Академический Документы
Профессиональный Документы
Культура Документы
405 P
Загружено:
api-2535982600 оценок0% нашли этот документ полезным (0 голосов)
25 просмотров11 страницОригинальное название
405p
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
25 просмотров11 страниц405 P
Загружено:
api-253598260Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 11
"#$%&'()*%# +,-.
(#/0 10(' 2*#(3
4&%50-)
Information Exchange Team Project: Final
Group 3 Topic 1
Northwestern University
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
Transition-of-care has become a hot-button issue in healthcare. The reasons for this are
multifaceted. Current initiatives (HITECH, ACA) are directed at improving the quality and lowering the
cost of healthcare to all. This focus has caused some very troubling and costly issues to bubble to the
surface; these issues must be addressed. The costs are in dollars and human lives. Two of the top issues are
preventable readmissions and medication errors. Providers, hospitals and nursing facilities are all
aggressively working to address both of these issues. One approach is to better manage the transition of
care via improved care coordination between all parties involved in the transition.
These problems and their potential solutions are addressed in the Meaningful Use Stage 2 requirements
below:
Stage 2 Transition-of-Care (TOC) Measures
Measure 1
The EP, eligible hospital or CAH that transitions or refers their patient to another setting of care or
provider of care provides a summary-of-care record for more than 50% of transitions-of-care and
referrals.
Measure 2
The eligible provider (EP), eligible hospital (EH) or critical access hospital (CAH) that transitions or
refers its patient to another setting-of-care or provider-of-care provides a summary-of-care record for
more than 10% of such transitions and referrals either:
1. electronically transmitted using certified electronic health record technology (CEHRT) to a
recipient; or
2. via exchange facilitated by an organization that is an eHealth Exchange participant, the recipient
receives the summary-of-care record.
Measure 3
An EP, eligible hospital or CAH must satisfy one of the two following criteria:
1. Conducts one or more successful electronic exchanges of a summary-of-care document, which is
counted in "measure #2," with a recipient who has EHR technology that was designed by a
different EHR technology developer than the sender's EHR technology, or
2. Conducts one or more successful tests with the CMS-designated test EHR during the EHR
reporting period.
Transition-of-care measures must be met by eligible providers and hospitals by either utilizing a
health information exchange or by having the capability to send and receive a CCDA document via Direct
or SOAP+XDR/XDM transport (as a Health Information Organization or HIO).
This project focuses on the continuity-of-care document (CCD) as a means to improve care
coordination at transitions-of-care. If the CCD were made available to those entities and providers
involved in the care of the patient, errors could be avoided, coordination would be improved, and costs
associated with suboptimal information flow could be reduced.
The proposed system is one to exchange continuity of care documents (CCD) to outlying small
physician clinics and regular/skilled nursing facilities. Our scenario involves a community hospital with a
fairly rigorous EMR implementation that has the capability of producing CCDs. Continuity-of-care is
very important, so the emergency room (ED) would like to provide information back to the primary care
provider and/or nursing facility-of-origin.
The intent here is to describe the pertinent stakeholders and their roles, describe and clarify the
proposed flow-of-information and architecture, and detail the data to be exchanged and the standards for
that exchange. Analysis of the potential challenges associated with this proposed solution are included and
summarized.
Stakeholders
Identifying stakeholders is a very important aspect of any project. Analyzing stakeholders allows
for systematic insight into positive and negative impacts of the project. It also may assist in identifying
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
persons or entities that may support or block implementation. Identifying persons that may have an
investment in the project also allows for careful planning while contemplating a project, preparing for
implementation, implementing the project itself, and continuing through to its maintenance. Stakeholder
analysis can only be done after the base project is defined so that appropriate stakeholders can be identified
and queried regarding their perception of its potential impact.
Important questions to ask when identifying stakeholders are:
1. Who is impacted?
2. Who will require new skills?
3. Who/what are the barriers or issues?
4. What is the potential for resistance?
The intent here is, first, to generate a list of potential stakeholders and then, to expand upon that list in
more detail to assist with change management, planning and implementation in order that the project will
be optimally implemented. Whether a stakeholder is key or secondary is a matter of perspective.
Financially, the CEO and CFO are primary; technologically, IT personnel would be primary. This analysis
is from a patient- centered perspective and thus is clinically- centered.
Key Stakeholders: Patients and their families, Emergency Department personnel (nurses and providers),
primary care providers and nursing/medical assistants, nursing facility personnel (DON, RN, LPN, CNA).
