Академический Документы
Профессиональный Документы
Культура Документы
RENAL DENERVATIONl PDF
Загружено:
Luis Fernando Morales Jurado0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров13 страницRNA has become the new buzz word in hypertension and interventional cardiology. Sympathetic fiber interruption through transvascular techniques that are minimally invasive. RNA can be used to treat a wide range of conditions, including resistant hypertension.
Исходное описание:
Оригинальное название
RENAL DENERVATIONl.pdf
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документRNA has become the new buzz word in hypertension and interventional cardiology. Sympathetic fiber interruption through transvascular techniques that are minimally invasive. RNA can be used to treat a wide range of conditions, including resistant hypertension.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров13 страницRENAL DENERVATIONl PDF
Загружено:
Luis Fernando Morales JuradoRNA has become the new buzz word in hypertension and interventional cardiology. Sympathetic fiber interruption through transvascular techniques that are minimally invasive. RNA can be used to treat a wide range of conditions, including resistant hypertension.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 13
Vasilios Papademetriou, Amir Adel Rashidi, Costas Tsioufis and Michael Doumas
and Future Directions
Renal Nerve Ablation for Resistant Hypertension: How Did We Get Here, Present Status,
Print ISSN: 0009-7322. Online ISSN: 1524-4539
Copyright 2014 American Heart Association, Inc. All rights reserved.
is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Circulation
doi: 10.1161/CIRCULATIONAHA.113.005405
2014;129:1440-1451 Circulation.
http://circ.ahajournals.org/content/129/13/1440
World Wide Web at:
The online version of this article, along with updated information and services, is located on the
http://circ.ahajournals.org//subscriptions/
is online at: Circulation Information about subscribing to Subscriptions:
http://www.lww.com/reprints
Information about reprints can be found online at: Reprints:
document. Permissions and Rights Question and Answer this process is available in the
click Request Permissions in the middle column of the Web page under Services. Further information about
Office. Once the online version of the published article for which permission is being requested is located,
can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Circulation in
Requests for permissions to reproduce figures, tables, or portions of articles originally published Permissions:
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1440
S
ympathetic renal denervation, or renal nerve ablation
(RNA), has become the new buzz word in hypertension
and interventional cardiology. Recent advances in catheter-
based approaches have allowed sympathetic ber interruption
through transvascular techniques that are minimally invasive
and can be delivered expeditiously and safely. Radiofrequency
(RF) energy sources are currently the preferred modalities,
but other sources of energy, such as cryoablation, microwave,
high-intensity focus ultrasound, and local neurotoxic agent
infusion, are under intense investigation. Results thus far have
been encouraging and offer promise for the future. The role
of the sympathetic nervous system (SNS) in the development
of resistant hypertension and cardiovascular disease has long
been known, and a great deal of work has been done through
the years trying to explore potential interventions to inter-
rupt the sympathetic inuence on systemic vasculature and
target organs. In this article we attempt an overview of time-
dependent interventions on the SNS and examine approaches
used in humans and in the many experimental models that
offer a better understanding of the role of sympathetic activ-
ity in cardiovascular disease. Naturally we focus on methods
and techniques addressing sympathetic renal denervation in
patients with drug-resistant hypertension, examine the current
state of the art, and attempt a look into the future.
Historic Perspective
In 1889, after meticulous experiments on dogs, Bradford
1
reported that stimulation of dorsal and splanchnic nerves
causes changes in blood pressure (BP) and kidney size
measured by plethysmography. Whether BP increased or
decreased depended on the anatomic area stimulated, as well
as the electric impulse frequency, but outcomes were consis-
tent and reproducible. Neurosurgical treatment of hyperten-
sion was independently suggested by researchers in 1923.
2
Adson, however, was the rst to performed surgical sym-
pathectomy for the treatment of malignant hypertension in
1925.
3
During the following years and in the 1930s, Peet in
Ann Arbor, Page and Heuer in New York, and Adson, Craig,
and Brown from the Mayo Clinic operated and reported on
series of patients all experiencing malignant hypertension.
4
At
the same time, renal decapsulation, which was considered a
form of sympathectomy by disrupting the bers between the
capsule and the renal cortex, was being performed to treat
unexplained hematuria and perinephritis. Sen
5
reported a sig-
nicant but not permanent decrease in BP in 85 subjects who
underwent decapsulation between 1925 and 1935.
Surgical denervation of the kidneys alone was rst per-
formed in humans by Papin and Ambard
6
in 1924 in an
attempt to relieve intractable pain originating from the kid-
ney. The rst case of bilateral sympathetic denervation of the
kidney to treat severe essential hypertension was presented
in 1934 by Page and Heuer.
7
The patient was a 25-yearold
woman who reported easy fatigability and had severe head-
aches and BP in the range of 208/140 mm Hg. The patient
underwent surgical staged, bilateral renal sympathectomy
with no clinically meaningful effect on BP after follow-up
for 5 months. However, the case established that the proce-
dure was safe and had no negative effect on renal function.
In 1935, Page and Heuer
8
reported bilateral renal denervation
in 5 patients with chronic and progressive nephritis, which
resulted in no change in renal clearance or concentrating
ability of the kidney but caused diminished proteinuria and
a decrease in BP that lasted for months in the majority of
those patients. Because of these early unsatisfactory results,
surgical renal denervation gave way to the more radical sym-
pathectomy procedure, the surgical removal of splanchnic
nerves (splanchnicectomy), which showed dramatic results
in the majority of patients with malignant hypertension. Peet
published series and case reports of patients with malignant
hypertension responding in a dramatic way to supradiaphrag-
matic splanchnicectomy.
9
Figure 1 shows the BP response
of a 22-yearold patient with known severe hypertension for
>3 years. She had been in bedrest for 8 months because of
the severity of symptoms, yet her BP remained at 280/190
mm Hg. Fundoscopic examination revealed stage IV retinopa-
thy with evidence of early papilledema, ame-shaped hem-
orrhages, and cotton wool exudates. On June 24, 1934 she
underwent bilateral supradiaphragmatic splanchnicectomy,
and postoperatively her BP was reduced to 110/90 mm Hg.
Fundoscopic examination 2 months later demonstrated com-
plete resolution of papilledema, with hemorrhages and exu-
dates resolved. The patient became asymptomatic, and 13
years later was free of any hypertensive complications with
BP, remaining within the normal range (Figure 1).
Since then and for the subsequent 2 decades, surgical
sympathectomy (thoracolumbar splanchnicectomy) became
(Circulation. 2014;129:1440-1451.)
2014 American Heart Association, Inc.
Circulation is available at http://circ.ahajournals.org DOI: 10.1161/CIRCULATIONAHA.113.005405
From the Department of Veterans Affairs and Georgetown University, Washington, DC (V.P., A.A.R.); Ippokration University Hospital, Athens, Greece
(C.T.); Aristotle University of Thessaloniki, Thessaloniki, Greece (M.D.).
Correspondence to Vasilios Papademetriou, MD, Veterans Affairs Medical Center, 50 Irving St, NW, 151-E, Washington, DC 20422. E-mail
vasilios.papademetriou@va.gov
Renal Nerve Ablation for Resistant Hypertension
How Did We Get Here, Present Status, and Future Directions
Vasilios Papademetriou, MD; Amir Adel Rashidi, MD; Costas Tsious, MD; Michael Doumas, MD
Contemporary Reviews in Cardiovascular Medicine
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1441
the procedure of choice for patients with severe/malignant
hypertension not responding to diet or to then-limited phar-
macologic therapy. Between 1938 and 1947, Smithwick and
Thompson
10
published results from 3500 patients with severe/
malignant hypertension. Of those, 2400 patients underwent
thoracolumbar splanchnicectomy, and the rest were fol-
lowed on a medical regimen. Of those, 1266 patients who had
splanchnicectomy, and 467 patients on medical therapy had
follow-up of 5 to 14 years and were included in the nal anal-
ysis. At 5 years of follow-up, all-cause mortality was 19% in
the surgical series and 54% in the medically treated patients.
Of the surgically treated patients, only 45% demonstrated
substantial BP reduction, but mortality benets were real-
ized across the board. Peet et al
11
reported 51.4% signicant
BP reduction and 3.4% operative mortality in 350 patients
with severe/malignant hypertension. However, an important
limiting complication was postural hypotension, which was
encountered in many patients postoperatively.
In the mid-1950s the rst oral antihypertensive medication
became available for the treatment of hypertension, and for
the rst time a well-tolerated regimen could be given long
term.
