Академический Документы
Профессиональный Документы
Культура Документы
Platelets and The Vessel Wall
Загружено:
Racquel JosephИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Platelets and The Vessel Wall
Загружено:
Racquel JosephАвторское право:
Доступные форматы
25
Platelets and the Vessel Wall
Peter J. Newman and Debra K. Newman
1379
Platelet Morphology and Subcellular
Organization, 1380
Platelet Genomics and Proteomics, 1382
Antithrombotic Components of the
Vessel Wall, 1382
Reacting to the BreachCell Surface
Receptors That Mediate Tethering and
Adhesion and Transmit Early Activation
Signals, 1384
Platelet Granules and Their Role in
Hemostasis, 1384
Feed-Forward Amplication Pathways
Involved in Platelet Recruitment and
Thrombus Stability, 1386
Activation of the Major Platelet Integrin
a
IIb
b
3
(GPIIb-IIIa Complex)The Final
Common End Point of Platelet
Activation, 1388
Cell Surface and Cytosolic Proteins That Limit
Platelet Responses, 1388
Additional Roles for Platelets in Vascular
Physiology: Vessel Repair (Angiogenesis),
Inammation, and Atherothrombosis, 1390
1380 HEMOSTASIS
In a 1881 communication to the Turin Royal Academy
of Medicine, the Italian physician Giulio Bizzozero dis-
closed the presence in circulating human blood of dis-
crete elements that he termed piastrine (blutplttchen
in a 1882 publication in a German journal and petites
plaques in a communication in French).
1
Previously
speculated to be merely nonphysiologic granular aggre-
gates, blood platelets have since become central to our
understanding of thrombosis and hemostasis, and detailed
understanding of their participation in cardiovascular
disease, stroke, and even cancer has led to remarkable
progress in the rational treatment of these disorders.
Although platelets are most often studied in the
context of their ability to form a hemostatically effective
plug, it is now widely recognized that their inuence
extends far beyond this process to all aspects of hemo-
stasis, as well as to wound healing and vascular remodel-
ing. For example, platelets generate or secrete biologically
active mediators such as thromboxane A
2
(TXA
2
) and
serotonin, which not only amplify platelet activation
responses but also modulate vascular tone. In addition,
platelets secrete a broad array of granule constituents
that stimulate vessel repair, induce megakaryocytopoie-
sis, promote coagulation, and limit brinolysis.
The same pathways that lead to platelet plug forma-
tion can also produce pathologic thrombosis, a process
that has been described as hemostasis occurring at the
wrong time or in the wrong place. Platelets are particu-
larly important for hemostasis on the arterial side of the
circulation, where blood ows under higher pressure and
experiences greater shear force. As a result, platelet func-
tion is generally considered to be critical to the patho-
genesis of arterial thrombosis and less so for venous
thrombosis, and antiplatelet drugs are most widely used
in the former setting. However, this distinction between
the mechanisms underlying arterial and venous throm-
bosis is not absolute, and the spectrum of thrombotic
disorders should be considered a continuum.
Arterial thrombosis is a particularly common problem
in middle-aged and older adults and is a major cause of
morbidity and mortality in developed countries. The
thrombi that arise in atherosclerotic vessels are predomi-
nantly platelet in origin and are the proximate cause of
myocardial infarction and most cerebrovascular acci-
dents. Although arterial thrombosis is considerably less
common in children than adults, it may contribute to
major morbidity in patients with sickle cell disease, as
well as complications of some childhood infections,
Kawasakis syndrome, and various forms of arteritis,
autoimmune disorders, hemolytic-uremic syndrome,
and thrombotic thrombocytopenic purpura (see Chapter
33).
In this chapter we review platelet structure and func-
tion, with special emphasis on the cell surface glycopro-
teins that function as sentries for areas of vascular damage
and the signal transduction events that both amplify and
limit platelet responsiveness. The information provided
here should be helpful in understanding subsequent
chapters that describe inherited and acquired platelet
disorders (see Chapters 29 and 33) and the role of the
adhesive protein von Willebrand factor (VWF) (see
Chapter 30) in hemostasis. Finally, there is growing
appreciation of the role that platelets play in inamma-
tion and the pathogenesis of atherothrombosis, which is
briey discussed at the end of the chapter.
PLATELET MORPHOLOGY AND
SUBCELLULAR ORGANIZATION
Platelets are adhesion and signaling machines that circu-
late as small, disc-shaped cellular fragments in the whole
blood of healthy individuals at a concentration of approx-
imately 150,000 to 300,000/L. Early studies suggested
that platelets might be produced via cytoplasmic frag-
mentation along a network of internal demarcation
membranes that were observed in large, polyploid mega-
karyocytes.
2,3
More recent studies,
4-6
however, support
the notion that proplatelets are assembled and packaged
with their various constituents at the ends of long cyto-
plasmic extensions of differentiated megakaryocytes that
have migrated from the proliferative osteoblastic niche to
the capillary-rich vascular niche of the bone marrow
microenvironment,
7
with the invaginated demarcation
membrane system serving simply as a reservoir of inter-
nal membrane used for proplatelet extension.
8,9
Once
adjacent to the adluminal face of the endothelium,
proplatelets are released into the bloodstream, where
they circulate as mature platelets for approximately 7 to
10 days before being cleared by the liver and spleen
10
their life span being controlled, at least in part, by
an antagonistic balance between the apoptotic proteins
Bcl-xL and Bak.
11
The size of resting platelets is somewhat variable,
averaging approximately 1.5 m in diameter and 0.5 to
1 m in thickness. Platelet size is undoubtedly regulated
by numerous factors during their biogenesis, but both the
224-kd nonmuscle myosin heavy chain IIA (MYHIIA)
and the cell surface glycoprotein Ib (GPIb) complex
appear to play critical roles. Thus, mutations in the
MYH9 gene predominantly interfere with contractile
events important for platelet formation,
12
whereas failure
to express GPIbthe molecular basis for the platelet
disorder known as Bernard-Soulier syndrome
13,14
dis-
rupts critical associations with the cytoskeletal protein
lamin
15,16
that play an essential role in both platelet
formation and platelet compliance.
17
In both these inher-
ited platelet disorders, platelets can appear as large as
lymphocytes (see Chapter 29). Correction of GPIb
expression in GPIb-decient (Bernard-Soulier) mice has
been shown to restore platelets to their normal size.
18
The volume of a platelet (mean platelet volume)
normally ranges from 6 to 10 fL (1 fL = 10
15
L). Platelet
density is also variable,
19
and the issue of whether young
platelets are more
20,21
or less
22
dense as they gain versus
lose content during their circulating lifetime has never
Chapter 25 Platelets and the Vessel Wall 1381
been satisfactorily resolved. Because platelets retain most
species of messenger RNA (mRNA) for a short period
after their release from bone marrow megakaryocytes,
23
young platelets can be distinguished from older ones by
their RNA content.
24
As shown in Figure 25-1A and C, resting platelets are
discoid in shape, largely because of the presence of a cir-
cumferential coil of microtubules,
25,26
and they are packed
with numerous electron-opaque alpha granules, a few
dense granules (granule contents and their functions are
discussed later), several mitochondria, and lysosomes.
27
Platelets also retain a few Golgi remnants, as well as occa-
sional vestiges of rough endoplasmic reticulumthe
exception being platelets from patients with rapid platelet
turnover, in whom very young platelets containing more
abundant protein synthesis machinery are readily observed
in the circulation. Platelets also contain two highly spe-
cialized membrane systems not found in other cells of the
body: the surface-connected open canalicular system
(OCS) (see Fig. 25-1B and C) and the dense tubular
system (DTS). The OCS is a series of tortuous invagina-
tions of the plasma membrane that appear to tunnel
throughout the cytoplasm of the cell
28
and serve as an
internal reservoir of plasma membrane that is called upon
when platelets round up, extend lamellipods and lopods
(see Fig. 25-1B and D), and spread during platelet activa-
tiona process that can increase the surface area of
exposed plasma membrane by more than 400%.
29
Because
OCS channels are proximal to internal granules, they also
probably function as a conduit for the rapid expulsion of
alpha and dense granule contents during platelet activa-
tion.
30
The DTS, on the other hand, is a remnant of the
smooth endoplasmic reticulum
31
and is found randomly
dispersed throughout the cytoplasm. The DTS appears to
be one of several organelles within the platelet known to
harbor high concentrations of calcium,
32,33
and it is
thought to contain a 100-kd calcium adenosine triphos-
phatase (ATPase) known as SERCA2b
34
that functions to
sequester and store cytosolic calcium in resting cells.
Recent evidence suggests that adenosine diphosphate
(ADP) is able to induce selective release of calcium from
the DTS
35
whereas activation of the GPIb/V/IX receptor
for VWF releases calcium primarily from a poorly dened
acidic compartment
36
within the cell.
35
Thrombin, a
strong platelet agonist, appears to elicit release of calcium
from both stores on binding to the platelet thrombin
receptor PAR1.
35
The platelet cytoskeleton is composed of a single
rigid, but dynamic microtubule approximately 100 m in
length that is coiled about 8 to 12 times around the
equatorial plane of the cell.
37-39
This marginal band of
microtubules is largely responsible for maintaining the
discoid shape of the resting cell, as illustrated by the
observations that (1) incubation of platelets with colchi-
cinean agent that dissolves microtubulesresults
in their rounding,
40
(2) platelets from mice lacking
A
B
C
D
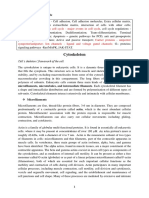
FIGURE 25-1. Platelet morphology. Resting platelets (shown in thin section in A and from a scanning electron micrograph of a ash-frozen,
freeze-dried platelet in C) are shaped like a disc and contain numerous electron-opaque alpha granules, a few dense granules, and several mito-
chondria and lysosomes. A circumferential coil of microtubules (mchighlighted with an oval) is responsible for maintaining their discoid shape.
Platelets also contain a number of cytoplasmic membrane systems that subserve specialized functions, including vestiges of the smooth endoplasmic
reticulum that sequester calcium and tortuous invaginations of the plasma membrane that form a surface-connected open canalicular system
(OCS). When platelets become activated (B and D), they rapidly round up, extend lamellipodia (lam) and lopodia (l), and release the contents
of their granules, often into the nearby OCS. (Photographs generously provided by John H. Hartwig and used with permission.)
1382 HEMOSTASIS
1
-tubulin remain largely spherical,
41
and (3) platelet
spherocytosis in humans results when tubulin fails to
polymerize normally into microtubules.
42
Directly under-
neath the plasma membrane lies an intricate, two-dimen-
sional, tightly woven membrane skeleton
43
composed of
nonerythroid spectrin,
44,45
a network of actin laments,
43,45
vinculin,
46
and the actin-binding protein lamin,
47
which
itself is tethered to the inner face of the plasma mem-
brane via linkages with the cytoplasmic domain of
GPIb.
15,47
The membrane skeleton, because of its loca-
tion, serves as a scaffold that links elements of the plasma
membrane with contractile elements of the cytoskeleton
and cytosolic signaling proteins and thereby regulates
such diverse functions as receptor mobility,
48,49
receptor
clustering,
50-52
and signal transduction.
53
Finally, the
platelet is lled with an extensive cytoplasmic network of
actin laments
45,54
organized by the actin-binding pro-
teins lamin
55,56
and -actinin
57
that constitute its
cytoskeleton.
When platelets become exposed to components of
the extracellular matrix
58
or to soluble agonists such as
ADP
59
or thrombin,
60,61
they undergo dramatic changes
in their morphology.
62,63
The marginal band of microtu-
bules disappears,
54
which allows the platelet to transform
from a disc to an irregular sphere. At nearly the same
time, the actin lamentcapping protein -adducin
becomes phosphorylated and dissociates from existing
F-actin laments,
64
thereby exposing the barbed end of
the lament to cytosolic actin monomers and driving
rapid polymerization of actin into microlaments.
62
This
has the dual effect of driving the extension of lamellipo-
dia and lopodia and forcing granules toward the center
of the platelet, where they can fuse with membranes of
the OCS and release their contents to the exterior of the
cell. Phosphorylation of myosin additionally induces
contractile events that facilitate centralization of the
granules.
65
PLATELET GENOMICS AND PROTEOMICS
Though anucleate, platelets contain measurable and
manipulable levels of megakaryocyte-derived mRNA,
23
at least some of which is capable of being synthesized
into small, but detectable amounts of protein.
66,67
Both
serial analysis of gene expression (SAGE) and gene
microarray analysis have been used to estimate the size
and composition of the platelet transcriptome.
68-70
A con-
sistent nding of all genomic analyses performed to date
is that mitochondrially derived transcripts dominate the
platelet transcriptomepresumably because of persis-
tent transcription of the mitochondrial genome after
platelet release from the bone marrow. This problem has
recently been addressed by analyzing the transcriptome
of cultured megakaryocytes derived from cord blood
stem cells.
71
Of the 20,488 genes present in the human
genome, 2000 to 3000 distinct transcripts have been
identied in unstimulated plateletsconsiderably fewer
than normally found in a nucleated cell, but perhaps
more than one might have expected from an anucleate
circulating cellular fragment. One of the more surprising
ndings in recent years has been the identication of
heterogeneous nuclear RNA (hnRNA) in the platelet
cytosol, as well as all of the spliceosome components
necessary to splice the hnRNA into mature message that
can thereafter be translated into protein.
72
Enlisted during
the activation process, signal-dependent protein transla-
tion has thus far been demonstrated for mRNA mole-
cules encoding interleukin-1 (IL-1),
72
tissue factor,
73
and Bcl-3,
74
the protein products of which have the
potential to inuence inammation, thrombosis, and
wound repair.
The platelet proteome appears to be equally complex
and diverse and, unlike the transcriptome, reports both
the breadth and relative amounts of protein products
actually present in the cell. Obtained by rened two-
dimensional gel electrophoretic techniques that were
originally developed in the 1970s
75,76
or by liquid chro-
matographic separation, proteins are fragmented and
separated via a combination of proteolytic and ionization
techniques and then analyzed by mass spectrometry.
Such analysis has allowed the identication of dozens of
proteins present in complex cellular lysates or subcellular
fractions (see elsewhere
77,78
for recent reviews of this
topic). In addition to yielding the expected menu of
major plasma membrane glycoprotein receptors, one of
the more complete global proling analyses to date
79
identied a core platelet proteome composed of 641 pro-
teins, including an abundance of molecules involved in
signal transduction, cytoskeletal change, and metabo-
lismunderstandable given the importance of cellular
activation and its control in platelet function. By combin-
ing prefractionation methods with suitable separation
techniques, proteomic analysis has also been used to
compile an inventory of proteins that are either (1) post-
translationally modied (normally by phosphorylation)
during the platelet activation process
80-82
or (2) present
at low abundance in the total platelet proteome but
enriched within various subcellular compartments,
including the platelet cytoskeleton,
83
alpha granules,
81,84,85
membrane fraction,
86
membrane rafts,
87
and
microparticles.
