Академический Документы
Профессиональный Документы
Культура Документы
98035
Загружено:
Aldy RinaldiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
98035
Загружено:
Aldy RinaldiАвторское право:
Доступные форматы
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
1
The Pediatric Infectious Disease Journal Publish Ahead of Print
DOI: 10.1097/INF.0000000000000336
Acquired Drug-Resistance during Inadequate Therapy in a Young Child with Tuberculosis
Anthony J. Garcia-Prats, MD
1
, Marianne Willemse, MB, ChB
2
, Heiner I. Seifart, PhD
3
,
Annemie M. Jordaan, Med Tech
4
, Cedric J. Werely, PhD
4
, Peter R. Donald, MD
1
, and H.
Simon Schaaf, MMed (Paed), MD (Paed)
1, 5
1
Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Faculty of Medicine
and Health Sciences, Stellenbosch University, Tygerberg, South Africa
2
Brooklyn Hospital for Chest Diseases, Cape Town, South Africa
3
Division of Pharmacology, Faculty of Medicine and Health Sciences, Stellenbosch University,
Tygerberg, South Africa
4
Division of Molecular Biology and Human Genetics, DST/NRF Centre of Excellence for
Biomedical Tuberculosis Research, MRC Centre for Molecular and Cellular Biology, Faculty of
Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
5
Tygerberg Childrens Hospital, Tygerberg, South Africa
Corresponding Author: Anthony J. Garcia-Prats
Email: garciaprats@sun.ac.za
Phone: +27 71 408 7306; +27 21 378 9177
Address: Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Clinical
Building, Room 0085, Faculty of Health Sciences, Stellenbosch University, P.O.
Box 19063, Tygerberg, South Africa
Abbreviated Title: Acquired Resistance in a Child with TB
Running Head: Acquired TB Resistance
Conflicts of Interest: None declared.
Funding Sources: None
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
2
Abstract: Drug resistance in children with tuberculosis is usually primary (transmitted),
however resistance acquisition during treatment is possible. We describe a child with
tuberculosis who acquired drug resistance while receiving directly-observed but
inadequate first-line therapy and the programmatic and clinical factors that may have
contributed to resistance acquisition.
Key Words: Tuberculosis, children, isoniazid monoresistance, acquired antibiotic
resistance, MDR
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
3
Background
Resistance acquired during treatment contributes to a substantial proportion of the drug-resistant
(DR) tuberculosis (TB) burden in adults.
1
Drug resistance is acquired following actual or
functional monotherapy most often associated with poor treatment adherence or pharmacokinetic
mismatch.
1
Because of the paucibacillary nature of childhood TB, DR-TB in children is most
often primary (transmitted) following infection with strains already drug-resistant, rather than
resistance being acquired during treatment.
2
Children with extensive TB disease with a large
Mycobacterium tuberculosis (M. tuberculosis) bacillary load are at greater risk for acquiring
drug resistance during inadequate treatment, though this is seldom described.
We report a young child with drug resistance acquired while receiving first-line directly
observed treatment, and we highlight factors potentially contributing to this treatment failure and
resistance acquisition.
Case
Table, Supplemental Digital Content 1, http://links.lww.com/INF/B865, summarizes the clinical
course and key microbiologic findings. A 25-month-old male presented to a rural hospital five
months before admission to our hospital, with a two week history of cough, weight loss and
decreased activity. His past medical history was significant for an episode of pneumonia one
month earlier. He was HIV-unexposed and had received Bacille Calmette-Gurin (BCG)
vaccination at birth. His family of two adults and two children lived in a one room house visited
regularly by a great-uncle who had pulmonary TB susceptible to isoniazid (INH) and rifampin
(RIF). Weighing 7.9 kg at initial presentation he was moderately underweight, with a weight-
for-age z-score of <-2; he was tachypneic with crepitations on lung examination, but without
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
4
neck stiffness. Chest radiography showed left-upper lobe opacification with cavities. A
tuberculin skin test, non-reactive the previous year, now measured 12 mm induration. He was
diagnosed with probable pulmonary TB and started on first-line three-drug treatment with a
fixed-dose combination containing INH 30mg (3.8 mg/kg), RIF 60mg (7.6 mg/kg), and
pyrazinamide (PZA) 150mg (19.0 mg/kg). Gastric aspirates were acid-fast bacilli (AFB) smear-
negative on microscopy but culture-positive for M. tuberculosis. Drug susceptibility testing
(DST) was not done.
