Академический Документы
Профессиональный Документы
Культура Документы
Paediatric Gastroenterology
Загружено:
ibbs91Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Paediatric Gastroenterology
Загружено:
ibbs91Авторское право:
Доступные форматы
Gastroenterolgy Presentations:
1.Vomiting:
Is the forceful ejection of gastric contents. Often benign and due to feeding disorders or mild GORD or gastroenteritis. Causes of vomiting in children red flags Associated clinical features Differential diagnoses Bile-stained vomit Haematemesis Projectile vomiting, in first few weeks of life Vomiting at the end of paroxysmal coughing Abdominal distension Hepatosplenomegaly Blood in the stool Severe dehydration, shock Intestinal obstruction Oesophagitis, peptic ulceration, oral/nasal bleeding Pyloric stenosis Whooping cough (pertussis) Intestinal obstruction, including strangulated inguinal hernia Chronic liver disease Intussusception, gastroenteritis salmonella or campylobacter Severe gastroenteritis, systemic infection (urinary tract infection, meningitis), diabetic ketoacidosis Raised intracranial pressure Gasto-oesophageal reflux, coeliac disease and other chronic gastrointestinal conditions
Bulging fontanelle or seizures Failure to thrive
Gastro-oesophageal reflux Occurs in otherwise normal infants, but risk is increased if neuromuscular problems or surgery to the oesophagus or diaphragm Investigations: (24hr pH monitoring, endoscopy) are performed if diagnosis is unclear or complications occur such as failure to thrive, oesophagitis and pulmonary aspiration. Management: Treated if troublesome with upright positioning, thickening, medication and sometimes fundoplication. Pyloric stenosis More common in Clinical features: forcefulness over feed
boys
and those with
maternal family history and
Vomiting, which increases in frequency time, ultimately becoming projectile
Signs: visible gastric peristalsis, palpable abdominal mass on test and possible dehydration Associated with hyponatraemia, hypokalaemia and hypochloraemic alkalosis
feed
Investigations: Diagnosis
may be
confirmed
by ultrasound
Management: Treated by surgery- pyloromyotomy after rehydration (0.45% saline and 5% dextrose with potassium supplements) and correction of electrolyte imbalance
2. Abdominal Pain
Causes of acute abdominal pain
Intra-abdominal Medical Surgical
Extra-abdominal
Acute appendicitis, Intestinal obstruction including intussusception, Inguinal hernia, Peritonitis, Inflamed Meckel diverticulum, Pancreatitis, Trauma
Non-specific abdominal pain, Gastroenteritis, Urinary tract: urinary tract infection acute pyelonephritis hydronephrosis renal calculus HenochSchnlein purpura, Diabetic ketoacidosis, Sickle cell disease, Hepatitis, Inflammatory bowel disease, Constipation, Recurrent abdominal pain of childhood, Gynaecological in pubertal females, Psychological, Lead poisoning, Acute porphyria (rare), Unknown
Upper respiratory tract infection, Lower lobe pneumonia,Torsion of the testis, Hip and spine problems.