Secondary Stakeholders: CEO, CFO, Hospital Directors of Operations, Emergency room directors,
Directors of IT, IT department personnel, vendor personnel, Nursing Home Administrators, primary care
clinic managers.
Tertiary Stakeholders: Federal, State and local government bodies interested in improvements in
interoperability, efficiency and population health.
Each stakeholder has his or her own perspective. They are impacted in different ways and have
impacts of their own on the project. It is useful to explore a few of these as they pertain to this project.
Primary stakeholders are those that are impacted clinically by this project. First and foremost, the
patient and his or her family are affected. The information exchanged pertains to the particular patient,
including his or her medical history, diagnoses and care. The entire purpose of improved interoperability is
to provide enhanced care to patients. Ensuring important medical details are not lost with transitions-of-
care has been an important focus over the last several years. This project takes aim at improving the
shortfalls of our current system by improving the completeness and fidelity of patient health information
through transitions-of-care. The providers on either side of the transitions make up the balance of the key
stakeholders. They need this information to appropriately care for the patient. Having accurate,
dependable information is key to optimal care. There should be few new skills required on either side of
the transition but the recipient may need some rudimentary training in accessing the documents. Having
complete information should result in minimal, if any, resistance other than that typically seen with the
implementation of any new technology.
Secondary stakeholders here are those that control the financials or the institutions that stand to
gain from meaningful use incentives unlocked by this mandatory functionality, or those necessary to
approve any aspect of the action or maintenance phase of the implementation. Clearly, administrative
support will be required at all points-of-care. Information technology (IT) personnel would be involved in
and key to many portions of the implementation. Cost is always a potential barrier; however, the intention
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
here is to create an implementation that is inexpensive. IT will always be cautious from a security
standpoint until it is clear that any security risks have been adequately addressed.
Tertiary stakeholders are listed here for completeness. They have no direct involvement in the
project although the big picture suggests this would assist in fulfilling their strategic vision of health
information interoperability locally, at the state level and nationwide.
Potential Challenges
All health information technology projects face challenges. This project has a few technical
challenges to overcome, but the real tasks are in the approval process, coordinating activities among three
disparate entities, and data security.
First and foremost, the project must be presented to those with final approval authority, which will
often be the leadership team. This team can consist of the CEO, CFO, CIO, General Counsel, and Vice
President of Clinical Operations. Cost is often the primary concern coupled at times to operational
improvement. Being compliant, adhering to regulations, improving patient safety, and/or meeting a
Meaningful Use stages criteria can overshadow financial concerns. This project, however, has a lower
financial commitment but a potentially higher return for process improvement, patient safety, and
satisfaction of a sizable portion of Meaningful Use Stage 2 requirements.
Once the project has been approved, other pre-implementation and implementation challenges
come into play. Information Technology organizations are perennially understaffed and overcommitted
because of projects and day-to-day operational activities. Having the CIO in the initial stakeholder meeting
is crucial. He or she can take back to the organization an understanding of the project and begin working
with team leads on the reprioritization of other projects to accommodate this project. Since this project
requires cooperation among three different entities, an IT and a clinical liaison will be necessary for
coordination and communication. A cross-disciplinary group will be assembled from staff in the
administration, IT and clinical areas, and will also require a program lead who has an overall understanding
of the process and an ability to communicate to both technical and non-technical people.
Technical challenges would likely be minimal on the hospital side. HL7 and CCD architectures
are fairly mature within the Community Medical Center (HIMMSS 6). The Medical Clinic uses a SaaS-
model EMR and has a fairly mature processes and capabilities. The TCC is the most remedial in
technological and employee capability. Since the TCC EMR is very basic and there is no HL7 interface
capability, receiving and sending the CCD via e-mail appears to be a viable solution. The challenge will be
to find a secure HIPAA compliant e-mail solution (e.g. www.hightail.com) that meets all of the
requirements of this project.
Information Flow and Architecture
The patients CCD information will be bi-directionally transmitted among three entities the
Community Medical Center (CMC), a small medical clinic, and a Transitional Care Center (TCC). A
hybrid data transfer model will be employed because not all of the providers support HL7 messaging
(Example 1). The CMC has a complete EMR and an interface engine, which is capable of HL7 messaging
and data transformation. The small medical clinic uses the SaaS model of eClinicWorks, which is also
capable of sending and receiving a HITSP C32 standardized CCD in HL7 message format (Example 2).