In follow-up two months later he was noted to have a weight of 7.85 kg and persistent abnormal
chest signs. Repeat gastric aspirates were AFB smear-negative and sent for mycobacterial
culture. Despite persistent symptoms he was changed to continuation phase treatment with INH-
RIF. Since the child first began TB treatment, medication administration had been directly
observed by a non-family treatment supporter. The gastric aspirates subsequently grew M.
tuberculosis resistant to INH with an inhA promoter region mutation, but susceptible to RIF by
line probe assay (LPA; GenoType MTBDRplus, Hain Lifescience, Nehren, Germany), but the
result was not communicated to the clinic.
He remained unwell, continued losing weight, and was seen by multiple different health care
providers (Table, Supplemental Digital Content 1, http://links.lww.com/INF/B865). Three
months later he was admitted to a secondary referral hospital where his mental status
deteriorated. A lumbar puncture was done and the cerebrospinal fluid (CSF) showed 1
neutrophil x 10
6
/L, 145 lymphocytes x10
6
/L, a protein of 7.5 g/L, and glucose of 1.8 mmol/L.
The child was then referred to our hospital.
At Tygerberg Childrens Hospital the patient had a Glasgow Coma Scale of 9/15. He was
wasted, weighing 6.69 kg. An urgent computed tomography scan of the brain showed bilateral
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
5
diffuse ring enhancing lesions with generalized edema, leptomeningeal and basal enhancement,
hydrocephalus with bilateral periventricular hypodensities, and hypodensities in the basal ganglia
consistent with infarcts, all indicative of tuberculous meningitis (TBM). A ventriculoperitoneal
shunt was placed, and CSF was sent for bacterial and mycobacterial culture. A chest radiograph
was consistent with cavitary pulmonary TB with bronchopneumonic spread. Gastric aspirates
were AFB smear-negative, and cultures were requested. The previous culture was traced and
because of INH resistance, recent treatment with INH-RIF only, and in the light of disease
progression he was started empirically on INH, RIF, PZA, ethambutol, ethionamide, ofloxacin,
amikacin, and terizidone for probable multidrug-resistant (MDR)-TB. After two weeks his
condition stabilized and he was transferred to Brooklyn Hospital for Chest Diseases for long-
term management.
Cultures from these gastric aspirates grew M. tuberculosis resistant to both INH and RIF by
LPA. The LPA identified both INH-resistant and INH-and-RIF-resistant organisms.
Spoligotyping of these MDR and previously identified INH-resistant RIF-susceptible strains
showed them to be Beijing strains of the same type making superinfection with a new MDR-
strain unlikely. As part of a study of pharmacokinetics (PK) of antituberculosis drugs, this child
had PK investigations on two occasions, which showed very low maximum INH serum
concentrations of 0.64 g/mL and 2.2 g/mL after exact oral doses of 20 mg/kg on two
occasions. Genotyping of the arylamine N-acetyltransferase 2 (NAT2) gene as previously
described,
3
delineated the NAT2*4/2*7B genotype, which is consistent with heterozygous rapid
acetylator genotype (FS).
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
6
The child completed 18 months of a standard MDR-TB treatment regimen after his first negative
culture and had a successful treatment response. He showed substantial neurologic
improvement, and was walking unassisted at the time of discharge.
Discussion
We describe a case of acquired drug resistance in a young child with extensive cavitating
pulmonary TB receiving inadequate therapy. Cavitations on chest radiography in young children
with TB, particularly those presenting late, are not rare, though may be due to breakdown in
lobar or segmental consolidations rather than typical adult-type TB.
4
As no DST was done on
the childs initial sputum we cannot definitively document that the child started treatment with a
fully drug-susceptible (DS) strain. Considering the only identified source case had documented
DS-TB, the high concordance of the isolates of young children with their source case, and the
well-documented potential for rapid emergence of INH resistance, this is most likely.
2
If so, this
child initially infected with DS-TB acquired first INH resistance followed by RIF resistance.
