Академический Документы
Профессиональный Документы
Культура Документы
Ncp-Ineffective Breathing Pattern
Загружено:
Roxanne Ganayo Claver100%(1)100% нашли этот документ полезным (1 голос)
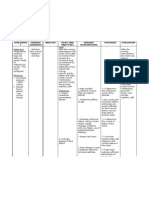
4K просмотров4 страницыNursing Care Plan: ineffective breathing pattern definition: Inspiration and / or expiration that does not provide adequate ventilation. Related Factors - Neuromuscular dysfunction; spinal cord injury; neurological immaturity. - Musculoskeletal impairment; bony / chest wall deformity - Anxiety; [panic attacks] - Pain - Perception / cognitive impairment - Fatigue; [deconditioning]; respiratory muscle fatigue.
Исходное описание:
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документNursing Care Plan: ineffective breathing pattern definition: Inspiration and / or expiration that does not provide adequate ventilation. Related Factors - Neuromuscular dysfunction; spinal cord injury; neurological immaturity. - Musculoskeletal impairment; bony / chest wall deformity - Anxiety; [panic attacks] - Pain - Perception / cognitive impairment - Fatigue; [deconditioning]; respiratory muscle fatigue.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
4K просмотров4 страницыNcp-Ineffective Breathing Pattern
Загружено:
Roxanne Ganayo ClaverNursing Care Plan: ineffective breathing pattern definition: Inspiration and / or expiration that does not provide adequate ventilation. Related Factors - Neuromuscular dysfunction; spinal cord injury; neurological immaturity. - Musculoskeletal impairment; bony / chest wall deformity - Anxiety; [panic attacks] - Pain - Perception / cognitive impairment - Fatigue; [deconditioning]; respiratory muscle fatigue.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
Nursing Care Plan: ineffective Breathing Pattern
May 26, 2012 Nursing Guide No comments
Nursing Care Plan: ineffective Breathing Pattern
Definition: Inspiration and/or expiration that does not provide adequate ventilation.
Related Factors
- Neuromuscular dysfunction; spinal cord injury; neurological immaturity.
- Musculoskeletal impairment; bony/chest wall deformity
- Anxiety; [panic attacks]
- Pain
- Perception/cognitive impairment
- Fatigue; [deconditioning]; respiratory muscle fatigue
- Body position; obesity
- Hyperventilation; hypoventilation syndrome [alteration of clients normal O2:CO2 ratio (e.g., lung diseases, pulmonary
hypertension, airway obstruction, O2 therapy in COPD)]
Defining Characteristics
Subjective
Feeling breathless
Objective
Dyspnea; orthopnea
Bradypnea; tachypnea
Alterations in depth of breathing
Timing ratio; prolonged expiration phases; pursed-lip breathing
Decreased minute ventilation, vital capacity
Decreased inspiratory/expiratory pressure
Use of accessory muscles to breathe; assumption of three-point position
Altered chest excursion; [paradoxical breathing patterns]
Nasal flaring; [grunting]
Increased anterior-posterior diameter
Desired Outcomes/Evaluation Criteria Client Will:
Establish a normal, effective respiratory pattern as evidenced by absence of cyanosis and other signs/symptoms of hypoxia,
with ABGs within clients normal or acceptable range.
Verbalize awareness of causative factors.
Initiate needed lifestyle changes.
Demonstrate appropriate coping behaviors.
Actions/Interventions
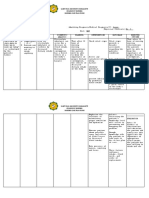
1- Determine presence of factors/physical conditions as noted in Related Factors
Rationale: that would cause breathing impairments.
2- Auscultate chest
Rationale: to evaluate presence/character of breath sounds and secretions.
3- Note rate and depth of respirations, type of breathing pattern (e.g., tachypnea, grunting, Cheyne-Stokes, other irregular
patterns).
4- Evaluate cough (e.g., tight or moist); presence of secretions,
Rationale: indicating possible obstruction.
5- Assist with/review results of necessary testing (e.g., chest xrays, lung volumes/flow studies, pulmonary function/sleep studies)
Rationale: to diagnose presence/severity of lung diseases.
