Академический Документы
Профессиональный Документы
Культура Документы
ERPM Revision
Загружено:
Nalin AbeysingheАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
ERPM Revision
Загружено:
Nalin AbeysingheАвторское право:
Доступные форматы
ERPM Revision 03
1. With regard to the obstetric history: a. Pregnancy is dated from conception b. Parity is the total number of pregnancies regardless of how they ended c. It is recommended that women should be seen on their own at least once d. A family history of pre-eclampsia should trigger increased antenatal surveillance e. The last menstrual period is reliable if the cycles are irregular FFTTF 2. The following terms are appropriate: a. Lie: cephalic b. Position: flexed c. Station: at the level of the spines d. Engagement: two-fifths e. Presenting part: shoulder FFTTT 3. With regard to routine antenatal care: a. There is no evidence in low-risk pregnancies that reduction in antenatal visits increase maternal or fetal mortality b. The Naegele rule states that the expected date of delivery (EDD) is calculated by adding 7 days to the last menstrual period (LMP) and then taking away 4 months c. Syphilis testing forms part of the routine booking visit d. Routine urine testing reduces preterm labour e. Every patient should have a named consultant TFTFF 4. The routine dating scan: a. Allows accurate dating of the pregnancy and a reduction in induction of labour for prolonged pregnancy b. Allows the detection of placenta praevia c. Allows early detection of twin pregnancies d. Allows detection of a failed pregnancy e. Allows detection of uterine abnormalities TFTTT 5. In relation to normal cardiotocograms at term: a. The baseline at term is usually 120160 beats per minute. b. The baseline variability is considered abnormal when it is <10 beats per minute. c. Acceleration is a baseline increase of 15 beats per minute for 15 seconds. d. A reactive trace would have one acceleration in 20 minutes. e. The tocograph trace indicates the strength of the contractions. FTTFF 6. Second trimester miscarriage: a. Is typically painless. b. Occurs between 12 and 24 weeks gestation. c. Can be associated with rupture of the fetal membranes. d. Is diagnosed after exclusion of infection, haemorrhage and multiple pregnancy e. Antibiotic prophylaxis is usually given FTTFF
7. Oligohydramnios is associated with the following fetal conditions: a. Tracheo-oesophageal fistula b. Talipes c. Intrauterine growth restriction d. Anecephaly e. Premature rupture of the fetal membranes FTTFT 8. Polyhydramnios is associated with the following: a. Maternal diabetes b. Neuromuscular fetal conditions c. Maternal non-steroidal anti-inflammatory drugs d. Postmaturity e. Chorioangioma of the placenta TFTFT 9. In twin delivery: a. The first twin is at greater risk then the second b. Cephaliccephalic presentation is the most common c. Labour usually occurs prior to term d. Labour is extended e. There is a risk of postpartum haemorrhage FTTFT 10. Pre-eclampsia is more common in: a. Multigravid women b. Women with congenital cardiac disease c. Multiple pregnancy d. Women with diabetes insipidus e. Women with pre-existing renal disease FFTFT 11. Women with congenital heart disease: a. Should have a detailed fetal cardiology scan. b. Should avoid becoming anaemic. c. Should have prophylactic antibiotics for operative deliveries. d. Commonly develop dysrhythmias. e. Should have a shortened second stage of labour. TTTFT 12. Hyperthyroidism in pregnancy: a. Should be treated surgically rather than with carbimazole. b. Can be diagnosed by total T4 measurements. c. 50 per cent are secondary to Graves disease. d. The main complications for the fetus include growth restriction and fetal bradycardia. e. Therapy should maintain free T4 and T3 levels in the low normal range. FFFFF 13. The infant of a diabetic mother is at increased risk of: a. Polycythemia. b. Hypermagnesaemia. c. Traumatic delivery. d. Neonatal jaundice. e. Hypoglycaemia. TFTTT
