Академический Документы
Профессиональный Документы
Культура Документы
Sterilization Methods and Principles
Загружено:
Chanthini VinayagamИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Sterilization Methods and Principles
Загружено:
Chanthini VinayagamАвторское право:
Доступные форматы
Introduction Sterilization can be defined as any process that effectively kills or eliminates transmissible agents (such as fungi, bacteria,
viruses and prions) from a surface, equipment, foods, medications, or biological culture medium. In practice sterility is achieved by exposure of the ob ect to be sterilized to chemical or physical agent for a specified time. !arious agents used as steriliants are" elevated temperature, ionizing radiation, chemical liquids or gases etc. #he success of the process depends upon the choice of the method adopted for sterilization. Pharmaceutical Importance of Sterilization $% &oist heat sterilization is the most efficient biocidal agent. In the pharmaceutical industry it is used for" Surgical dressings, Sheets, Surgical and diagnostic equipment, 'ontainers, 'losures, (queous in ections, )phthalmic preparations and Irrigation fluids etc. *% +ry heat sterilization can only be used for thermo stable, moisture sensitive or moisture impermeable pharmaceutical and medicinal. #hese include products like, +ry po-dered drugs, Suspensions of drug in non aqueous solvents, )ils, fats -axes, soft hard paraffin silicone, )ily in ections, implants, ophthalmic ointments and ointment bases etc. .% /aseous sterilization is used for sterilizing thermolabile substances like, hormones, proteins, various heat sensitive drugs etc. 0% 1.! light is perhaps the most lethal component in ordinary sunlight used in sanitation of garments or utensils. 2% /amma3rays from 'obalt 45 are used to sterilize antibiotic, hormones, sutures, plastics and catheters etc. 4% 6iltration sterilizations are used in the treatment of heat sensitive in ections and ophthalmic solutions, biological products, air and other gases for supply to aseptic areas. #hey are also used in industry as part of the venting systems on fermentors, centrifuges, autoclaves and freeze driers. &embrane filters are used for sterility testing. !ariables that affect sterilization include" $. #he dryness of devices to be processed *. #he temperature and humidity of the processing area .. 7hether or not the devices -ere properly prepared and loaded into the sterilizer 0. 7hether or not the sterilizing agent is properly delivered into the system 2. #he sterilizer8s condition and maintenance protocol 4. 7hether or not the correct sterilization method and cycle -ere used Terms commonly used Survivor curves #hey are plots of the logarithm of the fraction of survivors (microorganisms -hich retain
viability follo-ing a sterilization process) against the exposure time or dose.
Expression of resistance D-value +3value is indicative of the resistance of any organism to a sterilizing agent. 6or radiation and heat treatment, +3value is the time taken at a fixed temperature or the radiation dose required to achieve a 95: reduction in viable count. Z-value ;3value represents the increase in temperature needed to reduce the +3value of an organism by 95:. Methods of Sterilization #he various methods of sterilization are" $. <hysical ðod $. #hermal (=eat) methods *. >adiation method .. 6iltration method 'hemical ðod $. /aseous method
*.
$. Heat Sterilization =eat sterilization is the most -idely used and reliable method of sterilization, involving destruction of enzymes and other essential cell constituents. #he process is more effective in hydrated state -here under conditions of high humidity, hydrolysis and denaturation occur, thus lo-er heat input is required. 1nder dry state, oxidative changes take place, and higher heat input is required. #his method of sterilization can be applied only to the thermostable products, but it can be used 5 for moisture3sensitive materials for -hich dry heat ($453$?5 ') sterilization, and for moisture3 resistant materials for -hich moist heat ($*$3$.05') sterilization is used. #he efficiency -ith -hich heat is able to inactivate microorganisms is dependent upon the degree of heat, the exposure time and the presence of -ater. #he action of heat -ill be due to induction of lethal chemical events mediated through the action of -ater and oxygen. In the presence of -ater much lo-er temperature time exposures are required to kill microbe than in the absence of -ater. In this processes both dry and moist heat are used for sterilization. a. Dry Heat Sterilization @xamples of +ry heat sterilization are" $. Incineration *. >ed heat .. 6laming 0. =ot air oven It employs higher temperatures in the range of $453$?55' and requires exposures time up to * hours, depending upon the temperature employed. #he benefit of dry heat includes good penetrability and non3corrosive nature -hich makes it applicable for sterilizing glass-ares and
metal surgical instruments. It is also used for sterilizing non3aqueous thermostable liquids and thermostable po-ders. +ry heat destroys bacterial endotoxins (or pyrogens) -hich are difficult to eliminate by other means and this property makes it applicable for sterilizing glass bottles -hich are to be filled aseptically. Hot-air oven +ry heat sterilization is usually carried out in a hot air oven, -hich consists of the follo-ing" $) *) .) 0) 2) 4) !peration $) *) .) 0) (rticles to be sterilized are first -rapped or enclosed in containers of cardboard, paper or aluminum. #hen, the materials are arranged to ensure uninterrupted air flo-. )ven may be pre3heated for materials -ith poor heat conductivity. 5 #he temperature is allo-ed to fall to 05 ', prior to removal of sterilized material. (n insulated chamber surrounded by an outer case containing electric heaters. ( fan Shelves #hermocouples #emperature sensor +oor locking controls.
