Академический Документы
Профессиональный Документы
Культура Документы
How The Circadian Rhythm Affects Sleep, Wakefulness, and Overall Health
Загружено:
Rosemarie Fritsch100%(1)100% нашли этот документ полезным (1 голос)
238 просмотров62 страницыCircadian rhythm entrains an organism's functions to the environmental cycle of light and dark. Light has different effects on the circadian rhythm depending on when we are exposed to it. Circadian rhythm can be altered by a number of factors, especially stress.
Исходное описание:
Оригинальное название
How the Circadian Rhythm Affects Sleep, Wakefulness, And Overall Health
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документCircadian rhythm entrains an organism's functions to the environmental cycle of light and dark. Light has different effects on the circadian rhythm depending on when we are exposed to it. Circadian rhythm can be altered by a number of factors, especially stress.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
238 просмотров62 страницыHow The Circadian Rhythm Affects Sleep, Wakefulness, and Overall Health
Загружено:
Rosemarie FritschCircadian rhythm entrains an organism's functions to the environmental cycle of light and dark. Light has different effects on the circadian rhythm depending on when we are exposed to it. Circadian rhythm can be altered by a number of factors, especially stress.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 62
The Circadian
Rhythm and its
disorders
PROF. DRA. ROSEMARIE FRITSCH
MATERIAL DOCENTE
ANDREW D. KRYSTAL, MD, MS
How the Circadian Rhythm
Affects Sleep, Wakefulness,
and Overall Health
1
Properties of the Circadian
Rhythm
The field of circadian rhythm research was launched
in the early 18th century (AV 1).
1
The circadian rhythm
entrains an organisms functions to the environmental
cycle of light and dark. This rhythm is seen in nearly all
species and plays an important role in synchronizing
organ systems to optimal phase relationships with each
other. Variations in many biological processes occur
over roughly a 24-hour period (AV 2).
This type of endogenous rhythmicity is also seen in
many other biological measures. For example, levels of
plasma melatonin increase in the evening and early
part of the night, while levels of plasma cortisol
increase over the course of the night, peak at waking,
and diminish throughout the day.
2
Our innate circadian rhythm can be modified by a
number of factors, especially light. For example, when
you travel to a new time zone, your body is on a
different schedule from the new environment, because
it continues to function for some time on the circadian
rhythm you developed in your previous location. The
longer you stay in the new environment, the more your
body aligns with its new environmental clock. This
process is driven by cues, especially exposure to light,
which tells us when it is day or night.
2
Light has different effects on the circadian rhythm
depending on when we are exposed to it.
1
Thus, if we
are exposed to light late during the night, this shifts
our rhythm so that we tend to go to bed and wake up
earlier. If we are exposed to light in the early part of the
night, this shifts our rhythm so that we tend to stay up
and sleep later. Exposure to light during the period
when we are usually awake has no effect at all.
Other factors that can affect our internal clock include
when we eat, our activity level, and caffeine intake.
3,4
Thus we often have gastrointestinal upsets in a new
time zone because we are eating when our body does
not expect to eat (ie, our digestive hormones are out of
synch with our meal time).
5
Our innate circadian
rhythm also affects how our autonomic nervous system
and our brain function.
6
3
2
Anatomy of the Circadian
Rhythm
The important role of the suprachiasmatic nucleus
(SCN) in regulating periodic behavior
7
has been
confirmed by a number of findings in animal studies
(AV 3).
1. When the SCN is lesioned, circadian
rhythmicity goes away because the SCN is no longer
able to stimulate the production of melatonin and
other substances that modulate the sleep-wake
pattern.
8
2. If cells are removed from the SCN and grown
in vitro, they continue to show self-sustaining circadian
rhythmicity.
9
3. If the SCN is transplanted from one animal to
another, the recipient manifests the circadian rhythm
of the donor, showing that the SCN can entrain
biological activity and drive a circadian process on its
own.
10
4
3
Genetics of the Circadian
Rhythm
Although researchers had been able to breed for
changes such as different eye or hair color for a long
time, it was not until the 1960s that Benzer first
demonstrated that behavior could be modified
genetically by breeding circadian behavioral patterns
into fruit flies.
11
This demonstrated that the chemical
clock in the SCN is under genetic control. A relatively
small number of genes and proteins regulate this
biological clock. The critical components of this genetic
system are the Period, Clock, and Cryptochrome (Cry)
genes, and these can be manipulated to alter the
circadian cycle.
12
The role of genetic factors in our circadian rhythm is
supported by the observation that preferred
sleep/wake schedules (eg, being a night owl or a
morning lark) tend to run in families. The tendency to
go to bed and get up very early (sleep phase advance),
is linked to a mutation in the human Period-2 (hPer2)
gene that is an autosomal dominant trait.
13
The
tendency to stay up late and sleep late (sleep phase
delay) is associated with several genes, including the
human Period-3 (hPer3) gene.
14
In humans, the circadian rhythm is controlled by
several core genes that operate via a series of feedback
loops (Figure 1). A transcriptiontranslation
negative-feedback loop powers the system, with a delay
between the transcription of these genes and the
negative feedback being a key factor that allows the
system to oscillate.
5
4
Effects on Sleep/Wake
Function
The SCN regulates our sleeping and waking through its
effect on 3 brain regions
7
:
! Ventrolateral preoptic area: releases "-
aminobutyric acid (GABA) and promotes sleep
! Lateral hypothalamic area: releases the
transmitter hypocretin/orexin that promotes
wakefulness
! Paraventricular hypothalamus: involved
in the release of melatonin
The interaction shown in the sleep/wake model
15
produces a consolidated period of wakefulness, driven
by the circadian rhythm, and a consolidated period of
sleep that occurs when the homeostatic drive to sleep
has built up and the wake-promoting systems have
shut down (AV 4).
16
The circadian rhythm system
enables us to stay awake for extended periods, despite
a growing homeostatic drive for sleep. It does this by
modulating the release of neurotransmitters, in
particular hypocretin/orexin, that maintain
wakefulness. Otherwise, we would have great difficulty
functioning, since we would fall asleep as soon as a
great enough drive to sleep had built. This is what
happens in narcolepsy, which involves abnormalities in
the hypocretin/orexin system.
17
6
7
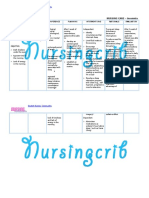
Process S represents
the homeostatic
built-up of sleep
pressure
Process C represents
the circadian rhythm
When the distance
between process S and
process C is largest,
sleep propensity will
be highest.
Borblys model of sleep-wake regulation (Borbly & Achermann, 1999).
Here you can see how sleep pressure keeps building up due to sleep deprivation, but since the circadian rhythm
keeps fluctuating by its regular 24 hour cycle, our sleep propensity will also fluctuate with this rhythm. In addition
this picture also shows that such sleep deprivation will lead to a higher slow wave activity (SWA, representing
deeper stages of sleep) during the recovery sleep. This type of activity is used as a marker for the homeostatic
process. When we for example go to bed earlier when homeostatic sleep pressure hasnt built up that much, this will
translate into less slow wave activity. Even within a sleep cycle itself you can see this phenomenon, with less
slow-wave activity during the second part of the sleep.
8
5
Problems in Sleep/Wake
Function
Problems can occur when the drive for wakefulness
and the drive for sleep are not correctly synchronized.
Thus, if you try to sleep when your body doesnt
normally sleep, you will sleep less and you will not
sleep as well because your circadian processes are
fighting the sleep drive. Individuals with circadian
rhythm sleep disorders often experience at least partial
sleep loss on a long-term basis. This is because they are
trying to sleep at an unfavorable time for extended
periods. Even modest prolonged sleep deprivation can
produce 4 types of serious physiological
abnormalities
18-23
:
! Metabolic dysfunction (increased appetite,
metabolism, or oxygen consumption; sympathetic
nervous system activation; decreased cerebral glucose
utilization in certain subcortical structures)
! Neuroendocrine abnormalities (low
thyroid-stimulating hormone; decreased levels of
growth hormone, prolactin, or leptin)
! Decreased resistance to infectious
disease
! Oxidative stress
9
Humans who experience prolonged sleep deprivation
also demonstrate higher rates of obesity and type 2
diabetes and neurobehavioral impairment, including a
shortening of voluntary and involuntary sleep latency
resulting in daytime sleepiness, microsleeps (intrusion
of sleep into wakefulness), and errors of omission and
commission on cognitive testing.
24,25
10
6
Role of the Circadian
Rhythm in Health and
Disease
By synchronizing the bodys biological clocks, the SCN
has extensive influence on peripheral tissues through
the autonomic nervous system.
26
For example, glucose
is released in a gradual, oscillating, sinusoidal-like
pattern over a 24-hour period. If animals are fed at
times other than their natural feeding times, the
original cycle continues. However, if you cut out the
SCN, glucose release becomes entrained to feeding
times and is no longer linked to other physiologic
processes related to eating and digestion.
27
Phase dyssynchrony occurs when the rhythms of
organs are out of synch with the SCN. Research in
animals and humans has shown that such disruptions
can have negative effects on health. For example, one
study found that disrupting the normal circadian
rhythmicity of hamsters with cardiomyopathy reduced
their median life span by 11%.