14. Congenital malformation can be attributed to maternal infection with: a. Poliomyelitis. b. Toxoplasmosis. c. Measles. d. Parvovirus. e. Syphilis. FTFFT 15. Progress in labour is measured by: a. The frequency of uterine contractions. b. The force of uterine contractions. c. Descent of the presenting part. d. Dilation of the cervix. e. The length of time since rupture of the membranes. FFTTF 16. In relation to the mechanism of labour: a. Engagement is said to have occurred when the widest part of the presenting part has passed through the false pelvis. b. Restitution occurs after external rotation. c. Extension occurs after internal rotation. d. Extension occurs at crowning. e. Descent of the fetal head is needed before flexion, internal rotation and extension can occur. FFTTT 17. Regarding face presentation: a. This occurs in 1:250 labours. b. The presenting diameter is the submento-bregmatic, which is 9.5 cm. c. It is commonly due to fetal thyroid tumours. d. The face can deliver vaginally with the chin meno-anterior. e. Oxytocin should be used to augment slow progress. FTFTF 18. Considering the Bishops score: a. It includes station of the presenting part. b. It includes the length of the cervical canal. c. It includes the gestation of the fetus. d. It includes parity of the mother. e. A score of 4 indicates the cervix is unfavourable. TTFFT 19. Concerning brow presentation: a. This may be treated in labour by craniotomy. b. It is the least common malposition. c. The presenting diameter is mento-vertical. d. It may be treated in labour by Caesarean section. e. This is incompatible with vaginal delivery FFTTF 20. The following complications are more likely after Caesarean section than after vaginal delivery: a. Pulmonary embolism. b. Secondary postpartum haemorrhage. c. Postnatal depression. d. Amniotic fluid embolism. e. Infection. TFTFT 3
21. With regard to clinical examination of the gynaecological patient: a. Abdominal examination is mandatory as part of the gynaecological examination. b. A chaperone is always needed for intimate examinations. c. Palpation below a pelvic mass is possible. d. Shifting dullness and fluid thrill can be seen due to urinary retention. e. Bidigital examination can determine whether a pelvic mass is ovarian or uterine in origin. TTFFT 22. In the XY genotype: a. Androgen insensitivity results in an XY genotype and female phenotype but with normal testes b. In 5-alpha-reductase deficiency, virilization of the cloaca fails to occur owing to the failure of the conversion of testosterone to 17-hydroxyprogesterone c. In androgen insensitivity,Mullerian ducts regress owing to the production of Mullerian inhibitory factor d. In androgen insensitivity, the Wolffian ducts regress owing to the absence of an androgen receptor e. In 5-alpha-reductase deficiency, the Mullerian ducts fail to regress owing to the lack of Mullerian inhibitory factor TFTTF 23. Within the follicular phase of the menstrual cycle: a. The follicular phase is always 14 days long to allow development of the follicle. b. Follicle-stimulating hormone (FSH) stimulates the granulosa cells to produce oestrogen. c. Each cycle usually involves the development, growth and