Академический Документы
Профессиональный Документы
Культура Документы
bcp0067 0671
Загружено:
biotech_vidhyaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
bcp0067 0671
Загружено:
biotech_vidhyaАвторское право:
Доступные форматы
British Journal of Clinical Pharmacology
DOI:10.1111/j.1365-2125.2009.03424.x
Medication errors: the importance of an accurate drug history
Richard J. FitzGerald
Department of Pharmacology and Therapeutics, University of Liverpool, Liverpool, UK
Correspondence
Dr Richard J. FitzGerald, Department of Pharmacology and Therapeutics, University of Liverpool, Ashton Street, Liverpool, L69 3GE. Tel: 0151 794 5557 Fax: 0151 794 5540 E-mail: richard.tzgerald@liverpool.ac.uk
----------------------------------------------------------------------
Keywords
electronic prescribing, medication errors, medicines reconciliation, prescribing errors
----------------------------------------------------------------------
Accepted
18 March 2009
1. Medication histories are important in preventing prescription errors and consequent risks to patients. Apart from preventing prescription errors, accurate medication histories are also useful in detecting drug-related pathology or changes in clinical signs that may be the result of drug therapy. A good medication history should encompass all currently and recently prescribed drugs, previous adverse drug reactions including hypersensitivity reactions, any over-the counter medications, including herbal or alternative medicines, and adherence to therapy. 2. Medication history errors, such as omitting drugs erroneously, are common and often have the potential to harm the patient. Hypersensitivity reactions are often poorly documented or not explored in detail, which may lead to unnecessary avoidance of a drug. Accurate documentation of concomitant herbal or alternative therapies is rare, despite the importance they may have in causing adverse effects or drug-drug interactions. Polypharmacy, specic drugs, and clinical specialty can affect the risk of medication history errors. 3. There are various strategies to reduce medication history errors. Pharmacists are better at taking an accurate medication history than many physicians or nurses. In the context of acute hospital admissions they reduce error, the risks of adverse drug reactions, and prescription costs. Electronic prescribing may reduce transcription errors, but it can facilitate other errors and still depends on an accurate medication history. 4. Education of prescribers, both in clinical pharmacology and in taking accurate medication histories is vitally important in reducing errors.
Over two and a half million prescriptions are written every day in the UKs National Health Service, and in a UK hospital of average size around 7000 medications will be administered daily [1]. Error is possible in any part of the medication process prescribing, transcription, dispensing, administration, or monitoring but it is in the prescribing phase that errors in the medication history may have their effect.
The medication history
There are several reasons for taking an accurate medication history [2]: A knowledge of the drugs a patient has taken in the past or is currently taking and of the responses to those drugs will help in planning future treatment. Drug effects should always be on the list of differential diagnoses, since drugs can cause illness or disease, either directly or as a result of an interaction. Drugs can mask clinical signs. For example, badrenoceptor antagonists can prevent tachycardia in a patient with haemorrhage, and corticosteroids can prevent abdominal pain and rigidity in a patient with a perforated duodenal ulcer. Drugs can alter the results of investigations. For example, amiodarone alters thyroid function tests. To take the opportunity to educate the patient about their medications. To help avoid preventable errors in prescribing, since an inaccurate history on admission to hospital may lead to
Br J Clin Pharmacol / 67:6 / 671675 / 671
Prescribing faults
Prescribing faults affect up to 11% of prescriptions, with a cost of around 400 million per year (the annual cost of running four district general hospitals) [1]. Around 16% of prescribing faults resulted in harm to patients; for example, between January 2005 and June 2006 there were 38 deaths in the UK that resulted direct from prescribing faults.1 Most of these errors were preventable: for example, drugs administered despite a contraindication, drugs given by an incorrect route, drugs given in an inappropriate dose, or drugs given with inadequate monitoring.
