Академический Документы
Профессиональный Документы
Культура Документы
Analysis of The Takeuchi Procedure For The Treatment of Anomalous Origin of The Left Coronary Artery From The Pulmonary Artery
Загружено:
Ana-Maria RamazanОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Analysis of The Takeuchi Procedure For The Treatment of Anomalous Origin of The Left Coronary Artery From The Pulmonary Artery
Загружено:
Ana-Maria RamazanАвторское право:
Доступные форматы
Original Article
Analysis of the Takeuchi Procedure for the Treatment of Anomalous Origin of the Left Coronary Artery from the Pulmonary Artery
Andrea Weirich Lenzi, Leo Solarewicz, Wanderley Saviollo Ferreira, Fbio Sallum, Nelson Itiro Miyague
Hospital Infantil Pequeno Prncipe, Curitiba, PR - Brazil
Summary
Background: Evaluation of a case series of anomalous origin of the left coronary artery from the pulmonary artery corrected with the Takeuchi procedure, analyzing their immediate and late surgical outcomes as well as the related morbidity. Objective: To report a case series of anomalous origin of the left coronary artery from the pulmonary artery corrected with the Takeuchi procedure. Methods: The analysis was based on data collected from the medical records of 12 patients undergoing surgical correction between 1981 and 2003. Results: The mean age of the patients was 5.9 1.7 months. The predominant manifestation was heart failure, especially in the infants. The baseline electrocardiogram showed a Q wave in DI and aVL and signs of myocardial ischemia in ten cases. Echocardiogram with a pattern of dilated cardiomyopathy and mitral regurgitation was found in six patients. The mean age at surgical correction was 31.8 14.3 months. The immediate surgical mortality was 16% (two patients), from cardiac dysfunction. In the outpatient follow-up we observed that the symptoms, ischemic electrocardiographic changes, cardiac function and mitral regurgitation improved. Three cases progressed with supravalvar pulmonary stenosis during follow-up. Conclusion: This heart disease should be suspected in every infant presenting with heart failure. Surgical correction with the Takeuchi procedure has proven efficient, with a low mortality rate. Cardiac function returns to normal and mitral regurgitation improves after surgical correction. (Arq Bras Cardiol 2008; 90(3):167-171) Key words: Coronary disease; cardiac output, low; heart defects, congenital; cardiomyopathies.
Introduction
Anomalous origin of the left coronary artery (ALCA) is a rare congenital anomaly in which the left coronary artery originates from the pulmonary artery or one of its branches. The estimated frequency is of 0.2% patients with congenital heart disease1,2. Approximately 80 to 90% of the patients die in their first year of life if left untreated. Morbidity is also high, and heart failure is the most frequent complication. This results from the ischemic cardiomyopathy induced by a reduction in myocardial perfusion. Infants survive thanks to the development of collaterals between the right and left coronary arteries, which reduces the ischemia2. The treatment of this condition is strictly surgical and consists of maintaining a viable two-coronary system, which is currently achieved using the technique of left coronary
Mailing address: Andrea Weirich Lenzi Rua Vicente Machado, 690/08 - Batel - 80420-011, Curitiba, PR - Brazil E-mail: andreawlenzi@yahoo.com.br Manuscript received February 26, 2007; revised manuscript received August 09, 2007; accepted October 16, 2007.
artery reimplantation into the aorta, or the creation of an intrapulmonary tunnel (Takeuchi procedure3). The objective of this study is to report a series of cases operated using the Takeuchi procedure, and to analyze the clinical profile of the patients as well as the surgical outcomes.
Materials and Methods
The sample studied is comprised of 12 patients seen at Hospital Infantil Pequeno Prncipe between 1981 and 2003, who underwent surgical correction using the Takeuchi procedure. Clinical, surgical, radiographic (chest), electrocardiographic, echocardiographic, and cardiac catheterization variables were analyzed. Mitral regurgitation was classified as mild, moderate and severe using color-Doppler analysis of the mitral regurgitant jet. All patients underwent surgical correction using the Takeuchi procedure performed by the same medical team. Data are expressed as means and standard deviation, and medians with limit values.