ovulation of a single follicle. d. Follicles over 20 mm need to be drained with ultrasound guidance. e. Oestrogen and inhibin have a positive feedback on the pituitary to release FSH and luteinizing hormone (LH). FTTFF 24. In relation to ovulation: a. LH induces theca cells to produce oestrogen. b. FSH induces a rise in LH receptors c. Ovulation occurs 14 hours after the LH surge. d. The release of an oocyte from the follicle requires a sperm to lyse the follicle membrane and results in ovulation. e. Ovulation can be confirmed by measurement of LH on day 14. FTFFF 25. Within the luteal phase of the menstrual cycle: a. The predominant hormone in the luteal phase is progesterone. b. The granulosa cells of the corpus luteum have a rich vascular supply and have a yellow pigment owing to accumulation of cholesterol. c. The luteal phase varies in duration depending on the time taken to degenerate a corpus luteum. d. The corpus luteum continues to degenerate in early pregnancy. e. Low levels of oestrogen and progesterone are the best indicators of the perimenopause TTFFF 26. Definitions: a. Polymenorrhoea is defined as prolonged increased menstrual flow. b. Oligomenorrhoea is defined as menses occurring at a < 21-day interval. c. Hypermenorrhoea is defined as excessive regular menstrual loss. d. Amenorrhoea is defined as absence of menstruation for more than 12 months. e. Menorrhagia is defined as menses at intervals of > 35 days. FFTFF
27. Regarding the investigation of menorrhagia: a. A full blood count is mandatory. b. Thyroid function tests are mandatory. c. A hysteroscopy and endometrial biopsy should be performed in women over the age of 25. d. A pelvic ultrasound scan is only indicated if one is suspicious of a pelvic mass or fibroids. e. A hormone profile including mid-luteal progesterone is essential to differentiate between ovulatory and non-ovulatory dysfunctional bleeding TFF(T)F 28. Considering the depot injection and hormonal implants: a. There are two types of depot injection. One contains medroxyprogesterone acetate 150 and lasts for 12 weeks, the other contains norethisterone 200 mg and lasts for 8 weeks. b. The depot is licensed for 2 years only, otherwise there is an increased risk of reduced bone density and osteoporosis. c. The depot can cause amenorrhoea but irregular bleeding is also a significant side effect d. The Implanon implant involves five rods to be inserted in the upper arm and lasts for 5 years e. With the Implanon implant, the return to ovulation after the implant is removed usually takes up to 1 year. TTTFF 29. Concerning the intrauterine contraceptive device (IUCD): a. Modern IUCDs can last for 510 years. b. The levonorgestrel intrauterine system (Mirena) is licensed for 8 years. c. Heavy bleeding can be a common side effect with the Mirena. d. The risk of pelvic inflammatory disease is increased with IUCD use. e. There is an increased risk of ectopic with IUCD use. TFFFT 30. The combined oral contraceptive pill (COCP): a. Inhibits ovulation. b. Improves cycle control. c. Has a 3-hour window. d. Is relatively contraindicated in patients with acute/severe liver disease. e. Has a risk of venous thromboembolism (VTE) of 15 per 100 000 in third-generation preparations. TTFFF 31. With regard to the investigation of the infertile couple: a. A full hormone profile, tubal patency testing and semen analysis should be completed on all couples attending a referral for primary infertility. b. A mid-luteal progesterone > 25 nmol/L confirms ovulation. c. A semen analysis should be performed prior to laparoscopy and dye to test