The TCC employs a minimal home-grown EMR and a DOS-based pharmacy system, which is only
capable of importing and exporting pre-defined formatted text files (Example 3). The process the TCC will
use, when sending a patient to the CMC Emergency Department (ED), is rather cumbersome, but necessary
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
because of system limitations. A TCC staff member will export a CCD text file from the basic EMR and
securely e-mail/upload it to a secure HIPAA-compliant e-mail/file site (i.e. HighTail). The hospitals
interface engine will poll this repository frequently for the retrieval of the TCC CCD, which will then be
transformed into an HL7 message for submission to the CMC EMR. Upon the patients discharge back to
the TCC, the CMC EMR interface engine will transform the Community Medical Center CCD into a text
file and securely e-mail it to the same service used by the TCC. A TCC HIM employee will receive an e-
mail notifying them that a CCD has been sent, whereupon the CCD will be downloaded and subsequently
uploaded to the TCCs rudimentary EMR (Example 1). Simultaneously, the CMC transmits an HL7-
formatted CCD to the Medical Clinic for the doctor to review. This is particularly important because the
medical clinic doctor would not otherwise know the patient was sent to the ED, nor what had transpired
there.
TCC sends
patient to
Community
Medical Center
EMR
TCC exports CCD
Txt file/securely
emails to CMC
CMC IE
retrieves
TCC CCD/
transforms
to HL7 msg
for EMR
Patient treated
and discharged
from CMC
CMC Staff
refer to TCC
CCD
CMC staff enter
data into EMR &
complete CCD
CMC IE
securely
emails
CCD in TXT
to TCC &
HL7 to
medical
clinic
TCC dwnlds CCD
txt file from
secure site/
imports into EMR
Med Clinic
receives
CCD HL7
msg/posts
in EMR
Internet
TCC
EMR/Pharmacy
Secure
Email Service
Community Medical
Center EMR
Page 1
Continuity of Care Document Data Flow
Example 1
November 10, 2013
Medical Clinic
EMR
VPN Tunnel
CCD Text File
Interface
Engine (IE)
Firewall
Interface
Engine (IE)
Bi-directional HL7
Messages
CCD Text File
Firewall
Firewall
Community Medical Center:
1. Bi-directional HL7 interface for CCD to MC
2. CCD transmitted to TCC via a secure email
service. IE transforms data in HL7 for EMR
posting.
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
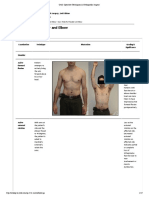
Golden Valley Medical Clinic -- Continuity of Care Document
(Example 2)
Created On: November 8, 2013
Patient: Johnny EMRTest III
1234 Emrdrive.
Lowry City, MO 64763
tel:+1-417-644-2600
MRN: 110589
Birthdate: March 31, 1960 Sex: Male
Guardian: Next of Kin:
Allergies/Adverse Reactions
Description Reaction Type Severity Date
Bee Sting SWELLING Adverse Reaction Severe
Glucophage(metformin) DIARRHEA Drug Allergy Moderate
Diagnostic Test Results
Lab Results:
Test Result Units Reference Range Date
EPITHELIAL CELLS: 10 - 25 EPI/LPF 07/08/2013
SPUTUM CULUTRE Culture set up 07/08/2013
Antibody Identification Anti-K (KELL SYSTEM) 07/01/2013
Immunizations
Vaccine Administration Date
Flu vaccine no preserv 3 & > 06/01/2012
(entries deleted to abbreviate example)
Medications
Description Dose/Frequency Quantity
Date
Prescribed
Date
Expired
Provider
Prednisone 10 MG Oral
Tablet
1 Once a day 5 08/27/2013
Mazal,
Benjamin
Prednisone 5 MG Oral
Tablet
1 Once a day 5 08/27/2013
Mazal,
Benjamin
Procedures
Description Code Date Provider
AIRWAY INHALATION TREATMENT 94640 05/11/2011 Dailey, William
ANTINUCLEAR ANTIBODIES 86038 11/14/2011 Bagley, Brendan
Significant Diagnoses
Description Code Date Provider
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
Description Code Date Provider
Venus embo&thromb uns dp ves lw ext 453.40 04/05/2013 Ali, Abul Fazal
(Example 3)
GOLDEN VALLEY TCC -- CONTINUITY OF CARE DOCUMENT
Created On: November 8, 2013
MRN: 110589
Patient: Johnny EMRTest III
1234 Emrdrive
Lowry City, MO 64763
tel: 417-644-2600
Birthdate: March 31, 1960
Sex: Male
Guardian:
Next of Kin:
ALLERGIES/ADVERSE REACTIONS
- Description/Reaction/Type/Severity/Date:
- Bee Sting, Swelling, Adverse Reaction, Severe
DIAGNOSTIC TESTS RESULTS
Lab Results: Test/Result/Units/Reference Range/Date:
- EPITHELIAL CELLS:,10 - 25 EPI/LPF, , ,07/08/2013
- SPUTUM CULUTRE, Culture set up, , ,07/08/2013
- Antibody Screen, POSITIVE, , ,07/01/2013
Immunizations: Vaccine/Administration Date:
- Flu vaccine no preserv 3 & >, 06/01/2012
MEDICATIONS:Desc/Dose/Freq/Quantity/DatePresc/DateExp/Provider:
- Prednisone 10 MG Oral Tablet 1, Once a day, 5, 08/27/2013, ,Mazal, Benjamin
- Prednisone 5 MG Oral Tablet 1, Once a day 5, 08/27/2013, ,Mazal, Benjamin
PROCEDURES:Desc/Code/Date/Provider:
- AIRWAY INHALATION TREATMENT, 94640, 05/11/2011, Dailey, William
- ANTINUCLEAR ANTIBODIES, 86038, 11/14/2011, Bagley, Brendan
SIGNIFICANT DIAGNOSES:Desc/Code/Date/Provider:
- Venus embo&thromb uns dp ves lw ext, 453.40, 04/05/2013, Ali, Abul Fazal
Data to be exchange and standards to be used
The CCD contains each of the key portions of a summary-of-care document; the sections contents
are dictated by the standards mandated for those areas. This makes the task of finding interoperable
solutions more feasible. The first portion that was considered when the CCD was designed is the
medication history, which conforms to Healthcare Information Technology Standards (HITSP) C32 criteria
(Phansalkar et al, 2009). Specifically, HITSP C32 represents a collection of terminologies including the
NLMs RxNorm for clinical drugs, the FDAs Unique Ingredient Identifiers (UNIIs) for ingredient name,
the FDAs Dosage Form, FDA Route of Administration, Unified Code for Units of Measure (UCUM) for
dose units of measure, and the Department of Veterans Affairs National Drug File Reference
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
Terminology (NDF- RT) for drug classes (Phansalkar et al, 2009). These specifications allow clinicians to
include information on a medications route, dosage form, frequency, interval and dose units of measure
(Phansalkar et al, 2009). Beyond these details, the CCD includes discrete elements such as date dispensed,
RxNorm clinical drug name, quantity dispensed, pharmacy where dispensed, (and) prescriber name
(Simonaitis et al, 2010). The utility of the CCD stems from its abilities to represent drug data in a common
format and to deliver medication data, reasonably quickly, to ambulatory care physicians (Simonaitis et
al, 2010).
Employing the RxNorm terminology standard also gives the CCD writer the ability to consolidate
medications using categorizations such as Semantic Clinical Drug (SCD), Semantic Clinical Drug Dose
Form (SCDF) or an Ingredient (IN) (Phansalkar et al, 2009). Newer iterations were designed with greater
interoperability in mind; information systems have been constructed to generate CCDs, whose format also
enables institutions to move easily from paper to electronic records (Simonaitis et al, 2010). The CCD
structures data in XML format and can translate National Drug Codes into RxNorm SCDs; clinicians are
able to represent medications in the way clinicians prescribe medications (Simonaitis et al, 2010). The
opposite was also achieved by using the CCD to provide clinicians with RxNorm Clinical Drug displays;
then, CCDs were expanded upon to include laboratory test results (Simonaitis et al, 2010). Technological
innovations allow for step-by-step data transformations such as using a (Saxon XSL) Transformation
Engine (to) apply an XSLT stylesheet to the CCD to generate a tree of formatting objects and an (Apache
FOP) Formatting Engine (to) convert this tree into a PostScript file when transferring data (Simonaitis et
al, 2010). Conversely, the CCD can be transformed by an XSLT stylesheet to a printed format; this
Level 2 CCD- with unstructured text- is sufficient to meet the certification criteria for Stage 1 of
Meaningful Use (Simonaitis et al, 2010). Thus, current CCDs are modeled in accordance with the 2008
CCHIT certification criteria requiring EHRs to demonstrate the ability to file and display, as well as
generate, Continuity of Care Documents (Phansalkar et al, 2009).
