Академический Документы
Профессиональный Документы
Культура Документы
12th Edition Brunner & Suddarth's Unit 15
Загружено:
colee5140%(1)0% нашли этот документ полезным (1 голос)
676 просмотров43 страницыunit 15 ch. 66-69
Оригинальное название
12th edition brunner & suddarth's unit 15
Авторское право
© © All Rights Reserved
Доступные форматы
DOC, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документunit 15 ch. 66-69
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
0%(1)0% нашли этот документ полезным (1 голос)
676 просмотров43 страницы12th Edition Brunner & Suddarth's Unit 15
Загружено:
colee514unit 15 ch. 66-69
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 43
Assessment of Musculoskeletal function
Anatomic and physiologic overview
The musculoskeletal system includes the bones, joints, muscles, tendons,
ligaments, and bursae of the body.
The bony structure provides protection for vital organs, including the brain, heart,
and lungs.
The bony skeleton provides a sturdy framework to support body structures.
The bone matrix stores calcium, phosphorus, magnesium and fluoride.
The red bone marrow located within bone cavities produces red and white blood
cells in a process called hematopoiesis.
Joints hold the bones together and allow the body to move.
The muscles attached to the skeleton contract, moving the bones and producing
heat, which helps to maintain body temperature.
tructure and function of the skeletal system
There are !"# bones in the human body, divided into four categories$
%ong bones &femur'
hort bones &metacarpals'
(lat bones &sternum'
)rregular bones &vertebrae'
*ones are constructed of cancellous &trabecular' or cortical &compact' bone
tissue.
+iaphysis , shaft of long bones
-piphysis , ends of long bones
-piphyseal plate , separates the epiphyses from the diaphysis and is the center
for longitudinal growth in children.
.artilage , tough,
elastic, avascular
tissue.
%ong bones , are
designed for weight
bearing and
movement.
hort bones ,
cancellous bone
covered by a layer of
compact bone.
(lat bones , important
sites for
hematopoiesis.
*one is composed of cells, protein matrix, and mineral deposits. The cells are of
three basic types$
/steoblasts , function in bone formation by secreting bone matrix.
/steocytes , mature bone cells.
/steoclasts , multinuclear cells involved in destroying, resorbing and
remolding bone.
/steon , microscopic functioning unit of mature cortical bone.
%amellae , minerali0ed bone matrix.
1eriosteum , dense, fibrous membrane covering the bone.
-ndosteum , thin, vascular membrane that covers the marrow cavity of long
bones and the spaces in cancellous bone.
*one marrow , vascular tissue located in the medullary cavity of long bones and
in flat bones. 2esponsible for producing red and white blood cells.
*one formation &osteogenesis'
/ssification , process by which the bone matrix is formed and hardening
materials are deposited on the collagen fibers.
Two basic process of ossification$
-ndochondral , a cartilage3like tissue &osteoid' is formed, resorbed, and
replaced by bone.
)ntramembranous , occurs when bone develops within membrane, as in
the bones of the face and skull.
