Академический Документы
Профессиональный Документы
Культура Документы
Cases History
Загружено:
Nabilah Sufian0 оценок0% нашли этот документ полезным (0 голосов)
94 просмотров7 страницOSCE
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документOSCE
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
94 просмотров7 страницCases History
Загружено:
Nabilah SufianOSCE
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 7
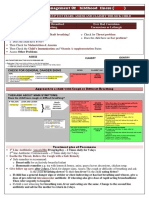
Cases History
1. Zainon, 63 y/o, worked in factory until 50 y/o, married with 5 kids
a. C/O: Shortness of breath with chest pain
b. HOPI: Crushing chest pain started 2 months ago upon exertion, getting more frequent
even when doing daily life activities. Pain radiate to the back. Sign of orthopnea and
PND. Also complained of blurry vision, polydipsia and cough.
c. PMH: DM (non-compliance to medications), high cholesterol and HTN, hospitalized
before d/t uterine prolapsed performed hysterectomy 10 years back.
d. FH: Positive family history from moms side
e. SH: Non-smoker, non-alcoholic drinker, exercise walking
f. PE: No other significant findings except: mild conjunctiva pallor
LEARNING ISSUES:
Angina pectoris
o Central chest tightness
o Brought by exertion, relieved by rest
o Radiate arm, neck, jaw
o Dyspnea, nausea, sweating, fainting
o Stable, unstable (increase risk of MI), prinzmetal
o ECG usually normal
o Management
Aspirin (prevent production of thromboxane A2)
Beta blocker (CI in asthma, COPD) (SE: lethargic, ED)
Nitrates GTN s/l (SE: headache)
Long-acting Ca antagonist amlodipine (if CI to beta-b) (SE: headache, flushes,
edema)
K channel activator nicorandil
o Percutaneous transluminal coronary angioplasty
Poor response to meds or intolerance
o Coronary artery bypass graft
Left main stem disease
Multi vessel disease
Not suitable for angioplasty
Acute coronary syndromes
o Unstable angina, evolving MI, STEMI/ NSTEMI
o Diagnosis: Cardiac biomarkers, ECG, pathological Q waves
o Symptoms: chest pain >20 mins, syncope, pulmonary edema, epigastric pain, acute
confusional state
o Maybe signs of heart failure: increase JVP, 3
rd
heart sound, creps, pansystolic murmur
o Test: ECG, blood, cardiac enzymes
2. Norwati, 36 y/o, married with 4 kids
a. C/O: weakness of right side of body stroke
b. HOPI: Vomiting for a day prior to hemiparesis on right side without any loss of
sensation, face is not affected, ascites 4/12, no loss of appetite, weight loss and
numbness of right arm
c. PMH: Pre-eclampsia while pregnant the 4
th
child, high cholesterol, underlying systemic
lupus erythematosus, took prednisolone ever since, allergic to crabs, claimed to have
renal calculi discovered by USS but could not undergo operation d/t total weakness
d. FH: Significant, dad died of stroke
e. SH: Exercise jogging
f. PE: Pulse is 68 bpm, slow rising, hyperpigmented fingers, hard nails, dehydrated skin
peeled off, alopecia for the past 1 year, no conjunctiva pallor, no jaundice, right leg
swelling, tenderness of left leg upon palpation, positive fluid thrill and shifting dullness
LEARNING ISSUES:
Stroke
o Causes
Small vessel occlusion - thrombosis
Cardiac emboli AF, endocarditis
Atherothromboembolism
CNS bleeds
o Signs
Cerebral hemisphere infarcts contralateral hemiplegia flaccid then spastic
Brainstem infarcts wide range
Lacunar infarcts small infarcts: basal ganglia, internal capsule, thalamus and
pons
Lacunar syndromes:
o Pure motor
o Ataxic hemiparesis
o Pure sensory
o Mixed sensorimotor
o Dysarthria
o Management
Airway
BP
Urgent CT/MRI
Thrombolysis
Nil by mouth (aspiration pneumonia)
Hydration
Explain
Anti platelet agents
Admit
Pre-eclampsia
o Hypertension
o Proteinuria
o Edema
o Causes:
Placenta not getting enough blood
Blood vessels not fully transformed
Systemic lupus erythematosus multisystem AI disease in which autoAb are made against a
variety of autoAg
o Malar rash, photosensitivity, oral ulcers, non-erosive arthritis, serositis pleuritis,
pericarditis, renal disorders, CNS disorder, hematological disorder, immunological
disorders, lymphadenopathy, alopecia, weight loss, stroke
3. Latifah, 58 y/o, work at warung until raya 2013
a. C/O: crushing chest pain while watching television
b. HOPI: chest pain comes together with profuse sweating, abdominal pain, nausea and
vomiting and weakness, claimed to take 4 pills of GTN but pain did not alleviate, has
