Академический Документы
Профессиональный Документы
Культура Документы
Blood Tests
Загружено:
clea1Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Blood Tests
Загружено:
clea1Авторское право:
Доступные форматы
About blood tests
What does it mean - and what is normal in Blood tests ? The names may be different in various countries
and so may the values. Please double-check with your own standards. Please find the tests in the boxes mentioned
below.
These pages contains two different explanations to the bloodtests. The first one is a longer one and very thorough -
with information about the normal ranges. (Please observe: there are different values in different countries). It might
mainly be for healthcare persons . It is divided into various groups: Liver Function - Liver enzymes - Blood chemistry -
Electrolytes - Lipids - Protein - Ratio's - Thyroid - Differential - and other. Please see the boxes.
There is also a shorter version = Common Laboratory Tests in Liver Diseases by Howard J. Worman, M. D. This
is meant to be read by patients and spouses.
Please observe: From the bloodtests: ALT (alanine aminotransferase) = SGPT (in Danish ALAT) - and AST (asparate
aminotransferase) = SGOT (in Danish ASAT)
Overall view
LIVER FUNCTION AST / SGOT (short) ALT / SGPT (short) ALT or SGPT, long AST or SGOT, long
Albumin Alkaline Phosphatase Bilirubin, Total Cholesterol
GGT Globulin LDH Protein, Total
Liver Enzymes SGOT (Serum Glutamic-Oxalocetic
Transaminase - AST)
SGPT (Serum
Glutamic-Pyruvic
Transaminase - ALT)
ALKALINE PHOSPHA-TASE GGT (Gamma-Glutamyl
Transpeptidase)
LDH (Lactic Acid Dehydrogenase) BILIRUBIN, TOTAL B.U.N. (Blood Urea Nitrogen) CREATININE
URIC ACID
Blood Chemistry
Definitions
Hematology HematocritHemoglobin MCH (Mean
Corpuscular
Hemoglobin)
MCV (Mean Corpuscular
Volume) -
MCHC (Mean Corpuscular
Hemoglobin
Concentration)
R.B.C. (Red Blood Cell Count) W.B.C. (White Blood
Cell Count)
PLATELET COUNT
Protein PROTEIN, TOTAL ALBUMIN GLOBULIN Albumin/Globulin Ratio
Electrolytes SODIUM POTASSIUM CHLORIDE CALCIUM
CO2 (Carbon Dioxide) PHOSPHORUS
Lipids CHOLESTE-ROL TRIGLY-CERIDES LDL (Low Density
Lipoprotein)
HDL (High Density
Lipoprotein)
CHOLESTE-ROL/LDL RATIO
Ratio's ANION GAP (Sodium + Potassium
- CO2 + Chloride)
BUN/CREATININE CALCIUM/PHOSPHORUS SODIUM/POTASSIUM
Thyroid THYROXINE (T4) FREE T4 INDEX
(T7)
T3-UPTAKE THYROID-STIMULATING
HORMONE (TSH)
Differential NEUTRO-PHILS and
NEUTROPHIL COUNT
LYMPHO-CYTES and
COUNT
MONOCYTES and
MONOCYTE COUNT
EOSINOPHILS and
EOSINOPHIL COUNT
BASOPHILS and BASOPHIL
COUNT
Other GLUCOSE (Fasting) IRON, TOTAL
The long version:
LIVER FUNCTION
A/G Ratio - Albumin - Alkaline Phosphatase - Bilirubin, Total - Cholesterol - GGT
Globulin - LDH - Protein, Total - AST/SGOT - ALT / SGPT
Liver Enzymes
ALT OR SGPT
ALT, an enzyme appears in liver cells, with lesser amounts in the kidneys, heart, and skeletal muscles, and is a
relatively specific indicator of acute liver cell damage. When such damage occurs, ALT is released from the liver cells
into the bloodstream, often before jaundice appears, resulting in abnormally high serum levels that may not return to
normal for days or weeks.
The purpose of this blood serum test is to help detect and evaluate treatment of acute hepatic disease, especially
hepatitis, and cirrhosis without jaundice. To help distinguish between mytyocardial (heart) and liver tissue damage
(used with the AST enzyme test). Also to assess hepatotoxicity of some drugs.
ALT levels by a commonly used method range from 10 to 32 U/L; in women, from 9 to 24 U/L. (There does exist
differing ranges used by various laboratories.)
The normal range for infants is twice that of adults.
Very high ALT levels (up to 50 times normal) suggest viral or severe drug-
induced hepatitis, or other hepatic disease with extensive necrosis (death of liver cells). (AST levels are also elevated
but usually to a lesser degree.) Moderate-to-high levels may indicate infectious mononucleosis, chronic hepatitis,
intrahepatic cholestasis or cholecystitis, early or improving acute viral hepatitis, or severe hepatic congestion due to
heart failure. Slight-to-moderate elevations of ALT (usually with higher increases in AST levels) may appear in any
condition that produces acute hepatocellular (liver cell) injury, such as active cirrhosis, and drug-induced or alcoholic
hepatitis.
Marginal elevations occasionally occur in acute myocardial infarction (heart attack), reflecting secondary hepatic
congestion or the release of small amounts of ALT from heart tissue.
Many medications produce hepatic injury by competitively interfering with cellular metabolism. Falsely elevated ALT
levels can follow use of barbiturates, narcotics, methotrexate, chlorpromazine salicylates (aspirin), and other drugs
that affect the liver.
Be Aware: Serum liver enzymes can create confusion for both patients and physicians for these tests are
highly sensitive, but very non-specific. Tests commonly referred to as liver function tests or LFT's do not
actually determine liver function. Instead, they are static, primarily diagnostic parameters that serve to detect
liver disease rather than quantitative liver function. Rather than liver function tests, it is more useful to refer to
these tests as serum liver tests and to mentally categorise them according to the pathophysiologic processes
they truly reflect.
SGPT (Serum Glutamic-Pyruvic Transaminase - ALT)
Serum Glutamic Pyruvic Transaminase or ALT is an enzyme found primarily in the liver but
also to a lesser degree, the heart and other tissues. It is useful in diagnosing liver function
more so than SGOT levels. Decreased SGPT in combination with increased cholesterol levels
is seen in cases of a congested liver. We also see increased levels in mononucleosis,
alcoholism, liver damage, kidney infection, chemical pollutants or myocardial infarction.
Normal Adult Range: 0 - 48 U/L
Optimal Adult Reading: 24
AST or SGOT
One of the two main liver function blood serum tests (the other being the ALT test). The purpose of this blood test is to
detect a recent myocardial infarction (heart attack); to aid detection and differential diagnosis of acute hepatic disease
and to monitor patient progress and prognosis in cardiac and hepatic diseases. AST levels by a commonly used
method range from 8 to 20 U/L although some ranges may express a maximum high in the 40s. (Check with your
physician.)
AST levels fluctuate in response to the extent of cellular necrosis (cell death) and therefore may be temporarily and
minimally elevated early in the disease process, and extremely elevated during the most acute phase. Depending on
when the initial sample was drawn, AST levels can rise- indicating increasing disease severity and tissue damage- or
fall- indicating disease resolution and tissue repair. Thus, the relative change in AST values serves as a reliable
monitoring mechanism.