for tubal patency. d. Hysterosalpingogram, and laparoscopy and dye insufflation will gain similar information and either can be used to assess tubal patency in all patients. e. A single semen analysis with a volume of 1 mL, a concentration of 10 million/mL and 30 per cent reduced motility confirms oligospermia, and serum testosterone, gonadotrophins and prolactin analysis should be performed FFTFF 32. With regard to miscarriage: a. Total loss of conception after fertilization is around 5070 per cent. b. The total rate of clinical miscarriage is around one-quarter to one-third of all pregnancies. c. Miscarriage is much greater before 6 weeks than after 9 weeks. d. The rate of miscarriage is the same in women over 40 years of age compared with women under 40. e. The most common cause of spontaneous miscarriage is infection. TTTFT
33. In relation to molar pregnancy: a. The uterus often appears larger on palpation than one would expect for gestation. b. Hyperemesis is often seen in patients with molar pregnancies. c. Ultrasound is not useful in the diagnosis of molar pregnancy and the diagnosis is usually made on histology. d. Complete hydatidiform molar pregnancies have a diploid chromosomal constitution owing to duplication of paternal chromosomes and no maternal complement. e. Partial molar pregnancies are usually diploid with duplication of the maternal set of chromosomes. TTFTF 34. Considering ectopic pregnancy: a. The rate of ectopic pregnancy is 0.5 per cent of all pregnancies. b. Ectopic pregnancy is associated with Group B streptococcus infection. c. Laparoscopic salpingectomy is the treatment of choice if the other tube is normal. d. The rate of persistent trophoblast is increased if the patient has a laparoscopic salpingotomy rather than salpingectomy. e. Methotrexate is contraindicated if the mass is > 1 cm in diameter on ultrasound. FFTTF 35. The following are risk factors for the development of endometrial cancer: a. Obesity. b. Diabetes. c. Multiparity. d. Early menopause. e. Unopposed oestrogen therapy. TTFFT 36. Considering treatments for cervical cancer: a. Preclinical invasive disease that is a depth of 6 mm and a width of 7 mm can be treated by large loop excision of the transformation zone alone. b. The risk of nodal involvement is 5 per cent if the depth of preclinical invasion is > 3mm. c. A Wertheims hysterectomy involves removal of the uterus, cervix, paracervical tissue, lymph node sampling and the upper two-thirds of the vagina. d. At Wertheims hysterectomy, the ovaries can be conserved. e. One main complication of Wertheims hysterectomy is poor bladder emptying owing to division of the S2, 3, 4 nerve roots of the pudendal nerve. FTFTF 37. The following are risk factors for ovarian cancer: a. Early menarche. b. Early menopause. c. Combined oral contraceptive pill usage. d. Infertility. e. Implanon implants. TFFTF 38. Regarding the pathophysiology of pelvic organ prolapse: a. Pelvic organ prolapse is commoner in nulliparous women than in multiparous women. b. Pelvic organ prolapse is never seen in nulliparous women. c. Prolapse is commoner after the menopause partly due to oestrogen deficiency. d. Epidural in labour is a risk factor for the subsequent development of prolapse. e. Forceps delivery is a risk factor for the development of prolapse. FFTFT
