Академический Документы
Профессиональный Документы
Культура Документы
Intern ACOG Bulletin Episiotomy and Repair1
Загружено:
sharu4291Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Intern ACOG Bulletin Episiotomy and Repair1
Загружено:
sharu4291Авторское право:
Доступные форматы
Procedure and
Repair Techniques
The American Co llege o f
Obstetricians and Gyneco lo gists
WO MEN S HEALTH CARE PHYSICIANS
EPISIOTOMY
v
Preface
Episiotomy is the most common operative procedure that most obste-
tricians will perform in their lifetime. Because it is so common and
considered minor surgery, teaching students or interns the principles
and techniques usually is left to the most junior of residents. As a
result, the Residency Review Committee for Obstetrics and Gynecology
( RRC) asked the American College of Obstetricians and Gynecologists
( ACOG) to prepare a teaching aid for all residents, but especially those
with the least experience. The result is this monograph.
As with most surgical procedures, there are many approaches and
modifications to episiotomy. However, the principle is the same. It
does not matter if your preference is 4-0 chromic catgut suture or 3-0
polyglycolic suture. What matters is how, where, and when you suture.
It is hoped that this monograph will be a guide to your approach to
episiotomy.
Many Fellows of ACOG participated in the development of this
monograph, and it would be impossible to name them all. However,
special thanks go to Frank Ling, MD, Howard Blanchette, MD, John
Hauth, MD, and Gary Hankins, MD. A very special thank you goes to
Tamara Tin-May Ho Chao, MD, resident member of the RRC, for her
insightful comments.
Finally, this document would not have been possible without the
support of the ACOG Development Committee. Countless members of
ACOG donate to the Development Fund annually to allow ACOG to
expand its activities and further our educational endeavors. This
monograph is just one example of how those donations can have a
major impact.
Ralph W. Hale, MD
ACOG Executive Vice President
Introduction
The first use of an episiotomy to facilitate the delivery of an infant is
lost in the past. Whether ancient midwives or birth attendants used
primitive knives has been questioned for years. Perhaps they did or per-
haps they did not. What is known, however, is that intentional incision
of the perineum was not practiced as a routine procedure until the 20th
century.
Treatises on management of the perineum as the fetal head
emerges at the time of delivery focused on protecting against tears
and lacerations. In the 1700s, the usual description of a delivery of
the infants head concentrated on preserving the intact perineum by
allowing a slow, controlled dilation and delivery by exerting pressure
on the perineum ( 1) .
In 1828, Ferdinand von Ritgen described a similar maneuver for
easing the head over an intact perineum ( 2) . His procedure, which he
modified to use extension rather than flexion of the head, also was
designed to prevent trauma to the perineum while facilitating the deliv-
ery ( 3) . This was accomplished by placing the examiners fingers on the
perineal body and gently pushing the head from flexion to extension.
This maneuver is still performed in deliveries today and is known as the
Ritgen maneuver.
Although procedures for increasing the size of the vaginal outlet
may have been used in the United States by Native Americans, immi-
grant midwives, or others, the first reported use was in Virginia in 1852
( 4) . However, there is little evidence that it gained any regional or wide-
spread acceptance as part of a vaginal delivery.
In 1893, Karl August Schuchardt, preparing to perform a vaginal
approach to excision of a large cervical cancer, performed a medio-
lateral incision of the perineum to obtain additional exposure ( 5) . He
reported on this procedure to increase exposure in the same year. In his
report, he described incision in the mediolateral tissue and muscles
with much the same anatomical detail we would use today. Although
1
he never used the word episiotomy, the procedure would be called
gynecologic episiotomy today.
J. B. Delee usually is credited with popularizing the use of the epi-
siotomy when he became the champion for the use of forceps to pro-
tect the fetal head during delivery ( 6) . He felt strongly that use of the
forceps always should be accompanied by an episiotomy to prevent
damage to the pelvic floor. Because of Delees stature in the field of
obstetrics, his premise rapidly became accepted by U.S. obstetricians.
As more and more women gave birth in hospitals rather than
homes, episiotomy became the rule rather than the exception. The
lithotomy position, especially if extreme, actually accentuated the tight-
ening of the perineal opening and further contributed to the perceived
need for a surgical approach to increase the vaginal opening. This pro-
cedure, which began as a mediolateral approach, slowly evolved in the
United States during the 1950s and 1960s to predominantly a midline
procedure.