28
In the next chapter, Dr
Roth will discuss the types of negative effects that can
occur in humans who experience such phase
dyssynchrony, as occurs when someone has Shift Work
Disorder.
11
The circadian rhythm, a self-sustained
rhythm of biological processes observed
in nearly all species, is determined by
both genetic and behavioral factors. It
plays an important role in coordinating
and modulating sleep/wake function and
in many other biological processes.
Disturbances of the circadian rhythm
cause misalignment among biological
and behavioral processes that can lead to
disturbances in sleep/wake function and
other types of impaired functioning and
may affect our capacity to fight off
disease.
xii
Summary
Comprobar
respuesta
Pregunta 1 de 4
The circadian rhythm is
A. The determinant of cicada
lifecycles
B. A self-sustained rhythm of
biological processes observed in
nearly all species
C. Another name for jet lag
THOMAS ROTH, PHD
Shift Work Disorder:
Overview and Diagnosis
1
Circadian Rhythm Sleep
Disorders
According to the second edition of the American
Academy of Sleep Medicines International
Classification of Sleep Disorders (ICSD-2),
1
the major
feature of circadian rhythm sleep disorders is a
misalignment between the patients sleep pattern and
the sleep pattern that is desired or regarded as the
societal norm (AV 1).
14
In addition to shift work disorder (SWD), the
ICSD-2 lists 8 other types of circadian rhythm sleep
disorders, including time zone change (jet lag)
syndrome and delayed and advanced sleep phase
syndromes. Many people have experienced jet lag
syndrome, caused by a lack of synchrony between your
internal clock and a new time zone in which you are
trying to function. Circadian rhythm disturbances can
also involve delayed or advanced sleep phases
(AV 2).
15
Because delayed and advanced sleep phase syndromes
often cause the person to be out of synchrony with the
prevailing sleep/wake patterns of society, they can lead
to significant morbidity. Recent studies
2-5
have found
that, when high school classes were started an hour or
two later, the number of car accidents decreased and
academic functioning improved. Problems can also
arise when there is chronic dyssynchrony between the
persons internal clock and external light and dark (ie,
when a person is required to stay awake and work
when it is dark and sleep when it is light), which can, in
some cases, lead to SWD.
16
2
Shift Work
It is important to distinguish between shift work and
SWD. Shift work is a job description. The vast majority
of people who work shifts adjust and do well. However,
a subgroup of people have great difficulty adjusting
their internal clocks and develop SWD due to a
mismatch between the sleep/wake schedule required
by their jobs and their own circadian sleep/wake
cycles.
Prevalence. It is estimated that 15%26% of the US
labor force works night, evening, or rotating shifts (AV
3).
6,7
Effects of shift work on the sleep/wake cycle.
Shift work affects the sleep/wake cycle in a number of
ways. No matter how many hours you have slept
during the day, trying to work during the downside of
the circadian rhythm (eg, between 12 AM and 6 AM) is
very difficult unless you can shift your internal clock.
Studies have found that, over a 24-hour cycle, both
subjective alertness and cognitive functioning decline
17
between 2 AM and 4 AM.8 Also, because you are not
sleeping at night, the homeostatic pressure to sleep is
not relieved, producing an ever-increasing pressure to
sleep.
9
However, only a subset of individuals who work
night or rotating shifts develop SWD, because
circadian rhythms are modulated not only by light and
dark, but also by other factors such as clock genes,
melatonin, and environmental cues (eg, noise).
10,11
18
3
Shift Work Disorder: An
Overview
Prevalence.
Drake et al12 found that 28% of those who work night
or rotating shifts, compared with 18% of day workers,
experienced insomnia and/or excessive sleepiness, and
they estimated the true prevalence of SWD to be
approximately 10% of those who work night or rotating
shifts. A study of 103 shift workers on a North Sea oil
rig (working 2 weeks on 7 nights/7 days, 12-hour shifts,
4 weeks off) by Waage et al13 found a relatively high
prevalence of SWD. They reported that 24 (23.3%) of
the shift workers were suffering from SWD and that,
during their 4-week period off work, the workers with
SWD reported significantly poorer sleep quality, more
subjective health complaints, and greater problems in
coping than individuals who did not have SWD. Shift
workers without SWD reported results similar to those
of day workers on the rig with regard to sleep,
sleepiness, subjective health complaints, and coping.
Diagnosis.
The ICSD-2 diagnostic criteria for circadian rhythm
sleep disorder, shift work type, are shown in (AV 4).
The differential diagnosis of SWD includes excessive
sleepiness due to obstructive sleep apnea, narcolepsy,
restless legs syndrome, and chronic insufficient sleep
due to daytime conflicts (eg, child care, environmental
factors, moonlighting at a second job). Comorbid
conditions (eg, increased prevalence of sleep apnea in
shift workers) can complicate the diagnosis of SWD.
Clinicians should also rule out comorbid disorders that
can cause insomnia and excessive sleepiness (eg,
primary insomnia, insomnia associated with
psychiatric disorders such as major depression), as
well as consider whether the person may be taking
medications or abusing drugs or alcohol to help with
sleep, which may be causing impairment at work.
19
20
4
Consequences of Shift
Work Disorder
Just as animal studies have found that disruptions in
circadian rhythm can affect health outcomes, studies in
humans have produced similar findings.
Gastrointestinal problems (eg, ulcers, functional
bowel disorders) are significantly increased in
individuals who work night or rotating shifts. However,
the increased prevalence of ulcers is associated not just
with shift work, but also with SWD. In a study
comparing 360 workers on rotating shifts, 174 on night
shifts, and 2,036 on day shifts, Drake et al12 found
that, among those who reported excessive sleepiness
and/or insomnia, the prevalence of ulcers was higher
among rotating shift workers (12.5%) and night shift
workers (15.4%) than day workers (6%). This effect was
not seen to any marked degree in those who worked
rotating or night shifts but did not have excessive
sleepiness and/or insomnia. Zhen Lu et al14 found that
the prevalence of functional bowel disorders was
higher in a sample of nurses who worked rotating
shifts (38%) than in those who worked day shifts (20%)
and that functional bowel disorder symptoms were
positively correlated with level of sleep disturbance.
Cancer. Shift work (whether or not the person has
SWD) has been found to be a risk factor for cancer.
Increased odds ratios for breast cancer have been
found in large samples of women who worked night
shifts, particularly with increasing duration of
nighttime employment.15-19 A study20 of 14,052
working men in Japan also found a significantly
increased risk of prostate cancer in those who worked
rotating shifts. The World Health Organization
International Agency for Research on Cancer has
concluded, Shift work that involves circadian
dysruption is probably carcinogenic to humans.21
Depression. The prevalence of depression is
significantly higher in those who work rotating and
night shifts than in day workers. In addition, while
insomnia or daytime sleepiness is a risk factor for
depression for all individuals, it is a much greater risk
factor for rotating or night shift workers.12
21
Cardiovascular effects. While insomnia is a risk
factor for hypertension in all individuals, it is a
significantly higher risk factor for shift workers with
insomnia.12 In contrast, although shift work is
associated with a significantly increased risk of heart
disease compared with nonshift work, this increased
risk is not associated with SWD.12
Excessive sleepiness and accidents. Insomnia is
associated with excessive sleepiness, which can impair
functioning, in rotating shift workers compared with
day workers.12 Studies have found a 12% frequency of
drowsy driving and an increased risk of driving
accidents related to sleepiness in rotating shift workers
with SWD compared with those without the disorder.
Relative risk of injuries and accidents increases with
each successive night shift worked.22 The effects of
shift work on patient and employee safety are an
important consideration in the health care field, where
many workers have extended shifts.23
Productivity. Similarly, it is the combination of night
or rotating shift work and daytime sleepiness or
insomnia that decreases productivity, not each factor
alone.12 Rotating shift workers with insomnia and/or
excessive sleepiness (SWD) missed significantly more
days of work (an average of 3 days per month over 3
months, a 10% decrease in productivity) than day
workers with these symptoms, who missed
approximately half a day of work per month over the
3-month period. This effect was not seen in shift
workers who did not have insomnia or excessive
sleepiness: they also missed a half day or less of work
over 3 months.12 Rotating shift workers who
experience both insomnia and excessive sleepiness are
at the greatest risk for lost productivity. (See Keller23
for a review of potential productivity problems in
health care workers on extended shifts.)
22
Shift work is very prevalent in our
society. However, only a subset of shift
workers meet criteria for SWD and need
treatment. Potential targets for treatment
are (1) the persons work schedule, (2)
difficulty sleeping during the day, and,
most important, given the accident data
discussed above, (3) difficulty
functioning because of excessive
sleepiness (eg, commuting home safely).
xxiii
Summary
Comprobar
respuesta
Pregunta 1 de 4
The Shift work disorder (SWD) is a
disruption of sleep patterns affecting
A. All people who work night or
rotating shifts
B. Primarily workers in natural
resources, con struction, and
maintenance occupations, such as
farmers, fishermen, and
construction workers
C. Approximately 10% of all shift
workers
D. Shift workers with hypertension
or cardiovascular disease
RICHARD D. SIMON, JR, MD
Shift Work Disorder:
Clinical Assessment and
Treatment Strategies
1
Identifying Circadian
Rhythm Disturbances
The most important clue that a patient may have a
circadian rhythm sleep disorder is an irregular
sleep/wake schedule. It is not possible for people to
change their circadian rhythm by more than 24 hours
in any given day.1,2 Thus, if a persons sleep/wake
schedule varies by more than 24 hours between days
on and off work, this suggests that he or she may have
circadian rhythm problems. One of the best ways to
identify such problems is to ask, Do you have
difficulty falling asleep at bedtime (insomnia) and
difficulty waking up when you need or want to
(hypersomnia)? If the patient says yes, this can
indicate a delayed sleep phase syndrome (ie, the
person may be a night owl). Individuals with this
sleep pattern often overuse the snooze button, hitting it
repeatedly. This pattern is frequently seen in teenagers.