6- Review laboratory data; for example, ABGs
Rationale: (determines degree of oxygenation, CO2 retention); drug screens; and pulmonary function studies (determines vital
capacity/tidal volume).
7- Note emotional responses (e.g., gasping, crying, reports of tingling fingers).
Rationale: Anxiety may be causing or exacerbating acute or chronic hyperventilation.
8- Assess for concomitant pain/discomfort
Rationale: that may restrict respiratory effort.
9- Administer oxygen at lowest concentration indicated and prescribed respiratory medications
Rationale: for management of underlying pulmonary condition, respiratory distress, or cyanosis.
10- Suction airway, as needed,
Rationale: to clear secretions.
11- Assist with bronchoscopy or chest tube insertion as indicated.
12- Elevate head of bed and/or have client sit up in chair, as appropriate,
Rationale: to promote physiological and psychological ease of maximal inspiration.
13- Encourage slower/deeper respirations, use of pursed-lip technique, and so on
Rationale: to assist client in taking control of the situation.
14- Have client breathe into a paper bag, if appropriate,
Rationale: to correct hyperventilation. (Research suggests this may not be effective and could actually stress the heart/respiratory
system, potentially lowering O2 saturation, especially if the hyperventilation is not simply anxiety based.)
15- Monitor pulse oximetry, as indicated,
Rationale: to verify maintenance/ improvement in O2 saturation.
16- Maintain calm attitude while dealing with client and SO(s)
Rationale: to limit level of anxiety.
17- Assist client in the use of relaxation techniques.
18- Deal with fear/anxiety that may be present. (Refer to NDs Fear; Anxiety.)
19- Encourage position of comfort. Reposition client frequently if immobility is a factor.
20- Splint rib cage during deep-breathing exercises/cough, if indicated.
21- Medicate with analgesics, as appropriate,
Rationale: to promote deeper respiration and cough. (Refer to NDs acute Pain; chronic Pain.)
22- Encourage ambulation/exercise, as individually indicated.
23- Avoid overeating/gas-forming foods
Rationale: that may cause abdominal distention.
24- Provide/encourage use of adjuncts, such as incentive spirometer,
Rationale: to facilitate deeper respiratory effort.
25- Supervise use of respirator/diaphragmatic stimulator, rocking bed, apnea monitor, and so forth
Rationale: when neuromuscular impairment is present.
26- Ascertain that client possesses and properly operates continuous positive airway pressure (CPAP) machine
Rationale: when obstructive sleep apnea is causing breathing problems.
27- Maintain emergency equipment in readily accessible location and include age/size appropriate ET/trach tubes (e.g., infant,
child, adolescent, or adult) Rationale: when ventilatory support might be needed.
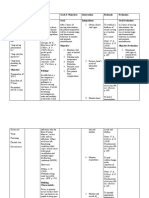
28- Review etiology and possible coping behaviors.
29- Stress importance of good posture and effective use of accessory musclesRationale: to maximize respiratory effort.
30- Teach conscious control of respiratory rate, as appropriate.
31- Assist client in breathing retraining (e.g., diaphragmatic, abdominal breathing, inspiratory resistive, and pursed-lip), as
indicated.
32- Recommend energy conservation techniques and pacing of activities.
33- Refer for general exercise program (e.g., upper and lower extremity endurance and strength training), as indicated,
Rationale: to maximize clients level of functioning.
34- Encourage adequate rest periods between activities
Rationale: to limit fatigue.
35- Discuss relationship of smoking to respiratory function.
36- Encourage client/SO(s) to develop a plan for smoking cessation. Provide appropriate referrals.
37- Review environmental factors (e.g., exposure to dust, high pollen counts, severe weather, perfumes, animal dander,
household chemicals, fumes, secondhand smoke; insufficient home support for safe care)
Rationale: that may require avoidance of triggers or modification of lifestyle or environment to limit
impact on clients breathing.
38- Advise regular medical evaluation with primary care provider
Rationale: to determine effectiveness of current therapeutic regimen and to promote general well-being.
39- Instruct in proper use and safety concerns for home oxygen therapy, as indicated.
40- Make referral to support groups/contact with individuals who have encountered similar problems.