The purpose of the procedure, which was explained to residents
year after year, was to facilitate the second stage of labor. It also was
reported to reduce perianal trauma, pelvic floor dysfunction and pro-
lapse, urinary and fecal incontinence, and sexual dysfunction. Benefits
to the fetus were a shortened second stage and less potential trauma to
the fetal head.
In the 1970s and 1980s, however, obstetricians began to question
the validity of the concept of protecting the perineum and the benefits
related to routine episiotomy. In 1981, the National Childbirth Trust
in London published a study that questioned the use of episiotomy as
a routine procedure ( 7) . This led to further review and questioning of
routine use of episiotomy for vaginal delivery given that there was little
evidence to support the reported benefits.
Today, episiotomy is still the most common surgical procedure
performed by most obstetricians; however, it is much less common
than in the 20th century. In 2003, 716,000 episiotomies were per-
formed in the United States, whereas 11 years earlier, more than 1.6
million episiotomies were performed ( 8, 9) ( see table) . It most often
is used in women who are having their first child and less frequently
used with later children.
2 Episiotomy
Вам также может понравиться
- UW Path NoteДокумент218 страницUW Path NoteSophia Yin100% (4)
- Low Back Pain - Mechanism, Diagnosis and Treatment 6th Ed - J. Cox (Williams and Wilkinson, 1999) WW PDFДокумент752 страницыLow Back Pain - Mechanism, Diagnosis and Treatment 6th Ed - J. Cox (Williams and Wilkinson, 1999) WW PDFMatei Teodorescu100% (5)
- Acog Practice Bulletin: Thromboembolism in PregnancyДокумент17 страницAcog Practice Bulletin: Thromboembolism in PregnancytriОценок пока нет
- Assessment Test Descriptions PyДокумент19 страницAssessment Test Descriptions PyDewa Ayu VeronicaОценок пока нет
- Deep Sleep ExperimentsДокумент12 страницDeep Sleep ExperimentsCristina Lemoing100% (1)
- Evaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusДокумент7 страницEvaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusGabyliz Gonzalez CastilloОценок пока нет
- 34 Pictures To See Which Muscle You Are StretchingДокумент16 страниц34 Pictures To See Which Muscle You Are Stretchinggprasadatvu100% (1)
- Wendy J. Dahl - Health Benefits of Pulses-Springer International Publishing (2019) PDFДокумент160 страницWendy J. Dahl - Health Benefits of Pulses-Springer International Publishing (2019) PDFSolomon AssefaОценок пока нет
- Mullarian AnomoliesДокумент85 страницMullarian AnomoliesPrathibha GuruguriОценок пока нет
- Hamerlynck2018 Article FertilityOutcomeAfterTreatmentДокумент7 страницHamerlynck2018 Article FertilityOutcomeAfterTreatmentMahida El shafiОценок пока нет
- Asherman - 2014Документ4 страницыAsherman - 2014salsaОценок пока нет
- Ultrasound Obstetric and Gynecologic PDFДокумент190 страницUltrasound Obstetric and Gynecologic PDFAndrei MurariuОценок пока нет
- Phobias - See What Makes Some People AfraidДокумент2 страницыPhobias - See What Makes Some People Afraidbeep777Оценок пока нет
- 2019 - Bowel and Bladder Injury Repair and Follow-Up After Gynecologic Surgery - 00006250-201902000-00012Документ10 страниц2019 - Bowel and Bladder Injury Repair and Follow-Up After Gynecologic Surgery - 00006250-201902000-00012Polyana FloresОценок пока нет
- TOG Vaginal HysterectomyДокумент6 страницTOG Vaginal HysterectomyYasmin AlkhatibОценок пока нет
- Pop, RevДокумент139 страницPop, RevYusof AndreiОценок пока нет
- HematuriaДокумент15 страницHematurianisaw_2Оценок пока нет