*one maintenance
*one is a dynamic tissue in a constant state of turnover
+uring childhood bones grow 4 form by a process called modeling
-arly adulthood &early !"s' remodeling is the primary process5 remodeling
maintains bone structure 4 function through simultaneous resportion 4
osteogenesis5 complete skeletal turnover occurs 67" years
*alance between bone resoprtion 4 formation is8
o 1hysical activity
9eight bearing activity acts to stimulate bone formation 4
remodeling5 tend to be thick 4 strong
1pl who are unable to engage in regular weigh bearing have
increased resorption from calcium loss 4 their bones become
osteopenic 4 weak
o +ietary intake of certain nutrients esp. calcium
7"""3!""" mg calcium daily is essential in maintain adult bone
mass
7#3!: ounces of milk daily
o several hormones
calcitriol functions to increase the amt of calcium in the blood by
promoting absorption of calcium from the ;) tract5 also facilitates
minerali0ation of osteoid tissue
a deficiency of <it + results in bone minerali0ation deficit,
deformity, 4 fracture
1T= 4 calcitonin are major hormonal regulators of calcium
homeostasis5 1T= regulates the concentration of calcium in the
blood, in part by promoting mvmt of calcium from the bone5 low
calcium levels cause increased levels of 1T=>deminerali0ation of
bone> formation of bone cysts5 .alcitonin &secreted by thyroid due
to increase of calcium' inhibits bone resorption 4 increases
deposit of calcium in bone
thyroid hormone 4 cortisol , excessive thyroid hormone
production in adults &graves?' can result in increased bone
resorption 4 decreased bone formation5 increased levels of
cortisol have the same effects5 pts receiving long3term synthetic
cortisol or corticosteroids are at increased risk for steroid induced
osteopenia 4 fractures
growth hormone , has direct 4 indirect effects on skeletal growth
4 remodeling5 stimulates liver 4 to produce insulin like growth
factor37 &);(37' which accelerates bone modeling in children 4
adolescents5 ;= also directly stimulates skeletal growth in
children 4 adolescents &believed that low levels of of ;= 4 );(37
that occur w> aging may be responsible for decreased bone
formation 4 resultant osteopenia'
sex hormones
estrogen stimulates osteoblast 4 inhibits osteoclast
therefore bone formation is enhanced 4 resorption is
inhibited
testosterone directly causes skeletal growth in
adolescence 4 has continued effects on skeletal muscle
growth throughout the lifespan5 testosterone converts to
estrogen in adipose tissue providing an additional source
of bone preserving estrogen for men
bone remodeling &1%-A- 2-<)-9 )@ *//A <-2B
./@(C)@;'
2A@A% , receptor for activated nuclear factor kappa *
ligand binds to the receptor for activated nuclear factor
kappa * &2A@A' present on the cell membranes of
osteoclast precursors causing them to differentiate 4
mature into osteoclast which cause bone resorption
/steoblast may produce osteoprogerin &/1;' which
blocks the effects 2A@A% thereby turning off bone
resorption
*lood supply , with diminished bllod supply or hyperemia
&congestion', osteogensis 4 bone density decrease , bone
necrosis occurs when the bone is deprived of blood
*one healing
(racture healing occurs in four areas including$
*one marrow , endothelial cells rapidly differentiate into osteoblast
*one cortex , where new osteons are formed
1eriosteum , where hard callus &fibrous tissue ' is formed through
intramembranous ossification peripheral to the fracture5 where cartilage
is formed through endochondral ossification adjacent to the fracture site
-xternal soft tissue , where bridging callus forms that provides ability to
the fractured bones
D phases of fracture healing$
2eactive phase
There is a bleeding into the injured tissue and formation of a
fracture hematoma.
cytokines are released that initiate the fracture healing process by
causing proliferation of fibroblast 4 that cause angiogenesis to
occur &growth of new blood vessels'
granulation tissue begins to form w> in the clot 4 becomes dense
)nflammation, swelling, and pain are present.
2eparative phase
;ranulation tissue initially replaced w> callus precursor, procallus
(ibroblast invade the procallus 4 produce a denser type of callus
that is composed mostly of fibrocartilage
(ibrocartilaginous callus is replaced w> denser bony callus w> in
approx. D3: weeks post3injury
%amellar bone then forms as the bony callus calcifies months
post3injury
2emodeling
The final stage of fracture repair.
2emodeling is the new bone into its former structural
arrangement.
May take months to years depending on the extent of bone
modification needed, the function of the bone, 4 functional
stresses on the bone
.ancellous bone heals and remodels more rapidly than does
compact cortical bone.