Documentation Focus
Assessment/Reassessment
Relevant history of problem.
Respiratory pattern, breath sounds, use of accessory muscles.
Laboratory values.
Use of respiratory aids or supports, ventilator settings, and so forth.
Planning
Plan of care, specific interventions, and who is involved in the planning.
Teaching plan.
Implementation/Evaluation
Response to interventions, teaching, actions performed, and treatment regimen.
Mastery of skills, level of independence.
Attainment or progress toward desired outcome(s).
Modifications to plan of care.
Discharge Planning
Long-term needs, including appropriate referrals and action taken, available resources.
Specific referrals provided.
Вам также может понравиться
- Ineffective Breathing PatternДокумент5 страницIneffective Breathing PatternruguОценок пока нет
- Impaired Gas ExchangeДокумент2 страницыImpaired Gas ExchangeHanya Bint PotawanОценок пока нет
- Nursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisДокумент2 страницыNursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisFatima Zainab Matlih IdjiraniОценок пока нет
- NCP-Deficient Fluid VolumeДокумент1 страницаNCP-Deficient Fluid Volumejanmichael8Оценок пока нет
- Ineffective Breathing PatternДокумент2 страницыIneffective Breathing PatternJoy Arizala CarasiОценок пока нет
- Worksheet#2-Maintaining Asepsis: Medical Asepsis Includes All Practices Intended To Confine A SpecificДокумент4 страницыWorksheet#2-Maintaining Asepsis: Medical Asepsis Includes All Practices Intended To Confine A SpecificCj MayoyoОценок пока нет
- Ineffective Breathing PatternДокумент8 страницIneffective Breathing PatternJansen Arquilita Rivera100% (2)
- Nursing Care Plan Problem: Acute Intermittent Moderate PainДокумент1 страницаNursing Care Plan Problem: Acute Intermittent Moderate PainDiana Laura Lei100% (3)
- NCP Ineffective Breathing Pattern TalaДокумент1 страницаNCP Ineffective Breathing Pattern TalaJhen Bitco Fidel70% (10)
- Impaired Gas Exchange-Sample NCPДокумент1 страницаImpaired Gas Exchange-Sample NCPKaycee BinanОценок пока нет
- NCP For InfectionДокумент1 страницаNCP For InfectionNathaniel EllanoОценок пока нет
- Impaired Gas ExchangeДокумент1 страницаImpaired Gas ExchangeAdelaine LorestoОценок пока нет
- NCPДокумент4 страницыNCPDaniel Garraton0% (1)
- Cues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalДокумент4 страницыCues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalKei Cruz100% (1)
- Mpaired Physical Mobility (Amputation) : Nursing Care PlanДокумент3 страницыMpaired Physical Mobility (Amputation) : Nursing Care PlanTheSweetpea5010% (2)
- NCP Ineffective Airway ClearanceДокумент5 страницNCP Ineffective Airway ClearanceEmm Estipona HaoОценок пока нет
- NCP HemothoraxДокумент3 страницыNCP Hemothoraxroseonabreeze0% (2)
- NCP - Ineffective Airway ClearanceДокумент2 страницыNCP - Ineffective Airway Clearancelarapatricia1215Оценок пока нет
- NCP - Ineffective Airway ClearanceДокумент4 страницыNCP - Ineffective Airway ClearanceKen RegalaОценок пока нет
- Fluid Volume Deficit BatuДокумент2 страницыFluid Volume Deficit Batumecz26Оценок пока нет
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale EvaluationДокумент2 страницыNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale EvaluationAdelaine LorestoОценок пока нет
- NCP - Impaired Gas ExchangeДокумент1 страницаNCP - Impaired Gas ExchangeRryje Salleva100% (1)
- NCP For UtiДокумент3 страницыNCP For UtiAaron Sanchez100% (1)