- MRCOG Module SummaryДокумент4 страницыMRCOG Module SummaryAmadeus KQОценок пока нет
- ACOG SMFM Joint Practice Bulletin Multiple Gestation 2004Документ15 страницACOG SMFM Joint Practice Bulletin Multiple Gestation 2004Reza ZulkarnainОценок пока нет
- Renal Urology HistoryДокумент131 страницаRenal Urology Historysharu4291Оценок пока нет
- ACOG Tech BullitinДокумент20 страницACOG Tech BullitinJosephОценок пока нет
- وتين ٥Документ26 страницوتين ٥Mohammad AlrefaiОценок пока нет
- Acog Practice Bulletin TiroidesДокумент10 страницAcog Practice Bulletin TiroidesMerpi Alvarez Goris100% (1)
- The Management of Asherman Syndrome: A Review of LiteratureДокумент11 страницThe Management of Asherman Syndrome: A Review of LiteratureEuphra Adellheid100% (1)
- Minimally Invasive Versus Abdominal Radical HysterectomyДокумент10 страницMinimally Invasive Versus Abdominal Radical HysterectomyClinton Franda Markus SitanggangОценок пока нет
- Postsurgical Barrier Strategies Hysteroscopic AdhesiolysisДокумент20 страницPostsurgical Barrier Strategies Hysteroscopic AdhesiolysisHarry PratamaОценок пока нет
- Endometritis Unrelated To Pregnancy - UpToDateДокумент9 страницEndometritis Unrelated To Pregnancy - UpToDateLeoberto Batista Pereira SobrinhoОценок пока нет
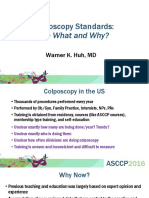
- 62 Colposcopy StandardsДокумент73 страницы62 Colposcopy Standardsrijal mahdiy pОценок пока нет
- The Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachДокумент8 страницThe Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachqisthiaufaОценок пока нет
- Abortion KuliahДокумент38 страницAbortion KuliahElsa Hasibuan100% (1)
- HSE Commitment and Policy?Документ6 страницHSE Commitment and Policy?radhesrikrishnaОценок пока нет
- Abdominal Organ Transplantation: State of the ArtОт EverandAbdominal Organ Transplantation: State of the ArtNizam MamodeОценок пока нет
- Vaginal Vault ProlapseДокумент9 страницVaginal Vault ProlapseOanaОценок пока нет
- Management of Benign Breast Conditions: Part 2 - Breast Lumps and LesionsДокумент3 страницыManagement of Benign Breast Conditions: Part 2 - Breast Lumps and Lesionspeter_mrОценок пока нет
- (Comprehensive Gynecology and Obstetrics) Hidetaka Katabuchi (Eds.) - Frontiers in Ovarian Cancer Science-Springer Singapore (2017)Документ313 страниц(Comprehensive Gynecology and Obstetrics) Hidetaka Katabuchi (Eds.) - Frontiers in Ovarian Cancer Science-Springer Singapore (2017)Suci NopitriОценок пока нет
- Surgery For Male InfertilityДокумент8 страницSurgery For Male InfertilityAkhmad MustafaОценок пока нет
- Laparoscopic Gynecologist Surgeon in HSR Layout BangaloreДокумент8 страницLaparoscopic Gynecologist Surgeon in HSR Layout BangaloreDr.Beena JeysinghОценок пока нет
- WeBSurg Winners 42 1Документ129 страницWeBSurg Winners 42 1Ana Adam100% (1)
- Approach To Episiotomy - UpToDateДокумент13 страницApproach To Episiotomy - UpToDatePedro Vilches Polaina100% (1)
- ACOG Bulletin MiscarriageДокумент12 страницACOG Bulletin Miscarriagebrabba19856403Оценок пока нет
- Acog Practice Bulletin Summary: Pregestational Diabetes MellitusДокумент3 страницыAcog Practice Bulletin Summary: Pregestational Diabetes MellitusMaría Fernanda Palma AcostaОценок пока нет
- Open Disclosure Principles Elements and ProcessДокумент11 страницOpen Disclosure Principles Elements and ProcessRedroses flowersОценок пока нет
- Urinary IncontinenceДокумент0 страницUrinary Incontinencemango91286Оценок пока нет
- Dystocia and Augmentation of LAbor PDFДокумент10 страницDystocia and Augmentation of LAbor PDFKathleenОценок пока нет