Although poor adherence is often postulated as the reason for acquired resistance, this childs
adherence was directly observed in the home by a treatment supporter. We hypothesize that
under-dosing, poor absorption, and heterozygous rapid acetylation are responsible for resistance
acquisition in this case, which is consistent with emerging evidence on the contribution of
individual pharmacokinetic variability to acquired resistance.
5
The initial dosages of INH 3.8
mg/kg, RIF 7.6 mg/kg, and PZA 19.0 mg/kg were less than currently recommended dosages.
Two-hour INH concentrations between 0.5-1.0 g/mL have early bactericidal activity of 0.342,
6
so even low concentrations as in this child, can assert a strong selective pressure. Based on
published RIF pharmacokinetics in children, this RIF dosage was likely insufficient to prevent
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
7
emergence of INH-resistant mutants.
7
Because INH is the most bactericidal of the first-line
antituberculosis drugs, loss of its protective effect rapidly leads to further resistance acquisition
against companion drugs, as was the case with this child. Despite his low INH dose,
concentrations may still have been adequate in a slow acetylator to provide some activity and
protection against acquiring RIF resistance considering the usual low-level INH resistance
associated with inhA mutations.
3, 8
In a rapid or intermediate acetylator however, as this child
was, the exposure could be inadequate to provide protection.
This case highlights additional important lessons for pediatric TB management. Antituberculosis
drug dosing in children is weight-dependent, and although standardized weight-banded dosing is
widely used, misdosing in children may be common and this case illustrates the reasons for the
recent changes in the recommended antituberculosis drug doses for children. Children on
antituberculosis treatment who deteriorate or do not respond need investigation; failure to
respond may be due to poor adherence, but a high index of suspicion for resistance is needed.
This child had multiple interactions with the health system after starting documented adherent
antituberculosis treatment; despite worsening disease and loss of weight, neither additional
investigations, treatment changes, nor possible drug resistance were considered. It is possible
that early recognition of the poor treatment response may have averted this poor outcome.
Although cultures for M. tuberculosis were sent after two months of treatment, it appears that
these results were not reported. He remained on his standard continuation phase INH-RIF,
though INH resistance would have prompted a change in treatment. INH-resistant TB (i.e. INH-
resistant, RIF-susceptible) is the most common form of DR-TB, representing 4.6-7.7% of
confirmed isolates in children in our setting,
9
and in adults has been associated with additional
acquired resistance. Pediatric guidelines recommend treatment of INH-resistant TB with RIF,
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
8
pyrazinamide, and ethambutol for 6-9 months, with addition of a fluoroquinolone for extensive
disease, though there is limited evidence for this recommendation.
10
This case demonstrates the
need for additional evidence on the most appropriate treatment of INH-resistant TB in children.
In conclusion, acquisition of drug-resistance in young children with TB is possible. Addressing
the clinical and programmatic challenges described here may help ensure the best possible
outcomes for children with TB.
Acknowledgements
We thank the Brooklyn Chest Hospital pediatric ward staff for their assistance with the care of
this child and the Desmond Tutu TB Centre MDR PK study team for assistance with the
pharmacokinetic studies.
Declaration
The mother of this child provided written informed consent for this case report and for the
childs participation in the pharmacokinetics study referenced here. Ethical approvals for this
pharmacokinetics study and for this case report were provided by the Health Research Ethics
Committee of the Faculty of Medicine and Health Sciences, Stellenbosch University.
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
9
References:
1. Mitchison DA. How drug resistance emerges as a result of poor compliance during short
course chemotherapy for tuberculosis. Int J Tuberc Lung Dis. 1998;2:10-15.
2. Schaaf HS, Van Rie A, Gie RP, et al. Transmission of multidrug-resistant tuberculosis.
Pediatr Infect Dis J. 2000;19:695-699.
3. Schaaf HS, Parkin DP, Seifart HI, et al. Isoniazid pharmacokinetics in children treated for
respiratory tuberculosis. Arch Dis Child. 2005;90:614-618.
4. Schaaf HS, Marais BJ, Whitelaw A, et al. Culture-confirmed childhood tuberculosis in Cape
Town, South Africa: a review of 596 cases. BMC Infect Dis. 2007;7:140.
5. Srivastava S, Pasipanodya JG, Meek C, Leff R, Gumbo T. Multidrug-resistant tuberculosis not
due to noncompliance but to between-patient pharmacokinetic variability. J Infect Dis.