Acute Appendicitis Commonest cause of abdominal pain in childhood. Occurs at any age, but uncommon in children <3. Clinical features: Symptoms Anorexia, Vomiting, Abdominal pain, initially central and colicky (appendicular midgut colic), localising to the RIF (from localised peritoneal inflammation) Signs: Flushed face, fever 37.238C, Abdominal pain worse on movement, Persistent tenderness with guarding in the RIF (McBurneys point). Management: Surgical Intussusception Invagination of proximal bowel into a distal segment. Occurs 3 months and 2 years Clinical features: paroxysmal colicky pain (sausage shaped) redcurrant jelly stool with pallor, abdominal
between
mass
Management: Reduction is attempted by rectal air insufflation unless peritonitis is present Surgery is required if reduction with air is unsuccessful or for peritonitis. Shock is an important complication and requires urgent treatment
Coeliac disease A gluten-sensitive enteropathy
Clinical features: Classical presentation is at 824 months with abnormal stools, failure to thrive, abdominal distension, muscle wasting and irritability Can have short stature, anaemia. Diagnosis: positive serology (IgA tissue transglutaminase and endomysial antibodies), flat mucosa on jejunal biopsy and resolution of symptoms and catch-up growth upon gluten withdrawal Management: gluten-free diet for life
Crohns disease A transmural, focal, subacute or chronic inflammatory disease, most affecting the distal ileum and proximal colon. commonly
Clinical features: General ill health: fever, lethargy, weight loss, growth failure, puberty delayed, Classical presentation (25%), abdominal pain, diarrhoea, weight loss Raised ESR/CRP Diagnosis: based on biopsy
Management: Remission is induced with nutritional therapy, when the normal diet is replaced by whole protein modular feeds (polymeric diet) for 68 weeks. This is effective in 75% of cases. Systemic steroids are required if ineffective. Immunosuppressant medi-cation (azathioprine, mercaptopurine or methotrexate), anti-TNF Ulcerative colitis Recurrent, inflammatory and ulcerating disease involving the the colon. 90% of children have a pancolitis. Clinical features: presents with rectal bleeding, pain. Weight loss and growth failure mucosa of
diarrhoea and colicky
Management: In mild disease, aminosalicylates used for maintenance Extensive disease requires steroids for acute exacerbations and immunosuppresants azathioprine Colectomy with an ileostomy or ileorectal pouch is undertaken for severe disease References Rapid peads Illustrated colour text of paediatrics
Вам также может понравиться
- SJT Answers & RationaleДокумент76 страницSJT Answers & RationaleFarhan SakunОценок пока нет
- London GP GroupsДокумент13 страницLondon GP Groupsibbs91Оценок пока нет
- A Year in The Life of A GP RegistrarДокумент2 страницыA Year in The Life of A GP RegistrarShahriar Kabir DaneОценок пока нет
- Appendix 1 - Person Specification Recruitment To One-Year Fixed Term Stand-Alone F2 ProgrammeДокумент3 страницыAppendix 1 - Person Specification Recruitment To One-Year Fixed Term Stand-Alone F2 Programmeibbs91Оценок пока нет
- Peterborough and Stamford Hospitals Nhs Foundation TrustДокумент5 страницPeterborough and Stamford Hospitals Nhs Foundation Trustibbs91Оценок пока нет
- Equipment Trolleys PDFДокумент7 страницEquipment Trolleys PDFibbs91Оценок пока нет
- MRCP 2016 September 1Документ32 страницыMRCP 2016 September 1ibbs91Оценок пока нет
- CCT in Icm Part III - Syllabus 2017 v2.3 PDFДокумент88 страницCCT in Icm Part III - Syllabus 2017 v2.3 PDFmarius vaidaОценок пока нет
- SJT Practice Paper 2 Answers Rationales 26-10-17Документ99 страницSJT Practice Paper 2 Answers Rationales 26-10-17scribdbazo100% (1)
- Tutorials Jan To July 2019Документ1 страницаTutorials Jan To July 2019ibbs91Оценок пока нет
- Case-Based Discussion (CBD) Assessment FormДокумент4 страницыCase-Based Discussion (CBD) Assessment Formibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
