Академический Документы
Профессиональный Документы
Культура Документы
Kastarinen HT Mott
Загружено:
Preha Prehaningrum0 оценок0% нашли этот документ полезным (0 голосов)
10 просмотров8 страницjurnal
Оригинальное название
Kastarinen Ht Mott
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документjurnal
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
10 просмотров8 страницKastarinen HT Mott
Загружено:
Preha Prehaningrumjurnal
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
Non-pharmacological treatment of hypertension in primary
health care: a 2-year open randomized controlled trial of
lifestyle intervention against hypertension in eastern Finland
Mika J. Kastarinen
a
, Pekka M. Puska
b
, Maarit H. Korhonen
c
,
Juha N. Mustonen
d
, Veikko V. Salomaa
e
, Jouko E. Sundvall
f
,
Jaakko O. Tuomilehto
e,g
, Matti I. Uusitupa
c
and Aulikki M. Nissinen
e
for the LIHEF Study Group
Objective To assess whether lifestyle counselling is
effective in non-pharmacological treatment of
hypertension in primary health care.
Design Open randomized controlled trial.
Setting Ten municipal primary health care centres in
eastern Finland.
Patients Seven hundred and fteen subjects aged 2574
years with systolic blood pressure 140179 mmHg and/or
diastolic blood pressure 90109 mmHg or
antihypertensive drug treatment.
Interventions Systematic health counselling given by local
public health nurses for 2 years.
Main outcome measures Blood pressure, lipids and
lifestyle data were collected annually.
Results Among participants with no antihypertensive drug
treatment, the net reductions after 1 year both in systolic
blood pressure [22.6 mmHg; 95% condence interval (CI),
24.7 to 20.5 mmHg] and in diastolic blood pressure
(22.7 mmHg; 95% CI, 24.0 to 21.4 mmHg) were
signicant in favour of the intervention group. This
difference in blood pressure change was maintained
during the second year. In participants with
antihypertensive drug treatment, no signicant difference
in blood pressure reduction was seen between the groups
during the study.
Conclusions A relatively modest, but systematic
counselling in primary health care can, at least among
untreated hypertensive subjects, produce reductions in
blood pressure levels that are modest for the individual,
but very important from the public health point of view.
J Hypertens 20:25052512 & 2002 Lippincott Williams &
Wilkins.
Journal of Hypertension 2002, 20:25052512
Keywords: hypertension, randomized controlled trial, life change events
a
Department of Public Health and General Practice, University of Kuopio, Kuopio,
Finland,
b
Department of Non-communicable Disease Prevention and Health
Promotion, WHO, Geneva, Switzerland,
c
Department of Clinical Nutrition,
University of Kuopio, Kuopio, Finland,
d
Department of Internal Medicine, North
Karelia Central Hospital, Joensuu, Finland,
e
Department of Epidemiology and
Health Promotion, National Public Health Institute, Helsinki, Finland,
f
Department of Health and Functional Capacity, National Public Health Institute,
Helsinki, Finland and
g
Department of Public Health, University of Helsinki,
Finland.
Sponsorship: This study has been supported by the grants from the following
institutions: the Social Insurance Institution of Finland, the Juho Vainio
Foundation, the National Public Health Institute, the Finnish Ofce for Health
Care Technology Assessment, the Graduate School of Public Health in the
University of Kuopio, the Finnish Foundation for Cardiovascular Research, the
North Savo Regional Fund of the Finnish Cultural Foundation, the Duodecim
Society, the Aarne and Aili Turunen Foundation, the Ida Montin Foundation and
the EVO Funding from the Kuopio University Hospital.
Correspondence and request for reprints to Mika Kastarinen, MD, Department of
Public Health and General Practice, University of Kuopio, PB 1627, 70211
Kuopio, Finland.
Tel: +358-17-162912; fax: +358-17-162937; e-mail: mika.kastarinen@uku.
Received 23 May 2002 Revised 26 July 2002
Accepted 21 August 2002
Introduction
Evidence indicates that lifestyle measures such as
weight reduction, moderation of alcohol consumption,
reduction in salt intake and increase in physical
activity are feasible and effective in lowering blood
pressure (BP), either alone or in combination with
antihypertensive drug therapy [16]. Some studies
have suggested that fat-modication of the diet or a
diet with low saturated fat intake, but rich in fruits,
vegetables and bre, have a signicant BP-lowering
effect [4,7]. In addition to its effect on BP, such
modication of lifestyle can also reduce the levels of
other cardiovascular risk factors. According to the
latest international and national hypertension guide-
lines, non-pharmacological measures are recommended
as the rst-line therapy for the patients with newly
diagnosed, uncomplicated hypertension and they
should also be applied in the treatment of every
Original article 2505
0263-6352 & 2002 Lippincott Williams & Wilkins 10.1097/01.hjh.0000042893.24999.db
hypertensive patient treated with antihypertensive
drugs [810].
