Академический Документы
Профессиональный Документы
Культура Документы
Kuliah 1 Cair
Загружено:
kolasasa0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров50 страницteknologi farmasi
Оригинальное название
Kuliah 1 Cair (1)
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документteknologi farmasi
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров50 страницKuliah 1 Cair
Загружено:
kolasasateknologi farmasi
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 50
Teknologi Farmasi I
Cair dan Semi Padat
Najma Annuria Fithri
Ganjil 2013
Self Introduction
Najma Annuria Fithri
Education
- SMP Al-Kautsar, Bandar Lampung
- SMA Al-Kautsar , Bandar Lampung
- S1 Farmasi Sains dan Industri UGM 2006
- Apt Fak. Farmasi UGM 2010
- S2 Ilmu Farmasi Sains dan Teknologi UGM 2011
CP
- email: empith@gmail.com
- HP : 081931769304 / 082325780787
Syllabus
Liquid excipients
Semi solid excipients
Tools and equipments in manufacture
Methods of manufacture liquid
Methods of manufacture semi solid
Quality control and evaluations
Quality control and evaluations (Task)
Scoring system
Final test (50%
Quizes (20%)
Tasks (20%)
Involvement in class (10%)
Types of LDF
Solutions
- Aqueous solutions + Sugar Syrup
- Hydroalcoholic Elixir
- Aromatic alcoholic solutions Spirit
- Aromatic aqueous solutions Aromatic water
- Extracted liquids from crude products Tincture
Emulsions
Suspensions
Type of excipients
Solvents/Co-solvents
Buffering agents
Anti microbial preservatives
Anti oxidants
Sequestering agents
Wetting agents
Anti foaming agents
Thickening agents
Sweetening agents
Colouring agents
Flavouring agents
Humectant
Solvents/Co-Solvents
Water is the solvent most widely used as a vehicle due to:
Lack of toxicity, physiological compatibility, and good solubilising power (high
dielectric constant), but
Likely to cause instability of hydrolytically unstable drugs
Good vehicle for microbial growth
Sorbitol, dextrose, etc. are often added as solubilisers, as
well as base sweeteners
Similar pros and cons to water alone
Water-miscible co-solvents are used to:
Enhance solubility, taste, anti-microbial effectiveness or stability
Reduce dose volume (e.g. oral, injections)
Or, conversely, optimise insolubility (if taste of API is an issue)
Examples: propylene glycol, glycerol, ethanol, low molecular weight PEGs
Water-immiscible co-solvents, e.g.
Emulsions / microemulsions using fractionated coconut oils
Some solvents for liquid preparations
Alcohol, Ethyl alcohol (ethanol)C
2
H
5
OH
1. Next to water, alcohol is the most useful solvent in pharmacy. It is used as a primary
solvent for many organic compounds.
2. It forms hydroalcoholic mixture with water that dissolves both alcohol-soluble and
water-soluble substances
3. Alcohol has been well recognized as a solvent and excipient in the formulation of oral
pharmaceutical products. Alcohol is often preferred because of its miscibility with
water and its ability to dissolve many water-insoluble ingredients, including drug
substances, flavorants, and antimicrobial preservatives.
4. It is also used in liquid products as an antimicrobial preservative alone or with
parabens, benzoates, sorbates, and other agents.
5. Toxicity of ingested alcohol particularly for children. For OTC oral products intended
for children under 6 years of age, the recommended alcohol content limit is 0.5%, for
products intended for children 6 to 12 years old, the recommended limit is 5% and for
children over 12 years and adults, the recommended limit is 10%.
Diluted alcohol
- Is prepared by mixing equal volumes of alcohol and purified water (50%).
- Diluted alcohol is a useful hydroalcoholic solvent in various pharmaceutical processes
and preparations.
Alcohol, Rubbing (alcohol rubbing compound)
- It contains about 70% ethyl alcohol by volume.
- It is employed as a rubefacient externally and as soothing rub for bedridden patients, a
germicide for instruments
- As vehicle for topical preparation
- As skin cleanser before injection
Isopropyl rubbing alcohol
- It has the advantage over ethyl alcohol in that the commonly available product contains
not over 1% of water, while ethyl alcohol contains about 5% water, which often a
disadvantages.