167
Lenzi et al Analysis of the Takeuchi Procedure in Hospital from Curitiba
Original Article
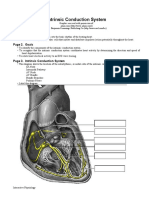
Surgical Technique In this service, the surgery is performed via a median sternotomy with the patient undergoing extracorporeal circulation with hypothermia. The Takeuchi procedure consists of the creation of an aortopulmonary window and of an intrapulmonary tunnel connecting the ostium of the left coronary artery to the aorta (Figure 1). For this purpose, the surgeon initially performs a transverse flap-shaped incision in the anterior wall of the pulmonary artery, thus exposing its interior, which enables the ostium of the left coronary artery to be located. Next, the surgeon creates a small aortopulmonary window through two longitudinal incisions, one in the aorta to the left, and the other in the basis of the pulmonary artery flap. Thus, a side-to-side anastomosis between these two orifices can be performed. Then, the flap obtained from the wall of the pulmonary artery is sutured to form a tunnel around the orifice of the coronary artery, using a running whipstitch suture. The resulting orifice in the anterior wall of the pulmonary artery is repaired with the placement of a PTF or pericardial patch using a running whipstitch suture. As the patient is weaned from the extracorporeal circulation, the surgeon checks the left coronary artery filling by the aorta and the need for reintervention. In the preoperative assessment, eight (66%) patients were referred for heart failure, and four (33%), for symptoms of irritability, dyspnea or refusal to eat. Five (41%) patients diagnosed with congestive heart failure were receiving medication regularly, and the most frequently used drugs were furosemide, captopril and digoxin. Ten (83%) patients presented a heart murmur suggestive of mitral regurgitation. All had cardiomegaly on chest radiography, with a mean cardiothoracic ratio of 0.6 0.06, and pulmonary congestion. The most frequent findings on resting electrocardiogram are shown in Table 1. The diagnosis of anomalous origin of the left coronary artery was confirmed by echocardiography in 10 patients (83%). Mitral regurgitation found in the 12 patients was graded as mild in five of them (42%), as moderate in six (54%), and as severe in one (4%). Six patients had a pattern of dilated cardiomyopathy, with a fractional shortening equal to or lower than 20% in five cases, and all had a left ventricular diastolic diameter higher than the normal values for the age. Three (25%) patients had associated congenital heart diseases: one with patent ductus arteriosus, another with patent ductus arteriosus plus ostium secundum atrial septal defect, and the third with pulmonary artery sling. Eight patients underwent cardiac catheterization for diagnostic confirmation, study of the coronary collateral circulation, and analysis of associated anomalies. Mean age at correction was 31.8 14.3 months. The modified technique was chosen, using PTFE for the construction of an intrapulmonary tunnel in two patients (cases 5 and 12 - Table 1). In one patient (case 7), mitral valve repair (posterior commissure plication) was also performed due to severe mitral regurgitation. All associated congenital anomalies were concomitantly corrected.
Results
Of the 12 patients analyzed, six were females. The mean age at the baseline visit was 5.9 1.7 months (2 months to 24 months), and by the time the study was carried out the median age was 57 months (17 to 167 months). The mean outpatient follow-up period was 37.6 14.4 months, with a median of 57.5 months.
Fig. 1 - Schematic Takeuchi procedure; A - side-to-side anastomosis between the aorta and the pulmonary artery after creation of an aortopulmonary window; B - construction of the intrapulmonary tunnel encircling the ostium of the left coronary artery; C - closure of the pulmonary artery with autologous tissue; D - final outcome; Source: KyrklinBarratt-Boyes. Cardiac Surgery third edition.