b.Moist Heat Sterilization &oist heat may be used in three forms to achieve microbial inactivation $. +ry saturated steam A (utoclaving *. Boiling -aterC steam at atmospheric pressure .. =ot -ater belo- boiling point &oist heat sterilization involves the use of steam in the range of $*$3$.0 5'. Steam under pressure is used to generate high temperature needed for sterilization. Saturated steam (steam in thermal equilibrium -ith -ater from -hich it is derived) acts as an effective sterilizing agent. Steam for sterilization can be either -et saturated steam (containing entrained -ater droplets) or dry saturated steam (no entrained -ater droplets). (utoclaves use pressurized steam to destroy microorganisms, and are the most dependable systems available for the decontamination of laboratory -aste and the sterilization of laboratory glass-are, media, and reagents. 6or efficient heat transfer, steam must flush the air out of the autoclave chamber. Before using the autoclave, check the drain screen at the bottom of the chamber and clean if blocked. If the sieve is blocked -ith debris, a layer of air may form at the bottom of the autoclave, preventing efficient operation. (utoclaves should be tested periodically -ith biological indicators like cultures of Bacillus stearothermophilus to ensure proper function. #his method of sterilization -orks -ell for many metal and glass items but is not acceptable for rubber, plastics, and equipment that -ould be damaged by high temperatures (6igure $).
6ig. $" (n (utoclave (utoclaves, or steam sterilizers essentially consist of follo-ing" $) *) .) 0) 2) 4) ( cylindrical or rectangular chamber, -ith capacities ranging from 055 to ?55 liters. 7ater heating system or steam generating system Steam outlet and inlet valves Single or double doors -ith locking mechanism. #hermometer or temperature gauge <ressure gauges
!peration 6or porous loads (dressings) sterilizers are generally operated at a minimum temperature of
$.0 ', and for bottled fluid, sterilizers employing a minimum temperature of $*$ ' are used. @nsure that there should be sufficient -ater in the autoclave to produce the steam. #he stages of operation of autoclaves include air removal, steam admission and sterilization cycle (includes heating up, holdingCexposure, and cooling stages). "aseous Sterilization #he chemically reactive gases such as formaldehyde, (methanol, =.'=)) and ethylene oxide ('=*)*) possess biocidal activity. @thylene oxide is a colorless, odorless, and flammable gas. #he mechanism of antimicrobial action of the t-o gases is assumed to be through alkylations of sulphydryl, amino, hydroxyl and carboxyl groups on proteins and amino groups of nucleic acids. #he concentration ranges (-eight of gas per unit chamber volume) are usually in range of ?553 $*55 mgCD for ethylene oxide and $23$55 mgCD for formaldehyde -ith operating temperatures of 0234.E' and F53F2E' respectively. Both of these gases being alkylating agents are potentially mutagenic and carcinogenic. #hey also produce acute toxicity including irritation of the skin, con unctiva and nasal mucosa.