The latest versions, known as Level 3 CCDs which are based on HITSP C83 specifications, now
contain problem lists and allergy lists, including such details as time of onset, current status, units of
measurement, dosing interval, severity and result interpretation, (although) unfortunately, the C32 construct
leaves most of the associated data (including hospitalizations and procedures) as optional (DAmore et al,
2011). For this information, SNOMED-CT and ICD-9 codes are employed, and recent history points to the
fact that more standard vocabularies (will be) endorsed for clinical modules of the CCD (DAmore et al,
2011). Our model makes use of recent developments including a CCD-based clinical data warehouse
(that) requires only a shared, secure server for integrated care teams to extract XML documents (DAmore
et al, 2011). The goal is to achieve the ability to share comprehensive CCDs through MU-standardized
databases and tailor the interfaces to different EMR systems, so that these systems can be integrated with
future models for health information exchanges (that) could also be potential aggregators of CCD-based
clinical content (DAmore et al, 2011). We felt justified in using this technology because the CCD
conforms to database rules and business query logic used to accommodate multiple vocabularies
(DAmore et al, 2011). However, we also agree that our project could benefit from a single document
including all standards, structures and vocabularies without reference to external sources (DAmore et al,
2011).
More Local Challenges and Future
All health information technology projects face challenges. The challenges discussed here center
primarily around project acceptance and planning. Challenges are dependent on perspective and parallel
the stakeholder issues. Rarely are technological hurdles particularly difficult to overcome. True challenges
are nearly always financial, social and cultural.
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
First and foremost, the project must be presented to those that can approve the project. In my
organization, this would be the administrative team. This team consists of the CEO, the Director of
Clinical Operations, the CFO and the Director of Nursing Operations. We have a strong CEO who makes
most of the decisions within the context of this team. Usually those kinds of decisions require a sound
financial analysis although in the context of meeting Stage 2 requirements this is usually glossed-over
somewhat, as long as we are within the budgeting cycle and the project is consistent with our vision and
strategy. The administrative challenges can be paramount and can keep even the best-planned and
presented project from even moving anywhere near change management. Many projects never get beyond
this step.
Making the assumption that this project was to get beyond the Admin Team, there would be
further significant pre-implementation and implementation challenges. IT would have to figure-out a way
to support the project amidst the numerous Stage 2 projects already underway. There would likely be a
myriad of IT personnel-support issues to deal with. Our IT department can do a fair job of controlling
equipment and resources within our healthcare system, but when it comes to interfacing with other
organizations, we will have major challenges. This project is going to require the cooperation of our
hospital with numerous outlying physician clinics and nursing facilities. This is not the kind of project
where you could simply send an e-mail to an organization and it would automatically be ready to receive it.
Significant resources will have to be put into working with the numerous entities to prepare them for this
kind of exchange. While IT departments possess the technical expertise, they fall far short of the requisite
skills necessary to coordinate with the numerous clinic managers and IT leaders of other organizations.
This would require a multidisciplinary approach, made possible by a blended clinical, administrative and IT
team. The team would be mandated to conduct focused discussions with primary and secondary
stakeholders at their organizations and would be required to possess significant change management skills.
This resembles the hospital admin approval process but would be on a per-entity basis. An alternative
approach would be to pick one or two key nursing facilities or physician practices as pilots and then, once
they are up-and-running, it could expand from there as other organizations chose to opt-in.
While technical challenges will likely be minimal on the hospital side, nearly all of the technical
challenges will be associated with the heterogeneity in outlying entity technology. Although all of the
clinics and nursing facilities have computers, many (especially the nursing facilities) do not have anything
beyond e-mail capabilities. Certainly, certificates would have to be obtained for authentication and
encryption. Third party vendors (EMRDIRECT) may have to be employed to support the secure e-mail.
Many of these vendors facilitate obtaining certificates to decrease the inertia associated with such projects.
This particular vendor has a web-mail based product, which would permit bypassing of almost all of the
details of local authentication/encryption within the least technologically advanced organizations.
