Академический Документы
Профессиональный Документы
Культура Документы
Inflammation Overview
Загружено:
Megan MorenoОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Inflammation Overview
Загружено:
Megan MorenoАвторское право:
Доступные форматы
7.
30 Asthma and Chronic Obstructive Pulmonary
Disease
G P Roth, Abbott Bioresearch Center, Worcester, MA, USA
D W Green, Amgen Inc., Cambridge, MA, USA
& 2007 Elsevier Ltd. All Rights Reserved.
7.30.1 Disease State 873
7.30.2 Disease Basis 875
7.30.2.1 Asthma: Leukocyte Activation and Trafcking 875
7.30.2.2 Asthma: Airway Remodeling 878
7.30.2.3 Chronic Obstructive Pulmonary Disease: Leukocyte Activation and
Trafcking 878
7.30.2.4 Chronic Obstructive Pulmonary Disease: Remodeling 879
7.30.3 Experimental Disease Models 880
7.30.4 Clinical Trial Issues 881
7.30.5 Current Treatment 883
7.30.6 Unmet Medical Needs 884
7.30.7 New Research Areas 884
7.30.7.1 Chemokine Receptor CCR3 884
7.30.7.2 CRTH2 and the DP-1 Receptor 888
7.30.7.3 Phosphodiesterase Type 4 893
7.30.7.4 Mast Cell Tryptase and Chymase 897
7.30.7.5 Interleukin-5 (IL5) Receptor Inhibitors 902
7.30.7.6 Inhibition of Leukotriene Biosynthesis 904
References 910
7.30.1 Disease State
Asthma and chronic obstructive pulmonary disease (COPD) are serious respiratory diseases that not only compromise
the health and daily activities of those affected, but also impose an economic burden on countries around the globe. As
communities become more industrialized, the incidence of asthma and COPD increases. It is estimated the global
incidence of asthma is 300 million people and accounts for one in every 250 deaths.
1
Global estimates for COPD
predict it will rank fth as a worldwide health burden by the year 2020.
2
In 1996 COPD was accountable for over
100 000 deaths in the US, putting it behind heart disease, cancer, and stroke as the major mortality diseases.
3
Age, sex,
race, and socioeconomic status are more important factors in the epidemiology of COPD than asthma. Incidence and
mortality of COPD incidence increase with age and prevalence is higher among males than females (although the
incidence in females is rising), whites than nonwhites, and blue-collar than white-collar workers.
4
Asthma occurs across
all demographics, but its escalating incidence in children is particularly alarming. It is the leading cause of childhood
hospitalization and school absenteeism in the US. In 1998, it was estimated that more than 15 million people in the US
have asthma, leading to 500 000 hospitalizations and 5 000 deaths annually.
3
At least 16 million people in the US have
COPD, which is divided between 14 million with chronic bronchitis and 2 million with emphysema.
5
The total annual
costs in the US for asthma
6
and COPD
7
have been estimated at over $12 billion and $14 billion, respectively. A
comparison of the epidemiology for asthma and COPD is summarized in Table 1.
Asthma and COPD are both characterized by airway obstruction that leads to signicant breathlessness (dyspnea).
Several diagnostic indicators can be used to distinguish the diseases from one another
8
as summarized and compared in
Table 2. Asthma typically involves a reversible airow limitation, the onset usually occurs in childhood, the symptoms
vary from day to day, and a family history is common. Airow limitation in COPD is not fully reversible, the onset occurs
873
in mid-life and is usually correlated with a long history of cigarette smoking, and the symptoms are slowly progressive.
Severe cases of asthma can be more difcult to distinguish from COPD, especially if the reversibility of airway
obstruction is diminished.
In asthma the frequency and severity of symptoms can vary greatly in the population as the disease progresses in an
individual.
9
An asthma attack can be triggered by a number of different factors including allergens (animal dander, dust
mites, etc.), viral infections, changes in temperature or humidity, exercise, environmental pollutants, or strong
emotional reactions (anxiety, crying, laughing, etc.).
1014
Bronchoconstriction and airway inammation contribute to
airway hyperreactivity in asthma, which typically results in coughing and wheezing. During the attack airway ow is
Table 1 Comparison of asthma and COPD epidemiology in the USA
Asthma COPD
Occurrence 15 million 16 million
Estimated annual costs $12 billion (2001) $14 billion (2000)
Deaths (Center for Disease Control (CDC) Reports) 4261 (2002) 119 054 (2000)
Common age of onset Childhood Over 50 years
Incidence by sex Male female Male4female
Incidence by race No difference White4nonwhite
Incidence by socioeconomic status No difference Blue-collar4white-collar
Table 2 Similarities and differences between asthma and COPD
Asthma COPD
Stimulus Allergens Environmental pollutant
Viral infections
Changes in temperature or humidity
Exercise
Environmental pollutants
Strong emotional reactions
Extent of airway inammation All airways (except parenchyma) Peripheral
Airway obstruction and dyspnea Yes; reversible Yes; not reversible
Cellular activation T cell and B cells Macrophages
IgE production Cytokines
Mast cells and basophils Proteases
Leukotrienes Prostaglandins
Histamine Leukotrienes
Cytokines Growth factors
Proteases Reactive O
2
Growth factors
Primary T cells CD4
CD8
Inltrating cells Eosinophils Neutrophils
Destruction of parenchyma No Yes
874 Asthma and Chronic Obstructive Pulmonary Disease
decreased by the constriction of the bronchi and can be exacerbated by inammation and increased mucus secretion.
Tachypnea and tachycardia are usually observed and in more severe cases patients have difculty speaking and
symptoms of cyanosis (blue skin) can appear as the attack worsens.
Pulmonary function tests are used to evaluate the progression of asthma and the response to therapeutic agents.
The most common test is spirometry, which measures the maximum airow during expiration (peak expiratory ow
(PEF) or forced expiratory lung volume (FEV
1
)). The diagnosis can also be conrmed by bronchial hyperresponsive-
ness to histamine or methacholine.
14
Asthma severity is classied into four stages, which are dened by the frequency
of attacks and results of spirometry tests.
9
In the least severe stage, mild intermittent asthma, attacks occur at a
frequency of less than two per week, night-time episodes are infrequent, and the effect on PEF or FEV
1
is less than
20% relative to healthy subjects. The next most severe stage, mild persistent asthma, is also characterized by a change
in PEF or FEV
1
of less than 20% but the frequency of attacks is three to six episodes per week and more than two
night-time attacks per month. In the third stage, moderate persistent asthma, the frequency of attacks (daily with
more than ve night-time episodes per month) and the effect on lung function (2040% change in PEF or FEV
1
) both
increase. In the most critical stage, severe persistent asthma, attacks are continuous and the effect on lung function is
greater than a 40% change in PEF or FEV
1
.
In contrast to asthma, COPD can almost always be linked to exposure to preventable environmental irritants. In
developed countries it is estimated that cigarette smoking accounts for more than 95% of COPD cases. Other risk
factors include exposure to air pollution such as indoor burning fuels, occupational exposure, and poor diet.
15
The onset
of symptoms is usually observed in people aged 5060 who have a long history of cigarette smoking. Most patients have
symptoms of chronic bronchitis and emphysema as well as mucus plugging but may differ in the degree of emphysema
and chronic bronchitis.
16
Individuals with an a
1
-antitrypsin deciency associated with a homozygous Z variant develop
emphysema earlier in life and this is worsened by smoking. Although this indicates a genetic predisposition to COPD,
fewer than 1% of COPD patients have an a
1
-antitrypsin deciency and other variants that result in decreased serum
levels of a
1
-antitrypsin have not been linked to COPD.
17
COPD and asthma can typically be distinguished from one another based upon the extent of obstruction,
inammation, and tissue damage in the airways.
15
Asthma usually involves inammation of all airways whereas
inammation in COPD is usually restricted to the bronchioles (peripheral or small airways). Inammation in asthma
results in airway hyperresponsiveness, whereas inammation in COPD results in alveolar destruction. In both diseases
inammation of the epithelial cells lining the airways (asthma) or bronchioles (COPD) results in enlargement of
mucus-secreting glands and the number of goblet cells, causing hypersecretion of mucus. Chronic inammation in
COPD and severe asthma results in repeated cycles of injury and repair, causing brosis and narrowing of the small
airways. These processes ultimately lead to dilation and destruction of the bronchioles in COPD followed by the
formation of large distended air sacs (bullae) in the lung. The symptoms associated with this COPD pathology are a
progressive dyspnea along with chronic cough and sputum production.
8
The severity of COPD has been classied into three stages distinguished by symptoms and spirometry scores relative
to normal pulmonary function.
8
Individuals with a chronic cough and sputum production but no change in spirometry
scores are considered at Stage 0 and at risk. Stage I (mild COPD) is characterized by mild airow limitation resulting in
an FEV
1
score decreased by up to 20% that is usually, but not always, associated with chronic cough and sputum
production. At Stage II (moderate COPD) patients usually seek medical attention due to dyspnea and increased cough
and sputum production. Pulmonary function is decreased by more than 20% at this stage and can be further subdivided
into Stage IIA or IIb depending upon whether FEV
1
has been effected more than 50% or not, respectively. In Stage III
(severe) COPD pulmonary function has decreased more than 70% and/or clinical symptoms of respiratory failure or right
heart failure are observed. Quality of life is signicantly affected and exacerbations of the disease can be life threatening.
7.30.2 Disease Basis
The cellular pathology of both asthma and COPD involves several types of immune cells and mediators, and the
cellular progression of disease follows a general sequence of leukocyte activation, trafcking, and airway remodeling.
Both diseases will be reviewed in the context of cellular pathology and therapeutic targets involved in each step.
7.30.2.1 Asthma: Leukocyte Activation and Trafcking
Current models of asthma pathology divide the disease into an early and late immune response.
18
The early immune
response refers to the events that lead up to the production of immunoglobulin E (IgE) (Figure 1) and cause acute
bronchospasm, edema, and airow obstruction that is reversible.
Asthma and Chronic Obstructive Pulmonary Disease 875
The acute process is initiated when a dendritic cell in the airway lining encounters an antigen and is stimulated
to migrate to the lymph node. There the antigen is presented to T and B cells, and the interaction between these
cells (referred to as costimulation) activates the B cell to produce IgE. Costimulation and the subsequent activation
of B cells is mediated by the interaction of two pairs of receptors between T and B cells. The rst pair involves
interleukin-4 (IL4) or IL13 secreted from Tcells and the respective receptor on the B cell. The second pair involves
CD40 on the surface of B cells and its receptor on the surface of T cells. Costimulation results in the activation of
intracellular signaling pathways that ultimately converge on the nucleus and lead to the expression and production of
IgE. The antibodies circulate and bind to high-afnity receptors (FceRI) on mast cells and basophils and to low-afnity
receptors (FceRII) on lymphocytes, eosinophils, platelets, and macrophages. The cross-linking of IgE-bound FceRI
receptors on mast cells activates intracellular signaling pathways that result in degranulation of histamine and
leukotrienes into the mucosal and submucosal sites of the airway. The cysteinyl leukotrienes (LTC
4
, LTD
4
, LTE
4
) are
peptide-conjugated lipids that arise from arachadonic acid metabolism, and along with histamine, cause contraction of
bronchial smooth muscle.
19
Mast cells also play a role in the late asthma response that leads to airway hyperresponsiveness (Figure 2).
Activated mast cells also release cytokines such as the interleukins 1 through 5 (IL1, IL2, IL3, IL4, IL5), interferon-g
(IFN-g), and tumor necrosis factor-a (TNF-a) as well as granulocytemacrophage colony-stimulating factor
(GM-CSF).
18
GM-CSF, IL3, and in particular IL5 are known to stimulate production of eosinophils in the bone
marrow.
20
Eosinophils released into the circulation constitutively express proteins such as the a
4
b
1
integrin VLA-4
(very late antigen-4), the b
2
integrin LFA-1 (lymphocyte function-associated antigen-1), L selectin, and P selectin
glycoprotein ligand (PSGL)-1. These proteins selectively bind to the adhesion molecules and selectins on the
endothelial cells.
21,22
Cytokines such as IL4, IL13, and other products of inammation induce the expression of
proteins on the surface of endothelial cells lining the vasculature such as the intracellular and vascular cell-adhesion
molecules ICAM-1 and VCAM-1, respectively, and the E and P selectins.
23
The interaction between eosinophil and
endothelial cell surface proteins is regulated by the interaction of specic chemoattractant cytokines known as
Figure 1 Production of IgE and its consequences in the early asthma immune response. (Reproduced with permission from
Busse, W. W.; Lemanske, R. F. N. Engl. J. Med. 2001, 344, 350362.)
876 Asthma and Chronic Obstructive Pulmonary Disease
chemokines with specic receptors on eosinophils. In particular, the chemokine eotaxin (CCL11) produced by
endothelial cells in response to IL4 or IL13
24
binds to the chemokine receptor CCR3 on the surface of eosinophils and
can inuence the afnity of the cell surface interactions between endothelial cells and eosinophils.
25
Eosinophils can
also migrate in response to chemoattractants such as prostaglandin D
2
through the receptors DP (D
2
prostaglandin)
and CRTH
2
(chemoattractant receptor-homologous molecule expressed on Th2 cells).
26
The result of all of these
interactions is the rolling of eosinophils across the endothelial lining of the vasculature, which enables trafcking to
inammation sites in airways.
Antigen stimulation of naive CD4
T cells not only results in costimulation of B cells to produce IgE, but also
in the differentiation of T cells into Th2 cells.
27
Naive CD4
T cells can differentiate into either Th1 or Th2 cells.
These two types of T cells can be distinguished from one another by the types of cytokines they produce upon
stimulation. Th1 cells play a role in protective immunity and produce IL2 and IFN-g. Th2 cells predominate in the
inamed tissue of asthmatics along with mast cells produce cytokines that mediate allergic inammation (IL4, IL5,
IL6, IL9, and IL13). Th2 cell migration to inammation sites from the lymph nodes is essentially mediated by the
same selectins, integrins, chemokines, and chemoattractants involved in eosinophil trafcking.
28
The proliferation of
Th2 cells at inammatory sites can be stimulated by neighboring eosinophils as the latter can produce lymphokines
such as IL4.
29
Figure 2 Mast cell, eosinophils, and Th2 cells in the late asthma immune response. (Reproduced with permission from Busse,
W. W.; Lemanske, R. F. N. Engl. J. Med. 2001, 344, 350362.) For denitions see text.
Asthma and Chronic Obstructive Pulmonary Disease 877
7.30.2.2 Asthma: Airway Remodeling
The convergence of mast cells, eosinophils, and Th2 cells in the airways can lead to thickening of the airway
walls, which is referred to as airway remodeling.
13,30
The individual abnormalities involved in airway remodeling
include smooth muscle hypertrophy and hyperplasia, extracellular matrix deposition, alterations in epithelial and
goblet cells, and vascular remodeling, which all contribute to increasing airow resistance. Mast cells, eosinophils,
and Th2 cells at inammatory sites produce cytokines, growth factors, and other mediators that contribute to
these processes.
In severe cases of asthma increased smooth muscle mass can reduce the airway lumen three- to fourfold,
signicantly contributing to increased airway resistance. Mast cell degranulation releases mitogens such as histamine,
IL1b, LTD
4
, platelet-derived growth factor (PDGF) and tryptase which can induce smooth muscle cell hypertrophy
and hyperplasia.
31,32
Based upon in vitro results under serum-free conditions, direct contact of Th2 cells with smooth
muscle cells is believed to also stimulate smooth muscle proliferation.
33
In addition to inammatory cells, stimulated
endothelial cells can produce growth factors that induce smooth muscle proliferation.
34
The extracellular matrix (ECM) is composed of brous proteins (collagen and elastin) and adhesive proteins
(bronectin and laminin) embedded in a hydrous gel of glycosaminoglycans (hyaluronic acid) and proteoglycans
(versican, etc.). This hydrated mix of carbohydrates and insoluble brous proteins provides resilient scaffolding which
supports tissue structure in the airway.
13
The ECM is also a dynamic structure where a homeostatic balance
between degradation and synthesis is critical, and broblasts are cells that govern this process. Fibroblasts produce
the components of the ECM as well as the proteases that turn over the ECM and the protease inhibitors that
regulate the proteolytic activity. These protease/inhibitor pairs include matrix metalloproteases (MMP) and tissue
inhibitors of metalloproteases (TIMP), and there are several individual protein members of both families.
35
During
inammation, transforming growth factor b (TGF-b) is released from eosinophils and drives the differentiation of
broblasts into myobroblasts. The proliferation of lung broblasts is stimulated by mast cell tryptase through a
protease-activated receptor, PAR-2.
36
The proliferation of broblasts and/or their differentiation into myobroblasts
contributes to excessive production of ECM components and disruption of the homeostatic balance between
proteases and their inhibitors, which can result in the increased brosis and decreased elasticity of the airway wall
observed in asthma.
37
Thickening of epithelial cells and increased mucus secretion are part of asthma pathology. The epithelium provides
a protective barrier between the airway and the vasculature and is lined with mucus glands and epithelial goblet cells
that produce mucus. The epithelium is composed of several layers including the lamina reticularis and basal lamina
(basement membrane). In asthma the lamina reticularis thickens but not the basal lamina.
13
Deposition of ECM
components by broblasts and myobroblasts can contribute to thickening of the lamina reticularis as well as
proliferation of epithelial cells in response to inammatory mediators such as histamine. Epithelial damage can also
result from inammatory mediators such as histamine from mast cells and granule proteins, oxygen free radicals, and
TNF-a from eosinophils that cause epithelial shedding and lead to microvascular permeability and leakage of plasma
into the airways. This contributes to restricting the airway as plasma proteins can mix with mucus and inammatory
cells to form viscid luminal plugs. Hypersecretion of mucus can be stimulated by mast cell histamine, PGD
2
and
cysteinyl leukotrienes, and mucus glands and goblet cells can proliferate and enlarge in response to cytokines as well as
proinammatory and toxic mediators released by eosinophils.
As a consequence of the hypertrophy and hyperplasia of smooth muscle and epithelial cells, blood vessels enlarge
and new blood vessels are produced (angiogenesis).
38,39
Blood vessel enlargement, sometimes referred to as
nonsprouting angiogenesis, is commonly proportionally to the proliferation of endothelial cells. There are a number of
agents that can stimulate blood vessel enlargement and angiogenesis, and they are directly or indirectly attributable to
mast cells, eosinophils or Th2 cells in asthma. IL15 is a known angiogenic mitogen and can is produced by activated
Th2 cells and broblasts. The TNF-a produced by eosinophils is also an angiogenic factor. Epithelial cells and
broblasts are sources of the angiogenic stimuli epidermal growth factor (EGF), broblast growth factor (FGF), and
platelet-derived growth factor (PDGF).
34
7.30.2.3 Chronic Obstructive Pulmonary Disease: Leukocyte Activation and
Trafcking
Airway remodeling, leukocyte activation, and trafcking of leukocytes are also important to the progression of disease in
COPD and each process has common and distinct features from asthma. Even though COPD is roughly equivalent to
asthma with respect to global incidence, mortality, and socioeconomic impact, little is known about the disease
mechanism relative to asthma.
878 Asthma and Chronic Obstructive Pulmonary Disease
In contrast to the wide variety of molecular antigens and other factors that are asthma triggers, COPD is associated
with an abnormal inammatory response of the lungs to noxious particles and gases.
40
Also in contrast to asthma, the
sequence of molecular and cellular events involved in the progression of the disease is less well dened in COPD.
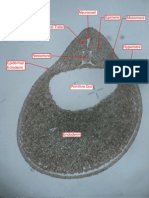
Some of the cellular mechanisms involved in the progression of COPD are depicted in Figure 3. As reactive oxygen
species are known to activate immune cells, it is likely that components of exogenous pollutants such a tobacco smoke
trigger inammation in COPD. Dendritic cells are abundant in the lung and increased in the airways of smokers, so
they are likely to be involved in initiating the COPD inammatory response.
41
However, there is no evidence to link
dendritic cell activation to COPD inammation. It is very likely that macrophages are involved in the pathogenesis of
COPD as they are dramatically increased in the lung tissue, airways, bronchiolar lavage, and sputum of COPD
patients
42
and can be localized to sites of alveolar damage.
43
Macrophages can be activated by cigarette smoke, which
induces the production of cytokines (IL8, TNF-a), elastolytic proteases (MMPs, cathepsins), lipid mediators such as
prostaglandin E
2
(PGE
2
) and leukotriene B
4
(LTB
4
), and GM-CSF, which releases neutrophils from bone marrow.
Interestingly, corticosteroids are not effective in treating inammation in COPD patients and cytokine and protease
production by macrophages from COPD patients is refractory to corticosteroids, but the production of GM-CSF is
not.
44
Cigarette smoke can also induce the production of GM-CSF and the cytokines TNF-a, IL1b, and IL8 in lung
epithelial cells. Neutrophils are also plentiful in the sputum and bronchiolar lavage, but not in the lung tissue and
airways of COPD patients.
45
It is possible they are relatively transient in lung tissue and airways relative to
macrophages. T cells are increased in the lung tissue and peripheral and central airways of COPD patients, but in
contrast to asthma, CD8
T
c
1 cells predominate over CD4
Th2 cells.
45
There is no increase in eosinophils, mast
cells, or the bronchoconstrictive agents histamine and cysteinyl leukotrienes in COPD.
46
Macrophages are resident in the lungs of COPD patients, but neutrophils and Tcells must migrate from the bone
marrow and lymph node, respectively, to the lung. Like eosinophils and CD4
T cells in asthma, neutrophils and
CD8
T cells trafc to inammatory sites through the interaction of VLA-4 and LFA-1 integrins and PSGL-1 with
endothelial adhesion molecules and selectins, respectively. Chemotaxis of CD8
T cells is mediated through
interactions between the chemokine receptor CXCR3 and its ligands IP-10, I-TAC, and Mig.
40
In contrast to
eosinophils, neutrophil chemoattractants include the cytokine/chemokine IL8 and the leukotriene LTB
4
. IL8 can bind
to either CXCR1 or CXCR2 chemokine receptors on neutrophils. Binding to CXCR1 is low afnity relative to the high-
afnity binding to CXCR2, and the former is thought to mediate effector functions such as protease and mediator
release while the latter is responsible for chemotaxis.
40
The neutrophil receptor for LTB
4
is BLT
1
, but this receptor can
also be found on Th1 and Th2 cells.
47
7.30.2.4 Chronic Obstructive Pulmonary Disease: Remodeling
There are multiple hypotheses that address the mechanism of airway obstruction and alveolar damage in COPD, and all
of these mechanisms probably contribute to the pathology of the disease. As mentioned earlier, reactive oxygen species
Cigarette smoke
Wood smoke
Numbers
Secretion
CTGF
TGF-1 Fibrosis
Elastolysis
MMP-9, MMP-12
Cathepsins K,L,S
Emphysema
Steroid
resistance
Peroxynitrite
ROS
NO
CXCR2
CXCR2
GRO-
GRO-
IL8
LTB
4
Ip-10
Mig
I-TAC
CXCR3
CD8
+
cells Monocytes
MCP-1
Neutrophils
Figure 3 Cellular mechanisms involved in COPD.
