Академический Документы
Профессиональный Документы
Культура Документы
When Supply
Загружено:
mango91286Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
When Supply
Загружено:
mango91286Авторское право:
Доступные форматы
When supply < demand
Classification (NYHA) I: No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath) II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea IV: Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased Stages (American College of Cardiology / American Heart Association) A: high risk, no structural heart disease or sx B: structural heart disease, no signs or sx C: structural heart disease, prior or current sx D: refractory, specialized interventions needed Causes Causes of high output: anemia, pregnancy, hyperthyroidism, AV fistulas, wet beriberi, Pagets disease of bone, MR, AR Systolic failure: ischemic heart disease, HTN cardiomyopathy, valvular heart disease, myocarditis, EtOH, radiation, hemochromatosis, thyroid disease, DM, smoking, obesity Diastolic failure: HTN myocardial hypertrophy, AS, MS, AR, restrictive cardiomyopathy (amyloidosis, sarcoidosis, hemochromatosis) Clinical features L sided failure symptoms: dyspnea, orthopnea, PND, noctuenal cough, confusion and memory impairment, diaphoresis and cool extremities at rest, PMI displaced laterally, S3, S4, crackles/rales at lung bases, dullness to percussion and decreased tactile fremitues of lower lung fields, increased intensity of P2, narrow pulse pressure R sided failure symptoms: peripheral pitting edema, nocturia, JVD, hepatomegaly, ascites, RV heave Diagnosis CXR: cardiomegaly, Kerley B lines (These are short parallel lines at the lung periphery. These lines represent interlobular septa), interstitial markings, pleural effusion TTE: initial test of choice. EF, systolic vs diastolic ECG: nonspecific. Chamber enlargement, ischemia, past MI Nuclear ventriculography: LVEF, RVEF Cardiac catheterization: quantitiatve Stress testing: assesses dynamic responses of HR, heart rhythm, BP Lab tests: cardiac profile, CBC, BNP Framingham clinical criteria for the diagnosis for heart failure 2 major OR 1 major + 2 minor criteria Major : PND, orthopnea, elevated JVP, pulmonary rales, S3, cardiomegaly on CXR, pulmonary edema on CXR, weight loss 4.5 kg in five days in response to treatment Minor: bilateral leg edema, nocturnal cough, DOE, hepatomegaly, pleural effusion, tachycardia (120), weight loss 4.5 kg in five days Treatment Systolic o <4g Na/day, weight loss, smoking cessation, alcohol restruction, exercise, monitor weight daily o Diuretics: sx control only o Spironolactone: decreases M&M in class III and IV (RALES trial) o ACE inhibitors: decerase mortality, prolong survivial, alleviate sx (CONSENSUS, SOLVD trials) o ARBs: if ACE inhibitors cause cough
Beta blockers: decrease mortality in px with post-MI heart failure, carvedilol > metoprolol (COMET trial), decreases tissue remodeling, improves sx o Digitalis: for refractory CHF, improves sx o Hydralazine, isorbide dinitrate: improves mortality in some patients o Contraindications: metformin, thazolidinediones, NSAIDs, negative inotropes o ICD, CRT, VAD, cardiac transplant Diastolic failure o Beta blockers o Diuretics o ACE inhibitors, ARBs: unclear o Digoxin, spironolactone: contraindicated General treatment principles o Mild (Classes I to II): <4g Na/day, less physical activity, loop diuretic, ACE inhibitor o Mild to moderate (Classes II to III): loop diuretic + ACE inhibitor beta blockers o Moderate to severe (Classes III to IV): loop diuretic + ACE inhibitor digoxin spironolactone o