Most of the clinical trials assessing the feasibility and
effects of health education targeted to the prevention
and control of hypertension have been performed in
academic study centres by expert personnel trained for
the trial. Because these studies were mainly designed
to test the efcacy of such interventions, the interven-
tion programmes have been intensive. Due to the
limited resources of the public health sector, the
implementation of such intensive lifestyle modication
programmes in primary health care, i.e. in the setting
where most of the hypertensive patients are treated,
would be difcult. Therefore, we decided to conduct a
randomized, controlled trial to assess the efcacy of a
relatively low-intensity patient-counselling programme
planned for hypertensive subjects in primary health
care.
Methods
Participants and randomization
The Lifestyle Intervention against Hypertension in
Eastern Finland (LIHEF) study was conducted in 10
municipal primary health care centres in eastern Fin-
land, mainly in the province of North Karelia. Eight of
the health care centres were located in rural municipa-
lities with 300012 000 inhabitants and two in the
towns with 50 000 and 90 000 inhabitants (51% of all
participants). The study protocol was approved by the
Ethics Committee of the Kuopio University Hospital.
The study participants were enrolled between February
1996 and June 1997. Eligible subjects were men and
women aged 2574 years with systolic blood pressure
(SBP) 140179 mmHg and/or diastolic blood pressure
(DBP) 90109 mmHg or on antihypertensive drug
therapy. Exclusion criteria included secondary hyper-
tension, mental or physical illness serious enough to
potentially inuence the compliance with the study
procedures, alcoholism, type 1 diabetes, current or
planned pregnancy and history of myocardial infarction
or stroke within the preceding 3 months.
Three screening visits in 1-week intervals were orga-
nized in the health centres to measure the BP of the
subjects not using any antihypertensive drugs. During
each screening visit, BP was measured twice from the
right arm of the subject according to the WHO
MONICA protocol with a standard mercury sphygmo-
manometer [11]. The mean of the BP measurements
performed in the second and third visit (four readings)
was used as the screening BP.
The randomization visit was organized within 30 days
after the third screening visit in a participating health
centre. A written informed consent was obtained from
every eligible person agreeing to participate, after
which they were randomized to receive intervention or
usual care by the same study physician using a dice
(odd numbers intervention group; even numbers
control group). Of the 813 subjects originally eligible
for the study, 715 were eventually assigned to the
intervention group or to the usual care group.
Measurements
Blood pressure, weight, waist and hip circumferences
were measured annually from every participant. Height
was measured at the baseline only. Body mass index
(BMI) was calculated as kg/m
2
. During the annual
visits, BP was measured twice using the same method
as during the screening and the mean was used in the
analyses. A single trained study nurse, who was blinded
to the treatment assignment, performed most of the BP
and anthropometrical measurements during the screen-
ing and the follow-up. Only in one health centre with
176 participants, another trained study nurse carried out
the measurements during the screening and randomiza-
tion visits.
Information on socio-economic status, medical history,
smoking, alcohol use, physical activity and daily medi-
cation were collected annually using questionnaires
with standard questions. A 4-day food record was
collected for the annual visits. The detailed information
of the dietary analyses used in the study will be
published elsewhere [12].
All biochemical assays were performed at the Depart-
ment of Biochemistry of the National Public Health
Institute in Helsinki. Blood samples were drawn at the
participating health centres from the study subjects
after 12-h fasting. Serum total and high-density lipopro-
tein (HDL) cholesterol, triglycerides and insulin were
determined. Low-density lipoprotein (LDL) cholesterol
concentrations were calculated using Friedewalds for-
mula [13]. Twenty-four-hour urine specimens were
collected for the determination of the 24-h potassium
and sodium excretion.
Intervention
The intervention goals for the study subjects were: (1)
normal weight (BMI , 25 kg/m
2
); (2) daily sodium
chloride intake less than 5 g; (3) alcohol consumption
fewer than two drinks per day; (4) to exercise at
moderate intensity at least three times per week for
30 min; and (5) to stop smoking, if a smoker.
The study physician and a nutritionist trained the local
public health nurses who participated in the study. The
training sessions dealt with simple counselling and
behaviour modication methods targeting weight re-
duction, reduction in salt, alcohol and saturated fat
consumption, as well as an increase in leisure-time
physical activity. The nurses were given a folder with
2506 Journal of Hypertension 2002, Vol 20 No 12
detailed information of the dietary recommendations
and with practical tips to achieve these recommenda-
tions in everyday life.
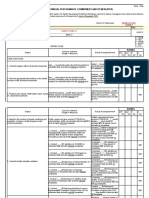
The core of the actual intervention (Fig. 1) consisted of
four visits by the participants to local public health
nurses during the rst year of the follow-up (1, 3, 6 and
9 months after randomization), and of three visits
during the second year (15, 18 and 21 months after the
randomization). At these visits, the participants were
systematically instructed to change their health behav-
iour primarily on the basis of their individual situation.
At each visit, BP and weight were measured, and the
values, as well as the changes in lifestyle factors to be
reached before the next study visit, were written down
using a special follow-up card designed for the study. A
written feedback of the 4-day food record was sent to
the public health nurse to support the intervention. In
addition, a 2-h group session was organized for the
intervention group in every health care centre at 6 and
18 months after the randomization. These two group
meetings concentrated mainly on advice targeting re-
duction of salt intake and overweight. During the 2-
year follow-up, the participants in the usual care group
were instructed to visit their own physicians and public
health nurses according to usual practices.