a# Ethylene oxide sterilizer (n ethylene oxide sterilizer consists of a chamber of $553.553Ditre capacity and surrounded by a -ater acket. (ir is removed from sterilizer by evacuation, humidification and conditioning of the load is done by passing sub3atmospheric pressure steam, then evacuation is done again and preheated vaporized ethylene oxide is passed. (fter treatment, the gases are evacuated either directly to the outside atmosphere or through a special exhaust system. @thylene oxide gas has been used -idely to process heat3sensitive devices, but the aeration times needed at the end of the cycle to eliminate the gas made this method slo-. $# %o& temperature steam formaldehyde '%TS() sterilizer (n D#S6 sterilizer operates -ith sub atmospheric pressure steam. (t first, air is removed by evacuation and steam is admitted to the chamber. %i*uid Sterilization a# Peracetic +cid li*uid sterilization <eracetic acid -as found to be sporicidal at loconcentrations. It -as also found to be -ater soluble, and left no residue after rinsing. It -as also sho-n to have no harmful health or environmental effects. It disrupts bonds in proteins and enzymes and may also interfere -ith cell membrane transportation through the rupture of cell -alls and may oxidize essential enzymes and impair vital biochemical path-ays. In a lo-3temperature liquid chemical sterile processing system, several steps must be follo-ed for effective sterilization" $. <re3cleaning of the devices is necessary because many devices have small connected lumens. *. Deak testing is done to ensure there are no leaks that could allo- fluid to enterCleak the ampoulesCvials and cause damage. .. #he appropriate trayCcontainer must then be selected, and if the device has lumens, the appropriate connector attached. 0. #he sterilant concentrate is provided in a sealed single3 use cup and requires no pre3mixing or dilution. #he disadvantages of this method of sterilization are that the devices must be immersible, must fit in the appropriate tray, and must be able to -ithstand the 22E' temperature the process uses. $# Hydro,en Peroxide Sterilization #his method disperses a hydrogen peroxide solution in a vacuum chamber, creating a plasma cloud. #his agent sterilizes by oxidizing key cellular components, -hich inactivates the microorganisms. #he plasma cloud exists only -hile the energy source is turned on. 7hen the energy source is turned off, -ater vapor and oxygen are formed, resulting in no toxic residues and harmful emissions. #he temperature of this sterilization method is maintained in the 05325E' range, -hich makes it particularly -ell3suited for use -ith heat3sensitive and moisture3sensitive medical devices. #he instruments are -rapped prior to sterilization, and can either be stored or used immediately.
#here are five phases of the hydrogen peroxide processing cycle" $. ( vacuum phase creates a vacuum in the chamber and the pressure drops to less than one pound per square inch. #his phase lasts about *5 minutes. *. In the in ection phase, the aqueous hydrogen peroxide is introduced into the vacuum chamber and is vaporized into a gas, -hich creates a rise in pressure due to the increase of molecules. .. +uring the diffusion phase the hydrogen peroxide vapor spreads throughout the chamber and the increased pressure drives the sterilant into the packs, exposing the instrument surfaces to the sterilant and killing the microorganisms. 0. +uring the plasma phase the radio frequency energy is applied, stripping the electrons from some of the molecules and producing a lo-3temperature plasma cloud. 6ollo-ing this reaction, the activated compounds lose their high energy and recombine to form oxygen and -ater. 2. #he purpose of the venting phase is to introduce filtered air into the chamber and return the chamber to atmospheric pressure so that the door can be opened. It lasts about one minute. -adiation Sterilization &any types of radiation are used for sterilization like electromagnetic radiation (e.g. gamma rays and 1! light), particulate radiation (e.g. accelerated electrons) .#he ma or target for these radiation is microbial +G(. /amma rays and electrons cause ionization and free radical production -hile 1! light causes excitation. >adiation sterilization -ith high energy gamma rays or accelerated electrons has proven to be a useful method for the industrial sterilization of heat sensitive products. But some undesirable changes occur in irradiated products, an example is aqueous solution -here radiolysis of -ater occurs. >adiation sterilization is generally applied to articles in the dry state, including surgical instruments, sutures, prostheses, unit dose ointments, plastic syringes and dry pharmaceutical products. 1! light, -ith its much lo-er energy, and poor penetrability finds uses in the sterilization of air, for surface sterilization of aseptic -ork areas, for treatment of manufacturing grade -ater, but is not suitable for sterilization of pharmaceutical dosage forms. a# "amma ray Sterilizer /amma rays for sterilization are usually derived from cobalt345 source, the isotope is held as pellets packed in metal rods, each rod carefully arranged -ithin the source and containing *5 H'i of activity. #his source is housed -ithin a reinforced concrete building -ith * m thick -alls. (rticles being sterilized are passed through the irradiation chamber on a conveyor belt and move around the raised source. .ltraviolet Irradiation #he optimum -avelength for 1! sterilization is *45 nm. ( mercury lamp giving peak emission at *20 nm is the suitable source of 1! light in this region.