serial x3rays are used to monitor the progress of bone healing
a. type of bone fracture, the ade6uacy of blood supply, the surface contact
of the fragments, the immobility of the fracture site, the age 4 general
health of the person influence the rate of fracture healing
b. ade6uate immobili0ation is essential until after there is x3ray evidence of
bone formation w> ossification
fractures treated w> open rigid compression plate fixation techni6ues, bony
fragments can be placed in direct contact
primary bone healing occurs through cortical bone &haversian' remodeling5 little
or no cartilaginous callus develops5 immature bone develops from the
endosteum5 intensive regeneration of new osteons &which develop the fracture
line by a process similar to normal bone maintainance
fracture strength is obtained when the new osteons have become established
tructure and function of the articular system
Joint &articulation' , the junction of two or more bones. Three basic kinds of
joints$
ynarthrosis , immovable joints
Amphiarthrosis , limited motion of joints
+iarthrosis , freely movable joints
Types of diarthrosis joints$
*all and socket joints , permit full freedom of movement
=inge joints , permit bending in one direction only
addle joints , allow movement in two planes at right angles to
each other
1ivot joints , permit rotation for such activities as turning a
doorknob
;liding joints , allow for limited movement in all directions
joint capsule , tough, fibrous sheath that surrounds the articulating bones.
ynovium , secretes the lubricating and shock absorbing synovial fluid into the
joint capsule.
%igaments , fibrous connective tissue bands that bind the articulating bones
together.
*ursa , a sac filled with synovial fluid that cushions the movement of tendons,
ligaments, and bones at a point of friction.
tructure and function of the skeletal muscle system
Tendons , cords of fibrous connective tissue that attach muscles to bones,
connective tissue, other muscles, soft tissue or skin.
(asciculi , parallel groups of muscle cells
(ascia , fibrous tissue encasing fasciculi
keletal muscle contraction
-ach muscle cell &also referred to as a muscle fiber' contains myofibrils.
arcomeres contain thick and thin actin filaments.
Muscle fibers contract in response to electrical stimulation delivered by an
effector nerve cell at the motor end plate. 9hen stimulated, the muscle cell
depolari0e and generates an action potential manner similar to that described for
nerve cells. These actions potentials propagate along the muscle cell membrane
and lead to the release of calcium ions that are stored in speciali0ed organelles
called arcoplasmic reticulum.
.alcium is rapidly removed from the sacromeres by active reaccumulation in the
sarcoplasmic reticulum. 9hen calcium concentration in the sacromere
decreases, the myosin and actin filaments cease to interact, and the sarcomere
returns to oits original resting length &relaxation'. Actin and myosin do not interact
in the absence of calcium.
The primary source of energy for the muscle cells is adenosine triphosphate
&AT1', which is generated through the cellular oxidative metabolism.
At low levels of activity &eg, sedentary activity', the skeletal muscle synthesi0es
AT1 from the oxidation of glucose to water and carbon dioxide. +uring strenuous
activity, when sufficient oxygen may not be available, glucose is metaboli0ed
primarily to lactic acid.
+uring isometric contraction, almost all of the energy is released in the form of
heat5 during isotonic contraction, some of the energy is expended in mechanical
work.
)n some situations, such as shivering because of cold, the need to generate heat
is the primary stimulus for muscle contraction.
Types of muscle contractions
)sometric contraction , the length of the muscles remain constant but the force
generated by the muscles are increased.
)sotonic contraction , shortening of the muscle with no increase in tension within
the muscle.
-x. +uring walking, isotonic contraction results in shortening of the leg and isometric
contraction causes the stiff leg to push against the floor.
Myoglobulin is a hemoglobin3like protein pigment present in striated muscle cells
that transports oxygen.
Muscles containing large 6uantities og myoglobulin &red muscles' have been
observed to contract slowly and powerfully &eg, respiratory and postural muscles'
Muscles containing little myoglobulin &white muscles' contract 6uickly &eg,
extraocular eye muscles'.
Muscle tone
Tone &tonus' , state of readiness
(laccid , muscle that is limp and without tone
pastic 3 muscle with greater3than3normal tone
Atonic , soft and flabby muscles
Muscle actions
ynergists , muscles assisting the prime mover
Antagonists , muscles causing movement opposite to that of the prime mover.
-xercise, disuse, and repair
Muscles need to be exercised to maintain function and strength.
=ypertrophy , increase in si0e of individual muscle fibers without an increase in
the number of muscle fibers.
Atrophy , decrease in the si0e of the muscle.
*ed rest and immobility cause loss of muscle mass and strength.