Statistical analyses
Statistical analyses were conducted with SPSS for
Windows version 10.0 (SPSS Inc., Chicago, Illinois,
USA). For continuous variables, the t-test was used to
test the differences and changes in mean values be-
tween the groups. Condence intervals (CI) for the
differences in proportions were calculated using a
special software package [14]. An intention-to-treat-
analysis was used, i.e. all subjects assigned to interven-
tion or usual care were included in the analysis. In the
case of missing responses, the last observed response
was used when calculating the 1- and 2-year changes in
continuous variables (the carry-forward method). The
same method was used with dichotomous variables. In
a separate analysis of BP changes in subjects without
previous antihypertensive drug treatment, the last BP
measurement without antihypertensive drug treatment
was used if drug treatment was initiated during the
trial. Accordingly, in subjects already on antihyperten-
sive medication, the last BP measurement with anti-
hypertensive drug treatment was used if the treatment
was discontinued during the trial. In the calculations of
BP changes, the changes in doses of antihypertensive
medication were not taken into account. Multiple linear
regression analysis was used to examine the associations
of changes in body weight, sodium and potassium
excretion, alcohol intake and leisure-time physical
activity (times/week) with the changes in BP, control-
ling for the baseline BP levels.
The original target sample size was 800 subjects, which
Follow-up,
Months
Randomisation
Measurements
at baseline,
12 months and
24 months:
PN, FFR
PN
PN,
GM
PN
FFR
PN PN,
GM
PN
Intervention
0 1 3 6 9 12 15 18 21 24
Usual care*
BP
Weight
Height (only at baseline)
Waist
Hip
Total cholesterol
HDL cholesterol
LDL cholesterol
Triglycerides
24-hour urinary sodium excretion
24-hour urinary potassium excretion
Insulin
Questionnaires
4-day Food record
Fig. 1
The design of the study. PN, public health nurse; FFR, feedback from the food record; GM, group meeting.
Usual care group visited their own
public health nurses as usual. BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Non-pharmacological treatment of hypertension Kastarinen et al. 2507
was not reached due to relatively numerous dropouts
before the randomization among the already recruited
subjects. It was estimated that this sample size would
enable detection of a 3.2 mmHg difference in change
of SBP and a 1.6 mmHg difference in change of DBP
between the intervention and usual care groups, with
80% power at the 5% signicance level.
Results
Baseline characteristics and adherence to treatment
The mean age of all participants was 54.3 years. Of the
participants, 52% were on antihypertensive drug treat-
ment at the beginning of the trial (Table 1). There
were no statistically signicant differences between the
groups in any of the baseline variables analysed.
Attendance rates at the 1-year and 2-year study visits
were satisfactory (Fig. 2). The attendance rate at both
group meetings organized for the intervention group
after 6 and 18 months of intervention was 50%. The
subjects who dropped out during the different phases
of the study were, at baseline measurements, signi-
cantly younger (50 versus 55 years) and heavier (83.1
versus 80.1 kg) compared with the attenders of the 2-
year visit. Also, alcohol use (73 versus 42 g/week) and
proportion of smokers (13 versus 7%) were signicantly
higher among the drop-outs at the baseline.
Changes in blood pressure and lifestyle factors
The changes in BP and other continuous variables in
the two groups are shown in Table 2. Without taking
into account the effect of antihypertensive drug treat-
ment, the reduction in DBP during the rst study year
was signicantly greater in the intervention group com-
pared to the usual care group. The reductions in SBP at
1-year follow-up and at 2-year follow-up and in DBP
from baseline to 2 years tended to be greater in the
intervention group, although they did not reach the
Table 1 Baseline characteristics of participants in the intervention and usual care groups. Values are mean
6SD or percentage
Intervention (n 360) Usual care (n 355)
Age (years) 54.4 10.1 54.2 9.9
Female (%) 52 54
Antihypertensive drug treatment (%) 52 53
Current smoker (%) 9 7
History of coronary heart disease (%) 5 3
Moderate physical activity at least three times per week (%) 51 51
Alcohol consumption (g/week) 47 83 48 74
Body weight (kg) 81.1 15.7 80.0 14.8
Body mass index (kg/m
2
) 28.9 4.6 28.5 4.5
Waist circumference (cm) 97.2 13.1 95.8 12.8
Hip circumference (cm) 104.7 10.4 104.1 10.0
Systolic blood pressure (mmHg) 149 16 148 16
No antihypertensive drug treatment 152 14 150 14
Antihypertensive drug treatment 147 18 146 18
Diastolic blood pressure (mmHg) 91 9 91 8
No antihypertensive drug treatment 93 8 93 9
Antihypertensive drug treatment 89 9 89 8
Total cholesterol (mmol/l) 5.66 0.91 5.59 0.93
LDL-cholesterol (mmol/l) 3.64 0.81 3.56 0.79
HDL-cholesterol (mmol/l) 1.32 0.33 1.36 0.38
Triglycerides (mmol/l) 1.56 1.01 1.49 1.00
24-h urinary sodium excretion (mmol) 146 56 142 56
24-h urinary potassium excretion (mmol) 83 27 83 28
Serum insulin (IU/l) 12.2 6.8 11.6 6.3
LDL, low-density lipoprotein; HDL, high-density lipoprotein.