2011;204:1951-1959.
6. Donald PR, Sirgel FA, Venter A, et al. The influence of human N-acetyltransferase genotype
on the early bactericidal activity of isoniazid. Clin Infect Dis. 2004;39:1425-1430.
7. Schaaf HS, Willemse M, Cilliers K, et al. Rifampin pharmacokinetics in children, with and
without human immunodeficiency virus infection, hospitalized for the management of severe
forms of tuberculosis. BMC Med. 2009;7:19.
8. Cynamon MH, Zhang Y, Harpster T, Cheng S, DeStefano MS. High-dose isoniazid therapy
for isoniazid-resistant murine Mycobacterium tuberculosis infection. Antimicrob Agents
Chemother. 1999;43:2922-2924.
9. Seddon JA, Hesseling AC, Marais BJ, Jordaan A, Victor T, Schaaf HS. The evolving epidemic
of drug-resistant tuberculosis among children in Cape Town, South Africa. Int J Tuberc Lung
Dis. 2012;16:928-933.
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
10
10. World Health Organization. Guidelines for the programmatic management of drug-resistant
tuberculosis: Emergency Update 2008 2008. Available at:
http://whqlibdoc.who.int/publications/2008/9789241547581_eng.pdf.
A
C
C
E
P
T
E
D
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
13
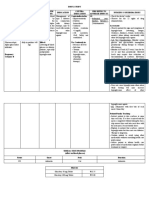
Supplemental Table 1. Clinical course, laboratory and microbiology results of a child with acquired tuberculosis drug resistance
Date Clinical, laboratory, and radiology notes
Wt
(kg)
Specimen
Type
AFB
Smear
Mtb
Culture
DST TB Treatment
25-Jul-2011 Presented with chronic cough, fever, loss of weight; TST reactive
(12mm); started on TB treatment
7.9 GA Neg Pos Not requested INH, RIF, PZA
GA Neg Pos Not requested
28-Sep-2011 Abnormal chest examination findings, poor weight gain 7.9 GA Neg Pos INH-R, RIF-S INH, RIF
GA Neg Pos Not requested
GA Neg Pos Not requested
Oct-2011 Tachypneic (RR 88 breaths/min), creptitations on chest
examination; admitted for presumed bacterial pneumonia
7.6
Nov-2011 Treated symptomatically by private physician for tiredness, loss of
appetite, fever, vomiting, rash
17-Dec-2011 Admitted to secondary referral hospital for fever, sore throat, rash;
deteriorating mental status during admission; CSF Poly 1/ml,
lymph 145/ml, Eryth 0, Prot 7.5g/L, Gluc 1.8mmol/L
19-Dec-2011 Transferred to Tygerberg Childrens Hospital; bilateral lung
crepitations, decreased strength, increased tone and brisk reflexes
throughout, GCS 9/15; CT Brain edema, basal enhancement,
multiple infarcts; Chest X-ray cavitations with bronchopneumonia
6.7 CSF Neg Neg INH, RIF, PZA,
EMB, ETO,
OFX, AMK, TZD
23-Dec-2011 GA Neg Pos INH-R, RIF-R, ETO-
S, OFX-S, AMK-S
GA Neg Pos
05-Jan-2012 Transfer to Brooklyn Chest Hospital, severe spastic quadriplegia 7.2
10-Jan-2012 Sputum Neg Pos
07-Feb-2012 All subsequent sputum specimens (n=13) were smear and culture
negative
Sputum Neg Neg
07-Mar-2012 Neurologic condition improved; spastic diplegia in lower limbs 7.8 Stop RIF
20-Jun-2012 Neurologic condition much improved; increased ankle tone, but
walking unsupported
9.4 Stop AMK
05-Aug-2013 Completed treatment 11.0 Stopped
Wt=weight, AFB= acid fast bacilli; M.tb.=Mycobacterium tuberculosis; DST=drug-susceptibility testing; TB=tuberculosis; TST=tuberculin skin test; GA=gastric aspirate;
Neg=negative; Pos=positive; INH=isoniazid; RIF=rifampicin; PZA=pyrazinamide; EMB=ethambutol; ETO=ethionamide; OFX=ofloxacin; AMK=amikacin; TZD=terizidone; CT=