39. Within the human ovary: a. The follicles are centrally placed in the medulla. b. The cortex and medulla contain stroma of endodermal origin. c. The stromal cells of the cortex and medulla produce predominantly androgens. d. There is a decline in the number of primordial follicles from around 7 million at 6 months gestation to 1.5 million at birth. e. Around 400 000 follicles that are present at puberty will progress to ovulation. FFTTF 40. Considering the pathophysiology of the menopause: a. Oestrogen is produced in the granulosa cells of the developing follicle. b. Oestrogen is produced from the precursors of androstenedione and testosterone by the enzyme 17hydroxylase. c. Theca cells are stimulated by FSH and granulosa cells are stimulated by LH. d. The first change in the endocrine system associated with the menopause is a fall in the hormone inhibin produced by the ovary. e. Levels of FSH start to fall as a secondary effect in the menopause and thus prevent stimulation of the ovaries to produce oestrogen. TFFTF
Dr Nalin Abeysinghe Senior House Officer in Obstetrics and Gynaecology
Вам также может понравиться
- Problem-based Approach to Gastroenterology and HepatologyОт EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisОценок пока нет
- Latest Gynecology Multiple Choice Questions and Answers For PDFДокумент10 страницLatest Gynecology Multiple Choice Questions and Answers For PDFMohamed Al-zichrawy100% (1)
- ERPM Viva Long Cases III v2.0Документ17 страницERPM Viva Long Cases III v2.0Bhagya Pramodh AriyarathnaОценок пока нет
- Erpm InfoДокумент16 страницErpm InfoPamudri Basnayake100% (1)
- Internal Medicine Question Papers For MBBS Final Year StudentsДокумент27 страницInternal Medicine Question Papers For MBBS Final Year Studentsprinceej100% (2)
- Erpm Viva Long Cases V v2.0Документ12 страницErpm Viva Long Cases V v2.0Bhagya Pramodh AriyarathnaОценок пока нет
- MCQ Recall Paper - October 2001Документ33 страницыMCQ Recall Paper - October 2001dr_gentel19Оценок пока нет
- DNB Gen Surgery Old Question Papers 1Документ28 страницDNB Gen Surgery Old Question Papers 1sidorai100% (1)
- 4 5820951304909882278 PDFДокумент386 страниц4 5820951304909882278 PDFMohamed HamoodОценок пока нет
- Obstetrics GynecologyДокумент10 страницObstetrics GynecologyDiane UyОценок пока нет
- Review QuizДокумент107 страницReview QuizAhmad JalladОценок пока нет
- Aiims PG 2005 (Based On Memory)Документ197 страницAiims PG 2005 (Based On Memory)Aadityarajsinh GohilОценок пока нет
- Mcqs BridginДокумент19 страницMcqs Bridginzoha555Оценок пока нет
- Mcqmeq Osce SurgeryДокумент71 страницаMcqmeq Osce SurgeryAshbirZammeriОценок пока нет
- MCQ Anaethesia Posting Group 4 2014Документ4 страницыMCQ Anaethesia Posting Group 4 2014Law YouОценок пока нет
- Medcosmos Surgery: Spleen MCQДокумент19 страницMedcosmos Surgery: Spleen MCQSajag GuptaОценок пока нет
- Krok 2 2011 + AnswersДокумент69 страницKrok 2 2011 + AnswersKrish RoopunОценок пока нет
- MCQ Year 3,26th July (Omega 7)Документ28 страницMCQ Year 3,26th July (Omega 7)Ammal Dzulfiqar Ismail100% (1)
- Gastroenterology Best RДокумент23 страницыGastroenterology Best RfrabziОценок пока нет
- MCQ Exam 2018 - 2Документ42 страницыMCQ Exam 2018 - 2aditya rajputОценок пока нет
- Bailey & Love MCQs-EMQs in Surgery-Part - 2Документ6 страницBailey & Love MCQs-EMQs in Surgery-Part - 2JockerОценок пока нет
- Passing Erpm Myths, Facts & ControversiesДокумент28 страницPassing Erpm Myths, Facts & ControversiesMathurange KrishnapillaiОценок пока нет
- End of 4 Year OSCE - SurgeryДокумент53 страницыEnd of 4 Year OSCE - SurgerySyed Irfan ArifОценок пока нет
- Final Surgery RevisionДокумент195 страницFinal Surgery RevisionAbdulziz Al-jedaieОценок пока нет
- Obstetric Highlights Elmar P. Sakala PDFДокумент47 страницObstetric Highlights Elmar P. Sakala PDFwalt65Оценок пока нет