orthopnea and PND for the past 6 months, shortness of breath occurs quite often since
the last 2-3 months, weight loss, coughing, blurry vision, thirsty, sometimes ankle
swelling, sock and glove pattern of numbness
c. PMH: DM and HTN 3 years back, poorly controlled, high cholesterol, heart problem
since last 3 months, admitted 3 times for pus removal of ulcer d/t DM
d. FH: Positive heart disease in both parents, DM in mom
e. SH: Jog and walk only for 2-3 months last year
f. PE: Alert, conscious, responsive, not tachypneic, hand is warm, dry, capillary refill is
normal, pulse is 66bpm, regular, strong volume, has mild conjunctiva pallor, no jaundice,
lips is pinkish and well hydrated, good oral hygiene, tongue and frenulum is pinkish,
deformity on right big toe, deviated to right side, no ulcer between toes, ulcer on left
side of left foot, no pitting edema, hyperpigmentation on both dorsum of feet, left foot
is swollen since pus removal cannot walk, hyperthermia on left leg below knee level,
tenderness on umbilicus and epigastric region, pain at right costal margin, bowel sound
can be heard, apex beat cannot be felt, S1 and S2 are heard, no added sounds, no
murmur, no palpable thrill and parasternal heave, no carotid bruit
LEARNING ISSUES
Diabetic mellitus
o
Abdominal pain
4. Nasir, 61 y/o, industrial consultant (businessman) after pension
a. C/O: generalized allergic reaction angioedema and itchiness
b. HOPI: Patient claimed that it was his first time taking pain killer. He had fever for three
days. On the second day, he took Panadol bought OTC and he felt better. He also had
low back pain and his wife asked him to take Ponstan also bought OTC. He took it once a
day, for 2 days. He had tea-colored urine since before fever but suspected that it was
d/t dehydration. Went to private clinic, took blood sample, said that his glucose level is
high, jaundice and ketonemic. Has no blurry vision, polydipsia, joint pain but relieved by
medication, polyuria, incontinence, incomplete urination since the past 1 month, frothy
and smelly urine, no appetite during fever and weight loss
c. PMH: 30 years back, was suspected HTN but not diagnosed and no meds, 14 years back
diagnosed with DM but not taking meds and not compliance to diet, prone to cough,
will get 2 weeks of cough at least per year
d. FH: Parents are healthy, grandmother had DM, siblings sinusitis, kids are all allergic.
e. SH: Not a chronic smoker, non alcoholic, not exercise only farming
f. Worries and concern: About company, payment for employees
g. PE: Alert, conscious, responsive, yellow discoloration of skin and eyes, not in any
obvious pain or respiratory distress, hands are warm and moist, yellowish tinge on skin,
no flapping tremor, capillary refill normal, no clubbing, pulse 70bpm, regular character,
strong volume, respiratory rate 14/min, no radio-radial delay, no conjunctiva pallor,
icteric sclera, corneal arcus, no angular stomatitis, good oral hygiene, no fetor
hepaticus, no gynecomastia, inverted umbilicus, visible pulsation seen, flat abdomen, on
light and deep palpation abdomen is soft, non tender, percussion sound is resonance for
all four quadrants, no hepatosplenomegaly, no renal a. bruit
LEARNING ISSUES:
Hepatitis
Portal hypertension
Liver cirrhosis
5. Faisal, 21y/o, work at catering place
a. C/O: follow up epilepsy, post epileptic
b. HOPI: Work under stress too hot or too tired, will get epileptic attack, felt fatigue
c. PMH: First episode, 6 y/o, ever since, claimed to get twice a day, get jerking before tonic
extension, asked to do lumbar puncture before, but did not do
d. FH: No significant
e. SH: Non-chronic smoker
LEARNING ISSUES:
Epilepsy
Lumbar puncture
6. Badri, 56y/o, self-working
a. C/O: Fever due to infection of hemocath (AV fistula on the neck)
b. HOPI: Comes with chills and rigor at night, suspected nephropathy d/t u/l DM
(ulceration), SOB, pulmonary edema, orthopnea, blurry vision
c. PMH: HTN, DM, stroke, heart disease, last month - hypoglycemia
d. FH: No significant
e. SH: Chronic smoker, not exercise
f. PE: Pulse 68bpm, strong volume, regular, cold, dry hand, no muscle wasting, palpable
mass umbilicus and suprapubic area, non-tender, no guarding, AV fistula on left hand,
right neck hemocath, scar below umbilicus PD, no ballotable kidney, no jaundice, no
pallor
LEARNING ISSUES:
Chronic kidney disease
Nephropathy secondary to diabetes mellitus
7. Mr Tan, 68 y/o, contract worker
a. C/O: Acute chest pain and shortness of breath after bathing
b. HOPI: SOB started since 2-3 months back, swollen ankle, defecation is normal,
numbness of hands and feet
c. PMH: Stroke last May, sent to Hosp Sg Buloh stayed in ICU 5 days, warded one week,
fully recovered (given medication for 1 month, then was not asked to continue any
medication), history of asthma until 16 y/o, blockage of arterial supply of heart (recently
diagnosed), denied any history of hypertension
d. FH: No significant family history
e. SH: Chronic smoker, no exercise, non-alcoholic
f. PE: Chest rise with inspiration, Hands warm and dry, no muscle wasting, normal capillary
refill, no tendon xanthomas, respiratory rate 16/min, pulse 88 bpm, normal character,
regular rhythm, branula on right arm, eye no jaundice, no conjunctiva pallor, lip is
pinkish, hydrated, tongue is pinkish, fissure on median sulcus, CVS visible apex
pulsation, apex beat normal, not deviated, no palpable thrill, no parasternal heave, S1
S2 sounds are heard, no carotid bruit, bibasal crepitations
LEARNING ISSUES:
Acute pulmonary edema
Management of myocardial infarction
Heart failure
8. Noranita, 42 y/o, housewife
a. C/O: Fever, gastritis
b. HOPI: Anemic, headache, profuse sweating, blurry vision, polydipsia, weight loss,
decrease appetite, nausea and vomiting, one week constipation, no swollen ankle,
urination is normal, always fatigue, chills and rigors, heat tolerance
c. Menstrual Hx: Menarche 14 y/o, 1 day use 5 pads until 4
th
day, blood clot of about 2
inches will come out, no post coital bleeding, no dyspareunia
d. PMH: Recently diagnosed with DM, mom positive of DM, father gout
e. SH: Not smoking, non alcoholic, non vege, tubectomy 5 years back d/t post delivery
hemorrhage
f. PE: Hyperpigmented dots all over body, koilonychia, no muscle wasting, splinter
hemorrhage, pulse 60bpm, strong, regular, conjunctiva pallor, no jaundice, lips pale and
dry, no central cyanosis, good oral hygience, frenulum pinkish, truncal obesity, no
edema but left ankle swollen, stomach no tenderness, no superficial mass, no guarding,
no rebound tenderness
LEARNING ISSUES
Anemia
Gastritis
9. Mohamad Sidek, 21 y/o, maintenance worker
a. C/O: Acute sharp chest pain (lasted for 30 mins) together with SOB (lasted for 5 mins)
occurred at rest, radiate to the back at subscapular region. Accompanied by profuse
sweating, palpitations and nauseous but no vomiting.
b. HOPI: Eyes have nystagmus but no diplopia. History of intermittent chest pain (3 times,
each lasted for about 30 mins), severity is 4, has dizziness (exposed to hot or cold
weather), vertigo, fever one day prior to admission (took Panadol and relieved), no
cough, no sorethroat, has flu, insomnia since he was 13 y/o and also heat intolerance.
Complained of SOB when walking too far and walking down stairs but claimed that this
is the first time it came with chest pain. He also has numbness and tingling sensation of
both feet, prone to falling down and syncope since 10 y/o, has good appetite yet having
weight loss, normal urination and bowel movement.
c. PMH: NKMI (this include epilepsy, HTN, DM, allergic) except for gastritis, first hospital
admission in Feb 2014 d/t chest pain for 3 days, no precious surgery, no medication
d. FH: Elder sister also has nystagmus, otherwise no significant family history.
e. SH: Non smoker, non alcoholic, jogging every Sunday (sometimes complained of SOB)
f. PE:
i. General:
1. Patient is alert, conscious and responsive. Not in any obvious pain or
respiratory distress. Hands are warm and moist, have some traumatic
scars on dorsum part of left hand, bony prominence on right middle
finger (PIP joint), capillary refill is normal, no clubbing, presence of fine
tremors. Pulse is 80bpm, regular and strong volume, normal character,
no radio-radial delay, no signs of dehydration. Eyes have no conjunctiva
pallor and no jaundice. Oral hygiene is good, no central cyanosis, pinkish
frenulum indicating no jaundice.
ii. CVS:
1. ECG electrode scars on chest upon inspection, no raised JVP. Apex beat
is at 5
th
ICS, 1 cm lateral to mid-clavicular line, no palpable thrill, no
parasternal heave. Upon auscultation, S1 and S2 are heard, no added
sounds, no murmur, no carotid bruit.