Electron +ccelerator #here are t-o types of electron accelerator machines, the electrostatic accelerator -hich produces electrons -ith maximum energies of 2 &e!, and the micro-ave linear accelerator -hich produces electrons -ith maximum energies of $5 &e!. =igher energies cause better penetration into the product but there is a risk of induced radiation. ( high energy electron beam is generated by accelerating electrons from a hot filament do-n an evacuated tube under high potential difference, and then additional energy is imparted to this beam in a pulsed manner by a synchronized traveling micro-ave. (rticles to be sterilized are arranged on a horizontal conveyor belt and are irradiated from one or both sides. (iltration Sterilization 6iltration process does not destroy but removes the microorganisms. It is used for both the clarification and sterilization of liquids and gases as it is capable of preventing the passage of both viable and non viable particles. #he ma or mechanisms of filtration are sieving, adsorption and trapping -ithin the matrix of the filter material. Sterilizing grade filters are used in the treatment of heat sensitive in ections and ophthalmic solutions, biological products and air and other gases for supply to aseptic areas. #hey are also used in industry as part of the venting systems on fermentors, centrifuges, autoclaves and freeze driers. &embrane filters are used for sterility testing. +pplication of filtration for sterilization of ,ases =@<( (=igh efficiency particulate air) filters can remove up to 99.9F: of particles I5.. micrometer in diameter. (ir is first passed through prefilters to remove larger particles and then passed through =@<( filters. #he performance of =@<( filter is monitored by pressure differential and airflo- rate measurements. #here are t-o types of filters used in filtration sterilization ($) Depth filters 'onsist of fibrous or granular materials so packed as to form t-isted channels of minute dimensions. #hey are made of diatomaceous earth, unglazed porcelain filter, sintered glass or asbestos. (*) Mem$rane filters #hese are porous membrane about 5.$ mm thick, made of cellulose acetate, cellulose nitrate, polycarbonate, and polyvinylidene fluoride, or some other synthetic material.#he membranes are supported on a frame and held in special holders. 6luids are made to transverse membranes by positive or negative pressure or by centrifugation. +pplication of filtration for sterilization of li*uids &embrane filters of 5.** micrometer nominal pore diameter are generally used, but sintered filters are used for corrosive liquids, viscous fluids and organic solvents. #he factors -hich affects the performance of filter is the titre reduction value, -hich is the ratio of the number of organism challenging the filter under defined conditions to the number of organism penetrating it. #he other factors are the depth of the membrane, its charge and the tortuosity of the channels. #he merits, demerits and applications of different methods of sterilization are given in #able $.
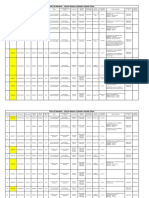
Ta$le / Merits0 Demerits and +pplications of Different Methods of Sterilization
Methods =eat sterilization Mechanism +estroys bacterial endotoxins Merits &ost -idely used and reliable method of sterilization, involving destruction of enzymes and other essential cell constituents. Demer its 'an be applied only to the thermostable product s +pplication s +ry heat is applicable for sterilizing glass-ares and metal surgical instruments and moi heat is st the most dependable method for decontamination of laboratory -aste and the sterilization of laboratory glass-are, media, and reagents. @thylene oxide gas use has been d -id ely to process heat3 sensitive devices. >adiation sterilization is generally applied to articles in the dry state, including surgical instruments, sutures, prostheses, unit dose
/aseous sterilization
(lkylation
<enetrati ng ability of gases
/ases being alkylati ng agents are potentially mutagenic and carcinogenic 1ndesirable change occu s r in irradiated products,an exampl e is aqueou s solutio -her n e radioly sis of -ater occurs.
>adiation sterilization
Ionization of nucleic acids
It is a useful method for the industrial sterilization of heat sensitive products.
6iltration sterilization
+oes not destroy but removes the microorganisms
It is used both clarificati on and sterilizati on liquids
fo r th e
+oes not differentiate bet-een viable and non viable particle s
ointments, plastics #his method is Sterilizing grade filters are used in the treatment of heat sensitive in ections and ophthalmic solutions, biological products and air and other gases for supply to aseptic area s.
of an d
gases as it is capable of preventin th g e passage of both viable no and n viable particles.