- Asthma Risk For Activity IntoleranceДокумент1 страницаAsthma Risk For Activity IntoleranceWdy Tanakht Sparrow100% (4)
- Burns - Airway Clearance, Risk For IneffectiveДокумент2 страницыBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20Оценок пока нет
- NCP MCMC Post OperativeДокумент3 страницыNCP MCMC Post OperativeKristiyanong KabataanОценок пока нет
- JVJV NCP Risk For Fluid Volume DeficitДокумент2 страницыJVJV NCP Risk For Fluid Volume DeficitvicenteturasОценок пока нет
- Impaired Gas Exchange Care PlanДокумент5 страницImpaired Gas Exchange Care Planjakifer50% (2)
- Impaired Gas Exchange NCPДокумент1 страницаImpaired Gas Exchange NCPCj AlconabaОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care Planapi-309251523Оценок пока нет
- NCP HyperthermiaДокумент6 страницNCP HyperthermiaGrax DeeОценок пока нет
- Ineffective Airway Clearance CareplanДокумент6 страницIneffective Airway Clearance CareplanderreshaОценок пока нет
- Electrolyte Imbalance NCPДокумент8 страницElectrolyte Imbalance NCPManuel Jacob YradОценок пока нет
- NCP Impaired Skin IntegrityДокумент4 страницыNCP Impaired Skin IntegrityElgie SantosОценок пока нет
- NCP Ineffective Breathing PatternДокумент2 страницыNCP Ineffective Breathing PatternChristianmel JavierОценок пока нет
- Ineffective Breathing Pattern Related To Bronchospasm, Decreased Lung ExpansionДокумент2 страницыIneffective Breathing Pattern Related To Bronchospasm, Decreased Lung ExpansionReylan Garcia43% (7)
- Cues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale Evaluation Subjective: NDX: Goal: Independent: Goal EvaluationДокумент5 страницCues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale Evaluation Subjective: NDX: Goal: Independent: Goal EvaluationNash DimarucotОценок пока нет
- NCP AidsДокумент16 страницNCP AidstferdianingsihОценок пока нет
- Nursing Care Plan - Impaired Gas ExchangeДокумент3 страницыNursing Care Plan - Impaired Gas ExchangeYum C86% (65)
- Mapagod at Manghina" As: Nursing Care Plan (NCP) For A Patient With AsthmaДокумент2 страницыMapagod at Manghina" As: Nursing Care Plan (NCP) For A Patient With AsthmaKian Herrera100% (1)
- Impaired Gas ExchangeДокумент2 страницыImpaired Gas ExchangeAura Salve Ildefonso Allas100% (3)
- 4 NCP's FinalДокумент9 страниц4 NCP's FinalZenel Yap100% (1)
- NCP Ineffective Airway Clearance Related To The Accumulation of Exudates in The Alveoli TBДокумент3 страницыNCP Ineffective Airway Clearance Related To The Accumulation of Exudates in The Alveoli TBMa. Elaine Carla Tating0% (1)
- NCP Impaired Gas ExchangeДокумент2 страницыNCP Impaired Gas ExchangeGabriel Tolentino70% (10)
- NCP Activity IntoleranceДокумент4 страницыNCP Activity IntoleranceKryza Dale Bunado Batican0% (1)
- NCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDSДокумент6 страницNCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDSTina Larsen100% (4)
- NCP PneumoniaДокумент3 страницыNCP Pneumoniakaiserdominick100% (2)
- Nursing Care PlanДокумент22 страницыNursing Care PlanjamОценок пока нет
- Acutepain PneumoniaДокумент3 страницыAcutepain PneumoniaJoy SalvadorОценок пока нет
- NCP CR Impaired Spontaneous VentilationДокумент8 страницNCP CR Impaired Spontaneous VentilationJosett Romano75% (4)
- Nursing Care PlanДокумент11 страницNursing Care Planaycee0316100% (1)
- NCP CopdДокумент10 страницNCP Copdarnnie100% (2)