2009 The Author Journal compilation 2009 The British Pharmacological Society
R. J. FitzGerald
unwanted duplication of drugs, drug interactions, discontinuation of long-term medications, and failure to detect drug-related problems [3]. Other aspects of the medical history and examination may also be important in preventing a prescribing fault. For example, a history of chronic renal insufciency will highlight the need for caution when introducing an angiotensin converting enzyme inhibitor. Furthermore, the effects of some drugs can be detected by examination, such as the benecial effect of salbutamol on the peak expiratory ow rate or the adverse effects of phenytoin on the central nervous system (nystagmus and ataxia). Errors are more common on admission to hospital for many reasons: patients often are not able to report their drug history accurately and may not bring either the drugs themselves or even a recent list of medications with them [35]. A drug prescribed in error will often not be checked until a pharmacist reviews the patients prescription, which may not be for up to 72 h after admission. Clearly, therefore, the medication history must be accurate at the time of admission and should be checked at the earliest opportunity during a patients hospital stay. The medication history should not simply be a list of a patients drugs and dosages. Other information, such as adherence to therapy and previous hypersensitivity reactions and adverse effects, should be noted and should be compared with the patients general practitioner (GP) records or previous prescription history in their hospital case notes. Adverse drug reactions are often poorly recorded; of 117 patients, 50 had had a total of 81 previous adverse reactions, but only 75% were recorded on medication charts and 57% and 64% in the medical and nursing notes, respectively [6]. Herbal remedies are infrequently recorded but may be important causes of morbidity. Constable et al. described a 77-year-old woman taking lansoprazole in whom induction of CYP2C19 by St Johns wort (reducing the effect of lansoprazole) plus inhibition of platelet aggregation by ginseng led to upper gastrointestinal haemorrhage [7]. Neither of these herbal medications was listed on the admission drug history, but they were both important in the presentation and had implications for the prevention of further episodes. In an audit conducted by the same authors, only one person out of 24 taking herbal medications had this documented in the case notes. Indeed, all forms of complementary and alternative medicine (CAM) are poorly recorded. In one study, 59 of 101 patients used 129 forms of CAM in the month before admission, but only 36 were documented in the medical records [8]. The details that should be elicited in a good medication history are described below.
672 / 67:6 / Br J Clin Pharmacol
History from the patient
When taking the history from the patient use the words medicines or medications, rather than drugs, which may be mistaken for drugs of abuse or recreational drugs. Elicit the following information: 1 Current prescribed drugs, formulations (e.g. modiedrelease tablets), doses, routes of administration (e.g. oral, transdermal, by inhalation), frequencies, duration of treatment. 2 Other medications (e.g. over-the-counter drugs and herbal or natural remedies, such as vitamins and glucosamine). 3 Drugs that have been taken in the recent past (important for drugs with long half-lives, such as amiodarone). 4 Previous drug hypersensitivity reactions, their nature and time course (e.g. a rash, anaphylaxis). 5 Previous adverse drug reactions, their nature and time course (e.g. nausea with erythromycin, peripheral oedema with amlodipine). 6 Adherence to therapy (e.g. are you taking your medication regularly?), recognizing that the information may be inaccurate.
History from the GP or community pharmacist
1 Up-to-date list of medications. 2 Previous adverse drug reactions. 3 Last order dates for each medication.
History from case notes
1 Previous prescriptions. 2 Previous adverse drug reactions.
Inspection
Drugs and their containers (for example, packs, bottles, vials) should be inspected for name, dosage, and the number of dosage forms taken since dispensed; it is often possible to identify a medicine by inspecting the formulation.