813 eligible subjects after screening
98 declined to participate
715 randomized
Intervention
n 360
Usual care
n 355
Attended 1-year study visit
317/360 (88%)
Attended 1-year study visit
275/355 (77%)
Attended 2-year study visit
304/360 (84%)
Attended 2-year study visit
283/355 (80%)
Fig. 2
The numbers of participants involved throughout the trial.
2508 Journal of Hypertension 2002, Vol 20 No 12
level of statistical signicance. In the subgroup with no
antihypertensive drug treatment, the reductions in both
SBP and DBP were signicantly greater in the inter-
vention group compared with the usual care during
both the rst and the second year of follow-up (Table
3). In subjects with antihypertensive drug treatment at
baseline, the BP reductions were of the same magni-
tude in both groups. In these subjects, the number of
antihypertensive drugs used per patient did not change
signicantly in either of the randomized groups during
the follow-up. In both groups, 70% of the drug-treated
patients were on monotherapy at the end of the study.
Among the subjects with antihypertensive drug treat-
ment, the self-reported frequency of BP measurements
during the previous year decreased signicantly more
in the intervention group during the rst year (net
change 2.3 measurements/year; 95% CI, 4.3 to 0.3;
data not shown). Otherwise the number of BP measure-
ments did not differ signicantly between the groups
during any phase of the study.
The net reductions (intervention versus usual care) in
weight at 1 and 2 years of follow-up were signicant.
Eight per cent of the initially overweight participants
(BMI > 25 kg/m
2
) assigned to intervention had achie-
ved normal weight at the end of the trial, which was
signicantly more than that in the usual care group
(Table 4). Also, the waist and hip circumferences fell
signicantly more in the intervention group than in
usual care throughout the study. The changes in 24-h
urinary sodium and potassium excretion were small,
with no signicant differences between the groups.
Self-reported alcohol consumption fell signicantly
more during the rst study year in the intervention
group, but this difference disappeared during the
second year. Compared to the usual care group, a
signicantly larger proportion of the participants in the
intervention group had increased their physical activity
to the target level at both 1-year and 2-year visits.
The net reduction in weight between the randomized
groups was signicantly greater in subjects with no
antihypertensive drug treatment during the rst year
compared to the group with antihypertensive drug
treatment (1.5 versus 0.8 kg, P for the interaction
Table 2 Changes in continuous variables at 1 and 2 years in the intervention and usual care groups
Change 01 year Change 02 years Difference in change (95% CI) (intervention versus usual care)
Intervention Usual care Intervention Usual care 01 year 02 years
Systolic blood pressure (mmHg) 4.7 3.4 6.2 4.2 1.3 (3.2, 0.6) 2.0 (4.3, 0.3)
Diastolic blood pressure (mmHg) 4.0 2.4 4.3 3.2 1.6 (2.7, 0.6) 1.1 (2.4, 0.2)
Body weight (kg) 1.5 0.2 1.5 0.3 1.3 (1.7, 0.9) 1.2 (1.7, 0.7)
Waist circumference (cm) 1.2 0.3 1.2 0.2 1.5 (2.1, 1.0) 1.4 (2.0, 0.8)
Hip circumfererence (cm) 1.4 0.5 1.4 0.4 0.9 (1.4, 0.4) 0.9 (1.5, 0.4)
Alcohol consumption (g/week) 7 1 7 5 8 (15, 0) 2 (9, 5)
Total cholesterol (mmol/l) 0.05 0.03 0.03 0.07 0.02 (0.11, 0.06) 0.11 (0.20, 0.01)
LDL-cholesterol (mmol/l) 0.06 0.01 0.11 0.04 0.05 (0.12, 0.03) 0.15 (0.23, 0.05)
HDL-cholesterol (mmol/l) 0.02 0.01 0.10 0.07 0.01 (0.01, 0.04) 0.03 (0.00, 0.07)
Triglycerides (mmol/l) 0.03 0.06 0.06 0.06 0.03 (0.05, 0.12) 0.00 (0.09, 0.10)
Urinary sodium excretion (mmol/day) 9 6 7 2 3 (10, 5) 5 (14, 3)
Urinary potassium excretion (mmol/day) 1 1 3 1 0 (4, 4) 2 (2, 5)
Serum insulin (IU/l) 0.8 0.2 1.1 0.5 0.6 (1.2, 0.1) 0.6 (1.1, 0.1)
CI, condence interval; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Table 3 Changes (95% CI in parentheses) in blood pressure levels stratied by antihypertensive drug treatment
status
No antihypertensive drug treatment Antihypertensive drug treatment
Intervention (n 175) Usual care (n 166) Intervention (n 185) Usual care (n 189)
Systolic blood pressure (mmHg)
Baseline mean 152 150 147 146
Change 01 year 3.0 (4.6, 1.4) 0.4 (1.8, 1.0) 4.8 (6.6, 2.9) 4.0 (5.9, 2.1)
Change 02 years 2.0 (3.7, 0.3) 0.4 (1.3, 2.0) 6.0 (8.5, 3.5) 4.7 (6.6, 2.6)
Net change 01 year 2.6 (4.7, 0.5) 0.8 (3.4, 1.9)
Net change 02 years 2.4 (4.7, 0.0) 1.3 (4.5, 1.8)
Diastolic blood pressure (mmHg)
Baseline mean 93 93 89 89
Change 01 year 3.3 (4.3, 2.3) 0.6 (1.4, 0.3) 3.6 (4.6, 2.7) 2.8 (3.9, 1.7)
Change 02 years 2.4 (3.4, 1.4) 0.4 (1.4, 0.6) 3.8 (5.1, 2.6) 3.7 (4.9, 2.6)
Net change 01 year 2.7 (4.0, 1.4) 0.8 (2.3, 0.6)
Net change 02 years 2.0 (3.4, 0.6) 0.1 (1.8, 1.6)
CI, condence interval.