- Pediatrics AnswersДокумент28 страницPediatrics Answersjaini_patel23Оценок пока нет
- Mini Osce 1 PDFДокумент138 страницMini Osce 1 PDFabdelaheem arabiatОценок пока нет
- Paediatrics and Child Health Practice Exam Questions and AnsweДокумент16 страницPaediatrics and Child Health Practice Exam Questions and AnsweGirmaОценок пока нет
- SurgeryДокумент14 страницSurgeryVinit ChoudharyОценок пока нет
- Breaking Bad News 1 PDFДокумент5 страницBreaking Bad News 1 PDFSaeed HasanОценок пока нет
- DAMS CBT 15 Oct 2017 1Документ121 страницаDAMS CBT 15 Oct 2017 1ReekBhattacharya100% (1)
- HHHHДокумент36 страницHHHHdger11Оценок пока нет
- 2 5429452623423996951 PDFДокумент70 страниц2 5429452623423996951 PDFNikhilBhatt100% (1)
- Osce PG 1Документ18 страницOsce PG 1Mobin Ur Rehman Khan100% (1)
- FMGE July 2023 PrepLadder 1Документ558 страницFMGE July 2023 PrepLadder 1Sahil AhlawatОценок пока нет
- Erpm 1Документ33 страницыErpm 1Nivethitha NarayanasamyОценок пока нет
- Pro 1213 MCQ 2Документ15 страницPro 1213 MCQ 2Jabraan JamilОценок пока нет
- Surgery Pretest SummaryДокумент9 страницSurgery Pretest SummaryPrince DuОценок пока нет
- Gynae 64Документ14 страницGynae 64Jha K SujitОценок пока нет
- Hematology SBAДокумент17 страницHematology SBAJared Khoo Er Hau100% (1)
- All Emqs Saqs Sample QsДокумент12 страницAll Emqs Saqs Sample QsSanathRaoОценок пока нет
- The First Answer (A) Is Correct!Документ44 страницыThe First Answer (A) Is Correct!Cynthia GОценок пока нет
- Cardiology EmqДокумент8 страницCardiology EmqislamawniОценок пока нет
- 1st Year Sendup MCQsДокумент8 страниц1st Year Sendup MCQsTARIQОценок пока нет
- 2003 2008 MCQДокумент81 страница2003 2008 MCQIshola Segun SamuelОценок пока нет
- Toacs Surgical Trainees 2009 AДокумент15 страницToacs Surgical Trainees 2009 AAnonymous bzHRfZzv100% (1)
- Pat An AnewДокумент126 страницPat An AnewgshchurovskiyОценок пока нет
- Adrenaline (Child, Adult, IM, IV... ) Ya Corticosteroids Too Asthma Ya Croup o ..Документ17 страницAdrenaline (Child, Adult, IM, IV... ) Ya Corticosteroids Too Asthma Ya Croup o ..raji selvakumaranОценок пока нет
- Pass Medicine Key Points 2020Документ53 страницыPass Medicine Key Points 2020fizaОценок пока нет
- Last Minute Revision Points LMRPДокумент4 страницыLast Minute Revision Points LMRPbetsyОценок пока нет
- Okell MedicineДокумент300 страницOkell MedicinePeprah Ondiba100% (2)
- How To Prepare Paeds Viva Practical Ospe MBBS Final Year PakistanДокумент3 страницыHow To Prepare Paeds Viva Practical Ospe MBBS Final Year PakistanAhmad HassanОценок пока нет
- Pediatrics One Liner For TestДокумент2 страницыPediatrics One Liner For TestArvindhanОценок пока нет
- Paediatrics Best RДокумент21 страницаPaediatrics Best RfrabziОценок пока нет
- Toacs 8Документ305 страницToacs 8Mobin Ur Rehman Khan100% (2)
- Core Topics in Internal MedicineДокумент4 страницыCore Topics in Internal MedicineKristina Anne CoОценок пока нет
- Abdominal Examination MCQДокумент12 страницAbdominal Examination MCQAsad ullahОценок пока нет
- Obg LMRP 2019Документ34 страницыObg LMRP 2019skОценок пока нет
- Guideline On Covid 19 in PregnancyДокумент21 страницаGuideline On Covid 19 in PregnancyNalin AbeysingheОценок пока нет
- TOG Manchester RepairДокумент6 страницTOG Manchester RepairNalin AbeysingheОценок пока нет
- TOG Manchester RepairДокумент6 страницTOG Manchester RepairNalin AbeysingheОценок пока нет
- Modified Bishop Score To Assess Cervical FavorabilityДокумент1 страницаModified Bishop Score To Assess Cervical FavorabilityNalin AbeysingheОценок пока нет