15
For denitions see text. (Reproduced with permission from Barnes, P. J.;
Shapiro, S. D., Pauwels, R. A. Eur. Respir. J. 2003, 22, 672688 & European Respiratory Society Journals Ltd.)
Asthma and Chronic Obstructive Pulmonary Disease 879
can activate immune cells. Reactive oxygen species such as superoxide anions and hydroxyl radicals are generated as
metabolic by-products by healthy cells but are quickly converted to less toxic molecules by enzymes such as catalase
and superoxide dismutase or nonenzymatic antioxidants such as glutathione and ascorbic acid. In COPD the
production of reactive oxygen species by cigarette smoke and activated neutrophils and macrophages can overwhelm
antioxidants to generate oxidative stress in the lungs.
40
Increased levels of reactive oxygen species cause increased
mucus production, constriction of airway smooth muscle, and plasma exudation in the airway. Epithelial cells can also
be stimulated to produce TGF-b, which can cause brosis through proliferation of broblasts and differentiation into
myobroblasts.
An imbalance between proteases and their endogenous inhibitors can cause increased mucus production and tissue
destruction. Serine proteases produced by neutrophils such as elastase and cathepsin G stimulate mucus secretion from
goblet epithelial cells and mucus glands.
48
Neutrophil elastase can also destroy elastin, which contributes to a loss of
elasticity in the lung tissue. Neutrophil elastase is usually kept in check by a
1
-antyrypsin inhibitor, but oxidation of the
inhibitor by cigarette smoke or reactive oxygen species can result in increased elastase activity in COPD.
40
A genetic
deciency of a
1
-antyrypsin is known to exacerbate COPD. The activity of matrix metalloproteases and cathepsins
produced by neutrophils and macrophages can overwhelm endogenous inhibitors such as TIMPs and cystatins. The
importance of MMP-12 to the development of COPD was demonstrated with MMP-12
/
mice exposed to tobacco
smoke as wild-type mice developed emphysema but knockout mice did not.
49
The cellular mechanisms involved in the pathology of asthma and COPD provide opportunities for therapeutic
intervention in these debilitating diseases, and the similarities and differences between these diseases are summarized in
Table 2. Blocking the activation of leukocytes has been approached by interfering with intracellular signaling pathways
through inhibition of phosphodiesterase type 4 (PDE4) or by blocking the inammatory mediators such as leukotrienes
by inhibiting their biosynthesis (5-lipoxygenase) or their interaction with receptors (BLT
1
receptor antagonists).
Interfering with the recruitment and trafcking of eosinophils in asthma has focused on blocking the action of IL5 or
antagonizing the CCR3 and CRTH2 receptors, while blocking the trafcking of neutrophils in COPD has been focused
on chemokine receptors such as CXCR2. The degranulation of leukocytes has also been targeted through inhibition of
the proteases that are released in this process including tryptase, elastase, cathepsins and matrix metalloproteases.
New approaches to identifying disease targets and treating asthma and COPD are also being explored. Genomic
linkage studies have led to the identication of new asthma targets such as the metalloprotease ADAM33,
50
a dipeptidyl
protease (DPP10) involved in cytokine processing,
51
and a putative transcription factor (PHF11).
52
Although genomic
linkage has not identied potential COPD therapeutic targets, a deciency in a
1
-antitrypsin inhibitor has been shown
to increase the susceptibility as mentioned in a previous section. In addition to several antibody approaches that will
be mentioned throughout the chapter, other nonconventional approaches have been considered as therapeutic strategies.
Given the importance of reactive oxygen species in COPD, antioxidant approaches such as N-acetylcysteine have
been initiated but antioxidant therapy with good bioavailability and sufcient potency to be effective in vivo has not been
achieved.
53
7.30.3 Experimental Disease Models
In any therapeutic area of drug discovery, animal models have limits with respect to mimicking human disease.
However, several asthma and COPD animal models have been developed that capture particular aspects of the
human disease. Most asthma models involve immunization and subsequent challenge with protein antigens such as
ovalbumin or immunogenic proteins from the nematode Ascaris suum
54
or cockroaches.
55
A wider variety of exogenous
agents are used to create emphysema in animals such as proteases (elastase, papain), chemicals (nitrogen dioxide,
ozone), particulates (coal dust, silica), and cigarette smoke.
56
The effect of these agents in both disease models
is measured by pulmonary function, cellular inltrate (bronchiolar lavage), and histopathology. Most clinical
therapeutic agents are effective in mammalian asthma and COPD models. Montelukast, a clinical cysteinyl
leukotriene-1 receptor antagonist, is efcacious in ovalbumin mouse
57
and A. suum sheep
58
asthma models. Zileuton, a
5-liopxygenase inhibitor, has also been shown to be efcacious in the A. suum sheep asthma model.
59
The adverse
effects of b
2
-agonist enantiomers such as (S)-albuterol were characterized in mouse asthma models and could inuence
therapeutic approaches with respect to using racemic mixtures or single enantiomers.
60
Thus, animal models can be
predictive of the human disease and have proven to be a valuable tool in the development of therapeutic agents for
asthma and COPD.
The majority of asthma and COPD animal models have been developed in rodents such as mice, rats, and guinea
pigs. In addition to the conventional model development described above, mice have afforded a genetic approach to
disease mechanisms in asthma and COPD through the development of transgenic and knockout mice. Genetic
880 Asthma and Chronic Obstructive Pulmonary Disease
manipulation of mice can be used for target identication in conventional models. It was mentioned in the previous
section that the importance of MMP-12 in the development of COPD was evaluated in MMP-12
/
mice exposed
to tobacco smoke.
49
Recent studies using BLT
1
knockout mice have demonstrated that the LTB
4
/BLT
1
axis is
required for the Th2 response in an ovalbumin-induced asthma model.
61
The generation of PDE4D knockout mice and
subsequent testing in an ovalbumin asthma model demonstrated that this PDE4 subtype is responsible for
bronchoconstriction in response to cholinergic stimulation but did not differ from wild-type mice with respect to
Th2-driven inammation.
62
This has important implications for the strategic design of PDE4 inhibitors that target
single or multiple PDE4 isoforms. The role of IFN-g in the pathology of COPD has been evaluated in transgenic mice
overexpressing IFN-g in the lung, which caused alveolar enlargement, enhanced lung volumes and pulmonary
compliance, and macrophage and neutrophil-enriched inammation. Induction of matrix metalloproteases and
cathepsins were observed with a concomitant decrease in secreted protease inhibitors.
63
Constitutive expression of
IL13 in the lungs of transgenic mice causes an inltration of eosinophils, lymphocytes, and macrophages into the
airways and hyperresponsiveness resembling asthma, and has been used to identify therapeutic targets associated with
the IL13 mechanism such as adenosine receptors.
64
Transgenic mice devoid of eosinophils have been created by
lineage-specic expression of a dyptheria toxin A protein that is selectively expressed in eosinophils (PHIL)
65
or
mutation of a transcription factor essential for eosinophil differentiation (Ddbl GATA).
66
Although both approaches
resulted in mice devoid of eosinophils, the PHIL mice were protected but the Ddbl GATA mice were not from airway
hyperresponsiveness and excess mucus production after immunization with ovalbumin. The Ddbl GATA mice did
demonstrate attenuated airway remodeling, which was not measured in PHIL mice. The results observed with the
Ddbl GATA mice more closely mirror the lack of effects observed in human clinical trials with an anti-IL5 antibody,
which also target eosinophils. The differences between the two transgenic mouse studies has been attributed to the
different strains that were used to create the PHIL (B6) and Ddbl GATA (Balb/c) mice, which coincidentally match
the phenotypic results of IL5 knockout mice in B6 or Balb/c strains. These studies illustrate the challenge of modeling
multigenic diseases such as asthma in animals.
67
In addition to enabling genetic approaches for animal model development, mice have several advantages over other
species for animal models with respect to reproductive turnover, short lifespans, and relatively inexpensive breeding,
housing, and maintenance costs. However, measuring pulmonary function in mice can be a challenge due to their size
and the obligate nasal breathing which lters tobacco smoke inefciently in COPD models. There are also physiological
differences from humans such as an absence of goblet cells and few submucosal glands in the trachea, and there is less
branching of the bronchial tree without respiratory bronchioles.
68
Signicant variation between species and strains with
respect to modeling COPD has been reported.
69
At a molecular level, mice can diverge from humans with respect to
drug target homology and cellular mechanisms. For example, there is only 70% amino acid sequence identity between
mouse and human CXCR2 receptors and mice do not have an orthologous protein for the human CXCR2 ligand IL8.
Nonhuman primate models offer the advantages of genetic, anatomical, and physiological similarity to humans and
relative ease in measuring pulmonary function.
70
Although the major drawback to using nonhuman primate models is
the cost relative to rodents, the genetic similarity to humans can be critical for testing biological therapeutic agents
such as antibodies against IL5
71
and differences in cellular mechanisms between species preclude the use of rodents as
with CXCR2 and IL8.
72
7.30.4 Clinical Trial Issues
Over the past decade several new classes of drugs targeting asthma and/or COPD have advanced into clinical trials.
It is perhaps not surprising that as asthma and COPD are complicated, multifactorial diseases clinical studies must be
designed carefully to evaluate the desired outcome. For example, it was mentioned in a previous section
that spirometry is the traditional method for assessing pulmonary function and drug efcacy in asthma and COPD.
This is a very facicle way to measure the efcacy of bronchodilators and other agents that target the acute
bronchospasm and airway ow obstruction phases of the diseases. However, it is only an indirect measure-
ment on the efcacy of agents that target the inammatory aspects of the disease. As inammation is now more widely
recognized as a critical part of the asthma and COPD disease mechanisms, measuring inammation biomarkers
as well as pulmonary function has become a more routine aspect of clinical trials.
53,73
The effect of anti-inammatory
agents has been addressed by invasive techniques such as bronchoscopy with biopsy, bronchiolar lavage, or
endobronchial brushings and by less invasive techniques such as induced sputum, exhaled breath condensate, or
gas analysis.
74
A trial measuring the effect of the leukotriene receptor antagonist montelukast examined the effect
on serum concentrations of the soluble IL2 receptor, IL4, soluble ICAM-1, and peripheral blood eosinophils in children
with asthma. Signicant decreases in each of these parameters correlated with improved pulmonary function.
75
Other
Asthma and Chronic Obstructive Pulmonary Disease 881
inammatory biomarker assays have been developed such as measuring levels of carboxyhemoglobin in patients with
COPD.
76
It must be noted that the measurement of biomarkers can be complicated by existing therapies. Asthmatic
patients are known to have increased eosinophils in sputum and exhale higher concentrations of nitric oxide. As
measuring exhaled nitric oxide would be a noninvasive, there was interest in developing it as a clinical biomarker.
However, dissociation between exhaled nitric oxide and sputum eosinophil counts can result from inhaled
corticosteroids. Therefore, exhaled nitric oxide is not viewed as a reliable biomarker given the prevalence of inhaled
corticosteroid use.
77
Other challenges in clinical trials include specic issues around the targets and therapies being developed.
A signicant challenge around the development of PDE4 inhibitors involved eliminating emetic effects associated
with the parent molecule rolipram. Although the exact mechanisms involved in the emetic effect have been debated
between high- and low-afnity interactions and PDE4 subclasses, several PDE4 inhibitors have apparently
overcome this obstacle and have advanced through clinical trials. Cilomilast from GlaxoSmithKline and rofumilast
from Altana and Pzer are in preregistration for COPD, and tetomilast from Otsuka has advanced into phase II trials
for COPD.
78
The development of therapeutic agents targeting eosinophils such as CCR3 antagonists has been called into
question based upon negative results in a phase II asthma trial for mepolizumab (SB-240563), a humanized antibody
against IL5.
79
Although treatment with the antibody signicantly decreased blood and airway eosinophils, no signicant
effect was observed in improving late asthmatic response or histamine-mediated airway responsiveness. However, the
design and implementation of the clinical trial has been questioned such that it cannot be readily concluded that IL5
and eosinophils are not involved in the late asthmatic response or airway hyperreactivity.
80
Although it was not
efcacious in asthma trials, mepolizumab has advanced into phase III clinical trials for hypereosinophilic syndrome.
81
Despite the controversy around IL5 and eosinophils in asthma, at least two CCR3 antagonists have advanced into
clinical trials for asthma; GSK-766994 is in phase II and BMS-639623 (DPC-168) is in phase I.
82
GlaxoSmithKline has
also advanced a CXCR2 antagonist (SB-322235) in clinical trials to target neutrophil trafcking in COPD.
83
As proteases have proven to be tractable and successful drug targets in other therapeutic areas (cardiovascular,
antivirals, etc.), parallel approaches have been attempted in asthma and COPD around neutrophil elastase, tryptase,
cathepsins, and matrix metalloproteases. ONO Pharmaceuticals has developed and launched the neutrophil elastase
inhibitor Sivelestat (ONO-5046) in Japan for acute lung injury
84
and it is anticipated that these inhibitors could be
efcacious in COPD.
85
Several pharmaceutical companies have been active in developing inhibitors of mast cell
b-tryptase, but few have reached clinical trials.
86
Axys/Celera advanced APC-366 into clinical trials for asthma despite
poor selectivity against other serine proteases such as trypsin and thrombin, but despite indications of clinical safety
and efcacy trials were stopped due to formulation issues. Johnson & Johnson have also advanced a tryptase inhibitor
into phase II trials for asthma (RWJ-56423), but poor bioavailability has limited its administration to aerosol delivery.
Inhibitors of cathepsins or matrix metalloproteases have not progressed into clinical trials for asthma or COPD, but are
being evaluated for other inammatory diseases. Serono and Vernalis (formerly British Biotech) are reported to have
advanced an MMP-12 inhibitor with a primary indication of multiple sclerosis into phase I clinical trials and a cathepsin
S inhibitor with a psoriasis indication has been advanced into phase I trials by Celera. Efcacy in these inammatory
diseases could lead to clinical evaluation in asthma and COPD.
Intensive efforts to develop therapeutic agents that interfere with the biosynthesis and activity of leukotrienes
have resulted in clinical success against asthma and more modest success against COPD.
87
Zileuton (Zyo),
a 5-lipoxygenase inhibitor,
88
and the leukotriene receptor antagonists zaprlukast (Accolate)
89
and montelukast
(Singulair)
90
, were some of the rst drugs to demonstrate clinical success but also highlight some of the issues in
clinical development of these drug classes. The clearance of zileuton from the circulation is relatively fast (half-life
of 4 h) and requires dosing at four times per day. The liver cytochrome P450 enzymes CYP1A2, CYP2C9, and
CYP3A4, mediate zileuton clearance, and inhibition of CYP1A2 can limit the use of zileuton as it appears to
interfere with the clearance of other drugs such as propanolol, theophyline, and waran.
91
Leukotriene receptor
antagonists such as zaprlukast and montelukast are more effective when used in combination with other
anti-inammatory drugs such as inhaled corticosteroids rather than as a monotherapy.
92
However, caution must
be taken when the use of inhaled corticosteroids is tapered as incidences of ChungStrauss syndrome, an eosino-
philic inltrative disorder, has been reported in combination with zaprlukast
93
or montelukast.
94
The incidence
of ChungStrauss syndrome associated with either leukotriene receptor antagonist is relatively low and is thought
to predate the antagonist therapy and is unmasked when inhaled corticosteroid is reduced. Thus, the risks of
either 5-lipoxygenase inhibitors or leukotriene receptor antagonists are relatively small when compared to their
therapeutic benet.
882 Asthma and Chronic Obstructive Pulmonary Disease
7.30.5 Current Treatment
Therapeutic approaches against asthma and COPD have been tailored to the severity of disease.
8,9
In all stages
of asthma, inhaled short-acting b
2
-agonists such as albuterol are recommended for quick relief from bronchospasms
on an as-needed basis (Table 3). Oral steroids such as triamcinolone may also be prescribed for acute relief. This
regimen is usually sufcient to treat mild intermittent asthma. In mild, moderate, and severe persistent stages, inhaled
corticosteroids (beclametasone) and long-acting b-agonists (salmeterol, formterol) are commonly prescribed for
daily use. Alternative approaches for mild and moderate persistent asthma include theophylline or leukotriene
modiers such as montelukast or zileuton. In some severe cases, systemic use of steroids such as prednisone has been
shown to be effective. For childhood and exercise-induced asthma, mast cell stabilizers such as nedocromil are
prescribed. An antibody against IgE, omalizumab (Xolair), has been demonstrated to be clinically effective on asthma
exacerbation rates, use of corticosteroids, and symptoms in both adults and children and was launched for use in the
USA in 2003.
95
In COPD smoking cessation is a primary objective for treatment as a long history of smoking is almost always linked
with developing the disease. The recommended therapy for those at Stage 0 (and also healthy individuals) is to avoid
risk factors such as tobacco smoke and other environmental pollutants (Table 4). Bronchodilators such as b2-agonists
are prescribed to patients in Stages I to III for symptomatic management of the disease. For Stage I bronchodilators are
recommended on an as-needed basis and for more advanced stages of COPD they are used regularly. Corticosteroids,
either inhaled or delivered orally, are recommended to patients with a spirometric response to the agent and/or are in
Table 3 Asthma severity and treatment
Severity Symptoms Pulmonary function
(PEF or FEV
1
)
Treatment
Mild, intermittent Attacks o1 per week, night-time
episodes infrequent
Decreased o20% Inhaled b
2
-agonist as needed
Mild, persistent Attacks 36 per week but o1 per
day, 42 night-time episodes
per month
Decreased o20% Inhaled b
2
-agonist as needed
Daily inhaled corticosteroid
or long-acting b
2
-agonist
Moderate, persistent Daily attacks, 45 night-time
episodes per month
Decreased 2040% Inhaled b
2
-agonist as needed
Daily inhaled corticosteroid
or long-acting b
2
-agonist
Severe, persistent Continuous attacks Decreased 440% Inhaled b
2
-agonist as needed
Daily inhaled corticosteroid
or long-acting b
2
-agonist
Table 4 COPD severity and treatment
Severity (stage) Pulmonary function (PEF or FEV
1
) Treatment
At risk (0) Normal spirometry but chronic cough and
sputum production
Avoid risk factors
Mild (I) Decreased o20% Inhaled b
2
-agonist as needed
Moderate (IIA) Decreased at least 20% but not more than 50% Inhaled b
2
-agonist regularly;
inhaled corticosteroid if effective
Moderate (IIB) Decreased at least 50% but not more than 70%
Severe (III) Decreased 470% Inhaled b
2
-agonist regularly
Inhaled corticosteroid if effective; oxygen
therapy; surgery
Asthma and Chronic Obstructive Pulmonary Disease 883
Stage II or III of the disease. However, corticosteroids are not effective in suppressing inammation in COPD
patients.
40
In severe (Stage III) COPD, long-term oxygen exposure to patients with respiratory failure is benecial but
surgical treatments such as bullectomy, lung volume reduction, or lung transplantation may have to be considered.
7.30.6 Unmet Medical Needs
As indicated in the previous section, current therapies for asthma and COPD are primarily directed at treating
the symptoms (e.g., b
2
-agonists for bronchoconstriction) rather than the disease. Treating symptoms has been generally
effective in the management of asthma, but not for a progressive disease like COPD. Even in asthma the use
of corticosteroids, especially in children, has risks associated with this general immunosuppressive agent. New
therapeutic approaches that target the immune mechanisms associated with the disease have shown clinical success
(zileuton, montekulast, etc.) and have initiated the search for new therapies targeting immune mechanisms in COPD
and asthma.
7.30.7 New Research Areas
7.30.7.1 Chemokine Receptor CCR3
The chemotactic cytokine (chemokine) eotaxin (CCL11), and its 7-transmembrane G protein-coupled receptor
(GPCR) CCR3 have been shown to be involved in modulating the trafcking of eosinophils to areas of allergen
challenge. While the ligand CCL11 is specic to its receptor target CCR3 has been shown to be quite promiscuous in
that at least 11 other endogenous ligands or their isoforms also exhibit afnity. Of the characterized allergy related
chemokine receptors,
9698
CCR3 has received the most attention due to a strong clinical observation that lung
disfunction correlates with the number of eosinophils that accumulate in the bronchioalveolar compartments,
specically in cases of bronchial asthma.
99,100
Although CCR3 is highly expressed on eosinophils (estimated to be 40 00050 000 sites per cell) it is also expressed
on basophils as well as a subset of T lymphocytes with Th2 properties. Additional supportive, benecial aspects of
modulating CCR3 pharmacology have been validated by a number of mechanisms. In the murine knockout models,
CCR3
/
animals have been shown to exhibit greatly attenuated recruitment of eosinophils to skin patches after
repeated sensitization with ovalbumin and exhibit decreased airway hyperresponsiveness to methacholine with 90%
reduction of cellular inux into the bronchioaveloar lavage after a single ovalbumin challenge.
101
Similar experiments
with CCL11
/
mice show a 70% reduction of relevant cellularity after challenge.
102
While several small-molecule
approaches will be reviewed within this section, it is worth mentioning that biologic approaches including one involving
monoclonal antibodies targeted at blocking ligandreceptor interactions have also been investigated. An example of a
murine antibody against CCL11 showed a reduction of in vivo eosinophil recruitment to the lung in response to
ovalbumin by 50%.
103
Again, much like the knockout studies, the corresponding receptor antibody 7B11 is able to block
second messenger Ca
2
ux and chemotaxis in human eosinophils in vitro.
104
Several small-molecule medicinal chemistry examples that demonstrate the relevance of CCR3 antagonism in
asthma models are presented. In addition to these illustrative examples, a recent, more comprehensive, chemotype
survey of the patent literature can be found in the review by Naya and Saeki.
105
High-throughput screening of corporate compound collections has lead to a variety of published pharmacophores
that effectively antagonize the CCR3 receptor and subsequent downstream signaling cascade. A nonselective
CCR1/CCR3 antagonist (1, CCR1 binding IC
50
0.9 mM versus CCR3 binding IC
50
0.6 mM) was identied and a
strategy based on a binding hypothesis to generate a focused combinatorial library that would incorporate cross receptor
selectivity SAR as developed.
106108
O
N
H
O N
+
Cl
Cl
H-bond acceptor
Electrostatic interaction/basic amine
Hydrophobic region
Hydrophobic region
1
884 Asthma and Chronic Obstructive Pulmonary Disease
This exercise subsequently generated a 770-member focused library that delivered the 2-(benzthiazole)thioace-
tamide (2) with good potency and 4800-fold improved selectivity. It is worth noting that 2 is also the rst reported
noncompetitive ligand described for CCR3 since binding IC
50
values did not increase predictably despite a 100-fold
increase in [
125
I]eotaxin concentration.