Maximum elevations are associated with certain diseases and conditions. For example, very high elevations
(more than 20 times normal) may indicate acute viral hepatitis, severe skeletal muscle trauma, extensive
surgery, drug- induced hepatic injury, and severe liver congestion. High levels (ranging from 10 to 20 times
normal) may indicate severe myocardial infarction (heart attack), severe infectious mononucleosis, and
alcoholic cirrhosis. High levels may also occur during the resolving stages of conditions that cause maximal
elevations. Moderate-to-high levels (ranging from 5 to 10 times normal) may indicate chronic hepatitis and
other conditions. Low-to-moderate levels (ranging from 2 to 5 times normal) may indicate metastatic hepatic
tumours, acute pancreatitis, pulmonary emboli, alcohol withdrawal syndrome, and fatty liver (steatosis).
SGOT (Serum Glutamic-Oxalocetic Transaminase - AST)
Serum Glutamic Oxalocetic Transaminase or AST is an enzyme found primarily in the liver,
heart, kidney, pancreas, and muscles. Seen in tissue damage, especially heart and liver, this
enzyme is normally elevated. Vitamin B deficiency and pregnancy are two instances where
the enzyme may be decreased.
Normal Adult Range: 0 - 42 U/L
Optimal Adult Reading: 21
Back to the English index
Blood Chemistry Definitions
Hematology - Hematocrit - Hemoglobin -
MCH (Mean Corpuscular Hemoglobin) -
MCV (Mean Corpuscular Volume) -
MCHC (Mean Corpuscular Hemoglobin Concentration)
R.B.C. (Red Blood Cell Count)
W.B.C. (White Blood Cell Count)
PLATELET COUNT
Hematology
HEMATOCRIT (HCT)
The word hematocrit means "to separate blood," a procedure which is followed following the
blood draw through the proper use of a centrifuge. Hematocrit is the measurement of the
percentage of red blood cells in whole blood. It is an important determinant of anemia
(decreased) , polycythemia (increased), dehydration (elevated), increased R.B.C. breakdown
in the spleen (elevated), or possible overhydration (elevated)
Normal Adult Female Range: 37 - 47%
Optimal Adult Female Reading: 42%
Normal Adult Male Range 40 - 54%
Optimal Adult Male Reading: 47
Normal Newborn Range: 50 - 62%
Optimal Newborn Reading: 56
HEMOGLOBIN (HGB)
Hemoglobin is the main transport of oxygen and carbon dioxide in the blood. It is composed
of globin a group of amino acids that form a protein and heme which contains iron atoms and
the red pigment, porphyrin. As with Hematocrit, it is an important determinant of anemia
(decreased), dehydration (increased), polycythemia (increased), poor diet/nutrition, or
possibly a malabsorption problem.
Normal Adult Female Range: 12 - 16%
Optimal Adult Female Reading: 14
Normal Adult Male Range: 14 - 18%
Optimal Adult Male Reading: 16
Normal Newborn Range: 14 - 20%
Optimal Newborn Reading: 17
MCH (Mean Corpuscular Hemoglobin)
Hemoglobin x 10
R.B.C.
Mean Corpuscular Hemoglobin (MCH) gives the average weight of hemoglobin in the red
blood cell. Due to its use of red blood cells in its calculation, MCH is not as accurate as
MCHC in its diagnosis of severe anemia's. Decreased MCH is associated with microcytic
anemia and increased MCH is associated with macrocytic anemia.
Normal Adult Range: 27 - 33 pg
Optimal Adult Reading: 30
MCV (Mean Corpuscular Volume)
Hematocrit x 10
R.B.C.
The Mean Corpuscular Volume reflects the size of red blood cells by expressing the volume
occupied by a single red blood cell. Increased readings may indicate macrocytic anemia or B6
or Folic Acid deficiency and decreased readings may indicate microcytic anemia, possibly
caused by iron deficiency.
Normal Adult Range: 80 - 100 fl
Optimal Adult Reading: 90
Higher ranges are found in newborns and infants
MCHC (Mean Corpuscular Hemoglobin Concentration)
Hemoglobin x 100
Hematocrit
This test measures the average concentration of hemoglobin in red blood cells. It is most
valuable in evaluating therapy for anemia because Hemoglobin and Hematocrit are used, not
R.B.C. in the calculation. Low MCHC means that a unit of packed R.B.C.s contain less
hemoglobin than normal and a high MCHC means that there is more hemoglobin in a unit of
R.B.C.s. Increased MCHC is seen in spherocytosis, and not seen in pernicious anemia
whereas decreased levels may indicate iron deficiency, blood loss, B6 deficiency of
thalassemia.
Normal Adult Range: 32 - 36 %
Optimal Adult Reading: 34
Higher ranges are found in newborns and infants
R.B.C. (Red Blood Cell Count)
Red blood cells main function is to carry oxygen to the tissues and to transfer carbon dioxide
to the lungs. This process is possible through the R.B.C. containing hemoglobin which
combines easily with oxygen and carbon dioxide.
Normal Adult Female Range: 3.9 - 5.2 mill/mcl
Optimal Adult Female Reading: 4.55
Normal Adult Male Range: 4.2 - 5.6 mill/mcl
Optimal Adult Male Reading: 4.9
Lower ranges are found in Children, newborns and infants
Panel: Hematology
W.B.C. (White Blood Cell Count)
White blood cells main function is to fight infection, defend the body by phagocytosis against
invasion by foreign organisms, and to produce, or at least transport and distribute, antibodies
in the immune response. There are a number of types of leukocytes (see differential) that are
classified as follows
Granulocytes Nongranulocytes
Band Neutrophiles Lymphocytes
Neutrophils Monocytes
Eosinophils
Basophils
Each cell, or leukocyte, has a different job in the body which is explained in
the Differential section.
Normal Adult Range: 3.8 - 10.8 thous/mcl
Optimal Adult Reading: 7.3
Higher ranges are found in children, newborns and infants.
PLATELET COUNT
Platelets (also known as thrombocytes) are the smallest formed elements of the blood. They
are vital to coagulation of the blood to prevent excessive bleeding. Elevated levels suggest
dehydration or stimulation of the bone marrow where the cells are produced and decreased
levels may indicate an immune system failure, drug reactions, B12 or folic acid deficiency.
Normal Adult Range: 130 - 400 thous/mcl
Optimal Adult Reading: 265
Higher ranges are found in children, newborns and infants.
Electrolytes
SODIUM - POTASSIUM - CHLORIDE - CO2 (Carbon Dioxide) - CALCIUM - PHOSPHORUS -
SODIUM
Sodium is the most abundant cation in the blood and its chief base. It functions in the body to
maintain osmotic pressure, acid-base balance and to transmit nerve impulses.
Normal Adult Range: 135-146 mEq/L
Optimal Adult Reading: 140.5
POTASSIUM
Potassium is the major intracellular cation in the blood. It, along with sodium, helps to
maintain osmotic balance and in also involved in acid-base balance. It is needed for proper
nerve and muscle action.
Normal Range: 3.5 - 5.5 mEq/L
Optimal Adult Reading: 4.5
CHLORIDE
Chlorides significance relates to its maintenance of cellular integrity through it influence on
osmotic pressure, it also helps monitor acid-base balance and water balance. Elevated levels
are related to acidosis as well as too much water crossing the cell membrane. Decreased
levels with decreased serum albumin may indicate water deficiency crossing the cell
membrane (edema).