88
ANTITHROMBOTIC COMPONENTS
OF THE VESSEL WALL
Although hundreds of thousands of platelets per micro-
liter circulate in blood, under normal conditions very few,
if any, interact with the intact vessel wall because the
endothelial lining of the blood vessel presents an excel-
lent nonthrombogenic surface. In fact, this property of
the vessel wall has not yet been duplicated in any pros-
thetic or extracorporeal device. Healthy endothelium not
only provides an effective barrier between blood compo-
nents and the highly thrombogenic components of the
Chapter 25 Platelets and the Vessel Wall 1383
subendothelium (see later) but also actively produces
both membrane-bound and secretory products that limit
brin generation and promote clot dissolution. For
example, heparin-like glycosaminoglycans present on the
luminal side of the endothelial cell surface recruit plasma
antithrombin, which effects a conformational change that
promotes binding and neutralization of thrombin and
other serine proteases.
89
Thrombin, when bound to the
endothelial cell surface receptor thrombomodulin, takes
on anticoagulant properties via its cleavage and activation
of protein C, which in turn cleaves coagulation factors V
and VIII, thereby further suppressing thrombin genera-
tion.
90
Endothelial cells also express a specic receptor
for activated protein C that serves to concentrate the
protein on the endothelial surface (see Chapter 26).
91
Finally, endothelial cells synthesize, secrete, and rebind
tissue plasminogen activator,
92,93
which activates plas-
minogen to facilitate brin dissolution (see Chapter 27).
These activities are summarized in schematic form in
Figure 25-2.
The endothelial cell also produces two important
inhibitors of platelet activation: prostacyclin (PGI
2
)
94-96
and nitric oxide (NO).
97-99
A labile oxygenated metabolite
of arachidonic acid generated by endothelial cell cyclo-
oxygenase-2 (COX-2), PGI
2
diffuses out of the cell and
binds to a platelet G
s
proteincoupled receptor (GPCR)
known as the isoprostenoid (IP) receptor.
100,101
Such
binding stimulates adenylate cyclase to increase cytosolic
cyclic adenosine monophosphate (cAMP) levels, which
(1) activates a pump in the DTS that decreases cytosolic
Ca
2+
, thereby helping keep platelets quiescent, and (2)
activates protein kinase A (PKA), the actions of which
will be discussed later. PGI
2
also has potent vasodilatory
effects by binding to IP on arterial smooth muscles cells
to effect vessel relaxation.
94
The PGI
2
produced by
vascular endothelium thus serves to counterbalance
the proaggregatory and vasoconstrictor activities of the
platelet-derived prostanoid TXA
2
, the biology of which is
discussed later. In fact, upsetting the delicate balance
between COX-1derived TXA
2
and COX-2derived
PGI
2
has been shown to increase the risk for adverse
cardiovascular events.
102
Whereas PGI
2
stimulates adenylate cyclase to produce
cAMP, NO, a product of -arginine generated by endo-
thelial nitric oxide synthase (eNOS),
103
directly activates
platelet guanylate cyclase, which results in increased cyto-
solic levels of cyclic guanosine mono phosphate (cGMP).
Although platelet responses to low levels of this cyclic
nucleotide can at rst be mildly stimulatory,
104
cGMP,
largely via its activation of protein kinase G (PKG), has
the overall effect of dampening platelet responses, inhibit-
ing platelet adhesion
105,106
and aggregation,
107-110
and
cAMP
C
D
3
9
E
P
C
R
T
M
COX-2 eNOS
NO PGI
2
GAGs
APC
ATIII Plasminogen
AMP
Plasmin
FV
on
, FVIII
on
ADP
Fv
off
, FVIII
off
thrombin
PC
TPA
Adenylate
cyclase
Guanylate
cyclase
G
s
G
s
Dense tubular
system
PKG
Platelet
Endothelium
Multiple inhibitory signaling pathways
PKA
S
E
R
C
A
2
b
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+ Ca
2+
Ca
2+
Ca
2+
Ca
2+
cGMP
FIGURE 25-2. Anticoagulant and antithrombotic
components of the vascular endothelium. Endothelial
cells produce a number of substances, including nitric
oxide (NO) and prostacyclin (PGI
2
), that act on plate-
let surface receptors to dampen platelet responsiveness.
They also scavenge the platelet agonist adenosine
diphosphate (ADP), inactivate thrombin, and activate
the brinolytic enzyme plasmin. APC, activated protein
C; AMP, adenosine monophosphate; ATIII, antithrom-
bin III; cAMP, cyclic adenosine monophosphate;
cGMP, cyclic guanosine monophosphate; COX-2,
cyclooxygenase-2; eNOS, endothelial nitric oxide syn-
thase; EPCR, endothelial cell protein C receptor; FV,
factor V; GAGs, glycosaminoglycans; TM, thrombo-
modulin; IP, isoprostenoid; PC, protein C; PKA,
protein kinase A; PKG, protein kinase G; TPA, tissue
plasminogen activator.
1384 HEMOSTASIS
impeding platelet-mediated recruitment of leukocytes
during the inammatory response.
111
Its mechanism of
action is discussed in more detail later.
In addition to the soluble metabolites PGI
2
and NO,
endothelial cells also express on their surface a potent
adenosine diphosphatase (ADPase) known as CD39 that
scavenges plasma ADP to prevent platelet aggrega-
tion.
112,113
Finally, it is important to note that inamma-
tory cytokines, oxidized lipids, and immune complexes
can, under pathologic conditions, inhibit these protective
biochemical pathways and impair the antithrombotic
state of the endothelial cell. The latter changes permit
unrestrained formation of platelet- and brin-containing
thrombi, as well as thrombus formation beyond sites of
vascular injury, and can thus contribute to atherothrom-
bosisa topic that is discussed more extensively at the
end of this chapter.
REACTING TO THE BREACHCELL SURFACE
RECEPTORS THAT MEDIATE TETHERING
AND ADHESION AND TRANSMIT EARLY
ACTIVATION SIGNALS
As antithrombotic as the endothelial lining is, the under-
lying extracellular matrix consists of a rich mixture of
glycosaminoglycans into which are embedded an abun-
dance of highly concentrated prothrombotic proteins,
including structural components such as collagen and
elastin (which constitute 30% of body weight) and
adhesive proteins such as laminin, bronectin, and VWF.
Not surprisingly, platelets have evolved receptors for
most of these proteins and initiate a series of rapid bio-
chemical events both on the surface and inside the cell
when exposed to them. As a result, adhesion is an activat-
ing event!
The large number of circulating red blood cells serve
to marginate platelets, and when the vessel wall is
breached, either by mechanical injury or after rupture
of atherosclerotic plaque, the rst layer of platelets to
encounter exposed matrix undergoes a series of sequen-
tial events similar to what leukocytes experience during
the inammatory responsenamely, tethering, initial
signaling to the cell interior, integrin-mediated adhesion,
and cytoskeletally directed cell spreading. Whereas leu-
kocyte tethering is mediated by members of the selectin
family, the rst layer of platelets become tethered on
VWF,
114
which is sprinkled on exposed collagen bers.
VWF interacts with a high-afnity, platelet-specic mul-
tisubunit receptor known as the GPIb/V/IX complex.
115
This latter complex, which is expressed at approximately
25,000 copies per cell,
116
binds to the A1 domain of
VWF
117
with high-enough afnity to tether platelets even
under conditions of arterial shear.
118
Loss of the GPIB/
V/IX receptor in both humans and mice results in a clini-
cal condition known as Bernard-Soulier syndrome,
13,14
which is characterized not only by an increase in platelet
size but also by prolonged bleeding caused, in large part,
by the inability of platelets to adhere to the vessel wall.
After engagement with its ligand, GPIb acts through
membrane-proximal Src family kinases,
119
through
adapter molecules,
120
and to a lesser extent, via its asso-
ciation with immunoreceptor tyrosinebased activation
motif (ITAM)-bearing subunits
121,122
to transmit early
activation signals
123,124
that together result in the recruit-
ment and activation by tyrosine phosphorylation of phos-
pholipase C2 (PLC2),
125,126
a key enzymatic component
of platelet amplication that is required to achieve throm-
bus growth and stability (Fig. 25-3).
127
Once tethered, two different platelet integrinseach
of which exists in a low-afnity state on the platelet
surfacebegin to engage specic extracellular matrix
components and, together with the small calcium tran-
sients and kinase-generated signals emanating from the
GPIb complex and from the mechanical shear force gen-
erated by the owing blood,
128
initiate the reciprocal pro-
cesses of platelet adhesion and activation. Thus, the
2
1
integrin binds to exposed collagen brils,
129
whereas the
integrin receptor
6
1
engages laminin.
130
Both these
integrins hand off to a member of the immunoglobulin
superfamily, GPVI,
131,132
which via its noncovalent asso-
ciation in the plane of the plasma membrane with the
ITAM-bearing Fc receptor chain dimer
131,133
elicits
strong PLC2-dependent events that (1) begin the
process of cytoskeletally directed shape change and
cell spreading (discussed earlier); (2) initiate signal trans-
duction pathways (illustrated in Fig. 25-3) that cause
dramatic structural changes in platelet integrins and
thereby result in their adopting a high-afnity, ligand-
bindingcompetent conformation
134
a process known
as inside-out signal transduction (to be described in
more detail later); and (3) facilitate fusion of alpha and
dense granules with the OCS and underlying plasma
membrane.
PLATELET GRANULES AND THEIR
ROLE IN HEMOSTASIS
Platelet-specic granules are synthesized, assembled, and
packaged during megakaryocyte biogenesis, and at later
stages of maturation they appear to come into contact
with microtubules, which then transport them, via the
microtubule motor protein kinesin, along the shafts of
proplatelets until they reach the proplatelet tips.
135
Once
inside a mature platelet, platelet granules remain rela-
tively evenly dispersed throughout the cytoplasm, their
contents awaiting threshold signals for cellular activation,
at which time their membranes fuse with the plasma
membrane or, more likely, the invaginated subdomains
of the plasma membrane known as the OCS
136
(see
earlier). The regulated secretion of granule contents
ensures that hemostasis remains highly localizedan
event that has recently been exploited to deliver non
platelet-derived procoagulant proteins such as factor VIII
to sites of vascular injury.
137,138
Chapter 25 Platelets and the Vessel Wall 1385
Collagen
Laminin
VWF
GPVI
IT AM
Fyn/Lyn
Syk
PLC2
IT AM
SH2
SH2
SH2
SH2
Granule secretion
Rap1 Integrin activation
Cytoskeletal rearrangements
Shape change
Integrin clustering
GPIb-V-IX
FcR
CRP
PI3K Src
Ca
2+
release from DTS
IP
3
+
DAG
PKC
C
a
lD
A
G
-G
E
F
Syk
A
k
t
2
G
S
K
3
RIAM
Talin
1
L
A
T
,
S
L
P
-
7
6
6
1
K
i
n
a
s
e
K
i
n
a
s
e
P
I
3
K
,
C
a
2
+
S S
G
a
d
s
,
B
t
k
G
a
d
s
, B
T
K
L
A
T
, S
L
P
-7
6
FIGURE 25-3. Platelet adhesion receptors that signal through phospholipase C2 (PLC2). Each of the cell surface receptors shown recognizes
different component of the extracellular matrix and thus works in coordinated fashion to send early activation signals into the cell. Binding of
platelets to von Willebrand factor (VWF) slows platelets down so that integrins can associate productively with matrix collagen and laminin. Signals
emanating from each of these events are transmitted into the cell interior, in part via the action of receptor-associated Src family kinases (Src, Fyn,
Lyn), which phosphorylate tyrosine residues within nearby immunoreceptor tyrosinebased activation motifs (ITAMs), thus forming a nucleation
point for the assembly of miniature organelles sometime referred to as signalosomes. Signalosomes are themselves composed of the adaptor proteins
LAT, SLP-76, and Gads and the receptor tyrosine kinase Btk and function to localize, phosphorylate, and then activate PLC2, which coordinates
all these responses by generating the classic signaling molecules 1,4,5-inositol triphosphate (IP
3
) and diacylglycerol (DAG). Details regarding the
molecular events that take place after the generation of IP
3
and DAG are shown in Figures 25-4 and 25-6. Btk, Brutons tyrosine kinase; CRP, C-
reactive protein; DTS, dense tubular system; GP1b, glycoprotein Ib; GSK3, glycogen synthase kinase 3; PI3K, posphatidylinositol-3-kinase;
PKC, protein kinase C; RIAM, Rap1
GTP
-interacting adaptor molecule; SH2, Src homology domain 2.
Platelets harbor three distinct types of granules (Box
25-1). Twoalpha and dense granulesare found only in
platelets, whereas lysosomes are present in nearly all cell
types. Alpha granules are by far the most numerous, with
as many as 40 to 80 per cell, and they contain a wide array
of proteins and bioactive peptides. For ease of discussion,
Box 25-1 classies alpha granule proteins as those that
reside within the alpha granule membrane (P-selectin
being the most diagnostic), those pinocytosed from
plasma and packaged (IgG, brinogen, albumin),
139
and
those synthesized by megakaryocytes and stored (VWF,
platelet factor 4, thrombospondin). mRNA molecules
encoding the latter group have all been identied in the
platelet cytoplasm. Upon platelet activation, granules
become redistributed toward the center of the cell,
136
at
which time SNARE (soluble N-ethylmaleimidesensitive
attachment protein receptor) proteins within the alpha
granule membrane facilitate fusion,
140
with members of
the Rab family of low-molecular-weight guanosine tri-
phosphatases (GTPases) playing a prominent role in
vesicle docking and exocytosis.
141,142
After membrane
fusion, P-selectin
143-145
and alpha granule membrane
1386 HEMOSTASIS
that contain the vasoconstrictive substance seroto -
nin,
160-162
adenine and guanine nucleotides such as ADP
and ATP, inorganic pyrophosphates
163
and polyphos-
phates,
164
and the divalent cation calcium.
165
Complexes
of the latter two are probably responsible for the dark
appearance of these bodies on thin-section electron
microscopy.