12
Pharmacologic therapy helped treat many patients with
severe hypertension, and the number of patients progressing
to accelerated/malignant stage gradually diminished,
13
thus
settling the issue for the next 5 decades. Very few patients not
responding to pharmacologic therapy have been referred for
splanchnicectomy in recent years. However, during this time a
great deal of research has been pursued to uncover and better
understand the role of the SNS and, in particular, of the renal
sympathetic nerves in the development and maintenance of
hypertension.
14
A wealth of experimental data in animals and humans point
toward an important role of SNS overactivity for the develop-
ment and persistence of hypertension.
15
Excessive SNS activ-
ity is involved in the metabolic syndrome, obesity, structural
and functional myocardial alterations,
16
and several other dis-
ease states, including congestive heart failure (HF), chronic
kidney disease, polycystic ovary syndrome, obstructive sleep
apnea, and cirrhosis.
1721
SNS regulation is multifactorial, and
several mechanisms modulate sympathetic activity.
15
Renal Nerves: Efferent and Afferent
Sympathetic Fibers
Kidneys act both as generators and recipients of sympathetic
signals (Figure 2).
22
Sympathetic afferent bers originate from
the kidneys and travel to the central nervous system, where,
Figure 1. Blood pressure response to splanchnicectomy in a young woman with malignant hypertension: a 13-year postoperative follow
up. Reprinted from Peet
9
with permission from the American Journal of Surgery.
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1442 Circulation April 1, 2014
after processing, coordinated by the nucleus tractus solitaries
of the midbrain, they regulate sympathetic outow and pro-
mote SNS overactivity in response to renal injury.
23
On the
other hand, renal efferent sympathetic nerves originate from
the brain, travel through the spinal cord, reach the kidney from
the second sympathetic ganglia, course through the adventitia
of the renal arteries, and innervate the peripheral segments in
the renal cortex, ending in glomerular arterioles, where they
can affect renal function. Overactivity of the efferent sym-
pathetic bers results in enhanced renin release, increased
sodium and water absorption, reduced renal blood ow, and
glomerular ltration rate.
24
It seems that both the afferent and
efferent bers contribute to the development and persistence
of hypertension.
By the 1980s it was well established that kidneys are impor-
tant sensory organs with abundant baroreceptors and chemo-
receptors and signicant afferent innervation. In 1987, Webb
and Brody
25
published results from a thesis in which they
addressed signal trafcking via the afferent sympathetic bers
in a rat model. Through extensive instrumentation and care-
ful monitoring, they demonstrated that electric stimulation of
afferent sympathetic bers can reduce BP in a dose-dependent
manner. They also demonstrated that BP responses could be
abolished by spinal transection and interruption of the efferent
sympathetic bers coursing through the spine. Subsequently,
in a controlled study, Campese and Kogosov
26
showed that
resection of the afferent renal nerves through ventral rhizot-
omy can prevent activation of the noradrenergic neurons in the
hypothalamus and can prevent the development of hyperten-
sion in rats with chronic renal insufciency.
In other studies, Converse et al
27
showed that patients on
hemodialysis who have undergone bilateral nephrectomy
have signicantly lower peripheral vascular resistance and
BP. Similar ndings were reported by Hausberg et al
28
in
renal transplant recipients before and after surgical removal of
native kidneys. Bilateral nephrectomy results in the interrup-
tion of both the afferent and efferent sympathetic bers.
Renal nerve stimulation results in vasoconstriction of
the renal vasculature.
29
Others have demonstrated that sym-
pathetic nerve endings directly release norepinephrine on
renal epithelial cells and can cause a 30% to 40% increase
in sodium and water reabsorption via 1 adrenergic
receptors even before any hemodynamic changes could be
detected.
30,31
In 1981, Osborn et al
32
demonstrated that low-
frequency stimulation of the renal nerve in dogs can directly
mediate renin secretion via -1 adrenergic receptors. In other
experiments, surgical renal denervation has been shown to
affect hypertension. In deoxycorticosterone acetatetreated
Figure 2. Diagram depicting the inuence of efferent and afferent sympathetic bers in modulating sympathetic responses of the kidney,
the heart, the vasculature, and other target organs.
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1443
miniature swine with established hypertension, OHagan
et al
33
demonstrated that renal denervation results in immense
natriuresis and BP reduction. Similarly, Huang et al
34
in a
hyperinsulinemia- induced hypertension model demonstrated
that renal denervation can prevent hypertension development
if done early or can normalize BP after hypertension is estab-
lished (Figure 3).
RNA for Drug-Resistant Hypertension
Renal sympathetic denervation has been performed, through
the years, both in experimental models and in humans by sur-
gical exposure of renal nerves. The renal nerves were inter-
rupted or resected using mostly a surgical scalpel, although
later electrocautery, cryoablation, and thermal (RF) ablation
have also been used. With progress in technology and the
advent of transcatheter techniques, it was natural to prog-
ress to transvascular methods to interrupt nerve integrity.
Catheter-based RF ablation techniques have been used in
electrophysiology for more than 2 decades to ablate acces-
sory pathways and abnormal cardiac structures in patients
with Wolff-Parkinson-White syndrome or supraventricular
and ventricular arrhythmia. In 1999, a series of experiments
completed at the University of Oklahoma using a basket cath-
eter demonstrated that it was possible to stimulate and ablate
autonomic nerves on the outside of blood vessels. Notably,
Schauerte et al used an innovative approach to stimulate
35
and
ablate
36
the vagal nerve to treat patients with vagally mediated
atrial brillation (AF). RF energy was applied transvascularly
to ablate the vagal nerve. The currently used technique for
catheter-based RNA uses a very similar concept.
Patients with drug-resistant hypertension have increased
sympathetic outow. Resistant hypertension is dened as
failure to achieve BP goals despite the use of at least 3 anti-
hypertensive drugs, 1 of which is a diuretic. The exact preva-
lence of resistant hypertension is not known, but by current
estimates, 12% of patients with hypertension are resistant
to treatment.
37,38
This would translate into 120 million
patients worldwide.
Given resistance to drug therapy, activation of SNS, the role
of renal nerves in the development of hypertension, and the
ease of approach of the sympathetic bers by catheter based
techniques, resistant hypertension was the perfect candidate
for interventional approaches.
39
Sympathetic bers course in
the adventitia of the renal arteries, are mostly situated within
2 to 3 mm from the inner layer of the renal artery,
40
and can be
easily reached and interrupted transvascularly using thermal
energy. To date, RF thermal energy has been delivered using
either a single-tip electrode catheter or multielectrode systems.
The objective of RF ablation is to place discrete lesions in a
circumferential pattern but not at the same cross-section of
the vessel, so as to minimize the risk of renal artery stenosis.
As of today, 6 devices received the CE marking to be
used for RNA. The rst device used in humans (Symplicity/
Ardian, Metronic) was a 6-French, steerable RF ablation cath-
eter inserted percutaneously through a femoral sheath and
a guide catheter engaging each renal artery sequentially.
41
This catheter is easy to use but it creates lesions with a less
predictable geometric pattern. The St Judes multielectrode
ablation system (EnligHTN) has 4 electrodes mounted on
a basket that can easily achieve circumferential distribution
Figure 3. Renal denervation in 2 animal models. A, Immense natriuresis and blood pressure reduction in a deoxycorticosterone ace-
tate (DOCA)-treated miniature swine model. B, Prevention of hypertension with early renal nerve ablation (RNA) and blood pressure
(BP) reduction to normal when RNA was performed 4 weeks after insulin infusion. Reprinted from Huang et al
34
with permission from
Hypertension and from OHagan et al
33
with permission from American Journal of Hypertension.
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1444 Circulation April 1, 2014
of lesions. The basket is collapsed, can be expanded by an
external mechanism, can achieve good wall apposition, and
can deliver thermal injury and ber interruption in a desir-
able and predictable way. The other 2 systems, the Vessix V2
system (Vessix Vascular-Boston Scientic), and the OneShot
system (Covidien), have the electrodes mounted on a balloon.
The Iberis system (Terumo) has a 4-French shaft that enables
radial access. The Paradise system using ultrasound tech-
nology has also been approved in Europe (ReCor Medical).
Below we briey review the studies performed to date and
attempt a well-intended critique of existing data.
The rst in-human proof-of-concept study (Symplicity I)
evaluated 50 patients with treatment-resistant hypertension.
