Академический Документы
Профессиональный Документы
Культура Документы
Suboxone - Notes For Pharmacists
Загружено:
garima_montu0 оценок0% нашли этот документ полезным (0 голосов)
58 просмотров1 страницаNapra Guide
Оригинальное название
Suboxone - Notes for Pharmacists
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документNapra Guide
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
58 просмотров1 страницаSuboxone - Notes For Pharmacists
Загружено:
garima_montuNapra Guide
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 1
SUBOXONE (BUPRENORPHINE/NALOXONE) IMPORTANT PRACTICE NOTES FOR PHARMACISTS
1. Who can prescribe Suboxone (buprenorphine/naloxone)?
Health Canada grants federal exemptions to physicians for methadone prescribing, with provincial
supervision performed by the College of Physicians & Surgeons. Conversely, the criteria and requirements
necessary to obtain an exemption to prescribe Suboxone is determined by the provincial medical colleges.
In Manitoba, it is necessary for the physician to hold a methadone exemption, take a 6 hour on-line
Suboxone course, and apply to the College of Physicians & Surgeons of Manitoba. The College of
Physicians & Surgeons of Manitoba keeps an updated list of physicians who can prescribe methadone and
Suboxone. It is the responsibility of the dispensing pharmacist to verify that the prescribing physician has
the appropriate exemption. This information can be confirmed by calling the MPhA Office at
(204)233-1411.
2. How is buprenorphine/naloxone different from methadone?
Buprenorphine/naloxone comes in the form of a sublingual tablet. Witnessing of doses is necessary, just
like methadone, as per the contract between patient, clinic and pharmacy. It may take 2 to 3 minutes for
the tablet to dissolve.
The pharmacological properties of buprenorphine can cause precipitated withdrawal syndrome if
administered to an individual who has taken a sufficient dose of a full agonist opioid and is physically
dependent on opioids. Therefore the correct timing and dosage of buprenorphine/naloxone according to
the patients last dose of opioid is important.
The purpose of including naloxone with buprenorphine is to prevent inappropriate IV usage. Rapid
binding of naloxone to the mu-opioid receptor precipitates a rapid opioid-withdrawal syndrome when
injected. Pharmacists should caution patients on this effect.
Buprenorphine is longer acting than methadone and therefore some patients may be able to take it three
times a week rather than daily.
Buprenorphine has a ceiling effect so doses over 24 mg are unlikely to be beneficial.
Most patients report fewer side effects on buprenorphine/naloxone (less sedation, less constipation,
more normal sexual function) and the risk of death from over-sedation is less than with Methadone.
Fatalities due to respiratory depression have occurred when buprenorphine was used in combination with
CNS depressants such as benzodiazepines, alcohol, or other opioids. The pharmacist must always assess
the patient with respect to other drug and medication use prior to providing buprenorphine/naloxone.
3. Contact with the Prescribing Practitioner
Pharmacies must contact the patients primary healthcare provider/prescriber if major behavioral
difficulties are observed (sedation, missing repeated doses) and dosages missed. If a patient misses more
than 5 doses, the prescription must be cancelled and the patient must contact the clinic staff in order to
resume buprenorphine/naloxone.
4. Education
A free six hour accredited professional development program covering the treatment of opiate dependent
patients with buprenorphine/naloxone is available online at www.suboxonecme.ca. The Manitoba
Pharmaceutical Associations Principles for the Provision of Methadone by Manitoba Pharmacists
Certificate Program is offered periodically throughout the year and also briefly reviews treatment with
buprenorphine/naloxone. Many other opioid dependence treatment training programs are available in
Canada. Pharmacists are encouraged to contact Kim McIntosh, Assistant Registrar at the MPhA office
(204)233-1411 ext 230, to discuss further resources.