Non-pharmacological treatment of hypertension Kastarinen et al. 2509
term 0.021), but such a difference was not detected in
the analysis from baseline to 2 years. Similarly, the net
reductions in alcohol consumption from baseline to
1-year and 2-year visits were signicantly greater in
this group compared to the group with antihypertensive
drug treatment (from baseline to 1-year visit 17 versus
1 g/week, P for the interaction term 0.025; from base-
line to 2-year visit 9 versus 5 g/week, P for the
interaction term 0.029). The response for the interven-
tion in terms of lifestyle changes did not differ sig-
nicantly between the sexes or according to the
baseline age. In a multiple linear regression analysis, a
positive relation with 2-year change in blood pressure
was found for weight change in both subjects with no
antihypertensive drug treatment (SBP, P 0.003; DBP,
P , 0.001) and in drug-treated subjects (SBP, P
0.034; DBP, P 0.012), but not for the changes in
other lifestyle variables. In a separate analysis among
the subjects with no antihypertensive drug treatment,
adjusting for both BP and weight at baseline, the
estimated effect of the 1 kg weight lost at 2 years was a
reduction of 0.55 mmHg in SBP and of 0.50 mmHg in
DBP
Changes in other cardiovascular risk factors
After 2 years of intervention, the net changes in total
(0.10 mmol/l) and in LDL cholesterol (0.15 mmol/l)
were signicant in favour of the intervention group. Also,
in persons without lipid-lowering drug treatment during
the study, the net reductions in total cholesterol
(0.11 mmol/l; 95% CI 0.20 to 0.02) and in LDL
cholesterol (0.13 mmol/l; 95% CI 0.22 to 0.03) were
larger in the intervention group than in the control group
(data not shown). Smoking was already rare at baseline,
and no signicant changes in that habit were observed
during the study. The serum insulin concentration de-
creased more among the persons assigned to interven-
tion, but the net change was not statistically signicant.
Discussion
The lifestyle counselling provided in the LIHEF study
could produce a signicant reduction in BP level of the
subjects with no antihypertensive drug treatment com-
pared with usual care for 2 years. Weight loss was
signicantly greater in the intervention group at the 1-
year visit, and this difference was maintained during
the second year. The intervention programme could
not induce any signicant reductions in salt intake.
Despite the fact that in 95% of the participants the
weekly alcohol consumption was already at the recom-
mended level at baseline, a small but signicant reduc-
tion in alcohol intake occurred in the intervention
group during the rst year. The self-reported leisure-
time physical activity increased signicantly more in
the intervention group throughout the study.
Large-scale randomized trials reporting the effects of
lifestyle intervention on BP and other cardiovascular risk
factors in hypertensive persons in the primary care setting
are rare. The very few previous studies have included
relatively small numbers of patients, with the maximum
follow-up time of 12 months [1517]. Iso et al. [18]
reported that a community-based trial lowered BP among
hypertensive subjects. In their study, the intervention
was based mainly on group sessions instead of the
individualized health counselling used in our study.
The net changes in BP and lipid levels detected in our
study are in accordance with trials of multiple risk
factor intervention or dietary intervention with people
at high risk but not necessarily hypertensive [1921].
The reduction achieved in body weight after 2 years of
intervention was almost the same as in some trials with
more intensive intervention [1]. In contrast, the BP
reduction observed in the subjects without antihyper-
tensive drug treatment was smaller compared to some
clinical trials of non-pharmacological treatment of
hypertension [4,22]. These trials used very intensive
intervention compared to our study. Thus it seems that
at least some of the results obtained in high-intensity
intervention trials can be translated successfully to
primary health care.