41
Of those, 45 were eligible for RNA and composed the treat-
ment group. BP reduction with RNA was signicant, smaller
in the rst month after RNA (14/10 mm Hg), and more pro-
nounced at 6-month and 1-year follow-up (27/17 mm Hg;
Figure 4). Ambulatory BP monitoring (ABPM) was done in
a small number of patients and demonstrated much less BP
reduction (11 mm Hg for systolic BP [SBP]).
The second study was randomized but not blinded and
performed soon after in a larger sample of 106 patients
with resistant hypertension and similar characteristics to the
proof-of-concept study.
42
RNA was performed in 52 patients,
whereas standard antihypertensive medications were contin-
ued in the remaining 54 patients. BP dropped signicantly in
the rst month in the active RNA group, but BP reduction was
much greater at 6 months (32/12 mm Hg). BP change was
minimal in the control group (1/0 mm Hg). BP reduction was
signicantly less in a smaller group of 20 patients who under-
went ambulatory BP measurement (11/7 mm Hg).
The Symplicity trials created a great deal of enthusiasm
and captured the imagination of the hypertension and inter-
ventional community alike. Nevertheless, these early studies
Baseline av 24 hr Ambulatory Blood Pressure
0
20
40
60
80
100
120
140
160
180
200
Symplicity-HTN I Symplicity-HTN II EnligHTN-I Sleep Apnea ABPM
Systolic BP Diastolic BP
N=12 N=20 N=46 N=10 N=303
Baseline Office Blood Pressure
0
20
40
60
80
100
120
140
160
180
200
Symplicity-HTN ISymplicity-HTN II EnligHTN-I Sleep Apnea ABPM
Systolic BP Diastolic BP
N=45 N=52 N=46 N=10 N=303
Change in ABPM: Symplicity-HTN I
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Change in Office BP: Symplicity-HTN I
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6 Month-12
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Change in Office BP: Symplicity-HTN II
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6
Change in ABPM: Symplicity-HTN II
Figure 4 (Continued). Baseline ofce and 24-hour ambulatory blood pressures and changes after renal denervation in 5 studies that
included both ofce and ambulatory blood pressure measurements (ABPM).
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1445
were accompanied by a number of questions and inconsisten-
cies, described below.
Initial ofce BP reduction was modest and improved with
time. The number of patients reported at each time point was
different (smaller at later time points), which raises the pos-
sibility that nonresponders were excluded. Other possibili-
ties include regression to the mean, improvement in patient
compliance, medication manipulation, or lifestyle changes.
Remodeling of resistance vessels has also been suggested by
the authors. The lack of placebo effect noted in Symplicity
II is also highly unusual for hypertension studies. The bigger
problem, however, with the Symplicity and other trials is the
discrepancy between ofce BP measurements and ABPM. A
small disparity in ofce and average 24-hour ambulatory BP
reduction is expected and has been reported previously; large
disparities, however, are unusual and raise questions.
43
There was a considerable discrepancy between average
ofce BP and average 24-hour BP at baseline, as well as a big
difference in the magnitude of BP reduction during follow up in
the Symplicity trials (Figure 4). Ambulatory BP was performed
only in a small subset of patients (12 of 45 patients in Symplicity
I and 20 of 49 patients in the active group of Symplicity II), and
BP reduction was only 41% and 34% of ofce BP reduction
in the 2 studies. A meta-analysis of antihypertensive drug ther-
apy revealed that ambulatory BP reduction should be 65% of
the reduction seen in ofce BP.
44
Similar disparities have been
noted in most recently published denervation trials.
We recently reported the 6-month data from the rst-in-
human trial, EnligHTN I.
45
This study included 46 patients
with resistant hypertension and baseline characteristics sim-
ilar to the Symplicity population. All of the patients under-
went RNA using a standardized technique aiming to achieve
complete renal denervation. In this rst in-human study,
ofce BP was reduced signicantly and substantially in
the rst month (28/10 mm Hg) and remained at the same
levels for 6 months. Results from all of the patients were
reported at all of the time points. Ambulatory BP measure-
ment was performed in all of the patients and demonstrated a
10/5-mm Hg reduction in average 24-hour BP, which also
remained the same until the 6-month follow-up. However,
Change in ABPM: EnligHTN-I
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6
Change in Office BP: EnligHTN-I
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6
Change in ABPM: Sleep Apnea
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6
Change in Office BP: Sleep Apnea
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6
Change in av 24 hr ambulatory BP: ABPM study
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6 Month-12
Change in Office BP: ABPM study
-35
-30
-25
-20
-15
-10
-5
0
Systolic BP Diastolic BP
Month-1 Month-3 Month-6 Month-12
Figure 4 (Continued).
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1446 Circulation April 1, 2014
the discrepancy between ofce and ambulatory BP reduction
remained. Baseline ofce SBP and heart rate correlated sig-
nicantly with BP response at 6 months.
46
Although several other studies reported signicant BP reduc-
tion after RNA, only a few performed ABPM to evaluate the
magnitude of BP reduction (Figure 4). A small study was per-
formed by Witkowski et al
47
in 10 patients with sleep apnea and
drug-resistant hypertension. The authors found a signicant
reduction in ofce BP at 3 and 6 months after RDN (34/13
mm Hg) but only a small change in SBP measured by ABPM (6
mm Hg). Another small study, by Hering et al,
48
in 15 patients
with moderate and severe chronic kidney disease and resistant
hypertension showed impressive ofce BP reduction at 3 and 6
months post-RNA (27/14 and 29/14 mm Hg, respectively),
but ABPM reductions were small and did not reach statistical
signicance (6/7 and 5/6 mm Hg, respectively). A pilot
study using the OneShot system in 8 patients with resistant
hypertension showed similar results.
49
After RNA, ofce BP
was reduced by 34/12 mm Hg at 6 months, but ABPM reduc-
tions were once again disappointingly small (3/4 mm Hg).
Recently, a larger study presented a series of patients who
underwent RNA for resistant hypertension and specically
examined the BP response as measured by ABPM.
50
In this
study, 346 patients with uncontrolled hypertension were eval-
uated. Of those, 303 patients were found by daytime ABPM
to have true resistant hypertension, and 43 had pseudoresis-
tant hypertension (ofce SBP, 16120 mm Hg; 24-hour SBP,
12120 mm Hg). At 3, 6, and 12 months of follow-up, ofce
SBP was reduced by 21/24/27 mm Hg and ofce diastolic BP
by 9/9/12 mm Hg. In patients with true treatment-resistant
hypertension, there was a signicant reduction in 24-hour
SBP (10/10/12 mm Hg; P<0.001) and diastolic BP (5/5/7
mm Hg; P<0.001) at 3, 6, and 12 months, respectively. There
was no effect on ABPM in pseudoresistant patients, whereas
ofce BP was reduced to a similar extent. The ndings of this
larger study were in line with the ndings of the 2 Symplicity
trials and the EnligH I study, conrming the antihyper-
tensive effect of RNA but once again demonstrating a much
smaller BP reduction when assessed by ABPM. This article
was accompanied by an editorial that criticized the results.
51
Figure 4 presents baseline ofce and 24-hour ambulatory BPs
and BP changes after RNA in 5 studies that included both
measures. Consistently the ABPM measurements are substan-
tially lower than the ofce measurements.
The mechanisms underlying the disparity between ofce
and ambulatory BP reduction remain poorly understood. We
proposed recently that the white coat effect might be impli-
cated, at least in part,
43
whereas regression to the mean and
other unclaried mechanisms might also apply. Of great inter-
est, the reduction in ofce and ambulatory BP was almost
identical in a recent study of 54 patients with moderate true
resistant hypertension (ofce BP between 140/90 and 160/100
mm Hg).
52
The ndings of the latter study offer another poten-
tial contributing factor, that is, the level of BP values before
applying RNA. It is known that the magnitude of BP reduc-
tion greatly depends on pretreatment levels, both with drug
therapy
53
and RNA.
54,55
It is therefore expected for BP reduc-
tion to be larger when pretreatment BP is higher (usually the
ofce BP) than when it is lower (usually the ambulatory BP).
Indeed, it was found that the reduction in ambulatory BP tends
to approach the ofce BP fall as the pretreatment BP levels
become lower.
56
However, further basic and clinical research
is needed to clarify the mechanisms underlying the disparity
and identify ways to overcome this problem.
Other published studies presented negative results. In 1
study, 12 patients with difcult-to-control hypertension
underwent RNA,
57
and results were recorded before and 5
months after denervation. Results indicated that RNA did
not change resting muscle sympathetic nerve activity, heart
rate, or heart rate variability, and there was no change in
ofce BP. One explanation for the results of this study is
patient selection. Patients had lower baseline BP (157/85
mm Hg), and more importantly many of them (5 of 12; 42%)
had normal BP (SBP <140 mm Hg), questioning the choice
of RNA for patient management.