People may also fall asleep very early, say at 8:00 PM
(hypersomnia), and wake up long before they want to
(eg, 3:00 AM). This sleep pattern reflects an advanced
sleep phase syndrome, a pattern frequently seen in the
elderly (AV 1).
25
2
Taking a Sleep History
The first step in assessing for shift work disorder
(SWD) is to take a thorough sleep history. The most
important item to ask about is the persons schedule of
work and sleep. Ask the person how his or her
sleep/wake schedule differs on work days, days off, and
vacation days. (The persons sleep schedule when on
vacation can give particularly helpful clues to the
persons intrinsic sleep/wake schedule.) (AV 2)
Assess the quality of sleep and wakefulness by asking
questions such as these:
! Do you sleep all night? Do you feel refreshed
in the morning? Or do you have fragmented sleep?
! Do you find it easy to stay alert throughout
the day? Or do you find yourself getting fatigued and
sleepy?
! Do you snore? Has anyone you live with
witnessed any episodes when your breathing appeared
to stop and then start again while you were asleep
(sleep apnea)?
Restless legs syndrome, characterized by an
uncomfortable, creeping, crawling, restless feeling in
the legs, can make it very difficult to fall asleep. If the
person reports snoring or witnessed episodes of apnea,
abnormal nocturnal behaviors (eg, injuring self or
others by acting out dreams), or symptoms suggesting
narcolepsy, a sleep study is required. It is also
important to ask about use of drugs or medications to
help with sleep or alertness (eg, caffeine in the
daytime, pills or alcohol to promote sleep) and the
quality and safety of the sleeping and waking
environments. A medical and psychiatric history is
necessary to identify conditions that might be
contributing to the sleep problems (eg, respiratory
problems, pain, depression, anxiety).
26
27
3
Assessment Tools
The simplest and most important assessment tool for
day-to-day clinical use by primary care physicians and
general psychiatrists is a sleep diary (AV 3).
Several easy-to-use scales are also commonly used in
sleep assessments. The Stanford Sleepiness Scale
3
and
the Epworth Sleepiness Scale
4
measure level of
excessive sleepiness. The Epworth Sleepiness Scale
asks the person to rate the likelihood of dozing in 8
different situations on a 4-point scale (0 = would never
doze to 3 = high chance of dozing), with a score of 10 or
greater suggesting the need for further evaluation. The
Insomnia Severity Index
5
assesses severity of current
sleep problems and their effect on daytime functioning.
Scales such as these are particularly useful for tracking
the effectiveness of an intervention over time.
In some situations, depression or anxiety scales or a
general outcome scale such as the Short-Form 36-Item
Health Survey, Version 2,
6
may be useful.
Actigraphy, which uses a device worn on the wrist to
record motion (ie, suggesting the person is awake) is
not generally necessary in assessing for SWD, since an
accurate history and a sleep diary will usually supply
all necessary information. Referral for overnight sleep
studies or polysomnography is also not indicated to
diagnose SWD, but is indicated if one suspects the
patient may have obstructive sleep apnea, parasomnias
leading to injurious nocturnal behaviors during sleep,
or narcolepsy. If narcolepsy is suspected in a shift
worker, it is usually necessary to have the worker
discontinue shift work for 24 weeks, because shift
work itself and the associated circadian misalignment
can confuse testing for narcolepsy. Narcolepsy is
suggested by a history of excessive sleepiness that often
started when the person was a teenager and predates
his or her shift work.
28
29
4
Differential Diagnosis and
Comorbid Conditions
Conditions that frequently occur in conjunction with
SWD include obstructive sleep apnea and restless
legs syndrome. Signs suggesting sleep apnea include
large neck size, crowded oropharynx, and reports of
witnessed apneas. Poor sleep habits of shift workers
can also cause them to develop learned insomnia
behaviors, referred to as psychophysiologic insomnia.
Other comorbid conditions include depressive
and/or anxiety disorders and chronic fatigue,
which can be difficult to distinguish in a person with
chronic circadian dyssynchrony.
30
5
Treatment Goals
The primary goal of treatment for SWD is to reduce the
degree of circadian misalignment by fostering better
sleep when it is desired and improved alertness and
functioning when appropriate. Other goals are to
identify and appropriately treat any intrinsic sleep
disorders (eg, apnea) and any medical or psychiatric
disorders that are present. Nonpharmacologic
strategies should be tried before considering use of
medications to promote sleep and/or alertness.
Zeitgebers: Strategies for
Shifting the Biological
Clock
The term zeitgeber (German for time giver) describes
an external cue that helps synchronize a plant or
animals internal clock to the earths 24-hour
light/dark cycle.
7
The most powerful zeitgebers in
humans are light, supplemental melatonin, dark, and
exercise.
Very bright light has powerful effects,
1,2
with
individuals being most sensitive to the effects of light
approximately 2 hours before or 12 hours after their
spontaneous wake time. If a pulse of very bright light is
given 24 hours before a persons spontaneous wake
time (eg, 3:00 AM for someone with a usual wake time
of 6:00 AM), the person is likely to wake up 24 hours
later (ie, to move toward a delayed sleep phase,
becoming more of a night owl). On the other hand, if
you expose the person to very bright light at the
spontaneous wake time or in the hour or so after, the
person is likely to wake up 24 hours earlier (ie, to
move toward an advanced sleep phase, becoming more
of a morning lark).
31
Melatonin acts in the opposite way.
1,2
When
administered in the evening, it tends to make the
person fall asleep and wake up earlier (ie, to advance
the sleep phase). When administered in the morning, it
tends to make the person stay up later and wake up
later (ie, to delay the sleep phase).
Dark also has powerful effects on sleep phase.
1,2
Thus,
naps in a darkened environment act in much the same
way as melatonin. Greatly limiting exposure to light in
the evening will help you go to sleep earlier.
Conversely, absence of light in the morning will help
you sleep later. Because primarily the shorter
wavelengths (eg, blue light) lead to phase shifts, one
strategy for exposing the biological clock to dark is to
wear dark or blue-blocking sunglasses.
Similar phase response curves have been found for
exercise.
1,2
Exercising in the early evening tends to
phase-advance you and make you more of a morning
person. Exercising after midnight generally does the
opposite. However, exercise is not often used to adjust
sleep phase in humans (AV 4).
32
6
Practical Strategies for
Sleep Problems Associated
With Shift Work
To minimize problems associated with shift work,
workers should have as predictable a work schedule as
possible. It is also helpful if employers provide
sufficient breaks at work, allow shift workers to take a
short nap at work, avoid schedules that involve
working multiple days in a row, and provide sufficient
time off between work days. These strategies are
important because the vast majority of shift workers do
not fully entrain (ie, their biological clocks never fully
synchronize with their required work and sleep
schedules). It is also useful to try to limit commuting
time and overtime.
Another key strategy is to minimize circadian
misalignment between work days and days off, which
involves educating and enlisting the support of
significant others in the shift workers family and
immediate social circle. For most shift workers, this
means producing a phase delay in their biological
clocks (ie, to make them more night owls). This is
done by changing the persons environment so that he
or she gets as much light as possible during the
scheduled day and as little light as possible during
the scheduled night and by minimizing the difference
in sleep/wake patterns between work days and days
off. Practically, this means having bright light at work,
wearing dark glasses during the drive home when one
is likely to be exposed to light, and keeping the
bedroom, bathroom, and other rooms that will be used
at home as dark as possible during the desired sleep
period.
Shift workers who achieve complete or even partial
entrainment (ie, their biological clocks become
realigned with a new sleep/wake schedule) show
marked improvements in psychomotor vigilance,
memory, reaction time, night work performance, and
mood and reductions in fatigue, excessive sleepiness,
and mental exhaustion compared with those who do
not
8,9
(AV 5).
33
34
SWD needs to be considered in all
patients who have a sleep/wake schedule
that differs by more than 24 hours on
work days compared with days off and
who exhibit symptoms of sleepiness at
work and difficulty sleeping during the
desired sleep time. Asking about snoring
and restless legs symptoms can lead to
comorbid diagnoses that, if treated, can
improve the shift workers sleep.
xxxv
Summary
Comprobar
respuesta
Pregunta 1 de 4
The most important clue that a patient may
have a circadian rhythm sleep disorder is:
A. Complaint of restless legs
syndrome
B. An irregular sleep/wake schedule
C. Depression
D. Sleep apne
4
Cases
1
The young man with
difficulty falling asleep
A 24-year-old male patient reports difficulty falling
asleep, followed by daytime sleepiness, a pattern that
has persisted for about 5 years since his days as a
student. His excessive sleepiness has become more
severe during the past year due to the 8 AM starting
time for his work shift. He recently needed to take 2
personal days off from work due to inability to report
on time. Once asleep, he does not have difficulty
staying asleep. His bedtime ranges from 11:30 PM to
1:00 AM, with time required to fall asleep averaging 2
hours. His wake time is scheduled for 6:45 AM on
workdays. Weekday mornings are particularly difficult.