- ACOG Practice Bulletin No 99 Management of 39 PDFДокумент26 страницACOG Practice Bulletin No 99 Management of 39 PDFhkdawnwongОценок пока нет
- Craniofacial AbnormalitiesДокумент12 страницCraniofacial Abnormalitiesnpr00Оценок пока нет
- Gestational Trophoblastic DiseaseДокумент6 страницGestational Trophoblastic DiseaseSJ IraaОценок пока нет
- Premature Rupture of Membranes 2016Документ13 страницPremature Rupture of Membranes 2016Berenice TrejoОценок пока нет
- Sof MarkersДокумент21 страницаSof MarkersHari NairОценок пока нет
- Infertility ACOGДокумент8 страницInfertility ACOGRifdaОценок пока нет
- Isuog Guideline IugrДокумент15 страницIsuog Guideline IugrericОценок пока нет
- ACOG 109 Cervical Cytology ScreeningДокумент12 страницACOG 109 Cervical Cytology ScreeningNatalya FlorezОценок пока нет
- Fetal Medicine - Bidyut KumarДокумент4 страницыFetal Medicine - Bidyut KumarpatoxyzuОценок пока нет
- Poly Hi DR AmnionДокумент7 страницPoly Hi DR Amnionwanwan_adongОценок пока нет
- Obstetric Anal Sphincter Injury (OASIS) - UpToDateДокумент39 страницObstetric Anal Sphincter Injury (OASIS) - UpToDateErickОценок пока нет
- Placenta Iugr PDFДокумент298 страницPlacenta Iugr PDFM Iqbal EffendiОценок пока нет
- Tuberculosis in Obstetrics and GynecologyДокумент42 страницыTuberculosis in Obstetrics and GynecologyameenОценок пока нет
- Caesarean Scar Ectopic Pregnancy: Case ReportДокумент3 страницыCaesarean Scar Ectopic Pregnancy: Case ReportDewi SaftariОценок пока нет
- Practice Bulletin: Antiphospholipid SyndromeДокумент8 страницPractice Bulletin: Antiphospholipid SyndromeSus ArОценок пока нет
- ACOG Practice Bulletin No 202 Gestational.49Документ25 страницACOG Practice Bulletin No 202 Gestational.49Diana Enco MurillosОценок пока нет
- Thesis Protocol: DR - Manali Kagathara Narayanamultispeciality Hospital, JaipurДокумент15 страницThesis Protocol: DR - Manali Kagathara Narayanamultispeciality Hospital, JaipurMaitree PОценок пока нет
- OSCE Student Exam in Obstetrics &gynecology: DR: Manal Behery Faculty of Medicine, Zagazig University 2014Документ64 страницыOSCE Student Exam in Obstetrics &gynecology: DR: Manal Behery Faculty of Medicine, Zagazig University 2014Karam SaadОценок пока нет
- Acog SDR AntifosfolipidicДокумент8 страницAcog SDR Antifosfolipidicleonar8Оценок пока нет
- GA by Ultrasound SOGCДокумент11 страницGA by Ultrasound SOGCBrendaОценок пока нет
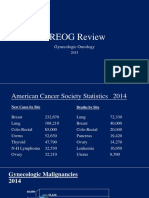
- 2015 Oncology CREOG Review PDFДокумент76 страниц2015 Oncology CREOG Review PDFRima HajjarОценок пока нет
- Judi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009Документ66 страницJudi Januadi Endjun: Gatot Soebroto Army Central Hospital/ Medical Faculty, University of Indonesia ISUOG, Bali, 2009emilyakmanОценок пока нет
- 2023 OB/GYN Coding Manual: Components of Correct CodingОт Everand2023 OB/GYN Coding Manual: Components of Correct CodingОценок пока нет
- Abortion and Sterilization: Medical and Social AspectsОт EverandAbortion and Sterilization: Medical and Social AspectsJane E. HodgsonОценок пока нет
- Comparison CarsДокумент5 страницComparison Carssharu4291Оценок пока нет
- ChoiДокумент19 страницChoiLuciana RafaelОценок пока нет
- Hyperglycemic Hyperosmolar Nonketotic Syndrome: R. Venkatraman and Sunit C. SinghiДокумент6 страницHyperglycemic Hyperosmolar Nonketotic Syndrome: R. Venkatraman and Sunit C. Singhisharu4291Оценок пока нет
- Approach To A Case of Hyperuricemia: Singh V, Gomez VV, Swamy SGДокумент7 страницApproach To A Case of Hyperuricemia: Singh V, Gomez VV, Swamy SGsharu4291Оценок пока нет