computed tomography scan; CSF=cerebrospinal fluid; Poly=polymorphonuclear leukocytes; Lymph=lymphocytes; Eryth=erythrocytes; Prot=protein;Gluc=glucose
A
C
C
E
P
T
E
D
Вам также может понравиться
- Healthy Sleep: Finding A SpecialistДокумент4 страницыHealthy Sleep: Finding A SpecialistAldy RinaldiОценок пока нет
- Am J Cllin Nutr 2000 Rogol Et Al. Growth and Pubertal Development in Children and AdolescentsДокумент8 страницAm J Cllin Nutr 2000 Rogol Et Al. Growth and Pubertal Development in Children and AdolescentsAldy RinaldiОценок пока нет
- Jurnal NeoДокумент4 страницыJurnal NeoAldy RinaldiОценок пока нет
- Abstract Pit Sby 2015Документ1 страницаAbstract Pit Sby 2015Aldy RinaldiОценок пока нет
- CP UpdateДокумент4 страницыCP UpdateAldy RinaldiОценок пока нет
- Natriuretic HormoneДокумент11 страницNatriuretic HormoneAldy RinaldiОценок пока нет
- Jurnal Allergi ImunДокумент6 страницJurnal Allergi ImunAldy RinaldiОценок пока нет
- Manajemen CPДокумент8 страницManajemen CPAldy RinaldiОценок пока нет
- Kurva Gizi CPДокумент11 страницKurva Gizi CPAldy RinaldiОценок пока нет
- Jurnal Nefro SubdivisiДокумент3 страницыJurnal Nefro SubdivisiAldy RinaldiОценок пока нет
- Jurnal PGD 2Документ13 страницJurnal PGD 2Aldy RinaldiОценок пока нет
- Gambar 5 BNPДокумент7 страницGambar 5 BNPAldy RinaldiОценок пока нет
- Daftar Pustaka VSDBNPДокумент12 страницDaftar Pustaka VSDBNPAldy RinaldiОценок пока нет
- Clinical Pediatrics: Impact of Vegetarian Diet On Serum Immunoglobulin Levels in ChildrenДокумент7 страницClinical Pediatrics: Impact of Vegetarian Diet On Serum Immunoglobulin Levels in ChildrenAldy RinaldiОценок пока нет
- Gambar Obesitas Menyebabkan DislipidemiaДокумент40 страницGambar Obesitas Menyebabkan DislipidemiaAldy RinaldiОценок пока нет
- Terapi Meta AnalisisДокумент8 страницTerapi Meta AnalisisAldy RinaldiОценок пока нет
- AsdДокумент28 страницAsdAldy RinaldiОценок пока нет
- Multidrug Resistant TuberculosisДокумент8 страницMultidrug Resistant TuberculosisAldy RinaldiОценок пока нет
- Terapi Meta AnalisisДокумент8 страницTerapi Meta AnalisisAldy RinaldiОценок пока нет
- Rifampicin ResistanceДокумент7 страницRifampicin ResistanceAldy RinaldiОценок пока нет
- 2012 - 12 Management of MDR-TB in Children A Field Guide - 0Документ58 страниц2012 - 12 Management of MDR-TB in Children A Field Guide - 0Aldy RinaldiОценок пока нет
- Clin Infect Dis. 2013 Seddon 1676 84Документ9 страницClin Infect Dis. 2013 Seddon 1676 84Aldy RinaldiОценок пока нет
- TB PDFДокумент10 страницTB PDFAgung Budiman Agustinus SilalahiОценок пока нет
- P ('t':'3', 'I':'3053683786') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Документ2 страницыP ('t':'3', 'I':'3053683786') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Aldy RinaldiОценок пока нет
- 2012 - 12 Management of MDR-TB in Children A Field Guide - 0Документ58 страниц2012 - 12 Management of MDR-TB in Children A Field Guide - 0Aldy RinaldiОценок пока нет
- TB in ChildrenДокумент27 страницTB in ChildrenAlberto ColoradoОценок пока нет
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceДокумент7 страницMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiОценок пока нет
- MM 6241Документ8 страницMM 6241Aldy RinaldiОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Dr. Dewi-Geriatric PharmacologyДокумент41 страницаDr. Dewi-Geriatric PharmacologyAnne Gustriwati0% (1)