Medication history errors: the scale of the problem, consequences, and prediction
Errors in the medication history can be classied into omission errors (drugs missed from the history), commission errors (drugs added to the history), frequency errors, and dose errors. Lau et al. showed that up to 67% of patients had at least one medication error on admission to hospital general medicine wards [3]. Most were omission errors, but this study did not consider errors in dose or frequency as medication errors and so probably underreported the frequency of errors. In addition, there was no measure of the
Medication errors and drug history
potential severity of the outcome of the error. A more recent systematic review of 22 individual studies showed that 1061% of patients had at least one omission error and 1322% had at least one commission error in their history; 41% of all errors were clinically important and 22% had the potential to cause harm during the patients admission [9]. However, a number of studies included in the review did not consider dose or frequency errors; this may explain the wide range of estimates for medication history errors reported in the systematic review. Furthermore, most studies do not differentiate between what is a deliberate change in medication for therapeutic reasons and what is an unintended medication change, making assessment of error a challenging task. It is also difcult to quantify the effects of medication history errors on patients (i.e.did they cause harm?), because sample sizes are small (often <100 participants) and potential severity is not elucidated. This variability in reporting methods for medication history errors and poor study quality make establishing the extent of the problem difcult, although it is clear that there is potential for signicant harm to patients.This is particularly true when the type of drug most commonly involved in medication history errors is considered: often these are drugs that have the potential for severe adverse effects and may have narrow therapeutic windows (e.g. digoxin). Cardiovascular drugs, sedatives, antibiotics, antithrombotic drugs, and analgesics were the most frequently involved in medication history errors [911], and given the potential for adverse effects from these drugs it is hardly surprising that in one study 59% of medication history errors would have resulted in potential harm if they had been continued beyond hospital discharge [12]. Cornish et al. reported that 39% of recorded errors had the potential to cause moderate or severe harm to patients in their study of 151 patients [13]. Examples included continued use of diclofenac in patients with upper gastrointestinal bleeding and the omission of a regular corticosteroid (prednisolone 7.5 mg day-1) in a patient with acute confusion. There were no signicant correlations between the time of admission (night-time, weekend) or polypharmacy and the mean error rate per patient. Previous hypersensitivity reactions may be documented without being explored in detail [14]. For example, a history of allergy to penicillin may not represent true hypersensitivity and may lead to unnecessary avoidance of a penicillin both currently and in the future. In one case, a patient thought that he was allergic to penicillin because he had developed facial folliculitis 1 month after a course of ampicillin; he was given ucloxacillin for cellulitis without mishap. Some adverse effects (e.g. peripheral oedema with amlodipine or a transient rise in liver function tests after starting rifampicin) need not preclude use of the drug in the future. This is especially important in chronic conditions such as hypertension, in which multiple adverse effects are more common [15].
Risk factors for errors in the medication history
Polypharmacy is a logical candidate as a risk factor for errors in transcribing drugs, but the evidence is contradictory [13, 16, 17]. Specic drugs, such as anticoagulants, cardiovascular drugs, nonsteroidal anti-inammatory drugs, opioids and corticosteroids, and modied-release formulations, are more likely to be subject to errors, although this may simply represent their widespread use and multiple formulations. Cornish et al. found no correlation between the time of admission and the rate of errors, but Picone et al. found that stafng changeover times were associated with a higher incidence of errors [16]. Finally, the clinical specialty alters the recording of a medication history: cardiologists and respiratory physicians reportedly take the most detailed histories [18].
Preventing medication errors from inadequate medication histories
There are various strategies for reducing the impact of errors in the medication history (such as a more involved role for pharmacists) and for preventing errors in the subsequent transcription of the medication history (better education for prescribers). Pharmacists have been involved with medication reconciliation for several years. In the context of acute general (internal) medicine admissions, pharmacists obtain better medication histories than many physicians and also identify more medication doses and frequencies [19]. These ndings are similar to those of Carter et al., who showed similar improvements in medication histories and documentation of allergies by pharmacists in Emergency Departments compared with physicians and nurses [20]. There are also reductions in medication errors when pharmacists are involved