Normal Adult Range: 95-112 mEq/L
Optimal Adult Reading: 103
CO2 (Carbon Dioxide)
The CO2 level is related to the respiratory exchange of carbon dioxide in the lungs and is part
of the bodies buffering system. Generally when used with the other electrolytes, it is a good
indicator of acidosis and alkalinity.
Normal Adult Range: 22-32 mEq/L
Optimal Adult Reading: 27
Normal Childrens Range - 20 - 28 mEq/L
Optimal Childrens Reading: 24
CALCIUM
The most abundant mineral in the body, it is involved in bone metabolism, protein absorption,
fat transfer muscular contraction, transmission of nerve impulses, blood clotting and cardiac
function. It is highly sensitive to elements such as magnesium, iron and phosphorus as well
as hormonal activity, vitamin D levels, alkalinity and acidity, and many drugs.
Normal Adult Range: 8.5-10.3 mEq/dl
Optimal Adult Reading: 9.4
PHOSPHORUS
Phosphorus is an abundant element found in most tissues and cells. It is closely related to the
calcium level with an inverse relationship. When calcium is increased, phosphorus tends to
decrease and vice versa. Careful following of blood draw procedures are necessary because
improper handling may cause false elevated readings. Phosphorus is needed for its buffering
action, calcium transport and osmotic pressure.
Normal Adult Range: 2.5 - 4.5 mEq/dl
Optimal Adult Reading: 3.5
Normal Childrens Range: 3 - 6 mEq/dl
Optimal Childrens Range: 4.5
Liver Enzymes
SGOT (Serum Glutamic-Oxalocetic Transaminase - AST) -
SGPT (Serum Glutamic-Pyruvic Transaminase - ALT)
ALKALINE PHOSPHATASE -
GGT (Gamma-Glutamyl Transpeptidase)
LDH (Lactic Acid Dehydrogenase)
BILIRUBIN, TOTAL
B.U.N. (Blood Urea Nitrogen)
CREATININE
URIC ACID
SGOT (Serum Glutamic-Oxalocetic Transaminase - AST)
Serum Glutamic Oxalocetic Transaminase or AST is an enzyme found primarily in the liver,
heart, kidney, pancreas, and muscles. Seen in tissue damage, especially heart and liver, this
enzyme is normally elevated. Vitamin B deficiency and pregnancy are two instances where
the enzyme may be decreased.
Normal Adult Range: 0 - 42 U/L
Optimal Adult Reading: 21
SGPT (Serum Glutamic-Pyruvic Transaminase - ALT)
Serum Glutamic Pyruvic Transaminase or ALT is an enzyme found primarily in the liver but
also to a lesser degree, the heart and other tissues. It is useful in diagnosing liver function
more so than SGOT levels. Decreased SGPT in combination with increased cholesterol levels
is seen in cases of a congested liver. We also see increased levels in mononucleosis,
alcoholism, liver damage, kidney infection, chemical pollutants or myocardial infarction.
Normal Adult Range: 0 - 48 U/L
Optimal Adult Reading: 24
ALKALINE PHOSPHATASE
Produced in the cells of the bone and liver with some activity in the kidney, intestine, and
placenta, it is mostly found in an alkaline state with a pH of 9. Used extensively as a tumor
marker it is also present in bone injury, pregnancy, or skeletal growth (elevated readings).
Growing children have normally higher levels of this enzyme also. Low levels are sometimes
found in hypoadrenia, protein deficiency, malnutrition and a number of vitamin deficiencies.
Normal Adult Range: 20 - 125 U/L
Optimal Adult Reading: 72.5
Normal Childrens Range: 40 - 400 U/L
Optimal Childrens Reading: 220
GGT (Gamma-Glutamyl Transpeptidase)
Believed to be involved in the transport of amino acids and peptides into cells as well as
glutithione metabolism, Gamma-Glutamyl Transpeptidase is mainly found in liver cells and as
such is extremely sensitive to alcohol use. Elevated levels may be found in liver disease,
alcoholism, bile-duct obstruction, cholangitis, drug abuse, and in some cases excessive
magnesium ingestion. Decreased levels can be found in hypothyroidism, hypothalamic
malfunction and low levels of magnesium.
Normal Adult Female Range: 0 - 45 U/L
Optimal Female Reading: 22.5
Normal Adult Male Range: 0 - 65 U/L
Optimal Male Reading: 32.5
LDH (Lactic Acid Dehydrogenase)
Lactic acid dehydrogenase is an intracellular enzyme from particularly in the kidney, heart,
skelatal muscle, brain, liver and lungs. Increases are usually found in cellular death and/or
leakage from the cell or in some cases it can be useful in confirming myocardial or pulmonary
infarction (only in relation to other tests). Decreased levels of the enzyme may be seen in
cases of malnutrition, hypoglycemia, adrenal exhaustion or low tissue or organ activity.
Normal Adult Range: 0 - 250 U/L
Optimal Adult Reading: 125
BILIRUBIN, TOTAL
A byproduct of the breakdown of red blood cells in the liver, bilirubin is a good indication of
the livers function. Excreted into the bile, bilirubin gives the bile its pigmentation. Elevated in
liver disease, mononucleosis, hemolytic anemia, low levels of exposure to the sun, and toxic
effects to some drugs, decreased levels are seen in people with an inefficient liver, excessive
fat digestion, and possibly a diet low in nitrogen bearing foods.
Normal Adult Range 0 - 1.3 mg/dl
Optimal Adult Reading: .65
Nitrogen Elements
B.U.N. (Blood Urea Nitrogen)
The nitrogen component of urea, B.U.N. is the end product of protein metabolism and its
concentration is influenced by the rate of excretion. Increases can be caused by excessive
protein intake, kidney damage, certain drugs, low fluid intake, intestinal bleeding, exercise or
heart failure. Decreased levels may be dur to a poor diet, malabsorption, liver damage or low
nitrogen intake.
Normal Adult Range: 7 - 25 mg/dl
Optimal Adult Reading: 16
CREATININE
Creatinine is the waste product of muscle metabolism. Its level is a reflection of the bodies
muscle mass. Low levels are sometimes seen in kidney damage, protein starvation, liver
disease or pregnancy. Elevated levels are sometimes seen in kidney disease due to the
kidneys job of excreting creatinine, muscle degeneration, and some drugs involved in
impairment of kidney function.
Normal Adult Range: .7 - 1.4 mg/dl
Optimal Adult Reading: 1.05
URIC ACID
Uric acid is the end product of purine metabolism and is normally excreted through the urine.
High levels are noted in gout, infections, kidney disease, alcoholism, high protein diets, and
with toxemia in pregnancy. Low levels may be indicative of kidney disease, malabsorption,
poor diet, liver damage or an overly acid kidney.
Normal Adult Female Range: 2.5 - 7.5 mg/dl
Optimal Adult Female Reading: 5.0
Normal Adult Male Range: 3.5 - 7.5 mg/dl
Optimal Adult Male Reading:5.5
Protein
PROTEIN, TOTAL
ALBUMIN
GLOBULIN
A/G RATIO (Albumin/Globulin Ratio)
PROTEIN, TOTAL
Proteins are the most abundant compound in serum. The protein makeup of the individual is
of important diagnostic significance because of proteins involvement in enzymes, hormones
and antibodies as well as osmotic pressure balance, maintaining acid-base balance and as a
reserve source of nutrition for the bodies tissues and muscles. The major serum proteins
measured are Albumin and Globulin (alpha1, alpha2, beta and gamma). Decreased levels
may be due to poor nutrition, liver disease, malabsorption, diarrhea, or severe burns.