-Is about 70% by volume isopropyl alcohol, with or without colour additives, stabilizers and
perfume oils
- It is used externally as a rubefacient and soothing rub and for topical products
- The commercially available 91% isopropyl alcohol solution are commonly employed by
diabetic patients in preparing needles and syringes for hypodermic injections of insulin
and for disinfecting the skin.
Glycerin, Glycerol
- It is a clear syrupy liquid with sweet taste
- It is miscible with water and alcohol
- As solvent it is comparable with alcohol, but because of
its viscosity, solutes are slowly soluble in it unless it is
rendered less viscous by heating.
- It is used as a stabilizer and as auxiliary solvent in
conjunction with water or alcohol.
- It has preservative qualities
- It is used in internal preparations
- It dissolves the fixed alkalies, a large number of salts
and vegetable acids, pepsin, tannin, some active
principals of plants, etc.
- It also dissolves gum, starch, etc.
Propylene glycol
- A viscous liquid, miscible with water, with acetone and with chloroform in all
proportions.
- It is soluble in ether and will dissolve many essential oils but is immiscible with
fixed oils.
- It is a useful solvent with wide range of application
- It is substituted for glycerol in modern pharmaceutical preparations
- It is used for formulation of digoxin, diazepam, phenobarbital injection
- As diluent for ear drops
Polyethyleneglycol, PEG 400
- It is miscible with water, acetone, alcohol and other glycols.
- It dissolves many water-soluble organic compounds as well as certain water
insoluble substances such as acetylsalicylic acid and theophyllin.
- Is used as a solvent in topical solution
- Used as co-solvent with alcohol and water
- Can be used for extraction processes
- In the formulation of veterinary solutions
Role of co-solvency
Weak electrolytes and non-polar molecules frequently have poor
water solubility
Their solubility usually can be increased by the addition of a water-
miscible solvent in
which the drug has good solubility.
This process is known as co-solvency, and the solvents
used in combination to
increase the solubility of the solute are known as co-
solvent
Co-solvents are employed not only to affect solubility of the
drug, but also to improve the solubility of volatile constituents
used to impart a desirable flavor and odour to the product.
Types of pharmaceutical water
Purified water, USP
Water for injection
Aromatic water
Physiological compatibility
Lack of toxicity
Possesses a high dielectric constant
ensuring the dissolution of a wide range of ionizable
materials
Lack of selectivity
Water is used both as vehicle and as a solvent for the desired
flavoring or medicinal ingredients.
Advantages: Tasteless, odourless, lack of pharmacological
activity, neutral and very cheap
Tap Water
It is not permitted to use tap water for the dispensing of
pharmaceutical dosage forms due to its possible bacterial
contamination and the presence of dissolved salts that destroy
the active ingredients or enhance their decomposition.
Freshly Boiled and Cooled Water
Boiling is seldom used to destroy vegetative bacteria. But, on
storage for long time spores may yield vegetative
microorganism.
Purified Water
Must be used for most pharmaceutical operations and in all the
tests and assays.
Such water is prepared by distillation, deionization (ion
exchange method) or reverse osmosis.
"Hard" waters are those that contain the Ca and Mg cations.
Alkaline" waters are those that contain bicarbonates as the
major impurity.
Ultraviolet energy, heat or filtration (Millipore filtration) can be
used to remove or kill the microorganisms present in the water.
Water for injection
Must be used for the formulation of parental solutions.
It is obtained by sterilizing pyrogen-free distilled water.
Aromatic Waters
Aromatic waters (medicated waters) are clear, saturated aqueous
solution of volatile oils or other aromatic or volatile substances.
They are used principally as flavored or perfumed vehicles.
Volatile oils solutions represent an incompatibility problem of
salting out. This occurs after the incorporation of a very soluble
salt in their solution.
Aromatic water will deteriorate with time therefore:
- should be made in small quantities
- protected from intense light and excessive heat by storing in air
tight, light resistant containers.
- If they become cloudy or otherwise deteriorate; they should be
discarded. Deterioration may be due to volatilization,
decomposition or mould growth.
