Академический Документы
Профессиональный Документы
Культура Документы
Recuperación Postartroplastia de Cadera
Загружено:
Alvaro Besoain SaldañaИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Recuperación Postartroplastia de Cadera
Загружено:
Alvaro Besoain SaldañaАвторское право:
Доступные форматы
Time course and extent of functional recovery during the rst postoperative
year after minimally invasive total hip arthroplasty with two different surgical
approachesa randomized controlled trial
Kharma C. Foucher, Markus A. Wimmer
n
, Kirsten C. Moisio, Madelaine Hildebrand, Martin C. Berli,
Matthew R. Walker, Richard A. Berger, Jorge O. Galante
Department of Orthopedic Surgery, Rush University Medical Center, 1653 W. Congress Parkway, Chicago, IL 60612, USA
a r t i c l e i n f o
Article history:
Accepted 19 October 2010
Keywords:
Total hip arthroplasty
Functional recovery
Biomechanics
Gait
Surgical approach
a b s t r a c t
While others have reported short-term comparisons between various minimally invasive surgical (MIS)
approaches to total hip arthroplasty (THA) and their conventional analogues, longer-termdata is lacking,
as is information indicating whether MIS approaches to THA provide a biomechanically complete
recovery. Furthermore, different MIS approaches have not been compared. Our approaches of interest
were a one-incision modied Watson-Jones, and a two-incision approach. Hypotheses: (1) There are
signicant differences in gait recovery patterns between the two surgical groups and (2) THA subjects
have signicant differences in function one year after surgery compared to control subjects. To test these
hypotheses, THA candidates (n26) were randomized to receive one of these MIS approaches and
evaluatedpreoperatively, and postoperatively at 3 weeks, and at 3, 6 and 12months. Evaluations included
three-dimensional gait analysis and 24-hour step-counts. The same data were obtained from 25 control
subjects. Recovery time-course was assessed using repeated measures ANOVA. T-tests were used to
compare controls with the pooled group of THA subjects. We found no differences between the two THA
surgical groups regarding the time-course of recovery (pZ0.591). Although recovery was statistically
complete by 3 months postoperatively for all variables, there were signicant differences fromcontrols at
12 months. Most notably, the external hip adduction moment, which reects hip abductor function, was
more than one standard deviation belownormal (po0.001). THA subject inactivity could not explain the
gait differences, since one year after surgery daily step counts were not signicantly different from
controls (p0.346). More work is necessary to determine ways to improve biomechanical outcomes for
todays patients with high expectations for function and implant longevity.
& 2010 Elsevier Ltd. All rights reserved.
1. Introduction
Total hip arthroplasty (THA), using conventional surgical
approaches, is a very successful procedure. However, despite
excellent clinical results, full functional recovery does not occur,
as most patients exhibit persistent abnormal patterns of hip
loading (Foucher et al., 2007, 2008). Minimally invasive surgical
(MIS) approaches to THA have been introduced in response to
increased patient demands and expectations. The assumption has
beenthat, because MIS approaches should cause less damage to the
soft tissue structures surrounding the hip, MIS approaches lead to
both faster and more complete recovery. Indeed, in the early
postoperative period MIS approaches have shown superior results
than conventional THA for some clinically important outcomes
suchas paincontrol andlengthof hospitalization(Dorr et al., 2007).
However, after the early days and weeks, both approaches show
comparable functional recovery as measured by range of motion,
walking speed or other timedistance parameters (Bennett et al.,
2006, 2007; Dorr et al., 2007; Ward et al., 2008).
Abnormal patterns of hip loading have been noted after conven-
tional THA, even when subjects have good clinical results (Foucher
et al., 2007, 2008; Long et al., 1993; Madsen et al., 2004; Perronet al.,
2000). However, gait of MIS THA patients has not been compared
to that of subjects without hip pathology, and the extent of bio-
mechanical recovery has not been assessed. Furthermore, even
among MIS techniques, functional outcomes between specic
surgical approaches vary. For example, a randomized study found
evidence, using comprehensive gait analysis, of greater abductor
dysfunction during gait after an anterolateral MIS approach than a
two-incision or a posterior approach, and suggested that different
approaches have different recovery rates (Meneghini et al., 2008).
WestudiedtwoMISapproaches usedat our institution: amodied
Watson-Jones exposure (Bertin and Rottinger, 2004), an anterior
approach that spares the abductor musculature, and a two-incision
Contents lists available at ScienceDirect
journal homepage: www.elsevier.com/locate/jbiomech
www.JBiomech.com
Journal of Biomechanics
0021-9290/$ - see front matter & 2010 Elsevier Ltd. All rights reserved.
doi:10.1016/j.jbiomech.2010.10.026
n
Corresponding author. Tel.: +1 312 942 2789; fax: +1 312 942 2101.
E-mail address: Markus_A_Wimmer@rush.edu (M.A. Wimmer).
Journal of Biomechanics 44 (2011) 372378
technique (Berger and Duwelius, 2004; Berger et al., 2004) that
includes a small anterior approach, that still spares the abductors, and
a small posterior incisioninthe buttocks. Witheither technique, early
recovery, including unrestricted range and level of activities, is
theoretically possible. It was unknown whether either approach
would have a biomechanical advantage. It was not clear a priori that
previous work comparing gait recovery in subjects receiving con-
ventional anterior and posterior approaches (Gore et al., 1982;
Madsen et al., 2004; Masonis and Bourne, 2002) could be generalized
to subjects with small, largely muscle sparing incisions.