Increased levels are seen in lupus, liver disease, chronic infections, alcoholism, leukemia,
tuberculosis amongst many others. Careful review of the individuals albumin, globulin and
A/G ratio are recommended.
Normal Adult Range: 6.0 -8.5 g/dl
Optimal Adult Reading: 7.25
ALBUMIN
Albumin is the major constituent of serum protein (usually over 50%). It is manufactured by
the liver from the amino acids taken through the diet. It helps in osmotic pressure regulation,
nutrient transport and waste removal. High levels are seen rarely in liver disease, shock,
dehydration, or multiple myeloma. Lower levels are seen in poor diets, diarrhea, fever,
infection, liver disease, inadequate iron intake, third-degree burns and edemas or
hypocalcemia.
Normal Adult Range: 3.2 - 5.0 g/dl
Optimal Adult Reading: 4.1
GLOBULIN
Globulin, a larger protein than albumin, is important for its immunologic responses, especially
its gamma portion (IgA, IgG, IgM, and IgE). Globulins have many diverse functions such as,
the carrier of some hormones, lipids, metals, and antibodies. When chronic infections, liver
disease, rheumatoid arthritis, myelomas, and lupus are present, elevated levels are seen.
You may find lower levels in immune compromised patients, poor dietary habits,
malabsorption and liver or kidney disease.
Normal Adult Range: 2.2 - 4.2 g/dl (calculated)
Optimal Adult Reading: 3.2
A/G RATIO (Albumin/Globulin Ratio)
A/G ratio is an important indicator of disease states although a high level is not considered
clinically significant.
Normal Adult Range: 0.8 - 2.0 (calculated)
Optimal Adult Reading: 1.9
Lipids
CHOLESTEROL
TRIGLYCERIDES
LDL (Low Density Lipoprotein)
HDL (High Density Lipoprotein)
CHOLESTEROL/LDL RATIO
CHOLESTEROL
Cholesterol is a critical fat that is a structural component of cell membrane and plasma
lipoproteins, and is important in the synthesis of steroid hormones, glucocorticoids, and bile
acids. Mostly synthesized in the liver, some is absorbed through the diet, especially one high
in saturated fats. High density lipoproteins (HDL) is desired as opposed to the low density
lipoproteins (LDL), two types of cholesterol. Elevated cholesterol has been seen in
artherosclerosis, diabetes, hypothyroidism and pregnancy. Low levels are seen in depression,
malnutrition, liver insufficiency, malignancies, anemia and infection.
Normal Adult Range: 120 - 240 mg/dl
Optimal Adult Reading: 180
TRIGLYCERIDES
Triglycerides, stored in adipose tissues as glycerol, fatty acids and monoglyceroids, are
reconverted as triglycerides by the liver. Ninety percent of the dietary intake and 95% of the
fat stored in tissues are triglycerides. Increased levels may be present in artherosclerosis,
hypothyroidism, liver disease, pancreatitis, myocardial infarction, metabolic disorders,
toxemia, and nephrotic syndrome. Decreased levels may be present in chronic obstructive
pulmonary disease, brain infarction, hyperthyroidism, malnutrition, and malabsorption.
Normal Adult Range: 0 - 200 mg/dl
Optimal Adult Reading: 100
LDL (Low Density Lipoprotein)
LDL is the cholesterol rich remnants of the lipid transport vehicle VLDL (very-low density
lipoproteins) there have been many studies to correlate the association between high levels of
LDL and arterial artherosclerosis. Due to the expense of direct measurement of LDL a
calculation, known as the Friedewald formula is used. It is Total Cholesterol - HDL
Cholesterol - Triglycerides/5. When triglyceride levels are greater than 400, this method is not
accurate.
Normal Adult Range: 62 - 130 mg/dl
Optimal Adult Reading: 81 mg/dl
HDL (High Density Lipoprotein)
HDL or High-density lipoprotein is the cholesterol carried by the alpha lipoproteins. A high
level of HDL is an indication of a healthy metabolic system if there is no sign of liver disease
or intoxication. the two mechanisms that explain how HDL offers protection against chronic
heart disease are that HDL inhibits cellular uptake of LDL and serves as a carrier that
removes cholesterol from the peripheral tissues and transports it back to the liver for
catabolism and excretion
Normal Adult Range: 35 - 135 mg/dl
Optimal Adult Reading: +85 mg/dl
CHOLESTEROL/LDL RATIO
The ratio of total cholesterol and LDL (low density lipoprotein).
Normal Adult Range: 1 - 6
Optimal Adult Reading: 3.5
Ratio's
ANION GAP (Sodium + Potassium - CO2 + Chloride)
BUN/CREATININE
CALCIUM/PHOSPHORUS
SODIUM/POTASSIUM
ANION GAP (Sodium + Potassium - CO2 + Chloride)
The anion gap is used to measure the concentration of cations (sodium and potassium) and
the anions (chloride and CO2) in the extracellular fluid of the blood. There are numerous
clinical implications that can be gathered from the Anion Gap. An increased measurement is
associated with metabolic acidosis due to the overproduction of acids (a state of alkalinity is in
effect). Decreased levels may indicate metabolic alkalosis due to the overproduction of
alkaloids (a state of acidosis is in effect).
Normal Adult Range: 4 - 14 (calculated)
Optimal Adult Reading: 9
BUN/CREATININE
A high reading in this calculation is normally indicative of too much BUN being formed and a
low reading may show that the BUN is low or that the creatinine is not being cleared
effectively by the kidney. This calculation is a good measurement of kidney and liver function.
Normal Adult Range: 6 -25 (calculated)
Optimal Adult Reading: 15.5
CALCIUM/PHOSPHORUS
Due to the delicate balance between calcium and phosphorus in the system, this calculation
is helpful in noting subtle and acute imbalances in the relationship between the two elements.
Normal Adult Range: 2.3 - 3.3 (calculated)
Optimal Adult Reading: 2.8
Normal Childrens range: 1.3 - 3.3 (calculated)
Optimal Childrens Reading: 2.3
SODIUM/POTASSIUM
As the two major blood electrolytes, sodium as the extracellular cation and potassium as the
intracellular cation, this is an important ratio to review and act upon when subtle or acute
imbalances are noted.
Normal Adult Range: 26 - 38 (calculated)
Optimal Adult Reading: 32
Differential
NEUTROPHILS and NEUTROPHIL COUNT
LYMPHOCYTES and LYMPHOCYTE COUNT
MONOCYTES and MONOCYTE COUNT
EOSINOPHILS and EOSINOPHIL COUNT
BASOPHILS and BASOPHIL COUNT
NEUTROPHILS and NEUTROPHIL COUNT
Also known as Granulocytes or segmented neutrophils, this is the main defender of the body
against infection and antigens. High levels may indicate an active infection, a low count may
indicate a compromised immune system or depressed bone marrow (low neutrophil
production.