- Ncp-Impaired S.i.-NavidasДокумент4 страницыNcp-Impaired S.i.-NavidasFran LanОценок пока нет
- 6639burn NCPДокумент18 страниц6639burn NCPDivina Grace Renon Camba100% (1)
- Ncp's FOR PLEURAL EFFUSIONДокумент4 страницыNcp's FOR PLEURAL EFFUSIONHania Polangi100% (1)
- Doengoes Bersihan Jalan Nafas Tidak EfektifДокумент4 страницыDoengoes Bersihan Jalan Nafas Tidak EfektifAnonymous ZdqtAqT1WОценок пока нет
- Nursing DiagnosisДокумент7 страницNursing DiagnosisMariya Mikaela Garcia SoledadОценок пока нет
- Nursing Care PlanДокумент3 страницыNursing Care PlanMarielle SorianoОценок пока нет
- Breathing Pattern, IneffectiveДокумент8 страницBreathing Pattern, IneffectiveRudhy SaputraОценок пока нет
- Asthma Nursing Care Plan - NCP - Ineffective Airway ClearanceДокумент2 страницыAsthma Nursing Care Plan - NCP - Ineffective Airway ClearanceCyrus De Asis92% (24)
- Jay Allen Marc J. SabandalДокумент3 страницыJay Allen Marc J. SabandalRoxanne Ganayo ClaverОценок пока нет
- CV MaelДокумент1 страницаCV MaelRoxanne Ganayo ClaverОценок пока нет
- Tila INFANT Kung MaglaroДокумент4 страницыTila INFANT Kung MaglaroRoxanne Ganayo ClaverОценок пока нет
- Monday Tuesday Wednesday Thursday Friday Saturday SundayДокумент12 страницMonday Tuesday Wednesday Thursday Friday Saturday SundayRoxanne Ganayo ClaverОценок пока нет
- Final CsДокумент92 страницыFinal CsRoxanne Ganayo ClaverОценок пока нет
- 10.) Head Nurse Structured ProgramДокумент4 страницы10.) Head Nurse Structured ProgramRoxanne Ganayo ClaverОценок пока нет
- Joanne G. Ediong: Owner, RO Abella BrokerageДокумент1 страницаJoanne G. Ediong: Owner, RO Abella BrokerageRoxanne Ganayo ClaverОценок пока нет
- The Social Support and Self-Image of The Students of Tagum Doctors College IncДокумент4 страницыThe Social Support and Self-Image of The Students of Tagum Doctors College IncRoxanne Ganayo ClaverОценок пока нет
- FDARДокумент2 страницыFDARRoxanne Ganayo ClaverОценок пока нет
- Ms. Kenji Casul: Head, HRDДокумент1 страницаMs. Kenji Casul: Head, HRDRoxanne Ganayo ClaverОценок пока нет
- Nursing Care Plan #3 DAT E& Shif T Assessment Nursing Diagnosis Need S Planning Intervention Rationale EvaluationДокумент2 страницыNursing Care Plan #3 DAT E& Shif T Assessment Nursing Diagnosis Need S Planning Intervention Rationale EvaluationRoxanne Ganayo ClaverОценок пока нет
- NCP Intra FinalДокумент7 страницNCP Intra FinalRoxanne Ganayo ClaverОценок пока нет
- Assessment A. Biographical DataДокумент5 страницAssessment A. Biographical DataRoxanne Ganayo ClaverОценок пока нет
- Generic Name: Co-Amoxiclav Brand Name: Augmentin Classification: Dosage: 625 MGДокумент6 страницGeneric Name: Co-Amoxiclav Brand Name: Augmentin Classification: Dosage: 625 MGRoxanne Ganayo ClaverОценок пока нет
- Will, End-Oflife Of: Kron L - Nllons. IivingДокумент12 страницWill, End-Oflife Of: Kron L - Nllons. IivingRoxanne Ganayo ClaverОценок пока нет
- ) With A Reading Capability of 780 NM Wavelength (Infrared and Red Edge) Semiconductor Laser, 1200 Kib/s (1×) - While USB Has A Capability of UpДокумент1 страница) With A Reading Capability of 780 NM Wavelength (Infrared and Red Edge) Semiconductor Laser, 1200 Kib/s (1×) - While USB Has A Capability of UpRoxanne Ganayo ClaverОценок пока нет
- Laboratory ResultsДокумент4 страницыLaboratory ResultsRoxanne Ganayo ClaverОценок пока нет
