology FA - 1Документ78 страницHematology FA - 1JaankiОценок пока нет
- Path 548 Coag Disorders 20150323Документ38 страницPath 548 Coag Disorders 20150323Bakul DalalОценок пока нет
- Coagulation: Bleeding TimeДокумент6 страницCoagulation: Bleeding TimeimperiouxxОценок пока нет
- Pain Management (DIS Perawat SMF Obgyn)Документ35 страницPain Management (DIS Perawat SMF Obgyn)Ceza DeimosОценок пока нет
- HaemostasisДокумент34 страницыHaemostasiskgzyvqqr4jОценок пока нет
- Anticoagulants ParamedДокумент20 страницAnticoagulants ParamedManikanta GupthaОценок пока нет
- ReviewerДокумент20 страницReviewerKC PalattaoОценок пока нет
- 1120314晨會 Miller Ch50. Patient Blood Management CoagulationДокумент56 страниц1120314晨會 Miller Ch50. Patient Blood Management Coagulationw8412358Оценок пока нет
- Cardio Lab MedsДокумент11 страницCardio Lab MedsDianne Erika MeguinesОценок пока нет
- Managing Coagulopathy ICUДокумент38 страницManaging Coagulopathy ICUMirabela Colac100% (1)
- Blood Coagulation and FibrinolysisДокумент63 страницыBlood Coagulation and FibrinolysisNora AboshanadyОценок пока нет
- Disorders of CoagulationДокумент27 страницDisorders of CoagulationRishikesh HukeriОценок пока нет
- Anticoagulants: Dr. Hassan Mohamed EnowДокумент37 страницAnticoagulants: Dr. Hassan Mohamed EnowFatimaОценок пока нет
- Acquired Coagulation - Disorders - 6Документ17 страницAcquired Coagulation - Disorders - 6jhonnybroОценок пока нет
- Blood - Anticoagulants: Ravi Sankar Venuturumilli, MD Global Hospitals, HyderabadДокумент30 страницBlood - Anticoagulants: Ravi Sankar Venuturumilli, MD Global Hospitals, HyderabadDrRavisankar VenuturumilliОценок пока нет
- Surgery FinalДокумент6 страницSurgery FinalMaebritt TibubosОценок пока нет
- When and How To Use Direct Oral Anticoagulants in Patients With Advanced Chronic Liver Disease?Документ6 страницWhen and How To Use Direct Oral Anticoagulants in Patients With Advanced Chronic Liver Disease?Felipe SotoОценок пока нет
- Hematologic Pathology p1-23Документ23 страницыHematologic Pathology p1-23zeroun24100% (2)
- Pharmacology RCR1 - CardioДокумент8 страницPharmacology RCR1 - CardioeamcrawleyОценок пока нет
- Anticoagulant/Thrombolytic 1. Anticoagulant: Parenteral AnticoagulantsДокумент4 страницыAnticoagulant/Thrombolytic 1. Anticoagulant: Parenteral AnticoagulantsHannaОценок пока нет
- Anticoagulants and AntiplateletsДокумент25 страницAnticoagulants and AntiplateletsIdrissa John Sebeh ContehОценок пока нет
- Disseminated Intravascular Coagulation: Keith Lewis, MDДокумент37 страницDisseminated Intravascular Coagulation: Keith Lewis, MDTimea DaniОценок пока нет
- Coagulation Disorders in Liver DiseaseДокумент14 страницCoagulation Disorders in Liver DiseaseVanessa MillarОценок пока нет
- Pathology Bleeding DisordersДокумент67 страницPathology Bleeding DisordersMarcelliaОценок пока нет
- Pos NoacДокумент40 страницPos NoacSanjeev Harry Budhooram100% (1)
- Coumadins (Vitamin K Antagonists)Документ7 страницCoumadins (Vitamin K Antagonists)Marvz BulawitОценок пока нет
- OLT Without BloodДокумент39 страницOLT Without BloodeodisseevaОценок пока нет
- Trombosis: DR - Suhaemi, SPPD, FinasimДокумент49 страницTrombosis: DR - Suhaemi, SPPD, FinasimLailatul AzizahОценок пока нет
- Final DX ResultsДокумент9 страницFinal DX ResultszysheaiОценок пока нет
- CoA Dis - RevДокумент60 страницCoA Dis - RevAzra Al AmanahОценок пока нет
- PTTДокумент6 страницPTTFitz JaminitОценок пока нет