Our study had two goals. First we sought to determine the time
course of recovery of hip biomechanical gait parameters during the
rst year after MIS THA. Second, we sought to determine whether
these patients ultimately regain normal hip function, as assessed
by moments andmotionduring gait. We also assessedactivity level
(steps/day), because others have measured it in conventional THA
patients (Kinkel et al., 2009; McClung et al., 2000; Morlock et al.,
2001; Schmalzried et al., 1998), because it is an important factor in
biomechanically mediated complications such as wear of implant
materials (Schmalzried et al., 2000; Schmalzried and Huk, 2004),
and because activity measures have been correlated with general
health-outcomes and hip-specic clinical measures (Bauman et al.,
2007; Beaule et al., 2006). The hypotheses testedwere: (1) there are
signicant differences in gait recovery patterns between the
two surgical groups and (2) one-year postoperatively there are
signicant functional differences (hip biomechanics during gait
and overall activity level) between THA subjects and controls.
2. Methods
2.1. Subjects
The study took place at Rush University Medical Center in Chicago, Illinois,
a tertiary care center in a major urban center. Our well-known orthopedic surgery
department attracts patients from a large geographical area. Biomechanical
evaluations were conducted at the Motion Analysis Laboratory in the Medical
Center. Thirty-two subjects scheduled for total hip replacements with a single
surgeon were randomized to our two MIS approaches. Inclusion criteria were a
diagnosis of primary unilateral hip osteoarthritis requiring THAand age between 40
and 80 years. Exclusion criteria were: no previous hip or knee surgery, a rheumatoid
arthritis diagnosis, polyarthritis, Crowe grade 3 or 4 hip dysplasia, signicant
lumbar spine disease, osteoporosis, or a historyof a neurological disorder that would
affect gait. In addition, we excluded patients within one year of myocardial
infarction, pulmonary embolism, or anticoagulation therapy. We also excluded
patients with considerable obesity (body mass index more than 35) or with three or
more important medical comorbidities that were not controlled. Institutional
Review Board (IRB) approval was obtained and all subjects gave informed consent.
Subjects were enrolled in pairs before randomization to ensure an equal
distribution of subjects in each of the two groups. Before subject enrollment, pairs
of opaque envelopes containing cards with the name of each of the two surgical
approaches were prepared by a nurse on the clinical team. On the morning of the
procedure, the surgeon drewa card for each subject without prior knowledge of the
cards contents. Therefore no one, including the subject, the surgeon, the nurse, and
the other research study staff had prior knowledge of group assignment before the
procedure. Also while preoperative data was collected before group assignment was
known, postoperative outcome data could not be blindly collected because it was
visually evident whether a subject had received a single or double incision
procedure. The nal study cohort included 26 subjects (13/group) who completed
study activities and clinical follow-up (Fig. 1). There were no signicant between-
group differences in age, height, weight (pZ0.069, Students t-tests), or male/
female or left/right ratios (pZ0.268, w
2
tests; Table 1).
All patients received the same type of cementless implant (acetabular
componentTrilogy; femoral componentVerSys 6 Beaded Full-Coat, Zimmer,
Warsaw, IN). Implantation of prosthetic devices was done as per manufacturer
recommendations (Zimmer, 2003). At the time of study initiation the surgeon had
performed each procedure over 300 times. Prior to surgery, patients started a pain
management andrehabilitationprotocol (Berger et al., 2004, 2005). Postoperatively,
patients were allowed to bear weight and perform activities of daily living within
hours of completion of the surgery, and were discharged within 24 h. They were
encouraged to ambulate with one crutch or preferably a cane as soon as tolerated;
precautions were maintained for 3 weeks.
To establish a control group of healthy subjects, we identied 55 asymptomatic
subjects with no history of joint pain, injury or diagnoses. They underwent gait
analysis, received hip and knee radiographs for a separate IRB-approved study, and
gave informed consent for their data to be used. These subjects had no radiographic
evidence of osteoarthritis anda Harris HipScore of 100/100(Harris, 1969) indicating
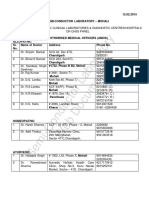
Fig. 1. Subject randomization and follow-up ow diagram following CONSORT guidelines (Moher et al., 2010; Schulz et al., 2010).
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 373
no pain or functional decits. Of the 55, a control group was selected to match the
THAgroupbasedonweight, height, gender, andage, inthat order, tominimize body-
size differences that might inuence joint loading (Moisio et al., 2003). Agroup of 25
subjects was successfully matched on these criteria: no signicant body size
differences were seen between the THA group and the control group (BMI was
2773 for the THA group and 2876 for controls (p0.449). The age range for the
THA group was 4279; for controls it was 4667.
2.2. Radiographic measurements
We obtained antero-posterior pelvic and femoral radiographs taken for clinical
purposes at each subjects one-year follow-up exam. The following measurements
were taken: horizontal and vertical positions of the joint center, length of the
abductor muscle moment arm, offset, leg length, and cup inclination angle. All
measurements were conducted by a single, trained, orthopedic surgeon who was
not involved in the procedures. The size of the implant head was measured fromthe
radiographs and the actual head-size was obtained from the operative record. The
ratio of the measured diameter to the actual head diameter was used to determine
the magnication to correct the other radiographic measurements.