166
Dense granule membranes contain a few
components in common with lysosomal membranes, such
as granulophysin (CD63, lysosome-associated membrane
protein-3 [LAMP-3])
167
and LAMP-2,
168
as well as mem-
brane proteins also present in alpha granule membranes,
such as P-selectin,
167
thus suggesting a common origin
during biogenesis. Like their alpha granule counterparts,
these dense granule membrane proteins become expressed
on the platelet cell surface after granule fusion and secre-
tion and can be used as platelet activation markers. Curi-
ously, a number of plasma membrane glycoproteins,
including GPIb and GPIIb-IIIa, have also been reported
in dense granule membranes.
169
Dense granule contents,
especially ADP,
170
play a physiologically important role in
hemostasis, as evidenced by characteristic platelet func-
tion defects in patients whose platelets lack dense gran-
ules or their contents,
171
collectively known as storage
pool disorders.
172-174
Chdiak-Higashi and Hermansky-
Pudlak
175
syndromes are two such examples of autosomal
recessive dense granule defects that lead to platelet dys-
function and bleeding, the former being associated with
immunodeciency and the latter with albinism (see
Chapter 29).
Primary lysosomes are the third organelle whose
contents are secreted upon platelet activation, but only
three or fewer per cell are normally identiable.
176
Although a clear role for lysosomes in platelet function
has not been identied, they do contain more than a
dozen different acid hydrolases, cathepsins D and E, and
other degradative enzymes that can be secreted if plate-
lets are subjected to strong agonist stimulation. Their
contents have been shown to be mildly reduced in the
platelets of individuals with GPS,
177
in keeping with the
notion that the latter disorder is caused by a defect in
packaging. The membrane proteins on platelet lysosomes
are typical of lysosomes in other cells and include LAMP-
1,
178
LAMP-2,
168
and LAMP-3.
167
FEED-FORWARD AMPLIFICATION
PATHWAYS INVOLVED IN PLATELET
RECRUITMENT AND THROMBUS STABILITY
Although platelet adhesion, early activation signals, and
granule release are prerequisites for thrombus formation,
efcient recruitment of additional platelets to the site of
the vascular lesion to yield a stable platelet plug requires
a host of additional receptor/ligand interactionseach of
which results in signal transmission and subsequent bio-
chemical and cell biologic changes that help sustain
platelet activation. Among the most important of these is
the binding of released ADP to one of its two platelet G
Box 25-1 Platelet Granules and Their Contents
ALPHA GRANULES
Membrane proteins enriched in the granule membrane: P-
selectin, TLT-1, CD40 ligand (which is cleaved after
exposure on the platelet surface to release soluble
CD40L), and tissue factor.
Membrane proteins present at similar concentrations as they are
in the plasma membrane: GPIIb-IIIa, GPIb, PECAM-1,
and perhaps many others
Granule contents:
Synthesized by megakaryocytes: Thrombospondin, VWF,
platelet factor 4, -thromboglobulin, PDGF
Endocytosed from plasma or origin not determined:
Albumin, brinogen, bronectin, IgG, Gas6,
coagulation factor V, and many chemokines and growth
factors, including RANTES, bFGF, EGF, TGF-, and
VEGF
DENSE GRANULES
ADP, ATP, 5-HT, Ca
2+
, polyphosphate
LYSOSOMES
Acid hydrolases, elastase, cathepsins, and other
degradative enzymes
ADP, adenosine diphosphate; ATP, adenosine triphosphate;
bFGF, basic broblast growth factor; EGF, epidermal growth
factor; Gas6, growth arrestspecic gene 6; GP, glycoprotein;
5-HT, 5-hydroxytryptamine; PDGF, platelet-derived growth
factor; PECAM-1, platelet endothelial cell adhesion molecule-
1; RANTES, regulated on activation, T cell expressed and
secreted; TGF-, transforming growth factor ; TLT-1, TREM
(triggering receptor expressed on myeloid cells)-like transcript-
1; VEGF, vascular endothelial growth factor; VWF, von
Willebrand factor.
specic proteins such as TLT-1
146
become expressed on
the platelet surface, and the contents of the granule are
released into the plasma milieu. Exposed P-selectin, diag-
nostic of an activated platelet,
147,148
serves to recruit leu-
kocytes to the site of injury,
149
one of a number of impor -
tant links between thrombosis and inammation
150
(discussed at the end of this chapter). Proteins secreted
from platelets include the adhesive ligands VWF and
brinogen, which serve to support platelet-platelet inter-
actions; growth factors and cytokines, which promote cell
migration
151
and wound healing
152
and maintain vascular
integrity
153
; and autocrine factors such as growth arrest
specic gene 6 (Gas6)
154
and CD40L,
155
which are released
and rebind platelet receptors to help amplify platelet
responsiveness. Finally, alpha granules and their contents
are a source of procoagulant proteins, with release of
factor V
156
and exposure of tissue factor
73,157
promoting
localized brin deposition at sites of vascular injury. Plate-
let alpha granules, or at least their contents,
158
are severely
reduced in an inherited bleeding disorder known as gray
platelet syndrome (GPS) (see Chapter 29).
159
Dense granules (four to eight per platelet) are mor-
phologically distinct, electron-opaque storage organelles
Chapter 25 Platelets and the Vessel Wall 1387
as a result of the action of phospholipase-generated 1,4,5-
inositol triphosphate (IP
3
, discussed in more detail
later)to remain cytosolic. Bioavailable calcium ions,
in turn, support a host of additional cellular events,
including more robust granule secretion, activation of
metal iondependent proteases, and activation of cell
surface integrins. The importance of ADP in amplifying
platelet responses is illustrated by the clinical effective-
ness of ticlopidine and clopidogrelwidely used phar-
macologic agents that antagonize the activity of P
2
Y
12
in pacifying platelet reactivity and inhibiting platelet
aggregation.
181
In addition to ADP-induced, P
2
Y
12
-mediated signal-
ing, nearly a dozen other soluble ligands are either gener-
ated or released at sites of vascular injury and function
in signal amplication and platelet activation. These
ligands can, for the sake of simplicity, be broken into
three classes according to the type of platelet receptor to
which they bind (Fig. 25-5). The rst class of ligands is
composed of ADP, thrombin, TXA
2
, and serotonin (5-
hydroxytryptamine [5-HT]), each of which binds to a
specic GPCR that is coupled to the heterotrimeric
subunit, G
q
. Thus, ADP binds to P
2
Y
1
,
182-185
thrombin to
the protease-activated receptors PAR1 and PAR4,
186,187
TXA
2
to the thromboxane receptor,
188,189
and serotonin
to 5-HT
2A
.
190
When released as a consequence of ligand
binding to any of these GPCRs, the G
q
subunit binds to
the isoform of phospholipase C (PLC). PLCs are lipid
hydrolases that act on membrane-associated phosphati-
dylinositol 4,5-diphosphate (PIP
2
) to produce the second
messengers IP
3
and diacylglycerol (DAG). IP
3
binds and
opens calcium channels, whereas DAG activates the most
abundant forms of protein kinase C (PKC), thereby
epi
2A
P
2
Y
12
Adenylate
cyclase
cAMP
Many other cell
biologic effects
Dense tubular
system
S
E
R
C
A
2
b
Granule
secretion
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
Ca
2+
G
i2
ADP
Gz
G
i2 Gz
FIGURE 25-4. G
i proteincoupled receptors on platelets inhibit
adenylate cyclase and lower cyclic adenosine monophosphate (cAMP)
levels. Shown are the two major receptors responsible for dampening
the activity of adenylate cyclase. As cAMP levels drop, the ability of the
SERCA2b calcium pump to sequester cytosolic calcium ions is
impaired, thereby allowing calcium-mediated activation events to occur
more readily.
Ca
2+
release
from DTS
IP
3
+
DAG
PKC
Granule secretion
Cytoskeletal rearrangements
Shape change
Integrin clustering
Rap1
RIAM
Talin
C
alD
A
G
-G
E
F
R
a
p
1
Integrin
activation
PLC
PLC
Gq
Gq
Integrins
Src
K
i
n
a
s
e
SH2
Syk
ITAM
SH2
ADP
Thrombin
TXA
2
5'HT
Fg, VWF, Collagen,
sCD40L, LM, FN
Gas6
Ephrins
GPCR RTK
L
A
T
, S
L
P
-7
6
G
a
d
s
, B
tk
FIGURE 25-5. Agonist receptors that initiate or amplify
platelet activation responses (or both). Three different
families of receptors are involved in signal amplication
pathways: G
q
-coupled GPCRs, integrins, and receptor
tyrosine kinases (RTKs). Note how each activates either
the or isoform of phospholipase C (PLC). The sum
total of PLC-generated products serves to determine the
activation state of the platelet, its ability to respond to
vascular injury, and its participation in thrombus growth.
ADP, adenosine triphosphate; Btk, Brutons tyrosine
kinase; DAG, diacylglycerol; DTS, dense tubular system;
GPCR, G
s
proteincoupled receptor; 5-HT, 5-hydroxy-
tryptamine; IP
3
, 1,4,5-inositol triphosphate; ITAM, immu-
noreceptor tyrosinebased activation motif; PKC, protein
kinase C; RIAM, Rap1
GTP
-interacting adaptor molecule;
SH2, Src homology domain 2; TXA
2
, thromboxane A
2
;
VWF, von Willebrand factor.
proteincoupled receptors, P
2
Y
12
.
179,180
Like the
2
recep-
tor for epinephrine, P
2
Y
12
is coupled to an inhibitory G
protein that slows down the activity of adenylate cyclase,
thus lowering cytosolic levels of cAMP (Fig. 25-4). This
greatly potentiates platelet responses by other agonists
because it allows calcium ionsreleased from the DTS
1388 HEMOSTASIS
initiating additional signaling cascades downstream of
this serine/threonine kinase. As shown in Figure 25-5, it
is the sum of these productsgenerated by the 2 isoform
of PLC in response to adhesion and by the isoform of
PLC in response to ligand-GPCR interactionsthat the
platelet integrates when deciding whether to become
fully activated. This concept is important in the context
of designing pharmacologic strategies to inhibit platelet
function because blocking adhesion and its consequent
activation of PLC2 leaves PLC-mediated platelet acti-
vation largely intact, and vice versa.
The second class of signal ampliers consists of the
cell surface integrins themselves.
191
As illustrated in the
middle section of Figure 25-5, when ligands bind to
integrins, the Src family kinases associated with integrin
cytoplasmic tails
192
trigger a series of incompletely under-
stood amplication events
193
that have been collectively
termed outside-in signaling.
194-196
Although this has best
been demonstrated after interaction of the major platelet
integrin
IIb
3
with its ligand brinogen, signals also
probably emanate from
2
1
134,197,198
and
6
1
132
upon
engaging collagen and laminin, respectively. Activation
signals from the latter two may be relatively weak by
comparison because of the fact that only a few thousand
of each are expressed on each platelet as compared with
50,000 to 80,000
IIb
3
receptors per cell.
199,200
The
protein kinases Syk and FAK have been shown to become
activated downstream of
IIb
3
engagement, as has activa-
tion of PLC2.
201
However, the details of these events
remain to be worked out. Finally, there is at least one
autocrine loop that uses integrin-mediated outside-in
signal amplicationthat being cleavage and rebinding
of soluble CD40L after alpha granule fusion and
secretion.
155
The third class of feed-forward amplication reac-
tions is mediated by ligand-activated plasma membrane
receptor tyrosine kinases. The rst of these to be described
were receptors for Gas6, a vitamin Kdependent protein
related to the anticoagulant protein S. Gas6 is thought
to reside in platelet alpha granules
202,203
and, like other
alpha granule proteins, becomes secreted upon platelet
activation. Interestingly, platelets have three different
receptors for Gas6Axl, Sky, and Merall of which
have active cytoplasmic tyrosine kinase activity (see Fig.
25-5). Upon engagement, Gas6 receptors appear to be
able to trigger tyrosine phosphorylation of the
3
integrin
cytoplasmic domain and thereby support outside-in inte-
grin signaling, as well as activate phosphatidylinositol-
3-kinase (PI3K) to further sustain granule secretion.
154
Platelets also express two members of the Eph receptor
tyrosine kinase family, EphA4 and EphB1, which when
in contact with their membrane-bound counter-receptor
Ephrin B1, stimulate tyrosine phosphorylation of the
integrin
3
tail and activate the integrin activator Rap1b.
204
Like Gas6 signaling,
154,205,206
genetic loss or pharmaco-
logic blockade of Ephrin/Eph kinase interactions results
in decreased ability to form a stable thrombus or retract
a brin clot.
207
ACTIVATION OF THE MAJOR PLATELET
INTEGRIN a
IIB
b
3
(GPIIB-IIIA COMPLEX)THE
FINAL COMMON END POINT OF PLATELET
ACTIVATION
Human platelets express at least ve different members
of the 24-member integrin family,
196,208
including three
1
integrins (
2
1
,
5
1
, and
6
1
specic for collagen,
bronectin, and laminin, respectively) and two
3
integ-
rins
v
3
and its close relative
IIb
3
(also known as the
GPIIb-IIIa complex).
IIb
3
is by far the most abundant
and well studied. This section focuses on our current
understanding of how
IIb
3
becomes transformed from
a resting to an active ligand-bindingcompetent confor-
mation, with the understanding that the biochemical and
cell biologic principles described for this integrin may
well apply to the others.
As shown in schematic form on the left side of Figure
25-6,
IIb
3
exists on the platelet surface in a bent-over
conformation that is unable to associate effectively with its
major soluble ligands brinogen, VWF, and bronec-
tin.
209,210
Though relatively short, the cytoplasmic domains
of
IIb
and
3
are thought to play a key role in maintaining
the off state of this integrin complex as a result of weak
charge interactions between them
211,212
that allow the
hydrophobic transmembrane domain helices of each
subunit to interact and maintain the integrin in a low-
afnity state.
213,214
When platelets become activated
either by adhesion- or soluble agonist-mediated
eventscalcium and DAG, generated as a result of the
actions of PLC2 and PLC (see Figs. 25-3 and 25-5),
bind to and activate PKC and the guanine exchange factor
CalDAG-GEF1. As illustrated in Figure 25-6, each of
these can independently activate Rap1
215-219
a low-
molecular-weight GTPase that has been implicated in
integrin activation.
220-222
Rap1 appears to activate integrins
via an effector molecule known as RIAM (Rap1
GTP
-inter-
acting adaptor molecule), which recruits the highly abun-
dant cytosolic protein talin to the inner face of the plasma
membrane to form an integrin activation complex. Binding
of RIAM-associated talin to the
3
integrin subunit repre-
sents the nal common step in integrin activation
223-225
because it disrupts the weak ionic clasp between the
IIb
3
tails and thereby allows tail separation and a dramatic,
rapid unfolding of the extracellular domain.