According to the separate analysis of the dietary data of
Table 4 The percentage of participants reaching the pre-dened goals for the intervention during the trial among the persons out of goals
at baseline
Year 1 Year 2
Intervention
a
Usual care
a
Difference in
change (95% CI) Intervention Usual care
Difference in
change (95% CI)
BMI , 25 kg/m
2
7.8 (294) 3.9 (279) 3.9 (0.1, 7.7) 8.2 3.6 4.6 (1.0, 8.4)
> 5% reduction in BMI 18.7 9.3 9.4 (3.8, 15.0) 22.1 10.4 11.7 (5.8, 17.7)
24-hour U-Na excretion , 85 mmol 10.6 (301) 8.7 (286) 1.9 (2.9, 6.7) 7.0 7.0 0.0 (4.1, 4.1)
> 10% reduction in 24-h U-Na excretion 41.5 33.6 7.9 (0.2, 15.8) 41.5 33.6 7.9 (0.2, 15.8)
, 2 alcohol drinks per day 27.8 (18) 9.5 (21) 18.3 (6.0, 42.5) 16.7 9.5 7.1 (14.2, 28.5)
Recommended level of physical activity
b
34.7 (173) 24.0 (171) 10.7 (1.2, 20.3) 34.1 22.8 11.3 (1.8, 20.8)
Not smoking 6.5 (31) 12.0 (25) 5.6 (20.9, 9.9) 12.9 12.0 0.9 (16.5, 18.3)
CI, condence interval; BMI, body mass index; U-Na, urinary sodium.
a
Number of subjects out of each goal at baseline in parentheses.
b
Leisure-time physical activity at
least three times per week and at least to 30 minutes.
2510 Journal of Hypertension 2002, Vol 20 No 12
this study, the proportion of fat, and especially of
saturated fats, in total energy intake decreased signi-
cantly more in the intervention group compared to
usual care [12]. Also, the total energy intake tended to
decrease more in the intervention group, although not
reaching the level of statistical signicance. In addition
to the increase in physical activity, these changes in
diet may have contributed to the observed differences
in changes of body weight, lipid levels and BP between
the randomized groups. The dietary data were in
accordance with the results of the 24-h urinary sodium
excretion, showing no signicant changes in sodium
intake. These results repeat the ndings of the many
other studies that have demonstrated the difculties in
achieving the recommended level of salt intake in free-
living subjects [23,24]. It has been suggested that the
main reason for this difculty in salt restriction seen in
all Western countries is the still relatively high concen-
tration of salt in processed foods [25].
The differences in BP reduction observed between the
groups could not be explained by accustomization with
BP measurement, because there was not any difference
in self-reported frequency of BP measurements be-
tween the groups during the study. One explanation for
the greater fall in blood pressure among the participants
who continued antihypertensive drug treatment com-
pared with the participants without antihypertensive
drugs could be a more regular use of antihypertensive
drugs during the trial than before.
As usual in volunteer-based intervention studies, the
study sample is seldom fully representative of the back-
ground population. Highly motivated volunteers are
usually more susceptible to accept the recommended
intervention than the population at large. On the other
hand, many volunteers in lifestyle intervention studies
have already previously changed their lifestyle, which
could reduce the power of the intervention. In our study,
the mean BMI, total cholesterol and the prevalence of
smoking were lower than in Finnish hypertensive sub-
jects in the population-based FINRISK study in 1997
[2628]. The study participants also came from a
geographical area with a long history of cardiovascular
disease prevention activities, and thus many of them
already had a relatively good knowledge about lifestyle
factors affecting the cardiovascular risk [29]. In addition,
the contamination of the control group, due to the fact
that their follow-up visits were done by the same nurses
as with the intervention group, might have reduced the
difference in the lifestyle changes between the groups.
Also, the fact that they were under systematic observa-
tion in an interesting study likely inuenced them.
Thus, our observed effects of the intervention, as usual
in this kind of studies, are likely to be conservative.
In conclusion, the favourable changes in BP and other
cardiovascular disease risk factors in hypertensive per-
sons participating in our study were smaller than in the
trials with more intensive interventions. However, the
principal aim of this study was to nd out the extent to
which lifestyle intervention will work in the usual
primary health care setting. From this point of view,
our results were quite satisfactory, considering the
limited requirement for the use of health care re-
sources. The potential of the intervention shown in this
study can certainly be much improved by further
development and systematic dissemination, especially
concerning newly detected hypertensive persons. Non-
pharmacological treatment of hypertension has been
advocated for a long time, but so far only limited
evidence and experience has been available as to its
effective implementation within primary care. The task
is not easy, due to the limited time and resources that
the public health service can allocate for such preven-
tive services. However, we have shown that this
approach works.
Acknowledgements
The statistician Pirjo Halonen, MSc, advised M. Kastar-
inen about data analysis. Mr Veli Koistinen was respon-
sible for preparing the database. Study nurses Anneli
Mitrunen and Mari Aalto screened the study subjects
and performed BP and anthropometrical measurements.
Registered dietitians Sari Aalto and Sointu Lassila were
responsible for the training of nurses in dietary issues
and for the group sessions organized for subjects
assigned to intervention. We thank for the staff of the
North Karelia Project for the help given in coordination
of the study. Antti Jula MD, PhD; Antti Malmivaara,
MD, PhD; Matti Romo, MD, PhD; Jyrki Olkinuora,
MD, Markku Helio vaara, MD, PhD; Erkki Vartiainen,
MD, PhD and Timo Lakka, MD, PhD were members
of the LIHEF study group and helped in designing the
study. The authors are grateful to all practice staff
working in the participating health care centres, as well
as to the hypertensive persons participating the study.
References
1 Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D,
et al. Long-term weight loss and changes in blood pressure: results of the
Trials of Hypertension Prevention, phase II. Ann Intern Med 2001; 134:
111.