- Impact of Delta On Viral Burden and Vaccine Effectiveness Against New SARS-CoV-2 Infections in The UKДокумент39 страницImpact of Delta On Viral Burden and Vaccine Effectiveness Against New SARS-CoV-2 Infections in The UKNalin AbeysingheОценок пока нет
- How To Make Sense of A Cochrane ReviewДокумент11 страницHow To Make Sense of A Cochrane ReviewNalin AbeysingheОценок пока нет
- IndexДокумент1 страницаIndexNalin AbeysingheОценок пока нет
- IndexДокумент1 страницаIndexNalin AbeysingheОценок пока нет
- Early Pregnancy Complications AssessmentДокумент1 страницаEarly Pregnancy Complications AssessmentNalin AbeysingheОценок пока нет
- Cervical OncologyДокумент17 страницCervical OncologyNalin AbeysingheОценок пока нет
- Early Pregnancy Complications-MiscarriageДокумент2 страницыEarly Pregnancy Complications-MiscarriageNalin AbeysingheОценок пока нет
- Impact of Delta On Viral Burden and Vaccine Effectiveness Against New SARS-CoV-2 Infections in The UKДокумент39 страницImpact of Delta On Viral Burden and Vaccine Effectiveness Against New SARS-CoV-2 Infections in The UKNalin AbeysingheОценок пока нет
- Abdominal Wall MusclesДокумент2 страницыAbdominal Wall MusclesNalin AbeysingheОценок пока нет
- Consultants PositionДокумент2 страницыConsultants PositionNalin AbeysingheОценок пока нет
- Giman HarinaДокумент2 страницыGiman HarinaNalin AbeysingheОценок пока нет
- 20th Amendment Draft Sri LankaДокумент43 страницы20th Amendment Draft Sri LankaRivira MediaОценок пока нет
- Cervical OncologyДокумент17 страницCervical OncologyNalin AbeysingheОценок пока нет
- Causes of Male InfertilityДокумент18 страницCauses of Male InfertilityNalin AbeysingheОценок пока нет
- Cervical OncologyДокумент17 страницCervical OncologyNalin AbeysingheОценок пока нет
- EmbryologyДокумент1 страницаEmbryologyNalin AbeysingheОценок пока нет
- Exploring The Concepts of Intended, Planned, and Wanted PregnancyДокумент9 страницExploring The Concepts of Intended, Planned, and Wanted PregnancyNalin AbeysingheОценок пока нет
- VAT Act No 14 (E) 2002 (Consolidation 2014) PDFДокумент120 страницVAT Act No 14 (E) 2002 (Consolidation 2014) PDFNalin AbeysingheОценок пока нет
- Motor Traffic Act - Road SignsДокумент85 страницMotor Traffic Act - Road SignsAudithya KahawattaОценок пока нет
- MRCOG NotesДокумент1 страницаMRCOG NotesNalin AbeysingheОценок пока нет
- Exposure Normal Cells Precursors Invasive Cancer: Natural History of Cervical CancerДокумент6 страницExposure Normal Cells Precursors Invasive Cancer: Natural History of Cervical CancerNalin AbeysingheОценок пока нет
- Tromboelas Tecnologia y AplicacionesДокумент5 страницTromboelas Tecnologia y Aplicacionesjavier511833Оценок пока нет
- Air AДокумент6 страницAir AAli AlisonОценок пока нет
- Modified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2Документ9 страницModified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2indirinoor5Оценок пока нет
- Exposure Normal Cells Precursors Invasive Cancer: Natural History of Cervical CancerДокумент6 страницExposure Normal Cells Precursors Invasive Cancer: Natural History of Cervical CancerNalin AbeysingheОценок пока нет
- LSCSДокумент70 страницLSCSNalin AbeysingheОценок пока нет
- English File: Grammar, Vocabulary, and PronunciationДокумент4 страницыEnglish File: Grammar, Vocabulary, and PronunciationFirstName100% (2)
- Phil. Organic ActДокумент15 страницPhil. Organic Actka travelОценок пока нет
- Module ConnectionsДокумент16 страницModule ConnectionsHemilton Cheng Modulos100% (1)
- Sound Culture: COMS 350 (001) - Winter 2018Документ12 страницSound Culture: COMS 350 (001) - Winter 2018Sakshi Dhirendra MishraОценок пока нет
- Recollections From Pine Gulch QuestionsДокумент2 страницыRecollections From Pine Gulch Questionsoliver abramsОценок пока нет