Вам также может понравиться
- Physicians Desk Reference (PDR) For Pain ManagementДокумент285 страницPhysicians Desk Reference (PDR) For Pain ManagementDante36100% (2)
- Opiate Guideline DetoxДокумент32 страницыOpiate Guideline DetoxboboОценок пока нет
- Medication Assisted Treatment 9-21-20121Документ6 страницMedication Assisted Treatment 9-21-20121GodstruthОценок пока нет
- Vivitrol TreatmentДокумент8 страницVivitrol TreatmentHarish RathodОценок пока нет
- Stimulant Use Disorder Assignment 2Документ15 страницStimulant Use Disorder Assignment 2Nathan MalamboОценок пока нет
- Medication Classes Cheat SheetДокумент2 страницыMedication Classes Cheat SheetJoax Wayne SanchezОценок пока нет
- Buprenorphine: Potential For AbuseДокумент8 страницBuprenorphine: Potential For Abuselosangeles100% (1)
- High Dose Methadone To Buprenorphine Transfer NHS Scottland PDFДокумент1 страницаHigh Dose Methadone To Buprenorphine Transfer NHS Scottland PDFohenriquezОценок пока нет
- Subutex Quick-Start-GuideДокумент6 страницSubutex Quick-Start-GuideDanОценок пока нет
- Wilmont's Drone Delivery Project ScopeДокумент3 страницыWilmont's Drone Delivery Project Scopegrg67% (3)
- 10-Implementing Policies and ProceduresДокумент56 страниц10-Implementing Policies and ProceduresMelai Rodriguez IbardalozaОценок пока нет
- A Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsОт EverandA Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Directory NPAДокумент1 934 страницыDirectory NPAAnonymous qWY12CYlmОценок пока нет
- Nitrofurantoin Drug StudyДокумент11 страницNitrofurantoin Drug StudyNicole Keesha MataОценок пока нет
- Total Parenteral Nutrition (TPN) PDFДокумент8 страницTotal Parenteral Nutrition (TPN) PDFMohamad SamirОценок пока нет
- Buvidal PDF 1158123740101Документ7 страницBuvidal PDF 1158123740101riffs_ahoyОценок пока нет
- Long Acting Injectable Buprenorphine Brief Clinical Guidelines 2Документ18 страницLong Acting Injectable Buprenorphine Brief Clinical Guidelines 2jasondominik91Оценок пока нет
- A Quick Reference For Managing Buprenorphine in The Perioperative SettingДокумент3 страницыA Quick Reference For Managing Buprenorphine in The Perioperative SettingJackieОценок пока нет
- OTP Protocol PharmacistsДокумент14 страницOTP Protocol PharmacistsericОценок пока нет
- PerioperativeДокумент15 страницPerioperativeJEFFERSON MUÑOZОценок пока нет
- Mat Presentation 1Документ23 страницыMat Presentation 1api-649066372Оценок пока нет
- Buprenorphine Management: DR Brenda Mogaka Ngara MAT Pharmacy LeadДокумент25 страницBuprenorphine Management: DR Brenda Mogaka Ngara MAT Pharmacy LeadJared KeburiОценок пока нет
- ZOMORPH Capsules 10mgДокумент6 страницZOMORPH Capsules 10mgFlorexan Malanday PasonОценок пока нет
- UTMB Food-Drug Interaction PolicyДокумент3 страницыUTMB Food-Drug Interaction PolicynatalikascribdОценок пока нет
- Pro Re Nata (PRN) Medication: PurposeДокумент4 страницыPro Re Nata (PRN) Medication: PurposeF̳̿a̳̿l̳̿a̳̿h̳̿ Opcional S̳̿u̳̿d̳̿i̳̿r̳̿a̳̿d̳̿i̳̿r̳̿e̳̿j̳̿a̳̿Оценок пока нет
- Orig 1 S 000 Cross RДокумент29 страницOrig 1 S 000 Cross RDon RedbrookОценок пока нет
- Intra Muscular Injection PDFДокумент19 страницIntra Muscular Injection PDFmarie0208Оценок пока нет
- Benzodiazepine and Hypnotic Guidelines (V1.0 July 2010)Документ18 страницBenzodiazepine and Hypnotic Guidelines (V1.0 July 2010)Deza IngridОценок пока нет
- Buprenorphine HydrochlorideДокумент3 страницыBuprenorphine Hydrochlorideapi-355433171Оценок пока нет
- Opioid Analgesics: Dosage Instructions, Side-Effects, Contra-Indications and WarningsДокумент6 страницOpioid Analgesics: Dosage Instructions, Side-Effects, Contra-Indications and WarningsteddypolОценок пока нет
- CPSBC Practice Standard on Safe Prescribing of Opioids and SedativesДокумент4 страницыCPSBC Practice Standard on Safe Prescribing of Opioids and SedativesSteve GreenОценок пока нет