The strengths of pharmaceutical preparations are usually expressed in terms of percent
strength, although for very dilute preparations, expressions of ratio strength may be
used.
Percentage (%)
% w/v (e.g., 1%w/v =1g constituent in 100 mL preparation)
%v/v (e.g., 1%v/v = 1mL constituent in 100 mL preparation)
% w/w (e.g.,1%w/w=1 g constituent in 100 g preparation)
Ratio strength
weight in volume (e.g., 1:1000 w/v= 1g constituent in 1000 mL
preparation)
volume in volume (e.g., 1:1000 v/v = 1ml constituent in 1000
mL preparation)
weight in weight (e.g., 1:1000 w/w = 1 g constituent in 1000 g
preparation)
Buffering Agents
Can be necessary to maintain pH of the formulation to:
Ensure physiological compatibility
Maintaining/optimising chemical stability
Maintaining/optimising anti-microbial effectiveness
Optimise solubility (or insolubility if taste is an issue)
But, optimum pH for chemical stability, preservative
effectiveness and solubility (or insolubility) may not be
the same
Compromises need to be made
Ex: carbonates, citrates, phosphate, lactates,
gluconates, tartarates, borates (external). Its
presence in solution resists any changes in pH
upon dilution or addition of small quantities of
acid or base. The usual buffering agents used in
oral liquid preparations are acetate and
phosphate buffer. The buffer increase
Anti-microbial Preservatives
Preservatives are used in multi-use cosmetic/pharmaceutical
products (including paediatric formulations)
Prevents an increased risk of contamination and proliferation by opportunistic
microbes (from excipients or introduced externally), that would result in potential
health issues
Avoid use wherever possible, especially in products aimed at younger paediatric
patients
e.g. not required for sterile, single-dose products (as recommended for neonates)
Ideally targeted for microbial cells - showing no toxicity/irritancy
towards mammalian cells
Challenge is that the active groups involved are usually harmful to all living tissue
There are a limited number of approved preservatives available for
multi-use oral products, and options are even more limited for other
routes of administration
Should not use in parenteral infusions
Must avoid access to cerebrospinal fluid and retro-ocular administration
This restricted number can be further reduced by consideration of
factors such as levels required (dose), pH-solubility profiles, API &
excipient incompatibilities, adsorption, irritancy and toxicity.
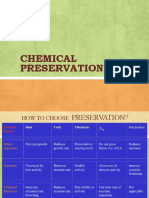
Choice of Preservative
The preservative selected should have the following
properties :
1. It should be effective against a wide range of
microorganisms.
2. It should be compatible with other ingredients of the
formulation.
3. It should be soluble in aqueous phase when used in
emulsions.
4. It should be nontoxic.
5. It should be free from odour and taste.
6. It should preserve the preparations and remain stable
for the shelf life of the product.
No singly preservative possesses all the qualities
therefore it becomes necessary to use a combination of
preservatives to prevent the growth of microorganisms.
The most commonly used preservatives are as follows:
1. Benzoic acid and sodium benzoate 0.1 to 0.2%.
2. Salicylic acid 0.1%.
3. Phenol 0.2 to 0.5%.
4. Chlorocresol 0.05 to 0.1%.
5. Alcohol 15 t 20%.
6. Chlorbutanol 0.5%.
7. Phenylmercuric nitrate 0.002 to 0.005%.
8. Sorbic cid and its salts 0.05 to 0.2%.
9. Benzalkoniumchloride 0.004 to 0.02 %.
10. Methyl paraben and propyl paraben 0.1% to
0.2%.
Anti-Oxidants
Used to control oxidation of:
API
Preservative, e.g. potassium sorbate
Vehicle, e.g. oils or fats susceptible to -oxidation (rancidification)
Colourants (ageing discolouration)
Sacrificial (more oxidisable than API, preservative, etc). Levels
will reduce with time. need to be monitored by specific assay
Light exposure and metal ion impurities can accelerate oxidative degradation and
hence depletion of antioxidant
Need to assess regulatory acceptability (differs in different
countries)
Efficacy can be affected by:
Compatibility with other excipients
Partitioning into micelles (from surfactants)
Adsorption onto surfaces (container, thickening agent and suspended particles)
Incompatibilities, e.g. with metal ions
Sequestering/Chelating agents
Chelating agent excipients are used in chelation therapy to
detoxify poisonous metal agents such as mercury [Hg],
arsenic [As], and lead [Pb] by converting them to a
chemically inert form that can be excreted without further
interaction with the body.