*ody movements produced by muscle contraction
(exion , bending at a joint &eg, elbow'
-xtension , straightening at a joint
Abduction , moving away from midline
Adduction , moving toward midline
2otation , turning around a specific axis &eg, shoulder joint'
.ircumduction , cone3like movement
upination , turning upward
1ronation , turning downward
)nversion , turning inward
-version , turning outward
1rotraction , pushing forward
2etraction , pulling backward
1hysical assessment$
1osture
The normal curvature of the spine is convex through the thoracic portion and
concave through the cervical and lumbar portions.
.ommon deformities of the spine include$
Ayphosis , increased forward curvature of the thoracic spine
%ordosis , or sway back, an exaggerated curvature of the lumbar spine
coliosis , lateral curving deviation of the spine
;ait
;ait is assessed by having the patient walk away from the examiner for a short
distance.
The examiner observes the patient?s gait for smoothness and rhythm.
Any unsteadiness or irregular movements are considered abnormal.
*one integrity
The bony skeleton is assessed for deformities and alignment.
ymmetric parts of the body are compared.
Joint function
The articular system is evaluated by noting the range of motion, deformity,
stability, and nodular formation.
2ange of motion is evaluated both actively and passively.
;oniometer , a protractor designed for evaluating joint motion.
Muscle strength and si0e
The muscular system is assessed by noting the patient?s ability to change
position, muscular strength and coordination, and the si0e of individual muscles.
kin
The nurse inspects the skin for edema, temperature, and color
@eurovascular tatus
1erform fre6uently b>c of risk for tissue 4 nerve damage
.ompartment syndrome , caused by pressure w>in a muscle compartment
that increases to such an extent that microcirculation diminishes leading to
nerve 4 muscle anoxia and necrosis5 function can be permanently lost if the
anoxic situation continues for longer than # hours
@erve Test of sensation Test of movement
1eroneal nerve 1rick the skin centered
between the great and
second toe
Ask the patient to dorsiflex
the ankle and extend the
toes.
Tibial nerve 1rick the medial and lateral
surface of the sole
Ask the patient to
plantarflex toes and ankle.
2adial nerve 1rick the skin centered
between the thumb and
second finger
Ask the patient to stretch
out the thumb, then the
wrist, and then the fingers
at the metacarpal joints.
Clnar nerve 1rick the fat pad at the top
of the small finger.
Ask the patient to spread all
fingers.
Median nerve 1rick the top or distal
surface of the index finger.
Ask the patient to touch the
thumb to the little finger.
Also observe whether the
patient can flex the wrist.
+iagnostic evaluation
)maging procedures
E3ray studies
*one x3rays determine bone density, texture, erosion, and changes in bone
relationships.
Multiple x3ray are needed for full assessment of the structure being
examined.
E3ray study of the cortex of the bone reveals any widening, narrowing, or
signs of irregularity.
Joint x3ray reveal fluid, irregularity, spur formation, narrowing, and changes in
the joint structure.
.omputed tomography
.T scan shows in detail a specific plane of involved bone and can reveal
tumors of the soft tissue or injuries to the ligaments or tendons.
)dentify the location and extent of fractures in areas that are difficult to
evaluate &eg, acetabulum'. .T studies, which may be performed with or
without the use of contrast agents, last about 7 hour.
Magnetic resonance imaging
Jewelry, hair clips, hearing aids, credit cards with magnetic strips, and other
metal3containing objects must be removed before the M2) is done5 otherwise
they can become dangerous projectile objects.
Arthrography
)s useful in identifying acute or chronic tears of the joint capsule or supporting
ligaments of the knee, shoulder, ankle, hip or wrist.
A radiopa6ue substance or air is injected into the joint cavity to outline soft
tissue structures and the contour of the joint.
*one densitometry
)s used to estimate bone mineral density &*M+'. This can be done through
the use of x3rays or ultrasound.
+ual3energy x3ray absorptiometry &+-EA' determines bone mineral density at
the wrist, hip or spine to estimate the extent of osteopososis and to monitor a
patient?s response to treatment for osteoporosis.