Arq Bras Cardiol 2008; 90(3) : 167-171
168
Lenzi et al Analysis of the Takeuchi Procedure in Hospital from Curitiba
Original Article
Table 1 - Clinical, electrocardiographic and echocardiographic data of the patients undergoing the Takeuchi procedure
Case 1 Age (months) 2 Manifestation CHF Baseline electrocardiogram LVO, LAO, q in DI and aVL, global alterations of ventricular repolarization LVO,LAO, q in DI and aVL, ST elevation DIII, global alterations of ventricular repolarization LVO, q in DI and aVL, global alterations of ventricular repolarization LVO, q in DI and aVL, global alterations of ventricular repolarization LVO, q in DI and aVL, LASDB , global alterations of ventricular repolarization LVO, q in DI and aVL, global alterations of ventricular repolarization LVO, LAO, RAO, q in DI and aVL, global alterations of ventricular repolarization RBBCA, q in DI and aVL, ST elevation V3-V6 LVO, LAO, RVO, global alterations of ventricular repolarization LVO, global alterations of ventricular repolarization LVO, q in DI and aVL, global alterations of ventricular repolarization LVO, q in DI and aVL, global alterations of ventricular repolarization Baseline echocardiogram ALCA, mild MR, DCM, FS 20% ALCA, moderate MR, DCM, FS 13% Mild MR, DCM, FS 25 %, PDA ALCA, mild MR, DCM, FS 17% ALCA, moderate MR, NHC ALCA, moderate MR, NHC Severe MR, NHC ALCA, moderate MR, DCM, FS 10 % ALCA, moderate MR, pulmonary artery sling ALCA, moderate MR, DCM, FS 10%, OS-ASD, PDA ALCA, mild MR, NHC Age at surgery (months) 2 Follow-up period (months) death
CHF
29
44
19
CHF
20
53
CHF
death
24
CHF
25
30
CHF
141
165
7 8 9
13 5 6
CHF Refusal to eat CHF
110 5 6
103 83 death
10
Irritability
15
11
Irritability
100
12
Dyspnea
ALCA, mild MR, NHC
109
LVO - left ventricular overload; RVO - right ventricular overload; RAO - right atrial overload; LAO - left atrial overload; LASDB - left anterior superior division block; RBBCA - right bundle branch conduction abnormalities; ALCA - anomalous origin of the left coronary artery; MR - mitral regurgitation; DCM - dilated cardiomyopathy; FS - fractional shortening; NHC - normal heart chambers; SPS - supravalvar pulmonary stenosis; SG - systolic gradient; LCA - left coronary artery.
The origin of the left coronary artery from the pulmonary artery was visualized during surgery. In six cases (50%), the left coronary artery originated from the left Valsalva sinus; in two cases from the right sinus; and in four cases from the posterior sinus. Two intraoperative deaths (16%) occurred (cases 1 and 4). The mean intensive care unit stay was 14.4 2.8 days. The clinical events that extended this stay were: infection (4 patients), diaphragmatic palsy (2 patients), myocardial ischemia (2 cases), chorea (2 cases), and low cardiac output syndrome (1 case). Six patients are being followed up in our service and one by the cardiologist in the city from which he had been referred. One patient died (case 9) in the late postoperative period, from non-cardiac death (pneumonia). The control test results showed improvement. On chest
radiography, the cardiac silhouette returned to normal and there were no signs of pulmonary congestion in all patients. A significant improvement of the preoperative ischemic alterations was observed on the electrocardiogram (Table 1). The echocardiogram showed return of the cardiac function to normal and patency of the left coronary artery in all patients assessed (Figure 2). Mitral regurgitation was resolved in most cases. Three patients developed supravalvar pulmonary stenosis (cases 2, 8 and 11) (Figure 3), as diagnosed on Doppler echocardiogram. Surgical correction was necessary in two cases (8 and 11), with supravalvar pulmonary peak systolic gradients of 72 mmHg and 127 mmHg. After pulmonary arterioplasty, these patients maintained a residual systolic gradient of 40 and 27 mmHg, respectively. The third case
169
Arq Bras Cardiol 2008; 90(3) : 167-171
Lenzi et al Analysis of the Takeuchi Procedure in Hospital from Curitiba
Original Article
of this heart disease have been found, focusing on the surgical techniques and their outcomes. Our case series with correction using the Takeuchi procedure is one of the largest in the literature reviewed3. ALCA is found as an isolated anomaly in most of the cases, but in 2 to 21% it may be associated with other cardiac malformations, mainly atrial septal defect, coarctation of the aorta, and ventricular septal defect4-7. In our study, only three patients presented other cardiac malformations (PDA, ostium secundum ASD, and pulmonary artery sling). The origin of the left coronary was predominantly from the left sinus, thus corroborating the literature8-10. Studies show that, in addition to Valsalva sinuses, the coronary artery may also originate from the pulmonary branches11. The predominance of patients with heart failure in this series results mainly from the prevalence of infants, which is the age range where this manifestation is more common. This presentation was also found in other studies such as Vouh et al8, in which 45% of the cases with heart failure were infants under 7 months of age; in Bunton et al5 study, in which 62% were infants with a mean age of 3 months; and Laks et al12 with 42% of the cases under 6 months of age. The electrocardiogram is of key importance in the diagnosis of anomalous origin of the left coronary artery, where the presence of a Q wave in the D1 and aVL leads suggests the diagnostic hypothesis of this heart disease. Amaral et al13 found a Q wave in aVL in 91% of the patients; Bunton et al5 in 95% of the cases; and Isomatsu et al14 in 82%. In the present study, this rate was 83% of the patients. Currently, the elective test for diagnostic confirmation is the echocardiogram; however, in our sample, eight patients underwent cardiac catheterization because diagnostic confirmation, investigation of associated lesions, study of collateral circulation and of the anatomic position of the left coronary artery were required. The Takeuchi procedure3 is used in some specific situations such as anomalous origin of the left coronary artery from the anterior or left Valsalva sinus, or in older patients, due to the development of collaterals around the sinuses, thus hindering the displacement of the main coronary artery. In our service, the Takeuchi procedure has been frequently used because the surgeons are familiar with it.