- Aluminium: Aluminium (Or Aluminum) Is A Chemical Element in The Boron Group With Symbol Al and Atomic Number 13. ItДокумент2 страницыAluminium: Aluminium (Or Aluminum) Is A Chemical Element in The Boron Group With Symbol Al and Atomic Number 13. ItRoxanne Ganayo ClaverОценок пока нет
- Ezy Tai-Chi PDFДокумент9 страницEzy Tai-Chi PDFKomang Tri Adi SuparwatiОценок пока нет
- RLS-134R MSDSДокумент6 страницRLS-134R MSDSmanderson3297Оценок пока нет
- JUE-410F Installation Manual PDFДокумент74 страницыJUE-410F Installation Manual PDFArshad JummaniОценок пока нет
- Osho - Third EyeДокумент4 страницыOsho - Third Eyesonaliforex1100% (1)
- Stress Management 01Документ23 страницыStress Management 01Sumayya LimbadaОценок пока нет
- Anatomical & Physiological Differences B/N Adult & Paediatric LungДокумент22 страницыAnatomical & Physiological Differences B/N Adult & Paediatric LungAmber JamaalОценок пока нет
- 829 Na1321ge EnglishДокумент6 страниц829 Na1321ge EnglishMeuMundoMinecraftОценок пока нет
- Oxygenation QuizДокумент3 страницыOxygenation QuizPOTENCIANA MAROMAОценок пока нет
- Quiz Competition: National Safety Week 2022Документ2 страницыQuiz Competition: National Safety Week 2022Gopal ChoudharyОценок пока нет
- An Eye Opener To LifeДокумент23 страницыAn Eye Opener To Life4ram20Оценок пока нет
- Manual How Maintain Nasal Breathing 24 7Документ3 страницыManual How Maintain Nasal Breathing 24 7Irina BranОценок пока нет
- Chronic Obstructive Pulmonary Disease (COPD) : Sultan Chaudhry Benny Dua Eric WongДокумент7 страницChronic Obstructive Pulmonary Disease (COPD) : Sultan Chaudhry Benny Dua Eric Wongjamil aldasriОценок пока нет
- PeppermintДокумент22 страницыPeppermintRezza HaryОценок пока нет
- Yoga Assignment ON Types of PranayamДокумент32 страницыYoga Assignment ON Types of PranayamH028 Deepshikha Sharma ECE100% (1)
- Now AffimrationsДокумент8 страницNow AffimrationschanduОценок пока нет
- Stavish - The Chamber of ReflectionДокумент8 страницStavish - The Chamber of Reflectionapi-3823319100% (2)
- Porter MXR and MXR 1 Flowmeter Users Manual FM 286Документ19 страницPorter MXR and MXR 1 Flowmeter Users Manual FM 286Μαριτίνα ΑλεξίουОценок пока нет
- Pain Management During BirthДокумент9 страницPain Management During BirthSheena Felicia-WillisОценок пока нет
- Ventilation: Kinematics and Kinetics.: Thorax Structure and FunctionДокумент52 страницыVentilation: Kinematics and Kinetics.: Thorax Structure and FunctionAlejandra RomeroОценок пока нет
- What Is Chinese MedicineДокумент44 страницыWhat Is Chinese MedicineCarleta StanОценок пока нет
- Ba ManualДокумент60 страницBa Manualapi-115711968Оценок пока нет
- Ujian Semester Gasal Kelas Xi IpaДокумент38 страницUjian Semester Gasal Kelas Xi IpaRichard sutantoОценок пока нет
- Art of Super-RealizationДокумент12 страницArt of Super-RealizationKristina Bogdanova100% (2)
- Transient Tachypnea of NewbornДокумент5 страницTransient Tachypnea of NewbornAyuindiraОценок пока нет
- Merkabah Merkabah Merkabah MerkabahДокумент66 страницMerkabah Merkabah Merkabah MerkabahNair Milau100% (5)
- VTI BenefitsДокумент73 страницыVTI BenefitsJoe FangОценок пока нет
- Imm Mcqs Solved (Umer Hayat and DR RaliДокумент129 страницImm Mcqs Solved (Umer Hayat and DR RaliJaved GabaОценок пока нет
- ICU Burns GuidelineДокумент24 страницыICU Burns GuidelineJonas BlaineОценок пока нет
- Resulting in Damage To Brain Tissue.: Definition: Independent: IndependentДокумент4 страницыResulting in Damage To Brain Tissue.: Definition: Independent: Independentalliahjoyce ignacioОценок пока нет