in pre-admission clinics for elective surgery: in a recent study, of the histories taken by pharmacists 13% contained a medication error with the potential to cause harm, compared with 30% in the standard care group (histories taken by physicians and nurses) [21]. Clearly, there is benet from using pharmacists in acute or elective admission processes, but doing so is expensive and time-consuming and may not be cost-effective. An alternative, particularly in UK hospitals, would be to have a pharmacist attend the post-take ward round. Fertleman et al. found that pharmacists identied and resolved more medication history errors and that mean increases in the costs of medications between admission and discharge were reduced (181 before intervention vs. 122 after, a 33% reduction) [22]; they proposed that having a pharmacist present when prescribing decisions were made would have a signicant impact on medication safety and costs in UK district general hospitals. Electronic prescribing may also have a role in preventing medication history errors. Electronic prescribing still depends on an accurate and complete medication history,
Br J Clin Pharmacol / 67:6 / 673
R. J. FitzGerald
but it will prevent some serious transcription errors (for example, prescribing methotrexate once a day rather than once a week). Electronic prescribing may alter prescribing behaviour; in one study there was a marked improvement in prescribing behaviour by junior doctors over a 3-week period, as measured by the number of warning messages generated by the electronic prescribing system [23]. As a whole, medication errors are reduced by electronic prescribing [24, 25], but they can also facilitate errors [26]. Drop-down boxes in response to predictive text are a common feature of electronic prescribing systems and can lead to the selection of an unintended drug (e.g. amiodarone instead of amoxicillin). Similar drug names and differing proprietary names of long-acting formulations are as much a problem with electronic prescribing as with paper prescribing [27]. Electronic prescribing reduces error, but does not remove the necessity of a through medication history. Education of prescribers is currently under review in the UK, and the draft version of the forthcoming edition of Tomorrows Doctors, the document in which the General Medical Council details the abilities that are expected of newly qualied doctors, now for the rst time contains details about prescribing [28]. However, there is a lack of clinical pharmacologists for teaching undergraduates [29] and while this is so, formal teaching of therapeutics, which is currently patchy, is unlikely to improve. Furthermore, there is currently no standardized assessment of prescribing competence, for either undergraduates or postgraduates [30]. Education of prescribers in basic and clinical pharmacology is key in preventing errors in the medication history and other medication errors. For example, when doctors were educated about the need to take a history of the use of complementary and alternative medicines and of previous adverse drug reactions, there were signicant improvements in the recording of these details [6, 8]. In addition, the concept of harm from unintended medication errors needs to be emphasized to all prescribers. Without this, errors will continue to occur and patients will suffer harm.
errors associated with transcription of medications. Finally, education of prescribers is vital to emphasize the importance of accurate medication histories and the clear potential for harm from unintended discrepancies.
Competing interests
None to declare.
REFERENCES
1 National Patient Safety Agency. Safety in Doses: Medication Safety Incidents in the NHS. London: The Stationery Ofce, 2007. 2 Grahame-Smith DG, Aronson JK. The drug history and the clinical examination and investigation of drug effects. In: The Oxford Textbook of Clinical Pharmacology and Drug Therapy, 3rd edn, ed. GrahemeSmith DG, Aronson JK. Oxford: Oxford University Press, 2002; 16770. 3 Lau HS, Florax C, Porsius AJ, de Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol 2000; 49: 597603. 4 Schwarz A, Faber U, Borner K, Keller F, Offermann G, Molzahn M. Reliability of drug history in analgesic users. Lancet 1984; 2: 116314. 5 Glintborg B, Hillestrom PR, Olsen LH, Dalhoff KP, Poulsen HE. Are patients reliable when self-reporting medication use? Validation of structured drug interviews and home visits by drug analysis and prescription data in acutely hospitalised patients. J Clin Pharmacol 2007; 47: 14409. 6 Sheneld GM, Robb T, Duguid M. Recording previous adverse drug reactions a gap in the system. Br J Clin Pharmacol 2001; 51: 6236. 7 Constable S, Ham A, Pirmohamed M. Herbal medicines and acute medical emergency admissions to hospital. Br J Clin Pharmacol 2006; 63: 2478. 8 Cockayne NL, Duguid M, Sheneld GM. Health professionals rarely record history of complementary and alternative medicines. Br J Clin Pharmacol 2005; 59: 2548. 9 Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005; 173: 5105. 10 Hardmeier B, Braunschweig S, Cavallaro M, Roos M, Pauli-Magnus C, Giger M, Meier PJ, Fattinger K. Adverse drug events caused by medication errors in medical inpatients. Swiss Med Wkly 2004; 134: 66470. 11 Kanjanarat P, Winterstein AG, Johns TE, Hatton RC, Gonzalez-Rothi R, Segal R. Nature of preventable adverse drug events in hospitals: a literature review. Am J Health Syst Pharm 2003; 60: 17509.