58
Furthermore, there was
no evidence of sympathetic activation (heart rate of 60 beats
per minute and normal muscle sympathetic nerve activity
discharge) at baseline;
59
despite this, heart rate was reduced
in 60% of these patients.
Future Directions: Other Potential
Applications of RNA
RNA might be benecial in other disease states characterized
by enhanced sympathetic activity, including chronic kidney
disease, congestive HF, sympathetically driven arrhythmias,
obstructive sleep apnea, and polycystic ovary syndrome.
RNA may eventually nd a role as a supplemental procedure
to improve outcomes in high-risk patients, such as patients
with coronary heart disease and or chronic kidney disease.
The Table presents a number of disease states accompanied
Table. Potential Targets for Renal Denervation Across
the Cardiometabolic Continuum and Other Disease States
Associated With Enhanced Sympathetic Activity
Cardiometabolic Targets Other Disease States
Metabolic syndrome* Chronic kidney disease 1-3a
Obesity* Chronic kidney disease 3b-4
Diabetes mellitus Chronic kidney disease ESRD
Hypertension mild* Chronic kidney disease peritoneal
Hypertension difcult to control hemodialysis*
Hypertension resistant Polycystic kidney disease
Atherosclerosis* Loin hematuria*
Coronary artery disease* Obstructive sleep apnea
Left ventricular hypertrophy Polycystic ovary syndrome
Diastolic LV dysfunction Cirrhosis*
Heart failure with preserved EF*
Systolic heart failure
Atrial brillation
Ventricular tachyarrhythmia
Sudden death*
LV indicates left ventricular; EF, ejection fraction; ESRD, end-stage renal
disease.
*No data available.
Limited data available.
Robust data available.
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1447
by sympathetic overactivity that potentially can benet
from RNA. Case reports or small pilot studies have been
reported in many of these populations and they are briey
mentioned below.
Hypertension
Drug-resistant hypertension will remain the primary target
for RNA, because this is a population with unmet medical
need and data so far look encouraging. When the random-
ized, blinded control trials in the United States are completed
(assuming positive results), RNA may become the procedure
of choice for these patients. Before getting there, however,
attention should be focused on key issues, such as preproce-
dural diagnostic workup, eligibility criteria for RNA, predic-
tors of response, and markers of success.
The diagnostic workup should aim to exclude secondary
causes of resistance (renal artery stenosis, primary hyperal-
dosteronism, pheochromocytoma, hyperthyroidism, etc), ana-
tomic abnormalities that would preclude RNA (multiple, small
caliper renal arteries or very tortuous or heavily calcied renal
arteries), and most importantly white coat hypertension. Large
observational studies have shown that white coat hypertension
can be detected in approximately one third of patients with
resistant hypertension.
38
The importance of pseudoresistance
has been highlighted in the study by Mahfoud et al,
50
which
demonstrated no response to RNA measured by ABPM in this
population. We, therefore, strongly believe that ABPM should
be mandatory in all patients considered for RNA to exclude
pseudoresistance.
43
Adherence to drug therapy and lifestyle
modication should also be thoroughly assessed, because they
frequently account for drug resistance. Furthermore, optimi-
zation of the drug regimen to include an aldosterone antago-
nist (spironolactone or eplerenone) should be implemented in
most patients before considering RNA. Exceptions, however,
can be considered for patients with drug-resistant hyperten-
sion because of habitual noncompliance or inability or unwill-
ingness to take prescribed medication.
The criteria for RNA eligibility currently include patients
with resistant hypertension and SBP levels >160 mm Hg
(150 mm Hg for patients with diabetes mellitus and estab-
lished cardiovascular disease), largely on the basis of the 2
Symplicity trials and the EnligHTN I study. However, pilot
studies already explore the efcacy and safety of RNA in
milder forms of resistant hypertension, that is, SBP between
140 and 160 mm Hg. In 2 studies of 20 and 54 such patients,
BP was reduced by 13/5 and 13/7 mm Hg, respectively, at 6
months post-RNA.
52,60
The European Society of Hypertension
and the European Society of Cardiology have recently pub-
lished position articles regarding RNA in an effort to clarify
eligibility criteria and avoid the wide application of RNA in
patients with questionable efcacy.
61,62
Efforts to identify predictors of response and markers of
procedural success currently remain elusive. As of today, only
baseline BP
46,50
and, to a lesser extent, baseline heart rate
46
have been shown to correlate with BP response after RNA,
whereas indices of sympathetic overactivity, such as muscle
sympathetic nerve activity or plasma noradrenaline levels,
do not correlate with BP response.
57,63
Renal blood ow and
electric stimulation of renal arterial nerves have been recently
proposed as markers of procedural success
64,65
; but both mark-
ers need validation in larger studies. Of note, heart rate was
signicantly reduced after RNA in some studies,
46,66
suggest-
ing that heart rate reduction might serve as a sensitive surro-
gate of RNA success.
Finally, the relative contribution of afferent and effer-
ent renal denervation in BP reduction in humans needs fur-
ther exploration. Partial attenuation of systemic sympathetic
activity, indicating afferent denervation, has been shown in
some
41,42,48,63
but not all
52
studies, whereas functional signals
of efferent denervation have been reported in some studies
as well. However, available data do not allow conclusions on
whether denervation of afferent or efferent bers is the main
contributor to BP reduction.
Milder Forms of Hypertension
RNA may have a role in the vastly larger population with
mild-to-moderate hypertension, but it is still too early to tell. It
seems very attractive to use RNA in this population to achieve
better BP control, to decrease the amount of antihypertensive
medication needed, or even to avoid lifelong drug therapy
altogether. Milder forms of hypertension, however, are less
likely to be associated with SNS activation, and patients with
lower baseline BP are less likely to respond to RNA. Yet, there
may be subgroups of these patients who can benet from the
procedure. These include patients who can be controlled on a
medical regimen but are intolerant to medication, those who
report frequent adverse effects, or those who simply they do
not like taking medicines. However, long-term (5 years)
efcacy and safety data are needed before RNA can be rec-
ommended for this population. Another attractive population
for RNA includes the newly diagnosed young patients with
known SNS overactivity. If RNA proves to be effective and
safe in this patient population, it may be possible to avoid,
attenuate, or delay lifelong drug therapy and even prevent tar-
get organ damage.
Heart Failure
A vast amount of evidence indicates that SNS is overacti-
vated in HF and greatly contributes to the poor outcome of
this patient population.
17,67
Furthermore, HF is characterized
by neurohormonal activation, increased vascular resistance,
and sodium and uid retention, all of which can be favor-
ably inuenced by renal denervation. Therefore, RNA seems
an attractive adjunct procedure to existing drug therapies
in patients with either systolic or diastolic HF. The inhibi-
tory effects of RNA on the renin-angiotensin system may
confer an additional benet in these patients. In a small
nonrandomized study of 7 HF patients with reduced ejec-
tion fraction (Renal Artery Denervation in Chronic Heart
Failure-Pilot study), RNA showed an increase in exercise
capacity,
68
and a larger study to assess cardiovascular out-
comes (Renal Sympathetic Denervation for Patients With
Chronic Heart Failure [RSD4CHF]) is currently underway.
Likewise, signicant improvements in myocardial structural
and functional characteristics have been observed in patients
with resistant hypertension and left ventricular hypertrophy.
Some of these patients (approximately one fourth) presented
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1448 Circulation April 1, 2014
with HF and preserved ejection fraction.
69
A large outcome
study (Denervation of the renAl sympathetIc nerveS in hearT
Failure With nOrmal Lv Ejection Fraction [DIASTOLE]) in
HF patients with preserved ejection fraction is now underway.
Chronic Kidney Disease
Overactivity of SNS has long been shown in animal models
with CKD
70
and has recently been veried in patients with
end-stage renal disease (ESRD) undergoing hemodialysis
27
and in renal transplant
28
patients. The diseased kidneys have
been shown to be the source of SNS overactivity, which was
attenuated by bilateral surgical removal of the native kid-
neys.
27,28
Therefore, RNA seems an attractive option for the
inhibition of SNS overactivity in these patients. Indeed, RNA
was successful and effective in 2 case reports of patients with
ESRD,
71,72
in a larger group of 15 patients with moderate
and severe CKD,
48
and in a study of 9 patients with ESRD.