210
Simultane-
ous conformational changes in the integrin head
226,227
result in the formation of an integrin receptor with high
afnity for its soluble adhesive ligands. Finally, clustering
of integrins occurs
228
and ensures that bound ligands effec-
tively broker with high avidity the platelet-platelet interac-
tions that permit thrombus growth and stabilization.
CELL SURFACE AND CYTOSOLIC PROTEINS
THAT LIMIT PLATELET RESPONSES
As anyone who has suffered a myocardial infarction or
thrombotic stroke can attest to, unrestrained thrombus
Chapter 25 Platelets and the Vessel Wall 1389
growth at inappropriate sites can be as harmful as exces-
sive bleeding because it can result in vessel occlusion,
ischemia, and tissue damage. Numerous active processes
are therefore in place to limit platelet responsiveness in
healthy vessels so that thrombus growth is kept localized
to specic sites of vascular injury and dissolution of the
platelet plug during recovery is facilitated.
As discussed earlier, healthy endothelium contrib-
utes to platelet passivation via rather continuous genera-
tion of PGI
2
and NO, which act on platelets by activating
adenylate and guanylate cyclases to increase intracellular
levels of cAMP and cGMP. These messengers activate
PKA and PKG, respectively (illustrated in Fig. 25-2).
PKG controls the threshold for platelet activation pri-
marily by phosphorylating the IP
3
receptorassociated
cGMP kinase substrate IRAG,
229
a protein that associates
with PKG and IP
3
receptor type I to inhibit IP
3
-induced
calcium release from intracellular stores.
230,231
Both PKA
and PKG interfere with platelet activation by phosphory-
lating and inactivating VASP (vasodilator-stimulated
phosphoprotein),
232
a molecule with anticapping activity
that is important for the processes of actin polymeriza-
tion and lopod formation.
233-237
PKC can also bind
VASP and interfere with its ability to promote lopodia
formation, although this pathway is unique to collagen-
stimulated platelets and does not involve regulation of
PKA- or PKG-mediated VASP phosphorylation.
238
One of the better characterized inhibitory receptors
in platelets is platelet endothelial cell adhesion molecule-
1 (PECAM-1)a cell surface molecule composed of
six extracellular immunoglobulin domains, the most
amino-terminal of which engages in homophilic interac-
tions with PECAM-1 molecules on other cells, and two
cytoplasmic immunoreceptor tyrosinebased inhibitory
motifs (ITIMs) that upon phosphorylation, recruit and
activate the cytosolic SH2 domaincontaining protein
tyrosine phosphatase-2 (SHP-2).
239,240
PECAM-1 has
been shown to negatively regulate both GPVI- and GPIb/
V/IX-mediated platelet activation
241-243
perhaps by con-
trolling the phosphorylation state of these two ITAM-
bearing signaling receptorsand appears to be one of
several inhibitory receptors that control the rate and
extent of platelet thrombus formation in vivo.
244
Platelets
have also recently been found to express two other immu-
noglobulin/ITIM-containing molecules: triggering recep-
tor expressed on myeloid (TREM) cellslike transcript-1
(TLT-1) and products of the G6b gene. TLT-1 is con-
tained within platelet alpha granules and is expressed
on the platelet surface in an activation-dependent
manner.
146,245
Although the two cytoplasmic ITIMs of
TLT-1 are capable of becoming phosphorylated and
recruiting SHP-2,
146
the extent to which TLT-1/SHP-2
complexes regulate platelet function is not yet known.
The G6b gene, which is located within the class III region
of the human major histocompatibility complex,
246
gives
rise to multiple alternatively spliced transcripts (G6b-A
through G6b-G).
247
Platelets contain at least two (G6b-A
and G6b-B)
71,86,248
and possibly four (G6b-A, G6b-B,
G6b-D, and G6b-E)
249
of these transcripts, and the G6b-
B isoform contains cytoplasmic ITIMs that are capable
of becoming tyrosine-phosphorylated and recruiting
SHP-1 and SHP-2.
247
In platelets, the G6b-B isoform has
been shown to be tyrosine-phosphorylated in resting and
activated platelets, but to associate with SHP-1 only
upon platelet activation.
248
Cross-linking of antibodies
specic for G6b gene products has been shown to inhibit
platelet aggregation in response to multiple stimuli
249
;
however, whether these effects are due to the inhibitory
function of G6b-B remains to be determined.
Several inhibitory pathways have been identied in
platelets that either regulate or are regulated by PI3Ka
lipid kinase that phosphorylates the 3 position of PIP
2
to generate phosphatidylinositol 3,4,5-triphoshate (PIP
3
),
thereby creating docking sites on the inner face of the
Ca
2+
+
DAG
CalDAG-GEF1
PKC
PKD1 Rap1
RIAM/Talin
Integrin
activation
complex (IAC)
PLC
PLC
Bent stalk
+
+
+++++
EGF4
EGF3
EGF2
EGF1
PSI
H
y
b
r
i
d
F
u
l
l
y
e
x
p
o
s
e
d
l
i
g
a
n
d
b
i
n
d
i
n
g
d
o
m
a
i
n
-
T
D
C
a
l
f
2
C
a
l
f
1
T
h
i
g
h
Clasped tails
IIb
3
Cryptic
ligand
binding
domain
FIGURE 25-6. Integrin activation. As shown in the schematic at the
bottom, calcium and diacylglycerol (DAG), generated as a result of the
combined actions of phospholipase (PLC) and PLC, activate two
proteins: (1) protein kinase C (PKC) and (2) the Rap guanine exchange
factor CalDAG-GEF1. Each of these is able to independently activate
the small guanosine triphosphates (GTPase) Rap1. In its GTP-bound
form, Rap1 binds to and activates one of its effector molecules, Rap1
GTP
-
interacting adaptor molecule (RIAM), which then binds talin to form
an integrin activation complex (IAC). When the IAC binds specic sites
within the
3
cytoplasmic domain, the clasp breaks, thereby destabiliz-
ing transmembrane domain helix associations that are thought to main-
tain the integrin in its low-afnity state (shown on the left). Breaking
the hinge causes extensive conformational changes in the extracellular
domain and produces a high-afnity, ligand-bindingcompetent integ-
rin (shown on the right). EGF, epidermal growth factor; PSI, plexin-
semiphorin-integrin; -TD, beta terminal domain. (Portions adapted
from Wegener KL, Partridge AW, Han J, et al: Structural basis of integrin
activation by talin. Cell 2007;128:171, with permission.)
1390 HEMOSTASIS
plasma membrane for Pleckstrin homology (PH)
domaincontaining molecules.
250
The actions of PI3K are
opposed by the lipid phosphatase SHIP1 (SH2 domain
containing inositol 5-phosphatase 1, which hydrolyzes
the 5-phosphate of PIP
3
).
251,252
In platelets, SHIP1 has
been shown to downregulate PIP
3
generation after
IIb
3
-
mediated outside-in signaling
253
and thus may interfere
with the feed-forward amplication pathways that
increase the efciency with which platelets are recruited
to growing thrombi. Interestingly, the 5-inositol phos-
phatase activity of SHIP1 appears to be enhanced, at
least in part, by the actions of the Src family tyrosine
kinase Lyn,
254-256
which itself has been shown to limit
platelet aggregation in response to GPVI-specic
stimuli
257
and after platelet spreading on immobilized
brinogen.
253
Akt (also known as protein kinase B) is a PH domain
containing serine/threonine kinase that is a well-charac-
terized effector of PI3K.
258,259
Akt contributes positively
to platelet activation in multiple ways, one of which
appears to be by inactivating the serine/threonine kinase
glycogen synthase kinase 3 (GSK3). The GSK3 family is
composed of three isoforms (, ,
2
) that are constitu-
tively active in resting cells but become inactivated in
activated cells by Akt-mediated phosphorylation.
260
Plate-
lets express two isoforms of GSK3 ( and ), both of
which become phosphorylated and inactivated after
exposure of the platelet to multiple agonists that activate
PI3K and Akt.
261
Whereas initial studies reported that
specic inhibitors of GSK3 activity block rather than
enhance platelet responses to agonist stimulation,
261
a
recent report suggest that as in other cells, the isoform
of GSK3 acts as a negative regulator of platelet function
both in vitro and in vivo.
262
ADDITIONAL ROLES FOR PLATELETS IN
VASCULAR PHYSIOLOGY: VESSEL REPAIR
(ANGIOGENESIS), INFLAMMATION, AND
ATHEROTHROMBOSIS
In addition to being essential for primary hemostasis,
activated platelets and their secreted products have the
ability to inuence a broad array of pathophysiologic
processes, including leukocyte trafcking and inamma-
tion, tissue regeneration and angiogenesis, and both the
beginning and end stages of atherosclerosis.
Activated platelets that become spread on compo-
nents of the extracellular matrix, or on each other, display
an altered surface phenotypethe most prominent of
which is exposure of several thousand copies of the alpha
granulederived membrane protein P-selectin. P-selectin
is also expressed on cytokine-activated endothelial cells.
Thus, after either a thrombotic or inammatory event,
P-selectin appears on the luminal face of the vessel wall,
where it serves to recruit monocytes and neutrophils into
the underlying tissue by binding PSGL-1a constitu-
tively expressed counter-receptor for P-selectin that is
present on most leukocytes. In vivo, mice lacking P-selec-
tin exhibit greatly diminished leukocyte rolling, delayed
recruitment into sites of inammation, and increased
susceptibility to infection.
263,264
Although endothelial P-
selectin no doubt has a major role in leukocyte capture,
platelet P-selectin probably plays a prominent role in
secondary capture.
265,266
As in platelets, tethering also
initiates activation of leukocyte integrins, which are then
able to mediate cell spreading and transendothelial migra-
tion. P-selectin/PSGL-1 interactions therefore constitute
an important link between thrombosis and inamma-
tion.
150,267
Other platelet/leukocyte receptor/counter-
receptor pairs have also been shown to facilitate the
inammatory response, including binding of platelet-
associated brinogen to the leukocyte integrin MAC-1
268
and platelet JAM-3 binding to MAC-1 on monocytes
269
and dendritic cells.
270
In addition to forming a platform for leukocyte
recruitment during acute inammation, platelets also
deliver to the vessel wall proinammatory chemokines
that are thought to play a role in the development of
atherosclerosis by promoting further chemoattraction of
leukocytes and stimulating proliferation of vessel wall
smooth muscle cells and broblasts. Such secreted factors
include the C-X-C chemokine platelet factor 4, macro-
phage inammatory protein 1a (MIP-1a), the C-C
chemokine RANTES (regulated on activation, T cell
expressed and secreted), CD40 ligand, platelet-derived
growth factor (PDGF), and transforming growth factor
(TGF-).
150,267,271,272
Activated platelets also synthesize
de novo IL-1,
273,274
a potent stimulator of endothelial
cells and monocytes that upregulates adhesion molecule
expression. Thus, platelets appear to contribute in a
number of ways to the development and progression of
atherosclerotic lesions.
Finally, so that one is not left with the impression
that platelets only exacerbate chronic human disease, it
should be noted that platelets and their secreted products
were shown as early as 1969
153
to be able to nurture
the vascular endothelium, and they have recently been
proposed as a source of biologic response modiers for
a plethora of uses, including organ preservation, gum
restoration after dental procedures, and tissue repair after
surgery.
152
Their ability to adhere at sites of vascular
injury and secrete both degradative enzymes and at the
same time growth-promoting factors such as vascular
endothelial growth factor (VEGF), PDGF, broblast
growth factor (FGF), epidermal growth factor (EGF),
and angiopoietin 1 allows them to play a uniquely sup-
portive role in endothelial cell migration and survival
during the process of wound healing and
angiogenesis.
151
Acknowledgment
The authors thank Robert I. Handin for valuable insights
gleaned from versions of this chapter that appeared in
earlier editions of this book. Research in the authors
Chapter 25 Platelets and the Vessel Wall 1391
laboratories is supported by grants from the American
Heart Association and the National Heart, Lung, and
Blood Institute of the National Institutes of Health.
REFERENCES
1. de Gaetano G. A new blood corpuscle: an impossible
interview with Giulio Bizzozero. Thromb Haemost. 2001;
86:973-979.
2. Yamada E. The ne structure of the megakaryocyte in the
mouse spleen. Acta Anat (Basel). 1957;29:267-290.
3. Shaklai M, Tavassoli M. Demarcation membrane system
in rat megakaryocyte and the mechanism of platelet for-
mation: a membrane reorganization process. J Ultrastruct
Res. 1978;62:270-285.
4. Italiano JE, Lecine P, Shivdasani RA, Hartwig JH. Blood
platelets are assembled principally at the ends of proplate-
let processes produced by differentiated megakaryocytes.
J Cell Biol. 1999;147:1299-1312.
5. Italiano JE Jr, Shivdasani RA. Megakaryocytes and
beyond: the birth of platelets. J Thromb Haemost. 2003;1:
1174-1182.
6. Patel SR, Hartwig JH, Italiano JE Jr. The biogenesis of
platelets from megakaryocyte proplatelets. J Clin Invest.
2005;115:3348-3354.
7. Avecilla ST, Hattori K, Heissig B, et al. Chemokine-medi-
ated interaction of hematopoietic progenitors with the
bone marrow vascular niche is required for thrombopoi-
esis. Nat Med. 2004;10:64-71.
8. Radley JM, Haller CJ. The demarcation membrane system
of the megakaryocyte: a misnomer? Blood. 1982;60:
213-219.
9. Schulze H, Korpal M, Hurov J, et al. Characterization of
the megakaryocyte demarcation membrane system and its
role in thrombopoiesis. Blood. 2006;107:3868-3875.
10. Aster RH. Platelet sequestration studies in man. Br J
Haematol. 1972;22:259-263.
11. Mason KD, Carpinelli MR, Fletcher JI, et al. Programmed
anuclear cell death delimits platelet life span. Cell. 2007;
128:1173-1186.
12. Franke JD, Dong F, Rickoll WL, et al. Rod mutations
associated with MYH9-related disorders disrupt nonmus-
cle myosin-IIA assembly. Blood. 2005;105:161-169.
13. Caen JP, Nurden AT, Jeanneau C, et al. Bernard-Soulier
syndrome: a new platelet glycoprotein abnormality. Its
relationship with platelet adhesion to the subendothelium
and with the factor VIII von Willebrand protein. J Lab
Clin Med. 1976;87:586-596.