- Blood Pharmacology 2Документ47 страницBlood Pharmacology 2Sosu YeОценок пока нет
- Case PresentationДокумент36 страницCase Presentationalmas khanОценок пока нет
- Idiopathic Thrombocytopenic PurpuraДокумент10 страницIdiopathic Thrombocytopenic PurpuramariakolandaОценок пока нет
- Novel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya SharmaДокумент8 страницNovel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya Sharma9493.karthikОценок пока нет
- Drugs Used in Disorders of CoagulationДокумент60 страницDrugs Used in Disorders of CoagulationTwinkle MazaredoОценок пока нет
- Deep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edОт EverandDeep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edРейтинг: 5 из 5 звезд5/5 (1)
- M9.22 - Drug MetabolismДокумент2 страницыM9.22 - Drug MetabolismKristin DouglasОценок пока нет
- HIS26: Rheumatoid Arthritis Describe The Manifestations and Consequences of Rheumatoid ArthritisДокумент2 страницыHIS26: Rheumatoid Arthritis Describe The Manifestations and Consequences of Rheumatoid ArthritisKristin DouglasОценок пока нет
- NM Learning Outcomes 1-25Документ113 страницNM Learning Outcomes 1-25Kristin DouglasОценок пока нет
- JC1 Final Exam PrepДокумент3 страницыJC1 Final Exam PrepKristin DouglasОценок пока нет
- HIS19: Infection and Disease. Outline The History of Infectious DiseaseДокумент1 страницаHIS19: Infection and Disease. Outline The History of Infectious DiseaseKristin DouglasОценок пока нет
- His 7Документ3 страницыHis 7Kristin DouglasОценок пока нет
- His 10Документ2 страницыHis 10Kristin DouglasОценок пока нет
- CPB 11 Ligand Receptor Interactions 1Документ3 страницыCPB 11 Ligand Receptor Interactions 1Kristin DouglasОценок пока нет
- HIS 6 - Haemoglobin Recall Oxygen Binding Properties of HB: Iron (II) - Protoporphyrin IXДокумент2 страницыHIS 6 - Haemoglobin Recall Oxygen Binding Properties of HB: Iron (II) - Protoporphyrin IXKristin DouglasОценок пока нет
- Immunosuppressant Drugs Drug Name Class Function Method/Receptor UseДокумент3 страницыImmunosuppressant Drugs Drug Name Class Function Method/Receptor UseKristin DouglasОценок пока нет
- Surgery Recommended For Patients With BMI 40, Hyperlipidemia, Hypertension, Diabetes Resolved in 70% of CasesДокумент2 страницыSurgery Recommended For Patients With BMI 40, Hyperlipidemia, Hypertension, Diabetes Resolved in 70% of CasesKristin DouglasОценок пока нет
- CPB 25Документ2 страницыCPB 25Kristin DouglasОценок пока нет
- Haemosiderosis: CPB 16 - 28 - Diseases, Drugs and Clinical ExamplesДокумент4 страницыHaemosiderosis: CPB 16 - 28 - Diseases, Drugs and Clinical ExamplesKristin DouglasОценок пока нет
- Drugs:: CPB10 - Intro To PharmacologyДокумент1 страницаDrugs:: CPB10 - Intro To PharmacologyKristin DouglasОценок пока нет
- CPB 6 From Nucleotides To ProteinsДокумент2 страницыCPB 6 From Nucleotides To ProteinsKristin DouglasОценок пока нет
- CPB 3 Principles of NutritionДокумент2 страницыCPB 3 Principles of NutritionKristin DouglasОценок пока нет
- CPB 1 Describe The Basic Details of The Four Major Classes of Biological MoleculesДокумент1 страницаCPB 1 Describe The Basic Details of The Four Major Classes of Biological MoleculesKristin DouglasОценок пока нет
- Cisapride Is Also Used When Nothing Else Works But Has Fatal Cardiac Arrhythmias PossibleДокумент5 страницCisapride Is Also Used When Nothing Else Works But Has Fatal Cardiac Arrhythmias PossibleKristin DouglasОценок пока нет