Normal Adult Range: 48 - 73 %
Optimal Adult Reading: 60.5
Normal Childrens Range: 30 - 60 %
Optimal Childrens Reading: 45
LYMPHOCYTES and LYMPHOCYTE COUNT
Lymphocytes are involved in protection of the body from viral infections such as measles,
rubella, chickenpox, or infectious mononucleosis. Elevated levels may indicate an active viral
infection and a depressed level may indicate an exhausted immune system or if the
neutrophils are elevated an active infection.
Normal Adult Range: 18 - 48 %
Optimal Adult Reading: 33
Normal Childrens Range: 25 - 50 %
Optimal Childrens Reading: 37.5
MONOCYTES and MONOCYTE COUNT
These cells are helpful in fighting severe infections and are considered the bodies second line
of defense against infection and are the largest cells in the blood stream. Elevated levels are
seen in tissue breakdown or chronic infections, carcinomas, leukemia (monocytic) or
lymphomas. Low levels are indicative of a state of health.
Normal Adult Range: 0 - 9 %
Optimal Adult Reading: 4.5
EOSINOPHILS and EOSINOPHIL COUNT
Eosinophils are used by the body to protect against allergic reactions and parasites.
Therefore, elevated levels may indicate an allergic response. A low count is normal.
Normal Adult Range: 0 - 5 %
Optimal Adult Reading: 2.5
BASOPHILS and BASOPHIL COUNT
Basophilic activity is not fully understood but it is known to carry histamine, heparin and
serotonin. High levels are found in allergic reactions, low levels are normal.
Normal Adult Range: 0 - 2 %
Optimal Adult Reading: 1
Thyroid
THYROXINE (T4)
T3-UPTAKE
FREE T4 INDEX (T7)
THYROID-STIMULATING HORMONE (TSH)
THYROXINE (T4)
Thyroxine is the thyroid hormone that contains four atoms of iodine. It is used to evaluate
thyroid function. It is the direct measurement of total T4 concentration in the blood serum.
Increased levels are found in hyperthyroidism, acute thyroiditis, and hepatitis. Low levels can
be found in Cretinism, hypothyroidism, cirrhosis, malnutrition, and chronic thyroiditis.
Normal Adult Range: 4 - 12 ug/dl
Optimal Adult Reading: 8 ug/dl
T3-UPTAKE
This test is an indirect measurement of unsaturated thyroxine binding globulin in the blood.
Increased levels are found in hyperthyroidism, severe liver disease, metastatic malignancy,
and pulmonary insufficiency. Decreased levels are found in hypothyroidism, normal
pregnancy, and hyperestrogenis status.
Normal Adult Range: 27 - 47%
Optimal Adult Reading: 37 %
FREE T4 INDEX (T7)
This index is a calculation used to correct the estimated total thyroxine for the amount of
thyroxine binding globulin present. It uses the T4 value and the T3 uptake ratio.
Normal Adult Range: 4 - 12
Optimal Adult Reading: 8
THYROID-STIMULATING HORMONE (TSH)
TSH, produced by the anterior pituitary gland, causes the release and distribution of stored
thyroid hormones. When T4 and T3 are too high, TSH secretion decreases, when T4 and T3
are low, TSH secretion increases.
Normal Adult Range: .5 - 6 miliIU/L
Optimal Adult Reading: 3.25 miliU/L
Other
GLUCOSE (Fasting)
IRON, TOTAL
GLUCOSE (Fasting)
Glucose, formed by the digestion of carbohydrates and the conversion of glycogen by the
liver is the primary source of energy for most cells. It is regulated by insulin, glucagon, thyroid
hormone, liver enzymes and adrenal hormones. It is elevated in diabetes, liver disease,
obesity, pancreatitis, steroids, stress, or diet. Low levels may be indicative of liver disease,
overproduction of insulin, hypothyroidism, or alcoholism.
Normal Adult Range: 60 - 115 mg/dl
Optimal Adult Reading: 87.5
IRON, TOTAL
Iron is necessary for the formation of some proteins, hemoglobin, myoglobin, and
cytochrome. Also it is necessary for oxygen transport, cellular respiration and peroxide
deactivation. Low levels are seen in many anemias, copper deficiencies, low vitamin C intake,
liver disease, chronic infections, high calcium intake and women with heavy menstrual flows.
High levels are seen in hemochromitosis, liver damage, pernicious anemia and hemolytic
anemia.
Normal Adult Range: 30 - 170 mcg/dl
Optimal Adult Reading: 100
Common Laboratory Tests in Liver Diseases
Howard J. Worman, M. D.
ALT - AST - Alkaline phosphatase - Gamma-glutamyltranspeptidase (GGT) - Bilirubin - Albumin - Prothrombin time
(PT) - Platelet count - Serum protein electrophoresis
The diagnosis of liver diseases depends upon a combination of history, physical examination, laboratory testing and
sometimes radiological studies and biopsy. Only a physician who knows all of these aspects of a specific case can
reliably make a diagnosis. Many individuals with liver diseases nonetheless have questions about their laboratory test
results and seek information about their significance. The purpose of this page is to briefly describe some of the
common laboratory tests that may be abnormal in individuals with liver diseases. Patients reading this page must keep
in mind that abnormalities of these laboratory tests are not diagnostic of specific diseases and that only a qualified
physician who knows the entire case can provide a reliable diagnosis.
Alanine aminotransferase (ALT)
ALT is an enzyme produced in hepatocytes, the major cell type in the liver. ALT is often inaccurately referred to as a
liver function test, however, its level in the blood tells little about the function of the liver. The level of ALT in the blood
(actually enzyme activity is measured in the clinical laboratory) is increased in conditions in which hepatocytes are
damaged or die. As cells are damaged, ALT leaks out into the bloodstream. All types of hepatitis (viral, alcoholic,
drug-induced, etc.) cause hepatocyte damage that can lead to elevations in the serum ALT activity. The ALT level is
also increased in cases of liver cell death resulting from other causes, such as shock or drug toxicity. The level of ALT
may correlate roughly with the degree of cell death or inflammation, however, this is not always the case. An accurate
estimate of inflammatory activity or the amount cell death can only be made by liver biopsy. (See also aspartate
aminotransferase below.)
Aspartate aminotransferase (AST)
AST is an enzyme similar to ALT (see above) but less specific for liver disease as it is also produced in muscle and
can be elevated in other conditions (for example, early in the course of a heart attack). AST is also inaccurately
referred to as a liver function test by many physicians. In many cases of liver inflammation, the ALT and AST activities
are elevated roughly in a 1:1 ratio. In some conditions, such as alcoholic hepatitis or shock liver, the elevation in the
serum AST level may higher than the elevation in the serum ALT level.
Alkaline phosphatase
Alkaline phosphatase is an enzyme, or more precisely a family of related enzymes, produced in the bile ducts,
intestine, kidney, placenta and bone. An elevation in the level of serum alkaline phosphatase (actually enzyme activity
is measured in the clinical laboratory), especially in the setting of normal or only modestly elevated ALT and AST
activities, suggests disease of the bile ducts. Serum alkaline phosphatase activity can be markedly elevated in bile
duct obstruction or in bile duct diseases such as primary biliary cirrhosis or primary sclerosing cholangitis. Alkaline
phosphatase is also produced in bone and blood activity can also be increased in some bone disorders.