14. Jenkins CS, Phillips DR, Clemetson KJ, et al. Platelet
membrane glycoproteins implicated in ristocetin-induced
aggregation. Studies of the proteins on platelets from
patients with Bernard-Soulier syndrome and von Wille-
brands disease. J Clin Invest. 1976;57:112-124.
15. Okita JR, Pidard D, Newman PJ, et al. On the association
of glycoprotein Ib and actin-binding protein in human
platelets. J Cell Biol. 1985;100:317-321.
16. Fox JE. Linkage of a membrane skeleton to integral mem-
brane glycoproteins in human platelets. Identication of
one of the glycoproteins as glycoprotein Ib. J Clin Invest.
1985;76:1673-1683.
17. White JG, Burris SM, Hasegawa D, Johnson M. Micro-
pipette aspiration of human blood platelets: a defect in
Bernard-Souliers syndrome. Blood. 1984;63:1249-
1252.
18. Ware J, Russell S, Ruggeri ZM. Generation and rescue of
a murine model of platelet dysfunction: the Bernard-
Soulier syndrome. Proc Natl Acad Sci U S A. 2000;97:
2803-2808.
19. Corash L, Tan H, Gralnick HR. Heterogeneity of human
whole blood platelet subpopulations. I. Relationship
between buoyant density, cell volume, and ultrastructure.
Blood. 1977;49:71-87.
20. Karpatkin S. Heterogeneity of rabbit platelets. VI. Further
resolution of changes in platelet density, volume, and
radioactivity following cohort labelling with
75
Se-seleno-
methione. Br J Haematol. 1978;39:459-469.
21. Corash L, Costa JL, Shafer B, et al. Heterogeneity of
human whole blood platelet subpopulations. III. Density-
dependent differences in subcellular constituents. Blood.
1984;64:185-193.
22. Mezzano D, Hwang K, Catalano P, Aster RH. Evidence
that platelet buoyant density, but not size, correlates with
platelet age in man. Am J Hematol. 1981;11:61-76.
23. Newman PJ, Gorski J, White GC, et al. Enzymatic ampli-
cation of platelet-specic messenger RNA using the
polymerase chain reaction. J Clin Invest. 1988;82:739-
743.
24. Kienast J, Schmitz G. Flow cytometric analysis of thiazole
orange uptake by platelets: a diagnostic aid in the evalua-
tion of thrombocytopenic disorders. Blood. 1990;75:
116-121.
25. White JG, Krivit W. An ultrastructural basis for the shape
changes induced in platelets by chilling. Blood. 1967;30:
625-635.
26. Kenney DM, Linck RW. The cystoskeleton of unstimu-
lated blood platelets: structure and composition of the
isolated marginal microtubular band. J Cell Sci. 1985;
78:1-22.
27. Bentfeld ME, Bainton DF. Cytochemical localization of
lysosomal enzymes in rat megakaryocytes and platelets. J
Clin Invest. 1975;56:1635-1649.
28. Behnke O. Electron microscopic observations on the
membrane systems of the rat blood platelet. Anat Rec.
1967;158:121-137.
29. Escolar G, Leistikow E, White JG. The fate of the open
canalicular system in surface and suspension-activated
platelets. Blood. 1989;74:1983-1988.
30. White JG, Escolar G. The blood platelet open canalicular
system: a two-way street. Eur J Cell Biol. 1991;56:
233-242.
31. Gerrard JM, White JG, Peterson DA. The platelet dense
tubular system: its relationship to prostaglandin synthesis
and calcium ux. Thromb Haemost. 1978;40:224-231.
32. Papp B, Enyedi A, Pszty K, et al. Simultaneous presence
of two distinct endoplasmic-reticulumtype calcium-
pump isoforms in human cells. Characterization by
radio-immunoblotting and inhibition by 2,5-di-(t-butyl)-
1,4-benzohydroquinone. Biochem J. 1992;288:297-
302.
33. Wuytack F, Papp B, Verboomen H, et al. A sarco/endo-
plasmic reticulum Ca
2+
-ATPase 3type Ca
2+
pump is
expressed in platelets, in lymphoid cells, and in mast
cells [published erratum appears in J Biol Chem.
1994;269(17):13056]. J Biol Chem. 1994;269:1410-
1416.
1392 HEMOSTASIS
34. Enouf J, Bredoux R, Papp B, et al. Human platelets
express the SERCA2-b isoform of Ca
2+
-transport ATPase.
Biochem J. 1992;286:135-140.
35. Jardin I, Ben-amor N, Bartegi A, et al. Differential involve-
ment of thrombin receptors in Ca
2+
release from two dif-
ferent intracellular stores in human platelets. Biochem J.
2007;401:167-174.
36. Lopez JJ, Camello-Almaraz C, Pariente JA, et al. Ca
2+
accumulation into acidic organelles mediated by Ca
2+
-
and vacuolar H
+
-ATPases in human platelets. Biochem J.
2005;390:243-252.
37. Haydon GB, Taylor DA. Microtubules in hamster plate-
lets. J Cell Biol. 1965;26:673-676.
38. Behnke O. Further studies on microtubules. A marginal
bundle in human and rat thrombocytes. J Ultrastruct Res.
1965;13:469-477.
39. White JG, Krumwiede M. Isolation of microtubule coils
from normal human platelets. Blood. 1985;65:1028-
1032.
40. White JG. Effects of colchicine and vinca alkaloids on
human platelets. I. Inuence on platelet microtubules and
contractile function. Am J Pathol. 1968;53:281-291.
41. Schwer HD, Lecine P, Tiwari S, et al. A lineage-restricted
and divergent beta-tubulin isoform is essential for the
biogenesis, structure and function of blood platelets. Curr
Biol. 2001;11:579-586.
42. White JG, de Alarcon PA. Platelet spherocytosis: a new
bleeding disorder. Am J Hematol. 2002;70:158-166.
43. Fox JE, Boyles JK, Berndt MC, et al. Identication of a
membrane skeleton in platelets. J Cell Biol. 1988;106:
1525-1538.
44. Fox JE, Reynolds CC, Morrow JS, Phillips DR. Spectrin
is associated with membrane-bound actin laments in
platelets and is hydrolyzed by the Ca
2+
-dependent prote-
ase during platelet activation. Blood. 1987;69:537-545.
45. Hartwig JH, DeSisto M. The cytoskeleton of the resting
human blood platelet: structure of the membrane skeleton
and its attachment to actin laments. J Cell Biol. 1991;
112:407-425.
46. Asijee GM, Sturk A, Bruin T, et al. Vinculin is a perma-
nent component of the membrane skeleton and is incor-
porated into the (re)organising cytoskeleton upon platelet
activation. Eur J Biochem. 1990;189:131-136.
47. Fox JEB. Identication of actin-binding protein as the
protein linking the membrane skeleton to glycoproteins
on platelet plasma membranes. J Biol Chem. 1985;260:
11970-11977.
48. Loftus JC, Choate J, Albrecht RM. Platelet activation and
cytoskeletal reorganization: high voltage electron micro-
scopic examination of intact and Triton-extracted whole
mounts. J Cell Biol. 1984;98:2019-2025.
49. Newman PJ, Hillery CA, Albrecht R, et al. Activation-
dependent changes in human platelet PECAM-1: phos-
phorylation, cytoskeletal association, and surface
membrane redistribution. J Cell Biol. 1992;119:
239-246.
50. Bennett JS, Zigmond S, Vilaire G, et al. The platelet cyto-
skeleton regulates the afnity of the integrin
IIb
3
for
brinogen. J Biol Chem. 1999;274:25301-25307.
51. Hato T, Pampori N, Shattil SJ. Complementary roles for
receptor clustering and conformational change in the
adhesive and signaling functions of integrin
IIb
3
. J Cell
Biol. 1998;141:1685-1695.
52. Fox JEB, Shattil SJ, Kinlough-Rathbone RL, et al. The
platelet cytoskeleton stabilizes the interaction between
IIb
3
and its ligand and induces selective movement
of ligand-occupied integrin. J Biol Chem. 1996;271:
7004-7011.
53. Fox JE, Lipfert L, Clark EA, et al. On the role of the
platelet membrane skeleton in mediating signal transduc-
tion. Association of GP IIb-IIIa, pp60c-src, pp62c-yes,
and the p21ras GTPase-activating protein with the
membrane skeleton. J Biol Chem. 1993;268:25973-
25984.
54. Nachmias VT. Cytoskeleton of human platelets at rest and
after spreading. J Cell Biol. 1980;86:795-802.
55. Phillips DR, Jennings LK, Edwards HH. Identication of
membrane proteins mediating the interaction of human
platelets. J Cell Biol. 1980;86:77-86.
56. Rosenberg S, Stracher A, Lucas RC. Isolation and char-
acterization of actin and actin-binding protein from
human platelets. J Cell Biol. 1981;91:201-211.
57. Rosenberg S, Stracher A, Burridge K. Isolation and char-
acterization of a calcium-sensitive alpha-actininlike pro-
tein from human platelet cytoskeletons. J Biol Chem.
1981;256:12986-12991.
58. Kroll MH, Harris TS, Moake JL, et al. von Willebrand
factor binding to platelet GPIb initiates signals for platelet
activation. J Clin Invest. 1991;88:1568-1573.
59. White JG. Fine structural alterations induced in platelets
by adenosine diphosphate. Blood. 1968;31:604-622.
60. Carlsson L, Markey F, Blikstad I, et al. Reorganization of
actin in platelets stimulated by thrombin as measured by
the DNase I inhibition assay. Proc Natl Acad Sci U S A.
1979;76:6376-6380.
61. Jennings LK, Fox JE, Edwards HH, Phillips DR. Changes
in the cytoskeletal structure of human platelets following
thrombin activation. J Biol Chem. 1981;256:6927-6932.
62. Fox JE, Phillips DR. Polymerization and organization
of actin laments within platelets. Semin Hematol.
1983;20:243-260.
63. Hartwig JH. Mechanisms of actin rearrangements medi-
ating platelet activation. J Cell Biol. 1992;118:1421-
1442.
64. Barkalow KL, Italiano JE Jr, Chou DE, et al. -Adducin
dissociates from F-actin and spectrin during platelet acti-
vation. J Cell Biol. 2003;161:557-570.
65. Fox JE, Phillips DR. Role of phosphorylation in mediating
the association of myosin with the cytoskeletal structures
of human platelets. J Biol Chem. 1982;257:4120-4126.
66. Booyse F, Rafelson ME Jr. In vitro incorporation of
amino-acids into the contractile protein of human blood
platelets. Nature. 1967;215:283-284.
67. Kieffer N, Guichard J, Farcet JP, et al. Biosynthesis of
major platelet proteins in human blood platelets. Eur J
Biochem. 1987;164:189-195.
68. Gnatenko DV, Dunn JJ, McCorkle SR, et al. Transcript
proling of human platelets using microarray and serial
analysis of gene expression. Blood. 2003;101:2285-
2293.
69. McRedmond JP, Park SD, Reilly DF, et al. Integration of
proteomics and genomics in platelets: a prole of platelet
proteins and platelet-specic genes. Mol Cell Proteomics.
2004;3:133-144.
70. Dittrich M, Birschmann I, Pfrang J, et al. Analysis of
SAGE data in human platelets: features of the transcrip-
Chapter 25 Platelets and the Vessel Wall 1393
tome in an anucleate cell. Thromb Haemost. 2006;95:
643-651.
71. Macaulay IC, Tijssen MR, Thijssen-Timmer DC, et al.
Comparative gene expression proling of in vitro differ-
entiated megakaryocytes and erythroblasts identies novel
activatory and inhibitory platelet membrane proteins.
Blood. 2007;109:3260-3269.
72. Denis MM, Tolley ND, Bunting M, et al. Escaping the
nuclear connes: signal-dependent pre-mRNA splicing in
anucleate platelets. Cell. 2005;122:379-391.
73. Schwertz H, Tolley ND, Foulks JM, et al. Signal-depen-
dent splicing of tissue factor pre-mRNA modulates the
thrombogenicity of human platelets. J Exp Med. 2006;203:
2433-2440.
74. Weyrich AS, Denis MM, Schwertz H, et al. mTOR-
dependent synthesis of Bcl-3 controls the retraction of
brin clots by activated human platelets. Blood. 2007;109:
1975-1983.
75. OFarrell PH. High resolution two-dimensional electro-
phoresis of proteins. J Biol Chem. 1975;250:4007-4021.
76. Ames GF, Nikaido K. Two-dimensional gel electro -
phoresis of membrane proteins. Biochemistry. 1976;15:
616-623.
77. Macaulay IC, Carr P, Gusnanto A, et al. Platelet genomics
and proteomics in human health and disease. J Clin
Invest. 2005;115:3370-3377.
78. Dittrich M, Birschmann I, Stuhlfelder C, et al. Under-
standing platelets. Lessons from proteomics, genomics
and promises from network analysis. Thromb Haemost.
2005;94:916-925.
79. Martens L, Van DP, Van DJ, et al. The human platelet
proteome mapped by peptide-centric proteomics: a func-
tional protein prole. Proteomics. 2005;5:3193-3204.
80. Marcus K, Moebius J, Meyer HE. Differential analysis of
phosphorylated proteins in resting and thrombin-stimu-
lated human platelets. Anal Bioanal Chem. 2003;376:
973-993.
81. Maguire PB, Fitzgerald DJ. Platelet proteomics. J Thromb
Haemost. 2003;1:1593-1601.
82. Garcia A, Senis YA, Antrobus R, et al. A global proteomics
approach identies novel phosphorylated signaling pro-
teins in GPVI-activated platelets: involvement of G6f, a
novel platelet Grb2-binding membrane adapter. Pro-
teomics. 2006;6:5332-5343.
83. Gevaert K, Eggermont L, Demol H, Vandekerckhove J. A
fast and convenient MALDI-MS based proteomic
approach: identication of components scaffolded by the
actin cytoskeleton of activated human thrombocytes. J
Biotechnol. 2000;78:259-269.
84. Maguire PB, Moran N, Cagney G, Fitzgerald DJ. Applica-
tion of proteomics to the study of platelet regulatory
mechanisms. Trends Cardiovasc Med. 2004;14:207-220.
85. Coppinger JA, Cagney G, Toomey S, et al. Characteriza-
tion of the proteins released from activated platelets leads
to localization of novel platelet proteins in human athero-
sclerotic lesions. Blood. 2004;103:2096-2104.
86. Moebius J, Zahedi RP, Lewandrowski U, et al. The human
platelet membrane proteome reveals several new potential
membrane proteins. Mol Cell Proteomics. 2005;4:1754-
1761.