Clearly, this project is merely a gap-filler. The future should provide much more robust systems
allowing true interoperability and should move toward patient data omniscience. The vision of being able
to know everything that is medically relevant, regardless of whoever the patient is who sits before us, is a
noble one and is worthy of pursuit. Realizing that vision, at some time in an uncertain future, will require
building block projects like this one to provide the foundation for trust, the evidence of benefit and,
hopefully, the cost reduction. Those very benefits will continue to drive medical data science well into the
future.
Conclusion
This project aims at solving a very difficult problem. That problem is incomplete, inaccurate
information at transitions of care. A simple inaccuracy such as a missed furosemide frequency could easily
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
result in a preventable readmission of a CHF patient. Simple missed instructions, like daily weights, could
have a similar outcome. Information that is lost in translation can cause financial implications for
stakeholders and result in avoidable morbidity and mortality imposed upon the most important stakeholder,
the patient.
This problem is not unique to this community. Technical issues are easily surmountable for a
project of this scale. The cultural issues of buy-in, cooperation and coordination with unaffiliated
community physicians and nursing facilities will be the real challenge. The common thread has to be
stressed in all negotiations, standard of care and patient safety. When distilled to this most fundamental
tenet of medicine, most resistant stances should become quickly untenable. The macro- and micro- scale
issues discussed are repeated in communities, hospitals, nursing homes and physician practices nationwide.
Each community and hospital will likely take a similar path until HIEs are operational and appropriately
utilized across the country. The benefits to the patients should be equally widespread.
"#$%&'()*%# +,-.(#/0 10(' 2*#(3
4&%50-)
References
DAmore, J. D., Sittig, D. F., Wright, A., Iyengar, M. S., & Ness, R. B. (2011). The promise of the CCD:
challenges and opportunity for quality improvement and population health. In AMIA Annual
Symposium Proceedings (Vol. 2011, p. 285). American Medical Informatics Association.
Morris, G., Afzal, S., & Finney, D. (2013, April 26). Key Considerations for Health Information
Organizations Supporting Meaningful Use Stage 2 Transition of Care Measures. Retrieved from
http://www.himss.org/ResourceLibrary/ResourceDetail.aspx?ItemNumber=21384
Phansalkar, S., Robinson, G., Getty, G., Shalaby, J., Tao, D., & Broverman, C. (2009). Challenges in
exchanging medication information: identifying gaps in clinical document exchange and
terminology standards. In AMIA Annual Symposium Proceedings (Vol. 2009, p. 526). American
Medical Informatics Association.
Simonaitis L., Belsito A., Cravens G., Shen C., & Overhage J. M. (2010). Continuity of Care Document
(CCD) Enables Delivery of Medication Histories to the Primary Care Clinician. In AMIA Annual
Symposium Proceedings (Vol. 2010, p. 747). American Medical Informatics Association.
Вам также может понравиться
- 404 RДокумент1 страница404 Rapi-253598260Оценок пока нет
- Administrator (Administrator#)Документ26 страницAdministrator (Administrator#)api-253598260Оценок пока нет
- 409 PДокумент9 страниц409 Papi-253598260Оценок пока нет
- 409 RДокумент1 страница409 Rapi-253598260Оценок пока нет
- 317 RДокумент1 страница317 Rapi-253598260Оценок пока нет
- 405 RДокумент1 страница405 Rapi-253598260Оценок пока нет
- Administrator (Administrator#)Документ26 страницAdministrator (Administrator#)api-253598260Оценок пока нет
- 317 RДокумент1 страница317 Rapi-253598260Оценок пока нет
- 406 PДокумент39 страниц406 Papi-253598260Оценок пока нет
- 406 RДокумент1 страница406 Rapi-253598260Оценок пока нет
- 404 PДокумент25 страниц404 Papi-253598260Оценок пока нет
- 403 PДокумент5 страниц403 Papi-253598260Оценок пока нет
- 403 RДокумент1 страница403 Rapi-253598260Оценок пока нет
- 481 PДокумент12 страниц481 Papi-253598260Оценок пока нет
- 407 RДокумент1 страница407 Rapi-253598260Оценок пока нет