Gamma-glutamyltranspeptidase (GGT)
An enzyme produced in the bile ducts that, like alkaline phosphatase, may be elevated in the serum of patients with
bile duct diseases. Elevations in serum GGT, especially along with elevations in alkaline phosphatase, suggest bile
duct disease. Measurement of GGT is an extremely sensitive test, however, and it may be elevated in virtually any
liver disease and even sometimes in normal individuals. GGT is also induced by many drugs, including alcohol, and its
serum activity may be increased in heavy drinkers even in the absence of liver damage or inflammation.
Bilirubin
Bilirubin is the major breakdown product that results from the destruction of old red blood cells (as well as some other
sources). It is removed from the blood by the liver, chemically modified by a process call conjugation, secreted into the
bile, passed into the intestine and to some extent reabsorbed from the intestine. Bilirubin concentrations are elevated
in the blood either by increased production, decreased uptake by the liver, decreased conjugation, decreased
secretion from the liver or blockage of the bile ducts. In cases of increased production, decreased liver uptake or
decreased conjugation, the unconjugated or so-called indirect bilirubin will be primarily elevated. In cases of
decreased secretion from the liver or bile duct obstruction, the conjugated or so-called direct bilirubin will be primarily
elevated. Many different liver diseases, as well as conditions other than liver diseases (e. g. increased production by
enhanced red blood cell destruction), can cause the serum bilirubin concentration to be elevated. Most adult acquired
liver diseases cause impairment in bilirubin secretion from liver cells that cause the direct bilirubin to be elevated in the
blood. In chronic, acquired liver diseases, the serum bilirubin concentration is usually normal until a significant amount
of liver damage has occurred and cirrhosis is present. In acute liver disease, the bilirubin is usually increased relative
to the severity of the acute process. In bile duct obstruction, or diseases of the bile ducts such as primary biliary
cirrhosis or sclerosing cholangitis, the alkaline phosphatase and GGT activities are often elevated along with the direct
bilirubin concentration.
Albumin
Albumin is the major protein that circulates in the bloodstream. Albumin is synthesized by the liver and secreted into
the blood. Low serum albumin concentrations indicate poor liver function. The serum albumin concentration is usually
normal in chronic liver diseases until cirrhosis and significant liver damage is present. Albumin levels can be low in
conditions other than liver diseases including malnutrition, some kidney diseases and other rarer conditions.
Prothrombin time (PT)
Many factors necessary for blood clotting are made in the liver. When liver function is severely abnormal, their
synthesis and secretion into the blood is decreased. The prothrombin time is a type of blood clotting test performed in
the laboratory and it is prolonged when the blood concentrations of some of the clotting factors made by the liver are
low. In chronic liver diseases, the prothrombin time is usually not elevated until cirrhosis is present and the liver
damage is fairly significant. In acute liver diseases, the prothrombin time can be prolonged with severe liver damage
and return to normal as the patient recovers. Prothrombin time can also be prolonged in cases of vitamin K deficiency,
by drugs (warfarin, used therapeutically as an anti-coagulant, prolongs the prothrombin time) and in non-liver
disorders.
Platelet count
Platelets are the smallest of the blood cells (actually fragments of larger cells known as megakaryocytes) that are
involved in clotting. In some individuals with liver disease, the spleen becomes enlarged as blood flow through the
liver is impeded. This can lead to platelets being sequestered in the enlarged spleen. In chronic liver diseases, the
platelet count usually falls only after cirrhosis has developed. The platelet count can be abnormal in many conditions
other than liver diseases.
Serum protein electrophoresis
In this test, the major proteins in the serum are separated in an electric field and their concentrations determined. The
four major types of serum proteins whose concentrations are measured in this test are albumin, alpha-globulins, beta-
globulins and gamma-globulins. Serum protein electrophoresis is a useful test in patients with liver diseases as it can
provide clues to several diagnostic possibilities. In cirrhosis, the albumin may be decreased (see above) and the
gamma-globulin elevated. Gamma-globulin can be significantly elevated in some types of autoimmune hepatitis. The
alpha-globulins can be low in alpha-1-antitrypsin deficiency.
Вам также может понравиться
- Understanding Blood TestДокумент19 страницUnderstanding Blood TestRueth AnnafeyeОценок пока нет
- Blood Test Results ExplainedДокумент5 страницBlood Test Results ExplainedAhmed Tolba0% (1)
- Hyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Blood Test PresentationДокумент129 страницBlood Test Presentationනුවන් චමීර ගුණවර්ධනОценок пока нет
- How To Interpret Your Blood Test ResultsДокумент23 страницыHow To Interpret Your Blood Test Resultstin1625100% (1)
- Blood Results in Clinical Practice: A practical guide to interpreting blood test resultsОт EverandBlood Results in Clinical Practice: A practical guide to interpreting blood test resultsОценок пока нет
- Lab Literacy for Doctors: A Guide to Ordering the Right Tests for Better Patient CareОт EverandLab Literacy for Doctors: A Guide to Ordering the Right Tests for Better Patient CareРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Diabetes Mellitus Type 3c, (Pancreatogenic Diabetes) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandDiabetes Mellitus Type 3c, (Pancreatogenic Diabetes) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Know Your Blood, Know Your Health: Prevent Disease and Enjoy Vibrant Health through Functional Blood Chemistry AnalysisОт EverandKnow Your Blood, Know Your Health: Prevent Disease and Enjoy Vibrant Health through Functional Blood Chemistry AnalysisРейтинг: 2.5 из 5 звезд2.5/5 (3)
- Essential Blood Test Reference SheetДокумент1 страницаEssential Blood Test Reference Sheetd3nny89Оценок пока нет
- Respiratory System: A Tutorial Study GuideОт EverandRespiratory System: A Tutorial Study GuideРейтинг: 5 из 5 звезд5/5 (1)