S
N
S
O
HN N
H
2
N
Cl
Cl
3,4-Cl optimal potency
and selectivity
2 Binding CCR3 IC
50
= 2.3 nM
Ca
2+
flux IC
50
= 27 nM
NH >> N-Me
S > O > SO >> SO
2
Region drives SAR
and selectivity
A variation of this chemotype advanced to rodent and nonhuman primate models of asthma. Analog 3 was evaluated
at 40 mg kg
1
(subcutaneous) in Cynomologus monkeys challenged with inhaled Ascaris pathogen resulting in a 50%
reduction of BAL eosinophils when compared to vehicle-treated animals.
109
N
OH
N
H
N
H
O
OMe
MeO
MeO
3 Binding IC
50
= 4 nM
Eosinophil chemotaxis IC
50
= 1.8 nM
Cl
In one lead optimization example, the structureactivity relationship (SAR) was explored with a synthesis strategy
focused on exploiting the fact that constrained variants of the piperidine ring can alter the spatial presentation of the
basic nitrogen which may interact with a key conserved glutamic acid residue located within the TM7 regional loop.
The bridged bicyclic analog 4 ultimately offered no potency increase over the parent piperidine derivative.
110
N
N
H
N
H
OH
O
OMe
MeO
MeO
Cl
4-Cl optimal potency and
lower plasma protein
binding versus 3,4-Cl
4 Binding IC
50
= 8 nM
Chemotaxis IC
50
= 2.4 nM
Poor in vivo PK profile
chair conformation favored SAR potency driver
The poor pharmacokinetic prole of 4 is driven by a combination of lipophilicity and a basic nitrogen that resulted in
a high volume of distribution and high clearance rate. This example also illustrates another important strategy typically
used in medicinal chemistry programs. Conformational restriction of rings or chains can often maintain target receptor
potency while assisting in improving selectivity over other off-target 7TM receptors, typically those in the central and
peripheral nervous system.
A common benzyl piperidine motif has emerged within various chemotypes reported to be selective antagonists of
CCR3. The bispiperidine series 5 was optimized using a systematic, iterative process coupled with library array
expansion where chemically feasible (amide formation).
Asthma and Chronic Obstructive Pulmonary Disease 885
N
N
O
N
Cl
Cl
HO
Library approach yielded
optimal heterocyclic system
3,4-Cl > 2,4-Cl > 2,5-Cl
4-Br > F > Cl >> OMe
cis >> trans substitution
R,R-Enantiomer preferred
CH
2
OH = OMe > OMe >> CH
2
NHCOMe
H, Me, Et, CH
2
=CH
2
, CH
2
F = c. 1540 nM
5 Binding IC
50
= 3.5 nM
Ca
2+
flux IC
50
= 9 nM
Eosinophil chemotaxis IC
50
= 160 nM
Overall the series showed good chemokine receptor cross-selectivity with only 11% inhibition and 8% inhibition of
CCR4 and CCR8 at 1 mM, respectively. It is important to note that while 5 maintained good afnity for the human and
monkey CCR3 receptors (K
i
3.3 and 7.2 nM) much lower afnity for the rodent receptors (rat K
i
2981 nM; mouse
K
i
606 nM) is seen. This problem of species selectivity is not atypical and often hinders many GPCR optimization
efforts providing signicant challenges with in vivo proling. As a nal point, this series was also hindered by an
undesired 85% (1 mM) hERG inhibition as measured in a voltage clamp assay.
111
Within the lead optimization strategy for this chemical series the orientation of the bispiperidine ring system was
reversed as shown below (6). The SAR indicated that the central pharmacophore could indeed be reversed and
reasonable CCR3 afnity could be maintained. Movement of the amide moiety to the 3-position of the reversed
piperidine followed by repositioning of the amide atom array provided an initial 60 nM inhibitor as measured in the
binding assay. The requirement for a 3,4-dichloro substituted benzyl group was conrmed and, based on a survey of
various CCR3 active chemotypes, this motif appears to provide an optimal binding interaction with a putative lipophilic
region of the receptor. Further SAR exploration yielded an unexpected surprise, that is, while competitive inhibition of
CCL11 binding was maintained, the functional activity (using a [
35
S]GTPgS binding assay)
112
reversed to that of an
agonist as illustrated by analogs 7 versus 8.
N
N
Cl
Cl
N
*
H
N
O
N
H
N
O
N
H
N
360 nM
*
Ar Ar
162 nM
Ar
O
60 nM
N
H
O
N
6 Binding IC
50
= 23 nM
Ca
2+
flux IC
50
= 215 nM
BAF3 chemotaxis IC
50
= 136
Poor rat PK (AUC iv)
*
N
N
H
N
O
N
Cl
Cl
Me
7 Antagonist activity
Binding K
i
= 50 nM
E
max
%(GTP S) = 8%
N
N
H
N
O
N
Cl
Cl
Me
8 Agonist activity
Binding K
i
= 7.3 nM
E
max
%(GTP S) = 96%
886 Asthma and Chronic Obstructive Pulmonary Disease
Similar reversal in functional activity has also been seen in another chemotype. During the investigation and
optimization of a series of pyrrolidinohydroquinazolines, analog 9 was identied as an antagonist with promising
potency. Further exploration furnished analog 10 with improved binding; however, agonist activity was conferred.
113
N
N
Br
9 Functional antagonist
Binding K
i
= 90 nM
H
H > Et > n-Bu >> Ph
2-substitution optimal
Br > Cl >> F, CF
3
= Et > Ph > OEt
N
N
Br
N
10 Functional agonist
Binding K
i
= 28 nM
H
H > Me >> CN
Another series of potent analogs containing benzylpiperidine and urea moieties illustrate clever SAR analog
strategies that allowed for the optimization of CCR3 potency, target selectivity over neuroreceptors, and
pharmacokinetic properties.
114117
In an iterative sequence the HTS hits represented by 11a, b were converted to
the corresponding urea linked analog 12 based upon a competitive analysis of the chemotype/target literature.
Subsequent recognition of a latent benzylpiperidine (bold lines in 11a) furnished the lead analog 13.
N
N
F
H
H
HTS hit
Binding IC
50
= 500 nM
N
N
H
H
O
F
11a
11b
HTS hit
Binding IC
50
= 1M
N
N N
H
N
H
H
H
O
CN
Binding IC
50
= 700 nM
12
N N
H
N
H
O
CN
Binding IC
50
= 200 nM
13
Structural changes in the piperidine functionality and continued exploration of aromatic substitution improved the
selectivity of the antagonists for CCR3 and drove potency to the picomolar range (14).
H
N
H
N
O
N
N
N
N
N
H
Optimized chain lengths shown
3-Piperidine substitution optimal
Piperidine 4-substitution tolerated
gem-Me > i-Pr, Et, Me > CF
3
, Ph
S-enantiomer threefold > R-enantiomer
4-F, 3-Cl > 2,4 and 3,4-di Cl, di F> Me, 3-F >>CF
3
, OMe, NMe
2
F
4
14 Binding IC
50
= 0.7 nM
Ca
2+
flux IC
50
= 27 nM
Chemotaxis = 51% I at 30 nM
Asthma and Chronic Obstructive Pulmonary Disease 887
The search for improved receptor selectivity continued with SAR exploration of the linker region, chain lengths, and
aromatic substitution, as well as identication of the optimal diastereomeric isomer which ultimately lead to analog 15
which proceeded to phase I clinical studies.
F
N
Binding CHO IC
50
=2 nM
Binding hEos IC
50
= 800 pM
Ca
2+
flux IC
50
= 8 nM
Eosinophil chemotaxis IC
50
= 34 pM
Selective over D2 and 5HT2a,2c
Murine F% = 20
Cyno F% = 8
Chimp F% = 22
t
1/2
= 25h
CL = 1.22 (L/h)/kg
Protein binding = 96%
OVA challenge: 50% 30 mpk, 86%
100 mpk po
HN
N
H
O
O
15 DPC-168 / BMS-639623
Although a detailed account of the discovery and SAR surrounding a second clinical candidate has not yet been
disclosed, the pharmacophore elements of the urea linkage and the 3,4-dichloro substituted benzylpiperidine has been
translated to the novel morpholine analog 16 as disclosed in a series of nine patent applications.
118
H
2
N
O
N
H
N
H
O
O
N
Cl
Cl
16 GSK-766994
Phase II clinical candidate for
asthma and allergic rhinitis
In conclusion, there is strong supportive evidence linking eosinophil recruitment and activation in the lung tissue
with asthma. Recently CCR3 has become a popular target and the landscape is very competitive. Given the lack of
crystal-based structural information to guide SAR development, computational approaches to ligand design are emerging
as exemplied by a ve-dimensional quantitative SAR (5D-QSAR) model.
119
Several excellent reviews exist that more
fully survey the breadth of patent literature.
105
It is also known that eosinophil trafcking is not an exclusively CCR3
mediated event and the clinical trials will determine whether CCR3 antagonists will achieve therapeutic potential.
7.30.7.2 CRTH2 and the DP-1 Receptor
The prostaglandin D
2
(PGD
2
) is the predominant prostanoid produced by allergen activated mast cells and it mediates
its effects as an agonist ligand for two different 7TM-GPCR receptors, DP-1 (45 nM) and CRTH2 (61 nM;
chemoattractant receptor-homologous molecule expressed on T cells, has also been named DP-2) (see Figure 4).
120
PGD
2
, along with a host of arachadonic acid derived prostanoid agonists, are inammatory mediators responsible for a host
of events including bronchoconstriction mediated by contraction of smooth muscle. CRTH2 is expressed on and
mediates chemotactic responses of eosinophils, basophils, and Th2 cells and plays a role in inducing eosinophil
degranulation thus, it stands to reason that activation of this receptor by PGD
2
may play a key role in modulating
inammatory response (Figure 4). CRTH2 is coupled with a Gai-type G protein and is thought to be involved in post-
PGD
2
stimulatory activities such as induction of cell migration and upregulation of adhesion molecules.
121,122
Research
targeting small-molecule mediators of the CRTH2 receptor is a relatively new eld. Although no clinical therapeutics
have yet emerged a number of intriguing small-molecule probes have been discovered. Recently, it has been shown that
the nonsteroidal anti-inammatory indomethacin (17) has afnity for the receptor. In the course of identifying PGD
2
as
the sole CRTH2 ligand produced by mast cells, indomethacin (a lipoxygenase inhibitor) was used to suppress PGD
2
production. It was unexpectedly found that 17 exhibited an agonistic effect thus activating the cells toward migration.
123
This observation is clinically signicant because it demonstrates that a widely utilized COX inhibitor can stimulate rather
than inhibit a chemotactic receptor leading to undesired migration of leukocytes at therapeutic blood levels.
888 Asthma and Chronic Obstructive Pulmonary Disease
N
OH
O
S
Cl
F
S >> CH
2
by 45-fold
S-enantiomer >> R-enantiomer
Drives selectivity over DP receptor
Carbocycle: 5 > 6-member ring
N
MeO
O
OH
O
Cl
17 Indomethacin
Binding IC
50
= 25 nM
Methyl ester inactive at CRTH2
18 Binding IC
50
= 0.8 nM
Selective
Full agonist based on substitution of PGD
2
Stimulated chemotaxis of eosinophils at 100 nM
Indomethacin
NSAIDs
PGD
2
BW245C
DP CRTH2
Eotaxins,
RANTES,
MCPs
CCR3
Ligands
Cell membrane
G proteins
Signaling
pathways
Responses
Direct and
indirect actions
Anti-inflammatory actions
predominantly via inhibition of COX
isoenzymes, however also
modulation of ATP levels and
induction of L-selection shedding
(neutrophils), inhibition of pro-
inflammatory gene transcription
DK-PGD
2
G
i
G
q
G
G
S
G
cAMP
G
i
G
q
G
Small GTP
binding proteins
COX-1, COX-2,
NF-kB, MAP
kinases
?
Ca
2+
PLC
MAPKs, ERK, JNK
PI-3kinase
Chemotaxis, respiratory burst,
shape change/actin re-organization, adhesion
molecule expression
Figure 4 Proposed signaling pathways for the CCR3 and CRTH2 receptors. (Reproduced with permission fromStubbs, V. E. L.
et al. J. Biol. Chem. 2002, 277, 26012 & American Society for Biochemistry & Molecular Biology.)
Asthma and Chronic Obstructive Pulmonary Disease 889
In order to understand the in vivo role of this receptor, a potent and highly selective agonist ligand for CRTH2 was
derived from manipulation of the core indole acetic acid moiety of indomethacin.
124,125
Analog 18 exhibited nearly
complete selectivity for CRTH2 over all other prostaniod receptors and the (S)-conguration at the chiral center was
pivotal for selectivity over DP-1, in which activity is conferred with the corresponding (R)-enantiomer. The analog has
excellent pharmacokinetic properties with bioavailability of 48% and should prove useful for in vivo mechanistic
studies.
The structurally related analog ramatroban (19) is one of the rst reported CRTH2 antagonists. It is cur-
rently marketed in Japan for treatment of allergic rhinitis and has been characterized as a selective TP anta-
gonist (thromboxane A
2
receptor).
126
The drug candidate is currently in phase III clinical trials for treatment of
asthma.
127,128
N
CO
2
H
HN
S
F
O
O
19 ramatroban
Antagonist activity
CRTH2 binding IC
50
= 100 nM
Ca
2+
flux IC
50
= 30 nM
During further mechanistic characterization it was discovered that 19 is also an antagonist of CRTH2 (measured
against
3
H-PGD
2
) suggesting its clinical efcacy may in part be through its modulation of chemotaxis. Further
synthesis and optimization of the ramatroban scaffold has furnished a series of isosteric analogs highlighted by 20.
Reversal of the scaffold substituents and subsequent optimization of both aromatic substitution and chain length
between the acid functional group and the indole nitrogen provided an antagonist 400-fold more selective for CRTH2
versus the TP receptor.
129
N
NH
CO
2
R
S
F
SO
2
linker required >> CH
2
>> CO = C(O)NH
4-F most potent substituent
Acetate > propionate >> benzoate
Alkyl substitution ablates activity
Substitution tolerated
Me > Ph >> t-Bu
Stereochemistry not addressed
Ring size may be varried (7 = 6 >> 5-member)
20 Binding HEK293 K
i
= 13 nM
Ca
2+
flux IC
50
= 9.7 nM
Selective over TP
O
O
It has also been shown that subtle manipulation of the ramatroban scaffold can greatly shift the selectivity prole
leading to complete loss of activity at the TP and DP-1 receptors. N-Methylation of the sulfonamide in combination
with shortening the acidic side chain furnished 21 as a highly potent antagonist. The antagonist prole included an
assessment of inositol phosphate, cAMP signaling second messenger functional activity and inhibition of agonist
mediated b-arrestin translocation.
890 Asthma and Chronic Obstructive Pulmonary Disease
N
CO
2
H
N
S
F
Selectivity Me >> H
Chain length alters selectivity
and potency(one methylene optimal)
Stereochemistry not defined
21 hCRTH2 binding IC
50
= 600 pM
Inositol phosphate IC
50
= 1.2 nM
-arrestin trans IC
50
= 3 nM
O
O
The analogs were prepared as racemates and resolution was not accomplished since the intent was to use 21 as a
mechanistic biochemical tool.
130
Additional chemotypes centering on indole, quinoline, and carbazole derivatives have
been reported in the patent literature
131
indicating intense competition in seeking a clinically relevant CRTH2
antagonist within a narrow privileged chemotype.
Given the PGD
2
ligand relationship between CRTH2 and DP-1, it is appropriate to bin discussion of these two
receptors together even though they do not share signicant sequence homology. It is important to remember that
even though these 7TM-GPCR receptors share a common ligand, DP-1 belongs to the prostaniod receptor family
(G
as
-coupled signaling) and CRTH2 is a member of the chemokine receptor family thus differentiating physiological
functional roles. As well, DP-1 is primarily expressed on smooth muscle and epithelial cells while CRTH2 is expressed
primarily on Tcells, basophils, and eosinophils. The development of novel antagonists in this area has been slow and
only few reports on the efcacy of DP-1 receptor antagonists in asthma models or against human disease are
available.
132
Most frequently reviewed is the hydantoin prostaniod mimetic 22 which exhibits moderate competitive
binding but is shown to be a partial agonist in functional assays.
133
O
OH
CO
2
H
OH
PGD2 DP-receptor binding K
i
= 21 nM
N
N
O
O
N
H
CO
2
H
HO
22 BW A868C
Binding K
i
= 220 nM
One approach to analog generation has been to exploit receptor class cross-reactivity and develop new chemical
entities from prostaglandin scaffolds. In this case, the bicyclo[2.2.1]heptane ring system,
134
as shown in analog 23, and
the bicyclo[3.1.1]heptane system
135
24 has provided a new class of antagonists originating from a thromboxane A
2
hit in
high-throughput screening. Based on observations in past programs, both series of analogs were optimized with a focus
on the o-chain that seemed most important for PGD
2
activity (versus other family receptors). This included the
incorporation and extensive SAR of aromatic moieties linked with a proper spacer. Ultimately the dibenzofuran
derivative 23 was selected as the ( ) enantiomer because of its selectivity prole.
NH
CO
2
H
S
O
O
O
OMe
23 Binding IC
50
= 24 nM
Functional cAMP IC
50
= 52 nM
NH
CO
2
H
O
S
OH
24 (S-5751) Binding IC
50
= 1.9 nM
Functional cAMP IC
50
= 0.9 nM
In general, the sulfonamide moiety was observed to be critical and it was suggested that the sulfonamide NH
mimicked the C15 hydroxyl proton of PGD
2
. Analog 23 was subsequently taken in vivo and exhibited 42% inhibition,
based on airway resistance, in the guinea pig asthma model at 10 mg kg
1
(orally). In a similar manner an alternate
Asthma and Chronic Obstructive Pulmonary Disease 891
ring structure was optimized to provide 24 after a stereochemical SAR study indicated the (1R,2R,3S,5S)-isomer
exhibited optimal potency. Next, the sulfonamide of 23 was substituted with the simpler amide linker. Subsequent
optimization of the heterocycle and substituents furnished an analog with good in vivo efcacy in the guinea pig asthma
model (70% inhibition at 10 mg kg
1
, orally). This analog is currently considered a promising clinical candidate, now in
development.
Several other pharmacophore cores have also emerged. In a hit-to-lead exercise, chemical manipulation of the anti-
inammatory indomethacin has furnished an indole-based chemotype that is currently under investigation. Iterative
synthesis and SAR at each substituent on indomethacin lead increased afnity for the DP-1 receptor with selectivity
over the EP subset. Potency seemed to have peaked until the acetic acid moiety was transferred from the indole C3
position to C4 providing analog 25 with an optimal substitution pattern.
136
N
MeO
O
Cl
CO
2
H
Indomethacin
DP binding IC
50
= >10 M
N
MeO
O
R
n( )
CO
2
H
R
N
O
25 Binding IC
50
= 300 nM
CO
2
H
O
O-Bu: para > meta >> ortho
Me >> H, Et
n = 3 > 1,2 > 4 >> 0
With the lead structure 25 identied, optimization continued through exploration of the indole nitrogen
substituent.
137
Employing a resin-based parallel synthesis approach, the para-alkoxy substitution was evaluated. A
series of chain and aryl ring substituents were prepared and the SAR data lead to the N-methylbenzomorpholine 26,
specically the (S)-stereoisomer.
N
O
CO
2
H
O
N
O
26 Human DP binding IC
50
= 2.1 nM
Murine DP binding IC
50
= 18 nM
A pharmacokinetic study demonstrated that 26 had good oral bioavailability (48% at 10 mg kg
1
), long t
1/2
(8 h), and
moderate clearance with good tissue distribution. Efcacy in an asthma model has not been reported however
suppression of allergic inammatory response was demonstrated in an ovalbumin (OVA)-induced increase of vascular
permeability in guinea pig conjunctiva.
In another chemotype derived from ramatroban, the development candidate 27 demonstrated exquisite PGD
2
binding inhibition potency at the DP-1 receptor.
138
The analog is reported to be relatively nonselective inhibiting TXA
2
at 11 nM and CRTH2 at 910 nM (note similarity to analog 18).
F
SO
2
Me
N
Cl
CO
2
H
27 Merck L-888839
DP binding K
i
= 0.07 nM
CRTH2 binding K
i
= 910 nM
892 Asthma and Chronic Obstructive Pulmonary Disease
In the sheep asthma model, 27 demonstrated efcacy with 33% inhibition of early phase and 74% inhibition of late
phase bronchoconstriction at 3 mg kg
1
. Also discovered as a result of a high-throughput screening campaign was the
structurally related N-benzyl benzimidazole analog 28. To explore the SAR the key 4-chloro-N-benzyl moiety was
retained and a systematic survey of aromatic substitution and linkers at the 2-position were probed, ultimately
furnishing the selective lead 29.
139
N
N
Cl
S
28 DP binding K
i
= 73 nM
TP binding K
i
= 9 M
N
N
Cl
CO
2
Me
4-substitution optimal
CO
2
Me = methyl oxadiazole > COMe >
CONMe
2
> SO
2
NH
2
> CO
2
H > H
CO
2
Me
CH
2
> S > S=O > NH
29 DP binding K
i
= 38 nM
TP binding K
i
= >75 M
In summary, it is clear that the anti-inammatory indomethacin (as a CRTH2 agonist) and ramatroban (a TXA
2
antagonist with similar activity in CRTH2) have played a pivotal role in dening a general pharmacophoric elements for
two functionally different GPCRs sharing a common, prostaniod ligand. As well, structurally diverse prostaglandin
mimetics provide an additional pharmacophore apparently unique to the DP-1 receptor. A number of interesting small-
molecule probes with both agonist and antagonist activity have been developed. This may lead to future discovery of
yet unknown prostaniod receptors that have evolved with differential functional activity.
7.30.7.3 Phosphodiesterase Type 4
The development of PDE4 inhibitors has been an active area of research for over 10 years now. These inhibitors act by
increasing intracellular concentrations of cyclic AMP (by inhibiting degradation) resulting in a broad range of anti-
inammatory effects, driven by reduction of TNF-a production, on various effector cells involved in both asthma and
COPD. As well, increased cAMP levels have also been shown to relax airway smooth muscle. Although the
phosphodiesterase family consists of 11 subtypes they differ in primary sequence, substrate specicity, and cofactor
requirements with PDE4 being the isozyme abundantly expressed across lymphocytes. During past decade, and
especially in the past 5 years, a series of rst- and second-generation compounds have progressed to the clinic.
140,141
Development has been slowed due to basic pharmacology issues that lead to a narrow therapeutic index over side
effects. The rst in class analog, rolipram (30) has a propensity to induce nausea and vomiting at therapeutic doses.
142
Rolipram has proven to be an excellent research tool and further hypotheses of rening the therapeutic window over
side effects have been generated. Initial attention focused on the rolipram binding site, which, besides being a catalytic
binding site, is believed to exist in two non- or slowly interconvertible conformations, exhibiting either a high and low
binding afnity state for 30.