- 1 Part 2 Final: Cloud-Based GIS Maps Displaying Aggregate Data On Medical MalpracticeДокумент11 страниц1 Part 2 Final: Cloud-Based GIS Maps Displaying Aggregate Data On Medical Malpracticeapi-253598260Оценок пока нет
- 481 RДокумент1 страница481 Rapi-253598260Оценок пока нет
- 408 PДокумент36 страниц408 Papi-253598260Оценок пока нет
- 408 RДокумент1 страница408 Rapi-253598260Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Documentation Sheet Sterilization EnglishДокумент2 страницыDocumentation Sheet Sterilization EnglishBanita CarmenОценок пока нет
- Giant Cell Tumor of Bone - An Overview: Current Concepts ReviewДокумент8 страницGiant Cell Tumor of Bone - An Overview: Current Concepts ReviewDwi fitria nivaОценок пока нет
- Product PlanДокумент19 страницProduct Planlily30109150% (2)
- Safety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingДокумент11 страницSafety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingShahid BhattiОценок пока нет
- Role of Hospital Pharmacist in Handling Radio Active SubstanceДокумент5 страницRole of Hospital Pharmacist in Handling Radio Active SubstanceAashish BhattaraiОценок пока нет
- Taylan Competency NeedsДокумент32 страницыTaylan Competency NeedsLovejoice Cha NnelОценок пока нет
- Adver PaperДокумент10 страницAdver PaperDee Jay de JesusОценок пока нет
- PДокумент3 страницыPPamela GuevaraОценок пока нет
- MoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Документ31 страницаMoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Steven SsemwangaОценок пока нет
- 2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationДокумент66 страниц2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationMoises Torres AlvarezОценок пока нет
- Risk Management Plan TemplateДокумент10 страницRisk Management Plan Templateamit singh0% (1)
- Pathologist Job SpecificationДокумент16 страницPathologist Job SpecificationLalaluluОценок пока нет
- Aspiracion Destornillador Implanto Roa-V1-Id1018Документ3 страницыAspiracion Destornillador Implanto Roa-V1-Id1018CesarAmorotoОценок пока нет
- Human Rights (ROTC)Документ6 страницHuman Rights (ROTC)shujin_samaОценок пока нет
- Nursepreneurs Essay by J. BacarisasДокумент17 страницNursepreneurs Essay by J. BacarisasCris GalendezОценок пока нет
- Applying A Feminist Lens To Indias Foreign Policy A Compendium of EssaysДокумент124 страницыApplying A Feminist Lens To Indias Foreign Policy A Compendium of EssaysRasced AliОценок пока нет
- Blue Green Yellow Modern English Intrapersonal Communication Educational Presentation - 20231109 - FixДокумент12 страницBlue Green Yellow Modern English Intrapersonal Communication Educational Presentation - 20231109 - FixmhailvandalzОценок пока нет
- Exam Table For Shoulder and ElbowДокумент17 страницExam Table For Shoulder and ElbowLouie OkayОценок пока нет
- BAYBAY AwardsДокумент63 страницыBAYBAY AwardsClennil Palmes SustraidoОценок пока нет
- 2021 A Guide To The African Human Rights System Celebrating 40 YearsДокумент115 страниц2021 A Guide To The African Human Rights System Celebrating 40 YearsChala Yuye KemerОценок пока нет
- Ejsr Vol 97 Issue 1 159 171Документ171 страницаEjsr Vol 97 Issue 1 159 171Raja ChandruОценок пока нет
- Antimicrobial Products-Test For Antimicrobial Activity and EfficacyДокумент14 страницAntimicrobial Products-Test For Antimicrobial Activity and EfficacyherfuentesОценок пока нет
- POCSOДокумент15 страницPOCSOThakur Avnish Singh100% (1)
- Internet Addiction - ResearchДокумент13 страницInternet Addiction - ResearchpipedsОценок пока нет
- Genesis Platinum Manual 8090Документ23 страницыGenesis Platinum Manual 8090Huni BuniОценок пока нет
- UConn Prosthodontics Clinic Manual 12-13Документ69 страницUConn Prosthodontics Clinic Manual 12-13lippincott2011Оценок пока нет
- Vulture ConservationДокумент14 страницVulture ConservationSaba Parvin Haque100% (2)
- Review Jurnal Varicella - Dewi Manik Aulia Fadli - 16700096Документ26 страницReview Jurnal Varicella - Dewi Manik Aulia Fadli - 16700096Lia FadliОценок пока нет
- Understanding and Completing The Reversion (25pp)Документ25 страницUnderstanding and Completing The Reversion (25pp)Tony Lambert100% (3)
- Minimall Tooth Preparation Garil GurelДокумент13 страницMinimall Tooth Preparation Garil GurelMónica BecerraОценок пока нет