2.3. Gait analysis
Kinematics and kinetics were measured using published gait analysis methods
(Andriacchi et al., 2005, 1980; Prodromos et al., 1985). Six passive retroreective
markers were placed onbony landmarks of the lower extremity at the most superior
point of the iliac crest, the greater trochanter, lateral knee joint line, lateral
malleolus, lateral most point on the calcaneus, and the head of the fth metatarsal.
A four-camera optoelectronic camera system (Qualisys, Gothenburg, Sweden)
recorded the 3D position of each marker. Ground reaction force and location
were measured with a multicomponent force plate (Bertec, Columbus, Ohio).
Timedistance parameters and sagittal plane motion at the hip, knee and ankle
were calculated. Inverse dynamics were used to calculate 3D external moments.
External moments were calculated at each time point (120 frames/s), using the
magnitude andlocationof the groundreactionforce andthe 3dimensional locations
of the joint centers, which are derived from the 3D spatial position of the markers
and anthropometric measurements and data. External moments were then normal-
ized to percent body weight times height (%BW*Ht) (Moisio et al., 2003).
Data for at least 6 trials per limb, 4 at a self-selected normal speed and 2 at either
self-selected fast (for controls and preop THA subjects) or slow (for controls and
postop THA subjects) speeds, were collected. Only the operated side was analyzed
for the THA subjects in this study. For control subjects, a study limb was selected
randomly. Trials were selected for the THA group such that speed differences
between visits were minimal. For control subjects, we selected a trial with a speed
closest to the average of the THA group trials. Variables of interest were peak
external hip moments and dynamic range of motion during walking.
2.4. Activity monitor
A commercially available activity monitor with accompanying processing
software was used (AMP 331Dynastream, Cochrane, Alberta, Canada). The
monitor, which is worn on the ankle (71.324.037.5 mm
3
; 50 g), uses accel-
erometer-based technology to detect its spatial position. To ensure correct place-
ment, monitors were tted immediately after each gait test. Activity was recorded
for Z24 h. Data for the rst complete 24-h period were analyzed. We used activity
data (#steps/24 h) from control subjects and from THA subjects one-year
evaluation.
2.5. Statistical analysis
Power analysis was based on a previous pilot study of 30 subjects using three
MIS approaches (Hildebrand et al., 2006). In the pilot, the external adduction
moment had an SD of 0.4% BW*Ht. Therefore, we determined that as few as 10
subjects per group could detect a difference of 0.53% BW*Ht in external adduction
moment. Thus, the current study was adequately powered. Next, we conrmed that
subjects in the two surgical approach groups were clinically equivalent preopera-
tively. Because joint geometry canaffect gait biomechanics (Foucher et al., 2009), we
also wanted to show that differences in reconstructed joint geometry were not
present because of the different approaches. Based on t-tests or MannWhitney
tests (radiographic data were not normally distributed), no signicant between-
groups differences were found for HHS or for any radiographic measure (p0.186 to
p0.960). This was expected because our subjects were randomized.
Dynamic range of motion and peak external moments were the primary
outcome measures. Activity level (steps/day) was a secondary outcome measure.
Repeated measures ANOVA was used to identify signicant differences in the time
course of recovery betweensurgical approaches (hypothesis 1). Signicant time-by-
incision interactions would indicate that surgical approaches differed. Helmert
contrasts, comparing data at each time point to each later time point, were used to
determine when maximum recovery was attained for each variable. To test
hypothesis 2, t-tests were used: (i) to detect signicant differences between control
subjects and fully recovered THA subjects (12-months postoperative) in gait
parameters and activity level, and (ii) to conrm that gait differences between
THA candidates and controls existed preoperatively. Pr0.05 was considered
signicant for statistical tests.
3. Results
3.1. Recovery time-course
Although isolated differences seemed visually apparent
between the two surgical groups (Fig. 2), no signicant time-by-
incision interactions were seen for any gait parameter (pZ0.591).
Thus, there were no differences in recovery patterns. Therefore, our
rst hypothesis was not supported and the two surgical approach
groups were pooled for subsequent analyses. Repeated measures
analysis then indicated that signicant improvement was seen for
some, but not all, gait parameters. Signicant time effects in the
ANOVA indicated that the dynamic hip range of motion and exten-
sion moment signicantly improved during year 1 (po0.001);
postoperatively, these variables increased by 38% and 63%, respec-
tively. Peak internal rotation moment increased by 23% but this
change was not statistically signicant (p0.089). No postopera-
tive change was seen in peak exion, peak adduction, peak
abduction, or peak external rotation moments (pZ0.245).
3.2. Extent of recoverycomparisons with control
As expected, many differences from the control group were
present in the THA group before surgery (Fig. 3). Compared to
controls, dynamic hip range of motion, adduction, and internal and
external rotation moments were lower (pr0.045), while abduc-
tion moment was signicantly increased (p0.045). Sagittal plane
moments were not different before surgery. At one year, signicant
differences remained between THA and controls for adduction and
internal rotation moments (pr0.001). In the THA group, these
moments were more than 1 SD below values for control subjects.