Вам также может понравиться
- 10562997Документ81 страница10562997Ppa Gpat AmitОценок пока нет
- EtO-MD Sterilization and Autoclave Sterilization Complement Each OtherДокумент3 страницыEtO-MD Sterilization and Autoclave Sterilization Complement Each OtherVer BautistaОценок пока нет
- Log Book HorizontalДокумент38 страницLog Book HorizontalmateoОценок пока нет
- Autoclave Tuttnauer 2340M Support - MAN - ManualДокумент47 страницAutoclave Tuttnauer 2340M Support - MAN - ManualDavid Hernandez100% (1)
- AXIS Eto Gas Sterilization System-Introduction Guide-2008Документ6 страницAXIS Eto Gas Sterilization System-Introduction Guide-2008sureshvgkОценок пока нет
- Autoclave 4136 PDFДокумент3 страницыAutoclave 4136 PDFSalvador PeraltaОценок пока нет
- SterilizationДокумент126 страницSterilizationj.k.kumar100% (7)
- Medical Sterilization Methods - LemoДокумент52 страницыMedical Sterilization Methods - LemoPedro GomesОценок пока нет
- Autoklaf Page 3.bin PDFДокумент16 страницAutoklaf Page 3.bin PDFNadya Rizky SОценок пока нет
- Bowie Dick Test RelevanceДокумент42 страницыBowie Dick Test RelevancePrakashKandaswamyОценок пока нет
- Biological Safety Cabinet SC2 - AДокумент4 страницыBiological Safety Cabinet SC2 - AlucasОценок пока нет
- Laboklav Steam Sterilizer User ManualДокумент29 страницLaboklav Steam Sterilizer User ManualMathesis ConsultoraОценок пока нет
- Instruction Manual Autoclave SEA-22B 17BДокумент32 страницыInstruction Manual Autoclave SEA-22B 17BAntónio ValenteОценок пока нет
- VHPДокумент2 страницыVHPschumonОценок пока нет
- CSSD CPT ManualДокумент3 страницыCSSD CPT Manualthirsal2003Оценок пока нет
- Ethylene Oxide Gas (Eto) Sterilizers: DE LAMA Holds The Quality System Certificates ISO 9001 and EN 46001Документ6 страницEthylene Oxide Gas (Eto) Sterilizers: DE LAMA Holds The Quality System Certificates ISO 9001 and EN 46001soajaniiОценок пока нет
- Washer disinfector user manual highlightsДокумент20 страницWasher disinfector user manual highlightsDodik E. PrasetyoОценок пока нет
- AMSCO Evolution - Technical InformationДокумент13 страницAMSCO Evolution - Technical InformationNimsi AstiviaОценок пока нет
- Presentasi SteelcoДокумент46 страницPresentasi SteelcoRSUD SOLOKОценок пока нет
- Brosura Sterlink PDFДокумент28 страницBrosura Sterlink PDFDana Andreea PopescuОценок пока нет
- HD 680 DE/DE-V/DEI-V - HD 650 D/DEДокумент4 страницыHD 680 DE/DE-V/DEI-V - HD 650 D/DERawandОценок пока нет
- Soring User Manual Macro Handpiece PDFДокумент9 страницSoring User Manual Macro Handpiece PDFDanilo FagundesОценок пока нет
- MEMMERT BR Heating Ovens English D13646Документ32 страницыMEMMERT BR Heating Ovens English D13646Anonymous Z6BF3n78Оценок пока нет
- Flame Photometer ManualДокумент50 страницFlame Photometer ManualNanjilaОценок пока нет
- Product Catalogue Biological Indicators, Process Challenge Devices and Accessories PDFДокумент24 страницыProduct Catalogue Biological Indicators, Process Challenge Devices and Accessories PDFscribdddcОценок пока нет
- Getinge 46-Series Washer Disinfector: Configuration SheetДокумент10 страницGetinge 46-Series Washer Disinfector: Configuration SheetDany RobinОценок пока нет
- Medical Waste ManagementДокумент50 страницMedical Waste ManagementNisa ShiningОценок пока нет
- Small SterilizerДокумент36 страницSmall Sterilizernotaden1849100% (1)
- Flash SterilizationДокумент0 страницFlash SterilizationTanya GoriОценок пока нет
- STERIS Century Series Autoclave: User Guidelines & Standard Operating Procedure For TheДокумент38 страницSTERIS Century Series Autoclave: User Guidelines & Standard Operating Procedure For TheNasr Eldin AlyОценок пока нет
- Biological Safety Cabinet SafesolДокумент9 страницBiological Safety Cabinet SafesolnatrajangОценок пока нет
- C4+ Maintenance ManualДокумент28 страницC4+ Maintenance Manualnorizam77100% (1)