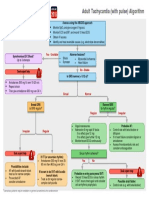
- G2015 Adult Tachycardia PDFДокумент1 страницаG2015 Adult Tachycardia PDFibbs91Оценок пока нет
- Pharma Pass Medicin 2020Документ654 страницыPharma Pass Medicin 2020VikrantОценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- KaleДокумент1 страницаKaleibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- Verbal Reasoning Word List 14Документ4 страницыVerbal Reasoning Word List 14ibbs91Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Off Grid Solar Hybrid Inverter Operate Without Battery: HY VMII SeriesДокумент1 страницаOff Grid Solar Hybrid Inverter Operate Without Battery: HY VMII SeriesFadi Ramadan100% (1)
- World BankДокумент28 страницWorld BankFiora FarnazОценок пока нет
- Intercultural Personhood and Identity NegotiationДокумент13 страницIntercultural Personhood and Identity NegotiationJoão HorrОценок пока нет
- ManualДокумент24 страницыManualCristian ValenciaОценок пока нет
- Richardson ResumeДокумент3 страницыRichardson Resumeapi-549248694Оценок пока нет
- Arc Hydro - Identifying and Managing SinksДокумент35 страницArc Hydro - Identifying and Managing SinkskbalОценок пока нет
- A Method For Prediction of Gas/Gas Ejector PerformanceДокумент6 страницA Method For Prediction of Gas/Gas Ejector PerformancedhavaleshОценок пока нет
- 1id Abstracts Season 2 Episode 6Документ406 страниц1id Abstracts Season 2 Episode 6Jennifer BrownОценок пока нет
- CESCOM 10 - Aircraft Status Report: Maintenance InspectionsДокумент78 страницCESCOM 10 - Aircraft Status Report: Maintenance InspectionsAlejandro BarradasОценок пока нет
- Installation of Submarine PE PipesДокумент84 страницыInstallation of Submarine PE Pipeswaseemiqbal133100% (2)
- The Other Twelve Part 1Документ5 страницThe Other Twelve Part 1vv380100% (2)
- Lesson Plan Letter SДокумент4 страницыLesson Plan Letter Sapi-317303624100% (1)
- Charles Zastrow, Karen K. Kirst-Ashman-Understanding Human Behavior and The Social Environment-Thomson Brooks - Cole (2007)Документ441 страницаCharles Zastrow, Karen K. Kirst-Ashman-Understanding Human Behavior and The Social Environment-Thomson Brooks - Cole (2007)joan82% (17)
- DADTCO Presentation PDFДокумент34 страницыDADTCO Presentation PDFIngeniería Industrias Alimentarias Itsm100% (1)
- Dress Code19sepДокумент36 страницDress Code19sepapi-100323454Оценок пока нет
- Big Brother Naija and Its Impact On Nigeria University Students 2 PDFДокумент30 страницBig Brother Naija and Its Impact On Nigeria University Students 2 PDFIlufoye Tunde100% (1)
- 1.classification of Reciprocating PumpsДокумент8 страниц1.classification of Reciprocating Pumpsgonri lynnОценок пока нет
- Te-Chemical Sem5 CPNM-CBCGS Dec19Документ2 страницыTe-Chemical Sem5 CPNM-CBCGS Dec19Mayank ShelarОценок пока нет
- S3 U4 MiniTestДокумент3 страницыS3 U4 MiniTestĐinh Thị Thu HàОценок пока нет
- (Bruno Bettelheim) Symbolic Wounds Puberty RitesДокумент196 страниц(Bruno Bettelheim) Symbolic Wounds Puberty RitesAmbrose66Оценок пока нет
- Kingroon ConfiguracoesДокумент3 страницыKingroon ConfiguracoesanafrancaОценок пока нет
- (Ebook - Antroposofia - EnG) - Rudolf Steiner - Fundamentals of TheraphyДокумент58 страниц(Ebook - Antroposofia - EnG) - Rudolf Steiner - Fundamentals of Theraphyblueyes247Оценок пока нет
- PV Power To Methane: Draft Assignment 2Документ13 страницPV Power To Methane: Draft Assignment 2Ardiansyah ARОценок пока нет
- Handout Waste Catch BasinДокумент2 страницыHandout Waste Catch BasinJonniel De GuzmanОценок пока нет
- Science9 Q4 Week2Документ16 страницScience9 Q4 Week2Maria Josie Lopez TumlosОценок пока нет
- AIP 2020 FINAL JuneДокумент5 страницAIP 2020 FINAL JuneVINA ARIETAОценок пока нет
- Very Hungry Caterpillar Clip CardsДокумент5 страницVery Hungry Caterpillar Clip CardsARTGRAVETO ARTОценок пока нет
- Ims DB DCДокумент90 страницIms DB DCpvnkraju100% (1)
- 3E Hand Over NotesДокумент3 страницы3E Hand Over NotesAshutosh MaiidОценок пока нет
- Week 3 Alds 2202Документ13 страницWeek 3 Alds 2202lauren michaelsОценок пока нет