The patient feels "out of it" until about noon. He has
fallen asleep while driving to work and has had several
near-miss traffic accidents the past month.
The patient is being treated with sertraline 50 mg for
depression, which was first diagnosed 2 years ago, and
with zolpidem 10 mg as needed for insomnia. He
suffers from exercise-induced asthma. His blood
pressure is stable at 130/80 mm Hg, and he has a body
mass index (BMI) of 26. His mother and brother both
suffer from similar types of insomnia symptoms.
Physical and neurological exams were normal. He had
a score of 12 on an ESS questionnaire.
37
Comprobar
respuesta
Which of the following additional assessments
would you next employ for this patient?
A. Polysomnogram
B. Actigraphy
C. Sleep diary
D. Multiple sleep latency test
Like the ESS, a sleep diary is a first-line diagnostic tool
for suspected sleep disorders because of its ease of
administration and low cost. A sleep diary will plot the
patient's sleep pattern and is suitable as the next test in
this case. Actigraphy may be used but is not
commonly available in primary care practices.
Polysomnograms and multiple sleep latency tests are
more elaborate diagnostic methods reserved for
validation of initial screening tests, or to evaluate for
other sleep disorders, such as OSA and narcolepsy.
Circadian rhythm sleep disorders are disorders of sleep
and wake timing. Thus, an essential aspect of
diagnosing and treating circadian rhythm sleep
disorders is to determine whether symptoms are due to
chronic or short-term misalignment of the patient's
circadian rhythms with external 24-hour cues, or due
to other etiologies. A sleep diary is an easily
administered diagnostic tool that can be easily used in
a primary care setting to determine if the patient's
internal circadian sleep and wake rhythm is misaligned
with work or social schedules.
The pathophysiology of circadian rhythm sleep
disorders is multifactorial, only partially understood.
What is of importance to clinicians is that they
consider the full range of physiological, behavioral, and
environmental factors involved in a clinical sleep
disorder when developing treatment strategies. In the
case of Circadian rhythm sleep disorders, their etiology
can be intrinsic due to endogenous factors, or extrinsic
due to factors in the environment.
ASSESSMENT
The patient completed a 7-day sleep diary during his
normal work week (see the Figure). The diary confirms
a bedtime of 10:30-11:45 PM on workdays and a
prolonged time to fall asleep of over 2 hours. On
weekends, bedtimes are later (midnight to 1 AM), but it
still takes 1-2 hours to fall asleep. Note that on
38
Saturday, he sleeps in until 11 AM, and on Thursday, he
took a nap in the afternoon between 3 to 4 PM.
Average sleep duration is less than 6 hours on
weekdays. The patient went on vacation for a 10-day
period shortly after his initial visit, providing an
opportunity for actigraphy monitoring during his
preferred sleep schedule. Actigraphy showed an
average bedtime of 3-4 AM and an average wake time
of 10 AM to noon while on vacation. After returning
from vacation, the patient said he had been able to
catch up on his sleep and feels much better. However,
after returning to work, he reports that his bedtime
insomnia has returned, often preventing him from
falling asleep before 2 AM.
39
Comprobar
respuesta
Pregunta 1 de 2
Based on the previous description, what is
the most suitable diagnosis for the patient
in case 1?
A. Psychophysiologic (conditioned)
insomnia
B. Insomnia due to depression
C. Advanced sleep-phase disorder
D. Delayed sleep-phase disorder
The patient's symptoms are consistent with delayed
sleep-phase disorder, namely a stable pattern of delay
in the nighttime sleep period until the early morning
hours followed by inability to wake up until the late
morning. In contrast, patients with insomnia disorder,
including psychophysiologic insomnia or insomnia
associated with depression, do not typically show a
stable pattern of delayed sleep and when allowed to
sleep at a later time have normal sleep duration.
Advanced sleep-phase disorder is characterized by
early sleep onset and premature awakening, the
opposite of delayed sleep-phase disorder.
Treatment should be aimed at advancing the timing of
sleep and wake cycle. Morning bright light exposure
(close to natural awakening) signals the circadian clock
to advance its timing. Similarly, low-dose melatonin
given in the late afternoon or early evening signals the
clock to advance. (Melatonin is not approved by the
FDA for the treatment of circadian rhythm sleep
disorder.) One should avoid bright light exposure in
the evening because it will delay or shift circadian
rhythms. An advance in the timing of circadian
rhythms (advance shift) will result in earlier sleep
onset and awakening, which is needed to synchronize
with the desired sleep/wake and work schedule. In
addition, bright light in the morning can have an
alerting effect, which can facilitate waking.
Pharmacologic therapies such as hypnotic agents or
antidepressants to treat symptoms of insomnia without
resetting the circadian clock will only partially address
symptoms, rather than the underlying cause of the
symptoms.
40
DIAGNOSIS
The patient's history confirms that his ability to
perform on the job is impaired by his excessive
sleepiness and lack of energy and alertness in the work
place. He thinks that his occasional feelings of
depression and anxiety are associated with poor sleep.
Although he is concerned about poor performance
associated with his sleep pattern, he does not feel
anxious overall. "I'm just never sleepy at 10:30 at
night," he says. He is diagnosed with delayed
sleep-phase disorder. According to the International
Classification of Diseases, 10th Revision (ICD-10),
diagnostic billing codes for Circadian rhythm sleep
disorders start with G47.2, with delayed sleep-phase
disorder G47.21.
41
Episodic and
paroxysmal
disorders G40-
G47
Sleep
disorders G47
Circadian
rhythm sleep
disorder G47.2
delayed sleep
phase type
G47.21
INITIAL TREATMENT
The patient was instructed to purchase a bright light
box, readily available on the Internet, and sit in front of
the light source (1-2 feet away) for 1 hour in the
morning, starting at 10:30 AM on a weekend day (off
work). Light box exposure was then advanced by 1 hour
each morning until he started treatment at his normal
workday wake up time of 6:30 AM. He was also
instructed to take melatonin 1 mg at 8 PM for the next
3 weeks.
Recognizing the pattern of the patient's sleep-wake
cycle is the key to both the diagnosis and treatment of
circadian rhythm sleep disorders. The goal of circadian
rhythm sleep disorder is to synchronize (entrain) the
sleep-wake cycle with the appropriate external physical
environment and work schedule. Treating symptoms of
insomnia or excessive sleepiness without resetting the
circadian rhythm sleep disorder patient's circadian
clock will only partially address the symptoms, rather
than the underlying cause of the symptoms. Thus, the
principal goal of therapy for the delayed sleep-phase
disorder patient (as illustrated in case 1) is to advance
the timing of circadian rhythms. Conversely, the goal of
therapy for an advanced sleep-phase disorder patient
would be to delay the timing of circadian rhythms.
42
Comprobar
respuesta
What is the principal goal in managing the
sleep disorder for this case?
A. Advance the timing of the patient's
circadian rhythms
B. Increase the duration of sleep
C. Provide treatment with the use of
prescription drugs
D. Avoid sleeping so late on weekends
FOLLOW-UP
The patient reported good compliance with nightly
MLT treatment but could tolerate morning light
therapy for only 30-40 minutes on some days. He
reports a bedtime of 11 PM, falling asleep by midnight
on most days. He is able to awaken with the aid of an
alarm clock at 6:30 AM on workdays, but feels like he
could sleep longer. He wakes up naturally at 8-10 AM
on weekends.
43
2
The old man with a history
of difficulty staying asleep
PRESENTATION AND PATIENT HISTORY
A 66-year-old man has a history of difficulty staying
asleep. This has caused him to be a habitual early riser
around 5 AM virtually every day for about 10 years. His
difficulty in staying asleep has become progressively
worse. His typical sleep pattern is to fall asleep on the
couch by 7 PM, wake up 90 minutes to 2 hours later,
and then go to bed around 9:30-10 PM. He usually
sleeps until 3-4 AM or until he goes to the bathroom,
after which he has difficulty going back to sleep. He
often lays awake in bed for up to 2 hours until he rises
at 5-5:30 AM. By the afternoon and early evening, he is
excessively sleepy and struggles not to fall asleep. He
reports that his ES has affected his social life and
relationship with his wife due to his drowsiness. He
says his ideal sleep schedule would be to fall asleep
about 10 PM and wake at 5-6 AM. His score on an ESS
questionnaire is 12.
He has a history of hypertension and hyperlipidemia,
for which he is treated with olmesartan and
atorvastatin. The patient has a paternal family history
of early risers. His wife has informed him that he
snores lightly but has not witnessed any breathing
irregularities during his sleep. He has no restless legs
symptoms and is not depressive, but he is frustrated by
his sleep problem. He has reflux symptoms when he
eats late. His physical examination, cognition, and
mental health status are normal.
44
Comprobar
respuesta
What is the most likely diagnosis for the patient
in this case?