143
Modulation of PDE4
high
, which is believed to be generally expressed in the central
nervous system, produces the adverse effect of emesis, while inhibition of the PDE4
low
afnity state has been
associated with favorable anti-inammatory activity. With this hypothesis, the design of the second-generation
inhibitors such as rofumilast (Daxas, 31)
144
and cilomilast (Ario, 32)
145,146
have shown better efcacy and therapeutic
potential in the clinic.
To date, the sole hypothesis of high versus low afnity receptor states has come under question especially since
cDNA has been identied for isoforms of PDE4 leading to four distinct PDE4 subtypes. All four PDE4 sybtypes have
the same general structure, especially in the catalytic domain. Regions N-terminal to the conserved catalytic domain
show the subtype variability and are believed to be involved in regulation of the catalytic activity and intracellular
targeting. A therapeutic hypothesis has emerged that is founded on subtype selectivity. The data is still controversial
but the common belief is that selectivity for either subtype-PDE4b or PDE4d can lead to an improved clinical prole
over side effects.
147,148
It has been shown that analog 32 which has 10-fold selectivity for PDE4d is better tolerated and
this may support the hypothesis that selectivity for subtype-PDE4d can contribute to improved clinical tolerance.
Asthma and Chronic Obstructive Pulmonary Disease 893
Whether the strategy of specically targeting subtype-PDE4b over PDE4d, or in combination with selectivity toward
low versus high afnity states, will help achieve an ideal therapeutic ratio for future analogs remains to be seen. There
is also an emerging third strategic component, that is, dual inhibition of a second PDE gene family isozyme along with
PDE4. Preliminary investigations indicate that addition of a PDE3 inhibitor, motapizone (in vitro) provides functional
synergy as measured by TNF-a inhibition in macrophages.
149
O
MeO
NH
O
30 Rolipram (Schering)
PDE4
lo
IC
50
= 300 nM
PDE4
hi
IC
50
= 5 nM
PDE4a IC
50
= 67 nM
PDE4b IC
50
= 220 nM
PDE4c IC
50
= 1250 nM
PDE4d IC
50
= 79 nM
CHF
2
O
O
N
H
O
N
Cl
Cl
31 Roflumilast (Altana)
PDE4 IC
50
= 0.8 nM
10-fold more potent in PDE4c
Reported to exhibit no other
subtype selectivity
32 Cilomilast (GSK)
PDE4
lo
IC
50
= 95 nM
PDE4
hi
IC
50
= 120 nM
PDE4a IC
50
= 160 nM
PDE4b IC
50
= 120 nM
PDE4c IC
50
= 8700 nM
PDE4d IC
50
= 13 nM
O
MeO
NC
CO
2
H
There has also been an ongoing and aggressive research effort which has identied a number of new chemotypes still
under investigation. To emphasize the point over 450 patents applications targeting PDE4 have been published in just
under the past 10 years. An analysis of the medicinal chemistry literature reveals several medicinal chemistry synthesis
strategies that have provided fruitful analog classes. A wealth of rolipram-like carbachol derivatives have been reported.
An excellent example is analog 33,
150
which was dropped from development due to lack of efcacy at a dose that did
not result in emesis. Good to potent catalytic site PDE4 inhibition is seen with 34 as well as a conformationally
constrained oxindole variant 35
151
which are selective for the low-afnity binding state. It is interesting to note that
removal of the oxindole fused phenyl ring in 35 increases potency (PDE4
lo
IC
50
6.3 nM); however, selectivity is lost
for the high-afnity binding site (PDE4
hi
IC
50
7.5 nM).
34 CDP 840 (Celltech)
PDE4
lo
IC
50
= 4.5 nM
MeO
O
N
MeO
O
NH
O
N
35 PDE4
lo
IC
50
= 400 nM
H > Bz > BOC > SO
2
Ph
3> 2 = 4-pyridyl >
N-oxide = Ph
MeO
O
N
H
O
N
Cl
Cl
33 Piclamilast (RPR/Aventis)
PDE4
lo
IC
50
= 1 nM
In the quest to reduce compound afnity for the [
3
H]rolipram high-afnity binding site, another series of oxindoles
were derived. Analog 36 also strategically substitutes the rolipram pyrrolidone ring with a similar oxindole motif followed
by SAR exploration of the phenyl substitution.
152
Extensive SAR did not allow for any correlation between the high- and
low-afnity sites and it was found that electron withdrawing substituents in the 5-position of the oxindole phenyl ring
were favored along with the Z-conguration at the alkene linker. Nothing larger then N-methyl was tolerated.
In another variant, a benzimidazole ring analog 37 was used to provide a proposed key hydrogen-binding motif at the
catalytic site.
153
This substitution allowed for inhibition potencies in the nanomolar range. Considerable potency was
afforded through the installation of an indanyl group and acceptable in vivo activity was seen in an antigen induces
airway obstruction model (78% inhibition at 10 mg kg
1
).
894 Asthma and Chronic Obstructive Pulmonary Disease
MeO
O
HN
N
CO
2
H
37 PDE4
lo
IC
50
= 2 nM
PDE4
hi
IC
50
= 32 nM
MeO
O
HN
O
36 PDE4
lo
IC
50
= 1.2 M
PDE4
hi
IC
50
= 62 M
NO
2
NO
2
> Br > Cl > H
Using CDP-840 (34) as a scaffold, continued SAR exploration to improve the overall prole has identied analog
series 38 as potential development candidates.
154156
Initial analogs with the ideal in vitro prole exhibited excessive
in vivo half-life due to the metabolically resistant bis(triuoromethyl) phenylcarbinol moiety (38a).
O
F
2
HCO
N
N
S
CF
3
HO
CF
3
O
OCHF
2
F
2
HCO
N
X
O
HO R
2
R
1
38a L-791943: R
1
, R
2
= CF
3
, R
3
= H, X = CH
PDE4A IC
50
= 4.2 nM
Rat t
1/2
= > 24h
38b L-826141: R
1
, R
2
= CF
3
, R
3
= Me, X = CH
PDE4A IC
50
= 1.3 nM
Rat t
1/2
= 10 h
38c R
1
= Me, R
2
= Ph, R
3
= H, X = N
PDE4A IC
50
= 2 nM
Rat t
1/2
= 1.5 h
R
3
39 L-869298
PDE4A IC
50
= 0.5 nM
Further optimization improved the pharmacokinetic properties to provide 38b; however, when cardiovascular
pharmacology studies were conducted on a related analog (38c), a signicant QTc interval prolongation was observed at
3 mg kg
1
in dogs. A second round of renement ultimately furnished 39, which not only further improved potency but
exhibited a reduced binding to the hERG channel (K
i
61 mM).
157
The analog exhibited human whole blood
inhibition of TNF-a potency of 90 nM and was efcacious in the Acaris-induced bronchoconstriction model in sheep
(68%/92% early/late at 0.5 mg kg
1
).
Additional novel analogs have been produced through the evolution of the rolipram pyrrolidone moiety. Although
the substituted catechol fragment has been retained, analogs 40, 41, and 42 illustrate the expanded scope of hetero-
and carbocyclic fragments that provide varied activity proles.
40 PDE4 IC
50
= 5 nM
MeO
OMe
N
N O
MeO
O
NC
H
H CO
2
H
41 PDE4
lo
IC
50
= 9 nM
MeO
O
N
NH
N
42 PDE4B IC
50
= 19 nM
Me
CN
Asthma and Chronic Obstructive Pulmonary Disease 895
Besides potent enzyme inhibition the racemic variant of the hexahydrophthalazinone 40 also demonstrated in vivo
efcacy.
158,159
Further study and diastereomeric resolution identied the ( )-isomer as the desired isomer offering
250-fold increase in potency. A second strategy was investigated with this scaffold using a combinatorial library/docking
approach. The report is informative as it captures the modern concept of technology-driven synthesis using a scaffold-
linker-functional group approach to lead nding.
160
Building on the scaffold of cilomilast (32), further exploration of
the spatial arrangement of the key pharmacophores (carboxy, nitrile, and carbachol moieties) furnished 41 which was
equipotent with 32 but demonstrated enhanced inhibition of TNF-a (0.4 versus 1.7 mg kg
1
, orally, respectively).
161
A novel series of imidazol-2-one based derivatives such as 42 have also been described.
162
Potent PDE4 inhibitors were
found and the corresponding 2-cyanoimino moiety of the (S)-isomer was shown to greatly inhibit gastrointestinal side
effects and lower afnity for PDE4
hi
over rolipram.
The 3-methoxy-4-cyclopentoxycarbachol motif has gradually given way to additional heterocyclic variants. The
indole isostere 43 is one of the rst reported carbachol variants.
163165
The initial SAR was analogous to that for
rolipram, and an earlier analog 33, as exhibited by the trend for lipophilic substituents on the heterocyclic system.
Another variant, 44, was nearly equipotent for both the high- and low-afnity binding states supporting the
pharmacophore relationship to the parent rolipram.
166
43 PDE4
lo
IC
50
= 30 nM
PDE4
hi
K
i
= 86 nM
ED
50
in vivo TNF- release = 7 mg kg
1
H
N
O N
Cl
Cl O
N
O
H
N
N
Cl
Cl
MeO
NH
N
44 PDE4
lo
IC
50
= 45 nM
PDE4
hi
K
i
= 45 nM
O
NH favored over N-Me
Lipophilic SAR
O
In another example, phthalazine analog 45 further challenges the carbachol substitution by taking advantage of
the 4-position of the phthalazine ring.
167169
The ring constrained design strategy was based on replacement of the
carbonyl functionality with a p-bond of an aromatic ring. A new structural series has been identied based on
the benzodiazepine ring system.
170172
Analog 46 demonstrated submicromolar activity with good selectivity as well as
in vivo inhibition of TNF-a production.
45 PDE4
lo
IC
50
= 4 nM
PDE4
hi
K
i
= 17 nM
TNF- release IC
50
= 3 nM
N
N
MeO
N
Cl
Cl
N S
O
N
N
O
NH
H
2
N
O N
46 PDE4 U937 cell IC
50
= 270 nM
PDE 1,3,5 IC
50
= > 100 M
In summary, a large scope of structurally diverse compounds have been identied that demonstrate acceptable
activity in preclinical animal asthma models. A void in the medicinal chemistry literature exists for analogs based on the
weak, nonselective inhibitor theophylline with only a few new micromolar leads being reported. The primary basis for
design has been the prototypical inhibitor rolipram where many strategies for modifying the pyrrolidone, carbachol, or
both fragments have proven fruitful in the quest for a selective inhibitor with attenuated (but not eliminated) side
effects. The development of a third generation of analogs using these structural clues
173,174
will be coupled with a
greater structural understanding of enzyme isoforms and afnity states although the role and selectivity for PDE4b
896 Asthma and Chronic Obstructive Pulmonary Disease
versus PDE4d remains to be resolved. Given the high value of the target, new screening strategies are being employed
such as fragment based x-ray identication of alternate pharmacophores.
175
The ultimate clinical outlook is
encouraging as demonstrated by several advanced phase II and III candidates with improved therapeutic windows over
undesired emesis as a side effect.
7.30.7.4 Mast Cell Tryptase and Chymase
Mast cells are highly granulated cells found in connective tissues at maturity and are important modulators of various
inammatory conditions, most importantly, allergic reactions that trigger asthma. A major component of mast cells are
serine proteases that comprises up to 2030% of the total protein mass. Specic protease activity has been clearly
demonstrated to play a key role in pulmonary inammation and allergic disease. One target of recent interest is
b-tryptase which is classied as a serine protease which is found almost exclusively in mast cells.
176
Several additional
isoforms have been identied resulting in a family size of ve to date, with b-tryptase being in high relative abundance
in mast cells. The crystal structure has been solved at high resolution (1.77 A
) revealing a ringlike homotetrameric
species with the active site facing a central pore.
177,178
Loss off enzymatic activity is believed to occur through a
spontaneous inactivation/dissociation process and there has been some controversy as to the physiological conditions
that cause this and the role of heparin in stabilizing the tetrameric form.
179,180
It is worth noting that each subunit is
believed to have catalytic activity and these active sites are located within the central cavity and have limited steric
accessibility. This structural feature apparently limits the substrate selectivity toward small peptides (or
peptidomimetics) or peptide loops/chains that be projected to the catalytic site. The intense interest to develop a
therapeutic agent is driven primarily by a decade worth of data derived from in vitro and in vivo experiments that
suggest a proinammatory role for this enzyme specically in the pathophysiology of asthma.
181
Consistent with mast
cell degranulation products exhibiting a causative effect, several therapeutic approaches to inhibit mast cell activation
have already demonstrated clinical utility. For example, mast cell stabilizers such as sodium cromoglycate and anti-IgE
therapy have been effective.
Release of tryptase upon mast cell degranulation, in parallel with histamine, PGD
2
, and LTC
4
, triggers airway
bronchoconstriction and hyperresponsivness and may have a role in brosis and thus airway remodeling. This is
validated in animal models; tryptase increases airway hyperresponsivness and induces a cellular inammatory inltrate
characteristic to human asthma.
182
Tryptase released from mast cells after allergen cross-linking can stimulate
neighboring mast cells resulting in amplication of the degranulation process. Cellular activation is then mediated
through proteolytic cleavage of the N-terminus chain of the 7TM-GPCR receptor PAR-2, located on smooth muscle,
epithelial cells, and leukocytes. PAR-2 activation is dependant on this proteolysis since it unmasks the N-terminal
tethered peptide ligand sequence (SLIGKV) which binds to the extracellular loop 2 initiating signal transduction.
Evidence for PAR-2s role in inammation is supported by the mouse knockout that was shown to have reduced airway
inammation following antigen challenge.
183
The strategy for designing therapeutic inhibitors of tryptase centers on three approaches, which are classied as
monofunctional or bifunctional inhibitors (these classes are also referred to as monobasic and dibasic inhibitors) and
tetramer disruption. The clinical candidate 47 represents the concept of a monofunctional inhibitor.
184
This analog
proceeded to phase II trials at which point it was discontinued most likely due to off-target effects based on lack of
compound selectivity against thrombin and trypsin.
185
47 Clinical candidate APC-366
Tryptase K
i
= 330 nM
Trypsin K
i
= 162 nM
N
H
O
NH
O
N
NH
2
O
OH
NH
2
HN
48 BABIM
Tryptase K
i
= 2 nM
Trypsin K
i
= 17 nM
N
H
N
NH
H
2
N
N
NH
NH
2
NH
The peptide analog was demonstrated to bind to each enzyme subunit in a 4:1 stoichiometry using a key salt bridge
between the arginine side chain and Asp 189 at the base of the subunits P1 pocket. This is accomplished in an
Asthma and Chronic Obstructive Pulmonary Disease 897
irreversible manner believed to be driven by serine addition to an activated form of the hydroxyl naphthalene moiety.
Another prototypical monobasic inhibitor is represented by analog 48. Again, the amidine moiety plays a key role as a
guanidine isostere at the P1 pocket and although this potent molecule behaves in a reversible manner, it is not selective
for the target.
186
The guanidine/amidine motif is prevalent across a wide variety of inhibitor series as is the peptidic
nature of the scaffold. Analog 49 illustrates these features and is an example of a chemotype with greatly improved
selectivity over that of BABIM. Analogs 50 and 51 further illustrate scaffolds that adequately present an essential lysine
or arginine-like residue to the enzyme. In particular, 51 demonstrated efcacy in vivo in a sheep model on antigen-
induced asthmatic response with 7075% blockade of the early response and complete ablation of the late response and
airway hyperresponsiveness.
187,188
49 Tryptase K
i
= 6 nM
Trypsin K
i
= > 6000 nM
N
H
N
O
N
H
N
NH
NH
2
50 Tryptase K
i
= 6 nM
N
N
O
S
O
O
H
2
N
NH
O
NH
51 Tryptase K
i
= 10 nM
N
O
HO
O
NH
O
S
N
NH
2
HN
HN
HN
O
O
NH
N
H
H
N
O
O
N
O
O
H
N
O
HN
HN NH
2
OH
OH
O
52 Tryptase K
i
= 5 nM
The screening of natural product extracts has provided a macrocyclic peptide from the marine sponge of the genus
Ircinia. Cyclotheonamide E4 (52) is potent inhibitor of tryptase with marginal selectivity over trypsin and thrombin.
189
A proven drug design strategy is illustrated in the atypical (nonbasic) analog 53 where the electrophilic saccharin
moiety is targeted in a time-dependent manner by an active site serine, thus becoming covalently bound to the enzyme
in a reversible manner.
190
S
N
O
O
O
O
O
53 Tryptase IC
50
= 64 nM
N
H
O
O
S
N
O
O
O
O
O
R
S
NH
O
O R
O
Ser195
O
S
N
O
Ser195
O
S
N
O
Ser195
O
His57
O O
O O
O O
898 Asthma and Chronic Obstructive Pulmonary Disease
Two additional examples of novel scaffolds displaying either the arginine (54) or lysine (55) residues are shown.
The b-lactam derivative 54
191
exhibited excellent potency compared to early lead compounds but still did not offer
good selectivity against trypsin. Further renement of substituents lead to the identication of additional analogs
exhibiting 43000-fold selectivity against trypsin as well selectivity against a broader panel of other proteases.
54 Tryptase IC
50
= 6 nM
N
O
N
O
N
NH
O
CO
2
H
N
H
HN
NH
2
55 Tryptase IC
50
= 68 nM
Selectivity >10 000-fold
NH
2
N
O
N
By leveraging past SAR work on factor Xa and the fact that there is high homology between the factor Xa and
tryptase S1 pockets, a strategy was employed where 2500 proprietary compounds from the factor Xa program were
screened against tryptase.
192,193
The resulting hits were then optimized using a rational approach based on
crystallography that resulted in potent, selective inhibitors exemplied by analog 55.
In order to take advantage of the tetrameric enzyme structure a rst generation series of bifunctional inhibitors have
been rationally designed. Figure 5 illustrates both the tetrameric nature of b-tryptase with a conceptualized
bifunctional molecule interacting with two subunits. The general design strategy is to develop compounds that possess
an extended length of about 2030 A
in a manner that bridges two monomeric active sites. The inhibitors reported to
date typically display a symmetrical motif with the following design characteristics: headlinkerscaffoldlinkerhead.
As with the monofunctional analogs they also display an arginine or lysine-like functional group attached to a
heterocyclic core. Analogs 56, 57, and 58 represent such designs.
194
Figure 5 Beta-tryptase tetramer crystal structure with a conceptual bifunctional ligand (blue).
Asthma and Chronic Obstructive Pulmonary Disease 899
O
O
BnO
O
N N
H
O
H
2
N
O
N
N
N
H
O
NH
2
O
N
56 Tryptase K
i
= 1.3 nM
O
O
O
O
H
N
O
H
N
H
2
N
NH
2
57 Tryptase K
i
= 7.5 nM
NH
H
2
N
O
N
H
O O
N
H
O
NH
2
NH
58 Tryptase K
i
= < 1 nM
An analysis of analog 58 illustrates the role played by the amidine moieties play in building the adjacent S1 pocket
interactions. It is subnanomolar in potency and a single change such as exchange of an amidine for a nitrile results in
analogs 2000-fold less potent. The analog possesses excellent selectivity (1 mM, trypsin; 4100 mM, thrombin; 4 mM,
plasmin) and has been shown to be efcacious when delivered intratracheally at 1 mg kg
1
in a guinea pig airway
hyperresponsiveness screen. This is an important point as the bifunctional inhibitors are limited to powder inhalation
formulations given their generally poor pharmacokinetic properties. Another way to exploit the bifunctional concept
toward inhibitor design is illustrated by analog 59. In this example the smaller monofunctional monomer can form a
dimeric species through hydrogen bonding of the primary amide group. The SAR shows that a charged acid species is
essentially inactive while the corresponding ethyl ester exhibited only modest potency (K
i
88 and 59 mM,
respectively).
195
When compared to the dimers linked by a covalent bond, the pseudodimeric associative approach may
offer some advantages in terms of molecules with lower molecular weight, better solubility, and improved
pharmacokinetic properties.
N
O
H
2
N
N
N
O
S
59 Tryptase K
i
= 1.5 nM
R
NH
2
O
R = F versus H increases hERG activity
(17 versus >30 mM)
Amide >> acid > ester
Bifunctional binding mode Dimeric binding mode
versus
The last strategy involves the concept of tetramer disruption. Although controversial, it is believed that dissociation
of the heparin-stabilized tryptase tetramer into monomeric units results in irreversible inactivation of the enzyme. It
has been shown that the heparin antagonists polybrene (IC
50
3.6 nM) and protamine (IC
50
65 nM) are both
potent inhibitors of human lung tryptase either competitively or noncompetitively.
196
Protamine is an arginine-rich
polycationic protein which is involved in DNA binding in spermatozoa, and it has been used clinically as a heparin
900 Asthma and Chronic Obstructive Pulmonary Disease
antagonist to reverse the effect of injected heparin during surgery. Other examples of inhibitors are lactoferrin, which is
a cationic, neutrophil-derived protein of 78 kDa which possesses unique heparin-binding domains, as well as the similar
cationic protein myeloperoxidase (118 kDa).
197
Chymase is classied as a chymotrypsin-like serine protease. Human
chymase is restricted to mast cell populations and is abundant in the skin and submucosal tissue of the respiratory and
gastrointestinal tracts.
198
It is stored along with tryptase in secretory granules but is released as a macromolecular
complex with carboxypeptidase and proteoglycans in response to immunological stimuli. The enzyme complex has an
extended substrate binding site that prefers a phenylalanine residue at pocket P1 and hydrophobic residues at P2 and
P3 in the catalytic cleft. This confers a somewhat broad spectrum of activity including degradation of extracellular
matrix proteins (tissue remodeling) and the synthesis of angiotensin-2. These features suggest that inhibition of
chymase could also provide therapeutic benet in cardiovascular disease.
199
The design of early inhibitors used a
traditional strategy targeting inhibition through substrate mimicry. These early peptides and peptidomimetics were
designed to be recognized by the enzyme and contained a activated functional substituent such as a carbonyl group
made susceptible to nucleophilic addition by the active site Ser195 hydroxyl group.
Several typical examples illustrate the different types or reactive moieties utilized. In general, a-haloketones,
aldehydes, boronic acids, and phosphonate esters can all provide the electrophilic component necessary for reversible
covalent interaction. The reader is referred to the appropriate references and reviews since this is a general,
well-established protease inhibition strategy.
200,201
O N
H
N
H
N
O
O O
O
F
F
N
H
O
CO
2
H
60 Example peptide-'warhead' inhibitor
chymase K
i
= 5.6 nM
Electrophilic center
N
N
H
2
N
O
OMe
NH
O
O
O
N
CO
2
Me
61 Example peptidomimetic
chymase K
i
= 4.8 nM
Despite excellent potency, the therapeutic use of peptide-based inhibitors is still limited due to poor bioavailability.