73
Large multicenter studies are currently underway to further
evaluate the effects of RNA in CKD. It is worth noting that,
in this population, available data indicate that renal function
does not deteriorate after RNA, and safety and efcacy for BP
response are similar as that found in patients without CKD.
54
Renal function was meticulously assessed using biomark-
ers for functional and structural kidney damage and found to
remain unaltered both in patients with and without CKD,
74
thus addressing previously raised concerns.
75
Furthermore,
renal function may improve with time in patients with mild-
to-moderate CKD, because RNA may result in improvement
in renal blood ow. This group of patients is known to have
high cardiovascular risk,
70
which may be partially mediated
by sympathetic activation and merits further study. Patients
with mild-to- moderate CKD should specically be studied for
improvement in cardiovascular outcomes after RNA, or stud-
ies of RNA should be specically designed for this patient
population. Finally, RNA is under investigation for the alle-
viation of pain in patients with polycystic kidney disease
76
and
loin pain hematuria.
77
Cardiac Arrhythmias
The SNS plays a crucial role in the pathogenesis and mainte-
nance of atrial and ventricular arrhythmias.
78
Data presented
recently at the annual American College of Cardiology meet-
ing from our group from 14 patients with resistant hyperten-
sion indicate that RNA can result in impressive reduction of
both supraventricular and ventricular ectopic activity.
79
The effect of RNA on AF has been addressed in other studies.
Data in pigs
80
and dogs
81
indicate that RNA reduces the induc-
ibility of AF and attenuates the ventricular rate. In humans, 27
patients with a history of symptomatic paroxysmal or persis-
tent refractory AF and resistant hypertension were randomly
assigned to pulmonary vein isolation (PVI) only or PVI with
RNA.
82
RNA with PVI was more effective than PVI alone
in preventing the recurrence of atrial brillation and reduc-
ing BP (27/12 mm Hg) at 6 months and 1 year. A large,
multicenter randomized study (Adjunctive Renal Sympathetic
Denervation to Modify Hypertension as Upstream Therapy
in the Treatment of Atrial Fibrillation [H-FIB]) is currently
underway, and results are eagerly awaited. RNA was recently
performed in 2 patients with congestive HF and ventricular
tachy- arrhythmias (monomorphic ventricular tachycardia,
recurrent polymorphic ventricular tachycardia, and ventricular
brillation) resistant to therapy.
83
RNA resulted in successful
termination of ventricular arrhythmias and patient discharge.
Obstructive Sleep Apnea
Sympathetic activity is enhanced and is thought to play a piv-
otal role in obstructive sleep apnea.
16,20
In animal models of
obstructive sleep apnea, RNA attenuated postapneic BP eleva-
tions in pigs and increased water excretion in rats.
80,84
RNA
was evaluated recently in 10 patients with obstructive sleep
apnea and resistant hypertension in a small, uncontrolled
study.
47
BP results have been discussed above. In addition, a
signicant improvement in sleep apnea severity was observed.
The median apnea-hypopnea index was reduced from 16.3
episodes per hour at baseline to 4.5 events per hour post-RNA,
suggesting that sympathetic overactivity is a major contributor
in sleep apnea severity and that RNA- induced attenuation of
sympathetic drive signicantly alleviates disease expression.
The study, however, is small, and larger numbers are needed to
evaluate the role of RNA as an adjunct therapy to continuous
positive airway pressure in patients with sleep apnea.
Polycystic Ovary Syndrome
Polycystic ovary syndrome is a common disorder in women
of reproductive age, characterized by endocrine abnormalities
coupled with metabolic disturbances. Sympathetic activity is
enhanced in women with this syndrome.
19
RNA performed in
2 young women with polycystic ovary syndrome
85
resulted
in moderate ofce BP reduction, substantial improvement in
insulin sensitivity, and reappearance of menses in 1 patient
who remained amenorrheic for 3 years. These data suggest
that RNA may result not only in BP reduction but also in
improvement in disease state. It is too early, however, to draw
any denite conclusions.
There are many more disease states that can potentially
become therapeutic targets for RNA that are beyond the scope
of this contemporary review (Table). These include patients
with metabolic syndrome/diabetes mellitus because RNA has
been shown to improve insulin resistance,
86
patients present-
ing with ST elevation myocardial infarction to prevent reverse
left ventricular remodeling (RNA can potentially be done
after primary percutaneous coronary intervention), and high-
risk patients to improve cardiovascular outcomes. The latter
will require long-term studies that include a large number of
high-risk patients, preferably with evidence of SNS activation,
including patients with CKD. One such study is underway (in
the design phase) and currently is planned to include >5000
patients (EnligHTMENT).
Commentary
Any new procedure or therapeutic approach to be accepted
by the medical community needs to be safe and effective. The
safety of RNA has been pretty well established. So far, only
rare cases of renal artery stenosis have been reported, and no
other signals of serious adverse events have been identied.
Long-term safety data, however, need to be accumulated. So
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1449
far, vascular complications have been reported rarely and were
inconsequential. Small hematomas, pseudo-aneurisms, minor
bleeds, some vasospasm of the renal artery post-RNA, and
1 dissection requiring stenting, but no serious or life threat-
ening adverse events, have been reported. The concern of
renal artery stenosis development is legitimate and has been
observed previously with RF ablation for AF in pulmonary
veins and coronary arteries adjacent to accessory pathways in
patients with Wolff-Parkinson-Whit syndrome. Fortunately,
so far only 2 cases of several thousand procedures have been
reported as procedure related. The effect on renal function has
been closely watched, and so far only minor deterioration of
estimated glomerular ltration rate and increase in serum cre-
atinine has been noted. No major renal function events have
been reported.
There is little doubt that RNA is effective in most patients
with renal-mediated sympathetic hyperactivity and resistant
hypertension. The overall magnitude of BP response, how-
ever, still needs to be determined. BP is a dynamic measure
and has considerable variability, particularly among patients
with resistant hypertension. Until well-done, blinded,
placebo- controlled, sham-masked studies are completed,
we will not be certain about the true effect of RNA in this
population. Sham-controlled studies are underway in the
United States (Symplicity III and EnligHTN IV).* These
studies will include a large number of patients with strict
evaluation at baseline, a sham-controlled arm, and separate
teams performing the interventional procedure and medi-
cal follow-up. Patients in these studies will be evaluated by
means of ofce BP and ABPM. Without doubt, these stud-
ies will provide credible information and allow the eld to
move forward. When these studies are completed, we may
nd out that the BP reduction overall is smaller than cur-
rently reported, but in these high-risk patients with uncon-
trolled hypertension, any BP reduction is welcome. It is also
a fact that current data suggest that not all patients respond
to RNA. There are undoubtedly some patients who demon-
strate dramatic BP reductions and others who do not respond
at all. Presumably the good responders are those with renal-
mediated sympathetic activation, whereas the nonresponders
have hypertension mediated by other mechanisms. It is
urgent and important, therefore, to seek and develop mark-
ers of good response so as to appropriately direct RNA to
the right patient population. The effect of RNA in the many
other disease states accompanied by sympathetic hyperactiv-
ity (Table) deserves careful study and consideration.
Acknowledgments
We acknowledge the contribution of Drs Doumas and Rashidi in the
creation of some of the gures included in this article. This was above
and beyond their contribution to the writing of the article.
Disclosures
Drs Papademetriou and Tsious are investigators and coauthors of
the EnligHTN I article and consultants to St Jude Medical. The other
authors report no conicts.
References
1. Bradford JR. The innervation of the renal blood vessels. J Physiol.
1889;10:358432.18.
2. Author unknown. Neurosurgical treatment, indications and results (chap-
ter 7, methods of operation). J Intern Med. 1947;127:7276.
3. Adson AW, McCraig W, Brown GE. Surgery in its relation to hyperten-
sion. Surg Gynecol Obstet. 1936;62:314331.
4. Weiss E. Recent advances in the pathogenesis and treatment of hyperten-
sion, a review. Psychosom Med. 1939;1:180198.
5. Sen SK. Some observations on decapsulation and denervation of the kid-
ney. Brit J Urol. 1936;8:319328.
6. Papin E, Ambard L. Resection of the nerves of the kidney for nephralgia
and small hydronephroses. J Urol. 1924;11:337349.
7. Page IH, Heuer GJ. The effect of renal denervation on the level of arterial
blood pressure and renal function in essential hypertension. J Clin Invest.
1935;14:2730.
8. Page IH, Heuer GJ. The effect of renal denervation on patients suffering
from nephritis. J Clin Invest. 1935;14:443458.