Fig. 3 - In this angiographic image of the pulmonary artery, the arrow shows supravalvar pulmonary stenosis, a complication of the Takeuchi procedure.
Fig. 2 - Aortogram showing patent left coronary artery after surgery.
of supravalvar pulmonary stenosis is being followed up; the respective systolic gradient did not increase in the past few months, and no surgical intervention was required.
Discussion
Anomalous origin of the left coronary artery from the pulmonary artery is an uncommon anomaly and cause of heart failure in infants. It was first described in 1886 by a pathologist, in a publication of two cases of ALCA1. In 1993, it was published under the name of Bland-WhiteGarland Syndrome 2,3. Since then, several descriptions
The mortality rate in this series was 16%, similar to that found in other health centers, where it ranges from 0 to 27%4,6,7,15,16. The late complications described are: aortic regurgitation, tunnel obstruction, and supravalvar pulmonary stenosis. In our study, three patients developed supravalvar stenosis, and two required surgical reintervention. This is the most frequent complication, and its incidence ranges from 18 to 60%3,4,5,10,13. The need for surgical reintervention is of approximately 12% to 42%. Surgical correction of mitral regurgitation performed in one of our patients is not routinely recommended in the index surgical procedure, because it may increase the surgical risk. Additionally, repair of ALCA provides improvement of the left ventricular function and size by improving ischemia; consequently, regression of mitral regurgitation occurs17.
Arq Bras Cardiol 2008; 90(3) : 167-171
170
Lenzi et al Analysis of the Takeuchi Procedure in Hospital from Curitiba
Original Article
Conclusion
Anomalous origin of the left coronary artery from the pulmonary artery should be suspected in infants presenting with heart failure, and its diagnosis may be made using noninvasive methods such as echocardiogram. The Takeuchi procedure is a surgical technique with good immediate outcome. Postoperative mortality is usually due to the cardiac dysfunction of dilated cardiomyopathy. During the follow-up of these patients, an improvement of symptoms, of the signs of myocardial ischemia on electrocardiogram, and of the cardiac function on echocardiogram can be observed. Mitral regurgitation following surgical correction resolves thanks to the improved left ventricular myocardial perfusion, thus mitral repair is not required. Late morbidity depends on the development of supravalvar pulmonary stenosis. This not so uncommon complication ultimately implies a repeat surgical intervention to alleviate obstruction, thus affecting the patients quality of life.