Reports on nonpeptidic inhibitors are somewhat limited and this is currently an active area of research. An example is
illustrated by the continued renement of analog 60 to furnish 61, which demonstrates that the combination of an
arylpyrimidone scaffold representing P2P3 interactions and the use of a heterocyclic ketone can rival potency while
offering good PK, selectivity, and bioavailability.
202,203
The arylpyrimidone scaffold has spawned a host of inhibitors
whereby researchers have mixed and matched pocket SAR information from peptide programs with a variety of
electrophilic warheads.
204,205
The b-lactams 62 and 63 also diverge from the traditional peptide SAR.
62 Chymase K
i
= 6 nM
N
O
O
HN
OMe
OMe
O O
S
N
N
N
N
CO
2
H
O
63 Shionogi BCEAB
Chymase K
i
= 4 nM
Cat G IC
50
= 35 nM
N
O
HN
O
O
CO
2
H
OEt
Development of a high-throughput screening hit originating from an antibacterial program lead to the discovery of
62, which offers high potency and is somewhat selective over a panel of proteases.
206
A related analog, 63, falls within
Asthma and Chronic Obstructive Pulmonary Disease 901
this compound class and, as expected, the active site Ser195 hydroxyl group is thought to attack the b-lactam carbonyl
leading to ring cleavage and acylation of the enzyme.
207
Analog 64 represents an emerging scaffold with a novel ketophosphonate moiety that offers potency for chymase
and also has been shown to inhibit another mast cell serine protease, cathepsin G (which plays a role in the activation of
PAR-4 leading to platelet activation).
200
Worth noting is the observation that the b-lactam 63 is also reported to have a
similar dual-target specicity demonstrating a cathepsin G in vitro potency of 35 nM. It has been shown that dual
inhibition or selectivity for either serine protease can be modulated through SAR modications at a related specicity
pocket in the active site.
64 Johnson & Johnson
Chymase K
i
= 2.3 nM
Cat G K
i
= 38 nM
N
O
N
O
O
P
OH
O
OH
Recent reports indicate that 64 is advancing to the clinic and has demonstrated in vivo efcacy in preventing
both early- and late-stage airway hyperreactivity in the sheep model at 0.1 mg kg
1
(twice daily aerosol dosing).
For completeness, a brief survey of additional classes of chymase inhibitors is illustrated by structures 6567 below.
205
Each exhibits a unique selectivity prole over related proteases and their optimization has been driven by structure-
based design.
N
N
S
CO
2
H
65 Chymase IC
50
= 1 nM
HO
2
C
O
H
N
S
O
O
66 Chymase IC
50
= 17 nM
S
F
S
HN
O
O
O
N
CO
2
H
67 Chymase IC
50
= 2 nM
Overall, mast cells and mast cell degranulation products play a critical role in modulation of the immune system.
Based on a variety of biological studies, b-tryptase appears to be best associated with a variety of allergic disease states
including asthma. Recent advances in the design of effective inhibitors has been driven by a solid understanding of
enzyme structure and the monofunctional series of analogs seems to hold the most promise. The bifunctional series is
the result of clever exploitation of the enzymes tetrameric structure, however, these molecules may suffer from
downstream development issues based on physicochemical properties. The development of chymase inhibitors has also
taken a structure-guided approach, since many analogs are peptide or peptidomimetic in nature thus taking advantage
of active site catalytic residues in order to covalently inactivate the enzyme. The physiological and pathological roles of
chymase are still to be fully elucidated and are an active area of research. Priority efforts are aligned to this need to
establish validation for the involvement of chymase in both cardiovascular and autoimmune diseases. In general, the
role of mast cell proteases is still under active investigation and the greatest challenge is to design and deliver a
selective, orally available inhibitor with robust efcacy.
7.30.7.5 Interleukin-5 (IL5) Receptor Inhibitors
Pronounced eosinophilic inltration is believed to play a crucial role in the pathogenesis of asthma. The cytokine
IL5 is produced by activated T cells, mast cells, and eosinophils, and functions as a promoter for the proliferation
902 Asthma and Chronic Obstructive Pulmonary Disease
of bone marrow precursor cells and their subsequent differentiation into mature basophils and eosinophils.
208
IL5 also has been shown to promote eosinophil survival and activation during allergic inammation. The high
afnity receptor for IL5 consists of two subunits (a- and b-chain) with the a-chain being the specic or unique
IL5 binding subunit in low afnity and the b-chain assisting in the formation of a high-afnity state receptor
through interaction with the a-chain. In this arrangement, the b-chain is shared by two other receptors, GM-CSF
and IL3.
211
As a method of target validation, it has been shown that wild-type mice treated with an anti-IL5 neutralizing
antibody or IL5
/
genetic knockouts
209
are able to suppress eosinophil recruitment to the lung and inhibit airway
hyperresponsivness to antigen challenge. While animal studies using the antibody approach were encouraging, human
clinical trials with mild atopic asthmatics did not show consistent effects on lung function despite a marked
suppression of circulating eosinophils in the blood. Currently this study design and resulting data has sparked a vigorous
debate on the role of both IL5 and eosinophils, in general, in the pathogenesis of asthmatic disease.
210
Nevertheless,
this level of target validation has generated the interest of medicinal chemistry and the search for small molecule
inhibitors of the IL5 receptor has received some attention. Analog 68 was shown to inhibit binding of IL5 to its
receptor on peripheral human eosinophils.
212,213
Given the lack of published, advanced data and modest potency, this
compound may have simply been used as a research tool to validate the targets signaling pathway through the JAK
kinase manifold.
MeO
MeO
N
N
N
68 YM-90709
Receptor binding IC
50
= 1 M
N
S
O
69 Isothiazolone chemical probe
Receptor binding IC
50
= 20 M
N
Receptor Cys66-SH
(Domain 1)
Another early exploratory approach has identied a class of compounds shown to covalently modify the receptor.
A series of isothiazolones (69) were shown to specically inhibit the IL5/IL5R interaction at the a-chain. This was
veried through the generation of a Cys66 alanine mutant that still bound IL5, which was not disrupted in the
presence of the probe molecule.
214
While not therapeutic drugs, these molecules illustrate that inhibition of the
receptor is chemically tractable. High-throughput screening has also uncovered several other compound classes that
can modulate IL5 binding. Several other irreversible ligands have been identied employing a surface plasmon
resonance/mass spectrometry afnity experiment. Analogs 70 and 71 are moderately active at the IL5 receptor and
were cross-reactive with the IL3 and GM-CSF receptors.
215
SMe
NHEt
OH
70 Chemical probe
Receptor binding IC
50
= ~8 M
N
S
HO
N
71 Chemical probe
Receptor binding IC
50
= ~11 M
Again, druglike molecules were not identied in this study. The probes furthered the understanding of receptor
function with regards to a shared b-chain. Included in this section is a series of recent compounds that have
been demonstrated to inhibit the production of IL5, rather than specically target the receptor. The azauracil
derivative 72 has demonstrated in vitro potency by inhibition of IL5 protein in activated human whole blood and in
isolated human peripheral blood monocytes as well as mouse splenocytes.
216
Message levels for other cytokines
remained unchanged.
Asthma and Chronic Obstructive Pulmonary Disease 903
72 R146225
hWhole blood IC
50
= 34 nM
hPBMC IC
50
= 24 nM
Murine splenocytes IC
50
= 6 nM
N
N S
Cl Cl
Cl
N
N
O O
73 Whole blood IC
50
= 78 nM
MCP-1 IC
50
= 220 nM
MCP-2 IC
50
= 580 nM
MCP-3 IC
50
= 80 nM
S
N
Cl
Cl
N N
O
O
O
O
HO
Since the observed potency was sufcient to test in vivo, the compound showed efcacy at 0.62.5 mg kg
1
orally in
a mouse model measuring pulmonary accumulation of eosinophils. It was found that chronic dosing in pregnant rats and
rabbits induced signs of teratogenesis and further development was halted. This triggered further SAR activity with an
objective to eliminate this adverse effect through the design of an inhaled prodrug as illustrated by analog 73. After a
survey of functionality, it was found that the hydroxypropyl ester offered high metabolic stability in lung tissue while it
was rapidly metabolized to the inactive carboxylic acid by human liver preparations.
217
This effectively translated to
low and short-lived plasma levels of 73. The activity prole suggested that the analogs might target Th2 cells given the
reduced levels of the chemotactic ligands MCP-1,2,3 as well as IL4. In vivo activity was demonstrated by intratracheal
administration of an aerosol in the Ascaris sheep model. Efcacy was seen whether the compound was dosed pre- or
post-antigen challenge with complete abrogation of the late phase response as well as reduced bronchial hyperreactivity
to inhaled carbachol.
Several approaches targeting the cytokine IL5 have been investigated using a variety of strategies in the past
years.
218,219
These include antibody approaches toward the receptor, small-molecule probes to inhibit ligand binding to
the receptor, and agents that prevent production of the cytokine itself. Given the dearth of small-molecule research in
the area, perhaps spawned by the failure of antibodies in the clinical setting, may lead one to conclude that given
asthma has a multifactorial pathogenesis, inhibition of a single signaling agent may not be sufcient for therapy.
7.30.7.6 Inhibition of Leukotriene Biosynthesis
The past decade has witnessed an explosion of activity in the eld of inhibition leukotrienes and outstanding,
comprehensive reviews are available to the reader.
88
Several intersections for intervention in the arachidonic acid pathway
have resulted in a rich history of chemotypes and strategies that an entire volume could be devoted to the discussion.
The following targets best represent these intersections: inhibitors of 5-lipoxygenase (5-LO), inhibitors of the redox
protein, ve lipoxygenase activating protein (FLAP), the leukotriene receptor LTD
4
(CysLT1), and LTB
4
. There has
been interest on other pathway enzymes with limited reports of small molecule research targeting LTA
4
hydrolase.
5-Lipoxygenase is a dioxygenase that incorporates molecular oxygen into arachidonic acid giving rise to the metastable
epoxide LTA
4
. Further processing by either LTA
4
hydrolase (neutrophils and monocytes) or LTC
4
synthetase (mast cells
and eosinophils) generated either LTB
4
or the cysteinyl leukotrienes LTC
4
, LTD
4
, and LTE
4
(Figure 6).
Intervention of 5-LO at the start of the cascade has been an intense area of research since its discovery in
1983.
220,221
Although an attractive target, there has been some concern about possible unwanted side effects especially
since an entire metabolic process would be interfered with. Some genetic knockout information is available and the
mice appear to develop normally.
222
In the design of inhibitors, many researchers targeted the active site, nonheme iron
atom and built in a weak chelator such as a hydroxamic group as best illustrated by Zyo (74, zileuton, Abbott).
223
74 Zileuton (Abbott)
hWhole blood IC
50
= 700 nM
S
N
HO NH
2
O
75 hWhole blood IC
50
= 80 nM
O
O
F
N
HO
O
NH
2
76 Atreleuton (Abbott)
hWhole blood IC
50
= 150 nM
S
F
N
HO
O
NH
2
904 Asthma and Chronic Obstructive Pulmonary Disease
Further structural modications following this design strategy generated the second-generation iron ligand
inhibitors 75 and 76.
224226
The objective of the advanced analogs was to improve potency and to improve duration
of action by inhibition of glucuronidation rate.
224
Analog 76, as the (R)-isomer, provided sustained ex vivo duration of
5-LO inhibition (as measure in a human whole blood assay) and progressed to the clinic with discontinuation after
phase III trials due to elevated liver enzymes. It was about vefold more potent that zileuton in animal models of
bronchospasm and had an oral half-life of B16 h.
Cys
Gly
Glu
COOH
OH
LTD
4
receptor
antagonists
LTE
4
Dipeptidase
LTD
4
LTC
4
-Glutamyl Transpeptidase
LTC
4
synthetase
Metabolism to peptidyl leukotrienes
LTA
4
Mediator of informations
leukocyte recruitment
and activaton
LTB
4
receptor
antagonists
Peptidyl leukotrienes
Mediators of allergy,
bronchoconstriction and
vascular permeability
Metabolism to leukotriene B
4
LTA
4
hydrolase
5-lipoxygenase
dehydration step
AA interacts with 5-lipoxygenase activating protein
(FLAP) 5-Lipoxygenase translocates to the nuclear
membrane where FLAP, AA and 5-LO interact
resulting in oxidative catalysis
5-lipoxygenase
oxidation step
5-LO Inhibitors
FLAP Inhibitors
Arachidonic acid
Phospholipases cleave arachidonic acid from
esterified phospholipids in membrane in reponse
to receptor-mediated intracellular influx of Ca
2+
Cell membrane phospholipids
COOH
COOH
OOH
COOH
O
5-HPETE
COOH
Cys-Gly
COOH
OH
Cys
COOH
OH
OH OH
Figure 6 Leukotriene inammatory pathway and key points of therapeutic intervention. (Reprinted with permission from
Brooks, C. D. W.; Summers, J. B. J. Med. Chem. 1996, 39, 2629 & American Chemical Society.)
Asthma and Chronic Obstructive Pulmonary Disease 905
A unique approach is represented by analog 77 which combines two concepts that could prove benecial in allergy
and asthma.
227
A series of N-hydroxycarbamates containing a histamine H1 antagonist pharmacophore was constructed
and exhibited the desired dual activity prole. Preclinical work in the guinea pig OVA model showed 77 to have a
better overall prole that a traditional 5-LO analog such as 74. Other dual target strategies have been employed
including COX-/5-LO, PAF/5-LO, and lipid and sugar metabolism enhancers/5-LO, although little is reported in the
medicinal chemistry literature. Beyond this approach, the set strategy has been to explore lipophilic groups and linkers
stemming from a terminal hydroxyurea moiety and many examples exist in the review articles. Several isosters of
hydroxyureas have been devised (e.g., analog 78)
133,228
offering modest potency; however, second-generation substrate
inhibitors emerged that were designed to t the 5-LO active site without the need for an iron-chelating group.
Analogs 79 and 80 represent ongoing discovery efforts in this area.
229231
N
N
F
F
O
N
OH
NH
2
O
77 Dual H1/5-LO inhibitor
H1 binding IC
50
= 3.6 nM
hWhole blood 5LO IC
50
= 89 nM
78 Rat basophil leukemia cell IC
50
= 60 nM
N O
HO
Iron chelation
O
OMe
N
S
N
O
O
OMe
F
O
Representative 5-LO substrate inhibitors
79 ZD-2138 (Zeneca)
hWhole blood LTB4 IC
50
= 24 nM
O
O
OMe
N
O
O
F
N
80 CJ-13454 (Pfizer)
hWhole blood LTB4 IC
50
= 34 nM
NH
2
O
The rst to be evaluated in the clinic was analog 79 in a 1-month safety study. A single dose (350 mg orally) was
shown to completely inhibit LTB
4
production in ex vivo blood samples. Phase II studies were designed as allergen
challenge in asthmatics using 79 at the same does. No effect was seen on both early and late stage response, however
identical ex vivo efcacy was seen. After several additional studies development was ultimately stopped. As a follow-on,
the imidazole analog 80 has illustrated improved pharmacokinetic and toxicology characteristics though clinical efcacy
remains to be seen.
FLAP inhibitors comprise a class of compounds that can inhibit leukotriene biosynthesis without direct inhibition of
5-LO. The indomethacin derivative 81 proved indispensable in the discovery of FLAP and understanding the
differential activity observed in intact versus lysed cell results on leukotriene biosynthesis.
232
While the precise
mechanism of action is not clearly understood, FLAP is hypothesized to be essential for activation of 5-LO through
assisting in either the membrane translocation process or as a vehicle for presentation of arachdonic acid. A series
of rst-generation (81, 83) and second-generation (82, 84) inhibitors were discovered and developed in the early to
mid-1990s.
233
By combining pharmacophoric regions of the rst-generation lead compounds researchers were able to
further optimize analog potency. A key observation was the conserved quinoline moiety which turned out to be a
prominent binding motif in many FLAP SAR programs.
906 Asthma and Chronic Obstructive Pulmonary Disease
81 MK-886
Binding IC
50
= 23 nM
N
Cl
CO
2
H
S
N
O
Cl
CO
2
H
S
N
82 MK-591
Binding IC
50
= 2 nM
O
N
CO
2
H
84 BAY-x1005 83 REV-5901
O
N
OH
A number of clinical trials were initiated with varied results. Compound 81, when dosed at 500 mg orally in
asthmatic patients prior to antigen challenge improved both early and late response by 58% and 44%, respectively, but
was discontinued based on the modest leukotriene inhibition measured ex vivo.
234,235
The second-generation analog 82
demonstrated better early and modest late phase response (79% and 39%, respectively) and the ex vivo inhibition of
leukotriene biosynthesis was 98% on ionophore challenge of whole blood up to 24 h. This demonstrated the clinical
efcacy of FLAP inhibition; however, larger studies showed that patient respiratory improvement was not aligned with
in vitro compound potency.
233
To date, no clinical candidate from these programs has emerged to the market. From a
medicinal chemistry point of view, optimization strategies including oxime insertion proved fruitful as illustrated by
analog 85 which provided the desired improvement in solubility and absorption properties.
236
85 Oxime insertion analog
hPMNL LTB
4
inhibition IC
50
= 15 nM
In vivo ED
50
= 0.5 mg kg
1
O
N
O
84 BAY-x1005
N
CO
2
H
86 Symmetrical core analog
hPMNL LTB
4
inhibition IC
50
= 20 nM
In vivo ED
50
= 1.5 mg kg
1
O
N
O
N
CO
2
H
O
N
R
R = H or Me
Further renement, as demonstrated by the symmetrical core analog 86, removed the stereocenter (which proved too
costly to develop) yet maintained superior potency in inhibiting LTB
4
formation in human neutrophils challenged with a
calcium ionophore. Given the efcacy in rodent asthma models, analog 86 progressed to phase I clinical trials.
237,238
The best-represented compounds in the area of LTD
4
(CysLT1) inhibition are the marketed drugs Singulair
(montelukast, Merck),
90,239
Accolate (zarlukast, AstraZeneca),
89,240
and Ultair (pranlukast, Ono).
241
The history of
the development of these drugs is a fascinating story and stems from SAR and privileged pharmacophores identied in
5-LO and FLAP research programs. Most importantly it was the seminal discovery that the active components of slow-
reacting substance of anaphylaxis (SRS-A) were the CysLTs, specically LTD
4
, LTC
4
, and LTE
4
.
242,243
This, coupled
with the strong evidence that SRS-A played a pivotal role in bronchoconstriction launched intense research efforts. The
resulting analogs generally comprise combined lipid, acid, and peptide mimetics representing the three key regions and
stereochemistry of LTD
4
.
Montelukast (88) represents a second-generation inhibitor stemming from its congener 87 which was designed
by combining the FLAP active quinioline pharmacophore with a thioacetal unit found in early high-throughput
screening hits.
244,245
Asthma and Chronic Obstructive Pulmonary Disease 907
N Cl
S
S
CO
2
H
CON(CH
3
)
2
87 Verlukast (Merck)
Binding IC
50
= 0.8 nM
N Cl
S
S CO
2
H
HO
88 Singulair (montelukast, Merck)
Binding IC
50
= 0.5 nM
Verlukast was in early clinical trials and only demonstrated about a 13% improvement in lung function following a
single oral or aerosol dose. The compound was ultimately withdrawn due to liver function abnormality. Replacement of
one of the thioacetal side chains with an arylalkyl moiety and installation of the geminal cyclopropane substituent
furnished the potent analog 88 which was devoid of undesired side effects especially peroxisomal enzyme induction
which had plagued the rst generation series. In moderate asthmatics, a single 100 mg dose produced an immediate
10% improvement in base line FEV
1
which stayed constant during a 9-h study. Pranlukast (89) and zarlukast (90)
were developed using similar strategies.
89 Pranlukast (Ono)
Binding K
i
= 46 nM
O
NH
O
O
O
N
N
N
H
N
90 Zafirlukast (AstraZeneca)
Binding K
i
= 0.5 nM
N
N
H
O
O
O
H
N
S
O
2
MeO
Analog 89 was identied from a weak high-throughput screening lead and was developed with a strategy that
involved replacement of a benzoic acid moiety with the chromone carboxylate core which increased potency 100-fold.
Subsequent replacement of the carboxylate with a tetrazole isostere furnished both in vitro and in vivo potency
increases. Finally, optimization of the lipophilic tail resulted in the clinical candidate that was approved in Japan in 1995
and was the rst LTD
4
(CysLT1) antagonist to be commercially available.
246,247
The discovery of zarlukast (90) is the subject of several excellent SAR review articles.
248,249
The indole-based
inhibitor was essentially developed by a hybridization between a leukotriene pharmacophore based on LTD
4
itself and
a hydroxyacetophenone series of antagonists found in a screening exercise. Early analogs suffered from pharmacokinetic
issues and poor bioavailability (o1%). Continued optimization of the SAR furnished the clinical candidate that
demonstrated a 117-fold shift (within 2 h) of the doseresponse curve using the LTD
4
induced bronchoconstriction
challenge in asthmatics and was effective in blocking a variety of environmental asthmatic triggers. Zarlukast was the
rst leukotriene modulator approved in the USA, which was then followed by montelukast.
Currently research has slowed in this area and it appears no new agents are being developed. This most likely is
because the market is saturated and these agents are still used in combination therapy with steroids and b-agonists as a
primary care standard for asthma. There has been some controversy over the effectiveness of these agents in the
general population and that still remains to be resolved. Current clinical work is focused on their use for other modes of
inammatory disease such as atopic dermatitis, aspirin- and exercise-induced asthma, as well as seasonal allergic
rhinitis.
The discovery of LTB
4
antagonists has been slower that of the LTD
4
(CysLT1) antagonists. Pharmacological
interest has focused on the proinammatory properties of this lipid mediator that is produced by several cell types
including neutrophils and macrophages. LTB
4
has also been shown to stimulate degranulation and chemotaxis of
inammatory cells through a receptor-based mechanism. Recently the distribution of LTB
4
receptors in human
hematopoietic cells has been studied and it was shown that it is widely distributed and also plays a role in endothelial
cells but not platelets.
250
A variety of diverse chemotypes have been discovered in the past decade with few new
reports since the mid-1990s. Two fundamental research strategies toward drug design have emerged, one based on the
discovery of a key fragment and the other based on mimicking the structure of LTB
4
.
908 Asthma and Chronic Obstructive Pulmonary Disease
O OH
Et
O N
NH
N
N
91 Binding IC
50
= 85 nM (human neutrophils)
O OH
Et
O
N
N
Et
CO
2
H
O
92 Binding IC
50
= 300 nM (human neutrophils)
Replace with OCH
3
IC
50
= 6 nM
OEt IC
50
= 4.8 nM
A key pharmacophore was found, along with some fundamental SAR resulting in various derivatives based on the 5-
ethyl-2,4-dihydroxyacetophone moiety which was hypothesized to be a mimetic of the triene moiety in LTB
4
. Two such
examples are illustrated by analogs 91 and 92.