Chelating agents inhibits auto oxidations by metal ions
Metal ions are a catalyst to auto oxidation process
Wetting Agents
To aid wetting and dispersion of a hydrophobic API,
preservative or antioxidant
Reduce interfacial tension between solid and liquid during manufacture or
reconstitution of a suspension
Not all are suitable for oral administration
Examples include:
Surface active agents, e.g.
Oral: polysorbates (Tweens), sorbitan esters (Spans)
Parenteral: polysorbates, poloxamers, lecithin
External: sodium lauryl sulphate
.but these can cause excessive foaming (see anti-foaming agents) and can
lead to deflocculation and undesirable physical instability (sedimentation) if
levels too high
Hydrophilic colloids that coat hydrophobic particles, e.g. bentonite, tragacanth,
alginates, cellulose derivatives. Also used as suspending agents, these can
encourage deflocculation if levels are too low.
Anti-Foaming Agents
The formation of foams during manufacturing processes or
when reconstituting liquid dosage forms can be undesirable
and disruptive.
Anti-foaming agents are effective at discouraging the
formation of stable foams by lowering surface tension and
cohesive binding of the liquid phase.
A typical example is Simethicone (polydimethylsiloxane-
silicon dioxide), which is used at levels of 1-50ppm.
Of course, a foam is also a very valid dosage form option for
certain situations, e.g. for topical administration and in
wound dressings.
In addition, wet granulation using a foam rather than aqueous
granulation fluid is gaining popularity.
Thickening Agents
Suspension stabilisers: prevent settling/sedimentation
(particularly if a wetting agent present)
They usually modify viscosity and are often thixotropic (where
viscosity is dependent on applied shear and exhibits shear
thinning)
Easily poured when shaken
Must permit accurate dosing with chosen method (e.g. graduated
syringe, spoon)
Quickly reforms gel-like structure
They can impact on flocculation at low levels
Work by entrapment of solid particles, e.g. API, in a viscous or
even
gel-like structure
Can be either water-soluble, e.g. methylcellulose or
hydroxyethylcellulose
Or water-insoluble, e.g. microcrystalline cellulose
Example:
semi-synthetic: thickening agents-methyl
cellulose, carboxy methyl cellulose,
hydroxypropyl cellulose, synthetic polymers and
gelatin. Sodium carboxy methyl cellulose (3.5%)
is used in injectable suspensions.
Clays: hydrated aluminiumsilicate or
magnesium silicate
Non-ionic: sorbitol, glycerin, sugar or
polycthylene glycols
Sweetening Agents
Natural sweeteners
Sucrose; soluble in water (vehicle), colourless, stable (pH 4-8), increases viscosity;
Arguably the best taste/mouthfeel overall but cariogenic & calorific avoid in
paediatrics?
Sorbitol (non-cariogenic, non-calorific - appropriate for paediatric formulations),
but lower sweetness intensity than sucrose (so you need more) & can cause
diarrhoea
Artificial sweeteners
Regulatory review required often restricted territories
Much more intense sweeteners compared with sucrose
As a consequence the levels are much lower (<0.2%) but still need to refer to
WHO Acceptable Daily Intakes (ADIs)
Can impart a bitter or metallic after-taste (hence used in combination with natural
sweeteners), e.g.
Saccharin, and its salts
Aspartame
Acesulfame K
Sucralose excellent sweetness, non-cariogenic, low calorie, wide & growing
regulatory acceptability but relatively expensive
Flavouring Agents
Supplement and complement a sweetening agent
Ensures patient compliance (especially in paediatric formulations a big issue)
Can be natural, e.g. peppermint, lemon oils,
Or artificial e.g. butterscotch, tutti-frutti flavour
Instability can be an issue combinations can be used to cover intended product
shelf-life
Taste appreciation is not globally consistent
Genetic element: one persons acceptable taste is anothers unacceptable taste
Territorial (cultural?) differences in preference; e.g. US vs. Japan vs. Europe
Affected by age (paediatric perception and preferences are different from adult)
Can be affected by certain disease states, e.g. during cancer chemotherapy
Regulatory acceptability of flavours needs to be checked
Different sources, different compositions, different flavour, e.g. there are >30
different strawberry flavours!