References
1. Freedom RM. Anomalous left coronary artery from the pulmonary artery: the natural and modified history of congenital heart disease. Australia: Blackwell Publishing; 2004. p 82-90. 2. Dodge-Khatami A, Mavroudis C, Backer C. Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy. Ann Thorac Surg. 2002; 74 : 946-55. 3. Takeuchi S, Imamura H, Katsumoto K, Hayashi I, Katohgi T, Yozu R, et al. New surgical method for repair of anomalous left coronary from pulmonary artery. J Thorac Cardiovasc Surg. 1979; 78 (1): 7-11. 4. Schwartz M, Jonas R, Colan S. Anomalous origin of left coronary artery from pulmonary artery: recovery of left ventricular function after dual coronary repair. J Am Coll Cardiol. 1997; 30: 547-53. 5. Bunton R, Jonas R, Lang P , Castaneda A. Anomalous origin of left coronary artery from pulmonary artery: ligation versus stablishment of a two coronary artery system. J Thorac Cardiovasc Surg. 1987; 93: 103-8. 6. Lambert V, Touchot A, Serraf A, Henglein D, Planche C. Midterm results after surgical repair of the anomalous origin of the coronary artery. Circulation. 1996; 94 (Suppl II): II-38-II-43. 7. Sauer U, Stern H, Meisner H, Sebening F. Risk factors for perioperative mortality in children with anomalous origin of left coronary artery from pulmonary artery. J Thorac Cardiovasc Surg. 1992; 104: 696-705. 8. Vouh PR, Tamisier D, Sidi D, Vernant F, Mauriat P , Povard P , et al. Anomalous left coronary artery from the pulmonary artery: results of isolated aortic reimplantation. Ann Thorac Surg. 1992; 54: 621-7. 9. Turley K, Szarnicki RJ, Flachsbart KD, Richter RC, Popper RW, Tarnoff H. Aortic implantation is possible in all cases of anomalous origin of left coronary artery from pulmonary artery. Ann Thorac Surg. 1995; 60: 84-9. 10. Alexi-Meskishvili V, Hetzer H, Weng Y, Lange PE, Berger F, Loebe M. Anomalous origin of left coronary artery from pulmonary artery: early results with direct aortic reimplantation. J Thorac Cardiovasc Surg. 1994; 108: 354-62. 11. Atik E, Barbero-Macial M, Ikari NM, Ebaid M, Jatene A . Origin of left coronary artery from right and left pulmonary arteries--clinical, anatomico surgical and follow-up evaluation of 3 cases. Arq Bras Cardiol. 1991; 57 (2): 121-7. 12. Laks H, Ardehali A, Grant PW, Allada V. Aortic implantation of anomalous left coronary artery. J Thorac Cardiovasc Surg. 1995; 109: 519-23. 13. Amaral F, Carvalho JS, Granzotti JA, Shinebourne EA. Anomalous origin of left coronary artery from pulmonary artery: profile practices medicine and results medium term of the surgical treatment. Arq Bras Cardiol. 1999; 72: 307-13. 14. Isomatsu Y, Imai Y, Shin oka T, Aoki M, Iwata Y. Surgical intervention for anomalous origin of left coronary artery from pulmonary artery: the Tokyo Experience. J Thorac Cardiovasc Surg. 2001; 121: 792-7. 15. Guikahue MK, Sidi D, Kachaner J, Cohen P , Vouhe P , Neveux JY. Anomalous left coronary artery arising from the pulmonary artery in infancy: is early operation better? Br Heart J. 1988; 60: 522-6. 16. Berdjis F, Takahashi M, Wells W, Stiles Q, Lindesmith GG. Anomalous origin of left coronary artery from pulmonary artery: significance of intercoronary collaterals. J Thorac Cardiovasc Surg. 1994; 108: 17-20. 17. Michielon G, DiCarlo D, Toscano A, Di Donato RM. Anomalous coronary artery origin from the pulmonary artery: correlation between surgical timing and left ventricular function recovery. Ann Thorac Surg. 2003; 76: 581-8.