- Physics Tadka InstituteДокумент15 страницPhysics Tadka InstituteTathagata BhattacharjyaОценок пока нет
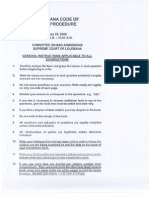
- July 2006 Bar Exam Louisiana Code of Civil ProcedureДокумент11 страницJuly 2006 Bar Exam Louisiana Code of Civil ProcedureDinkle KingОценок пока нет
- MCS 150 Page 1Документ2 страницыMCS 150 Page 1Galina NovahovaОценок пока нет
- Abb PB - Power-En - e PDFДокумент16 страницAbb PB - Power-En - e PDFsontungОценок пока нет
- Vulnerabilidades: Security Intelligence CenterДокумент2 страницыVulnerabilidades: Security Intelligence Centergusanito007Оценок пока нет
- SMA Releases Online Version of Sunny Design For PV System ConfigurationДокумент3 страницыSMA Releases Online Version of Sunny Design For PV System ConfigurationlakliraОценок пока нет
- Connecting Microsoft Teams Direct Routing Using AudioCodes Mediant Virtual Edition (VE) and Avaya Aura v8.0Документ173 страницыConnecting Microsoft Teams Direct Routing Using AudioCodes Mediant Virtual Edition (VE) and Avaya Aura v8.0erikaОценок пока нет
- SMM Live Project MICA (1) (1)Документ8 страницSMM Live Project MICA (1) (1)Raj SinghОценок пока нет
- Stance AdverbsДокумент36 страницStance Adverbsremovable100% (3)
- Peace Corps Samoa Medical Assistant Office of The Public Service of SamoaДокумент10 страницPeace Corps Samoa Medical Assistant Office of The Public Service of SamoaAccessible Journal Media: Peace Corps DocumentsОценок пока нет
- ColceruM-Designing With Plastic Gears and General Considerations of Plastic GearingДокумент10 страницColceruM-Designing With Plastic Gears and General Considerations of Plastic GearingBalazs RaymondОценок пока нет
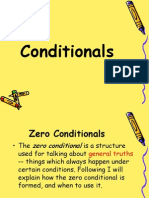
- 4aeaconditionals 110228122737 Phpapp01Документ24 страницы4aeaconditionals 110228122737 Phpapp01Luis Fernando Ponce JimenezОценок пока нет
- Miraculous MedalДокумент2 страницыMiraculous MedalCad work1Оценок пока нет
- The Best John Green QuotesДокумент10 страницThe Best John Green Quotesapi-586467925Оценок пока нет
- Bruce and The Spider: Grade 5 Reading Comprehension WorksheetДокумент4 страницыBruce and The Spider: Grade 5 Reading Comprehension WorksheetLenly TasicoОценок пока нет
- Conflict Management and Negotiation - Team 5Документ34 страницыConflict Management and Negotiation - Team 5Austin IsaacОценок пока нет
- The Craving Mind From Cigarettes To Smartphones To Love - Why We Get Hooked and How We Can Break Bad Habits PDFДокумент257 страницThe Craving Mind From Cigarettes To Smartphones To Love - Why We Get Hooked and How We Can Break Bad Habits PDFJacques Savariau92% (13)
- 39 Nts General Merit List 22 Mar 18Документ26 страниц39 Nts General Merit List 22 Mar 18Lakshmi VedanarayananОценок пока нет
- Critical Evaluation of Biomedical LiteraturesДокумент34 страницыCritical Evaluation of Biomedical LiteraturesPratibha NatarajОценок пока нет
- Two Gentlemen of VeronaДокумент13 страницTwo Gentlemen of Veronavipul jainОценок пока нет
- SurrealismДокумент121 страницаSurrealismLaurence SamonteОценок пока нет
- UBFHA V S BF HomesДокумент11 страницUBFHA V S BF HomesMonique LhuillierОценок пока нет
- Reading 7.1, "Measuring and Managing For Team Performance: Emerging Principles From Complex Environments"Документ2 страницыReading 7.1, "Measuring and Managing For Team Performance: Emerging Principles From Complex Environments"Sunny AroraОценок пока нет
- 7C Environment Test 2004Документ2 страницы7C Environment Test 2004api-3698146Оценок пока нет
- Lesson PlansДокумент9 страницLesson Plansapi-238729751Оценок пока нет