9. Peet MM. Hypertension and its surgical treatment by supradiaphragmatic
splanchnicectomy. Am J Surg. 1948;LXXV:4868.
10. Smithwick RH, Thompson JE. Splanchnicectomy for essential hyperten-
sion; results in 1,266 cases. J Am Med Assoc. 1953;152:15011504.
11. Peet MM, Woods WW, Braden S. The surgical treatment of hypertension.
JAMA. 1940;115:18751885.
12. Freis ED, Wanko A, Wilson IM, Parrish AE. Treatment of essential hyper-
tension with chlorothiazide (diuril); its use alone and combined with other
antihypertensive agents. J Am Med Assoc. 1958;166:137140.
13. VA Cooperative Study Group. Effects of treatment on morbidity in hyper-
tension. Results in patients with diastolic blood pressures averaging 115
through 129 mm Hg. JAMA. 1967;202:10281034.
14. Wallin BG, Charkoudian N. Sympathetic neural control of integrated car-
diovascular function: insights from measurement of human sympathetic
nerve activity. Muscle Nerve. 2007;36:595614.
15. Grassi G, Seravalle G, Quarti-Trevano F. The neuroadrenergic hypoth-
esis in hypertension: current evidence. Exp Physiol. 2010;95:581586.
16. Fisher JP, Young CN, Fadel PJ. Central sympathetic overactivity: maladies
and mechanisms. Auton Neurosci. 2009;148:515.
17. Floras JS. Sympathetic nervous system activation in human heart fail-
ure: clinical implications of an updated model. J Am Coll Cardiol.
2009;54:375385.
18. Grassi G, Quarti-Trevano F, Seravalle G, Arenare F, Volpe M, Furiani S,
DellOro R, Mancia G. Early sympathetic activation in the initial clinical
stages of chronic renal failure. Hypertension. 2011;57:846851.
19. Sverrisdttir YB, Mogren T, Kataoka J, Janson PO, Stener-Victorin E. Is
polycystic ovary syndrome associated with high sympathetic nerve activity
and size at birth? Am J Physiol Endocrinol Metab. 2008;294:E576E581.
20. Prabhakar NR, Kumar GK. Mechanisms of sympathetic activation
and blood pressure elevation by intermittent hypoxia. Respir Physiol
Neurobiol. 2010;174:156161.
21. Stadlbauer V, Stadlbauer VP, Wright GA, Banaji M, Mukhopadhya A,
Mookerjee RP, Mookerjee R, Moore K, Jalan R. Relationship between
activation of the sympathetic nervous system and renal blood ow auto-
regulation in cirrhosis. Gastroenterology. 2008;134:111119.
22. DiBona GF, Esler M. Translational medicine: the antihypertensive
effect of renal denervation. Am J Physiol Regul Integr Comp Physiol.
2010;298:R245R253.
23. Campese VM, Ku E, Park J. Sympathetic renal innervation and resistant
hypertension. Int J Hypertens. 2011;2011:814354.
24. DiBona GF. Physiology in perspective: the wisdom of the bodyneu-
ral control of the kidney. Am J Physiol Regul Integr Comp Physiol.
2005;289:R633R641.
25. Webb RL, Brody MJ. Functional identication of the central projections
of afferent renal nerves. Clin Exp Hypertens A. 1987;9(suppl 1):4757.
26. Campese VM, Kogosov E. Renal afferent denervation prevents hypertension
in rats with chronic renal failure. Hypertension. 1995;25(4 pt 2):878882.
27. Converse RL Jr, Jacobsen TN, Toto RD, Jost CM, Cosentino F, Fouad-
Tarazi F, Victor RG. Sympathetic overactivity in patients with chronic
renal failure. N Engl J Med. 1992;327:19121918.
*About three months after this paper was accepted for publication
it became known that EnligHTN IV was suspended (due to slow
enrollment). Continuation of the study will be re-evaluated after the
results of Symplicity HTN III are fully analyzed. In the meantime, the
sponsors of Symplicity HTN III announced that the study failed to meet
its primary end point, although the study met its primary safety objective.
While details from Symplicity III are anxiously awaited, we feel that
these developments in no way affect statements and opinions expressed
throughout this manuscript.
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
1450 Circulation April 1, 2014
28. Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters
K, Dietl KH, Rahn KH. Sympathetic nerve activity in end-stage renal dis-
ease. Circulation. 2002;106:19741979.
29. Malpas SC, Evans RG. Do different levels and patterns of sympa-
thetic activation all provoke renal vasoconstriction? J Auton Nerv Syst.
1998;69:7282.
30. DiBona GF, Sawin LL. Effect of renal nerve stimulation on NaCl and H2O
transport in Henles loop of the rat. Am J Physiol. 1982;243:F576F580.
31. Smyth DD, Umemura S, Pettinger WA. Renal nerve stimulation
causes alpha 1-adrenoceptor-mediated sodium retention but not alpha
2-adrenoceptor antagonism of vasopressin. Circ Res. 1985;57:304311.
32. Osborn JL, DiBona GF, Thames MD. Beta-1 receptor mediation of renin
secretion elicited by low-frequency renal nerve stimulation. J Pharmacol
Exp Ther. 1981;216:265269.
33. OHagan KP, Thomas GD, Zambraski EJ. Renal denervation decreases
blood pressure in DOCA-treated miniature swine with established hyper-
tension. Am J Hypertens. 1990;3:6264.
34. Huang WC, Fang TC, Cheng JT. Renal denervation prevents and
reverses hyperinsulinemia-induced hypertension in rats. Hypertension.
1998;32:249254.
35. Schauerte P, Scherlag BJ, Scherlag MA, Goli S, Jackman WM, Lazzara
R. Ventricular rate control during atrial brillation by cardiac parasym-
pathetic nerve stimulation: a transvenous approach. J Am Coll Cardiol.
1999;34:20432050.
36. Schauerte P, Scherlag BJ, Pitha J, Scherlag MA, Reynolds D, Lazzara R,
Jackman WM. Catheter ablation of cardiac autonomic nerves for preven-
tion of vagal atrial brillation. Circulation. 2000;102:27742780.
37. Persell SD. Prevalence of resistant hypertension in the United States,
2003-2008. Hypertension. 2011;57:10761080.
38. De la Sierra A, Segura J, Banegas JR, Gorostidi M, De la Cruz JJ, Armario
P, Oliveras A, Ruilope LM. Clinical features of 8295 patients with resis-
tant hypertension classied on the basis of ambulatory blood pressure
monitoring. Hypertension. 2011;57:898902.
39. Doumas M, Douma S. Renal sympathetic denervation: the jury is still out.
Lancet. 2010;376:18781880.
40. Atherton DS, Deep NL, Mendelsohn FO. Micro-anatomy of the renal
sympathetic nervous system: a human postmortem histologic study. Clin
Anat. 2012;25:628633.
41. Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus
K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler
M. Catheter-based renal sympathetic denervation for resistant hyperten-
sion: a multicentre safety and proof-of-principle cohort study. Lancet.
2009;373:12751281.
42. Symplicity HTN-2 Investigators. Renal sympathetic denervation in
patients with treatment-resistant hypertension (the Symplicity HTN-2
Trial): a randomised controlled trial. Lancet. 2010;376:19031909.
43. Doumas M, Anyfanti P, Bakris G. Should ambulatory blood pressure
monitoring be mandatory for future studies in resistant hypertension: a
perspective. J Hypertens. 2012;30:874876.
44. Mancia G, Parati G. Ofce compared with ambulatory blood pressure
in assessing response to antihypertensive treatment: a meta-analysis.
J Hypertens. 2004;22:435445.
45. Worthley SG, Tsious CP, Worthley MI, Sinhal A, Chew DP, Meredith IT,
Malaiapan Y, Papademetriou V. Safety and efcacy of a multi- electrode
renal sympathetic denervation system in resistant hypertension: the
EnligHTN I trial. Eur Heart J. 2013;34:21322140.
46. Papademetriou V, Tsious C, Worthley M, Chew D, Meredith I, Malaiapan
Y, Sinhal A, Worthley SG. Percutaneous sympathetic renal denervation
in patients with drug-resistant hypertension: results from the EnligHTN,
rst-in-human multi-center study. J Clin Hypertens. 2013;15:516517.