*one sonometry &ultrasound' measures heel bone 6uantity and 6uality and is
used to estimate *M+ and the risk of fracture for people with osteoporosis.
*one density sonography is a cost3effective, readily available screening tool
for disgnosing osteoporosis and predicting a person?s risk for fracture.
@ursing interventions $
*efore the patient undergoes an imaging study, the nurse should assess for
conditions that may re6uire special considerations during the study or that may
be contraindications to the study.
)t is essential that the patient remove all jewelry, hair clips, hearing aids, and
other metal before having an M2).
)f contrast agent will be used, the nurse should carefully assess the patient for
possible allergy.
*one scan
)s performed to detect metastatic and primary bone tumors, osteomyelitis,
certain faractures, and aseptic necrosis.
@ursing interventions $
*efore a bone scan, the nurse should ask about possible allergy to radioisotope.
Assess for any condition that would contraindicate performing the procedure.
-ncourage the patient to drink plenty of fluids.
Ask the patient to empty the bladder before the procedure.
Arthroscopy
)s a procedure that allows direct visuali0ation of a joint to diagnose joint
disorders.
The procedure is carried out in the operating room under sterile conditions5
injection of a local anesthetic into the joint or general anesthesia is used.
A large3bore needle is inserted, and the joint is distended with saline.
The arthroscope is introduced, and joint structures, synovium and articular
surfaces are visuali0ed.
After the procedure, the puncture wound is closed with adhesive strips or
sutures and covered with a sterile dressing.
@ursing interventions$
9rap the joint with a compression dressing to control swelling.
Apply ice to control edema.
-xtend and elevate the joint.
-xplain to the patient and family the symptoms to watch for to determine
occurrence of complications.
Arthrocentesis
&joint aspiration' is carried out to obtain synovial fluid for purposes of
examination or to relieve pain due to effusion.
-lectromyography
1rovides information about the electrical potential of the muscles and the
nerves leading to them.
*iopsy
May be performed to determine the structure and composition of bone
marrow, bone, muscle or synovium to help siagnose specific disease.
The nurse monitors the biopsy site for edema, bleeding and edema.
Analgesics are administered as prescribed for comfort.
%aboratory studies
*lood and urine
o .*., hemoglobin level, 9*.
*efore surgery, coagulation studies are performed to detect bleeding tendencies.
erum calcium level
erum phosphorus level
Acid phosphatase is elevated in 1aget?s disease and metastatic cancer.
Alkaline phosphatase is elevated during early fracture healing and in disease with
increased osteoblastic activity &eg, metastatic bone tumors'
*one metabolism may be evaluated through thyroid studies and determination of
calcitonin, parathyroid hormone and vitamin + levels
erum en0ymes
Aldolase is elevated in muscle disease &eg, muscular dystrophy, skeletal muscle
necrosis'
erumosteocalcin &bone ;%A protein' indicates the rate of bones turnover.
Musculoskeletal ystem
Action taken as a result of nervous system stimulation is largely the function of
the musculoskeletal system.
This system enables the human organism to move the glands and organs to
function.
)t carries out the direction of the nervous and endocrine system.
MC.%-
carry out movements of the body. D Types$
7. M//T=
This type of muscle is also called visceral, plain and involuntary muscles.
This muscle is present as sheets in the walls of the blood vessels, the
gastrointestinal tract, urinary bladder, ducts of the reproductive system,
ureters, respiratory passages, lymphatic vessels, capsule of the spleen,
around hair follicles, within connective tissue of the skin and within the
eyeball.
)t is not under voluntary control.
!. .A2+)A. MC.%-
This type of muscle is also called striated involuntary or heart muscle.
)t beats spontaneously and in rhythm.
D. A-%-TA% MC.%-
This type of muscle is striated voluntary and attached to bones.
)t is composed of parallel bundles of fibers which are the units of histological
organi0ation.
keletal muscles are attached to the skeleton and permit movements.
The are excitable and capable of contraction or extension.