2 Puddey IB, Beilin LJ, Vandongen R. Regular alcohol use raises blood
pressure in treated hypertensive subjects. A randomised controlled trial.
Lancet 1987; 1:647651.
3 Cutler JA, Follmann D, Allender PS. Randomised trials of sodium reduction:
an overview. Am J Clin Nutr 1997; 65 (suppl 2):643651.
4 Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al.
Effects on blood pressure of reduced dietary sodium and the Dietary
Approaches to Stop Hypertension (DASH) diet. DASHSodium Colla-
borative Research Group. N Engl J Med 2001; 344:310.
5 Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, Andrews GR.
The effectiveness of exercise training in lowering blood pressure: a meta-
analysis of randomised controlled trials of 4 weeks or longer. J Hum
Hypertens 1997; 11:641649.
6 Neaton JD, Grimm RH Jr, Prineas RJ, Stamler J, Grandits GA, Elmer PJ,
et al. Treatment of Mild Hypertension Study. Final results. Treatment of
Mild Hypertension Study Research Group. JAMA 1993; 270:713724.
Non-pharmacological treatment of hypertension Kastarinen et al. 2511
7 Puska P, Iacono JM, Nissinen A, Korhonen HJ, Vartiainen E, Pietinen P,
et al. Controlled, randomised trial of the effect of dietary fat on blood
pressure. Lancet 1983; 1:15.
8 The sixth report of the Joint National Committee on prevention, detection,
evaluation, and treatment of high blood pressure. Arch Intern Med 1997;
157:24132446.
9 Guidelines Subcommittee.1999 World Health OrganizationInternational
Society of Hypertension Guidelines for the Management of Hypertension.
J Hypertens 1999; 17:151183.
10 Ramsay L, Williams B, Johnston G, MacGregor G, Poston L, Potter J, et al.
Guidelines for management of hypertension: report of the third working
party of the British Hypertension Society. J Hum Hypertens 1999;
13:569592.
11 Kuulasmaa K, Hense HW, Tolonen H for the WHO MONICA project.
Quality assessment of data on blood pressure in the WHO MONICA
project. http:www.ktl./publications/monica/bp/bpqa.htm. [Accessed 13
March 2002].
12 Korhonen M, Kastarinen M, Uusitupa M, Puska P, Nissinen A. The effect of
intensied diet counselling on the diet of hypertensive subjects in primary
health care. A 2-year open randomised controlled trial of lifestyle intervention
against hypertension in Eastern Finland (LIHEF). Prev Med 2002, (in press).
13 Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration
of low-density lipoprotein cholesterol in plasma, without use of the
preparative ultracentrifuge. Clin Chem 1972; 18:499502.
14 Gardner M, Gardner S, Winter P. Condence interval analysis (CIA).
Microcomputer program manual. London: BMJ Publishing Group and MJ
Gardner; 1991.
15 Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary
treatment of patients with mild to moderate hypertension in a general
practice: a pilot intervention study (1). The rst three months. J Hum
Hypertens 1990; 4:368371.
16 Cohen MD, DAmico FJ, Merenstein JH. Weight reduction in obese
hypertensive patients. Fam Med 1991; 23:2528.
17 Woollard J, Beilin L, Lord T, Puddey I, MacAdam D, Rouse I. A controlled
trial of nurse counselling on lifestyle change for hypertensives treated in
general practice: preliminary results. Clin Exp Pharmacol Physiol 1995;
22:466468.
18 Iso H, Shimamoto T, Yokota K, Sankai T, Jacobs DR Jr, Komachi Y.
Community-based education classes for hypertension control. A 1.5-year
randomised controlled trial. Hypertension 1996; 27:968974.
19 Ebrahim S, Smith GD. Systematic review of randomised controlled trials of
multiple risk factor interventions for preventing coronary heart disease.
BMJ 1997; 314:16661674.
20 Brunner E, White I, Thorogood M, Bristow A, Curle D, Marmot M. Can
dietary interventions change diet and cardiovascular risk factors? A meta-
analysis of randomised controlled trials. Am J Public Health 1997;
87:14151422.
21 Steptoe A, Doherty S, Rink E, Kerry S, Kendrick T, Hilton S. Behavioural
counselling in general practice for the promotion of healthy behaviour
among adults at increased risk of coronary heart disease: randomised trial.
BMJ 1999; 319:943947.
22 Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr,
Kostis JB, et al. Sodium reduction and weight loss in the treatment of
hypertension in older persons: a randomized controlled trial of non-
pharmacologic interventions in the elderly (TONE). TONE Collaborative
Research Group. JAMA 1998; 279 (11):839846.
23 Pietinen P, Tanskanen A, Nissinen A, Tuomilehto J, Puska P. Changes in
dietary habits and knowledge concerning salt during a community-based
prevention programme for hypertension. Ann Clin Res 1984; 16 (suppl
43):150155.
24 Evers SE, Bass M, Donner A, McWhinney IR. Lack of impact of salt
restriction advice on hypertensive patients. Prev Med 1987; 16:213220.
25 Kumanyika S. Behavioral aspects of intervention strategies to reduce
dietary sodium. Hypertension 1991; 17 (suppl 1):190195.