- Agitation, Diaphoresis, Diarrhea, Fever, Hyperreflexia, Incoordination, Confusion, Myoclonus, Shivering or TremorДокумент2 страницыAgitation, Diaphoresis, Diarrhea, Fever, Hyperreflexia, Incoordination, Confusion, Myoclonus, Shivering or TremorMark Darren MiguelОценок пока нет
- 32 Safety Alert of Potential Risk of Abuse Dependence and Withdrawal With BenzodiazepinesДокумент4 страницы32 Safety Alert of Potential Risk of Abuse Dependence and Withdrawal With BenzodiazepinesFatima BaburОценок пока нет
- 1047-PPP66 Policy Guide SROMДокумент13 страниц1047-PPP66 Policy Guide SROMWael BebawyОценок пока нет
- Service20spec20es22020repeat20dispensing20 V1201020oct2004Документ2 страницыService20spec20es22020repeat20dispensing20 V1201020oct2004Mihai VladescuОценок пока нет
- use of GnRH agonists - british societyДокумент3 страницыuse of GnRH agonists - british societytheonlinegeekhubОценок пока нет
- Medications To Treat Opioid Use Disorder Research ReportДокумент34 страницыMedications To Treat Opioid Use Disorder Research ReportBakthika KumarageОценок пока нет
- KTHR Pharm AuthДокумент5 страницKTHR Pharm AuthdmuscleОценок пока нет
- BUTRANS-buprenorphine Patch, Extended Release Purdue Pharma LPДокумент64 страницыBUTRANS-buprenorphine Patch, Extended Release Purdue Pharma LPmeiraimОценок пока нет
- Acep Equal Opiod Wave IiДокумент43 страницыAcep Equal Opiod Wave IiJesse M. MassieОценок пока нет
- 00481-Overview Evaluation Waiver ProgramДокумент5 страниц00481-Overview Evaluation Waiver ProgramlosangelesОценок пока нет
- Opioid Conversion Ratios - Guide To Practice 2010: Released December 2010Документ12 страницOpioid Conversion Ratios - Guide To Practice 2010: Released December 2010Ronald WaiОценок пока нет
- Warfarin Collaborative Practice Dosing ProtocolДокумент17 страницWarfarin Collaborative Practice Dosing ProtocolSadiah Hasyim AlweiniОценок пока нет
- NARCOTIC&CONTROLLEDДокумент56 страницNARCOTIC&CONTROLLEDMelai Rodriguez IbardalozaОценок пока нет
- jhmbf01472 Sup 0001Документ10 страницjhmbf01472 Sup 0001simbamed235Оценок пока нет
- GL2006 019Документ195 страницGL2006 019GОценок пока нет
- Depot Antipsychotic Medication Guidelines - PHA04 - February 2020 - 0Документ29 страницDepot Antipsychotic Medication Guidelines - PHA04 - February 2020 - 0Obinna AnozieОценок пока нет
- Vancouver 2010 Paralympic Pharmacy GuideДокумент146 страницVancouver 2010 Paralympic Pharmacy GuideVsevolod BentsianovОценок пока нет
- Antiemetic Guidelines For ChemotherapyДокумент11 страницAntiemetic Guidelines For ChemotherapyAaron AntonioОценок пока нет
- Controlled Prescription Program August 2011: Program Objective Additional InformationДокумент2 страницыControlled Prescription Program August 2011: Program Objective Additional InformationKiranОценок пока нет
- 1 Barnett Comparison of Cost MTD - BPN Addiction 2009Документ11 страниц1 Barnett Comparison of Cost MTD - BPN Addiction 2009GRi CardozoОценок пока нет
- College of Physicians and Surgeons of British Columbia: Safe Prescribing of OpioidsДокумент4 страницыCollege of Physicians and Surgeons of British Columbia: Safe Prescribing of OpioidsAshley WadhwaniОценок пока нет
- Mifepristone Misoprostol Abortion ProtocolДокумент6 страницMifepristone Misoprostol Abortion ProtocolFawaaz KhurwolahОценок пока нет
- New Zealand Data Sheet: 1. Product NameДокумент13 страницNew Zealand Data Sheet: 1. Product NameIvan MakОценок пока нет
- Opioid WithdrawalДокумент18 страницOpioid WithdrawalMaria Ignacia GonzalezОценок пока нет
- GuidelineДокумент12 страницGuidelinemacmzОценок пока нет
- DF Buprenorphine Maintenance-FinalДокумент4 страницыDF Buprenorphine Maintenance-FinalDawn FarmОценок пока нет