Arrangement of the skeleton is usually in antagonistic pairs so that one
muscle is extended while the other contracts. After a force that has been
applied to a muscle is released, the muscle will return to its normal length
because of the characteristics of elasticity. The muscles are attached to the
bones at points of insertion by strong fibrous tendons. -ach muscle also has
a point of origin, which is usually more fixed than the point of insertion.
Muscle contraction is initiated by a nerve impulse that reaches the muscle
fiber at the myoneural junction. The nerves are located in the middle of the
fiber so that the impulse spread out toward both ends, allowing for more
coincident contraction of all sacromeres. -nergy for contraction is supplied by
the breakdown of AT1. /xygen and glucose are also needed for this
reaction.
keletal muscles are divided according to the following$
7. According to location
a. )ntercostal , muscle between ribs
b. (emoris , muscle in the femur
c. *rachii , muscle in the arm
!. According to direction of fibers
a. 2ectus , straight
b. Transverse , across
c. /bli6ue , obli6ue, diagonal
D. According to the type of action performed
a. Abductor , muscle which move limb &or other part' away from the midline
of body.
b. (lexor , muscle which bend a limb at a joint
c. %evator , muscle which lift a part eg, eyelid
d. -xtensor , muscle which straighten a limb at a joint
e. Adductor , muscle which move a limb &or other part' towards the midline.
:. According to the shape or si0e
a. +eltoid , from greek letter FdeltaG
b. Trape0ius , four3sided
c. Maximus , largest
d. %ongus , longest
e. Minimus , smallest
f. *revis , short
g. (usiform , spindle shaped
h. 2homboid , 6uadrilateral
H. According to the number of the heads or origin
a. *iceps , muscle with ! heads
b. Triceps , muscle with D heads
c. Iuadriceps , muscle with : heads
A skeletal muscle has D parts namely$
7. /rigin, the end which is the more fixed point of attachment
!. )nsertion, the end which is freely movable.
D. *ody or *elly, the portion between the origin and insertion.
Attachment of skeletal muscle may either be tendons or fasciae.
7. Tendons attach muscle to bone. *road sheats of tendons are termed
aponeurosis.
!. (asciae &singular fascia' are tough fibrous connective tissues which separate
muscles from one another and hold them in position.
Muscles are also named according to movement
7. 1rime mover or agonist muscle which execute actual movement e.g., the
biceps in flexion of elbow
!. Antagonist muscle that acts against the prime mover, e.g., the triceps in flexion
D. ynergist muscle that enables prime mover e.g., perform the action efficiently
and smoothly.
:. (ixator muscle which studies the bone giving origin to the prime mover so that
the insertion will move.
A-%-T/@
The bone consist of cells, fibers and ground substances.
)t is calcified, making it hard substance suited for supportive and protective
functions.
*one tissue is nourished by the haversian system. i.e., a network of minute
canals traversed with blood vessels.
*one tissue is constantly crerated and reabsorbed.
These ! processes$ i.e., bone creation &deposition' by osteoblasts and bone
reabsorption, determine skeletal bone si0e and strength.
). A-%-TA% (C@.T)/@
7. 1rovides attachment of muscles, tendons and ligaments
!. 1rotects delicate: organs of the body &e.g., brain, heart, lungs and other soft
tissue'
D. tores minerals salts, e.g., calcium, phosphorous and release them whenever
necessary.
:. -ncloses bone marrow which is responsible for production of blood corpuscles.
H. Assists with movement by providing leverage and attachment for muscles.
)). */@- =)T/%/;B
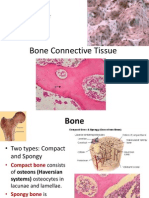
=istologically, bones consist of ! types
7. .ompact bone i.e., strong and dense with closely spaced lamellae &concentric
layers of mineral depositions'.
!. .ancellous i.e., spongy appearance with more widely spaced lamellae.
*etween layers of lamellae are small cavities called lacunae. uspended in tisuue
fluid within each lacuna is an osteocyte &mature bone forming cells'. Tiny canals
&canaliculi' connects the lacunae and hence the osteocytes.
2ed bone marrow has a hematopoietic function &manufactures red and white blood
cells' and is located in cancellous bone spaces.