26 Kastarinen MJ, Nissinen AM, Vartiainen EA, Jousilahti PJ, Korhonen HJ,
Puska PM, et al. Blood pressure levels and obesity trends in hypertensive
and normotensive Finnish population from 1982 to 1997. J Hypertens
2000; 18:255262.
27 Kastarinen M, Tuomilehto J, Vartiainen E, Jousilahti P, Sundvall J, Puska P,
et al. Trends in lipid levels and hypercholesterolaemia in hypertensive and
normotensive Finnish adults from 1982 to 1997. J Intern Med 2000;
247:5362.
28 Kastarinen M, Tuomilehto J, Vartiainen E, Jousilahti P, Nissinen A, Puska P.
Smoking trends in hypertensive and normotensive Finns during 1982
1997. J Hum Hypertens 2002; 16:299303.
29 Puska P, Tuomilehto J, Nissinen A, Vartiainen E. The North Karelia Project:
20-year results and experiences. Helsinki: National Public Health Institute;
1995.
2512 Journal of Hypertension 2002, Vol 20 No 12
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Learning DisabilityДокумент240 страницLearning DisabilityKUNNAMPALLIL GEJO JOHNОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Guide To: Raising DucksДокумент16 страницGuide To: Raising DucksNeil MenezesОценок пока нет
- OMFC Application RequirementsДокумент1 страницаOMFC Application RequirementshakimОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Investigation and Treatment of Surgical JaundiceДокумент38 страницInvestigation and Treatment of Surgical JaundiceUjas PatelОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Benign Paratesticlar Cyst - A Mysterical FindingДокумент2 страницыBenign Paratesticlar Cyst - A Mysterical FindingInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Health According To The Scriptures - Paul NisonДокумент306 страницHealth According To The Scriptures - Paul NisonJSonJudah100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Verbalizing Importance of Adequate Nutrition Feeds Self UnassistedДокумент2 страницыVerbalizing Importance of Adequate Nutrition Feeds Self UnassistedMasruri EfendyОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Occupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiДокумент99 страницOccupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiDea MaharaniОценок пока нет
- Bharat India: Extremely Bad Status of Testing & VaccinationДокумент308 страницBharat India: Extremely Bad Status of Testing & VaccinationP Eng Suraj SinghОценок пока нет
- Columbian Exchange Graphic OrganizerДокумент2 страницыColumbian Exchange Graphic Organizerapi-327452561100% (1)
- Radiographic InterpretationДокумент46 страницRadiographic InterpretationSanaFatimaОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- DCA and Avemar A Theoretical Protocol FoДокумент33 страницыDCA and Avemar A Theoretical Protocol FosiesmannОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- MSDS Jun-Air SJ-27FДокумент8 страницMSDS Jun-Air SJ-27FJuan Eduardo LoayzaОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Aioh Position Paper DPM jdk2gdДокумент26 страницAioh Position Paper DPM jdk2gdRichardОценок пока нет
- Neurogenic Shock in Critical Care NursingДокумент25 страницNeurogenic Shock in Critical Care Nursingnaqib25100% (4)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Crim 2 Assignment Title 8 of RPC Book 2Документ8 страницCrim 2 Assignment Title 8 of RPC Book 2Gio AvilaОценок пока нет
- Individual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledДокумент12 страницIndividual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledTiffanny Diane Agbayani RuedasОценок пока нет
- BehandlungskarteiДокумент2 страницыBehandlungskarteidenyse bakkerОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Millennials Generation's Role Is Questioned. How Does It Affect Life Aspects?Документ3 страницыMillennials Generation's Role Is Questioned. How Does It Affect Life Aspects?AjengОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- List of Medical SymptomsДокумент6 страницList of Medical SymptomsAndré Raffael MoellerОценок пока нет
- Malaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Документ40 страницMalaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Livia HanisamurtiОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Grape Growing in TennesseeДокумент28 страницGrape Growing in TennesseeDbaltОценок пока нет
- What Explains The Directionality of Flow in Health Care? Patients, Health Workers and Managerial Practices?Документ7 страницWhat Explains The Directionality of Flow in Health Care? Patients, Health Workers and Managerial Practices?Dancan OnyangoОценок пока нет
- Python Ieee Projects 2021 - 22 JPДокумент3 страницыPython Ieee Projects 2021 - 22 JPWebsoft Tech-HydОценок пока нет
- Lab 1: Food SpoilageДокумент15 страницLab 1: Food SpoilageAdibHelmi100% (2)
- Sodium+Bicarbonate Neo v2 0 PDFДокумент3 страницыSodium+Bicarbonate Neo v2 0 PDFApres SyahwaОценок пока нет
- EMOTIONS Are Metaphysical! - TriOriginДокумент1 страницаEMOTIONS Are Metaphysical! - TriOriginStellaEstel100% (2)
- An Overview of Mechanical Ventilation in The Intensive Care UnitДокумент9 страницAn Overview of Mechanical Ventilation in The Intensive Care UnitJaime Javier VegaОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Cyclooxygenase PathwayДокумент8 страницCyclooxygenase PathwayIradatullah SuyutiОценок пока нет
- Nguyen 2019Документ6 страницNguyen 2019ClintonОценок пока нет