- Guidelines+ +Opioids+ChapterДокумент16 страницGuidelines+ +Opioids+ChapterRajinder Kumar BassanОценок пока нет
- October 2022 New Jersey NewsletterДокумент8 страницOctober 2022 New Jersey NewsletterAmyОценок пока нет
- Member Guidelines OUDДокумент7 страницMember Guidelines OUDheffsworld440Оценок пока нет
- AMC MAT Induction With Home Induction FinalДокумент6 страницAMC MAT Induction With Home Induction FinalJenn GoochОценок пока нет
- Prescribing PBS Medicines - What Prescribers Need to KnowДокумент3 страницыPrescribing PBS Medicines - What Prescribers Need to KnowMehreen BatoolОценок пока нет
- Phresh Pharmacy: New Ideas for the Business of Community PharmacyОт EverandPhresh Pharmacy: New Ideas for the Business of Community PharmacyОценок пока нет
- Tabla de Cremas FagronДокумент2 страницыTabla de Cremas FagroncastimaxОценок пока нет
- Prescription Analysis OverviewДокумент19 страницPrescription Analysis OverviewJunimy GamonganОценок пока нет
- Pharmaceutical LicensingДокумент13 страницPharmaceutical Licensingkumari astha rupaliОценок пока нет
- Ethical Considerations of Pharmaceutical Marketing and PromotionДокумент31 страницаEthical Considerations of Pharmaceutical Marketing and Promotionkhizer iqbalОценок пока нет
- dmHVAC06 TableДокумент446 страницdmHVAC06 TableARUL SANKARANОценок пока нет
- Powders and GranulesДокумент2 страницыPowders and GranulesPietОценок пока нет
- Practice School Report - PrajwalДокумент44 страницыPractice School Report - PrajwalTry TryОценок пока нет
- Stok 30 Juni 2021Документ16 страницStok 30 Juni 2021melita Aditya SariОценок пока нет
- Answer Sheet Gpat Exam 1Документ1 страницаAnswer Sheet Gpat Exam 1KUMARAN SОценок пока нет
- Walmart Drug ListДокумент6 страницWalmart Drug ListShirley Pigott MDОценок пока нет
- Pharmexpert 2010 EngДокумент163 страницыPharmexpert 2010 EngMed PlusОценок пока нет
- Semi Solid DosageДокумент6 страницSemi Solid Dosagekamini bahirОценок пока нет
- Laporan Perbekalan Farmasi Obat Rusak KadaluarsaДокумент2 страницыLaporan Perbekalan Farmasi Obat Rusak KadaluarsakarinaОценок пока нет
- Vitamin K (Phytomenadione) 2016: Indication Action Drug Type Trade Name Presentation Dosage / IntervalДокумент3 страницыVitamin K (Phytomenadione) 2016: Indication Action Drug Type Trade Name Presentation Dosage / IntervalDeni Yuda Adi SaputraОценок пока нет
- Departments of a HospitalДокумент20 страницDepartments of a HospitalXYZОценок пока нет
- Jurnal Inovasi Farmasi IndonesiaДокумент7 страницJurnal Inovasi Farmasi IndonesiaMuhammad Rizki AssaniОценок пока нет
- Omnicell-HealthTrust Overview BrochureДокумент8 страницOmnicell-HealthTrust Overview BrochuregurbaxeeshОценок пока нет
- AstraZeneca, Merck, Ofthalmi and other pharmaceutical products listДокумент4 страницыAstraZeneca, Merck, Ofthalmi and other pharmaceutical products listcloris gilОценок пока нет
- ISMP AssessmentДокумент56 страницISMP AssessmentKamalakar KaramchetiОценок пока нет
- BIOT 1 Lecture 1 - Introduction To GMPsДокумент29 страницBIOT 1 Lecture 1 - Introduction To GMPsfaisalОценок пока нет
- Vaccine FormДокумент56 страницVaccine FormPamela PatawaranОценок пока нет
- Prescription & Its PartsДокумент8 страницPrescription & Its Partsmadhumay23100% (1)
- Financial Statement Analysis of Glenmark PharmaceuticalДокумент44 страницыFinancial Statement Analysis of Glenmark PharmaceuticalNarayan GroverОценок пока нет
- Treating Skin Conditions and DiseasesДокумент1 страницаTreating Skin Conditions and DiseasesVirda Desta100% (1)
- Stevens V Rite Aid CorporationДокумент6 страницStevens V Rite Aid CorporationYinmeng HuОценок пока нет
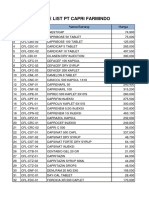
- Price List PT Capri Farmindo: No. Kode Barang Nama Barang HargaДокумент2 страницыPrice List PT Capri Farmindo: No. Kode Barang Nama Barang HargaAqma SkincareОценок пока нет