Usually complex of composition (so refer to internationally recognised standards)
Colouring agents
Colouring agents may be defined as the substances used to
impart colour to foods, drugs and cosmetics to increase their
organoleptic properties. In pharmaceutical preparations
they may be used to increase their acceptability by the
patients, to give warning, or to produce standard
preparations.
The examples of mineral colours are ferric oxide (yellow
and red), carbon black, titanium dioxide and ultramarine.
Only the permitted colours are used in food and
pharmaceutical preparations. Caramel or burnt sugar, an
artificial colour is used to produce brown colour in cough
syrups. elixirs and other oral liquid preparation.
Certified color additives are classified according to
their approved use: (a) FD&C color additives,
which may be used in foods, drugs, and cosmetics;
(b) D&C color additives, some of which are
approved for use in drugs, some in cosmetics, and
some in medical devices; and (c) external D&C
color additives, the use of which is restricted to
external parts of the body, not including the lips
or any other body surface covered by mucous
membrane
Humectants
Hygroscopic excipients used at ~5% in aqueous
suspensions and emulsions for external application.
Their function is to retard evaporation of aqueous
vehicle of dosage form:
To prevent drying of the product after application to the skin
To prevent drying of product from the container after first opening
To prevent cap-locking caused by condensation onto neck of
container-closure of a container after first opening
Examples include:
propylene glycol
glycerol
PEG
Overview thoughts for paediatric dosage forms
So..
A quite wide range of excipients and dosage forms
needs to be considered
Key considerations for paediatric formulations are
to
minimize the use of excipients, understand the
limitations of those types of excipient that can and
are used and be able to justify their use at the dose
levels involved.
General philosophy regarding excipients for
liquid dosage forms
Choose the appropriate dosage formfor the target
population(s)
Avoid health hazards apply a benefit vs. risk balance
assessment:
Minimum age of target population
Maximum duration of therapy
Double-check age-related safety of established (adult dosage form?) excipients
Novel excipients need comprehensive safety testing
Justify inclusion and minimise number of excipients and
quantity to
be used:
Especially younger age groups
Choose dosage forms that achieve this
Not for aesthetic or cosmetic purposes
Avoid sugar for long-term use
Can any taste issue be reduced without resorting to the use of additives? e.g. through
dilution, pH control, API version selection (does reduced API solubility resolve the issue?)
Avoid biologically active excipients e.g. preservatives, anti-oxidants, unless dosage
flexibility warrants inclusion. Use lowest feasible levels.
Compliance with relevant regulations and be alert to the latest guidance
Solvents/Preservatives
Propylene Glycol Toxicity
Propylene glycol (PG) is a general solvent with anti-
microbial properties used in a wide range of
pharmaceutical preparations including oral liquids,
topicals and parenteral preparations
However, its use in large volumes in children is
very much discouraged:
PG has been associated with cardiovascular, hepatic, respiratory and
CNS adverse events, especially in neonates where the biological half-
life is prolonged (~17h) compared with adults (5h).
I.V. parenterals containing PG must be infused slowly
PG also has a laxative action at high oral doses through high osmotic
pressure effects.
