Академический Документы
Профессиональный Документы
Культура Документы
Hepatitis B
Загружено:
Lance Overdosed JarielОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hepatitis B
Загружено:
Lance Overdosed JarielАвторское право:
Доступные форматы
21 Jesse Lance Jariel 22 Hannah Lorraine Lim
Hepatitis B
I.
Definition
Hepatitis B, also known as serum hepatitis, is the inflammation of the liver caused by Hepatitis B Virus (HBV), a double stranded deoxyribonucleic acid (DNA). It can lead to acute hepatitis, chronic hepatitis, progression of chronic hepatitis to cirrhosis, fulminant hepatitis with massive hepatic necrosis, and the carrier state, and also participates in the development of hepatitis D (delta hepatitis). The virus is found to have infected humans, monkeys, and chimpanzees. In humans, it has been found in kidneys, spleen, pancreas, skin, bone marrow, RBC, and liver (greatest affinity). Hepatitis B has 2 stages, acute and chronic hepatitis. Acute hepatitis may be asymptomatic. No specific treatment is required and the majority of adult-acquired infection resolves within 2 months of the onset of jaundice (if symptom occur). HBsAg seroconversion (conversion of HBsAg to anti-HBs) indicates resolution of infection. The person is now non-infectious and most cases will have life-long immunity to HBV infection. Chronic hepatitis, however, has 4 phases: Immune tolerance phase, immune clearance phase, inactive carrier state, and reactivation of replication. Immune tolerance phase is characterized by HBeAg positivity with high levels of HBV DNA and normal serum ALT. It has very low chances of liver damage. In immune clearance phase, there is a determined attack on infected hepatocytes. HBeAg seroconversion is also observed which produces bursts of increased inflammatory activity but without a sustained decline in HBV DNA levels (hepatic flares peaks in ALT levels). The inactive carrier state which is HBeAg negative, is characterized by low levels of HBV DNA and normal ALT. For some patients, this phase will continue indefinitely but some are for reactivation of replication where HBeAg is still negative. The HBV DNA levels fluctuate but frequently exceed 100 000 coipes/mL. In the United States, about 1.5 million people are infected with the hepatitis B virus. However, worldwide, about 400 million people have the virus, with most of these people living in Asia. Clearly, this is a significant public health and medical problem. II.
Description of the Causative Agent
A. PHYSICAL
HBV is a member of the Hepadnaviridae family. The mature HBV virion isa 42-nm, spherical double layered Dane Particle. It is comprised of a nucleocapsid core protein (hepatitis B CORE antigen/ HBcAg), enclosed by a surface lipoprotein which contains hepatitis B SURFACE antigen/ HBsAg. The core contains the HBV DNA (partially double stranded) and DNA polymerase. Its genome contains four major viral genes namely: Core gene encodes HBcAg which is important for viral packaging and production of HBeAg. Surface gene encodes three surface proteins (Pre-S1, pre-S2, and S) Large HBsAg contains Pre-S1, Pre-S2, and S Middle HBsAg contains Pre-S2 and S Small HBsAg contains S only
X gene encodes X protein which has trasnactivating properties making it important for hepatocarcinogenesis. Polymerase gene codes for enzyme essential to the replicative cycle.
B. LIFE CYCLE Viral replication starts after attachment and entry of the HBV into the hepatocyte. The viral genome is then transported to the nucleus where relaxed circular form of the HBV DNA is converted into covalently closed circular DNA (cccDNA) which serves as the template for transcription, and includes the formation of pregenomic and subgenomic RNA (both act as mRNA). The pregenomic RNA serves as the template for reverse transcription, it is incorporated together with viral polymerase into the maturing nucleocapsid and is used for minus-strand DNA synthesis (which in turn is used for plus-strand DNA synth). The core particles formed are enveloped with surface proteins in the ER and are released from the cells. The hepatocytes infected with HBV also release non-infectious particles. Some of the non-enveloped nucleocaspids recirculate from the cytoplasm to the nucleus to serve as additional templates for transcription. The important aspect of HBV infection is the ability of the viral DNA to be integrated into the host cell genome. III.
Virulence Factors
The key virulence factor in hepatitis B is the overproduction of the hepatitis B surface antigen (HbsAg). These antigens form aggregates that are noninfectious because they are not related to the viral RNA. Since HBV can hide the surface antigen from the immune system, the excess HbsAg may act as a decoy binding to the specific HBV antibodies, therefore limiting the number of antibodies that could bind to the infective HBV virion. Another virulence factor is the tropism of HBV for liver cells. The virus attaches itself to the hepato-specific receptors and obstructs the hepatocyte specific transcription factors within the cell. Once the body recognize various HBV-derived peptides on the surface of the hepatocytes, the immune system makes specialized cells called cytotoxic T lymphocytes (CTLs) or killer T-cells, which attacks the infected cells by invading the virus. In this process, it is inevitable that some of the healthy liver cells may also be attacked, thereby causing liver damage.