251253
The location of the alkyl chain of 91 proved critical to selectivity
over LTD
4
. Further SAR work optimizing chain length, carboxy isosteres, and aryl SAR ultimately drove binding potency
down to 4.8 nM and afforded a potent analog that was active in blocking LTB
4
-induced bronchoconstriction in vivo.
Several reviews have been published that are devoted to analogs derived from the parent leukotriene structure.
254
N
H
O
OMe
93 Binding IC
50
= 17 nM (human neutrophils)
NH
N N
N
Replace with CO
2
H IC
50
= 70 nM
94 Binding IC
50
= 6.4 nM (human neutrophils)
O
OH
CO
2
H
Two recent leukotriene-like examples are illustrated by analogs 93 and 94.
255,256
Both the biaryl and carboxy (or
isostere) functionality are required for potency and the design concept is based on a rigid platform with key
functionality appropriately displayed. Analog 94 demonstrated high afnity for the LTB
4
receptor and for related cell
responses. Oral administration in the guinea pig at 3 mg kg
1
blocked 75% of neutrophil response to 12-R-HETE
challenge. Phase I studies used ex vivo inhibition of LTB
4
-induced CD11b in healthy subjects. The analog produced a
10-fold shift in the dose response curve and was well tolerated up to 640 mg kg
1
. Due to its exceptionally long
half-life (t
1/2
420 h) it was discontinued for development.
257
Overall, clinical success has yet to be achieved with this
class of antagonists. It is not clear whether the receptors response to LTB
4
is exclusive or subject to stimulation
by other more potent chemoattractants or whether the primary role of LTB
4
may be coupled with binding to the
BLTR2 receptor.
A key enzyme in the biosynthesis of LTB
4
is LTA
4
hydrolase, which is a zinc-containing metalloenzyme and is
involved in the rate-limiting step for the production of LTB
4
through the hydrolysis of the epoxide moiety. Many early
analogs were dipeptidic in nature as illustrated by the kelatorphan analog 95.
258
N
H
O
HO
O
CO
2
H
Kelatorphan
LTA
4
hydrolase IC
50
= 5 nM
Aminopeptidase IC
50
= 7 nM
NEP IC
50
= 46 nM
ACE IC
50
= > 10 M
N
H
O
HO
O
N
95
LTA
4
hydrolase IC
50
= 8 nM
Aminopeptidase IC
50
= 10 nM
NEP IC
50
= 17 M
ACE IC
50
= 40 M
CO
2
H
Asthma and Chronic Obstructive Pulmonary Disease 909
A systematic study of the peptide and substituent SAR demonstrated that potent compounds could be derived with
selectivity against NEP and ACE could be gained. Overall, the analogs retained their aminopetdidase activity. In all
cases the hydroxamic moiety was required to retain inhibitory activity.
More recently a series of nonpeptide nitrogen heterocycles have been described that are effective inhibitors of LTA
4
hydrolase. They are unique in that they do not appear to bind zinc as the hydroxamic acid inhibitors do and unlike the
peptide, they demonstrate good oral bioavailability. Analogs 96, 97, and 98 illustrate the SAR of this class.
259
O N
Me
CO
2
H
96 SC-57461A
Hydrolase IC50 = 2.5 nM
N
CO
2
Et
O
97 SC-56938
Hydrolase IC
50
= 3 nM
98 Hydrolase IC
50
= 0.8 nM
N
O
N
N
CN
As can be seen in the examples, increased potency can be obtained through optimization of the amine or
heterocyclic component. The series produced two clinical candidates that were chosen based on ex vivo versus in vitro
potency using blood samples. The primary candidate was 96 that was designed through a series of iterative steps
exploring chain length and linker substitution as well as amine substitution. Besides potency in the enzyme assay good
whole blood LTB
4
production inhibition was seen (IC
50
49 nM). This analog demonstrated excellent oral
bioavailability in the mouse ex vivo assay with an ED
90
in the 13 mg kg
1
range. The clinical backup was analog 97
(mouse ex vivo LTB
4
production ED
90
97% Inhibition at 3 mg kg
1
) which was selected based on a rhesus monkey
assay and showed excellent potency when dosed orally, inhibiting the production of LTB
4
with an ED
90
o10 mg kg
1
.
Unfortunately, these compounds failed preclinical safety studies due to the accumulation of a long-lived metabolite in
adipose tissue and mild hepatic toxicity.
260
To date, leukotriene modulation has been approached from several different avenues resulting in few marketed
products. Most clinical trials have focused and concluded for asthma and only recently has the trend shifted toward
other inammation targets.
References
1. Masoli, M.; Fabian, D.; Holt, S.; Beasley, R. Allergy 2004, 59, 469478.
2. Lopez, A. D.; Murray, C. C. J. L. Nat. Med. 1998, 4, 12411243.
3. Mannino, D. M.; Homa, D. M.; Pertowski, C. A.; Ashizawa, A.; Nixon, L.; Johnson, C. A. Morb. Mortal. Wkly Rep. 1998, 47, 128.
4. Strassels, S. A.; Smith, D. H.; Sullivan, S. D.; Mahajan, P. S. Chest 2001, 119, 344352.
5. Tinkelman, D.; Corsello, P. Am. J. Manag. Care 2003, 9, 767771.
6. Weiss, K. B.; Sullivan, S. D. J. Allergy Clin. Immunol. 2001, 107, 38.
7. Hurd, S. Chest 2000, 117, 14.
8. Pauwels, R. A.; Buist, A. S.; Calverley, P. M. A.; Jenkins, C. R.; Hurd, S. S. Am. J. Respir. Crit. Care Med. 2001, 163, 12561276.
9. Williams, S. G.; Schmidt, D. K; Redd, S. C.; Storms, W. Morb. Mortal. Wkly Rep. 2003, 52, 18.
10. McFadden, E. R.; Gilbert, I. A. N. Engl. J. Med. 1994, 330, 13621367.
11. Martinez, F. M. Am. J. Respir. Crit. Care Med. 1995, 151, 16441647.
12. Platts-Mills, T. A. E.; Carter, M. C. N. Engl. J. Med. 1997, 336, 13821384.
13. Bousquet, J.; Jeffery, P. K.; Busse, W. W.; Johnson, M.; Vignola, A. M. Am. J. Respir. Crit. Care Med. 2000, 161, 17201745.
14. Stirling, R. G.; Chung, K. F. Allergy 2001, 56, 825840.
15. Barnes, P. J.; Shapiro, S. D.; Pauwels, R. A. Eur. Respir. J. 2003, 22, 672688.
16. Barnes, P. J. N. Engl. J. Med. 2000, 343, 269280.
17. Mahadeva, R.; Lomas, D. A. Thorax 1998, 53, 501505.
18. Busse, W. W.; Lemanske, R. F. N. Engl. J. Med. 2001, 344, 350362.
19. Kanaoka, Y.; Boyce, J. A. J. Immunol. 2004, 173, 15031510.
20. Sanderson, C. J. Blood 1992, 79, 31013109.
21. Sriramarao, P.; DiScipio, R. G.; Cobb, R. R.; Cybulsky, M.; Stachnick, G.; Castaneda, D.; Elices, M.; Broide, D. H. Blood 2000, 95,
592601.
910 Asthma and Chronic Obstructive Pulmonary Disease
22. Larbi, K. Y.; Dangereld, J. P.; Culley, F. J.; Marshall, D.; Haskard, D. O.; Jose, P. J.; Williams, T. J.; Nourshargh, S. J. Leukoc. Biol. 2003, 73,
6573.
23. Carlos, T. M.; Harlan, J. M. Blood 1994, 84, 20682101.
24. Terada, N.; Hamano, N.; Nomura, T.; Numata, T.; Hirai, K.; Nakajima, T.; Yamada, H.; Yoshie, O.; Ikeda-Ito, T.; Konno, A. Clin. Exp. Allergy
2000, 30, 348355.
25. Tachimoto, H.; Burdick, M. M.; Hudson, S. A.; Kikiuchi, M.; Konstantopolous, K.; Bochner, B. S. J. Immunol. 2000, 165, 27482754.
26. Hata, A. N.; Zent, R.; Breyer, M. D.; Breyer, R. M. J. Pharmacol. Exp. Therapeut. 2003, 306, 463470.
27. El Biaze, M.; Boniface, S.; Koscher, V.; Mamessier, E.; Dupuy, P.; Milhe, F.; Ramadour, M.; Vervloet, D.; Magnan, A. Allergy 2003, 58, 844853.
28. Clissi, B.; DAmbrosio, D.; Geginat, J.; Colantonio, L.; Morrot, A.; Freshney, N. W.; Downward, J.; Sinigaglia, F.; Pardi, R. J. Immunol. 2000, 164,
32923300.
29. Shi, H.-Z.; Humables, A.; Gerard, C.; Jin, Z.; Weller, P. F. J. Clin. Invest. 2000, 105, 945953.
30. Lazaar, A. L.; Panettieri, R. A. Am. J. Med. 2003, 115, 652659.
31. Hawker, K. M.; Johnson, P. R. A.; Hughes, J. M.; Black, J. L. Am. J. Physiol. Lung Cell Mol. Physiol. 1998, 275, L469L477.
32. Page, S.; Ammit, A. J.; Black, J. L.; Armour, C. L. Am. J. Physiol. Lung Cell Mol. Physiol. 2001, 281, L1313L1323.
33. Chung, K. F. Eur. Respir. J. 2000, 15, 961968.
34. Barnes, P. J.; Chung, K. F.; Page, C. P. Pharmacol. Rev. 1998, 50, 515596.
35. Parks, W. C.; Shapiro, S. D. Respir. Res. 2001, 2, 1019.
36. Akers, I. A.; Parsons, M.; Hill, M. R.; Hollenberg, M. D.; Sanjar, S.; Laurent, G. J.; McAnulty, R. J. Am. J. Physiol. Lung Cell Mol. Physiol. 2000,
278, L193L201.
37. Vignola, A. M.; Mirabella, F.; Costanzo, G.; Di Giorgi, R.; Gjomarkaj, M.; Bellia, V.; Bonsignore, G. Chest 2003, 123, 417423.
38. Busse, W.; Elias, J.; Sheppard, D.; Banks-Schlegel, S. Am. J. Respir. Crit. Care Med. 1999, 160, 10351042.
39. McDonald, D. M. Am. J. Respir. Crit. Care Med. 2001, 164, S39S45.
40. Barnes, P. J. Pharmacol. Rev. 2004, 56, 515548.
41. Soler, P.; Moreau, A.; Basset, F.; Hance, A. J. Am. Rev. Respir. Dis. 1989, 139, 11121117.
42. Shapiro, S. Am. J. Respir. Crit. Care Med. 1999, 160, S29S32.
43. Meshi, B.; Vitalis, T. Z.; Ionescu, D.; Elliott, W. M.; Liu, C.; Wang, X.-D.; Hayashi, S.; Hogg, J. C. Am. J. Respir. Mol. Cell. Biol. 2002, 26, 5257.
44. Keatings, V. M.; Barnes, P. J. Am. J. Respir. Crit. Care Med. 1997, 155, 453459.
45. Finkelstein, R.; Fraser, R. S.; Ghezzo, H.; Cosio, M. G. Am. J. Respir. Crit. Care Med. 1995, 152, 16661672.
46. Csoma, Z.; Kharitonov, S. A.; Balint, B.; Bush, A.; Wilson, N. M.; Barnes, P. J. Am. J. Respir. Crit. Care Med. 2002, 166, 13451349.
47. Tager, A. M.; Bromley, S. K.; Medoff, B. D.; Islam, S. A.; Bercury, S. D.; Friedrich, E. B.; Carafone, A. D.; Gerstzen, R. E.; Luster, A. D. Nat.
Immunol. 2003, 4, 982990.
48. Sommerhoff, C. P.; Nadel, J. A.; Basbaum, C. B.; Caughey, G. H. J. Clin. Invest. 1990, 85, 682689.
49. Hautamaki, R. D.; Kobayashi, D. K.; Senior, R. M.; Shapiro, S. D. Science 1997, 277, 20022004.
50. Van Eerdewegh, P.; Little, R. D.; Dupuis, J.; Del Mastro, R. G.; Falls, K.; Simon, J.; Torrey, D.; Pandit, S.; McKenny, J.; Braunschweiger, K.
et al. Nature 2002, 418, 426430.
51. Allen, M.; Heinzmann, A.; Noguchi, E.; Abecasis, G.; Broxholme, J.; Ponting, C. P.; Bhattacharyya, S.; Tinsley, J.; Zhang, Y.; Holt, R. et al. Nat.
Genet. 2003, 35, 258263.
52. Zhang, Y.; Leaves, N. I.; Anderson, G. G.; Ponting, C. P.; Broxholme, J.; Holt, R.; Edser, P.; Bhattacharyya, S.; Dunham, A.; Adcock, I. M. et al.
Nat. Genet. 2003, 34, 181186.
53. Buhl, R.; Farmer, S. G. Proc. Am. Thorac. Soc. 2005, 2, 8393.
54. Ambler, J.; Miller, J. N.; Orr, T. S. C. Int. Arch. Allergy Appl. Immunol. 1994, 46, 427437.
55. Campbell, E. M.; Kunkel, S. L.; Strieter, R. M.; Lukacs, N. W. J. Immunol. 1998, 161, 70477051.
56. Mahadeva, R.; Shapiro, S. D. Thorax 2002, 57, 908914.
57. Pizzichini, E.; Leff, J. A.; Reiss, T. F.; Hendeles, L.; Boulet, L.-P.; Wei, L. X.; Efthimiadis, A. E.; Zhang, J.; Hargreave, F. E. Eur. Respir. J. 1999,
14, 1218.
58. Sabater, J. R.; Wanner, A.; Abraham, W. M. Am. J. Respir. Crit. Care Med. 2002, 166, 14571460.
59. Abraham, W. L.; Ahmed, A.; Cortes, A.; Sielczak, M. W.; Hinz, W.; Bouska, J.; Lanni, C.; Bell, R. L. Eur. J. Pharmacol. 1992, 217, 119126.
60. Henderson, W. R.; Banerjee, E. R; Chi, E. Y. J. Allergy Clin. Immunol. 2005, 116, 332340.
61. Terawaki, K.; Yokomizo, T.; Nagase, T.; Toda, A.; Taniguchi, M.; Hasizume, K.; Yagi, T.; Shimizu, T. J. Immunol. 2005, 175, 42174225.
62. Hansen, G.; Jin, S. L. C.; Umetsu, D. T.; Conti, M. Proc. Natl. Acad. Sci. USA 2000, 97, 67516756.
63. Wang, Z.; Zheng, T.; Zhu, Z.; Homer, R. J.; Riese, R. J.; Chapman, H. A.; Shapiro, S. D.; Elias, J. A. J. Exp. Med. 2000, 192, 15871599.
64. Elias, J. A.; Zheng, T.; Lee, C. G.; Homer, R. J.; Chen, Q.; Ma, B.; Blackburn, M.; Zhu, Z. Chest 2003, 123, 339345.
65. Lee, J. J.; Dimina, D.; Macias, M. P.; Ochkur, S. I.; McGarry, M. P.; ONeill, K. R.; Protheroe, C.; Pero, R.; Nguyen, T.; Cormier, S. A. et al.
Science 2004, 305, 17731776.
66. Humbles, A. A.; Lloyd, C. M.; McMillan, S. J.; Friend, D. S.; Xanthou, G.; McKenna, E. E.; Ghiran, S.; Gerard, N. P.; Yu, C.; Orkin, S. H. et al.
Science 2004, 305, 17761779.
67. Wills-Karp, M.; Karp, C. L. Science 2004, 305, 17261729.
68. Dawkins, P. A.; Stockley, R. A. Thorax 2001, 56, 972977.
69. Wright, J. L.; Chung, A. Chest 2002, 122, 301306.
70. Coffman, R. L.; Hessel, E. M. J. Exp. Med. 2005, 201, 18751879.
71. Mauser, P. J.; Pitman, A. M.; Fernandez, X.; Feran, S. K.; Adams, G. K.; Kreutner, W.; Egan, R. W.; Chapman, R. W. Am. J. Respir. Crit. Care Med.
1995, 152, 467472.
72. Chang, M. M.-J.; Wu, R.; Plopper, C. G.; Hyde, D. M. Am. J. Physiol. 1998, 275, L524L532.
73. Frew, A. J. J. Allergy Clin. Immunol. 2002, 109, 210213.
74. Renard, S. I. Am. Proc. Am. Thorac. Soc. 2004, 1, 282287.
75. Stelmach, I.; Jerzymska, J.; Kuna, P. J. Allergy Clin. Immunol. 2002, 109, 257263.
76. Yasuda, H.; Yarnaya, M.; Nakayma, K.; Ebihara, S.; Sasaki, T.; Okinaga, S.; Inoue, D.; Asada, M.; Nemoto, M.; Saski, H. Am. J. Respir. Crit. Care
Med. 2005, 171, 12461251.
77. Berlyne, G. S.; Parameswaran, K.; Kamada, D.; Efthimiadis, A.; Hargreave, F. E. J. Allergy Clin. Immunol. 2000, 106, 638644.
78. Odingo, J. O. Expert Opin. Ther. Patents 2005, 15, 773787.
Asthma and Chronic Obstructive Pulmonary Disease 911
79. Lecklie, M. J.; ten Brinke, A.; Khan, J.; Diamant, Z.; OConnor, B. J.; Walls, C. M.; Mathur, A. K.; Cowley, H. C.; Chung, K. F.; Djukanovic, R.
et al. Lancet 2000, 356, 21442148.
80. OByrne, P. M.; Inman, M. D.; Parameswaran, K. J. Allergy Clin. Immunol. 2001, 108, 503508.
81. Plo tz, S.-G.; Uwe-Simon, H.; Darsow, U.; Simon, D.; Vassina, E.; Youse, S.; Hein, R.; Smith, T.; Behrendt, H.; Ring, J. N. Engl. J. Med. 2003,
349, 23342339.
82. Naya, A.; Saeki, T. Expert Opin. Ther. Patents 2004, 14, 716.
83. Traves, S. L.; Donnelly, L. E. Curr. Respir. Med. Rev. 2005, 1, 1532.
84. Hoshi, K.; Kurosawa, S.; Kato, M.; Andoh, K.; Satoh, D.; Kaise, A. Tohuku J. Exp. Med. 2005, 207, 143148.
85. Barnes, P. J. Eur. Respir. Rev. 2005, 14, 211.
86. Cairns, J. A. Pulmon. Pharmacol. Ther. 2005, 18, 5566.
87. Donohue, J. F. Chest 2004, 126, 125S137S.
88. Brooks, C. D. W.; Summers, J. B. J. Med. Chem. 1996, 39, 26292654.
89. Kelloway, J. S. Ann. Pharmacother. 1997, 31, 10121021.
90. Noonan, M. J.; Chervinsky, P.; Brandon, M.; Zhang, J.; Kundu, S.; McBurney, J.; Reiss, T. F. Eur. Respir. J. 1998, 11, 12321239.
91. Lu, P.; Schrag, M. L.; Slaughter, D. E.; Raab, C. E.; Shou, M.; Rodrigues, A. D. Drug Metab. Dispos. 2003, 31, 13521360.
92. Currie, G. P.; Srivastava, P.; Dempsey, O. J.; Lee, D. K. C. Q. J. Med. 2005, 98, 171182.
93. Wechsler, M. E.; Garpestad, E.; Flier, S. R.; Kocher, O.; Weiland, D. A.; Polito, A. J.; Klinek, M. M.; Bigby, T. D.; Wong, G. A.; Helmers, R. A.
et al. JAMA 1998, 279, 455457.
94. Solans, R.; Bosch, J. A.; Selva, A.; Orriols, R.; Vilardell, M. Thorax 2000, 57, 183185.
95. Djukanovic, R.; Wilson, S. J.; Kraft, M.; Jarjour, N. N.; Steel, M.; Chung, K. F.; Bao, W.; Fowler-Taylor, A.; Matthews, J.; Busse, W. W. et al.
Am. J. Respir. Crit. Care Med. 2004, 170, 583593.
96. Bisset, L. R.; Schmid-Grendelmeier, P. Curr. Opin. Pulmon. Med. 2004, 11, 3542.
97. Rot, A.; VonAdrian, U. H. Ann. Rev. Immunol. 2004, 22, 891928.
98. Carter, P. H. Curr. Opin. Chem. Biol. 2002, 6, 510525.
99. Wardlaw, A. J.; Dunnette, S.; Gleich, G. J.; Collins, J. V.; Kay, A. B. Am. Rev. Respir. Dis. 1988, 137, 6269.
100. Corrigan, C. Curr. Opin. Invest. Drugs 2000, 1, 321328.
101. Humbles, A. A.; Lu, B.; Friend, D. S.; Okinaga, S.; Logarawi, J.; Martin, T. R.; Gerard, N. P.; Gerard, C. Proc. Natl. Acad. Sci. USA 2002, 99,
14791484.
102. Rothenberg, M. E.; MacLean, J. A.; Pearlman, E.; Luster, A. D.; Leder, P. J. Exp. Med. 1997, 185, 785790.
103. Gonzalo, J. A.; Lloyd, C. M.; Kremer, L. J. Clin. Invest. 1996, 98, 23322345.
104. Heath, H.; Qin, S.; Rao, P.; LaRosa, G.; Kassam, N.; Ponath, P. D.; Mackay, C. R. J. Clin. Invest. 1997, 99, 178184.
105. Naya, A.; Saeki, T. Expert Opin. Ther. Patents 2004, 14, 716.
106. Naya, A.; Kobayashi, K.; Ishikawa, M.; Ohwaki, K.; Saeki, T.; Noguchi, K.; Ohtake, N. Bioorg. Med. Chem. Lett. 2001, 11, 12191223.
107. Saeki, T.; Ohwaki, K.; Naya, A.; Kobayashi, K.; Ishikawa, M.; Ohtake, N.; Noguchi, K. Biochem. Biophys. Res. Commun. 2001, 281, 779782.
108. Naya, A.; Kobayashi, K.; Ishikawa, M.; Ohwaki, K.; Saeki, T.; Noguchi, K.; Ohtake, N. Chem. Pharm. Bull. 2003, 51, 697701.
109. Bryan, S. A.; Jose, P. J.; Topping, J. R.; Wilhelm, R.; Soderberg, C.; Kertesz, D.; Barnes, P. J.; Williams, T. J.; Hansell, T. T.; Sobroe, I. Am. J.
Resp. Crit. Care Med. 2002, 165, 1602.
110. Gong, L.; Hogg, J. H.; Collier, J.; Wilhelm, R. S.; Soderberg, C. Bioorg. Med. Chem. Lett. 2003, 13, 35973600.
111. Ting, P. C.; Lee, J. F.; Wu, J.; Umland, S. P.; Aslanian, R.; Cao, Z. J.; Dong, Y.; Garlisi, C. G.; Gilbert, E. J.; Huang, Y. et al. Bioorg. Med. Chem.