A. Advanced sleep-phase disorder
B. Delayed sleep-phase disorder
C. Irregular sleep-wake pattern
D. Insomnia due to nocturia
The patient's symptoms are consistent with advanced
sleep-phase disorder, a stable pattern of sleep onset
several hours earlier than the usual nighttime sleep
period and sleep offset several hours before the normal
or desired wake time. Advanced sleep-phase disorder is
more common in older adults. Nighttime urination
typically occurs in men of the patient's age but is not
the primary cause of an advanced sleep-wake cycle or
daytime sleepiness in this case.
Schematic of typical sleep phase vs 4 circadian rhythm
sleep disorders. A feature of ASPD, DSPD, and
non-24-hour sleep pattern is that the sleep architecture
and total amount of sleep are comparable to the
normal pattern, but timing of sleep does not conform
to a conventional 24-hour schedule.
45
46
47
ASSESSMENT
The patient returns 3 weeks later and provides a 7-day
sleep diary (Figure). The diary shows that he lays
awake for 1-2 hours before getting out of bed at 5-5:30
in the morning. The premature wake times are
preceded by involuntary drowsiness and napping in the
early evening from 5:30-8 PM. His symptoms support
a diagnosis of Advanced sleep-phase disorder.
48
Comprobar
respuesta
Which treatment is most appropriate for
this patient?
A. An antidepressant
B. A stimulant
C. Melatonin
D. Light therapy
Timed light exposure for 1-2 hours in the evening (7-9
PM) is indicated as standard first-line therapy to delay
onset of the sleep cycle in cases of advanced
sleep-phase disorder. In addition, the patient is
counseled on sleep hygiene and told to avoid naps
before a targeted bedtime of 10:30 PM. Physical
activity such as walking before or after dinner is
recommended to maintain wakefulness during the
evening. Low-dose Melatonin taken in the morning
may be useful but may induce residual sleepiness. The
patient does not suffer from mood disorders, so
antidepressant medication is not indicated. Stimulants
have a limited role in treating advanced sleep-phase
disorder. Caffeine taken in moderation is acceptable
for maintaining wakefulness but is not considered a
primary therapy for advanced sleep-phase disorder.
The wake-promoting agents modafinil and armodafinil
are approved for short-term use in treating excessive
sleepiness associated with sleep apnea, narcolepsy, and
shift-work disorder, but not advanced sleep-phase
disorder.
49
Actigraphy
Consiste en un pequeo aparato que se coloca en la mueca del individuo y
registra sus movimientos a lo largo de la noche. Los datos obtenidos se
analizan mediante un sistema computarizado que permite acumular datos
hasta un mximo de 22 das consecutivos, y estimar diversos parmetros del
sueo (Hauri & Wisbey, 1992). Contrariamente a la polisomnografa, la
actigrafa de mueca no es un instrumento costoso ni intrusivo y su
utilizacin es sencilla. Permite registrar periodos de 24 horas y proporciona
informacin del ritmo circadiano. No obstante, slo mide vigilia y sueo y no
estadios especficos de sueo.
Trminos del glosario relacionados
ndice
Captulo 4 - The young man with difficulty falling asleep
Arrastrar trminos relacionados aqu
Buscar trmino
Chronic fatigue
El Sndrome de Fatiga Crnica (SFC) es una enfermedad grave compleja y debilitante
caracterizada por una fatiga intensa, fsica y mental, que no remite, de forma
significativa, tras el reposo y que empeora con actividad fsica o mental. La aparicin
de la enfermedad obliga a reducir sustancialmente la actividad y esta reduccin de
actividad se produce en todas las Actividades de la Vida Diaria (AVD).
El impacto del SFC en la vida del enfermo es demoledor, tanto por la enfermedad en s
misma como por el aislamiento e incomprensin del entorno, de hecho, las medidas
validadas de calidad de vida, cuando se comparan con otras enfermedades, evidencian
que el SFC es una de las enfermedades que peor calidad de vida lleva aparejada.
Adems de estas caractersticas bsicas, algunos pacientes de Sndrome de Fatiga
Crnica (SFC) padecen diversos sntomas inespecficos, como debilidad muy especial
en las piernas, dolores musculares y articulares, deterioro de la memoria o la
concentracin, intolerancia a los olores, insomnio y una muy lenta recuperacin, de
forma que la fatiga persiste ms de veinticuatro horas despus de un esfuerzo.
Casi siempre la enfermedad es crnica (curaciones inferiores al 5-10%) y de un gran
impacto en la vida del enfermo. De hecho, la mejor medida del impacto de la
enfermedad es evaluar las actividades previas y posteriores a la instauracin de la
enfermedad, tanto en la esfera fsica, como en la intelectual, aunque disponemos de
escalas validadas de Clasificacin de la Severidad e Impacto de la Fatigabilidad
Anormal en un paciente concreto, como por ejemplo la Escala IFR de Fatigabilidad
Anormal.
Trminos del glosario relacionados
ndice
Captulo 3 - Differential Diagnosis and Comorbid Conditions
Arrastrar trminos relacionados aqu
Buscar trmino
Circadian rhythm
Los ritmos biolgicos endgenos pueden ser de diferentes frecuencias [Adn; 1995,
Goldbeter; 2008,Haus; 2009,Ohdo; 2010,Smolensky et al; 2007,Valds-Rodrguez;
2009,Volpato et al; 2005]:
Ritmos de frecuencia alta (con periodos cortos menores a 30 minutos):
- Ritmos con periodos de un milisegundo a 10 segundos de duracin, como el de la
actividad elctrica cortical.
- Ritmos con periodos de segundos de duracin, como el cardaco y respiratorio.
- Ritmos con periodos de 30 segundos a 20 minutos de duracin, como las oscilaciones
bioqumicas.
Ritmos de frecuencia media (con periodos intermedios desde media hora
hasta 6 das de duracin):
- Ritmos ultradianos, ciclos de media hora a 20 horas de duracin, como los ritmos
hormonales, las fases del sueo, la depresin pospandrial o post-lunch.
- Ritmos circadianos o nictamerales, con periodos alrededor de 24 horas de duracin
(24 4 horas), producidos por la rotacin terrestre y que determinan los ciclos del da
y la noche (luz-oscuridad) fundamentales para regular la temperatura corporal, la
secrecin de cortisol y melatonina, el ciclo de vigilia-sueo, etc.
- Ritmos dianos, con periodos de 24 2 horas de duracin.
- Ritmos infradianos, con periodos de 28 horas a 6 das de duracin, como los procesos
metablicos.
Ritmos de frecuencia baja (con periodos largos de ms de 6 das de
duracin):
- Ritmos circaseptanos, con periodos de 7 3 das de duracin, como el del bienestar
subjetivo.
- Ritmos circadiseptanos, con periodos de 14 3 das de duracin.
- Ritmos circavigintanos, con periodos de 21 3 das de duracin.
- Ritmos circatrigintanos o circamensuales, con periodos de unos 30 das de duracin
(30 5 das), definidos por el ciclo lunar de traslacin lunar y que determinan la
alternancia de las mareas y la luminosidad del cielo nocturno.
- Ritmos circanuales o estacionales, con periodos de aproximadamente 1 ao de
duracin (1 ao 2 meses), definidos por el ciclo solar de traslacin terrestre y que
determinan las estaciones del ao, con sus diferencias en intensidad de luz y
temperatura y regulan la reproduccin e hibernacin animal.
- Ritmos de aos de duracin, como en ecologa y epidemiologa.
De todos ellos los ms estudiados son los circadianos y los estacionales.
Trminos del glosario relacionados
ndice
Captulo 1 - Properties of the Circadian Rhythm
Arrastrar trminos relacionados aqu
Buscar trmino
Circadian rhythm sleep disorders
LOS TRASTORNOS DEL SUEO POR ALTERACIN DEL RITMO CIRCADIANO
Ante situaciones extremas para el individuo se pierde la periodicidad circadiana de
aproximadamente 24 horas, (como en el turno laboral nocturno, enfermedades
intercurrentes, etc.). Hay una interrupcin transitoria del funcionamiento del NSQ y
pierde el control de los osciladores perifricos. [Haus;
2009,www.sleepassociation.org]. Es lo que ocurre en los TSRC en los que la
perturbacin del patrn de sueo es consecuencia de la desincronizacin entre el ritmo
de vigilia-sueo deseado (por las circunstancias del entorno del individuo) y su propio
ritmo vigilia-sueo circadiano marcado por el marcapasos interno o reloj biolgico
[Barion et al; 2007,Haus et al; 2006,Lu et al; 2006, Martinez et al; 2010]. Las
repercusiones que tendrn en estas personas (hasta que se adapte su ritmo) sern
alteraciones del sueo (insomnio de conciliacin y mantenimiento y excesiva
somnolencia diurna [Lu et al; 2006]), biolgicas a nivel celular y molecular, cambios
en la actividad cerebral, alteraciones funcionales y del metabolismo de lpidos y
carbohidratos, cambios en la resistencia a la insulina, cambios hormonales-endocrinos
(secrecin de hormona de crecimiento, melatonina, etc.), etc. [Haus et al;
2006,www.sleepassociation.org].