IV.
Transmission
Hepatitis B virus can be transmitted through: 1. The use of HBV contaminated instruments during acupuncture, ear piercing, tattooing, and manicure. 2. Sharing of drug needles, shaving, sexual activities, and transfusion of contaminate blood. 3. Continuous personal contact (such as in home, or where there is saliva involved) 4. Sexual contact with an infected person 5. Having multiple sex partners 6. During pregnancy (from the mother to her infant)
V.
Signs and Symptoms
The clinical features of HBV are similar to those of other hepatitis viruses and range from asymptomatic infection to jaundice following a flulike prodromal illness. However, persons with HBV infections are more likely to develop serum sickness like illness (arthritis, arthralgia, uticarial rash), and chronic infection is associated with glomerulonephritis or vasculitis resembling periarteries nodosa. Some signs and symptoms include: 1. Jaundice (yellowish coloration of the eyes and the skin) 2. Fatigue (excessive tiredness) 3. Appetite loss 4. Nausea and Vomiting 5. Itching all over the body 6. Dark urine (color of cola or tea) 7. Pale-colored stools (grayish or clay colored) 8. Headache, fever and flu 9. Pain over the location of the liver (on the right side of the abdomen, under the lower rib cage) 10. Hepatomegaly 11. Anorexia VI.
Diagnostic Tests
A. Serological Assays 1. HBsAg - Hepatitis B Surface Antigen - first serological marker to appear - high levels in acute and chronic infection (active Hepa B infection) - indicates ongoing infection 2. Anti-HBs - Anti-hepatitis B surface antibody - Indicates recovery from past infection and immunity to HBV, or passive antibody from HBIG, or immune response from HBV vaccine 3. Anti-HBc (IgG) - Anti-hepatitis B core antibody (IgG) - Indicates current or resolved HBV infection 4. Anti-HBc (IgM) - Anti-hepatitis B core antibody (IgM) - Acute HBV infection or flare or chronic HBV 5. HBeAg - Hepatitis B e Antigen - marker of the core antigen - Active viral replication 6. Anti-HBe - Anti-hepatitis B e antibody - May indicate immune control but acute viral replication may still occur 7. HBV DNA - Hepatitis B DNA - Direct measurement of viral particles: range 1-10 log IU/mL
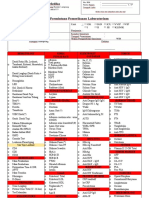
B. PNR tests -detect and measure the amount of HBV DNA, called the viral load, in clinical specimens C. CT scan or ultrasound - These diagnostic imaging tests are used to detect the extent of liver damage and may also detect cancer of the liver caused by chronic hepatitis B. D. Liver biopsy This involves removal of a tiny piece of the liver. It is usually done by inserting a long needle into the liver and withdrawing the tissue. The tissue is examined under a microscope to detect changes in the liver. A liver biopsy is often recommended for patients with intermittent or persistent elevation in ALT levels, but is not mandatory. Histologic evaluation of liver biopsy specimens is a more sensitive and accurate indicator of liver disease than ALT levels. It may be useful to establish the baseline status of liver histology at initial evaluation prior to initiation of therapy and to exclude other causes of liver disease. However, liver biopsy is not always used as part of the diagnostic evaluation and is resisted by some patients due to its invasive nature SCREENING FOR HBV INTERPRETATION OF SEROLOGIC TEST RESULTS FOR DIAGNOSIS OF HBV INFECTION HBSAG + + Total ANTI-HBC + + + IGM ANTI-HBC + + ANTI-HBS + Interpretation Susceptible; never infected Early acute infection Acute Infection Acute Resolving Infection Past infection; recovered and immune Chronic Infection False positive (susceptible); past infection; low level chronic infection; passive transfer to infant born to HBV infected mother Immune is titer >= 10 mIU/mLg
+ -
+ +
VII.
Period of Communicability
Period of infectivity depends upon the presence of HBsAg. The period of infectivity is during the positivity of HBsAg until its negativity.
VIII.
Incubation period
HBV has an incubation period of 4-26 weeks. It remains in the blood until and during active episodes of acute and chronic hepatitis.
IX.
Outcome and Prognosis
A. Acute Infection - Hospitalization rates range from 25-35% with a higher rate among older patients. - Case fatality rates are generally <2%. - Co-infection with hepatitis D may result in a more severe clinical course of acute hepatitis B. B. Chronic Infection age of infection is inversely correlated with the risk of chronic infection. the risk of developing chronic infection is 90% among newborns infected perinatally, 50% for children infected at 1 year of age, 20% for children infected at 1 to 4 years of age, and 5-7% for older children and adults. patients with chronic hepatitis B are susceptible to superinfection with hepatitis D virus, which increases the risks of development of cirrhosis and of mortality.