87. Maguire PB, Foy M, Fitzgerald DJ. Using proteomics to
identify potential therapeutic targets in platelets. Biochem
Soc Trans. 2005;33:409-412.
88. Garcia BA, Smalley DM, Cho H, et al. The platelet mic-
roparticle proteome. J Proteome Res. 2005;4:1516-
1521.
89. Damus PS, Hicks M, Rosenberg RD. Anticoagulant
action of heparin. Nature. 1973;246:355-357.
90. Esmon CT. The roles of protein C and thrombomodulin
in the regulation of blood coagulation. J Biol Chem.
1989;264:4743-4746.
91. Fukudome K, Esmon CT. Identication, cloning, and reg-
ulation of a novel endothelial cell protein C/activated
protein C receptor. J Biol Chem. 1994;269:26486-26491.
92. Levin EG. Latent tissue plasminogen activator produced
by human endothelial cells in culture: evidence for an
enzyme-inhibitor complex. Proc Natl Acad Sci U S A.
1983;80:6804-6808.
93. Hajjar KA, Hamel NM, Harpel PC, Nachman RL.
Binding of tissue plasminogen activator to cultured human
endothelial cells. J Clin Invest. 1987;80:1712-1719.
94. Bunting S, Gryglewski R, Moncada S, Vane JR. Arterial
walls generate from prostaglandin endoperoxides a sub-
stance (prostaglandin X) which relaxes strips of mesen-
teric and coeliac arteries and inhibits platelet aggregation.
Prostaglandins. 1976;12:897-913.
95. Gryglewski RJ, Bunting S, Moncada S, et al. Arterial walls
are protected against deposition of platelet thrombi by a
substance (prostaglandin X) which they make from pros-
taglandin endoperoxides. Prostaglandins. 1976;12:685-
713.
96. Moncada S, Gryglewski R, Bunting S, Vane JR. An enzyme
isolated from arteries transforms prostaglandin endoper-
oxides to an unstable substance that inhibits platelet
aggregation. Nature. 1976;263:663-665.
97. Furchgott RF, Zawadzki JV. The obligatory role of endo-
thelial cells in the relaxation of arterial smooth muscle by
acetylcholine. Nature. 1980;288:373-376.
98. Ignarro LJ, Buga GM, Wood KS, et al. Endothelium-
derived relaxing factor produced and released from artery
and vein is nitric oxide. Proc Natl Acad Sci U S A.
1987;84:9265-9269.
99. Palmer RM, Ferrige AG, Moncada S. Nitric oxide release
accounts for the biological activity of endothelium-derived
relaxing factor. Nature. 1987;327:524-526.
100. Boie Y, Rushmore TH, Darmon-Goodwin A, et al. Cloning
and expression of a cDNA for the human prostanoid IP
receptor. J Biol Chem. 1994;269:12173-12178.
101. Namba T, Oida H, Sugimoto Y, et al. cDNA cloning of a
mouse prostacyclin receptor. Multiple signaling pathways
and expression in thymic medulla. J Biol Chem. 1994;
269:9986-9992.
102. Cheng Y, Austin SC, Rocca B, et al. Role of prostacyclin
in the cardiovascular response to thromboxane A
2
. Science.
2002;296:539-541.
103. Pollock JS, Forstermann U, Mitchell JA, et al. Purication
and characterization of particulate endothelium-derived
relaxing factor synthase from cultured and native bovine
aortic endothelial cells. Proc Natl Acad Sci U S A. 1991;
88:10480-10484.
104. Li Z, Xi X, Gu M, et al. A stimulatory role for cGMP-
dependent protein kinase in platelet activation. Cell.
2003;112:77-86.
105. Radomski MW, Palmer RM, Moncada S. Endogenous
nitric oxide inhibits human platelet adhesion to vascular
endothelium. Lancet. 1987;2:1057-1058.
1394 HEMOSTASIS
106. Sneddon JM, Vane JR. Endothelium-derived relaxing
factor reduces platelet adhesion to bovine endothelial
cells. Proc Natl Acad Sci U S A. 1988;85:2800-2804.
107. Azuma H, Ishikawa M, Sekizaki S. Endothelium-depen-
dent inhibition of platelet aggregation. Br J Pharmacol.
1986;88:411-415.
108. Radomski MW, Palmer RM, Moncada S. The anti-aggre-
gating properties of vascular endothelium: interactions
between prostacyclin and nitric oxide. Br J Pharmacol.
1987;92:639-646.
109. Macdonald PS, Read MA, Dusting GJ. Synergistic inhibi-
tion of platelet aggregation by endothelium-derived relax-
ing factor and prostacyclin. Thromb Res. 1988;49:
437-449.
110. Stamler J, Mendelsohn ME, Amarante P, et al. N-acetyl-
cysteine potentiates platelet inhibition by endothelium-
derived relaxing factor. Circ Res. 1989;65:789-795.
111. Michelson AD, Benoit SE, Furman MI, et al. Effects of
nitric oxide/EDRF on platelet surface glycoproteins. Am
J Physiol. 1996;270:H1640-H1648.
112. Kaczmarek E, Koziak K, Sevigny J, et al. Identication
and characterization of CD39/vascular ATP diphospho-
hydrolase. J Biol Chem. 1996;271:33116-33122.
113. Marcus AJ, Broekman MJ, Drosopoulos JH, et al. The
endothelial cell ecto-ADPase responsible for inhibition of
platelet function is CD39. J Clin Invest. 1997;99:
1351-1360.
114. Dopheide SM, Maxwell MJ, Jackson SP. Shear-dependent
tether formation during platelet translocation on von Wil-
lebrand factor. Blood. 2002;99:159-167.
115. Lopez JA, Berndt MC. The GPIb-IX-V Complex.
Platelets. San Diego, CA, Academic Press, 2002, pp
85-97.
116. Coller BS, Peerschke EL, Scudder IE, Sullivan CA.
Studies with a murine monoclonal antibody that abolishes
ristocetin-induced binding of von Willebrand factor to
platelets: additional evidence in support of GPIb as a
platelet receptor for von Willebrand factor. Blood. 1983;
61:99-110.
117. Lankhof H, Wu YP, Vink T, et al. Role of the glycoprotein
Ib-binding A1 repeat and the RGD sequence in platelet
adhesion to human recombinant von Willebrand factor.
Blood. 1995;86:1035-1042.
118. Savage B, Saldivar E, Ruggeri ZM. Initiation of platelet
adhesion by arrest onto brinogen or translocation on von
Willebrand factor. Cell. 1996;84:289-297.
119. Kasirer-Friede A, Cozzi MR, Mazzucato M, et al.
Signaling through GP Ib-IX-V activates alpha IIb beta
3 independently of other receptors. Blood. 2004;103:
3403-3411.
120. Kasirer-Friede A, Moran B, Nagrampa-Orje J, et al.
ADAP is required for normal
lIb
3
activation by VWF/GP
Ib-IX-V and other agonists. Blood. 2007;109:
1018-1025.
121. Sullam PM, Hyun WC, Szollosi J, et al. Physical proximity
and functional interplay of the glycoprotein Ib-IX-V
complex and the Fc receptor FcRIIA on the platelet
plasma membrane. J Biol Chem. 1998;273:5331-
5336.
122. Falati S, Edmead CE, Poole AW. Glycoprotein Ib-V-IX, a
receptor for von Willebrand factor, couples physically and
functionally to the Fc receptor -chain, fyn, and lyn to
activate human platelets. Blood. 1999;94:1648-1656.
123. Nesbitt WS, Kulkarni S, Giuliano S, et al. Distinct glyco-
protein Ib/V/IX and integrin
lIb
3
-dependent calcium
signals cooperatively regulate platelet adhesion under
ow. J Biol Chem. 2002;277:2965-2972.
124. Mazzucato M, Pradella P, Cozzi MR, et al. Sequential
cytoplasmic calcium signals in a 2-stage platelet activation
process induced by the glycoprotein Ib mechanorecep-
tor. Blood. 2002;100:2793-2800.
125. Jackson SP, Nesbitt WS, Kulkarni S. Signaling events
underlying thrombus formation. J Thromb Haemost.
2003;1:1602-1612.
126. Mangin P, Yuan Y, Goncalves I, et al. Signaling role for
PLC2 in platelet glycoprotein Ib calcium ux and cyto-
skeletal reorganization involvement of a pathway distinct
from FcR-chain and FcRIIA. J Biol Chem. 2003;278:
32880-32891.
127. Rathore V, Wang D, Newman DK, Newman PJ. Phospho-
lipase C2 contributes to stable thrombus formation on
VWF. Febs Lett. 2004;573:26-30.
128. Goncalves I, Nesbitt WS, Yuan Y, Jackson SP. Importance
of temporal ow gradients and integrin
IIb
3
mechano-
transduction for shear activation of platelets. J Biol Chem.
2005;280:15430-15437.
129. Staatz WD, Rajpara SM, Wayner EA, et al. The membrane
glycoprotein Ia-IIa (VLA-2) complex mediates the Mg
2+
-
dependent adhesion of platelets to collagen. J Cell Biol.
1989;108:1917-1924.
130. Sonnenberg A, Modderman PW, Hogervorst F. Laminin
receptor on platelets is the integrin VLA-6. Nature.
1988;336:487-489.
131. Gibbins JM, Okuma M, Farndale R, et al. Glycoprotein
VI is the collagen receptor in platelets which underlies
tyrosine phosphorylation of the Fc receptor -chain. Febs
Lett. 1997;413:255-259.
132. Inoue O, Suzuki-Inoue K, McCarty OJ, et al. Laminin
stimulates spreading of platelets through integrin
6
1
-
dependent activation of GPVI. Blood. 2006;107:
1405-1412.
133. Tsuji M, Ezumi Y, Arai M, Takayama H. A novel
association of Fc receptor -chain with glycoprotein
VI and their co-expression as a collagen receptor
in human platelets. J Biol Chem. 1997;272:23528-
23531.
134. Chen H, Kahn ML. Reciprocal signaling by integrin and
nonintegrin receptors during collagen activation of plate-
lets. Mol Cell Biol. 2003;23:4764-4777.
135. Richardson JL, Shivdasani RA, Boers C, et al. Mecha-
nisms of organelle transport and capture along proplate-
lets during platelet production. Blood. 2005;106:
4066-4075.
136. Stenberg PE, Shuman MA, Levine SP, Bainton DF.
Redistribution of alpha-granules and their contents in
thrombin-stimulated platelets. J Cell Biol. 1984;98:
748-760.
137. Yarovoi HV, Kufrin D, Eslin DE, et al. Factor VIII ectopi-
cally expressed in platelets: efcacy in hemophilia A treat-
ment. Blood. 2003;102:4006-4013.
138. Shi Q, Wilcox DA, Fahs SA, et al. Factor VIII ectopically
targeted to platelets is therapeutic in hemophilia A with
high-titer inhibitory antibodies. J Clin Invest. 2006;116:
1974-1982.
139. Handagama PJ, George JN, Shuman MA, et al. Incorpo-
ration of a circulating protein into megakaryocyte and
Chapter 25 Platelets and the Vessel Wall 1395
platelet granules. Proc Natl Acad Sci U S A. 1987;84:
861-865.
140. Reed GL. Platelet secretory mechanisms. Semin Thromb
Hemost. 2004;30:441-450.
141. Swank RT, Jiang SY, Reddington M, et al. Inherited
abnormalities in platelet organelles and platelet formation
and associated altered expression of low molecular weight
guanosine triphosphatebinding proteins in the mouse
pigment mutant gunmetal. Blood. 1993;81:2626-
2635.
142. Shirakawa R, Yoshioka A, Horiuchi H, et al. Small GTPase
Rab4 regulates Ca
2+
-induced alpha-granule secretion in
platelets. J Biol Chem. 2000;275:33844-33849.
143. Stenberg PE, McEver RP, Shuman MA, et al. A platelet
alpha-granule membrane protein (GMP-140) is expressed
on the plasma membrane after activation. J Cell Biol.
1985;101:880-886.
144. Berman CL, Yeo EL, Wencel-Drake JD, et al. A platelet
alpha granule membrane protein that is associated with
the plasma membrane after activation. J Clin Invest.
1986;78:130-137.
145. Beckstead JH, Stenberg PE, McEver RP, et al. Immuno-
histochemical localization of membrane and alpha-granule
proteins in human megakaryocytes: application to plastic-
embedded bone marrow biopsy specimens. Blood.
1986;67:285-293.
146. Washington AV, Schubert RL, Quigley L, et al. A TREM
family member, TLT-1, is found exclusively in the alpha-
granules of megakaryocytes and platelets. Blood. 2004;
104:1042-1047.
147. Ruf A, Patscheke H. Flow cytometric detection of acti-
vated platelets: comparison of determining shape change,
brinogen binding, and P-selectin expression. Semin
Thromb Hemost. 1995;21:146-151.
148. Michelson AD, Furman MI. Laboratory markers of plate-
let activation and their clinical signicance. Curr Opin
Hematol. 1999;6:342-348.
149. Palabrica T, Lobb R, Furie BC, et al. Leukocyte accumu-
lation promoting brin deposition is mediated in vivo
by P-selectin on adherent platelets. Nature. 1992;359:
848-851.
150. Wagner DD, Burger PC. Platelets in inammation and
thrombosis. Arterioscler Thromb Vasc Biol. 2003;23:2131-
2137.
151. Kisucka J, Buttereld CE, Duda DG, et al. Platelets and
platelet adhesion support angiogenesis while preventing
excessive hemorrhage. Proc Natl Acad Sci U S A. 2006;
103:855-860.
152. Anitua E, Andia I, Ardanza B, et al. Autologous platelets
as a source of proteins for healing and tissue regeneration.
Thromb Haemost. 2004;91:4-15.
153. Gimbrone MA Jr, Aster RH, Cotran RS, et al. Pre -
servation of vascular integrity in organs perfused in
vitro with a platelet-rich medium. Nature. 1969;222:33-
36.
154. Angelillo-Scherrer A, Burnier L, Flores N, et al. Role of
Gas6 receptors in platelet signaling during thrombus sta-
bilization and implications for antithrombotic therapy. J
Clin Invest. 2005;115:237-246.
155. Prasad KS, Andre P, He M, et al. Soluble CD40 ligand
induces
3
integrin tyrosine phosphorylation and triggers
platelet activation by outside-in signaling. Proc Natl Acad
Sci U S A. 2003;100:12367-12371.
156. Camire RM, Pollak ES, Kaushansky K, Tracy PB. Secre-
table human platelet-derived factor V originates from the
plasma pool. Blood. 1998;92:3035-3041.