- Chapter 23 - Chronic Anticoagulation - Crossing The "Bridge" Level IIДокумент5 страницChapter 23 - Chronic Anticoagulation - Crossing The "Bridge" Level IIela.sofiaОценок пока нет
- PT-INR TestДокумент5 страницPT-INR Testmandawa786Оценок пока нет
- Antithrombotic Treatment GuidelinesДокумент9 страницAntithrombotic Treatment GuidelinesAnh NguyenОценок пока нет
- Thyme Increase The Levothyroxine Dose by 30-50%: This Is For Mild To Moderate But For Severe We Will Give Him TriptansДокумент66 страницThyme Increase The Levothyroxine Dose by 30-50%: This Is For Mild To Moderate But For Severe We Will Give Him TriptansOuf'ra AbdulmajidОценок пока нет
- SICH MGMTДокумент12 страницSICH MGMTLennon Ponta-oyОценок пока нет
- Citrasate: Product ManualДокумент30 страницCitrasate: Product ManualfidabimeeОценок пока нет
- Periodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsДокумент8 страницPeriodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsYehya Al KhashabОценок пока нет
- Anti-Coagulants & Fibrinolytics Feb 2019Документ50 страницAnti-Coagulants & Fibrinolytics Feb 2019Muhd NuhОценок пока нет
- Impedance Measurement Monitors Blood Coagulation - CN PDFДокумент3 страницыImpedance Measurement Monitors Blood Coagulation - CN PDFchshfengОценок пока нет
- Overview of Acute Pulmonary Embolism in AdultsДокумент18 страницOverview of Acute Pulmonary Embolism in AdultscrucaioОценок пока нет
- Therapeutic Apheresis: Inside The Black BoxДокумент70 страницTherapeutic Apheresis: Inside The Black BoxAhmad Ripani Musyaffa AhdanLabОценок пока нет
- PRP PreparationДокумент12 страницPRP PreparationhalegaОценок пока нет
- Liv HaemДокумент166 страницLiv HaemvistamaniacОценок пока нет
- European J of Haematology - 2020 - Rasmussen - Unexpected Isolated Activated Partial Thromboplastin Time Prolongation AДокумент7 страницEuropean J of Haematology - 2020 - Rasmussen - Unexpected Isolated Activated Partial Thromboplastin Time Prolongation Akallolchakraborty779204Оценок пока нет
- Phlebotomy SopДокумент11 страницPhlebotomy SopLourdette TorrefielОценок пока нет
- Full Download Book Usmle Step 2 Secrets PDFДокумент41 страницаFull Download Book Usmle Step 2 Secrets PDFpeter.davis552100% (14)
- Preoperative Evaluation and Preparation For Anesthesia and SurgeryДокумент18 страницPreoperative Evaluation and Preparation For Anesthesia and SurgeryanantosbiОценок пока нет
- Jointly Team: SMLE GroupДокумент31 страницаJointly Team: SMLE GroupAkpevwe EmefeОценок пока нет
- Pharma Nca1 Notes MidtermДокумент8 страницPharma Nca1 Notes MidtermAICEL A. ABILОценок пока нет
- Oral Anticoagulation in Patients With Chronic Liver DiseaseДокумент23 страницыOral Anticoagulation in Patients With Chronic Liver DiseaseSophia PapathanasiouОценок пока нет
- A Systematic Review of Warfarin Use in Post-Bariatric Surgery PatДокумент6 страницA Systematic Review of Warfarin Use in Post-Bariatric Surgery PatGestne AureОценок пока нет
- Spring 2022 Longitudinal Ippe SyllabusДокумент7 страницSpring 2022 Longitudinal Ippe Syllabusapi-602288180Оценок пока нет
- Ghicavîi Victor: - Name: Creliciuc Maria - Age: 64ani (15/04/1949) - Location: KishinauДокумент30 страницGhicavîi Victor: - Name: Creliciuc Maria - Age: 64ani (15/04/1949) - Location: KishinauMoataz TrabehОценок пока нет
- AHCCCS Pharmacy and Therapeutics Committee May 19, 2021Документ247 страницAHCCCS Pharmacy and Therapeutics Committee May 19, 2021hussam mazinОценок пока нет
- Deep Vein ThrombosisДокумент15 страницDeep Vein ThrombosisAngela TenorioОценок пока нет