Lett. 2005, 15, 13751378.
112. Wan, Y.; Jakway, J. P.; Qiu, H.; Shah, H.; Garlisi, C. G.; Tian, F.; Ting, P.; Hesk, D.; Egan, R. W.; Billah, M. M.; Umland, S. P. Eur. J. Pharmacol.
2002, 456, 110.
113. Anderskewitz, R.; Bauer, R.; Bodenbach, G.; Gester, D.; Gramlich, B.; Morschhauser, G.; Birke, F. W. Bioorg. Med. Chem. Lett. 2005, 15,
669673.
114. Wacker, D. A.; Santella, J. B., III; Gardner, D. S.; Varnes, J. G.; Estrella, M.; DeLucca, G. V.; Ko, S. S.; Tanabe, K.; Watson, P. S.; Welch, P. K.
et al. Bioorg. Med. Chem. Lett. 2002, 12, 17851789.
115. Batt, D. G.; Houghton, G. C.; Roderick, J. R.; Santella, J. B., III; Wacker, D. A.; Welch, P. K.; Orlovsky, Y. I.; Wadman, E. A.; Trzaskos, J. M.;
Davies, P. et al. Bioorg. Med. Chem. Lett. 2005, 15, 787791.
116. Varnes, J. G.; Gardner, D. S.; Santella, J. B., III; Duncia, J. V.; Estrella, M.; Watson, P. S.; Clark, C. M.; Ko, S. S.; Welch, P.; Covington, M. et al.
Bioorg. Med. Chem. Lett. 2004, 14, 16451649.
117. DeLucca, G. V.; Kim, U. T.; Vargo, B. J.; Duncia, J. V.; Santella, J. B., III; Gardner, D. S.; Zheng, C.; Liauw, A.; Wang, Z.; Emmett, G. et al.
J. Med. Chem. 2005, 48, 21942211.
118. Expert Opin. Ther. Patents 2004, 14, 577-582.
119. Vedani, A.; Dobler, M.; Dillinger, H.; Hasselbach, K. M.; Birke, F.; Lill, M. A. J. Med. Chem. 2005, 48, 15151527.
120. Hirai, H.; Tanaka, K.; Yoshie, O.; Ogawa, K.; Kenmotsu, K.; Takamori, Y.; Ichimasa, M.; Sugamura, K.; Nakamura, M.; Takano, S.; Nagata, K.
J. Exp. Med. 2001, 193, 255261.
121. Liu, F.; Gonzalo, J. A.; Manning, S.; OConnell, L. E.; Fedyk, E. R.; Burke, K. E.; Elder, A. M.; Pulido, J. C.; Cao, W.; Tayber, O. et al.
Prostaglandins Leukot. Essent. Fatty Acids 2005, 76, 133147.
122. Sinigaglia, F.; Bordignon, P. P.; dAmbrosio, D. Clin. Exp. Allergy Rev. 2004, 4, 167170.
123. Hirai, H.; Tanaka, K.; Takano, S.; Ichimasa, M.; Nakamura, M.; Nagata, K. J. Immunol. 2002, 165, 981985.
124. Gervais, F. G.; Morello, J.-P.; Beaulieu, C.; Sawyer, N.; Denis, D.; Greig, G.; Malebranche, D.; ONeill, G. P. Mol. Pharmacol. 2005, 67,
18341839.
125. Hata, A. N.; Lybrand, T. P.; Marnett, L. J.; Breyer, R. M. Mol. Pharmacol. 2005, 67, 640647.
126. Sugimoto, H.; Shichijo, M.; Iino, T.; Manabe, Y.; Watanabe, A.; Shimazaki, M.; Gantner, F.; Bacon, K. B. J. Pharmacol. Exp. Ther. 2003, 305,
347352.
127. Ohkubo, K.; Gotoh, M. Allergol. Int. 2003, 52, 131138.
128. Aizawa, H.; Shigyo, M.; Nogami, H.; Hirose, T.; Hara, N. Chest 1996, 109, 338342.
129. Robarge, M. J.; Bom, D. C.; Tumey, L. N.; Varga, N.; Gleason, E.; Silver, D.; Song, J.; Murphy, S. M.; Ekema, G.; Doucette, C. et al. Bioorg.
Med. Chem. Lett. 2005, 15, 17491753.
130. Ulven, T.; Kostenis, E. J. Med. Chem. 2005, 48, 897900.
912 Asthma and Chronic Obstructive Pulmonary Disease
131. Expert Opin. Ther. Patents 2005, 15, 115-117.
132. Kabashima, K.; Narumiya, S. Prostaglandins Leukot. Essent. Fatty Acids 2003, 69, 187194.
133. Coleman, R. A.; Kennedy, I.; Humphrey, P. P. A.; Bunce, K.; Lumley, P. In Comprehensive Medicinal Chemistry; Emmet, J. C., Ed.; Pergamon Press:
Oxford, UK, 1989; Vol. 3, pp 643714.
134. Mitsumori, S.; Tsuri, T.; Honma, T.; Hiramatsu, Y.; Okada, T.; Hashizume, H.; Inagaki, M.; Arimura, A.; Yasui, K.; Asanuma, F. et al. J. Med.
Chem. 2003, 46, 24362445.
135. Mitsumori, S.; Tsuri, T.; Honma, T.; Hiramatsu, Y.; Okada, T.; Hashizume, H.; Kida, S.; Inagaki, M.; Arimura, A.; Yasui, K. et al. J. Med. Chem.
2003, 46, 24462455.
136. Torisu, K.; Kobayashi, K.; Iwahashi, M.; Egashira, H.; Nakai, Y.; Okada, Y.; Nanbu, F.; Ohuchida, H.; Nakai, H.; Toda, M. Bioorg. Med. Chem.
Lett. 2004, 14, 45574562.
137. Torisu, K.; Kobayashi, K.; Iwahashi, M.; Nakai, Y.; Onoda, T.; Nagase, T.; Sugimoto, I.; Okada, Y.; Matsumoto, R.; Nanbu, F. et al. Bioorg. Med.
Chem. 2004, 12, 53615378.
138. ONeill, G. The Prostanoid DP1 Receptor as a Target for Respiratory Disease. Proceedings of the 12th International Conference of the Inammation
Research Association, Bolton Landing, NY, Oct 37, 2004.
139. Beaulieu, C.; Wang, Z.; Denis, D.; Greig, G.; Lamontagne, S.; ONeill, G.; Slipetz, D.; Wang, J. Bioorg. Med. Chem. Lett. 2004, 14, 31953199.
140. Giembycz, M. A. Monaldi Arch. Chest. Dis. 2002, 57, 4864.
141. Souness, J. E.; Alsous, D.; Sargent, C. Immunopharmacology 2000, 47, 127162.
142. Giembycz, M. A. Curr. Opin. Pharmacol. 2005, 5, 238244.
143. Souness, J. E.; Rao, S. Cell. Signal. 1997, 9, 227236.
144. Reid, P. Curr. Opin. Investig. Drugs 2002, 3, 11651170.
145. Giembycz, M. A. Expert Opin. Investig. Drugs 2001, 10, 13611379.
146. Christensen, S. B.; Guider, A.; Forster, C. J.; Gleason, J. G.; Bender, P. E.; Karpinski, J. M.; DeWolf, W. E., Jr.; Barnette, M. S.; Underwood, D. C.;
Griswold, D. E. et al. J. Med. Chem. 1998, 41, 821835.
147. Lipworth, B. J. Lancet 2005, 365, 167175.
148. MacKenzie, S. J. Allergol. Int. 2004, 53, 101110.
149. Odingo, J. O. Expert Opin. Ther. Patents 2005, 15, 773787.
150. Ashton, M. J.; Cook, D. C.; Fenton, G.; Karlsson, J. A.; Palfreyman, M. N.; Raeburn, D.; Ratcliffe, A. J.; Souness, J. E.; Thurairatnam, S.;
Vicker, N. J. Med. Chem. 1994, 37, 16961703.
151. Hulme, C.; Poli, G. B.; Huang, F. C.; Souness, J. E.; Djuric, S. W. Bioorg. Med. Chem. Lett. 1998, 8, 175178.
152. Masamune, H.; Cheng, J. B.; Cooper, K.; Eggler, J. F.; Marfat, A.; Marshall, S. C.; Shirley, J. T.; Tickner, J. E.; Umland, J. P.; Vazquez, E. Bioorg.
Med. Chem. Lett. 1995, 5, 19651968.
153. Cheng, J. B.; Cooper, K.; Duplantier, A. J.; Eggler, J. F.; Kraus, K. G.; Marshall, S. C.; Marfat, A.; Masamune, H.; Shirley, J. T.; Tickner, J. E.
et al. Bioorg. Med. Chem. Lett. 1995, 5, 19691972.
154. Guay, D.; Hamel, P.; Blouin, M.; Brideau, C.; Chan, C. C.; Chauret, N.; Ducharme, Y.; Huang, Z.; Girard, M.; Jones, T. R. et al. Bioorg. Med.
Chem. Lett. 2002, 12, 14571461.
155. Frenette, R.; Blouin, M.; Brideau, C.; Chauret, N.; Ducharme, Y.; Friesen, R. W.; Hamel, P.; Jones, T. R.; Laliberte, F.; Li, C. et al. Bioorg. Med.
Chem. Lett. 2002, 12, 30093013.
156. Ducharme, Y.; Friesen, R. W.; Blouin, M.; Co te, B.; Dube, D.; Ethier, D.; Frenette, R.; Laliberte, F.; Mancini, J.; Masson, P. et al. Bioorg. Med.
Chem. Lett. 2003, 13, 19231926.
157. Friesen, R. W.; Ducharme, Y.; Ball, R. G.; Blouin, M.; Boulet, L.; Co te, B.; Frenette, R.; Girard, M.; Guay, D.; Huang, Z. et al. J. Med. Chem.
2003, 46, 24132426.
158. Van der Mey, M.; Boss, H.; Couwenberg, D.; Hatzelmann, A.; Sterk, G. J.; Goubitz, K.; Schenk, H.; Timmerman, H. J. Med. Chem. 2002, 45,
25262533.
159. Van der Mey, M.; Boss, H.; Hatzelmann, A.; Van der Laan, I. J.; Sterk, G. J.; Timmerman, H. J. Med. Chem. 2002, 45, 25202525.
160. Krier, M.; de Araujo-Junior, J. X.; Schmitt, M.; Duranton, J.; Justiano-Basaran, H.; Lugnier, C.; Bourguignon, J. J.; Rogna Van der Mey, M.;
Boss, H.; Couwenberg, D. et al. J. Med. Chem. 2005, 48, 38163822.
161. Ochiai, H.; Ohtani, T.; Ishida, A.; Kishikawa, K.; Obata, T.; Nakai, H.; Toda, M. Bioorg. Med. Chem. Lett. 2004, 14, 13231327.
162. Andres, J. I.; Alonso, J. M.; D az, A.; Ferna ndez, J.; Iturrino, L.; Mart nez, P.; Matesanz, E.; Freyne, E. J.; Deroose, F.; Boeckx, G. et al. Bioorg.
Med. Chem. Lett. 2002, 12, 653658.
163. Stafford, J. A.; Feldman, P. L.; Marron, B. E.; Schoenen, F. J.; Valvano, N. L.; Unwalla, R. J.; Domanico, P. L.; Brawley, E. S.; Leesnitzer, M. A.;
Rose, D. A. et al. Bioorg. Med. Chem. Lett. 1994, 4, 18551860.
164. Hulme, C.; Mathew, R.; Moriarty, K.; Miller, B.; Ramanjulu, M.; Cox, P.; Souness, J.; Page, K. M.; Uhl, J.; Travis, J. et al. Bioorg. Med. Chem. Lett.
1998, 8, 30533058.
165. Hulme, C.; Moriarty, K.; Miller, B.; Mathew, R.; Ramanjulu, M.; Cox, P.; Souness, J.; Page, K. M.; Uhl, J.; Travis, J. et al. Bioorg. Med. Chem. Lett.
1998, 8, 18671872.
166. Regan, J.; Bruno, J.; McGarry, D.; Poli, G.; Hanney, B.; Bower, S.; Travis, J.; Sweeney, D.; Miller, B.; Souness, J. et al. Bioorg. Med. Chem. Lett.
1998, 8, 27372742.
167. Napoletano, M.; Norcini, G.; Pellacini, F.; Marchini, F.; Morazzoni, G.; Ferlenga, P.; Pradella, L. Bioorg. Med. Chem. Lett. 2000, 10, 22352238.
168. Napoletano, M.; Norcini, G.; Pellacini, F.; Marchini, F.; Morazzoni, G.; Ferlenga, P.; Pradella, L. Bioorg. Med. Chem. Lett. 2001, 11, 3337.
169. Napoletano, M.; Norcini, G.; Pellacini, F.; Marchini, F.; Morazzoni, G.; Fattori, R.; Ferlenga, P.; Pradella, L. Bioorg. Med. Chem. Lett. 2002, 12, 58.
170. Pascal, Y.; Andrianjara, C. R.; Auclair, E.; Avenel, N.; Bertin, B.; Calvet, A.; Feru, F.; Lardon, S.; Moodley, I.; Ouagued, M. et al. Bioorg. Med.
Chem. Lett. 2000, 10, 3538.
171. Devillers, I.; Pevet, I.; Jacobelli, H.; Durand, C.; Fasquelle, V.; Puaud, J.; Gaudilliere, B.; Idrissi, M.; Moreau, F.; Wrigglesworth, R. Bioorg. Med.
Chem. Lett. 2004, 14, 33033306.
172. Burnouf, C.; Auclair, E.; Avenel, N.; Bertin, B.; Bigot, C.; Calvet, A.; Chan, K.; Durand, C.; Fasquelle, V.; Feru, F. et al. J. Med. Chem. 2000, 43,
48504867.
173. Manallack, D. T.; Hughes, R. A.; Thompson, P. E. J. Med. Chem. 2005, 48, 34493462.
174. Conti, M. Nat. Struct. Mol. Biol. 2004, 11, 809810.
175. Card, G. L.; Blasdel, L.; England, B. P.; Zhang, C.; Suzuki, Y.; Gillette, S.; Fong, D.; Ibrahim, P. N.; Artis, D. R.; Bollag, G. et al. Nat. Biotechnol.
2005, 23, 201207.
Asthma and Chronic Obstructive Pulmonary Disease 913
176. Schwartz, L. B.; Irani, A. M. A.; Roller, K.; Castells, M. C.; Schechter, N. M. J. Immunol. 1987, 138, 26112615.
177. Pereira, P. J. B.; Bergner, A.; Macedo-Riberiro, S.; Huber, G.; Matschiner, G.; Fritz, H.; Sommerhoff, C. P.; Bode, W. Nature 1998, 392, 306.
178. Sommerhoff, C. P.; Bode, W.; Matschiner, G.; Bergner, A.; Fritz, H. Biochim. Biophys. Acta 2000, 1477, 7589.
179. Schwartz, L. B.; Bradford, T. R. J. Biol. Chem. 1986, 261, 73727379.
180. Selwood, T.; Smolensky, H.; McCaslin, D. R.; Schechter, N. M. Biochemistry 2005, 44, 35803590.
181. Burgess, L. E. Drug News Perspect. 2000, 13, 147157.
182. Gangloff, A. R. Curr. Opin. Invest. Drugs 2000, 1, 7985.
183. Carins, J. A. Pulm. Pharmacol. Ther. 2005, 18, 5566.
184. Rice, K. D.; Sprengeler, P. A. Curr. Opin. Drug Disc. Dev. 1999, 2, 463474.
185. Clark, J. M.; Moore, W. R.; Tanaka, R. D. Drugs Future 1996, 21, 811816.
186. Caughey, G. H.; Raymond, W. W.; Bacci, E.; Lombardy, R. J.; Tidwell, R. R. J. Pharmacol. Exp. Ther. 1993, 264, 676682.
187. Combrink, K. D.; Gulgeze, H. B.; Meanwell, N. A.; Pearce, B. C.; Zulan, P.; Bisacchi, G. S.; Roberts, D. G. M.; Stanley, P.; Seiler, S. M. J. Med.
Chem. 1998, 41, 48544860.
188. Costanzo, M. J.; Yabut, S. C.; Almond, A. R.; Andrade-Gordon, P.; Corcoran, T. W.; deGaravilla, L.; Kauffman, J. A.; Abraham, W. M.; Recacha,
R.; Chattopadhyay, D. et al. J. Med. Chem. 2003, 46, 38653876.
189. Murakami, Y.; Takei, M.; Shindo, K.; Kitazume, J.; Tanaka, J.; Higa, T.; Fukamachi, H. J. Nat. Prod. 2002, 65, 259261.
190. Yu, K. L.; Civiello, R.; Roberts, D. G. M.; Seiler, S. M.; Meanwell, N. A. Bioorg. Med. Chem. Lett. 1999, 9, 663666.
191. Qian, X.; Zheng, B.; Burke, B.; Saindane, M. T.; Kronenthal, D. R. J. Org. Chem. 2002, 67, 3595-3600 (and references cited therein).
192. Levell, J.; Astles, P.; Eastwood, P.; Carins, J.; Houille, O.; Aldous, S.; Merriman, G.; Whiteley, B.; Pribish, J.; Czekaj, M. et al. Bioorg. Med. Chem.
2005, 13, 28592872.
193. Hopkins, C. R.; Czekaj, M.; Kaye, S. S.; Gao, Z.; Pribish, J.; Pauls, H.; Liang, G.; Sides, K.; Cramer, D.; Carins, J. et al. Bioorg. Med. Chem. Lett.
2005, 15, 27342737.
194. Martin, T. J. Fifth International Electronic Conference on Synthetic Organic Chemistry (ECSOC-5), Sep 2001, C0011. http://www.mdpi.org/
(accessed April 2006).
195. Vaz, R. J.; Gao, Z.; Pribish, J.; Chen, X.; Levell, J.; Davis, L.; Albert, E.; Brollo, M.; Ugolini, A.; Cramer, D. M. et al. Bioorg. Med. Chem. Lett.
2004, 14, 60536056.
196. Hallgren, J.; Estrada, S.; Karlson, U.; Alving, K.; Pejler, G. Biochemistry 2001, 40, 73427349.
197. Cregar, L.; Elrod, K. C.; Putnam, D.; Moore, W. R. Arch. Biochem. Biophys. 1999, 366, 125130.
198. Miller, H. R. P.; Pemberton, A. D. Immunology 2002, 105, 375390.
199. DellItalia, L. J.; Husain, A. Curr. Opin. Cardiol. 2002, 17, 374379.
200. Maryanoff, B. E. J. Med. Chem. 2004, 47, 769787.
201. Doggrell, S. A.; Wanstall, J. C. Expert Opin. Invest. Drugs 2003, 12, 14291432.
202. Akahoshi, F.; Ashimori, A.; Sakashita, H.; Yoshimura, T.; Eda, M.; Imada, T.; Nakajima, M.; Mitsutomi, N.; Kuwahara, S.; Ohtsuka, T. et al.
J. Med. Chem. 2001, 44, 12971304.
203. Akahoshi, F.; Ashimori, A.; Sakashita, H.; Yoshimura, T.; Imada, T.; Nakajima, M.; Mitsutomi, N.; Kuwahara, S.; Ohtsuka, T.; Fukaya, C. et al.
J. Med. Chem. 2001, 44, 12851296.
204. Akahoshi, F. Drugs Future 2002, 27, 765770.
205. Muto, T.; Fukami, H. IDrugs 2002, 5, 11411150.
206. Aoyama, Y.; Uenaka, M.; Konoike, T.; Iso, Y.; Nishitani, Y.; Kanda, A.; Naya, N.; Nakajima, M. Bioorg. Med. Chem. Lett. 2000, 10, 23972401.
207. Aoyama, Y.; Uenaka, M.; Kii, M.; Tanaka, M.; Konoike, T.; Hayasaki-Kajiwara, Y.; Naya, N.; Nakajima, M. Bioorg. Med. Chem. 2001, 9,
30653075.
208. Greenfeder, S.; Umland, S. P.; Cuss, F. M.; Chapman, R. W.; Egan, R. W. Respir. Res. 2001, 2, 7179.
209. Uings, I.; McKinnon, M. Curr. Pharma. Des. 2002, 8, 18371844.
210. Minnicozzi, M. Expert Opin. Ther. Patents 1999, 9, 147156.
211. Miyajima, A.; Kitamura, T.; Harada, N.; Yokota, T.; Arai, K. Annu. Rev. Immunol. 1992, 10, 295331.
212. Morokata, T.; Suzuki, K.; Ida, K.; Yamada, T. Immunol. Lett. 2005, 98, 161165.
213. Morokata, T.; Ida, K.; Yamada, T. Int. Immunol. 2002, 2, 16931702.
214. Devos, R.; Guisez, Y.; Plaetinck, G.; Cornelis, S.; Tavernier, J.; Van der Heuden, J.; Foley, L. H.; Schefer, G. Eur. J. Biochem. 1994, 225,
635640.
215. Wiekowski, M.; Prosser, D.; Taremi, S.; Tsarbopoulos, A.; Jenh, C. H.; Chou, C. C.; Lundell, D.; Zavodny, P.; Narula, S. Eur. J. Biochem. 1997,
246, 625632.
216. Van Wauwe, J.; Aerts, F.; Cools, M.; Deroose, F.; Freyne, E.; Goossens, J.; Hermans, B.; Lacrampe, J.; Van Genechten, H.; Van Gerven, F. et al.
J. Pharmacol. Exp. Ther. 2000, 295, 655661.
217. Freyne, E. J.; Lacrampe, J. F.; Deroose, F.; Boeckx, G. M.; Willems, M.; Embrechts, W.; Coesemans, E.; Willems, J. J.; Fortin, J. M.; Ligney, Y.
et al. J. Med. Chem. 2005, 48, 21672175.
218. Williams, T. J. J. Clin. Invest. 2004, 113, 507509.
219. OByrne, P. M.; Inman, M. D.; Parameswaran, K. J. Allergy Clin. Immunol. 2001, 503-508.
220. Samuelson, B. Science 1983, 220, 568.
221. Werz, O.; Steinhilber, D. Expert Opin. Ther. Patents 2005, 15, 505519.
222. Chen, X. S.; Naumann, T. A.; Kurre, U.; Jenkins, N. A.; Copeland, N. G.; Funk, C. D. J. Biol. Chem. 1995, 270, 1799317999 (and references
cited therein).
223. Carter, G. W.; Young, P. R.; Albert, D. H.; Bouska, J. B.; Dyer, R. D.; Bell, R. L.; Summers, J. B.; Brooks, D. W.; Rubin, P. R.; Kesterson, J. In
Leukotrienes and Prostanoids in Health and Disease, New Trends in Lipid Mediators Research; Zor, U., Naor, Z., Danon, A., Eds.; Karger: Basel,
Switzerland, 1989; Vol. 3, pp 5055.