- Molecules 18 08976Документ18 страницMolecules 18 08976sharu4291Оценок пока нет
- ABC Emergency Differential DiagnosisdrererДокумент3 страницыABC Emergency Differential Diagnosisdrerersharu4291Оценок пока нет
- Prospectus MDMSJULY2015Документ39 страницProspectus MDMSJULY2015sharu4291Оценок пока нет
- Chapter 23: Hyperuricemia and Gout: BackgroundДокумент2 страницыChapter 23: Hyperuricemia and Gout: Backgroundsharu4291Оценок пока нет
- ABC Emergency Differential DiagnosisffДокумент3 страницыABC Emergency Differential Diagnosisffsharu4291Оценок пока нет
- ABC Emergency Differential DiagnДокумент3 страницыABC Emergency Differential Diagnsharu4291Оценок пока нет
- Intern ACOG Bulletin Episiotomy and Repair3Документ3 страницыIntern ACOG Bulletin Episiotomy and Repair3sharu4291Оценок пока нет
- ABC Emergency Differential Diagnosis1Документ4 страницыABC Emergency Differential Diagnosis1sharu4291Оценок пока нет
- ABC Emergency Differential DiagnosisewwwwweДокумент3 страницыABC Emergency Differential Diagnosisewwwwwesharu4291Оценок пока нет
- 3390 3396 PDFДокумент7 страниц3390 3396 PDFXavier Alexandro Ríos SalinasОценок пока нет
- 2Документ6 страниц2muiОценок пока нет
- 13 Areas of Assessment Pedia DutyДокумент3 страницы13 Areas of Assessment Pedia DutyJoshua MendozaОценок пока нет
- Youth Stress EssayДокумент3 страницыYouth Stress EssayGemma100% (1)
- Jan 5, 2021 TDIR Worksheet (COG 2)Документ122 страницыJan 5, 2021 TDIR Worksheet (COG 2)Clarabelle Mae Dela RosaОценок пока нет
- Brucellosis - DR Esayas Kebede GudinaДокумент44 страницыBrucellosis - DR Esayas Kebede GudinaEsayas KebedeОценок пока нет
- Format Nutritional StatusДокумент43 страницыFormat Nutritional StatusDirkie Meteoro Rufin83% (6)
- City Government of Kabankalan: State Protect TheДокумент2 страницыCity Government of Kabankalan: State Protect ThefortunecОценок пока нет
- Cossh Risk Assessment: Carried Out By: Department: Date: Substance Name: CRA NumberДокумент2 страницыCossh Risk Assessment: Carried Out By: Department: Date: Substance Name: CRA NumberNiraОценок пока нет
- Citation WorksheetДокумент5 страницCitation WorksheetZafar Ibn Kader 2013819030Оценок пока нет
- Tapan Majhi 10.12.21Документ6 страницTapan Majhi 10.12.21Suman MajhiОценок пока нет
- NHS Change ManagementДокумент20 страницNHS Change ManagementMary NjeriОценок пока нет
- Intussusception - A Case ReportДокумент3 страницыIntussusception - A Case ReportAgustinus HuangОценок пока нет
- Nooriya Prabhakaran Visualcv Resume 2017Документ2 страницыNooriya Prabhakaran Visualcv Resume 2017api-372799602Оценок пока нет
- Arousal Scoring - ASSMДокумент21 страницаArousal Scoring - ASSMkawaiiriceОценок пока нет
- MMHA - Decriminalization & Thresholds - CPT Members - April 21, 2022Документ6 страницMMHA - Decriminalization & Thresholds - CPT Members - April 21, 2022Tyler HarperОценок пока нет
- Bioethics EssayДокумент7 страницBioethics Essayapi-336568283Оценок пока нет
- PEDIATRIC DRUG DOSAGES (Neonatal Doses Are Different) : NebulisationsДокумент9 страницPEDIATRIC DRUG DOSAGES (Neonatal Doses Are Different) : NebulisationsAvi KhannaОценок пока нет
- Jurnal InternasionalДокумент110 страницJurnal InternasionalRafi DevianaОценок пока нет
- Liposuction: Immediately After SurgeryДокумент1 страницаLiposuction: Immediately After SurgeryScott J. Zevon, MD, FACSОценок пока нет
- MScHandbook Imperial Chemical EnggДокумент87 страницMScHandbook Imperial Chemical EnggMurugeshОценок пока нет
- Crown & Bridge RemovalДокумент1 страницаCrown & Bridge RemovalCamilaОценок пока нет