The abduction moment remained slightly elevated, but this
difference was no longer statistically signicant (p0.072) 12
months postoperatively.
Despite decits ingait biomechanics, activity levels were within
the normal range one year postoperatively. Control subjects
walked 1000 more steps/day (869573490) than THA subjects
Table 1
Characteristics of each subject group.
Modied Watson-Jones
Group
Two-incision group Surgical approach
group p-value
Control group THA vs. control
p-value
Age (years) 5778 6379 0.069 5476 0.288
Height (m) 1.8170.08 1.7070.10 0.513 1.7170.69 0.250
Body mass (kg) 79.5711.8 88.3718.2 0.164 81.6713.3 0.274
Male/Female 8/5 7/6 0.691 12/13 0.683
Left/Right 4/9 8/5 0.116 13/12 0.896
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 374
(768773024; p0.346). Activity levels were categorized into ve
levels fromSedentary to Highly Active based on classications
proposed by Tudor-Locke and Bassett (2004). Most subjects in both
groups were classiedas somewhat active (30%inthe THAgroup,
34% in the control group), having walked 750010,000 steps/day.
Four percent of control subjects and 5%of THAsubjects were highly
Fig. 2. Biomechanical recovery over the rst postoperative year after MIS THA using either a modied Watson-Jones approach (light bars) or a two-incision approach (dark
bars). No signicant differences in the time course of recovery were observed. For reference, the mean of the control group is shown as a horizontal line in each panel.
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 375
active (412,500 steps/day). A chi-square test conrmed that
control and THA groups had similar distributions of activity levels
(p0.654).
4. Discussion
Although MIS approaches to THA have clinical advantages over
conventional procedures, their relative functional merits are con-
troversial. Our study was designed to begin to resolve that
controversy. We found no signicant differences in gait recovery
patterns between the two surgical groups when the full year of
recovery was considered. Our results complement recent ndings
reportedinthe literature (Krychet al., 2009; Meneghini et al., 2008;
Pagnano et al., 2008).
The more signicant nding is that, despite the use of less
invasive approaches, the hip abductors do not recover (as sug-
gested by the external adduction and internal rotation moments).
The adductionmoment is largely balancedby activityof the gluteus
medius and minimus. The posterior bers of the gluteus medius
also likely participate in balancing the internal rotation moment
seen in the second half of stance based on their signicant external
rotationfunctionwhenthe hipis extended(Gottschalket al., 1989).
Our group has previously reported nearly identical gait decits
after conventional THA (Foucher et al., 2007).
Others have alsoobservedother features of postoperative function
that are likely remnants of preoperative gait patterns. These include
slower preferred walking speeds and retained preoperative patterns
of muscle activity measured through electromyography (Long et al.,
1993; Perrin et al., 1985). Reduced muscle strength has also been
documented (Murray et al., 1975; Shih et al., 1994). Therefore, it
seems likely that the functional decits seen in our current patient
group are likewise a remnant of the gait pattern that developed as a
result of hiposteoarthritis, rather thanbeingtraumaticinorigin. Inthe
absence of more effective rehabilitation protocols, patients may not
be able to reverse the losses suffered due to the long period (often
years) of preoperative pain and disuse preceeding their arthroplasty
procedures. It is possible that patients undergoing THA through both
MIS and conventional approaches may benet from more aggressive
long-term rehabilitation as well as from the intensive early rehabi-
litation protocols that patients currently receive. A call for more
intensive postoperative rehabilitation for THA patients has been
building (Bhave et al., 2007; Long et al., 1993; Shih et al., 1994;
Trudelle-Jackson et al., 2002; Trudelle-Jackson and Smith, 2004); in
fact a recent meta-analysis reported that there was insufcient
evidence to make denitive conclusions about the efcacy of post-
operative physical therapy after THA (Minns Lowe et al., 2009).
Activity level analyses indicated that the functional decits
measured by gait analysis are not caused by relative inactivity of
patients after THA. Step count was not decreased compared to
normal, despite the abnormal gait and the fact that the THA
subjects were slightly older than the control subjects as a group.
Indeed, a previous study found that activity did not decline as
quickly with increased age in subjects with THAs as it did in control
subjects (Goldsmithet al., 2001). One year after surgery, this cohort
of MIS THA subjects was substantially more active than similarly
aged groups previously reported (McClung et al., 2000; Morlock
et al., 2001; Schmalzried et al., 1998). Since implant wear and other
biomechanical consequences of THA are related to the number of
loading cycles (Schmalzried et al., 2000; Schmalzried and Huk,
2004), it will be necessary in future work to fully characterize the
activity levels of this patient population, which may be distinct
from previously evaluated groups.
The study was limited by the inclusion of only two of the
currently performed MIS THA procedures. The two-incision
approach we studied has also been surrounded by some contro-
versy. While rapid rehabilitation and recovery has been reported
(Berger and Duwelius, 2004; Berger et al., 2004), a slower early
recovery was shown in a randomized clinical trial when compared
to a minimally invasive posterolateral approach (Pagnano et al.,
2008, 2009). Furthermore, longer operation times and increased
technical difculties have been reported (Pagnano et al., 2006,
2009). In the US, a posterolateral MIS approach is more commonly
performed than the techniques in this study. Nevertheless, our
nding of no statistically signicant differences in recovery pat-
terns, particularly when the rst year of recovery is examined as a
whole, is consistent with literature reports and can likely be
extrapolated to other MIS approaches.