Los TSRC segn la segunda edicin de la Clasificacin Internacional de los Trastornos
del Sueo [Westchester; 2005] de la Academia Americana de Medicina del Sueo
(American Academy of Sleep Medicine o AASM) pueden ser primarios, por mal
funcionamiento del reloj biolgico, (Sndromes del retraso y adelanto de fase, Patrn
irregular del ciclo vigilia-sueo y Sndrome de ciclo vigilia-sueo diferente a 24 horas);
secundarios, en los que son las circunstancias del medio ambiente las que provocan el
desfase del reloj biolgico, (Jet lag, TSRC secundario al trabajo a turnos, TSRC
secundario a enfermedades y al consumo de frmacos u otras sustancias) y otros TSRC
no especificados [Martinez et al; 2010].
Trminos del glosario relacionados
ndice
Captulo 2 - Circadian Rhythm Sleep Disorders
Arrastrar trminos relacionados aqu
Buscar trmino
Delayed or advanced sleep phases
Sndrome de la fase del sueo retrasada. Se caracteriza, como su propio nombre
indica, por un retraso habitualmente mayor de dos horas en los tiempos de
conciliacin del sueo y despertar, en relacin con los horarios convencionales o
socialmente aceptados. Los individuos afectados por esta entidad tienen una prctica
imposibilidad para dormirse y despertarse a una hora razonable, hacindolo ms tarde
de lo habitual. La estructura del sueo es normal, destacando nicamente en los
estudios polisomnogrficos un importante alargamiento de la latencia del sueo o el
tiempo que tardan en dormirse los pacientes. Estos tienen con frecuencia problemas
socio-laborales, ya que sus horas de mayor actividad suelen ser las de la noche. En
estos individuos estn tambin retrasados otros ciclos biolgicos circadianos, como
son el de la temperatura y el de la secrecin de melatonina.
Sndrome de la fase del sueo adelantada. Es menos frecuente que el sndrome
de la fase retrasada. Los periodos de conciliacin del sueo y de despertar son muy
tempranos o precoces con respecto a los horarios normales o deseados. Los sujetos que
padecen este sndrome suelen quejarse de somnolencia durante la tarde y tienen
tendencia a acostarse muy pronto, y se despiertan espontneamente tambin muy
pronto por la maana. Cuando se acuestan muy tarde, por factores exgenos, sufren
un dficit de sueo, ya que su ritmo circadiano les despierta igualmente pronto. No se
conoce su prevalencia, pero se estima en torno al 1% en los adultos y ancianos, y
aumenta con la edad (probablemente porque con la edad se acorta el ritmo
circadiano). Afecta a ambos sexos por igual.
Trminos del glosario relacionados
ndice
Captulo 2 - Circadian Rhythm Sleep Disorders
Arrastrar trminos relacionados aqu
Buscar trmino
Endogenous rhythmicity
La periodicidad circadiana, como la del ritmo vigilia-sueo, est mediada
genticamente, tiene un control y est sincronizada al ciclo regular de 24 horas de
luz-oscuridad ambiental por los osciladores internos, y por ltimo est modulada por
influencias ambientales que permiten su adaptacin a las condiciones variables del
entorno [Adn; 2004,Aschoff; 1967,Chiesa et al; 1999, Haus et al; 2006]:
Trminos del glosario relacionados
ndice
Captulo 1 - Properties of the Circadian Rhythm
Arrastrar trminos relacionados aqu
Buscar trmino
Escala de Somnolencia de Epworth
La Escala de Somnolencia de Epworth (Johns, 1991) estima la somnolencia
subjetiva diurna de individuos adultos. La escala de ocho tems, pide al
individuo que punte de 0 a 3 el grado de somnolencia en diferentes
situaciones cotidianas, diferenciando somnolencia de fatiga. Actualmente,
un puntaje de 10 o ms se considera como el punto de corte ms
apropiado para detectar somnolencia patolgica. La Escala de
Somnolencia de Epworth es sencilla de administrar, es actualmente la
medida subjetiva de somno- lencia diurna ms corrientemente empleada.
Chung (2000) en su estudio encontr que la escala resultaba ser un
instrumento til para diferenciar pacientes con y sin un grado patolgico de
somnolencia objetiva diurna. Tambin Sanford, Lichstein, Durrence, Riedel,
Taylor & Bush (2006) detectaron que los sujetos con insomnio obtienen
puntuaciones ms elevadas en la Escala de Somnolencia de Epworth que los
sujetos sin insomnio, lo que puede ayudar a discriminar sujetos con el
trastorno de aquellos sin el mismo. La escala ha sido traducida al alemn y
espaol y se ha encontrado que su uso no resulta afectado por factores
culturales o de lenguaje (Chung, 2000; Izquierdo-Vicario, Ramos-Platn,
Conesa-Peraleja & Lozano-Parra, 1997).
Trminos del glosario relacionados
ndice
Captulo 4 - The young man with difficulty falling asleep
Captulo 4 - The young man with difficulty falling asleep
Captulo 4 - The old man with a history of difficulty staying asleep
Arrastrar trminos relacionados aqu
Buscar trmino
Genetic control
En las clulas del organismo (en cerebro y tejidos perifricos), el mantenimiento de la
ritmicidad circadiana depende de algunos genes que hay en su ncleo, genes del reloj
o genes circadianos, que componen la maquinaria molecular del reloj circadiano
[Haus; 2009,Hofman et al; 2005]. Se expresan mediados por seales humorales y
neuronales, como la melatonina, que parten de los osciladores internos [Haus et al;
2006,Hofman et al; 2005].
Las lneas de investigacin gentica han tratado de identificar los polimorfismos y
mutaciones que sufren estos genes y se asocian al cronotipo de una persona (medido
por el Cuestionario de matutinidad-vespertinidad de Horne y stberg), determinados
TSRC en algunas familias, adicciones (a drogas y alcohol) y otras enfermedades
(diabetes, enfermedades cardiovasculares, cncer, etc.) [Bechtold et al; 2010,Eismann
et al; 2010,Rosenwasser; 2010,Sack et al; 2007b].
Trminos del glosario relacionados
ndice
Captulo 1 - Genetics of the Circadian Rhythm
Arrastrar trminos relacionados aqu
Buscar trmino
Obstructive sleep apnea
El sndrome de apnea e hipopnea obstructiva del sueo (SAHOS) es una enfermedad
frecuente que afecta al 4% de la poblacin adulta. Su sntoma cardinal es la
somnolencia diurna excesiva que, junto a la alteracin del nimo y deterioro cognitivo,
producen un deterioro progresivo en la calidad de vida de los pacientes. Adems, se ha
asociado a mayor riesgo de hipertensin arterial, morbimortalidad cardiovascular,
accidentes laborales y de trnsito. Esta entidad est ostensiblemente subdiagnosticada,
por lo que es necesario mejorar su conocimiento para aumentar la pesquisa para su
adecuado tratamiento.
Trminos del glosario relacionados
ndice
Captulo 3 - Differential Diagnosis and Comorbid Conditions
Arrastrar trminos relacionados aqu
Buscar trmino
Restless legs syndrome
Corresponde a un trastorno del movimiento caracterizado por la presencia de
sensaciones desagradables localizadas en extremidades inferiores que llevan a la
imperiosa necesidad de moverlas. Esta sensacin empeora con el reposo e interfiere
con el sueo.
La prevalencia de este sndrome es variable segn los estudios y va de 10,6% en USA, y
11,6% en Espaa con una mayor proporcin de mujeres versus hombres de 3:1. La
prevalencia va aumentando con la edad, incluso los primeros sntomas pueden
aparecer en la infancia.
Trminos del glosario relacionados
ndice
Captulo 3 - Differential Diagnosis and Comorbid Conditions
Arrastrar trminos relacionados aqu
Buscar trmino
Shift work disorder
Trastorno del sueo por alteracin del ritmo circadiano (TSRC) de Tipo trabajo a
turnos segn la segunda edicin de la Clasificacin Internacional de los Trastornos del
Sueo (ICSD-2 [Westchester; 2005]) de la Academia Americana de Medicina del
Sueo, o Trastorno del sueo por horarios cambiantes de trabajo.
Este TSRC se produce cuando el horario laboral se solapa con el periodo de sueo
habitual para el trabajador y no consigue adaptar su ritmo biolgico a este horario de
vigilia-sueo que, debido a sus circunstancias laborales, debe seguir [Lu et al; 2006,
Martinez et al; 2010,Waage et al; 2009].
Puede darse en trabajos con guardias nocturnas ocasionales, turnos rotatorios, horario
fijo nocturno y aquellos que empiezan muy temprano por las maanas (antes de las 6
a.m.) [Barion et al; 2007,Sack et al; 2007].
Trminos del glosario relacionados
ndice
Captulo 2 - Circadian Rhythm Sleep Disorders
Arrastrar trminos relacionados aqu
Buscar trmino
Zeitgebers
The four most important time givers:
! The light (and thus the rising hour) controls the melatonin secretion. It is
proven that the exposure to light has an arousing effect and an influence on the sleep
rhythms. Phototherapy has shown its efficiency in a large number of pathologies
(insomnia, depression, fibromyalgia...).
! Physical exercice has a significant influence on the body temperature. The
warmer the organism was during the day, the stronger becomes the action of
melatonin on the fall of body temperature in the evening. Endurance sports (walking,
jogging, swimming, ski...) are traditionally associated with a deeper sleep.(Cf.) On the
opposite, it is not advised to practice an intensive sport less than three hours before
going to sleep.