47. Witkowski A, Prejbisz A, Florczak E, Kdziela J, liwiski P, Biele P,
Michaowska I, Kabat M, Warcho E, Januszewicz M, Narkiewicz K, Somers
VK, Sobotka PA, Januszewicz A. Effects of renal sympathetic denervation
on blood pressure, sleep apnea course, and glycemic control in patients with
resistant hypertension and sleep apnea. Hypertension. 2011;58:559565.
48. Hering D, Mahfoud F, Walton AS, Krum H, Lambert GW, Lambert EA,
Sobotka PA, Bhm M, Cremers B, Esler MD, Schlaich MP. Renal denerva-
tion in moderate to severe CKD. J Am Soc Nephrol. 2012;23:12501257.
49. Ormiston JA, Watson T, van Pelt N, Stewart R, Stewart JT, White JM,
Doughty RN, Stewart F, Macdonald R, Webster MW. Renal denerva-
tion for resistant hypertension using an irrigated radiofrequency balloon:
12-month results from the Renal Hypertension Ablation System (RHAS)
trial. EuroIntervention. 2013;9:7074.
50. Mahfoud F, Ukena C, Schmieder RE, Cremers B, Rump LC, Vonend O,
Weil J, Schmidt M, Hoppe UC, Zeller T, Bauer A, Ott C, Blessing E,
Sobotka PA, Krum H, Schlaich M, Esler M, Bhm M. Ambulatory blood
pressure changes after renal sympathetic denervation in patients with
resistant hypertension. Circulation. 2013;128:132140.
51. Parati G, Ochoa JE, Bilo G. Renal sympathetic denervation and daily
life blood pressure in resistant hypertension: simplicity or complexity?
Circulation. 2013;128:315317.
52. Ott C, Mahfoud F, Schmid A, Ditting T, Sobotka PA, Veelken R, Spies
A, Ukena C, Laufs U, Uder M, Bhm M, Schmieder RE. Renal dener-
vation in moderate treatment-resistant hypertension. J Am Coll Cardiol.
2013;62:18801886.
53. Lacourcire Y, Crikelair N, Glazer RD, Yen J, Calhoun DA. 24-Hour
ambulatory blood pressure control with triple-therapy amlodipine, valsar-
tan and hydrochlorothiazide in patients with moderate to severe hyperten-
sion. J Hum Hypertens. 2011;25:615622.
54. Mahfoud F, Cremers B, Janker J, Link B, Vonend O, Ukena C, Linz D,
Schmieder R, Rump LC, Kindermann I, Sobotka PA, Krum H, Scheller B,
Schlaich M, Laufs U, Bhm M. Renal hemodynamics and renal function
after catheter-based renal sympathetic denervation in patients with resis-
tant hypertension. Hypertension. 2012;60:419424.
55. Symplicity HTN-1 Investigators. Catheter-based renal sympathetic dener-
vation for resistant hypertension: durability of blood pressure reduction
out to 24 months. Hypertension. 2011;57:911917.
56. Head GA, Mihailidou AS, Duggan KA, Beilin LJ, Berry N, Brown MA,
Bune AJ, Cowley D, Chalmers JP, Howe PR, Hodgson J, Ludbrook
J, Mangoni AA, McGrath BP, Nelson MR, Sharman JE, Stowasser M;
Ambulatory Blood Pressure Working Group of the High Blood Pressure
Research Council of Australia. Denition of ambulatory blood pressure
targets for diagnosis and treatment of hypertension in relation to clinic
blood pressure: prospective cohort study. BMJ. 2010;340:c1104.
57. Brinkmann J, Heusser K, Schmidt BM, Menne J, Klein G, Bauersachs J,
Haller H, Sweep FC, Diedrich A, Jordan J, Tank J. Catheter-based renal
nerve ablation and centrally generated sympathetic activity in difcult-
to-control hypertensive patients: prospective case series. Hypertension.
2012;60:14851490.
58. Mahfoud F, Bhm M, Rump LC, Vonend O, Schmieder RE, Kintscher U.
Catheter-based renal nerve ablation and centrally generated sympathetic
activity in difcult-to-control hypertensive patients: prospective case
series. Hypertension. 2013;61:e17.
59. Schlaich M, Hering D, Lambert G, Lambert E, Esler M. Blood pres-
sure and sympathetic nervous system response to renal denervation.
Hypertension. 2013;61:e13.
60. Kaltenbach B, Franke J, Bertog SC, Steinberg DH, Hofmann I, Sievert H.
Renal sympathetic denervation as second-line therapy in mild resistant
hypertension: a pilot study. Catheter Cardiovasc Interv. 2013;81:335339.
61. Schmieder RE, Redon J, Grassi G, Kjeldsen SE, Mancia G, Narkiewicz
K, Parati G, Ruilope L, van de Borne P, Tsious C; European Society of
Hypertension. Updated ESH position paper on interventional therapy of
resistant hypertension. EuroIntervention. 2013;9(suppl R):R58R66.
62. Mahfoud F, Lscher TF, Andersson B, Baumgartner I, Cifkova R, Dimario
C, Doevendans P, Fagard R, Fajadet J, Komajda M, Lefvre T, Lotan
C, Sievert H, Volpe M, Widimsky P, Wijns W, Williams B, Windecker
S, Witkowski A, Zeller T, Bhm M; European Society of Cardiology.
Expert consensus document from the European Society of Cardiology on
catheter- based renal denervation. Eur Heart J. 2013;34:21492157.
63. Hering D, Lambert EA, Marusic P, Walton AS, Krum H, Lambert GW,
Esler MD, Schlaich MP. Substantial reduction in single sympathetic
nerve ring after renal denervation in patients with resistant hypertension.
Hypertension. 2013;61:457464.
64. Tsious C, Papademetriou V, Dimitriadis K, Tsiachris D, Thomopoulos
C, Park E, Hata C, Papalois A, Stefanadis C. Catheter-based renal sympa-
thetic denervation exerts acute and chronic effects on renal hemodynamics
in swine. Int J Cardiol. 2013;168:987992.
65. Chinushi M, Izumi D, Iijima K, Suzuki K, Furushima H, Saitoh O, Furuta
Y, Aizawa Y, Iwafuchi M. Blood pressure and autonomic responses to
electrical stimulation of the renal arterial nerves before and after ablation
of the renal artery. Hypertension. 2013;61:450456.
66. Ukena C, Mahfoud F, Spies A, Kindermann I, Linz D, Cremers B, Laufs
U, Neuberger HR, Bhm M. Effects of renal sympathetic denervation on
heart rate and atrioventricular conduction in patients with resistant hyper-
tension. Int J Cardiol. 2013;167:28462851.
67. Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon
AB, Rector T. Plasma norepinephrine as a guide to prognosis in patients
with chronic congestive heart failure. N Engl J Med. 1984;311:819823.
68. Davies JE, Manisty CH, Petraco R, Barron AJ, Unsworth B, Mayet J,
Hamady M, Hughes AD, Sever PS, Sobotka PA, Francis DP. First-in- man
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Papademetriou et al Renal Nerve Ablation: Perspectives 1451
safety evaluation of renal denervation for chronic systolic heart failure: pri-
mary outcome from REACH-Pilot study. Int J Cardiol. 2013;162:189192.
69. Brandt MC, Mahfoud F, Reda S, Schirmer SH, Erdmann E, Bhm M,
Hoppe UC. Renal sympathetic denervation reduces left ventricular hyper-
trophy and improves cardiac function in patients with resistant hyperten-
sion. J Am Coll Cardiol. 2012;59:901909.
70. Papademetriou V, Doumas M, Anyfanti P, Faselis C, Kokkinos P, Tsious
K. Renal nerve ablation for hypertensive patients with chronic kid-
ney disease [published online ahead of print July 31, 2013]. Curr Vasc
Pharmacol. doi: 10.2174/15701611113119990143. http://www.eurekas-
elect.com/113766/article. Accessed March 10, 2014.
71. Schlaich M. Sustained reduction of central sympathetic outow after renal
denervation in end stage renal disease. J Hypertens. 2011;29:e103.
72. Prochnau D, Lauten A, Busch M, Kuehnert H, Figulla HR, Surber R.
Catheter-based radiofrequency ablation therapy of the renal sympathetic-
nerve system for drug resistant hypertension in a patient with end-stage
renal disease. Int J Cardiol. 2012;154:e29e30.
73. Schlaich MP, Bart B, Hering D, Walton A, Marusic P, Mahfoud F, Bhm M,
Lambert EA, Krum H, Sobotka PA, Schmieder RE, Ika-Sari C, Eikelis N,
Straznicky N, Lambert GW, Esler MD. Feasibility of catheter- based renal
nerve ablation and effects on sympathetic nerve activity and blood pressure
in patients with end-stage renal disease. Int J Cardiol. 2013;168:22142220.