Another limitation of our study is that activity data for THA
subjects were only collected for a 24-h period beginning immedi-
ately after the gait test. This means that we cannot assert that this
represented a typical day for these subjects. Afull week of data was
available for control subjects, but, for consistency, all activity data
were handled in the same way in this study. The effect of this
potential systematic error would be an underestimation of the true
activity level for all subjects. Therefore, we caution the reader
against interpreting our specic step numbers as anything more
than a snapshot; but our data supports the conclusion that, as a
whole, contemporary subjects with total hip replacements are not
less active than subjects with no joint pathology. In addition, we
cannot exclude the possibility of selection biassubjects who
chose to participate in the study may constitute a sample of highly
functional THA candidates. This would not have affected the
conclusions regarding any differences between the two surgical
Fig. 3. Dynamic range of motion and peak external moments for the pooled THA group before surgery (light gray bars), one year after surgery (dark gray bars) and control
subjects (black bars). Lines above the bars indicate signicant differences from normal.
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 376
groups. Our ndings with regard to persistent biomechanical
decits when compared to control subjects, however, are all the
more striking in light of any potential bias.
Although this issue of having highly active patients who have
abnormal muscle function has not been recognized as a large
clinical problem, negative consequences may become evident in
the future. For example, past studies have shown that patients with
THRs are at increased risk of undergoing contralateral total joint
arthroplasties (Goker et al., 2000; Shakoor et al., 2002; Umeda et al.,
2009). In particular, the contralateral knee adduction moment, a
known biomechanical marker of knee osteoarthritis, is increased in
such subjects (Shakoor et al., 2003). Risk of contralateral joint
degeneration may be further increased in these highly active
patients. The presence of an abnormal hip loading pattern may
also directly affect the long-termclinical outcome and durability of
the articial hip due to high cycle numbers. The relationships
among abnormal hip biomechanics, high activity levels, and
contralateral joint loading should be investigated further. The
predicted explosive increase in the number of THA procedures
performed annually over the coming decades (Kurtz et al., 2007)
makes addressing this issue even more urgent.
Inconclusion, our results conrmandextendrecent reports that
found no compelling evidence that different MIS approaches result
indifferent patterns of functional recovery. Furthermore, evenwith
minimally invasive approaches that seek minimal soft tissue
damage during surgery, functional recovery is not
completenormal gait is not fully restored by THA. Since there
is evidence that a decit in postoperative gait is likely a remnant of
a decit in preoperative gait, and that advances in surgical
technique appear to have already achieved maximum benet,
the best way to improve functional outcomes after THA may be
perioperative rehabilitation protocols. This may be of particular
value to a contemporary patient population with higher expecta-
tions regarding quantity as well as types of physical activity.
Conict of interest statement
None of the authors report any relationships that could have
inuenced the content of the work presented here.
Acknowledgment
Rush Arthritis and Orthopedic Institute provided partial
research funding. Research fellows funded by Margarete und
Walter Lichtenstein-Stiftung, Theodor Engelmann Stiftung, Swiss
Orthopaedic Society, Zimmer Germany and University of Martin-
Luther Halle. The study sponsors had no role in the study design, in
the collection, analysis and interpretation of data, in the writing of
the manuscript, or in the decision to submit the manuscript for
publication.
References
Andriacchi, T.P., Natarajan, R.N., Hurwitz, D.E., 2005. Musculo-skeletal dynamic
locomotion and clinical applications.. Lippincott, Philadelphia, pp. 91-121.
Andriacchi, T.P., Andersson, G.B., Fermier, R.W., Stern, D., Galante, J.O., 1980. A study
of lower-limb mechanics during stair-climbing. The Journal of Bone and Joint
Surgery American Volume 5, 749757.
Bauman, S., Williams, D., Petruccelli, D., Elliott, W., de Beer, J., 2007. Physical activity
after total joint replacement: a cross-sectional survey. Clinical Journal of Sport
Medicine: Ofcial Journal of the Canadian Academy of Sport Medicine 2,
104108.
Beaule, P.E., Dorey, F.J., Hoke, R., Leduff, M., Amstutz, H.C., 2006. The value of patient
activity level in the outcome of total hip arthroplasty. The Journal of Arthro-
plasty 4, 547.
Bennett, D., Ogonda, L., Elliott, D., Humphreys, L., Beverland, D.E., 2006. Comparison
of gait kinematics in patients receiving minimally invasive and traditional
hip replacement surgery: a prospective blinded study. Gait & Posture 3,
374382.
Bennett, D., Ogonda, L., Elliott, D., Humphreys, L., Lawlor, M., Beverland, D., 2007.
Comparison of immediate postoperative walking ability in patients receiving
minimally invasive and standard-incision hip arthroplasty: a prospective
blinded study. The Journal of Arthroplasty 4, 490495.
Berger, R.A., Duwelius, P.J., 2004. The two-incision minimally invasive total hip
arthroplasty: technique and results. The Orthopedic Clinics of North America 2,
163172.