224. Brooks, C. D. W.; Stewart, A. O.; Kolasa, T.; Basha, A.; Bhatia, P.; Ratajczyk, J. D.; Craig, R. A.; Gunn, D.; Harris, R. A.; Bouska, J. B. et al. Pure
Appl. Chem. 1998, 70, 271274.
225. Stewart, A. O.; Bhatia, P. A.; Martin, J. G.; Summers, J. B.; Rodriques, K. E.; Martin, M. B.; Holms, J. H.; Moore, J. L.; Craig, R. A.; Kolasa, T.
et al. J. Med. Chem. 1997, 40, 19551968.
226. Brooks, C. D. W.; Stewart, A. O.; Basha, A.; Bhatia, P.; Ratajczyk, J. D.; Martin, J. G.; Craig, R. A.; Kolasa, T.; Bouska, J. B.; Lanni, C. et al.
J. Med. Chem. 1995, 38, 47684775.
914 Asthma and Chronic Obstructive Pulmonary Disease
227. Lewis, T. A.; Bayless, L.; DiPesa, A. J.; Eckman, J. B.; Gillard, M.; Libertine, L.; Scannell, R. T.; Wypij, D. M.; Young, M. A. Bioorg. Med. Chem.
Lett. 2005, 15, 10831085.
228. Wright, S. W.; Pinto, D. J.; Sherk, S. R.; Green, A. M.; Magolda, R. L.; Bioorg. Med. Chem. Lett. 1992, 2, 10791084.
229. Mano, T.; Stevens, R. W.; Ando, K.; Nakao, K.; Okumura, Y.; Sakakibara, M.; Okumura, T.; Tamura, T.; Miyamoto, K. Bioorg. Med. Chem. 2003,
11, 38793887.
230. Mano, T.; Stevens, R. W.; Okumura, Y.; Kawai, M.; Okumura, T.; Sakaibara, M. Bioorg. Med. Chem. Lett. 2005, 15, 26112615.
231. Mano, T.; Okumura, Y.; Sakaibara, M.; Okumura, T.; Tamura, T.; Miyamoto, K.; Stevens, R. W. J. Med. Chem. 2004, 47, 720725.
232. Young, R. N.; Gillard, J. W.; Hutchinson, J. H.; Leger, S.; Prasit, P. J. Lipid Mediators 1993, 6, 233238.
233. Prasit, P.; Belley, M.; Brideau, C.; Chan, C.; Charleson, S.; Evans, J. F.; Fortin, R.; Ford-Hutchinson, A. W.; Gillard, J. W.; Guay, J. et al. Bioorg.
Med. Chem. Lett. 1992, 2, 13951398.
234. OByrne, P. M.; Israel, E.; Deazen, J. M. Ann. Int. Med. 1997, 127, 472480.
235. Friedman, B. S.; Bel, E. H.; Buntinx, A.; Tanaka, W.; Han, Y.; Shingo, S.; Spector, R.; Sterk, P. Am. Rev. Respir. Dis. 1993, 147, 839844.
236. Bel, E. H.; Tanaka, W.; Spector, R.; Freidman, B.; VondeVeen, J. H.; Dijkman, J. H.; Sterk, P. J. Am. Rev. Respir. Dis. 1990, 141, A31.
237. Kolasa, T.; Gunn, D. E.; Bhatia, P.; Woods, K. W.; Gane, T.; Stewart, A. O.; Bouska, J. B.; Harris, R. R.; Hulkower, K. I.; Malo, P. E. et al. J. Med.
Chem. 2000, 43, 690705.
238. Kolasa, T.; Gunn, D. E.; Bhatia, P.; Basha, A.; Craig, R. A.; Stewart, A. O.; Bouska, J. B.; Harris, R. R.; Hulkower, K. I.; Malo, P. E. et al. J. Med.
Chem. 2000, 43, 33223334.
239. Nayak, A. Expert Opin. Pharmacother. 2004, 5, 679686.
240. Turner, C. R.; Smith, W. B.; Andresen, C. J.; Swindell, A. C.; Watson, J. W. Pulmon. Pharmacol. 1994, 7, 4958.
241. Nabe, T.; Kohno, S.; Tanpo, T.; Saeki, Y.; Yarnamura, H.; Horiba, M.; Ohata, K. Prostaglandins Leukot. Essent. Fatty Acids 1994, 51, 163171.
242. Dahlen, S.; Hedqvist, P.; Hammarstrom, S.; Samuelsson, S. Nature 1980, 4, 484486.
243. Murphy, R.; Hammarstrom, C. S.; Samuelsson, B. Proc. Natl. Acad. Sci. USA 1979, 76, 42754279.
244. Zamboni, R.; Belley, M.; Champion, E.; Charette, L.; DeHaven, R.; Frenette, R.; Gauthier, J. Y.; Jones, T. R.; Leger, S.; Masson, P. et al. J. Med.
Chem. 1992, 35, 38323844.
245. Labelle, M.; Belley, M.; Gareau, Y.; Gauthier, J. Y.; Guay, D.; Gordon, R.; Grossman, S. G.; Jones, T. R.; Leblanc, Y.; McAuliffe, M. et al. Bioorg.
Med. Chem. Lett. 1995, 5, 283288.
246. Nakagawa, T.; Mizushima, Y.; Ishii, A.; Nambu, F.; Motoishi, M.; Yui, Y.; Shida, T.; Miyamoto, T. Adv. Prostaglandin Thromboxane Leukot. Res.
1991, 21a, 465.
247. Fujimura, M.; Sakahoto, S.; Kamis, Y.; Matsuda, T. Respir. Med. 1993, 87, 133.
248. Matassa, V. G.; Maduskuie, T. P., Jr.; Shapiro, H. S.; Hesp, B.; Snyder, D. W.; Aharony, D.; Krell, R. D.; Keith, R. A. J. Med. Chem. 1990, 33,
17811790.
249. Brown, F. J.; Yee, Y. K.; Cronk, L. A.; Hebbel, K. C.; Krell, R. D.; Snyder, D. W. J. Med. Chem. 1990, 33, 17711781.
250. Dasari, V. R.; Jin, J.; Kunapuli, S. P. Immunopharmacology 2000, 48, 157163.
251. Sawyer, J. S.; Baldwin, R. F.; Froelich, L. L.; Saussy, D. L., Jr.; Jackson, W. T. Bioorg. Med. Chem. Lett. 1993, 3, 19811984.
252. Soa, M. J.; Jackson, W. T.; Saussy, D. L., Jr.; Silbaugh, S. A.; Froelich, L. L.; Cockerham, S. L.; Stengel, P. W. Bioorg. Med. Chem. Lett. 1992, 2,
16691674.
253. Kawakami, H.; Ohmi, N.; Nagata, H. Bioorg. Med. Chem. Lett. 1994, 4, 14611466.
254. Koch, K.; Melvin, L. S.; Reiter, L. A.; Biggers, M. S.; Showell, H. J.; Grifths, R. J.; Pettipher, E. R.; Cheng, J. B.; Milici, A. J.; Breslow, R. et al.
J. Med. Chem. 1994, 37, 31973199 (and references cited therein).
255. Greenspan, P. D.; Main, A. J.; Bhagwat, S. S.; Barsky, L. I.; Doti, R. A.; Engle, A. R.; Frey, L. M.; Zhou, H.; Lipson, K. E.; Chin, M. H. et al.
Bioorg. Med. Chem. Lett. 1997, 7, 949954.
256. Reiter, L. A.; Melvin, L. S., Jr.; Crean, G. L.; Showell, H. J.; Koch, K.; Biggers, M. S.; Cheng, J. B.; Breslow, R.; Conklyn, M. J.; Farrell, C. A.
et al. Bioorg. Med. Chem. Lett. 1997, 7, 23072312.
257. Koch, K.; Melvin, L. S.; Reiter, L. A.; Biggers, M. S.; Showell, H. J.; Pettipher, E. R.; Hackman, B.; Cheng, J. B.; Milici, A. J.; Breslow, R. et al.
In 7th International Conference of the Inammation Research Association, White Haven, PA, 1994, W6.
258. Penning, T. D.; Askonas, L. J.; Djuric, S. W.; Haack, R. A.; Yu, S. S.; Michener, M. L.; Krivi, G. G.; Pyla, E. Y. Bioorg. Med. Chem. Lett. 1995, 5,
25172522.
259. Penning, T. D. Curr. Pharmac. Des. 2001, 7, 163179 (and references cited therein).
260. Penning, T. D.; Chandrakumar, N. S.; Desai, B. N.; Djuric, S. W.; Gasiecki, A. F.; Liang, C. D.; Miyashiro, J. M.; Russell, M. A.; Askonas, L. J.;
Gierse, J. K. et al. Bioorg. Med. Chem. Lett. 2002, 12, 33833386.
Asthma and Chronic Obstructive Pulmonary Disease 915
Biographies
Gregory P Roth, PhD, is currently Associate Director of Medicinal Chemistry at the Abbott Bioresearch Center
located in Worcester, MA. Greg obtained his doctorate degree in asymmetric synthesis under the supervision of Prof
Albert I Meyers at Colorado State University in 1988. Prior to joining Abbott Laboratories, Greg contributed to drug
discovery efforts at Bristol-Myers Squibb starting in 1988 and then joined Boehringer Ingelheim Pharmaceuticals in
1994 where he was involved in process research, combinatorial chemistry, and immunoscience-based drug discovery
programs.
David W Green, PhD, is Senior Associate Director of High Throughput Screening and Molecular Phamacology at
Amgen, Inc. in Cambridge, MA. He received his graduate training in mechanistic enzymology at the University of Iowa
with Prof Bryce V Plapp (PhD, 1988) and as a postdoctoral fellow in Monsanto Corporate Research. He joined
SmithKline Beecham in 1989 and contributed to anti-inammatory and antiviral drug discovery teams. David went on
to lead cardiovascular drug discovery programs at Bristol-Myers Squibb before managing enzymology and HTS groups
involved in structure-based drug design at 3-Dimensional and Cubist Pharmaceuticals. Before joining Amgen, he was
Associate Director of Molecular and Cellular Biology at Abbott Bioresearch Center where his responsibilities included
leading projects targeting cellular receptors for the development of anti-inammatory drugs.
& 2007 Elsevier Ltd. All Rights Reserved Comprehensive Medicinal Chemistry II
No part of this publication may be reproduced, stored in any retrieval system or transmitted
in any form by any means electronic, electrostatic, magnetic tape, mechanical, photocopying,
recording or otherwise, without permission in writing from the publishers
ISBN (set): 0-08-044513-6
ISBN (Volume 7) 0-08-044520-9; pp. 873916
916 Asthma and Chronic Obstructive Pulmonary Disease
Вам также может понравиться
- HSNS264 Assessment 1Документ6 страницHSNS264 Assessment 1Sophie AndersonОценок пока нет
- COPD ExacerbationДокумент12 страницCOPD ExacerbationJeffrey ShermanОценок пока нет
- Tail PCR ProtocolДокумент4 страницыTail PCR ProtocolFelipe ZapataОценок пока нет
- LymphomaДокумент78 страницLymphomaastriwahyuni100% (4)
- Chronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepДокумент55 страницChronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepGlory Stefanny NorotumilenaОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент37 страницChronic Obstructive Pulmonary Diseasematchees-gone rogueОценок пока нет
- Case PresentationДокумент12 страницCase PresentationMary Mae BuellaОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент8 страницChronic Obstructive Pulmonary DiseaseGeozel VivienneОценок пока нет
- COPD2019Документ9 страницCOPD2019ClintonОценок пока нет
- Sam CD Asthma ReciveredДокумент36 страницSam CD Asthma ReciveredDr. Muha. Hasan Mahbub-Ur-RahmanОценок пока нет
- Chapter 10 Interstitial Lung DiseaseДокумент10 страницChapter 10 Interstitial Lung DiseaseAleksandar Tasic100% (1)
- Description: Chronic Bronchitis EmphysemaДокумент16 страницDescription: Chronic Bronchitis EmphysemaJay-ar Zars0% (1)
- Asthma: A. Practice EssentialsДокумент8 страницAsthma: A. Practice EssentialsCandha NurcahyaОценок пока нет
- Hide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyДокумент29 страницHide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyAngie Mandeoya100% (1)
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesДокумент17 страницAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengОценок пока нет
- 3 CopdДокумент17 страниц3 Copdshanfiza_92Оценок пока нет
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of LiteratureДокумент5 страницPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of Literatureamelya asryОценок пока нет
- An Understanding of The Genetic Basis of Asthma: Review ArticleДокумент13 страницAn Understanding of The Genetic Basis of Asthma: Review ArticlerastiooОценок пока нет
- Allergy-Asthma ConnectionДокумент11 страницAllergy-Asthma ConnectionLaras Bani WasesoОценок пока нет
- Acute Severe AsthmaДокумент5 страницAcute Severe AsthmaRizsa Aulia DanestyОценок пока нет
- NatureDP 2015 Chronic Obstructive Pulmonary DiseaseДокумент21 страницаNatureDP 2015 Chronic Obstructive Pulmonary DiseasePaloma GBОценок пока нет
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofДокумент12 страницChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanОценок пока нет
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofДокумент12 страницChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент8 страницChronic Obstructive Pulmonary DiseaseYessamin Paith RoderosОценок пока нет
- The EssayДокумент33 страницыThe EssayAnonymous bLaVaKSbdBОценок пока нет
- Adult Asthma: Key PointsДокумент10 страницAdult Asthma: Key PointsDejan ŽujovićОценок пока нет
- Chronic Obstructive Pulmonary Disease: Prof. Ma. Nancy T. MartinezДокумент24 страницыChronic Obstructive Pulmonary Disease: Prof. Ma. Nancy T. MartinezKrizzia Charmaine Rallonza BaggayanОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент5 страницChronic Obstructive Pulmonary DiseaseElvando SimatupangОценок пока нет
- Immunology of Asthma and ChronicДокумент10 страницImmunology of Asthma and ChronicMeldaОценок пока нет
- Chronic Lower Respiratory DiseaseДокумент3 страницыChronic Lower Respiratory DiseaseRonie PatuboОценок пока нет
- Astm SeverДокумент18 страницAstm SeverCristian GrigorasОценок пока нет
- GM 112Документ10 страницGM 112Thanasis PapatheodorouОценок пока нет
- Copd 2Документ26 страницCopd 2Abid SunhanОценок пока нет
- Age Related Changes in Respiratory System I. Structural Changes 1. Lung Elasticity: II. Functional ChangesДокумент4 страницыAge Related Changes in Respiratory System I. Structural Changes 1. Lung Elasticity: II. Functional ChangesElienai de LeonОценок пока нет
- Nursing Care Management 103 Cap MRДокумент9 страницNursing Care Management 103 Cap MRkarenfaye00Оценок пока нет
- DR Ambreen Shams NephrologistДокумент58 страницDR Ambreen Shams NephrologistAamer NaeemОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент28 страницChronic Obstructive Pulmonary DiseaseZhe Kang LimОценок пока нет
- Small Airways Disease, A Condition in Which Small Bronchioles Are NarrowedДокумент30 страницSmall Airways Disease, A Condition in Which Small Bronchioles Are Narrowedanon_396086051Оценок пока нет
- Evaluationandtreatmentof Chroniccough: Genji Terasaki,, Douglas S. PaauwДокумент13 страницEvaluationandtreatmentof Chroniccough: Genji Terasaki,, Douglas S. PaauwRSU DUTA MULYAОценок пока нет
- 1 s2.0 S0025712522000244 MainДокумент13 страниц1 s2.0 S0025712522000244 Mainlmra89Оценок пока нет
- Immunology of Asthma and Chronic Obstructive Pulmonary DiseaseДокумент10 страницImmunology of Asthma and Chronic Obstructive Pulmonary DiseaseClaudio Luis VenturiniОценок пока нет
- An Overview: Chronic Obstructive Pulmonary DiseaseДокумент9 страницAn Overview: Chronic Obstructive Pulmonary Diseaseulfiandi rizkiОценок пока нет
- EmphysemaДокумент29 страницEmphysemaMisheel OrgilsaikhanОценок пока нет
- Chronic Obstructive Pulmonary Disease: Continuing Education ActivityДокумент11 страницChronic Obstructive Pulmonary Disease: Continuing Education ActivityBBD BBDОценок пока нет
- Chronic Obstructive Pulmonary Disease in Elderly PatientsДокумент14 страницChronic Obstructive Pulmonary Disease in Elderly PatientsFranz MiguelОценок пока нет
- Barnes2015 2Документ21 страницаBarnes2015 2Lourdes ColomaОценок пока нет
- CopdДокумент155 страницCopdDian zaini PutraОценок пока нет
- Chronic Obstructive Pulmonary DiseasesДокумент7 страницChronic Obstructive Pulmonary DiseasesGeoffreyОценок пока нет
- Therefore Proper and Early Management of COPD Is NeededДокумент11 страницTherefore Proper and Early Management of COPD Is NeededAwliyatul FitriyahОценок пока нет
- Practice EamДокумент35 страницPractice EamMYKRISTIE JHO MENDEZОценок пока нет
- Copd Exacerbations in EdДокумент23 страницыCopd Exacerbations in EdEzequiel MenesesОценок пока нет
- Acute Respiratory InfectionДокумент28 страницAcute Respiratory InfectionMazharОценок пока нет
- Status AsthmaticusДокумент22 страницыStatus AsthmaticusGali Kesuma100% (1)
- SL NO Content NOДокумент12 страницSL NO Content NOPdianghunОценок пока нет
- Chronic Obstructive Pulmonary DiseaseДокумент17 страницChronic Obstructive Pulmonary DiseaseMark Adrian Jintalan ManzanoОценок пока нет
- COPD NotesДокумент38 страницCOPD NotesKudingLimMingYaoОценок пока нет
- Emphysema BrochureДокумент2 страницыEmphysema Brochureapi-242394302Оценок пока нет
- Fiopatologia EPOCДокумент9 страницFiopatologia EPOCJames D. EspinozaОценок пока нет
- Asthma in The Primary Care Setting 2019 Medical Clinics of North AmericaДокумент18 страницAsthma in The Primary Care Setting 2019 Medical Clinics of North AmericaYony Morales LeonОценок пока нет
- Fast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlОт EverandFast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlОценок пока нет
- Diagnosis and Treatment of Chronic CoughОт EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoОценок пока нет
- Rocafort Et Al., 2020 Apoplastic Effector Proteins of Plant-Associated Fungi and Oomycetes PDFДокумент11 страницRocafort Et Al., 2020 Apoplastic Effector Proteins of Plant-Associated Fungi and Oomycetes PDFJuan Muñoz CuellarОценок пока нет
- Effective Microbial Bioremediation Via The Multi-Omics Approach: An Overview of Trends, Problems and ProspectsДокумент19 страницEffective Microbial Bioremediation Via The Multi-Omics Approach: An Overview of Trends, Problems and ProspectsUMYU Journal of Microbiology Research (UJMR)Оценок пока нет
- PCR Troubleshooting-Part 1 "No Bands": Hints, Tips and Trouble Shooting For Molecular Biology TechniciansДокумент6 страницPCR Troubleshooting-Part 1 "No Bands": Hints, Tips and Trouble Shooting For Molecular Biology Technicianssam911101Оценок пока нет
- 155:411 Introduction To Biochemical Engineering Fall 2012 Exam 1 October 10, 2012 From 5:00-8:00 P.MДокумент2 страницы155:411 Introduction To Biochemical Engineering Fall 2012 Exam 1 October 10, 2012 From 5:00-8:00 P.Mmanthan2120% (1)
- E Bio Key Sex Linked 13u899xДокумент4 страницыE Bio Key Sex Linked 13u899xKlynt BasadreОценок пока нет
- Digestive System Exam IIДокумент13 страницDigestive System Exam IIhugomiso100% (3)
- Biology Feynman TechniquesДокумент9 страницBiology Feynman TechniquesmuthulaxmiОценок пока нет
- Biochemistry and MetabolismДокумент8 страницBiochemistry and MetabolismPrincess Angie GonzalesОценок пока нет
- Neural TubeДокумент4 страницыNeural TubeRuth Danielle GasconОценок пока нет
- Pharmacoinformatics: A Tool For Drug DiscoveryДокумент29 страницPharmacoinformatics: A Tool For Drug Discoveryahirebhupendra100% (1)
- Nagarmotha PDFДокумент17 страницNagarmotha PDFMuhammad Vaqar HussainОценок пока нет
- Sagala (2011)Документ8 страницSagala (2011)Ahmad ZulfikarОценок пока нет
- Chapter 10 Kingdom Animalia MCQs PDF Class 11Документ11 страницChapter 10 Kingdom Animalia MCQs PDF Class 11Rahi HabibОценок пока нет
- Anatomy Tubuh ManusiaДокумент12 страницAnatomy Tubuh ManusiaMuhammad YusufОценок пока нет
- Chapter 1.3 Structures and Functions of OrganellesДокумент35 страницChapter 1.3 Structures and Functions of OrganellesFairview PenangОценок пока нет
- Telescopium DewasaДокумент11 страницTelescopium DewasaBayu KrisnaОценок пока нет
- Inducible Expression of Claudin-1-Myc But Not occludin-VSV-G Results in Aberrant Tight Junction Strand Formation in MDCK CellsДокумент12 страницInducible Expression of Claudin-1-Myc But Not occludin-VSV-G Results in Aberrant Tight Junction Strand Formation in MDCK CellsKarina B Hernandez AОценок пока нет
- Drug Development ProcessapolloДокумент19 страницDrug Development Processapollotamara_0021Оценок пока нет
- Lecture 9: Mutualism and Symbiosis Lecture 9: Mutualism and SymbiosisДокумент5 страницLecture 9: Mutualism and Symbiosis Lecture 9: Mutualism and SymbiosisBruce WayneОценок пока нет
- As91603 Plant and Animal ResponsesДокумент2 страницыAs91603 Plant and Animal Responsesapi-323107386Оценок пока нет
- PlanktonДокумент12 страницPlanktonRen ObeñaОценок пока нет
- Conservation of BiodiversityДокумент19 страницConservation of BiodiversityAnkit AgarwalОценок пока нет
- Infection Prevention and Control SpeakerДокумент28 страницInfection Prevention and Control Speakerfouzia100% (2)
- Dissolution of Spike Protein by Nattokinase: Holy Grail of COVID-19 Vaccine DetoxificationДокумент6 страницDissolution of Spike Protein by Nattokinase: Holy Grail of COVID-19 Vaccine DetoxificationtyakimisОценок пока нет
- Digestive SystemДокумент12 страницDigestive SystemdelianamandhitaОценок пока нет
- SDS PageДокумент12 страницSDS PageShadia HeyariОценок пока нет
- SerotoninaДокумент12 страницSerotoninajodieОценок пока нет
- Characteristics of Life UpdatedДокумент12 страницCharacteristics of Life UpdatedYla Mae Buo AcejoОценок пока нет