Be careful, that advice for insomniacs must not lead the sick people to stop all activity
too early in the evening, like some bad sleepers do who "wait for the train of sleep"
from 9 PM on and hope to find sleep in trying not to do anything.
! The meal hours influence the brain through hormones that have been
discovered quite recently like the hypocretin/orexin (which has a common action in
the food intake behaviors and the circuits of sleep).
! Social contacts, love, laughter and pleasure also play a role that is not to
be neglected in the synchronization of the sleep rythms.
These new "somnications" are rarely the subject of specific scientific studies but some
observations suggest their importance.
In 1532, Rabelais already asserted very opportunely that "The cheerful always recover"
The pleasures of life are often associated with a short and efficient sleep whereas
"clinophilia" (the need to lie down), in which the tired subjects seek shelter, prolonges
the sleep duration but diminishes the slow wave activity, thus making the sensation of
tiredness even worse. (Cf. "hypo-sleep syndrome) Besides, it is known that (like in
cases of forced bed rest), the sudden decrease of activity induces sleep disturbances
and functional disorders very quickly.
Trminos del glosario relacionados
ndice
Captulo 3 - Sin ttulo
Arrastrar trminos relacionados aqu
Buscar trmino
Вам также может понравиться
- Biological RhythmsДокумент4 страницыBiological RhythmsMarco Alfieri100% (1)
- On Circadian RhythmsДокумент65 страницOn Circadian RhythmsDipti100% (1)
- Circadian RhythmsДокумент2 страницыCircadian RhythmsOmar SalehОценок пока нет
- Treatment of Circadian Rhythm Sleep Disorders With LightДокумент8 страницTreatment of Circadian Rhythm Sleep Disorders With LightshibutaОценок пока нет
- The Circadian Code Health Assessment PDFДокумент3 страницыThe Circadian Code Health Assessment PDFPablo Padilla MuñozОценок пока нет
- Circadian RhythmsДокумент6 страницCircadian Rhythmshafsa111100% (1)
- Primary Symptoms of Night Eating Syndrome AreДокумент3 страницыPrimary Symptoms of Night Eating Syndrome AreAisa Shane100% (1)
- Circadian Rhythms: Altered States of Awareness What Is An Altered State of Awareness?Документ1 страницаCircadian Rhythms: Altered States of Awareness What Is An Altered State of Awareness?api-461452779Оценок пока нет
- Human Biological ClockДокумент8 страницHuman Biological ClockShehani Liyanage100% (1)
- The Power of A Good SleepДокумент28 страницThe Power of A Good SleepJose PradoОценок пока нет
- Sulforaphane Q & AДокумент7 страницSulforaphane Q & AuL7iMaОценок пока нет
- Book About Cfs Titel Magical-Medicine Source Quelle Www-meactionuk-Org-uk) Magical-medicine-PDF Date 24-February-2010Документ442 страницыBook About Cfs Titel Magical-Medicine Source Quelle Www-meactionuk-Org-uk) Magical-medicine-PDF Date 24-February-2010xmrvОценок пока нет
- Molecular Biology of Circadian Rhythms PDFДокумент286 страницMolecular Biology of Circadian Rhythms PDFSupratik Chakraborty100% (1)
- What Is Functional NeurologyДокумент2 страницыWhat Is Functional NeurologydrtimadamsОценок пока нет
- 0 Tips For Deep, Rejuvenating, Age-Reversing SleepДокумент7 страниц0 Tips For Deep, Rejuvenating, Age-Reversing SleepFlori MarcociОценок пока нет
- SleepДокумент78 страницSleepbiswajitsinha100% (4)
- How The Circadian Rhythm Affects Sleep Wakefulness and Overall HealthДокумент62 страницыHow The Circadian Rhythm Affects Sleep Wakefulness and Overall HealthSlavicaОценок пока нет
- Circadian RhythmДокумент5 страницCircadian Rhythmapi-253459532Оценок пока нет
- Sleep Wake CycleДокумент27 страницSleep Wake CycleNadina TintiucОценок пока нет
- Circadian RhythmsДокумент10 страницCircadian RhythmsJerome Ysrael EОценок пока нет
- The Circadian RhythmsДокумент1 страницаThe Circadian RhythmsUrielОценок пока нет
- Biological Clock Control of Glucose Meta PDFДокумент28 страницBiological Clock Control of Glucose Meta PDFpradeep pОценок пока нет
- Chrono NutritionДокумент8 страницChrono NutritionLoona LuОценок пока нет
- Endo & Exogenous Pacemakersin Biological RhythmsДокумент2 страницыEndo & Exogenous Pacemakersin Biological RhythmsMiss_M90Оценок пока нет
- Biological Clock: Biology Department Birla Public School, Doha-QatarДокумент11 страницBiological Clock: Biology Department Birla Public School, Doha-QatarShreya BalajiОценок пока нет
- How Sleep & Nutrition Interact - Sigma NutritionДокумент16 страницHow Sleep & Nutrition Interact - Sigma NutritionJpwilderОценок пока нет
- Discuss The Role Played by Endogenous Pacemakers and Exogenous Zeitgebers in Biological RhythmsДокумент3 страницыDiscuss The Role Played by Endogenous Pacemakers and Exogenous Zeitgebers in Biological RhythmsiaindownerОценок пока нет
- Review Article: The Impact of Sleep and Circadian Disturbance On Hormones and MetabolismДокумент10 страницReview Article: The Impact of Sleep and Circadian Disturbance On Hormones and MetabolismRENTI NOVITAОценок пока нет
- Do All Animals Sleep?: Jerome M. SiegelДокумент6 страницDo All Animals Sleep?: Jerome M. Siegelantoni_gamundi3942Оценок пока нет
- 5 - Gerer Le Jet LagДокумент8 страниц5 - Gerer Le Jet LagRimaTresnawatiОценок пока нет
- Psychology: Unit 3: Biorhythms, Aggression, RelationshipsДокумент16 страницPsychology: Unit 3: Biorhythms, Aggression, RelationshipsRimi_xОценок пока нет
- The Effect of Sleep On Gastrointestinal Functioning (ERGE y Dormir) PDFДокумент9 страницThe Effect of Sleep On Gastrointestinal Functioning (ERGE y Dormir) PDFAlejo RiveraОценок пока нет
- The Visually ImpairedДокумент21 страницаThe Visually ImpairedAnanthi balaОценок пока нет
- Circadian Rhythms - BB VerДокумент90 страницCircadian Rhythms - BB VerAlejandro CallanaupaОценок пока нет
- Final Paper-Turn In1Документ12 страницFinal Paper-Turn In1api-272378934Оценок пока нет
- 1 Circadian Rhythms in Attention, 2019Документ12 страниц1 Circadian Rhythms in Attention, 2019miryam25almaОценок пока нет
- Circadian Rhythm: Effect of Circadian DisruptionДокумент9 страницCircadian Rhythm: Effect of Circadian DisruptionJoshua MarkosОценок пока нет
- Chrononutrition: Summary Well-Regulated Eating Habits Are Said To Be Important For Health. A MajorДокумент3 страницыChrononutrition: Summary Well-Regulated Eating Habits Are Said To Be Important For Health. A MajorFranklin Howley-Dumit SerulleОценок пока нет
- The Relationship Between Sleep Disturbances and DiabetesДокумент15 страницThe Relationship Between Sleep Disturbances and Diabeteskarar.hasan2000Оценок пока нет
- Biological Rhythms With Respect To EndocrinologyДокумент6 страницBiological Rhythms With Respect To EndocrinologyTehseen KhanОценок пока нет
- Effects of Age On Circadian RhythmДокумент4 страницыEffects of Age On Circadian RhythmJulie AmalaОценок пока нет
- SLEEPДокумент19 страницSLEEPRegimae BartolomeОценок пока нет
- Circardian RhythmДокумент15 страницCircardian RhythmGopika SОценок пока нет
- Sleep and Dreams Booklet 1Документ36 страницSleep and Dreams Booklet 1joffriennetriolОценок пока нет
- Outline and Evaluate Infradian And/or Ultradian Rhythms (16 Marks)Документ2 страницыOutline and Evaluate Infradian And/or Ultradian Rhythms (16 Marks)HumaОценок пока нет
- Animal Behavior Biological RhythmsДокумент3 страницыAnimal Behavior Biological RhythmsAlok PatraОценок пока нет
- Assignment of EndocrinologyДокумент12 страницAssignment of EndocrinologySaba RiazОценок пока нет
- CircadianДокумент3 страницыCircadianPrernaОценок пока нет
- Daily Rhythms of The Sleep-Wake Cycle: Review Open AccessДокумент14 страницDaily Rhythms of The Sleep-Wake Cycle: Review Open AccessCintya RambuОценок пока нет
- Sleep N Wake DisorderДокумент55 страницSleep N Wake DisorderFUN FLARE SHADOWОценок пока нет
- Term Paper On Circadian RhythmsДокумент8 страницTerm Paper On Circadian Rhythmsaflspfdov100% (1)
- Heavy Sleepers: SleepДокумент2 страницыHeavy Sleepers: SleepPatrickReisingerОценок пока нет
- The Effect of Sleep On Gastrointestinal FunctioningДокумент9 страницThe Effect of Sleep On Gastrointestinal FunctioningMércia FiuzaОценок пока нет