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- CsДокумент11 страницCsmango91286Оценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- PreTest Vignettes For 2CK, 8th EditionДокумент295 страницPreTest Vignettes For 2CK, 8th Editionmango91286100% (7)
- Psychoanalysis ReportДокумент16 страницPsychoanalysis ReportianneОценок пока нет
- Organizational Behavior: Stephen P. RobbinsДокумент24 страницыOrganizational Behavior: Stephen P. Robbinskria1167% (3)
- Ethics & Legal Issues in PsychiatryДокумент91 страницаEthics & Legal Issues in PsychiatryShah OzairОценок пока нет
- Conrad Fischer MCQsДокумент328 страницConrad Fischer MCQsPopescu Tina100% (1)
- Nursing Care Plan for Community Acquired PneumoniaДокумент2 страницыNursing Care Plan for Community Acquired PneumoniaEngely Mercader100% (1)
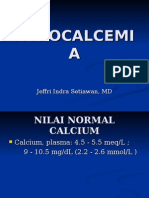
- HYPOCALCEMIAДокумент27 страницHYPOCALCEMIAJeffri SetiawanОценок пока нет
- Beginners' Guide To Health and FitnessДокумент25 страницBeginners' Guide To Health and FitnessMahmood HikmetОценок пока нет
- NCP For Bladder CaДокумент4 страницыNCP For Bladder CaChris Tine CaccamОценок пока нет
- Cisapride Use in Pediatric Patients With Intestinal Failure and Its Impact On Progression of Enteral NutritionДокумент6 страницCisapride Use in Pediatric Patients With Intestinal Failure and Its Impact On Progression of Enteral Nutritionmango91286Оценок пока нет
- Epidemiologyand Pathophysiologyof Gastroparesis: Baha Moshiree,, Michael Potter,, Nicholas J. TalleyДокумент14 страницEpidemiologyand Pathophysiologyof Gastroparesis: Baha Moshiree,, Michael Potter,, Nicholas J. Talleymango91286Оценок пока нет
- Probiotics in GI DisordersДокумент35 страницProbiotics in GI Disordersmango91286Оценок пока нет
- Factors Associated With Success and Failure of Weaning Children From Prolonged Enteral Nutrition - A Retrospective Cohort StudyДокумент6 страницFactors Associated With Success and Failure of Weaning Children From Prolonged Enteral Nutrition - A Retrospective Cohort Studymango91286Оценок пока нет
- SubtitleДокумент30 страницSubtitlemango91286Оценок пока нет
- Hepatorenal SyndromeДокумент1 страницаHepatorenal Syndromemango91286Оценок пока нет
- Medical Care For Immigrant ChildrenДокумент36 страницMedical Care For Immigrant Childrenmango91286Оценок пока нет
- Constipation and Bowel RegimensДокумент17 страницConstipation and Bowel Regimensmango91286Оценок пока нет
- MeningitisДокумент1 страницаMeningitismango91286Оценок пока нет
- Cannabis in GI and Liver DiseaseДокумент19 страницCannabis in GI and Liver Diseasemango91286Оценок пока нет
- Past Journal Club QuestionsДокумент3 страницыPast Journal Club Questionsmango91286Оценок пока нет
- FHДокумент1 страницаFHmango91286Оценок пока нет
- Lower Gastrointestinal BleedingДокумент1 страницаLower Gastrointestinal Bleedingmango91286Оценок пока нет
- BacteriaДокумент7 страницBacteriamango91286Оценок пока нет
- Acute CholecystitisДокумент1 страницаAcute Cholecystitismango91286Оценок пока нет
- Micro Exam 3 NotesДокумент7 страницMicro Exam 3 Notesmango91286Оценок пока нет
- Urinary IncontinenceДокумент0 страницUrinary Incontinencemango91286Оценок пока нет
- Congestive Heart FailureДокумент1 страницаCongestive Heart Failuremango91286Оценок пока нет