157. Panes O, Matus V, Saez CG, et al. Human platelets syn-
thesize and express functional tissue factor. Blood.
2007;109:5242-5250.
158. Rosa JP, George JN, Bainton DF, et al. Gray platelet syn-
drome. Demonstration of alpha granule membranes that
can fuse with the cell surface. J Clin Invest. 1987;80:
1138-1146.
159. Raccuglia G. Gray platelet syndrome. A variety of qualita-
tive platelet disorder. Am J Med. 1971;51:818-828.
160. Da Prada M., Pletscher A, Tranzer JP, Knuchel H.
Subcellular localization of 5-hydroxytryptamine and
histamine in blood platelets. Nature. 1967;216:1315-
1317.
161. White JG. The dense bodies of human platelets. Origin of
serotonin storage particles from platelet granules. Am J
Pathol. 1968;53:791-808.
162. Davis RB, White JG. Localization of 5-hydroxytryptamine
in blood platelets: an autoradiographic and ultrastructural
study. Br J Haematol. 1968;15:93-99.
163. Silcox DC, Jacobelli S, McCarty DJ. Identication of
inorganic pyrophosphate in human platelets and its release
on stimulation with thrombin. J Clin Invest. 1973;52:
1595-1600.
164. Ruiz FA, Lea CR, Oldeld E, Docampo R. Human plate-
let dense granules contain polyphosphate and are similar
to acidocalcisomes of bacteria and unicellular eukaryotes.
J Biol Chem. 2004;279:44250-44257.
165. Lages B, Scrutton MC, Holmsen H, et al. Metal ion
contents of gel-ltered platelets from patients with storage
pool disease. Blood. 1975;46:119-130.
166. Gerrard JM, Rao GH, White JG. The inuence of reser-
pine and ethylenediaminetetraacetic acid (EDTA) on
serotonin storage organelles of blood platelets. Am J
Pathol. 1977;87:633-646.
167. Israels SJ, Gerrard JM, Jacques YV, et al. Platelet dense
granule membranes contain both granulophysin and P-
selectin (GMP-140). Blood. 1992;80:143-152.
168. Israels SJ, McMillan EM, Robertson C, et al. The lyso-
somal granule membrane protein, LAMP-2, is also present
in platelet dense granule membranes. Thromb Haemost.
1996;75:623-629.
169. Youssean T, Masse JM, Rendu F, et al. Platelet and
megakaryocyte dense granules contain glycoproteins Ib
and IIb-IIIa. Blood. 1997;89:4047-4057.
170. Lages B, Holmsen H, Weiss HJ, Dangelmaier C. Throm-
bin and ionophore A23187induced dense granule secre-
tion in storage pool decient platelets: evidence for
impaired nucleotide storage as the primary dense granule
defect. Blood. 1983;61:154-162.
171. Weiss HJ, Ames RP. Ultrastructural ndings in storage
pool disease and aspirin-like defects of platelets. Am J
Pathol. 1973;71:447-466.
172. Holmsen H, Weiss HJ. Hereditary defect in the release
reaction caused by a deciency in the storage pool of
platelet adenine nucleotides. Br J Haematol. 1970;19:
643-649.
173. Weiss HJ, Witte LD, Kaplan KL, et al. Heterogeneity in
storage pool deciency: Studies on granule-bound sub-
stances in 18 patients including variants decient in
alpha-granules, platelet factor 4, -thromboglobulin and
1396 HEMOSTASIS
platelet-derived growth factor. Blood. 1979;54:1296-
1319.
174. Weiss HJ, Hawiger J, Ruggeri ZM, et al. Fibrinogen-inde-
pendent platelet adhesion and thrombus formation on
subendothelium mediated by glycoprotein IIb-IIIa
complex at high shear rate. J Clin Invest. 1989;83:
288-297.
175. Hermansky F, Pudlak P. Albinism associated with hemor-
rhagic diathesis and unusual pigmented reticular cells in
the bone marrow: report of two cases with histochemical
studies. Blood. 1959;14:162-169.
176. Bentfeld-Barker ME, Bainton DF. Identication of
primary lysosomes in human megakaryocytes and plate-
lets. Blood. 1982;59:472-481.
177. Srivastava PC, Powling MJ, Nokes TJ, et al. Grey platelet
syndrome: studies on platelet alpha granules, lysosomes
and defective response to thrombin. Br J Haematol. 1987;
65:441-446.
178. Febbraio M, Silverstein RL. Identication and character-
ization of LAMP-1 as an activation-dependent platelet
surface glycoprotein. J Biol Chem. 1990;265:18531-
18537.
179. Jantzen HM, Gousset L, Bhaskar V, et al. Evidence for
two distinct G-proteincoupled ADP receptors mediating
platelet activation. Thromb Haemost. 1999;81:111-
117.
180. Murugappan S, Shankar H, Kunapuli SP. Platelet recep-
tors for adenine nucleotides and thromboxane A
2
. Semin
Thromb Hemost. 2004;30:411-418.
181. Conley PB, Delaney SM. Scientic and therapeutic
insights into the role of the platelet P
2
Y
12
receptor in
thrombosis. Curr Opin Hematol. 2003;10:333-338.
182. Leon C, Hechler B, Vial C, et al. The P
2
Y
1
receptor is an
ADP receptor antagonized by ATP and expressed in
platelets and megakaryoblastic cells. FEBS Lett. 1997;403:
26-30.
183. Hechler B, Leon C, Vial C, et al. The P
2
Y
1
receptor is
necessary for adenosine 5-diphosphateinduced platelet
aggregation. Blood. 1998;92:152-159.
184. Jin J, Daniel JL, Kunapuli SP. Molecular basis for ADP-
induced platelet activation. II. The P
2
Y
1
receptor mediates
ADP-induced intracellular calcium mobilization and
shape change in platelets. J Biol Chem. 1998;273:
2030-2034.
185. Leon C, Hechler B, Freund M, et al. Defective platelet
aggregation and increased resistance to thrombosis in
purinergic P
2
Y
1
receptor-null mice. J Clin Invest. 1999;
104:1731-1737.
186. Vu T-KH, Hung DT, Wheaton VI, Coughlin SR. Molecu-
lar cloning of a functional thrombin receptor reveals a
novel proteolytic mechanism of receptor activation. Cell.
1991;64:1057-1068.
187. Kahn ML, Nakanishi-Matsui M, Shapiro MJ, et al. Pro-
tease-activated receptors 1 and 4 mediate activation of
human platelets by thrombin. J Clin Invest. 1999;103:
879-887.
188. Shenker A, Goldsmith P, Unson CG, Spiegel AM. The G
protein coupled to the thromboxane A
2
receptor in human
platelets is a member of the novel G
q
family. J Biol Chem.
1991;266:9309-9313.
189. Kinsella BT, OMahony DJ, Fitzgerald GA. The human
thromboxane A
2
receptor alpha isoform (TP alpha) func-
tionally couples to the G proteins G
q
and G
11
in vivo and
is activated by the isoprostane 8-epi prostaglandin F
2
alpha. J Pharmacol Exp Ther. 1997;281:957-964.
190. Hourani SM, Cusack NJ. Pharmacological receptors on
blood platelets. Pharmacol Rev. 1991;43:243-298.
191. Du XP, Plow EF, Frelinger AL, et al. Ligands activate
integrin
IIb
3
(platelet GPIIb- IIIa). Cell. 1991;65:
409-416.
192. Shattil SJ. Integrins and Src: dynamic duo of adhesion
signaling. Trends Cell Biol. 2005;15:399-403.
193. Obergfell A, Eto K, Mocsai A, et al. Coordinate interac-
tions of Csk, Src, and Syk kinases with
IIb
3
initiate
integrin signaling to the cytoskeleton. J Cell Biol. 2002;
157:265-275.
194. Law DA, Nanniaai-Alaimo L, Phillips DR. Outside-in
integrin signal transduction.
IIb
3
(GPIIb-IIIa) tyrosine
phosphorylation induced by platelet aggregation. J Biol
Chem. 1996;271:10811-10815.
195. Shattil SJ. Signaling through platelet integrin
IIb
3
: inside-
out, outside-in, and sideways. Thromb Haemost. 1999;82:
318-325.
196. Shattil SJ, Newman PJ. Integrins: dynamic scaffolds for
adhesion and signaling in platelets. Blood. 2004;104:
1606-1615.
197. Keely PJ, Parise LV. The
2
1
integrin is a necessary co-
receptor for collagen-induced activation of syk and the
subsequent phosphorylation of phospholipase C2 in
platelets. J Biol Chem. 1996;271:26668-26676.
198. Inoue O, Suzuki-Inoue K, Dean WL, et al. Integrin
2
1
mediates outside-in regulation of platelet spreading on
collagen through activation of Src kinases and PLC2. J
Cell Biol. 2003;160:769-780.
199. Newman PJ, Allen RW, Kahn RA, Kunicki TJ. Quantita-
tion of membrane glycoprotein IIIa on intact human
platelets using the monoclonal antibody, AP-3. Blood.
1985;65:227-232.
200. Wagner CL, Mascelli MA, Neblock DS, et al. Analysis
of GPIIb/IIIa receptor number by quantication of
7E3 binding to human platelets. Blood. 1996;88:907-
914.
201. Goncalves I, Hughan SC, Schoenwaelder SM, et al. Inte-
grin
IIb
3
-dependent calcium signals regulate platelet-
brinogen interactions under ow: involvement of PLC2.
J Biol Chem. 2003;278:34812-34822.
202. Angelillo-Scherrer A, de Frutos P, Aparicio C, et al. De-
ciency or inhibition of Gas6 causes platelet dysfunction
and protects mice against thrombosis. Nat Med. 2001;
7:215-221.
203. Balogh I, Hazi S, Stenhoff J, et al. Analysis of Gas6 in
human platelets and plasma. Arterioscler Thromb Vasc
Biol. 2005;25:1280-1286.
204. Prevost N, Woulfe DS, Tognolini M, et al. Signaling by
ephrinB1 and Eph kinases in platelets promotes Rap1
activation, platelet adhesion, and aggregation via effector
pathways that do not require phosphorylation of ephrinB1.
Blood. 2004;103:1348-1355.
205. Gould WR, Baxi SM, Schroeder R, et al. Gas6 receptors
Axl, Sky and Mer enhance platelet activation and regulate
thrombotic responses. J Thromb Haemost. 2005;3:733-
741.
206. Saller F, Burnier L, Schapira M, Angelillo-Scherrer A.
Role of the growth arrest-specic gene 6 (gas6) product
in thrombus stabilization. Blood Cells Mol Dis. 2006;36:
373-378.
Chapter 25 Platelets and the Vessel Wall 1397
207. Prevost N, Woulfe DS, Jiang H, et al. Eph kinases and
ephrins support thrombus growth and stability by regulat-
ing integrin outside-in signaling in platelets. Proc Natl
Acad Sci U S A. 2005;102:9820-9825.
208. Hynes RO. Integrins: bidirectional, allosteric signaling
machines. Cell. 2002;110:673-687.
209. Xiong JP, Stehle T, Diefenbach B, et al. Crystal structure
of the extracellular segment of integrin
V
3
. Science.
2001;294:339-345.
210. Takagi J, Petre BM, Walz T, Springer TA. Global confor-
mational rearrangements in integrin extracellular domains
in outside-in and inside-out signaling. Cell. 2002;110:
599-611.
211. Vinogradova O, Velyvis A, Velyviene A, et al. A structural
mechanism of integrin
IIb
3
inside-out activation
as regulated by its cytoplasmic face. Cell. 2002;110:
587-597.
212. Vinogradova O, Vaynberg J, Kong X, et al. Membrane-
mediated structural transitions at the cytoplasmic face
during integrin activation. Proc Natl Acad Sci U S A.
2004;101:4094-4099.
213. Luo BH, Springer TA, Takagi J. A specic interface
between integrin transmembrane helices and afnity for
ligand. PLoS Biol. 2004;2:e153.
214. Partridge AW, Liu S, Kim S, et al. Transmembrane domain
helix packing stabilizes integrin
IIb
3
in the low afnity
state. J Biol Chem. 2005;280:7294-7300.
215. Medeiros RB, Dickey DM, Chung H, et al. Protein kinase
D
1
and the
1
integrin cytoplasmic domain control
1
integrin function via regulation of Rap1 activation. Immu-
nity. 2005;23:213-226.
216. Ebinu JO, Bottorff DA, Chan EY, et al. RasGRP, a Ras
guanyl nucleotidereleasing protein with calcium- and
diacylglycerol-binding motifs. Science. 1998;280:1082-
1086.
217. Eto K, Murphy R, Kerrigan SW, et al. Megakaryocytes
derived from embryonic stem cells implicate CalDAG-
GEFI in integrin signaling. Proc Natl Acad Sci U S A.
2002;99:12819-12824.
218. Crittenden JR, Bergmeier W, Zhang Y, et al. CalDAG-
GEFI integrates signaling for platelet aggregation and
thrombus formation. Nat Med. 2004;10:982-986.
219. Han J, Lim CJ, Watanabe N, et al. Reconstructing and
deconstructing agonist-induced activation of integrin
IIb
3
. Curr Biol. 2006;16:1796-1806.
220. Bertoni A, Tadokoro S, Eto K, et al. Relationships between
Rap1b, afnity modulation of integrin
IIb
3
, and the actin
cytoskeleton. J Biol Chem. 2002;277:25715-25721.
221. de Bruyn KM, Zwartkruis FJ, de Rooij J, et al. The small
GTPase Rap1 is activated by turbulence and is involved
in integrin
IIb
3
-mediated cell adhesion in human mega-
karyocytes. J Biol Chem. 2003;278:22412-22417.
222. Bos JL, de Bruyn K, Enserink J, et al. The role of Rap1
in integrin-mediated cell adhesion. Biochem Soc Trans.
2003;31:83-86.
223. Tadokoro S, Shattil SJ, Eto K, et al. Talin binding to
integrin beta tails: a nal common step in integrin activa-
tion. Science. 2003;302:103-106.
224. Wegener KL, Partridge AW, Han J, et al. Structural
basis of integrin activation by talin. Cell. 2007;128:
171-182.
225. Petrich BG, Fogelstrand P, Partridge AW, et al. The
antithrombotic potential of selective blockade of talin-
dependent integrin
IIb
3
(platelet GPIIb-IIIa) activation.
J Clin Invest. 2007;117:2250-2259.
226. Xiao T, Takagi J, Coller BS, et al. Structural basis for
allostery in integrins and binding to brinogen-mimetic
therapeutics. Nature. 2004;432:59-67.