Solvents
Ethanol Toxicity
Widely used as a co-solvent to aid solubility
In US, maximum permitted quantities in OTC products:
<0.5% for children under 6-years
<5% for children 6-12-years
<10% for children over 12-years
Acute (overdose) or chronic (long-term use) toxicity is possible
May cause adverse symptoms of intoxication, lethargy, stupor, coma,
respiratory depression and cardiovascular collapse
Peanut Oil Toxicity
Peanut oil is used as a food additive and as a solvent in intra-muscular
injections
It has been suggested that the use of peanut oil in childhood (infant
formula and topical preparations) can lead to later episodes of
hypersensitivity, and therefore should be discontinued
Sweeteners
Saccharin
Restricted regulatory acceptability
Poor aftertaste
Hypersensitivity reactions; mainly dermatologic
Paediatrics with allergy to sulphonamides should avoid saccharin
Aspartame Toxicity
Source of phenylalanine possibly an issue for phenylketoneurics
Aspartame has been blamed for hyperactivity in children but as yet
unproven
Sorbitol
Can induce diarrhoea
Solvents/Solvent sweeteners
Need for oral liquid preparations (that children
typically find easier to swallow) often
necessitates:
Taste-masking; which often relies on sweeteners
Addition of co-solvents to improve drug solubility if a solution is wanted
(elegance/mouth feel vs. taste)
Most commonly used solvent sweeteners are
Propylene glycol
Glycerine (Glycerol)
Anti-microbial Preservatives
Benzyl Alcohol toxicity in neonates
Widely used as a preservative in cosmetics, foods and pharmaceuticals
(including injectables and oral liquids)
Toxic syndrome observed in neonates it was attributed to the practice
of flushing out umbilical catheters with solutions containing benzyl
alcohol (BA), because of trace levels of benzaldehyde that were present
Dilution of nebulisation solutions with BA-preserved saline led to
severe respiratory complications and even death in neonates.
Attributed to accumulation of BA due to an immature metabolic
capability.
Only dilute inhaled solutions with non-preserved, sterile diluents
Anti-microbial Preservatives
Sodium Benzoate toxicity
Widely used as a preservative in cosmetics, foods and pharmaceuticals
(including injectables and oral liquids)
Injectable combinations of Na Benzoate and Caffeine should not be
used in neonates; found to elicit non-immunological contact reactions,
including urticaria and atopic dermatitis
Limitation on dosing of NA benzoate to neonates - 10mg/kg/day
due to immature metabolic capability
Thimerosal toxicity
Formerly widely used as a preservative in cosmetics, in soft contact lens
solutions and pharmaceuticals (primarily vaccines)
Being phased out from most paediatric vaccines as better options
emerge
Possible links with toxicity in paediatric vaccines, e.g. linked with
childhood autism but not proven
Diluents/Fillers
Lactose toxicity (immature metabolism)
Lactose occurs widely in dairy products and is used in infant feed formulae.
In pharmaceutical preparations it is widely used as a diluent in tablets and
capsules, in lyophilised powders, as a sweetener in liquid formulations and
as a carrier in dry powder inhalation products.
Lactose intolerance occurs when there is a deficiency in the intestinal
enzyme lactase, leading to GIT build-up of lactose. There is then the risk of
abdominal bloating and cramps.
Lactase is normally present at high levels at birth, declining rapidly in early
childhood (4-8 years) . Hypolactasia (malabsorption of lactose) can thus
occur at an early age and, furthermore, this varies among different ethic
groups.
Significant lactose intolerance can also occur in adults but this is rare.
E numberAdditives
(Colourants, preservatives, stabilisers, anti-
oxidants, etc.)
Current high profile concerns...
Some opinion that additives in processed foods are linked to children's
allergies.
Particular attention has been paid to infants and children's products
because their immature organs are less efficient at removing such
toxins from their systems.
Certain combinations of the following artificial food colours: sunset
yellow (E110), quinoline yellow (E104), carmoisine (E122), allura red
(E129), tartrazine (E102) and ponceau 4R (E124) have been linked to a
negative effect on childrens behaviour.