Berger, R.A., Jacobs, J.J., Meneghini, R.M., Della Valle, C., Paprosky, W., Rosenberg, A.G.,
2004. Rapid rehabilitation and recovery with minimally invasive total hip
arthroplasty. Clinical Orthopaedics and Related Research 429, 239247.
Berger, R.A., Sanders, S., Gerlinger, T., Della Valle, C., Jacobs, J.J., Rosenberg, A.G., 2005.
Outpatient total knee arthroplasty with a minimally invasive technique. The Journal
of Arthroplasty 7 (Suppl 3), 3338.Bertin, K.C., Rottinger, H., 2004. Anterolateral
mini-incision hip replacement surgery: a modied Watson-Jones approach. Clinical
Orthopaedics and Related Research 429, 248255.
Bhave, A., Marker, D.R., Seyler, T.M., Ulrich, S.D., Plate, J.F., Mont, M.A., 2007.
Functional problems and treatment solutions after total hip arthroplasty. The
Journal of Arthroplasty 6 (Suppl 2), 116124.
Dorr, L.D., Maheshwari, A.V., Long, W.T., Wan, Z., Sirianni, L.E., 2007. Early pain relief
and function after posterior minimally invasive and conventional total hip
arthroplasty. A prospective, randomized, blinded study. The Journal of Bone and
Joint Surgery American Volume 6, 11531160.
Foucher, K.C., Hurwitz, D.E., Wimmer, M.A., 2009. Relative importance of gait vs.
joint positioning on hip contact forces after total hip replacement. Journal of
Orthopaedic Research: Ofcial Publication of the Orthopaedic Research Society.
Foucher, K.C., Hurwitz, D.E., Wimmer, M.A., 2008. Do gait adaptations during stair
climbing result in changes in implant forces in subjects with total hip
replacements compared to normal subjects? Clinical Biomechanics (Bristol
Avon).
Foucher, K.C., Hurwitz, D.E., Wimmer, M.A., 2007. Preoperative gait adaptations
persist one year after surgery in clinically well-functioning total hip replace-
ment patients. Journal of Biomechanics 15, 34323437.
Goker, B., Doughan, A.M., Schnitzer, T.J., Block, J.A., 2000. Quantication of
progressive joint space narrowing in osteoarthritis of the hip: longitudinal
analysis of the contralateral hip after total hip arthroplasty. Arthritis and
Rheumatism 5, 988994.
Goldsmith, A.A., Dowson, D., Wroblewski, B.M., Siney, P.D., Fleming, P.A., Lane, J.M.,
Stone, M.H., Walker, R., 2001. Comparative study of the activity of total hip
arthroplasty patients and normal subjects. The Journal of Arthroplasty 5,
613619.
Gore, D.R., Murray, M.P., Sepic, S.B., Gardner, G.M., 1982. Anterolateral compared to
posterior approach in total hip arthroplasty: differences in component posi-
tioning, hip strength, and hip motion. Clinical Orthopaedics and Related
Research 165, 180187.
Gottschalk, F., Kourosh, S., Leveau, B., 1989. The functional anatomy of tensor fasciae
latae and gluteus medius and minimus. Journal of Anatomy, 179189.
Harris, W.H., 1969. Traumatic arthritis of the hip after dislocation and acetabular
fractures: treatment by mold arthroplasty. An end-result study using a new
method of result evaluation. The Journal of Bone and Joint Surgery American
Volume 4, 737755.
Hildebrand, M., Wimmer, M.A., Moisio, K.C., Della Valle, C.R., Berger, R., Galante, J.O.,
2006. The inuence of MIS surgical approach on postoperative gait in patients
with THA. In: Transactions of the 52nd Annual Meeting, Orthopaedic Research
Society, Chicago, IL.
Kinkel, S., Wollmerstedt, N., Kleinhans, J.A., Hendrich, C., Heisel, C., 2009. Patient
activity after total hip arthroplasty declines with advancing age. Clinical
Orthopaedics and Related Research 8, 20532058.
Krych, A.J., Pagnano, M.W., Wood, K.C., Meneghini, R.M., Kaufmann, K., 2009. No
benet of the two-incision THA over mini-posterior THA: a pilot study of
strength and gait. Clinical Orthopaedics and Related Research.
Kurtz, S., Ong, K., Lau, E., Mowat, F., Halpern, M., 2007. Projections of primary and
revision hip and knee arthroplasty in the United States from 2005 to 2030. The
Journal of Bone and Joint Surgery American Volume 4, 780785.
Long, W.T., Dorr, L.D., Healy, B., Perry, J., 1993. Functional recovery of non-
cemented total hip arthroplasty. Clinical Orthopaedics and Related Research
288, 7377.
Madsen, M.S., Ritter, M.A., Morris, H.H., Meding, J.B., Berend, M.E., Faris, P.M.,
Vardaxis, V.G., 2004. The effect of total hip arthroplasty surgical approach on
gait. Journal of Orthopaedic Research: Ofcial Publication of the Orthopaedic
Research Society 1, 4450.
Masonis, J.L., Bourne, R.B., 2002. Surgical approach, abductor function, and total hip
arthroplasty dislocation. Clinical Orthopaedics and Related Research 405,
4653.
McClung, C.D., Zahiri, C.A., Higa, J.K., Amstutz, H.C., Schmalzried, T.P., 2000.