- Preventive Maintenance Manual for FEDEGARIAUTOCLAVE Borozontal FOF2/A NA3018BA8 NA3019BAДокумент62 страницыPreventive Maintenance Manual for FEDEGARIAUTOCLAVE Borozontal FOF2/A NA3018BA8 NA3019BAAndre FikasОценок пока нет
- Air Techniques CompressorsДокумент20 страницAir Techniques CompressorsHaris Krnić0% (1)
- Central Sterile Supply Services Policy KKM PDFДокумент53 страницыCentral Sterile Supply Services Policy KKM PDFGerald TalledoОценок пока нет
- SOP: Tuttnauer 3850 ELV Autoclave Operation: ApprovalsДокумент5 страницSOP: Tuttnauer 3850 ELV Autoclave Operation: Approvalsfrank luОценок пока нет
- Hydrogen Peroxide DeconДокумент6 страницHydrogen Peroxide DeconSurendar KesavanОценок пока нет
- BS 3970-5-1990 - (2018-06-20 - 03-47-55 Am)Документ16 страницBS 3970-5-1990 - (2018-06-20 - 03-47-55 Am)Rankie ChoiОценок пока нет
- HS SLSMAN 01 Rev.W - Pasteurizer 520 115V Operation ManualДокумент33 страницыHS SLSMAN 01 Rev.W - Pasteurizer 520 115V Operation ManualErick LoganОценок пока нет
- Validation Benchtop Sterilizers db9804Документ47 страницValidation Benchtop Sterilizers db9804anon-285784Оценок пока нет
- Cytoperm & BBD 6220Документ285 страницCytoperm & BBD 6220here_rkОценок пока нет
- Operation & Maintenance Manual for Tuttnauer Steam SterilizersДокумент48 страницOperation & Maintenance Manual for Tuttnauer Steam SterilizersJuan Jose Palomino Quispe100% (1)
- Technician Manual for Tuttnauer Steam SterilizersДокумент104 страницыTechnician Manual for Tuttnauer Steam SterilizerscaseroizeОценок пока нет
- KaVo QUATTROcare 2104 BrochureДокумент2 страницыKaVo QUATTROcare 2104 Brochuretopobuccia100% (1)
- Disinfection vs Sterilization: A Comparison of Key AspectsДокумент33 страницыDisinfection vs Sterilization: A Comparison of Key AspectsFitri AnggraeniОценок пока нет
- Hot Air Oven SterilizationДокумент13 страницHot Air Oven SterilizationDevanandDongreОценок пока нет
- Hanshin Hs 2519vdДокумент2 страницыHanshin Hs 2519vdnotaden1849Оценок пока нет
- Sanyo Mls 2420u 3020u Manual EngДокумент32 страницыSanyo Mls 2420u 3020u Manual EngKo HeinОценок пока нет
- 531-Autoclave Inspection and Routine Maintenance - SOP-finalДокумент8 страниц531-Autoclave Inspection and Routine Maintenance - SOP-finalIcee SinlapasertОценок пока нет
- Disinfection and Sterilization: Mary T. Post, RN, MS, CNS, CICДокумент58 страницDisinfection and Sterilization: Mary T. Post, RN, MS, CNS, CICPriya ManimalaОценок пока нет
- Multiprobe Temperature Verification Kit 4460108AДокумент57 страницMultiprobe Temperature Verification Kit 4460108APatricia MendozaОценок пока нет
- Biological Safety CabinetsДокумент4 страницыBiological Safety CabinetsHedy Mae Bautista100% (1)
- Reverberi Full Clave B16, B20 - Service ManualДокумент34 страницыReverberi Full Clave B16, B20 - Service ManualMoyses Moy100% (2)
- Moist Heat SterilizatiojnДокумент16 страницMoist Heat Sterilizatiojnajitjoshi950Оценок пока нет
- Auto Clave Validation ProcedureДокумент2 страницыAuto Clave Validation ProcedureSafira Nazlisa IstighfarinОценок пока нет
- How To SterilizeДокумент27 страницHow To SterilizeTanzeil_Rehman_4731Оценок пока нет
- Pharmaceutical Sterilization MethodsДокумент21 страницаPharmaceutical Sterilization MethodsSiva Raman100% (1)
- New 2ND Year Sterilization (8694)Документ13 страницNew 2ND Year Sterilization (8694)Barry AllenОценок пока нет
- Bhutan Final BacteriologyДокумент56 страницBhutan Final Bacteriology99nonameОценок пока нет
- SterilizationДокумент40 страницSterilizationRajib SarkarОценок пока нет
- 30 Days Push Up ChallengeДокумент3 страницы30 Days Push Up ChallengeChanthini VinayagamОценок пока нет
- Cardinal Utility ApproachДокумент5 страницCardinal Utility ApproachChanthini VinayagamОценок пока нет
- StorytellingДокумент5 страницStorytellingChanthini VinayagamОценок пока нет
- GM DietДокумент8 страницGM DietChanthini Vinayagam100% (1)
- MBE NotesДокумент154 страницыMBE NotesSimson SimОценок пока нет