- Acute CholecystitisДокумент1 страницаAcute Cholecystitismango91286Оценок пока нет
- Micro Final CsДокумент13 страницMicro Final Csmango91286Оценок пока нет
- Answer SheetДокумент1 страницаAnswer Sheetmango91286Оценок пока нет
- Abdominal PainДокумент78 страницAbdominal Painmango91286Оценок пока нет
- NBME PercentilesДокумент1 страницаNBME Percentilesmango91286Оценок пока нет
- NBME PercentilesДокумент1 страницаNBME Percentilesmango91286Оценок пока нет
- Abnormal Uterine BleedingДокумент0 страницAbnormal Uterine Bleedingmango91286Оценок пока нет
- Student Objectives - ACOGДокумент164 страницыStudent Objectives - ACOGmango91286100% (1)
- Cba Ospe RevisedДокумент11 страницCba Ospe RevisedSadia YousafОценок пока нет
- Gait AssessmentДокумент12 страницGait Assessmentahmed K.Abd el SaterОценок пока нет
- Nursing Practice IДокумент9 страницNursing Practice IMonique Porcadilla SantiagoОценок пока нет
- Effects of Mobile LegendsДокумент3 страницыEffects of Mobile LegendsRiziel SolaresОценок пока нет
- Drug Study: Acetadote, Mucomyst MucolyticsДокумент2 страницыDrug Study: Acetadote, Mucomyst MucolyticsMae Ann Bueno CastillonОценок пока нет
- Data Dictionary: NO Label Operational Scale of Measurem ENT 1Документ6 страницData Dictionary: NO Label Operational Scale of Measurem ENT 1nik nur nisa azlinОценок пока нет
- Hu4640.u5 Powerpoint 1Документ14 страницHu4640.u5 Powerpoint 1Driley121Оценок пока нет
- Mechanisms of Cough From AngiotensinДокумент1 страницаMechanisms of Cough From AngiotensinironОценок пока нет
- Medical Tourism: A Study of Kerala: Project SynopsisДокумент2 страницыMedical Tourism: A Study of Kerala: Project SynopsisbhatiaharryjassiОценок пока нет
- Chapter 2 Physical Therapy ModalitiesДокумент54 страницыChapter 2 Physical Therapy Modalitiessheila roma sibugОценок пока нет
- Unlocking The Prediction of Preeclampsia, A Widespread, Life-Threatening Pregnancy ComplicationДокумент5 страницUnlocking The Prediction of Preeclampsia, A Widespread, Life-Threatening Pregnancy ComplicationImam SantosoОценок пока нет
- Rare autoimmune skin disease in pregnant 15-year-old: A case reportДокумент5 страницRare autoimmune skin disease in pregnant 15-year-old: A case reportsri karuniaОценок пока нет
- Obat-Obat Baru 2010Документ262 страницыObat-Obat Baru 2010UdtjeVanDerJeykОценок пока нет
- Physiology of LaborДокумент49 страницPhysiology of LaborGunung MahameruОценок пока нет
- Marlene JordanДокумент2 страницыMarlene Jordanapi-121407787Оценок пока нет
- The Bozola Flap in Oral Cavity Reconstruction PDFДокумент4 страницыThe Bozola Flap in Oral Cavity Reconstruction PDFPorcupine TreeОценок пока нет
- Bedaquiline TB PDFДокумент2 страницыBedaquiline TB PDFHana Fauzyyah HanifinОценок пока нет
- Sebaceous Hyperplasia Treatment With Combination oДокумент2 страницыSebaceous Hyperplasia Treatment With Combination oAndreОценок пока нет
- AripiprazolДокумент12 страницAripiprazolGabriel LemosОценок пока нет
- What Are The Causes of Albinism?Документ15 страницWhat Are The Causes of Albinism?Viviana VarelaОценок пока нет
- Evidence Based Medicine BlepharoplastyДокумент11 страницEvidence Based Medicine Blepharoplastycarlitos1207Оценок пока нет
- Prescription vs OTC Drug RisksДокумент19 страницPrescription vs OTC Drug Risks19-28 Manan PopatОценок пока нет
- L Carnosine in ADHDДокумент8 страницL Carnosine in ADHDVivekОценок пока нет