Relationship between body mass index and activity in hip or knee arthroplasty
patients. Journal of Orthopaedic Research: Ofcial Publication of the Ortho-
paedic Research Society 1, 3539.
Meneghini, R.M., Smits, S.A., Swinford, R.R., Bahamonde, R.E., 2008. A randomized,
prospective study of 3 minimally invasive surgical approaches in total hip
arthroplasty: comprehensive gait analysis. The Journal of Arthroplasty 6 (Suppl
1), 6873.
Minns Lowe, C.J., Barker, K.L., Dewey, M.E., Sackley, C.M., 2009. Effectiveness of
physiotherapy exercise following hip arthroplasty for osteoarthritis: a systema-
tic review of clinical trials. BMC Musculoskeletal Disorders, 98.
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 377
Moher, D., Hopewell, S., Schulz, K.F., Montori, V., Gotzsche, P.C., Devereaux, P.J.,
Elbourne, D., Egger, M., Altman, D.G., Consolidated Standards of Reporting Trials
Group, 2010. CONSORT 2010 explanation and elaboration: updated guidelines
for reporting parallel group randomised trials. Journal of Clinical Epidemiology
8, e137.
Moisio, K.C., Sumner, D.R., Shott, S., Hurwitz, D.E., 2003. Normalization of joint
moments during gait: a comparison of two techniques. Journal of Biomechanics
4, 599603.
Morlock, M., Schneider, E., Bluhm, A., Vollmer, M., Bergmann, G., Muller, V., Honl, M.,
2001. Duration and frequency of everyday activities intotal hip patients. Journal
of Biomechanics 7, 873881.
Murray, M.P., Brewer, B.J., Gore, D.R., Zuege, R.C., 1975. Kinesiology after McKee-
Farrar total hip replacement. A two-year follow-up of one hundred cases. . The
Journal of Bone and Joint Surgery American Volume 3, 337342.
Pagnano, M.W., Trousdale, R.T., Meneghini, R.M., Hanssen, A.D., 2009. Slower
recovery after two-incision than mini-posterior-incision total hip arthroplasty.
Surgical technique. The Journal of Bone and Joint Surgery American Volume,
5073.
Pagnano, M.W., Trousdale, R.T., Meneghini, R.M., Hanssen, A.D., 2008. Slower
recovery after two-incision than mini-posterior-incision total hip arthroplasty.
A randomized clinical trial. The Journal of Bone and Joint Surgery American
Volume 5, 10001006.
Pagnano, M.W., Trousdale, R.T., Meneghini, R.M., Hanssen, A.D., 2006. Patients
preferred a mini-posterior THA to a contralateral two-incision THA. Clinical
Orthopaedics and Related Research, 156159.
Perrin, T., Dorr, L.D., Perry, J., Gronley, J., Hull, D.B., 1985. Functional evaluation of
total hip arthroplasty with ve- to ten-year follow-up evaluation. Clinical
Orthopaedics and Related Research 195, 252260.
Perron, M., Malouin, F., Moffet, H., McFadyen, B.J., 2000. Three-dimensional gait
analysis in women with a total hip arthroplasty. Clinical Biomechanics (Bristol,
Avon) 7, 504515.
Prodromos, C.C., Andriacchi, T.P., Galante, J.O., 1985. Arelationship betweengait and
clinical changes following high tibial osteotomy. The Journal of Bone and Joint
Surgery American Volume 8, 11881194.
Schmalzried, T.P., Huk, O.L., 2004. Patient factors and wear in total hip arthroplasty.
Clinical Orthopaedics and Related Research 418, 9497.
Schmalzried, T.P., Shepherd, E.F., Dorey, F.J., Jackson, W.O., dela Rosa, M., Favae, F.,
McKellop, H.A., McClung, C.D., Martell, J., Moreland, J.R., Amstutz, H.C., 2000. The
John Charnley Award. Wear is a function of use, not time. Clinical Orthopaedics
and Related Research 381, 3646.
Schmalzried, T.P., Szuszczewicz, E.S., Northeld, M.R., Akizuki, K.H., Frankel, R.E.,
Belcher, G., Amstutz, H.C., 1998. Quantitative assessment of walking activity
after total hip or knee replacement. The Journal of Bone and Joint Surgery
American Volume 1, 5459.
Schulz, K.F., Altman, D.G., Moher, D., 2010. CONSORT Group, 2010. CONSORT 2010
statement: updated guidelines for reporting parallel group randomized trials.
Annals of Internal Medicine 11, 726732.
Shakoor, N., Block, J.A., Shott, S., Case, J.P., 2002. Nonrandom evolution of end-stage
osteoarthritis of the lower limbs. Arthritis and Rheumatism 12, 31853189.
Shakoor, N., Hurwitz, D.E., Block, J.A., Shott, S., Case, J.P., 2003. Asymmetric knee
loading in advanced unilateral hip osteoarthritis. Arthritis and Rheumatism 6,
15561561.
Shih, C.H., Du, Y.K., Lin, Y.H., Wu, C.C., 1994. Muscular recovery around the hip joint
after total hip arthroplasty. Clinical Orthopaedics and Related Research 302,
115120.
Trudelle-Jackson, E., Emerson, R., Smith, S., 2002. Outcomes of total hiparthroplasty:
a study of patients one year postsurgery. The Journal of Orthopaedic and Sports
Physical Therapy 6, 260267.