171
Arq Bras Cardiol 2008; 90(3) : 167-171
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- ECG Made Easy For Allied Health ProfessionalsДокумент47 страницECG Made Easy For Allied Health ProfessionalsDr GowrishankarPotturi PT100% (3)
- 062 Pathology MCQ Respiratory SystemДокумент4 страницы062 Pathology MCQ Respiratory Systemمجتبى علي100% (13)
- Physiotherapy in Cardiopulmonary Conditions MCQ PDFДокумент2 страницыPhysiotherapy in Cardiopulmonary Conditions MCQ PDFDrGyanaranjan Pradhan PT60% (5)
- Pediatric Cardiovascular DisordersДокумент9 страницPediatric Cardiovascular Disorderscayla mae carlos0% (1)
- Aomi 2018Документ64 страницыAomi 2018Simona IonitaОценок пока нет
- Terapia Anticoagulanta in Tromboza Venoasa Profunda - Ghidurile ACCP 2012Документ78 страницTerapia Anticoagulanta in Tromboza Venoasa Profunda - Ghidurile ACCP 2012Ana-Maria RamazanОценок пока нет
- Diabetic Foot Brochure - VasaprostanДокумент15 страницDiabetic Foot Brochure - VasaprostanAna-Maria RamazanОценок пока нет
- ILVOДокумент2 страницыILVOAna-Maria RamazanОценок пока нет
- Respiratory NotesДокумент2 страницыRespiratory NotesLidy CastilloОценок пока нет
- Pneumothorax: - Hitesh Rohit (3 Year B.P.T.)Документ22 страницыPneumothorax: - Hitesh Rohit (3 Year B.P.T.)Hitesh RohitОценок пока нет
- Thoracic IncisionsДокумент10 страницThoracic IncisionsRadioputro WicaksonoОценок пока нет
- Defek Septum Atrium: PJB Asianotik Shunt Dari Atrium Kiri Ke KananДокумент10 страницDefek Septum Atrium: PJB Asianotik Shunt Dari Atrium Kiri Ke KananFrida Neila RahmatikaОценок пока нет
- Aortic ValveДокумент8 страницAortic ValveIfeanyichukwu OgbonnayaОценок пока нет
- PJB Pada Dewasa AASДокумент54 страницыPJB Pada Dewasa AAS1e23e2ewОценок пока нет
- Ecg Basics - NAVEENДокумент65 страницEcg Basics - NAVEENNaveen MathieuОценок пока нет
- Chapter 022Документ32 страницыChapter 022Nur SusiawantyОценок пока нет
- CVS - Embrology and AnatomyДокумент28 страницCVS - Embrology and AnatomyThe Medical PostОценок пока нет
- Heart Dissection Lab Report GuideДокумент6 страницHeart Dissection Lab Report Guideelorenzana0511100% (1)
- 5 EkgДокумент6 страниц5 EkgJessica BОценок пока нет
- Ross Wilson AnatomyДокумент1 страницаRoss Wilson AnatomyGeorgie Stephen100% (2)
- Class 7 Holiday Homework-MergedДокумент29 страницClass 7 Holiday Homework-MergedidkОценок пока нет
- An Anatomical Review of The Right VentricleДокумент6 страницAn Anatomical Review of The Right VentricleAracely Escarleth Aguirre de la CruzОценок пока нет
- DCRV PPT NowДокумент22 страницыDCRV PPT NowKarthik RamanОценок пока нет
- Human Heart: Anatomy, Function & FactsДокумент2 страницыHuman Heart: Anatomy, Function & FactsFlorie Fe Rosario OrtegaОценок пока нет
- Cardiovascular System DevelopmentДокумент63 страницыCardiovascular System DevelopmentAdan Iman100% (1)
- Vagus Nerve Cranial Nerve X OverviewДокумент6 страницVagus Nerve Cranial Nerve X OverviewdimiОценок пока нет
- ICRJ-Validation of Cornell Product As A Method of Assessing Left Ventricular HypertrophyДокумент5 страницICRJ-Validation of Cornell Product As A Method of Assessing Left Ventricular Hypertrophysamir raflaОценок пока нет
- Dr. Naitik Trivedi & Dr. Upama Trivedi: Cardiovascular SystemДокумент20 страницDr. Naitik Trivedi & Dr. Upama Trivedi: Cardiovascular SystemAhmed ImranОценок пока нет
- Apical Four Chamber Echocardiogram ViewДокумент6 страницApical Four Chamber Echocardiogram ViewMaria EdelОценок пока нет
- Autopsy of Heart External ExaminationДокумент20 страницAutopsy of Heart External ExaminationchinnnababuОценок пока нет
- CT Shows Diffuse Fatty Thickening of Interatrial SeptumДокумент13 страницCT Shows Diffuse Fatty Thickening of Interatrial SeptumHaluk AlibazogluОценок пока нет
- Intrinsic Conduction System ExplainedДокумент5 страницIntrinsic Conduction System ExplainedUta Provinsiana SukmaraОценок пока нет
- The Heart Shadow in The MediatinumДокумент7 страницThe Heart Shadow in The MediatinumRolando Reyna100% (1)
- Ventricular Septal Defects: Embryology and Imaging FindingsДокумент7 страницVentricular Septal Defects: Embryology and Imaging FindingsYosephus GorisОценок пока нет