- Knowledge, Attitude and Practice of Medical Professionals Towards The Safe Disposal of Unused Medications in South IndiaДокумент9 страницKnowledge, Attitude and Practice of Medical Professionals Towards The Safe Disposal of Unused Medications in South IndiaDenise Yanci DemiarОценок пока нет
- Salinan Dari Jadwal KF Kedung CowekДокумент47 страницSalinan Dari Jadwal KF Kedung Cowekdwikamaliyatissholehah94Оценок пока нет
- (9781585286584 - ASHP® Injectable Drug Information™) Preliminary MaterialДокумент24 страницы(9781585286584 - ASHP® Injectable Drug Information™) Preliminary MaterialSathundorn NuntaОценок пока нет
- Nama Obat Jumlah Order DistributorДокумент22 страницыNama Obat Jumlah Order DistributorNdaa NandaОценок пока нет
- Acarbose Drug Study OverviewДокумент3 страницыAcarbose Drug Study OverviewKian HerreraОценок пока нет
- ICU Floor Stock Inventory ListДокумент2 страницыICU Floor Stock Inventory Listicu paling nubОценок пока нет
- 029 Medication TrayДокумент3 страницы029 Medication TrayS BindhiyaОценок пока нет
- Farmacoacupuntura JungДокумент33 страницыFarmacoacupuntura JungCEMICG OFICIALОценок пока нет
- Farmakoterapi Antifungi 2021Документ18 страницFarmakoterapi Antifungi 2021TiaraОценок пока нет
- Unani Product List PDFДокумент109 страницUnani Product List PDFEdward Ebb Bonno81% (16)
- Newer Antiepileptic Drugs and Recent Advances in Drug Therapy of EpilepsyДокумент9 страницNewer Antiepileptic Drugs and Recent Advances in Drug Therapy of EpilepsySanjay NavaleОценок пока нет
- Npi (Print)Документ11 страницNpi (Print)Daryl Valerio FranciscoОценок пока нет
- Valium Drug AnalysisДокумент1 страницаValium Drug AnalysisFerdinand Sherwin MorataОценок пока нет
- Uas Praktikum Xii F 2020Документ9 страницUas Praktikum Xii F 2020bledok khatolОценок пока нет
- Ped Med HandbookДокумент33 страницыPed Med HandbookDaniela Marie RonquilloОценок пока нет
- Safety and Efficacy Therapy New CombinationДокумент11 страницSafety and Efficacy Therapy New CombinationFalisha Belvia KairinОценок пока нет
- Anti Anxiety DrugsДокумент26 страницAnti Anxiety DrugsSANJIV KUMAR YADAV100% (1)
- Kidney 1Документ26 страницKidney 1Zainurain Zainal AbidinОценок пока нет
- CV 0000111Документ2 страницыCV 0000111shamseerОценок пока нет
- PT. ANTARMITRA SEMBADA - Healthcare & Consumer MarketerДокумент49 страницPT. ANTARMITRA SEMBADA - Healthcare & Consumer MarketerAyu RiskaОценок пока нет
- Chapter 51Документ37 страницChapter 51Aan KurniawanОценок пока нет
- Fda'S Question-Based Review (QBR) : A Risk-Based Pharmaceutical Quality Assessment ToolДокумент50 страницFda'S Question-Based Review (QBR) : A Risk-Based Pharmaceutical Quality Assessment Toollalooprasad15Оценок пока нет
- Topical Steroids (Sep 16)Документ7 страницTopical Steroids (Sep 16)lalaОценок пока нет
- Serotonin Drugs: SSRIs, SNRIs, TCAs, MAOIs and Atypical AntidepressantsДокумент4 страницыSerotonin Drugs: SSRIs, SNRIs, TCAs, MAOIs and Atypical AntidepressantsPauline NguyenОценок пока нет
- Ag Listing 05oct2023Документ98 страницAg Listing 05oct2023kiranduggarajuОценок пока нет
- DetailingДокумент5 страницDetailingNoor MuhammadОценок пока нет
- Did Seizures QN 1Документ31 страницаDid Seizures QN 1api-608647584Оценок пока нет
- Formularium CitamaДокумент37 страницFormularium Citamars citamaОценок пока нет
- Lesson Plan Fonn S.3Документ17 страницLesson Plan Fonn S.3Sandeep MeenaОценок пока нет