Conclusion
Medication errors are common and can signicantly harm patients. An important component is the medication history, which is often incomplete and inaccurate. Current studies suggest that this is a common and worldwide problem, but the results are limited by small numbers, differing measures, and poor assessment of consequences. Pharmacists can play an important role in preventing unintended errors, by being involved in obtaining medication histories during acute admissions or on post-take ward rounds. Electronic prescribing is not a substitute for an accurate medication history, although it may prevent some
674 / 67:6 / Br J Clin Pharmacol
Medication errors and drug history
12 Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalised patients. Am J Health Syst Pharm 2004; 61: 168995. 13 Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, Etchells EE. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005; 165: 4249. 14 Chamisa I, Zulu BM. Setting the records straight a prospective audit of the quality of case notes in a surgical department. S Afr J Surg 2007; 45: 925. 15 Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336: 11147. 16 Picone DM, Titler MG, Dochterman J, Shever L, Kim T, Abramowitz P, Kanak M, Qin R. Predictors of medication errors among elderly hospitalized patients. Am J Med Qual 2008; 23: 11527. 17 Aronson JK. In defence of polypharmacy. Br J Clin Pharmacol 2004; 57: 11920. 18 Yusuff KB, Tayo F. Does a physicians speciality inuence the recording of medication history in patients case notes? Br J Clin Pharmacol 2008; 66: 30812. 19 Reeder TA, Mutnick A. Pharmacist-versus physician-obtained medication histories. Am J Health Syst Pharm 2008; 65: 85760. 20 Carter MK, Allin DM, Scott LA, Grauer D. Pharmacist-acquired medication histories in a university hospital emergency department. Am J Health Syst Pharm 2006; 63: 25003.
21 Kwan Y, Fernandes OA, Nagge JJ, Wong GG, Huh JH, Hurn DA, Pond GR, Bajcar JM. Pharmacist medication assessments in a surgical preadmission clinic. Arch Intern Med 2007; 167: 103440. 22 Fertleman M, Barnett N, Patel T. Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Qual Saf Health Care 2005; 14: 20711. 23 Anton C, Nightingale PG, Adu D, Lipkin G, Ferner RE. Improving prescribing using a rule based prescribing system. Qual Saf Health Care 2004; 13: 18690. 24 Voeffray M, Pannatier A, Stupp R, Fucina N, Leyvraz S, Wasserfallen JB. Effect of computerisation on the quality and safety of chemotherapy prescription. Qual Saf Health Care 2006; 15: 41821. 25 Donyai P, OGrady K, Jacklin A, Barber N, Franklin BD. The effects of electronic prescribing on the quality of prescribing. Br J Clin Pharmacol 2007; 65: 2307. 26 Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerised physician order entry systems in facilitating medication errors. JAMA 2005; 293: 1197203. 27 Aronson JK. Medication errors resulting from the confusion of drug names. Expert Opin Drug Saf 2004; 3: 16772. 28 General Medical Council. Tomorrows Doctors 2009: a draft for consultation. Available at https://gmc.e-consultation.net/ econsult/uploads/TD%20Final.pdf (last accessed 3 February 2009). 29 Aronson JK, Henderson G, Webb DJ, Rawlins MD. A prescription for better prescribing. BMJ 2006; 333: 45960. 30 Aronson JK. A prescription for better prescribing. Br J Clin Pharmacol 2006; 61: 48791.