X.
Complications
Complications of Hepatitis B include: Cirrhosis Primary HCC (Hepatocellular carcinoma) Fulminant hepatitis Liver fibrosis Some extrahepatic manifestations include: glomerular nehpritis serum sickness arthralgias arthritis skin rashes: uritcaria and papular acrodermatitis (Gianotti-Crosti)
XI.
Treatment
Treatment aims to suppress viral replication and to reduce inflammation.It is required to prevent fibrosis progression and the development of cirrhosis. There are 2 groups of drugs for the treatment of HBV infection: Alfa-interferons - augment the host immune system response to HBV infection - interferon alfa-2b, interferon alfa-2a, and pegylated interferon alfa 2a/PEG-IFN - higher rate of HBeAg seroconversion - expensive, significant side effects, and unacceptable for prolonged treatment Nucleo(t)ide analogues (NAs) - Interrupt the process of viral replication - Lamivudine, Adefovir, Tenofovir, and Entecavir
- For longer duration of treatment - HBeAg seroconversion is improved by prolonged treatment - Fewer reported cases of side effects - Risk of development of drug-resistant virus There are several factors to consider before beginning HBV infection treatment, including amount of fibrosis, degree of inflammatory activity, and the predicted risk of future liver damage. XII.
Prevention and Control Measures
A. Preexposure prophylaxis For those who are at risk of HBV infection, 3 IM (deltoid) injections of hepatitis B vaccine (Recombivax-HB by Merck or Engerix-B by GSK) are recommended at 0, 1, and 6 months. B. Postexposure prophylaxis For those unvaccinated persons sustaining an exposure to HBV, combination of HBIG and hepatitis B vaccine is recommended, they may be given at the same time but at different sites. 1. Perinatal exposure of infants A single dose of 0.5 mL HBIG should be administered in the thigh immediately after birth followed by complete course of three injections of recombinan hepatitis B vaccine to be started within the first 12 h of life. 2. For those experiencing direct percutaneous inoculation or transmucosal exposure to HBsAg positive blood/body fluid A single IM 0.06 mL/kg dose of HBIG should be administered as soon after exposure and followed by complete course of hepatitis B vaccine to begin with the first week. 3. For those exposed to sexual contact A single IM 0.06 mL/kg dose of HBIG should be administered within 14 days of exposure followed by complete course of hepatitis B vaccine C. Control Measures Immunization Education of high risk groups Promotion of acceptance of vaccination schemes Screening of blood products to reduce blood supply system that contains HBV Used needles especially ones used on infected persons, shall be disposed immediately to prevent repetition of usage. Personal hygiene must be observed and prevent using other peoples personal stuff that could be infected with the virus. Healthcare workers must follow the standard precautions especially wearing gloves if handling blood. Handling needles and sharps should also be followed to prevent viral contamination. As much as possible, prevent having sexual contact with an infected person. Practice safe sex
Notes: Virulence factors: HBsAg hepatitis B surface antigen (for protection)
HBcAg hepatits B core antigen (holds the nucleus of infected hepatocyte) HBeAg hepatitis B e Antigen (for replication, reproductivity, infectivity)
Seroconversion- conversion of antigen to antibody Liver biopsy- most specific test to detect liver damage (for example liver fibrosis). Result of liver test: increase in AST (aspartate aminotransferase) presence of Hepa B virus only. Increase in ALT (alanine aminotransferase)- presence of liver damage. Drug of choice: Lamivudine Signs and symptoms: same with other hepatitis If HBsAg (-), active vaccine (+), passive vaccine If anti-HB is < 10 IU/ml , give another dose (vaccine) Vaccine- 3 doses: 0, 1, and 6 months
Вам также может понравиться
- Friction Forces on a Banana BoxДокумент4 страницыFriction Forces on a Banana BoxLance Overdosed JarielОценок пока нет
- AДокумент4 страницыALance Overdosed JarielОценок пока нет