- Lab Values: An Easy Guide to Learn Everything You Need to Know About Laboratory Medicine and Its Relevance in Diagnosing DiseaseОт EverandLab Values: An Easy Guide to Learn Everything You Need to Know About Laboratory Medicine and Its Relevance in Diagnosing DiseaseРейтинг: 5 из 5 звезд5/5 (2)
- Coughing, A Simple Guide to The Condition, Treatment and Related ConditionsОт EverandCoughing, A Simple Guide to The Condition, Treatment and Related ConditionsОценок пока нет
- Diabetic Nephropathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandDiabetic Nephropathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- AnaemiaДокумент27 страницAnaemiaSamahir F HusseinОценок пока нет
- Lab Values WorksheetДокумент57 страницLab Values WorksheetpcbthyОценок пока нет
- Commonly Used Lab Values at A Glance Chem 7 1Документ9 страницCommonly Used Lab Values at A Glance Chem 7 1annatw100% (10)
- Dictionary of Blood TestsДокумент6 страницDictionary of Blood Teststvland1098Оценок пока нет
- Laboratory Diagnostics of (Selected) Endocrine DisordersДокумент48 страницLaboratory Diagnostics of (Selected) Endocrine DisordersPaulina PaskeviciuteОценок пока нет
- Blood Test and Normal RangeДокумент40 страницBlood Test and Normal Rangeethirukumaran0% (1)
- Interpret Liver TestsДокумент4 страницыInterpret Liver TestsKaram Ali ShahОценок пока нет
- Pituitary Disorders - Adrenal Disorders - Thyroid DiseasesДокумент207 страницPituitary Disorders - Adrenal Disorders - Thyroid Diseasesnurliah armandОценок пока нет
- Making The Right Dental-ChoiceДокумент16 страницMaking The Right Dental-ChoiceNo Boundaries100% (1)
- Home Remedies For High Blood Pressure - Treatment & Cure - Natural Remedy For High Blood Pressure - High Blood Pressure DietДокумент8 страницHome Remedies For High Blood Pressure - Treatment & Cure - Natural Remedy For High Blood Pressure - High Blood Pressure DietRama PrajapatiОценок пока нет
- Rotine Stool AnalysisДокумент93 страницыRotine Stool AnalysisMaath KhalidОценок пока нет
- Pathophysiology of EndocrinologyДокумент25 страницPathophysiology of EndocrinologyISRAELОценок пока нет
- NAC - Are You Ready For NACДокумент4 страницыNAC - Are You Ready For NACVickiОценок пока нет
- Laboratory Data InterpretationДокумент24 страницыLaboratory Data InterpretationDanish KamalОценок пока нет
- ENDOCRINE SYSTEM OverviewДокумент39 страницENDOCRINE SYSTEM OverviewAnn M. Hinnen Sparks50% (2)
- Renal EmergenciesДокумент11 страницRenal EmergenciesDemuel Dee L. BertoОценок пока нет
- Blood ChemistryДокумент3 страницыBlood ChemistryHal Theodore Maranian BallotaОценок пока нет
- ValuesДокумент19 страницValuescabrerahazel100% (1)
- Summary - Blood Chemistry TestsДокумент38 страницSummary - Blood Chemistry TestspayatingОценок пока нет
- Endocrinology Endocrine System Review SheetДокумент6 страницEndocrinology Endocrine System Review SheetRazvan SerbanОценок пока нет
- Medical MnemonicsДокумент3 страницыMedical Mnemonicsle chix100% (1)
- Increasing Paltelet Blood CountsДокумент8 страницIncreasing Paltelet Blood CountssrkmОценок пока нет
- Critical Lab ValuesДокумент1 страницаCritical Lab ValuesCrystal GlassОценок пока нет
- Microbiology For Dummies Cheat Sheet - For DummiesДокумент3 страницыMicrobiology For Dummies Cheat Sheet - For DummiesSkylarОценок пока нет
- Lab Result Chart With Normal Range, Purpose, Reason For High/low Results (Nursing)Документ5 страницLab Result Chart With Normal Range, Purpose, Reason For High/low Results (Nursing)Linsey Bowen100% (6)
- Med Geeks Clinical Lab GuideДокумент17 страницMed Geeks Clinical Lab GuideHuy Hoang100% (1)
- Phlebotomy Procedure 3rd PDFДокумент4 страницыPhlebotomy Procedure 3rd PDFFranciska Gledy AmbaritaОценок пока нет
- Approach in MiscellaneousДокумент12 страницApproach in MiscellaneousRapid MedicineОценок пока нет
- 22 - Proteinuria and HematuriaДокумент73 страницы22 - Proteinuria and HematuriaArsalan NadeemОценок пока нет
- The Concept of Swapna (Dream) in Ayurveda - A Literary ReviewДокумент11 страницThe Concept of Swapna (Dream) in Ayurveda - A Literary ReviewSamhitha Ayurvedic ChennaiОценок пока нет
- Abdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixДокумент5 страницAbdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixRemelou Garchitorena AlfelorОценок пока нет
- Clinical KardexДокумент2 страницыClinical KardexJackie Frey100% (2)
- 63 Lab ValuesДокумент4 страницы63 Lab ValuesYemaya84Оценок пока нет
- Nursing Patho CardsДокумент195 страницNursing Patho Cardsgiogmail100% (1)
- Normal Lab ValuesДокумент5 страницNormal Lab ValuesNadiya Elfira BilqisОценок пока нет
- Abg Made EasyДокумент24 страницыAbg Made EasynbvillarazoОценок пока нет
- Liver Function Testing PDFДокумент2 страницыLiver Function Testing PDFRajesh KumarОценок пока нет
- Blood Test Normal ValuesДокумент11 страницBlood Test Normal Valueschristophe1967Оценок пока нет
- Clinical PathologyДокумент42 страницыClinical PathologyRathinaKumarОценок пока нет
- Chapter 3: Lymphatic SystemДокумент22 страницыChapter 3: Lymphatic Systemfatin harrisОценок пока нет
- Blood TestsДокумент10 страницBlood TestsMay Mawzi WahabОценок пока нет
- Homeopathic Tips and TechniqueДокумент8 страницHomeopathic Tips and TechniqueFarasat KhanОценок пока нет
- Liver Function TestДокумент18 страницLiver Function TestMuhammad Waqas MunirОценок пока нет
- Blood Test Reference Range Chart Test Reference Range (Conventional Units )Документ3 страницыBlood Test Reference Range Chart Test Reference Range (Conventional Units )QaSeh ISnaОценок пока нет
- Mazo Riascos Review of Systems ChecklistДокумент1 страницаMazo Riascos Review of Systems Checklistammen17Оценок пока нет
- Liver Function TestДокумент5 страницLiver Function TestAnne Sison100% (1)
- A Color at Pinkie PieДокумент1 страницаA Color at Pinkie Pieclea1Оценок пока нет
- What Is A Reflective Journal?Документ4 страницыWhat Is A Reflective Journal?solo_gauravОценок пока нет
- BUSINESS Curriculum An 1Документ6 страницBUSINESS Curriculum An 1clea1Оценок пока нет
- What Is A Reflective Journal?Документ4 страницыWhat Is A Reflective Journal?solo_gauravОценок пока нет
- QuestionДокумент2 страницыQuestionclea140% (5)
- What Is A Reflective Journal?Документ4 страницыWhat Is A Reflective Journal?solo_gauravОценок пока нет
- Put A Ruffle On ItДокумент29 страницPut A Ruffle On Itclea1Оценок пока нет
- Service Chesterfield - Danesmoor 51: Monday - Friday (Not Bank Holidays)Документ10 страницService Chesterfield - Danesmoor 51: Monday - Friday (Not Bank Holidays)clea1Оценок пока нет
- QuestionДокумент4 страницыQuestionclea17% (15)
- SimplepastexercisesДокумент3 страницыSimplepastexercisesPetrache Valentina RoxanaОценок пока нет
- 54 TimetableДокумент9 страниц54 Timetableclea1Оценок пока нет
- Dot To Dot Zoo 6Документ1 страницаDot To Dot Zoo 6clea1Оценок пока нет