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Pizza Hut IngredientsДокумент18 страницPizza Hut Ingredientsnital001Оценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Phle Reviewer Module 5 PharmaceuticsДокумент97 страницPhle Reviewer Module 5 PharmaceuticsCarlstine Ileto100% (3)
- Listening and Speaking 4 Q: Skills For Success Unit 5 Student Book Answer KeyДокумент4 страницыListening and Speaking 4 Q: Skills For Success Unit 5 Student Book Answer KeyNgoc Thanh100% (1)
- Food AdditivesДокумент21 страницаFood AdditivesHarish Srinivasan100% (1)
- Calcium PropionateДокумент8 страницCalcium PropionateGaganpreet KaurОценок пока нет
- Consumer Chemistry Q2 M3Документ22 страницыConsumer Chemistry Q2 M3Garcia Family Vlog57% (7)
- Chapter 5 Curing Fish and Other Marine ProductsДокумент9 страницChapter 5 Curing Fish and Other Marine ProductsGraceCayabyabNiduaza100% (1)
- Finalization: (Banana Peelings As An Alternative Substitute To Vinegar)Документ6 страницFinalization: (Banana Peelings As An Alternative Substitute To Vinegar)Myka Gomez OtnamОценок пока нет
- FOOD INGREDIENTS NUMBERS (E-Numbers) - WorldOfIslam - Halal & Haram FoodДокумент13 страницFOOD INGREDIENTS NUMBERS (E-Numbers) - WorldOfIslam - Halal & Haram FoodMatthew BrownОценок пока нет
- Unit 5. Food Processing and Preservation TechniquesДокумент30 страницUnit 5. Food Processing and Preservation Techniquesfeyisa100% (1)
- Deterioration of FishДокумент12 страницDeterioration of FishZeenat MoambarОценок пока нет
- Meets BC Regulatory Requirements: Sample Food Safety PlanДокумент9 страницMeets BC Regulatory Requirements: Sample Food Safety PlanPSAОценок пока нет
- CBCS PDFДокумент227 страницCBCS PDFali skОценок пока нет
- PreservativeДокумент40 страницPreservativeKrishnan vijayОценок пока нет
- Novel Natural Food Preservatives and Applications in Seafood Preservation A ReviewДокумент11 страницNovel Natural Food Preservatives and Applications in Seafood Preservation A ReviewAbe LimОценок пока нет
- Use of Natural Preservatives in Seafood PDFДокумент17 страницUse of Natural Preservatives in Seafood PDFAnonymous SKlyU5sJ5AОценок пока нет
- 8 Science MicroorganismsДокумент6 страниц8 Science MicroorganismsAjay AnandОценок пока нет
- CITATION Mas19 /L 1033Документ3 страницыCITATION Mas19 /L 1033Fadhlin SakinahОценок пока нет
- CosmeticsДокумент4 страницыCosmeticsMadhu Kiran DhondalayОценок пока нет
- Chemistry (Yang Ini)Документ45 страницChemistry (Yang Ini)Nabil MuhammadОценок пока нет
- 2 - 1 Chemical PreservationДокумент18 страниц2 - 1 Chemical PreservationAn FakeihahОценок пока нет
- ProClin® Preservatives For in Vitro Diagnostic Materials: Efficacy vs. Thimerosal and Sodium AzideДокумент2 страницыProClin® Preservatives For in Vitro Diagnostic Materials: Efficacy vs. Thimerosal and Sodium AzideSAFC-Global100% (1)
- Effect of Water ActivityДокумент2 страницыEffect of Water ActivityMariel GeleraОценок пока нет
- Summative Test 4 Tle 6Документ4 страницыSummative Test 4 Tle 6Jovanni Bendulo LegaspinaОценок пока нет
- Hyperspectral Imaging Technique For Evaluating Food Quality AndsafetyДокумент11 страницHyperspectral Imaging Technique For Evaluating Food Quality AndsafetyRaluca Alexandra NeculaОценок пока нет
- COMMON METHODS of PROCESSING and PRESERVING of FOODS 3rd QuarterДокумент13 страницCOMMON METHODS of PROCESSING and PRESERVING of FOODS 3rd QuarterMaymay AuauОценок пока нет
- Pengembangan Farmasetik Bentuk Sediaan Cair (Larutan)Документ40 страницPengembangan Farmasetik Bentuk Sediaan Cair (Larutan)niantri laiaОценок пока нет
- Application of Ftir For The Characterisation of Sustainable Cosmetics and Ingredients With Antioxidant PotentialДокумент9 страницApplication of Ftir For The Characterisation of Sustainable Cosmetics and Ingredients With Antioxidant PotentialChiper Zaharia DanielaОценок пока нет
- Q2 Week 2 Con ChemДокумент18 страницQ2 Week 2 Con ChemB05 - SAMAN GERARD JOHN ALBERTОценок пока нет
- Methods of Dairy Milk PreservationДокумент5 страницMethods of Dairy Milk PreservationAbdy ShahОценок пока нет