- Sleep and WakingДокумент36 страницSleep and WakingPayal MulaniОценок пока нет
- Thesis LiewДокумент29 страницThesis Liewfpm5948Оценок пока нет
- Sleep and Circadian Rhythms: Key Components in The Regulation of Energy MetabolismДокумент10 страницSleep and Circadian Rhythms: Key Components in The Regulation of Energy MetabolismAacg MeryendОценок пока нет
- Sexual Dimorphism in Body ClocksДокумент3 страницыSexual Dimorphism in Body ClocksDjinОценок пока нет
- Circadian RhythmДокумент65 страницCircadian RhythmDipti PunjalОценок пока нет
- Wal Jee 2018Документ2 страницыWal Jee 2018Rosemarie FritschОценок пока нет
- Utilizing The DSM-5 Anxious Distress Specifier To Develop Treatment Strategies For Patients With Major Depressive DisorderДокумент12 страницUtilizing The DSM-5 Anxious Distress Specifier To Develop Treatment Strategies For Patients With Major Depressive DisorderRosemarie FritschОценок пока нет
- PDFДокумент532 страницыPDFRosemarie FritschОценок пока нет
- Reference Subjects Age (Yr) Gender (% F) Baseline HAM D 17 / Madrs Study Design OutcomesДокумент8 страницReference Subjects Age (Yr) Gender (% F) Baseline HAM D 17 / Madrs Study Design OutcomesRosemarie FritschОценок пока нет
- Safety and Efficacy of Lorcaserin: A Combined Analysis of The BLOOM and BLOSSOM TrialsДокумент12 страницSafety and Efficacy of Lorcaserin: A Combined Analysis of The BLOOM and BLOSSOM TrialsRosemarie FritschОценок пока нет
- Adult 22q11 Study - UCLAДокумент1 страницаAdult 22q11 Study - UCLARosemarie FritschОценок пока нет
- Teachers & Carers Guide PDFДокумент11 страницTeachers & Carers Guide PDFRosemarie FritschОценок пока нет
- Update On ParasomniasДокумент8 страницUpdate On ParasomniasRosemarie FritschОценок пока нет
- BIPOLAR DEPRESSION A Comprehensive Guide El MallakhДокумент278 страницBIPOLAR DEPRESSION A Comprehensive Guide El MallakhRosemarie Fritsch100% (3)
- Effect of Sleep Deprivation On College Students' Academic PerformanceДокумент10 страницEffect of Sleep Deprivation On College Students' Academic PerformanceVirgil Viral Shah0% (1)
- Best Practices of Dave ElmanДокумент2 страницыBest Practices of Dave ElmanEliferion100% (4)
- Relax Release and Dream OnДокумент3 страницыRelax Release and Dream OnKing GeorgeОценок пока нет
- All About Sleep LISTO InglesДокумент6 страницAll About Sleep LISTO InglesMeisson CabreraОценок пока нет
- A Brief History of Sleep ResearchДокумент3 страницыA Brief History of Sleep ResearchAleh ValençaОценок пока нет
- Black Book of Forbidden Knowledge - Lucid DreamingДокумент11 страницBlack Book of Forbidden Knowledge - Lucid Dreamingorakuldragyn83% (30)
- Idiopathic Hypersomnia Its All in Their HeadДокумент2 страницыIdiopathic Hypersomnia Its All in Their HeadSambo Pembasmi LemakОценок пока нет
- End The Insomnia Struggle - A Step-by-Step Guide To Help You Get To Sleep and Stay Asleep PDFДокумент234 страницыEnd The Insomnia Struggle - A Step-by-Step Guide To Help You Get To Sleep and Stay Asleep PDFBella Donna100% (1)
- Prevalence of Sleep Disorder Among Dental Students - A PDFДокумент8 страницPrevalence of Sleep Disorder Among Dental Students - A PDFSara VegaОценок пока нет
- Classification ParagraphДокумент2 страницыClassification ParagraphPamela MarquezОценок пока нет
- Sleep ParalysisДокумент7 страницSleep ParalysisAireeseОценок пока нет
- Sleep Disorders in Children and Adolescents: Deepti Shenoi MDДокумент50 страницSleep Disorders in Children and Adolescents: Deepti Shenoi MDCitra Sukri Sugesti100% (1)
- Crew Handbook (Appendix B) Fatigue Risk Guidance For CrewДокумент41 страницаCrew Handbook (Appendix B) Fatigue Risk Guidance For CrewIanA100% (1)
- Exotic Hypnosis Inductions - Unusual & Unique Hypnosis TechniquesДокумент3 страницыExotic Hypnosis Inductions - Unusual & Unique Hypnosis Techniquesgmeades33% (3)
- Sleep Is ScientificДокумент42 страницыSleep Is ScientificGlucose DRglucoseОценок пока нет
- Endo & Exogenous Pacemakersin Biological RhythmsДокумент2 страницыEndo & Exogenous Pacemakersin Biological RhythmsMiss_M90Оценок пока нет
- Info-Sleep HygieneДокумент1 страницаInfo-Sleep Hygieneapi-326398113Оценок пока нет
- The Link Between Fatigue and Safety PDFДокумент18 страницThe Link Between Fatigue and Safety PDFAndre MarsОценок пока нет
- Erickson Hypnosis PDFДокумент2 страницыErickson Hypnosis PDFWilliam0% (2)
- Wark 1996Документ13 страницWark 1996Francisca GonçalvesОценок пока нет
- Bruni-2004-Sleep Disturbances in As A Questionnaire StudyДокумент8 страницBruni-2004-Sleep Disturbances in As A Questionnaire Studybappi11Оценок пока нет
- How To Have Wake Induced Lucid Dreams (WILDs)Документ19 страницHow To Have Wake Induced Lucid Dreams (WILDs)Wig WamОценок пока нет
- Sleep Deprivation and Mental HealthДокумент4 страницыSleep Deprivation and Mental Healthapi-341198049Оценок пока нет
- Dement& Kleitman Short QuestionsДокумент2 страницыDement& Kleitman Short QuestionsKashmira JeevaОценок пока нет
- Nursing Care Plan For Insomnia NCPДокумент2 страницыNursing Care Plan For Insomnia NCPderic83% (24)
- Athens Insomnia Scale EnglishДокумент1 страницаAthens Insomnia Scale EnglishditadpОценок пока нет
- Normal Sleep PDFДокумент54 страницыNormal Sleep PDFGeraldine TaveraОценок пока нет
- CSHQ Article PDFДокумент9 страницCSHQ Article PDFmerawatidyahsepitaОценок пока нет
- Sleep and Rest NCPДокумент2 страницыSleep and Rest NCPDhan LopezОценок пока нет
- Dreams (English Department - Morning Assembly Speech)Документ1 страницаDreams (English Department - Morning Assembly Speech)Syafiqah RedzwanОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- To Explain the World: The Discovery of Modern ScienceОт EverandTo Explain the World: The Discovery of Modern ScienceРейтинг: 3.5 из 5 звезд3.5/5 (51)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Dark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseОт EverandDark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseРейтинг: 3.5 из 5 звезд3.5/5 (69)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (5)
- Gut: the new and revised Sunday Times bestsellerОт EverandGut: the new and revised Sunday Times bestsellerРейтинг: 4 из 5 звезд4/5 (393)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceОт EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceРейтинг: 4.5 из 5 звезд4.5/5 (517)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (59)
- How Emotions Are Made: The Secret Life of the BrainОт EverandHow Emotions Are Made: The Secret Life of the BrainРейтинг: 4.5 из 5 звезд4.5/5 (440)
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОт EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОценок пока нет
- Critical Care: A New Nurse Faces Death, Life, and Everything in BetweenОт EverandCritical Care: A New Nurse Faces Death, Life, and Everything in BetweenРейтинг: 3.5 из 5 звезд3.5/5 (159)
- Sully: The Untold Story Behind the Miracle on the HudsonОт EverandSully: The Untold Story Behind the Miracle on the HudsonРейтинг: 4 из 5 звезд4/5 (103)
- Tales from Both Sides of the Brain: A Life in NeuroscienceОт EverandTales from Both Sides of the Brain: A Life in NeuroscienceРейтинг: 3 из 5 звезд3/5 (18)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessОт Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessРейтинг: 4 из 5 звезд4/5 (33)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincОт EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincРейтинг: 3.5 из 5 звезд3.5/5 (137)
- A Brief History of Time: From the Big Bang to Black HolesОт EverandA Brief History of Time: From the Big Bang to Black HolesРейтинг: 4 из 5 звезд4/5 (2193)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsОт EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsРейтинг: 4.5 из 5 звезд4.5/5 (6)
- Algorithms to Live By: The Computer Science of Human DecisionsОт EverandAlgorithms to Live By: The Computer Science of Human DecisionsРейтинг: 4.5 из 5 звезд4.5/5 (722)
- Lessons for Survival: Mothering Against “the Apocalypse”От EverandLessons for Survival: Mothering Against “the Apocalypse”Рейтинг: 5 из 5 звезд5/5 (2)