- Concept and Principles of HomeopathyДокумент2 страницыConcept and Principles of HomeopathyChanthini VinayagamОценок пока нет
- ModuleДокумент26 страницModuleSantosh KumarОценок пока нет
- A Survey of TQM Application in Healthcare - Case Analysis: Chanthini.VДокумент15 страницA Survey of TQM Application in Healthcare - Case Analysis: Chanthini.VChanthini VinayagamОценок пока нет
- Common Prefixes and SuffixesДокумент2 страницыCommon Prefixes and SuffixesChanthini Vinayagam100% (1)
- Basic Introduction Communicable DiseaseДокумент15 страницBasic Introduction Communicable DiseaseChanthini VinayagamОценок пока нет
- Understand the BCG growth-share matrix with this guideДокумент5 страницUnderstand the BCG growth-share matrix with this guideChanthini VinayagamОценок пока нет
- MotivationДокумент234 страницыMotivationChanthini VinayagamОценок пока нет
- Mohr V WilliamДокумент5 страницMohr V WilliamChanthini VinayagamОценок пока нет
- Perception Online NotesДокумент13 страницPerception Online NotesChanthini VinayagamОценок пока нет
- Adv N Disadv of Privatisation of Health Sector in IndiaДокумент5 страницAdv N Disadv of Privatisation of Health Sector in IndiaChanthini VinayagamОценок пока нет
- ABCs of CPR: A Simple Life-Saving ProcedureДокумент3 страницыABCs of CPR: A Simple Life-Saving ProcedureChanthini VinayagamОценок пока нет
- First Aid - CPR - AED Adult Ready ReferenceДокумент12 страницFirst Aid - CPR - AED Adult Ready Referenceadamiam100% (1)
- Approaches of MGMTДокумент17 страницApproaches of MGMTChanthini VinayagamОценок пока нет
- MANAGING InfectionДокумент11 страницMANAGING InfectionHumayun KhanОценок пока нет
- PhysiotherapyДокумент2 страницыPhysiotherapyChanthini VinayagamОценок пока нет
- Concepts and Principles of AyurvedaДокумент4 страницыConcepts and Principles of AyurvedaChanthini VinayagamОценок пока нет
- Pharmaceutical Sterilization MethodsДокумент21 страницаPharmaceutical Sterilization MethodsSiva Raman100% (1)
- Highlights of National Health Policy 2002Документ5 страницHighlights of National Health Policy 2002manasranjanpradhanОценок пока нет
- Change Management Leadership GuideДокумент30 страницChange Management Leadership GuideChanthini Vinayagam100% (2)
- The International Network of Health Promoting Hospitals and Health CareДокумент24 страницыThe International Network of Health Promoting Hospitals and Health CareChanthini Vinayagam100% (1)
- Change Management Leadership GuideДокумент30 страницChange Management Leadership GuideChanthini Vinayagam100% (2)
- 50 Home Remedies For Treating WrinklesДокумент5 страниц50 Home Remedies For Treating WrinklesChanthini VinayagamОценок пока нет
- Spru301c - Manual Ccs - Code Composer StudioДокумент126 страницSpru301c - Manual Ccs - Code Composer StudioJandfor Tansfg ErrottОценок пока нет
- Cupcake RecipesДокумент15 страницCupcake RecipesChanthini VinayagamОценок пока нет
- Resume Template & Cover Letter Bu YoДокумент4 страницыResume Template & Cover Letter Bu YoRifqi MuttaqinОценок пока нет
- Guidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016Документ76 страницGuidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016kofafa100% (1)
- Liebert PSP: Quick-Start Guide - 500VA/650VA, 230VДокумент2 страницыLiebert PSP: Quick-Start Guide - 500VA/650VA, 230VsinoОценок пока нет
- Ir35 For Freelancers by YunojunoДокумент17 страницIr35 For Freelancers by YunojunoOlaf RazzoliОценок пока нет
- 2010 - Impact of Open Spaces On Health & WellbeingДокумент24 страницы2010 - Impact of Open Spaces On Health & WellbeingmonsОценок пока нет
- Wasserman Chest 1997Документ13 страницWasserman Chest 1997Filip BreskvarОценок пока нет
- The Impact of School Facilities On The Learning EnvironmentДокумент174 страницыThe Impact of School Facilities On The Learning EnvironmentEnrry Sebastian71% (31)
- Reader's Digest (November 2021)Документ172 страницыReader's Digest (November 2021)Sha MohebОценок пока нет