227. Zhu J, Boylan B, Luo BH, et al. Tests of the extension and
deadbolt models of integrin activation. J Biol Chem.
2007;282:11914-11920.
228. Buensuceso C, de Virgilio M, Shattil SJ. Detection of
integrin
IIb
3
clustering in living cells. J Biol Chem.
2003;278:15217-15224.
229. Antl M, von Bruhl ML, Eiglsperger, C et al. IRAG medi-
ates NO/cGMP-dependent inhibition of platelet aggre-
gation and thrombus formation. Blood. 2007;109:
552-559.
230. Schlossmann J, Ammendola A, Ashman K, et al. Regula-
tion of intracellular calcium by a signalling complex of
IRAG, IP
3
receptor and cGMP kinase Ib. Nature. 2000;
404:197-201.
231. Ammendola A, Geiselhoringer A, Hofmann F, Schloss-
mann J. Molecular determinants of the interaction between
the inositol 1,4,5-trisphosphate receptorassociated
cGMP kinase substrate (IRAG) and cGMP kinase Ib. J
Biol Chem. 2001;276:24153-24159.
232. Butt E, Abel K, Krieger M, et al. cAMP- and cGMP-
dependent protein kinase phosphorylation sites of the
focal adhesion vasodilator-stimulated phosphoprotein
(VASP) in vitro and in intact human platelets. J Biol
Chem. 1994;269:14509-14517.
233. Lambrechts A, Kwiatkowski AV, Lanier LM, et al. cAMP-
dependent protein kinase phosphorylation of EVL, a
Mena/VASP relative, regulates its interaction with actin
and SH3 domains. J Biol Chem. 2000;275:36143-
36151.
234. Bachmann C, Fischer L, Walter U, Reinhard M. The
EVH2 domain of the vasodilator-stimulated phosphopro-
tein mediates tetramerization, F-actin binding, and actin
bundle formation. J Biol Chem. 1999;274:23549-23557.
235. Svitkina TM, Bulanova EA, Chaga OY, et al. Mechanism
of lopodia initiation by reorganization of a dendritic
network. J Cell Biol. 2003;160:409-421.
236. Mejillano MR, Kojima S, Applewhite DA, et al. Lamelli-
podial versus lopodial mode of the actin nanomachinery:
pivotal role of the lament barbed end. Cell. 2004;118:
363-373.
237. Barzik M, Kotova TI, Higgs HN, et al. Ena/VASP proteins
enhance actin polymerization in the presence of barbed
end capping proteins. J Biol Chem. 2005;280:
28653-28662.
238. Pula G, Schuh K, Nakayama K, et al. PKC regulates
collagen-induced platelet aggregation through inhibition
of VASP-mediated lopodia formation. Blood. 2006;108:
4035-4044.
239. Newman PJ. Switched at birth: a new family for PECAM-
1. J Clin Invest. 1999;103:5-9.
240. Newman PJ, Newman DK. Signal transduction pathways
mediated by PECAM-1. New roles for an old molecule
in platelet and vascular cell biology. Arterioscler Thromb
Vasc Biol. 2003;23:953-964.
241. Patil S, Newman DK, Newman PJ. Platelet endothelial
cell adhesion molecule-1 serves as an inhibitory receptor
that modulates platelet responses to collagen. Blood.
2001;97:1727-1732.
1398 HEMOSTASIS
242. Jones KL, Hughan SC, Dopheide SM, et al. Platelet
endothelial cell adhesion molecule-1 is a negative regula-
tor of platelet-collagen interactions. Blood. 2001;98:
1456-1463.
243. Rathore V, Stapleton MA, Hillery CA, et al. PECAM-1
negatively regulates GPIb/V/IX signaling in murine plate-
lets. Blood. 2003;102:3658-3664.
244. Falati S, Patil S, Gross PL, et al. Platelet PECAM-1
inhibits thrombus formation in vivo. Blood. 2006;107:
535-541.
245. Barrow AD, Astoul E, Floto A, et al. Cutting edge: TREM-
like transcript-1, a platelet immunoreceptor tyrosinebased
inhibition motif encoding costimulatory immunoreceptor
that enhances, rather than inhibits, calcium signaling via
SHP-2. J Immunol. 2004;172:5838-5842.
246. Ribas G, Neville M, Wixon JL, et al. Genes encoding three
new members of the leukocyte antigen 6 superfamily and
a novel member of Ig superfamily, together with genes
encoding the regulatory nuclear chloride ion channel
protein (hRNCC) and an N-N-dimethylarginine
dimethylaminohydrolase homologue, are found in a 30-kb
segment of the MHC class III region. J Immunol. 1999;
163:278-287.
247. de Vet EC, Aguado B, Campbell RD. G6b, a novel immu-
noglobulin superfamily member encoded in the human
major histocompatibility complex, interacts with SHP-1
and SHP-2. J Biol Chem. 2001;276:42070-42076.
248. Senis YA, Tomlinson MG, Garcia A, et al. A comprehen-
sive proteomics and genomics analysis reveals novel trans-
membrane proteins in human platelets and mouse
megakaryocytes including G6b-B, a novel immunorecep-
tor tyrosinebased inhibitory motif protein. Mol Cell Pro-
teomics. 2007;6:548-564.
249. Newland SA, Macaulay IC, Floto AR, et al. The novel
inhibitory receptor G6B is expressed on the surface of
platelets and attenuates platelet function in vitro. Blood.
2007;109:4806-4809.
250. Cantley LC. The phosphoinositide 3-kinase pathway.
Science. 2002;296:1655-1657.
251. Lioubin MN, Algate PA, Tsai S, et al. p150Ship, a signal
transduction molecule with inositol polyphosphate-5-
phosphatase activity. Genes Dev. 1996;10:1084-1095.
252. Damen JE, Liu L, Rosten P, et al. The 145-kDa protein
induced to associate with Shc by multiple cytokines is an
inositol tetraphosphate and phosphatidylinositol 3,4,5-tri-
phosphate 5-phosphatase. Proc Natl Acad Sci U S A.
1996;93:1689-1693.
253. Maxwell MJ, Yuan Y, Anderson KE, et al. SHIP1 and Lyn
kinase negatively regulate integrin
IIb
3
signaling in plate-
lets. J Biol Chem. 2004;279:32196-32204.
254. Gardai S, Whitlock BB, Helgason C, et al. Activation of
SHIP by NADPH oxidasestimulated Lyn leads to
enhanced apoptosis in neutrophils. J Biol Chem. 2002;
277:5236-5246.
255. Baran CP, Tridandapani S, Helgason CD, et al. The
inositol 5-phosphatase SHIP-1 and the Src kinase Lyn
negatively regulate macrophage colony-stimulating factor-
induced Akt activity. J Biol Chem. 2003;278:
38628-38636.
256. Phee H, Jacob A, Coggeshall KM. Enzymatic activity of
the Src homology 2 domaincontaining inositol phospha-
tase is regulated by a plasma membrane location. J Biol
Chem. 2000;275:19090-19097.
257. Quek LS, Pasquet JM, Hers I, et al. Fyn and Lyn phos-
phorylate the Fc receptor gamma chain downstream of
glycoprotein VI in murine platelets, and Lyn regulates a
novel feedback pathway. Blood. 2000;96:4246-4253.
258. Kandel ES, Hay N. The regulation and activities of the
multifunctional serine/threonine kinase Akt/PKB. Exp
Cell Res. 1999;253:210-229.
259. Scheid MP, Woodgett JR. PKB/AKT: functional insights
from genetic models. Nat Rev Mol Cell Biol. 2001;2:
760-768.
260. Kim L, Kimmel AR. GSK3 at the edge: regulation of
developmental specication and cell polarization. Curr
Drug Targets. 2006;7:1411-1419.
261. Barry FA, Graham GJ, Fry MJ, Gibbins JM. Regulation
of glycogen synthase kinase 3 in human platelets: a pos-
sible role in platelet function? FEBS Lett. 2003;553:
173-178.
262. Woulfe DS, August S, Li D. GSK3b is a negative regulator
of platelet function in vitro and in vivo [abstract]. Blood.
2006;108:395.
263. Mayadas TN, Johnson RC, Rayburn H, et al. Leukocyte
rolling and extravasation are severely compromised in P
selectindecient mice. Cell. 1993;74:541-554.
264. Frenette PS, Mayadas TN, Rayburn H, et al. Susceptibil-
ity to infection and altered hematopoiesis in mice de-
cient in both P- and E-selectins. Cell. 1996;84:563-574.
265. Diacovo TG, Roth SJ, Buccola JM, et al. Neutrophil
rolling, arrest, and transmigration across activated,
surface-adherent platelets via sequential action of P-selec-
tin and the
2
-integrin CD11b/CD18. Blood. 1996;88:
146-157.
266. Kuijper PH, Gallardo Torres HI, van der Linden JA, et al.
Platelet-dependent primary hemostasis promotes selec-
tin- and integrin-mediated neutrophil adhesion to
damaged endothelium under ow conditions. Blood.
1996;87:3271-3281.
267. Gawaz M, Langer H, May AE. Platelets in inammation
and atherogenesis. J Clin Invest. 2005;115:3378-3384.
268. Weber C, Springer TA. Neutrophil accumulation on acti-
vated, surface-adherent platelets in ow is mediated by
interaction of Mac-1 with brinogen bound to
IIb
3
and
stimulated by platelet-activating factor. J Clin Invest.
1997;100:2085-2093.
269. Santoso S, Sachs UJ, Kroll H, et al. The junctional adhe-
sion molecule 3 (JAM-3) on human platelets is a counter-
receptor for the leukocyte integrin Mac-1. J Exp Med.
2002;196:679-691.
270. Langer HF, Daub K, Braun G, et al. Platelets recruit
human dendritic cells via Mac-1/JAM-C interaction and
modulate dendritic cell function in vitro. Arterioscler
Thromb Vasc Biol. 2007;27:1463-1470.
271. von HP, Weber KS, Huo Y, et al. RANTES deposition by
platelets triggers monocyte arrest on inamed and athero-
sclerotic endothelium. Circulation. 2001;103:1772-
1777.
272. Huo Y, Ley KF. Role of platelets in the development of
atherosclerosis. Trends Cardiovasc Med. 2004;14:18-22.
273. Hawrylowicz CM, Santoro SA, Platt FM, Unanue ER.
Activated platelets express IL-1 activity. J Immunol.
1989;143:4015-4018.
274. Lindemann S, Tolley ND, Dixon DA, et al. Activated
platelets mediate inammatory signaling by regulated
interleukin 1b synthesis. J Cell Biol. 2001;154:485-490.
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Protein Structure WorksheetДокумент7 страницProtein Structure WorksheetkarendbrooksОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- April 28 FibrinolysisДокумент7 страницApril 28 FibrinolysisCzarina Mae IlaganОценок пока нет
- Sodium Dodecyl Sulfate Polyacrylamide Gel Electrophoresis IIДокумент36 страницSodium Dodecyl Sulfate Polyacrylamide Gel Electrophoresis IIYUEALVIN17Оценок пока нет
- Dintzis ExerciseДокумент5 страницDintzis ExerciserichschurОценок пока нет
- Actin Structure and FunctionДокумент20 страницActin Structure and FunctionMonoj BaruahОценок пока нет
- Chapter 2 - NotesДокумент22 страницыChapter 2 - NotesanusoumyaОценок пока нет
- Membrane Transport: To Accompany Biochemistry, 2/e by Reginald Garrett and Charles GrishamДокумент79 страницMembrane Transport: To Accompany Biochemistry, 2/e by Reginald Garrett and Charles GrishamMarione Thea RodriguezОценок пока нет
- nsb1200 1121Документ4 страницыnsb1200 1121Nicolas RuizОценок пока нет
- Transcription Factor - WikipediaДокумент112 страницTranscription Factor - WikipediaBaikuntha SabarОценок пока нет
- Actividad 1 Tema 1Документ2 страницыActividad 1 Tema 1David BravoОценок пока нет
- Master's in Advanced Cosmetic Sciences Protein Structure & PurificationДокумент71 страницаMaster's in Advanced Cosmetic Sciences Protein Structure & Purificationurooj ilyasОценок пока нет
- Simulation of Enzymes and InhibitionДокумент6 страницSimulation of Enzymes and InhibitionJohn OsborneОценок пока нет
- CollagenДокумент18 страницCollagenAhsan AliОценок пока нет
- Enzymology 1Документ18 страницEnzymology 1THE A plus ACADMYОценок пока нет
- Immune Regulation by GlucocorticoidsДокумент35 страницImmune Regulation by GlucocorticoidsSyifa SariОценок пока нет
- Role of Molecular Chaperones in Protein FoldingДокумент2 страницыRole of Molecular Chaperones in Protein FoldingSanele100% (1)
- Cell Physiology Revision QuestionsДокумент6 страницCell Physiology Revision QuestionsjoojoОценок пока нет
- Kegg No Interproscan Pfam: Anhydro-N-acetylmuramic Acid KinaseДокумент47 страницKegg No Interproscan Pfam: Anhydro-N-acetylmuramic Acid KinaseNikhil MohaneОценок пока нет
- Protein MicroarrayДокумент5 страницProtein Microarraysudhu sudsОценок пока нет
- Study Questions ENZYMДокумент2 страницыStudy Questions ENZYMEmad Qasim KhaleelОценок пока нет
- 001192187GS01Документ33 страницы001192187GS01radhoinezerellyОценок пока нет
- Problem Set 2 ProteinsДокумент4 страницыProblem Set 2 ProteinsJustine EscobalОценок пока нет
- ENZYMESДокумент18 страницENZYMESJennifer DesRochersОценок пока нет
- ZOO 103 Lecture 09 19 ProteinsДокумент12 страницZOO 103 Lecture 09 19 ProteinsKaelyn MontefalconОценок пока нет
- Proteins As Drug Targets: ReceptorsДокумент25 страницProteins As Drug Targets: ReceptorsAns JavidОценок пока нет
- Cytoskeleton 13.4.20Документ39 страницCytoskeleton 13.4.20NikhilОценок пока нет
- Protein Translation ProcessДокумент8 страницProtein Translation ProcessKempetsОценок пока нет
- Protein C DeficiencyДокумент6 страницProtein C DeficiencyDimas Rio BaltiОценок пока нет
- Translation in Prokaryotes: NEET 2020Документ1 страницаTranslation in Prokaryotes: NEET 2020ADIKKI ANOOHYAОценок пока нет
- 5.protein ClassificationДокумент41 страница5.protein ClassificationAhmad SobihОценок пока нет