- HAHAHAHAДокумент2 страницыHAHAHAHALance Overdosed JarielОценок пока нет
- HAHAHAHAДокумент2 страницыHAHAHAHALance Overdosed JarielОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Pautas de Pruebas y Manejo de Retrovirus Felino AAFP 2020Документ26 страницPautas de Pruebas y Manejo de Retrovirus Felino AAFP 2020Leandro FerreyraОценок пока нет
- Tuberculosis BasicsДокумент95 страницTuberculosis Basicstummalapalli venkateswara rao100% (1)
- Lesson Plan With COMPREHENSIVE SEXUALITY EDUCATIONДокумент15 страницLesson Plan With COMPREHENSIVE SEXUALITY EDUCATIONHanna Banana100% (1)
- Mcqs Inflammatory Bowel DiseaseДокумент2 страницыMcqs Inflammatory Bowel Diseaseiwennie100% (1)
- Common Childhood Diseases and Healthy HabitsДокумент6 страницCommon Childhood Diseases and Healthy HabitsHF ManigbasОценок пока нет
- Pediatric Vaccine Àd Vaccination PDFДокумент257 страницPediatric Vaccine Àd Vaccination PDFntnquynhpro100% (1)
- Acinetobacter Ursingii Masquerading As Gram-Positive CocciДокумент2 страницыAcinetobacter Ursingii Masquerading As Gram-Positive CocciMiguel CarlosОценок пока нет
- Acute Flaccid ParalysisДокумент37 страницAcute Flaccid ParalysisBold Ronald OjanОценок пока нет
- Barangay Monthly Inventory of Vaccinated PopulationДокумент2 страницыBarangay Monthly Inventory of Vaccinated PopulationGenzo TaniaОценок пока нет
- MCS +: Multicomponent Collection SystemДокумент18 страницMCS +: Multicomponent Collection SystemRamiro LozaОценок пока нет
- Topic Presentation Henoch-Schonlein Purpura (HSP) : Name: Sweta Jaanvhi Raj S160258 DATE: 16/09/2020Документ26 страницTopic Presentation Henoch-Schonlein Purpura (HSP) : Name: Sweta Jaanvhi Raj S160258 DATE: 16/09/2020Alusio Navosailagi VUNIIVIОценок пока нет
- Ringworm (Tinea Capitis)Документ15 страницRingworm (Tinea Capitis)farmasi_hmОценок пока нет
- RockerДокумент2 страницыRockerwan hseОценок пока нет
- Vermikompos and Gliocladium Effectiveness Against Fusarium WiltДокумент8 страницVermikompos and Gliocladium Effectiveness Against Fusarium WiltJioWongMenengОценок пока нет
- Biology 9th Solving A Biological ProblemДокумент5 страницBiology 9th Solving A Biological Problemmhussainshigri786Оценок пока нет
- IMNCI - 6th SemДокумент32 страницыIMNCI - 6th SemAbhishek AgrawalОценок пока нет
- AMENDMENT DIRECTIVE TO CONTROL COVID 19 PANDEMIC No 933 2022 EthiopiaДокумент3 страницыAMENDMENT DIRECTIVE TO CONTROL COVID 19 PANDEMIC No 933 2022 EthiopiaAhmed AdemОценок пока нет
- Swapan Kumar Nath Sanjay G Revankar Problem-Based PDFДокумент1 163 страницыSwapan Kumar Nath Sanjay G Revankar Problem-Based PDFRestu100% (1)
- Journal Reading Survey OphtalmologyДокумент17 страницJournal Reading Survey OphtalmologynadyajondriОценок пока нет
- Blood Type Test ExperimentДокумент8 страницBlood Type Test ExperimentUpz PhaОценок пока нет
- Vaccine Adverse Reaction Reporting System by Vaccine and MaufacturerДокумент1 191 страницаVaccine Adverse Reaction Reporting System by Vaccine and MaufacturerGuy RazerОценок пока нет
- Form Lab RSBM NewДокумент2 страницыForm Lab RSBM NewKiki OlivianaОценок пока нет
- English Essay Topics on COVID-19 PandemicДокумент4 страницыEnglish Essay Topics on COVID-19 Pandemicmaria evangelistaОценок пока нет
- Hairy Leukoplakia As An Early OralДокумент4 страницыHairy Leukoplakia As An Early OralJessicaLisaNugrohoОценок пока нет
- Laporan Harian Diagnosa 21022022-012015Документ20 страницLaporan Harian Diagnosa 21022022-012015puskesmas sukanegaraОценок пока нет
- By: Alex B. Olivar JR., RN CHN Study Bullets Drug of Choice Disease Drug of ChoiceДокумент5 страницBy: Alex B. Olivar JR., RN CHN Study Bullets Drug of Choice Disease Drug of ChoiceAlexОценок пока нет
- Treatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionДокумент24 страницыTreatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionMuhammad Farras Razin PerdanaОценок пока нет
- White Blood Cells: The Immune System's DefendersДокумент1 страницаWhite Blood Cells: The Immune System's DefendersSulochana ChanОценок пока нет
- Pathogen Research AssignmentДокумент2 страницыPathogen Research AssignmentDeven BaliОценок пока нет
- Hiv and Aids NotesДокумент4 страницыHiv and Aids NotesEllen WolffОценок пока нет