Trudelle-Jackson, E., Smith, S.S., 2004. Effects of a late-phase exercise program after
total hip arthroplasty: a randomized controlled trial. Archives of Physical
Medicine and Rehabilitation 7, 10561062.
Tudor-Locke, C., Bassett Jr, D.R., 2004. Howmany steps/day are enough? Preliminary
pedometer indices for public health. Sports Medicine (Auckland, N.Z.) 1, 18.
Umeda, N., Miki, H., Nishii, T., Yoshikawa, H., Sugano, N., 2009. Progression of
osteoarthritis of the knee after unilateral total hip arthroplasty: minimum
10-year follow-up study. Archives of Orthopaedic and Trauma Surgery 2,
149154.
Ward, S.R., Jones, R.E., Long, W.T., Thomas, D.J., Dorr, L.D., 2008. Functional recovery
of muscles after minimally invasive total hip arthroplasty. Instructional Course
Lectures, pp. 249254.
Zimmer, 2003. Versys beaded full-coat hip prosthesis. 0805-H10.
K.C. Foucher et al. / Journal of Biomechanics 44 (2011) 372378 378
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Contact and skills summary for a drug safety professionalДокумент5 страницContact and skills summary for a drug safety professionalAbhinav Gaddam100% (1)
- Transdermal Drug Delivery System: A Review: The Pharma InnovationДокумент10 страницTransdermal Drug Delivery System: A Review: The Pharma InnovationAlfiyana YuniarОценок пока нет
- Pharmaceutical Stability The Science and RegulationsДокумент32 страницыPharmaceutical Stability The Science and RegulationsMostofa Rubal100% (1)
- Bloom's Verbs For Digital LearningДокумент1 страницаBloom's Verbs For Digital LearningGUNARSO GUNARSOОценок пока нет
- 1B Approval Form PDFДокумент1 страница1B Approval Form PDFGummie Akalal SugalaОценок пока нет
- Action Research in HealthcareДокумент13 страницAction Research in HealthcareIan HughesОценок пока нет
- Sampling Techniques and Research DesignДокумент7 страницSampling Techniques and Research Designnatrix029Оценок пока нет
- Main EssayДокумент7 страницMain EssayKen UcheonyeОценок пока нет
- Ganga DiagnosticsДокумент3 страницыGanga Diagnosticsgaurav guptaОценок пока нет
- Cliantha CorpДокумент23 страницыCliantha CorpMaulik PatelОценок пока нет
- PTCДокумент24 страницыPTClola&losa farhanОценок пока нет
- Asking the Right Questions in Health ResearchДокумент13 страницAsking the Right Questions in Health ResearchHanan HagarОценок пока нет
- Chss Dir 130215Документ3 страницыChss Dir 130215PankajОценок пока нет
- Clinical Trial SummeryДокумент3 страницыClinical Trial Summerysnayhil100% (1)
- Protocol Deviation Tracking Log Ver2!07!17-2015Документ3 страницыProtocol Deviation Tracking Log Ver2!07!17-2015Kesava Sumanth AОценок пока нет
- Consensus of Prostho On Implants-2017Документ148 страницConsensus of Prostho On Implants-2017Faheemuddin MuhammadОценок пока нет
- Samah Aboulsoud-ResumeДокумент2 страницыSamah Aboulsoud-Resumeapi-400387662Оценок пока нет
- 9 - DR Arun Bhatt - Schedule YДокумент27 страниц9 - DR Arun Bhatt - Schedule Yvivek100% (1)
- Superior efficacy of pancreatin 25 000 MMS in PEI after pancreatic surgeryДокумент12 страницSuperior efficacy of pancreatin 25 000 MMS in PEI after pancreatic surgeryNikola StojsicОценок пока нет
- Utero-Placental Doppler Ultrasound For Improving Pregnancy Outcome (Review)Документ50 страницUtero-Placental Doppler Ultrasound For Improving Pregnancy Outcome (Review)Diapositivas08Оценок пока нет
- 165 Health Technology Assessment in IndiaДокумент12 страниц165 Health Technology Assessment in IndiaVinay GОценок пока нет
- Good Clinical Laboratory Practice GCLPДокумент36 страницGood Clinical Laboratory Practice GCLPPatrick Kosgei100% (1)
- Evidence Based Medicine & GuidelinesДокумент32 страницыEvidence Based Medicine & GuidelinesCarmel Joy DifuntorumОценок пока нет
- Assessing Diabetes AwarenessДокумент7 страницAssessing Diabetes AwarenessDrDeepak PawarОценок пока нет
- Guidelines for Microbiology Specimen ProcessingДокумент48 страницGuidelines for Microbiology Specimen ProcessingAl- ImanuddinОценок пока нет
- SUGAMMADEXДокумент6 страницSUGAMMADEXJulio Alfonso Castro PerezОценок пока нет
- Interpretation of The Correlation Coefficient - A Basic Review PDFДокумент5 страницInterpretation of The Correlation Coefficient - A Basic Review PDFLam KCОценок пока нет
- LIPUS TRUST StudyДокумент7 страницLIPUS TRUST StudymedtechyОценок пока нет
- Meditation Report 140106Документ439 страницMeditation Report 140106Laurynas Bambalas100% (1)