74. Drr O, Liebetrau C, Mllmann H, Achenbach S, Sedding D, Szardien
S, Willmer M, Rixe J, Troidl C, Elssser A, Hamm C, Nef HM. Renal
sympathetic denervation does not aggravate functional or structural renal
damage. J Am Coll Cardiol. 2013;61:479480.
75. Petidis K, Anyfanti P, Doumas M. Renal sympathetic denervation: renal
function concerns. Hypertension. 2011;58:e19; author reply e20.
76. Shetty SV, Roberts TJ, Schlaich MP. Percutaneous transluminal renal
denervation: a potential treatment option for polycystic kidney disease-
related pain? Int J Cardiol. 2013;162:e58e59.
77. de Beus E, Blankestijn PJ, Fox JG, Zoccali C. Catheter-based renal dener-
vation as a novel treatment for loin pain haematuria syndrome. Nephrol
Dial Transplant. 2013;28:21972199.
78. Doumas M, Faselis C, Tsious C, Papademetriou V. Carotid barorecep-
tor activation for the treatment of resistant hypertension and heart failure.
Curr Hypertens Rep. 2012;14:238246.
79. Tsious K, Papademetriou V, Tsiachris D, Dimitriadis K, Thomopoulos
C, Kefala A, Stefanadis C. Renal sympathetic denervation signicantly
reduces mean heart rate and exerts a favorable effect on atrial and ven-
tricular arrhythmias in resistant hypertensives. J Am Coll Cardiol.
2013;61:E1376.
80. Linz D, Mahfoud F, Schotten U, Ukena C, Neuberger HR, Wirth K, Bhm
M. Renal sympathetic denervation suppresses postapneic blood pres-
sure rises and atrial brillation in a model for sleep apnea. Hypertension.
2012;60:172178.
81. Zhao Q, Yu S, Zou M, Dai Z, Wang X, Xiao J, Huang C. Effect of renal
sympathetic denervation on the inducibility of atrial brillation during
rapid atrial pacing. J Interv Card Electrophysiol. 2012;35:119125.
82. Pokushalov E, Romanov A, Corbucci G, Artyomenko S, Baranova V, Turov
A, Shirokova N, Karaskov A, Mittal S, Steinberg JS. A randomized com-
parison of pulmonary vein isolation with versus without concomitant renal
artery denervation in patients with refractory symptomatic atrial brilla-
tion and resistant hypertension. J Am Coll Cardiol. 2012;60:11631170.
83. Ukena C, Bauer A, Mahfoud F, Schreieck J, Neuberger HR, Eick C,
Sobotka PA, Gawaz M, Bhm M. Renal sympathetic denervation for
treatment of electrical storm: rst-in-man experience. Clin Res Cardiol.
2012;101:6367.
84. Franquini JV, Medeiros AR, Andrade TU, Arajo MT, Moyss MR, Abreu
GR, Vasquez EC, Bissoli NS. Inuence of renal denervation on blood
pressure, sodium and water excretion in acute total obstructive apnea in
rats. Braz J Med Biol Res. 2009;42:214219.
85. Schlaich MP, Straznicky N, Grima M, Ika-Sari C, Dawood T, Mahfoud
F, Lambert E, Chopra R, Socratous F, Hennebry S, Eikelis N, Bhm M,
Krum H, Lambert G, Esler MD, Sobotka PA. Renal denervation: a poten-
tial new treatment modality for polycystic ovary syndrome? J Hypertens.
2011;29:991996.
86. Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, Brandt
MC, Hoppe UC, Vonend O, Rump LC, Sobotka PA, Krum H, Esler M,
Bhm M. Effect of renal sympathetic denervation on glucose metabo-
lism in patients with resistant hypertension: a pilot study. Circulation.
2011;123:19401946.
KEY WORDS: cardiology
hypertension
kidney
by JUAN ESPINOSA on April 7, 2014 http://circ.ahajournals.org/ Downloaded from
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Focus On IELTS - Answer KeysДокумент32 страницыFocus On IELTS - Answer KeysKhang Minh Truong53% (40)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Ed Coan - Core Manual For Strength Training (Version 2.0)Документ40 страницEd Coan - Core Manual For Strength Training (Version 2.0)blackhawk896% (28)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Exercice TRX PDFДокумент1 страницаExercice TRX PDFnoreadil0% (2)
- DRUG STUDY EpinephrineДокумент2 страницыDRUG STUDY EpinephrineCarlo Francisco D. Canto78% (9)
- Healthy LifestyleДокумент14 страницHealthy LifestyleSaadОценок пока нет
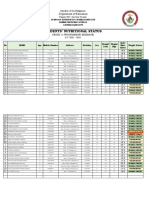
- Students Nutritional Status Template 1Документ4 страницыStudents Nutritional Status Template 1Jeffreynald Arante FranciscoОценок пока нет
- 43 110 1 SMДокумент8 страниц43 110 1 SMMarioSuilaОценок пока нет
- BIO 101 Worksheet 10Документ4 страницыBIO 101 Worksheet 10Xia AlliaОценок пока нет
- Diagram AlirДокумент6 страницDiagram AlirZulman EfendiОценок пока нет
- Demands in Ice HockeyДокумент16 страницDemands in Ice Hockeysara_damato10Оценок пока нет
- Men's Health 01.02 2019Документ118 страницMen's Health 01.02 2019Mike MarineОценок пока нет
- Case Study Project - DiverticulosisДокумент12 страницCase Study Project - Diverticulosisapi-347981380100% (1)
- VitaClay Mini Slow Cooker and Yogurt Maker RecipesДокумент28 страницVitaClay Mini Slow Cooker and Yogurt Maker RecipesvalentindanielОценок пока нет
- Here Are The Interesting Facts That You Shouls Know About Your Hair1. Your HairДокумент4 страницыHere Are The Interesting Facts That You Shouls Know About Your Hair1. Your Hairyogesh280785Оценок пока нет
- Obesity Powerpoint G-5Документ14 страницObesity Powerpoint G-5cheryl tubliganОценок пока нет
- Alia OPD PresentationДокумент42 страницыAlia OPD PresentationALia NadhirahОценок пока нет
- Skin Fold TestДокумент5 страницSkin Fold TestMiljana VujanovicОценок пока нет
- Results 1 DayДокумент6 страницResults 1 Dayxosmar185Оценок пока нет
- Preeclampsia Prevalence, Risk Factors, and Pregnancy OutcomesДокумент14 страницPreeclampsia Prevalence, Risk Factors, and Pregnancy OutcomesHaris FadillaОценок пока нет
- hlth634 Brief Marketing Plan Outline Jewel BrooksДокумент6 страницhlth634 Brief Marketing Plan Outline Jewel Brooksapi-299055548Оценок пока нет
- The Five Tibetan RitesДокумент14 страницThe Five Tibetan Ritesreha-kaubaОценок пока нет
- Adjectives Superlatives and Superlatives 1Документ4 страницыAdjectives Superlatives and Superlatives 1transa012Оценок пока нет
- Farmakokinetika Klinik Vancomycin: Riri Tifani 1201108Документ21 страницаFarmakokinetika Klinik Vancomycin: Riri Tifani 1201108Rahmatul HusnaОценок пока нет
- Body Parts Governed by PlanetsДокумент2 страницыBody Parts Governed by PlanetsBratva Ankit Mishra100% (1)
- Practice Essentials: Ralph Downey, Iii, PHD Staff Sleep Specialist, Cleveland Clinic Foundation AssociateДокумент18 страницPractice Essentials: Ralph Downey, Iii, PHD Staff Sleep Specialist, Cleveland Clinic Foundation AssociateMaulana 'Sugat' Iskandar DinataОценок пока нет
- Therapeutic DietДокумент3 страницыTherapeutic DietPaul BenterОценок пока нет
- Impact of Methyl Jasmonate On Squalene Bio Synthesis in MicroalgaДокумент5 страницImpact of Methyl Jasmonate On Squalene Bio Synthesis in MicroalgaGerman ColqueОценок пока нет
- 1 Shiong LW SARCOPENIA UPDATEДокумент8 страниц1 Shiong LW SARCOPENIA UPDATEdavidtuanandartuaОценок пока нет
- Shahad 4Документ15 страницShahad 4Mohammed OmarОценок пока нет
- Ehy 339Документ98 страницEhy 339Xarisis IoannisОценок пока нет