Br J Clin Pharmacol
67:6 /
675
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Facs ProtocolДокумент7 страницFacs ProtocolmisterxОценок пока нет
- BT 2019Документ13 страницBT 2019biotech_vidhyaОценок пока нет
- Stripping For ReprobingДокумент2 страницыStripping For ReprobingStella SalvatoreОценок пока нет
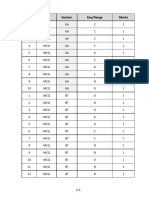
- Q.No. Type Section Key/Range MarksДокумент3 страницыQ.No. Type Section Key/Range Marksbiotech_vidhyaОценок пока нет
- Stripping For ReprobingДокумент2 страницыStripping For ReprobingStella SalvatoreОценок пока нет
- Polymerase Chain Reaction (PCR)Документ3 страницыPolymerase Chain Reaction (PCR)biotech_vidhyaОценок пока нет
- Brad FordДокумент12 страницBrad FordQi ChaoОценок пока нет
- SDS PageДокумент2 страницыSDS Pagebiotech_vidhyaОценок пока нет
- Buffer Preparation Guide for DNA/Protein Work (Shi LabДокумент6 страницBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaОценок пока нет
- Troubleshooting SDS-PAGE 1Документ3 страницыTroubleshooting SDS-PAGE 1biotech_vidhyaОценок пока нет
- Polymerasen GuideДокумент16 страницPolymerasen Guidebiotech_vidhyaОценок пока нет
- Components Reaction MixtureДокумент3 страницыComponents Reaction Mixturebiotech_vidhyaОценок пока нет
- Buffer Preparation Guide for DNA/Protein Work (Shi LabДокумент6 страницBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaОценок пока нет
- TNPSC Group 1 Prelim Book List PDFДокумент2 страницыTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaОценок пока нет
- Whole Cell ExtractДокумент1 страницаWhole Cell Extractbiotech_vidhyaОценок пока нет
- TNPSC Group 1 Prelim Book List PDFДокумент2 страницыTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaОценок пока нет
- Befcv List PDFДокумент22 страницыBefcv List PDFbiotech_vidhyaОценок пока нет
- Nuclear ExtractsДокумент2 страницыNuclear Extractsbiotech_vidhyaОценок пока нет
- Qpaper PondyДокумент21 страницаQpaper Pondybiotech_vidhyaОценок пока нет
- Ies 17 Set A Me Q AДокумент67 страницIes 17 Set A Me Q Abiotech_vidhyaОценок пока нет
- TNPSC Group 1 Prelim Book List PDFДокумент2 страницыTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaОценок пока нет
- A.E. (Mechanical Engineering I) 2007Документ24 страницыA.E. (Mechanical Engineering I) 2007Mukesh KumarОценок пока нет
- Qpaper PondyДокумент21 страницаQpaper Pondybiotech_vidhyaОценок пока нет
- ESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionДокумент52 страницыESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionpataОценок пока нет
- Img Word-To PDFДокумент3 страницыImg Word-To PDFbiotech_vidhyaОценок пока нет
- Mechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010Документ20 страницMechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010biotech_vidhyaОценок пока нет
- TDC 41597 A (Mechanical Engg.) - 2012Документ20 страницTDC 41597 A (Mechanical Engg.) - 2012biotech_vidhyaОценок пока нет
- Recruitment RulesДокумент5 страницRecruitment Rulesbiotech_vidhyaОценок пока нет
- Part and Mold Design GuideДокумент170 страницPart and Mold Design GuideminhtintinОценок пока нет
- 1 TolerancesДокумент1 страница1 Tolerancesbiotech_vidhyaОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Geriatrics: Roger E. ThomasДокумент44 страницыGeriatrics: Roger E. ThomasSubhash SharmaОценок пока нет
- Malaysia PRP Private Hospital LogbookДокумент229 страницMalaysia PRP Private Hospital LogbookAiWeiОценок пока нет
- Personal Details and Training Log for Provisionally Registered PharmacistsДокумент48 страницPersonal Details and Training Log for Provisionally Registered PharmacistsB024-MASWANIE SOFEAОценок пока нет
- Geriatric Giants - DR SeymourДокумент108 страницGeriatric Giants - DR SeymourSharon Mallia100% (1)
- Health LiteracyДокумент5 страницHealth LiteracyHillary JamesОценок пока нет