- Kalanchoe CareДокумент3 страницыKalanchoe Caresfantu_29Оценок пока нет
- A Magazine For European Collaboration: Theme: Friendship and Collaboration Across EuropeДокумент2 страницыA Magazine For European Collaboration: Theme: Friendship and Collaboration Across Europeclea1Оценок пока нет
- Keeping A Reader's Journal: © 2002 WWW - Teachit.co - Uk Readjrnl Page 1 of 1Документ0 страницKeeping A Reader's Journal: © 2002 WWW - Teachit.co - Uk Readjrnl Page 1 of 1clea1Оценок пока нет
- Lot de ConstructiiДокумент3 страницыLot de Constructiiclea1Оценок пока нет
- ModeleДокумент54 страницыModeleclea1Оценок пока нет
- Activity: Read The Information and Draw The Picture. Start in The Middle of The PaperДокумент1 страницаActivity: Read The Information and Draw The Picture. Start in The Middle of The Paperclea1Оценок пока нет
- Do You Know These Popular Stories?Документ1 страницаDo You Know These Popular Stories?clea1Оценок пока нет
- Proiecte DiyДокумент91 страницаProiecte Diyclea1Оценок пока нет
- Photoc 2 Unt 1 Les 6Документ2 страницыPhotoc 2 Unt 1 Les 6clea1Оценок пока нет
- Unit 1: What's Missing? Draw. Then Colour.: Colouring & Activity Book © Express Publishing PHOTOCOPIABLE 1Документ4 страницыUnit 1: What's Missing? Draw. Then Colour.: Colouring & Activity Book © Express Publishing PHOTOCOPIABLE 1clea1Оценок пока нет
- Fisa EnglezaaaaaaДокумент5 страницFisa Englezaaaaaaclea1Оценок пока нет
- Plans A Color at ApplejackДокумент1 страницаPlans A Color at Applejackclea1Оценок пока нет
- Cotton Classic Stitch Sample Pullover: To Obtain GaugeДокумент3 страницыCotton Classic Stitch Sample Pullover: To Obtain Gaugeclea1Оценок пока нет
- 633668860142495000Документ84 страницы633668860142495000clea1Оценок пока нет
- Planificare Optional - Limba Engleza Grupa Pregatitoare The First SemesterДокумент5 страницPlanificare Optional - Limba Engleza Grupa Pregatitoare The First Semesterclea1Оценок пока нет
- Tnspectoratul $colar Al Muntctptulut Bucure$Ti Oltmptada Creattv - Ta Til 201 2 Etapa Pe Sector - Clasa A Vilt-A-VlДокумент3 страницыTnspectoratul $colar Al Muntctptulut Bucure$Ti Oltmptada Creattv - Ta Til 201 2 Etapa Pe Sector - Clasa A Vilt-A-Vlclea1Оценок пока нет
- The Medieval Horse: Coloring BookДокумент50 страницThe Medieval Horse: Coloring Bookclea1Оценок пока нет
- Fuzzy Expert System For The Diagnosis of Common Liver DiseaseДокумент7 страницFuzzy Expert System For The Diagnosis of Common Liver Diseasetusharrsangole100% (1)
- Heme Breakdown, JAUNDICE & LFTДокумент58 страницHeme Breakdown, JAUNDICE & LFTnirmalramyaОценок пока нет
- T. Akahoshi H. Sugimori N. Kaku K. Tokuda T. Nagata E. Noda M. Morita M. Hashizume Y. MaeharaДокумент8 страницT. Akahoshi H. Sugimori N. Kaku K. Tokuda T. Nagata E. Noda M. Morita M. Hashizume Y. Maeharadr. Ayu Nabila Kusuma PradanaОценок пока нет
- Us Chughtais Lab Rate ListДокумент2 страницыUs Chughtais Lab Rate Listapi-525272944Оценок пока нет
- SGPT (Serum Glutamic-Pyruvic Transaminase), ALT (Alanine Aminotransferase), InterpretationsДокумент55 страницSGPT (Serum Glutamic-Pyruvic Transaminase), ALT (Alanine Aminotransferase), InterpretationsReman A. AlingasaОценок пока нет
- Case History and Data Interpretation in Medical Practice, 3e (January 31, 2015) - (9351523756) - (Jaypee Brothers Medical Pub)Документ492 страницыCase History and Data Interpretation in Medical Practice, 3e (January 31, 2015) - (9351523756) - (Jaypee Brothers Medical Pub)Khan100% (3)
- Physiology of The Liver and Biliary System M.GДокумент54 страницыPhysiology of The Liver and Biliary System M.GTsega WesenОценок пока нет
- Nieuw 3Документ12 страницNieuw 3Jasmijn AlmuliОценок пока нет
- Sir Yahaya Memorial Hospital Birnin Kebbi: Nursing DepartmentДокумент7 страницSir Yahaya Memorial Hospital Birnin Kebbi: Nursing DepartmentyusufОценок пока нет
- Clinical Enzymology: Enzyme Classification and NomenclatureДокумент27 страницClinical Enzymology: Enzyme Classification and NomenclaturePatrick DazaОценок пока нет
- (CC2 Lec Modules) L1-L4Документ37 страниц(CC2 Lec Modules) L1-L4Kyla CastilloОценок пока нет
- RDF-Purchase Request Form - For Medicine: S.N. Item Description Unit Remark Quantity RequestedДокумент48 страницRDF-Purchase Request Form - For Medicine: S.N. Item Description Unit Remark Quantity Requestedbirhane gebreegziabiher67% (3)
- Understanding Lab Values : InstructionsДокумент9 страницUnderstanding Lab Values : InstructionssinnetrbОценок пока нет
- Quick Reference Guide: SGPT (Alat) KitДокумент1 страницаQuick Reference Guide: SGPT (Alat) KitDharmesh PatelОценок пока нет
- Purpose: Alanine AminotransferaseДокумент3 страницыPurpose: Alanine AminotransferaseRona PieОценок пока нет
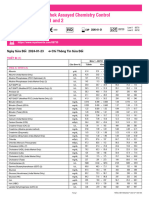
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Ngày Sửa Đổi 2024-01-23 Chỉ Thông Tin Sửa ĐổiДокумент2 страницыLyphochek Assayed Chemistry Control Levels 1 and 2: Ngày Sửa Đổi 2024-01-23 Chỉ Thông Tin Sửa ĐổiquankddОценок пока нет
- ENZYMES OF CLINICAL IMPORTANCE ChapterДокумент18 страницENZYMES OF CLINICAL IMPORTANCE ChapterKeerthy VasanОценок пока нет
- Medical Test ReportДокумент10 страницMedical Test ReportPadmaraj NairОценок пока нет
- AlexJPediatr313112-658022 014940Документ8 страницAlexJPediatr313112-658022 014940justmokhtarОценок пока нет
- Mindray BS380 User ManualДокумент8 страницMindray BS380 User ManualMichael Okeke100% (2)
- Sepsis Notes Amended On 24th Feb 2019Документ31 страницаSepsis Notes Amended On 24th Feb 2019Ereny66Оценок пока нет
- The SGOT/SGPT Ratio - An Indicator of Alcoholic Liver DiseaseДокумент4 страницыThe SGOT/SGPT Ratio - An Indicator of Alcoholic Liver DiseaseSahara MaindokaОценок пока нет
- Hospitalization PolicyДокумент33 страницыHospitalization PolicySudheer ChОценок пока нет
- Beacon Control Norm & Path (LP10-007)Документ2 страницыBeacon Control Norm & Path (LP10-007)psychejaneОценок пока нет
- Acute Liver Injury and FailureДокумент14 страницAcute Liver Injury and FailureWeslei ChaconОценок пока нет
- Cariprazine PDFДокумент162 страницыCariprazine PDFige zaharaОценок пока нет
- First Aid For The USMLE Step1 2023Документ849 страницFirst Aid For The USMLE Step1 2023Nawal Phongtiko95% (19)
- Risky Drinking and Alcohol Use Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateДокумент20 страницRisky Drinking and Alcohol Use Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateGoddness leeОценок пока нет
- Cardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101Документ26 страницCardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101bagasОценок пока нет
- PranithaДокумент15 страницPranithaKumar VijayОценок пока нет