iii. Respi:
1. Chest rises and falls symmetrically. Chest expansion is symmetrical on
both sides. Tactile fremitus is equal on both sides. Lungs are resonance
upon percussion. Upon, auscultation, faint vesicular sound is heard
(diminished air entry on left side)
iv. CNS:
1. Dysdiadochokinesia negative, missed nose to finger touch, heel to shin
is normal, no slurred speech, hypotonia on left side, intentional tremors,
presence of nystagmus, late visual acuity, head is tilted to right side
while walking with broad-based gait, cannot perform heel to toe
movement, Rhombergs test is positive
LEARNING ISSUES
Nystagmus
Brain lesion
10.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- AeonДокумент4 страницыAeonsancsa_74Оценок пока нет
- Original Sandeha NivariniДокумент117 страницOriginal Sandeha NivariniHmis BlrОценок пока нет
- IMCI UpdatedДокумент5 страницIMCI UpdatedMalak RagehОценок пока нет
- Water Chemistry - An Introduction To The Chemistry of Natural and Engineered Aquatic Systems-Páginas-483-492Документ10 страницWater Chemistry - An Introduction To The Chemistry of Natural and Engineered Aquatic Systems-Páginas-483-492jhonier guevaraОценок пока нет
- Chapter 5 TEstДокумент18 страницChapter 5 TEstJeanneau StadegaardОценок пока нет
- Cho Gsas - Harvard 0084L 11462Документ503 страницыCho Gsas - Harvard 0084L 11462Claudemiro costaОценок пока нет
- WL4000Документ1 страницаWL4000Laser PowerОценок пока нет
- American Pile Driving Equipment Equipment CatalogДокумент25 страницAmerican Pile Driving Equipment Equipment CatalogW Morales100% (1)
- Air System Sizing Summary For NIVEL PB - Zona 1Документ1 страницаAir System Sizing Summary For NIVEL PB - Zona 1Roger PandoОценок пока нет
- Soccer Training DiaryДокумент1 страницаSoccer Training DiaryMark DeaconОценок пока нет
- Hyundai Forklift Catalog PTASДокумент15 страницHyundai Forklift Catalog PTASjack comboОценок пока нет
- Sample Dewa Inspection CommentsДокумент2 страницыSample Dewa Inspection Commentsrmtaqui100% (1)
- Lesson Notes Lecture 14Документ5 страницLesson Notes Lecture 14Quantum SaudiОценок пока нет
- Quality Traits in Cultivated Mushrooms and Consumer AcceptabilityДокумент40 страницQuality Traits in Cultivated Mushrooms and Consumer AcceptabilityShivendra SinghОценок пока нет
- Safety Procedures For Vertical Formwork PDFДокумент17 страницSafety Procedures For Vertical Formwork PDFbalya7Оценок пока нет
- Kulkarni Shilpa A.Документ148 страницKulkarni Shilpa A.MSKCОценок пока нет
- Chapter 01Документ16 страницChapter 01deepak_baidОценок пока нет
- Motor Starting: Why Do The Calculation?Документ13 страницMotor Starting: Why Do The Calculation?carlos_eqnОценок пока нет
- Annie Ovenden Exibition 2017Документ19 страницAnnie Ovenden Exibition 2017Vitaliy ChuenkoОценок пока нет
- Digital ElectronicsДокумент18 страницDigital ElectronicsHarry BeggyОценок пока нет
- DSR Codes - 1Документ108 страницDSR Codes - 1lakkireddy seshireddyОценок пока нет
- PT4115EДокумент18 страницPT4115Edragom2Оценок пока нет
- Massage Techniques in SpaДокумент1 страницаMassage Techniques in SpaALISA SAITAОценок пока нет
- Water Vapor Permeability of Polypropylene: Fusion Science and TechnologyДокумент5 страницWater Vapor Permeability of Polypropylene: Fusion Science and TechnologyBobОценок пока нет
- Introduction To The New 8-Bit PIC MCU Hardware Peripherals (CLC, Nco, Cog)Документ161 страницаIntroduction To The New 8-Bit PIC MCU Hardware Peripherals (CLC, Nco, Cog)Andres Bruno SaraviaОценок пока нет
- Equipment in The NICUДокумент7 страницEquipment in The NICUGheDine PeracionОценок пока нет
- WD 02Документ1 страницаWD 02Elezer BatchoОценок пока нет
- 33 Mpact - of - The - Great - Earthquake-2015 - On - Hospitality PDFДокумент30 страниц33 Mpact - of - The - Great - Earthquake-2015 - On - Hospitality PDFJoannabelОценок пока нет
- Book 2 - Koning (COMPLETO)Документ100 страницBook 2 - Koning (COMPLETO)Kevin VianaОценок пока нет
- 1943 Dentures Consent FormДокумент2 страницы1943 Dentures Consent FormJitender ReddyОценок пока нет