- Dr. Dewi-Geriatric PharmacologyДокумент41 страницаDr. Dewi-Geriatric PharmacologyAnne Gustriwati0% (1)
- Best Practice Skin TearsДокумент25 страницBest Practice Skin TearsJacinta MontesОценок пока нет
- Too Many Pills - How Too Much Me - James Le FanuДокумент274 страницыToo Many Pills - How Too Much Me - James Le Fanumohamed gaberОценок пока нет
- Assessment of Rational Drug Use at Nagelle Arsi Veterinary Clinic West Arsi, Oromia, EthiopiaДокумент51 страницаAssessment of Rational Drug Use at Nagelle Arsi Veterinary Clinic West Arsi, Oromia, EthiopiaTamirat WakoОценок пока нет
- Ranitidine + OndansetronДокумент7 страницRanitidine + OndansetronAllicia PutriОценок пока нет
- Geri Assess Tools ArticleДокумент9 страницGeri Assess Tools ArticleThesmith FamОценок пока нет
- The Origin and Nature of Sorcery-Pharmakeia-Pharmaceutical ExplainedДокумент40 страницThe Origin and Nature of Sorcery-Pharmakeia-Pharmaceutical ExplainedArnulfo Yu LanibaОценок пока нет
- Test Bank For Ebersole and Hess Toward Healthy Aging 8th Edition Theris A TouhyДокумент8 страницTest Bank For Ebersole and Hess Toward Healthy Aging 8th Edition Theris A TouhyGraceLopezyfmox100% (31)
- Rapid Geriatric Assessment of Hip FractureДокумент14 страницRapid Geriatric Assessment of Hip FractureJuliana Moreno LadinoОценок пока нет
- Ageing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesДокумент24 страницыAgeing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesepraetorianОценок пока нет
- 2014 Geriatric Emergency Department GuidelinesДокумент19 страниц2014 Geriatric Emergency Department GuidelinesjujucastellОценок пока нет
- Fall Prevention: How Can Older Adults Prevent Falls?Документ4 страницыFall Prevention: How Can Older Adults Prevent Falls?Amalina ZahariОценок пока нет
- Pharmaceutical Care PDFДокумент18 страницPharmaceutical Care PDFAhmed IsseОценок пока нет
- NCM 113 EVIDENCE-BASED GERONTOLOGICAL NURSINGДокумент11 страницNCM 113 EVIDENCE-BASED GERONTOLOGICAL NURSINGAisha CorobongОценок пока нет
- GERIA Unit 4 LearnersДокумент34 страницыGERIA Unit 4 Learners3D - AURELIO, Lyca Mae M.Оценок пока нет
- New Approach For CV Risk Management (Prof. DR - Dr. Djanggan Sargowo, SPPD, SPJP (K) )Документ56 страницNew Approach For CV Risk Management (Prof. DR - Dr. Djanggan Sargowo, SPPD, SPJP (K) )Yulia SumarnaОценок пока нет
- Effect of Pharmacy Intervention To Patient With Polypharmacy - JournalДокумент7 страницEffect of Pharmacy Intervention To Patient With Polypharmacy - Journalanon_529380518Оценок пока нет
- StoppFrail PaperДокумент8 страницStoppFrail PaperEric LiangОценок пока нет
- Chapter 003 Geriatric Pharmacology: Multiple Choice QuestionsДокумент15 страницChapter 003 Geriatric Pharmacology: Multiple Choice QuestionsgoldfishxОценок пока нет
- Pharmacology and The Nursing Process 7th Edition Lilley Test BankДокумент25 страницPharmacology and The Nursing Process 7th Edition Lilley Test BankStevenCookexjrp100% (40)
- Polypharmacy in the elderlyДокумент3 страницыPolypharmacy in the elderlyjosephОценок пока нет
- Common Drug Side Effects - Drug Interactions - Elderly - Primary Care - 2017Документ8 страницCommon Drug Side Effects - Drug Interactions - Elderly - Primary Care - 2017opulgarОценок пока нет
- Exploring The Pharmaco-Clinical View On Bhanga (Cannabis Sativa Linn.) : A Classical Unfamiliar PortrayalДокумент20 страницExploring The Pharmaco-Clinical View On Bhanga (Cannabis Sativa Linn.) : A Classical Unfamiliar PortrayalVikram DravidОценок пока нет
- Adr Management and MonitoringДокумент5 страницAdr Management and MonitoringRaju NiraulaОценок пока нет
- Top-Rate Geriatric Care at Grace Nursing HomeДокумент11 страницTop-Rate Geriatric Care at Grace Nursing HomeRolli SptОценок пока нет