- Sharp Ar5731 BrochureДокумент4 страницыSharp Ar5731 Brochureanakraja11Оценок пока нет
- The Berkeley Review: MCAT Chemistry Atomic Theory PracticeДокумент37 страницThe Berkeley Review: MCAT Chemistry Atomic Theory Practicerenjade1516Оценок пока нет
- Budgetary ControlsДокумент2 страницыBudgetary Controlssiva_lordОценок пока нет
- Memo Roll Out Workplace and Monitoring Apps Monitoring Apps 1Документ6 страницMemo Roll Out Workplace and Monitoring Apps Monitoring Apps 1MigaeaОценок пока нет
- Acne Treatment Strategies and TherapiesДокумент32 страницыAcne Treatment Strategies and TherapiesdokterasadОценок пока нет
- Logic and Set Theory PropositionДокумент3 страницыLogic and Set Theory PropositionVince OjedaОценок пока нет
- Polyol polyether+NCO Isupur PDFДокумент27 страницPolyol polyether+NCO Isupur PDFswapon kumar shillОценок пока нет
- Rubber Chemical Resistance Chart V001MAR17Документ27 страницRubber Chemical Resistance Chart V001MAR17Deepak patilОценок пока нет
- Maverick Brochure SMLДокумент16 страницMaverick Brochure SMLmalaoui44Оценок пока нет
- Honda Wave Parts Manual enДокумент61 страницаHonda Wave Parts Manual enMurat Kaykun86% (94)
- CMC Ready ReckonerxlsxДокумент3 страницыCMC Ready ReckonerxlsxShalaniОценок пока нет
- TDS Sibelite M3000 M4000 M6000 PDFДокумент2 страницыTDS Sibelite M3000 M4000 M6000 PDFLe PhongОценок пока нет
- Numerical Methods Chapter 10 SummaryДокумент8 страницNumerical Methods Chapter 10 SummarynedumpillilОценок пока нет
- DLP in Health 4Документ15 страницDLP in Health 4Nina Claire Bustamante100% (1)
- Trading As A BusinessДокумент169 страницTrading As A Businesspetefader100% (1)
- Algorithms For Image Processing and Computer Vision: J.R. ParkerДокумент8 страницAlgorithms For Image Processing and Computer Vision: J.R. ParkerJiaqian NingОценок пока нет
- Tension field beams: Aircraft wing spar analysisДокумент19 страницTension field beams: Aircraft wing spar analysisPrajeesh RajОценок пока нет
- 4 Wheel ThunderДокумент9 страниц4 Wheel ThunderOlga Lucia Zapata SavaresseОценок пока нет
- Mission Ac Saad Test - 01 QP FinalДокумент12 страницMission Ac Saad Test - 01 QP FinalarunОценок пока нет
- DC Motor Dynamics Data Acquisition, Parameters Estimation and Implementation of Cascade ControlДокумент5 страницDC Motor Dynamics Data Acquisition, Parameters Estimation and Implementation of Cascade ControlAlisson Magalhães Silva MagalhãesОценок пока нет
- Olympics Notes by Yousuf Jalal - PDF Version 1Документ13 страницOlympics Notes by Yousuf Jalal - PDF Version 1saad jahangirОценок пока нет
- Bharhut Stupa Toraa Architectural SplenДокумент65 страницBharhut Stupa Toraa Architectural Splenအသွ်င္ ေကသရОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesОт EverandThe Ultimate Guide To Memory Improvement TechniquesРейтинг: 5 из 5 звезд5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementОт EverandTechniques Exercises And Tricks For Memory ImprovementРейтинг: 4.5 из 5 звезд4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОценок пока нет
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 5 из 5 звезд5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingОт EverandThe Happiness Trap: How to Stop Struggling and Start LivingРейтинг: 4 из 5 звезд4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 5 из 5 звезд5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 3.5 из 5 звезд3.5/5 (31)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОт EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОценок пока нет
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossОт EverandThe Tennis Partner: A Doctor's Story of Friendship and LossРейтинг: 4.5 из 5 звезд4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisОт EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisРейтинг: 5 из 5 звезд5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)