Bellow marrow occurs in the shaft of long bones and extends into the haversian
systems. Bellow marrow is connective tissue composed of fat cells. *lood supply to
bone comes$
&a' via arterioles through the haversian canals,
&b' via vessels in the periosteum that center bone through the minute <olkmann5s
.anals,
&c' via blood vessels in the marrow and bone ends.
*one is supplied with a network of sensory nerves.
))). */@- .%A)().AT)/@ A../2+)@; T/ =A1-
7. %ong bones , consist of epiphysis, articular cartilage, diaphysis, periosteum and
medullary cavity. This type is found in the extremities and as levers.
-xample$ humerus, radius, fibula
-1)1=B) , -nd of long bones and is composed of cancellous bone.
A2T).C%A2 .A2T)%A;- , .overs long bone ends and provides smooth
surfaces for joint movement.
+)A1=B) , Main shaft of a long bone and is composed of compact
bone. )t provides structural support.
M-TA1=B) , (lared port of a long bone between the epiphysis and
diaphysis.
M-+C%%A2B .A<)TB &MA22/9' , )s in the center of the diaphysis.
!. hort bones , consist of cancellous bone covered by a thin layer of compact
tissue. These type of bones are cube3shaped and provide strength.
-xample$ carapls, tarsals, palanches
D. (lat bones , consist of cancellous bone encased in two flat plates of compact
bone. These bones protect delicate organs.
-xample , skull, scapula, ribs, sternum
:. )rregular bones , are bones of no definite shape. The thinner part consist of two
plates of compact bone with cancellous bone between them while the bulky part
consist of cancellous bone surrounded by a layer of compact bone.
-xample$ skull and vertebrae
H. esamoid bones , are rounded, bones which develop in the capsules of joints or
in tendons. The function of this bone is to eliminate friction and increase leverage
of muscle.
-xample$ patella, knee cap
)<. +)<))/@ /( =CMA@ A-%-T/@
- There are a total of !"# bones in the human body. The skeleton has been
divided into axial and appendicular skeleton.
A. AXIAL SKELETON
- The axial skeleton comprises the bones of the vertebral column, thorax
and skull. )t has a total of J" bones$ !K bones of the skull &J cranial, 7:
bones of the face, # bones of the middle ears and 7 hyoid bone'$ !#
bones of the thorax &sternum and ribs'
AC%% */@-
- The skull includes the cranial and facial bones joined together by the
mandible &lower jaw'. There is a total of !K skull bones.
7.' .ranial bones
a. (rontal bone3 forms the forehead, roof of the nasal cavity and the orbits
b. 1arietal bone , forms the sides and roof of the cranium and are joined at
the sagittal suture in the midline
c. /ccipital bone , forms the back and base of the cranium and joints the
parietal bone anteriorly at the lambdoid through which the spinal cord
joints the medulla oblongata of the brain.
d. Temporal bone , helps to form the sides and base of the cranium.
e. pheroid bone , forms the anterior portion of the base of the cranium.
f. -thmoid bone , principal supporting structure of the nasal cavity and
contributes to the formation of the orbits.
Structure between Cranial bones
Sutures , the articulation between the cranial bones.
a. coronal suture between the frontal and parietal bones
b. lambdoid suture between parietal bones and occipital bones
c. s6uamous suture between part of the temporal and parietal
d. sagittal suture units parietal bones.
Fontanels are soft boneless areas in the skull which are later closed up by the formation
of cranial bones, occurring at birth. There are usually # fontanels, namely$
a. Anterior or bregmatic fontanel the largest and diamond shape located at
junctions of the coronal, sagittal and frontal sutures which closes at the middle of
the second year of life at 7J
th
months stage.
b. 1osterior fontanel , triangular in shape, located at the union of sagittal and
lambdoid sutures. .loses one month after birth.
c. Anterol lateral and posterolateral , on each side of the skull5 normally closed a
month or two after birth.
!.' kull bones
- the facial bones consist of 7 mandible 7 vomer, ! maxillary, ! xygomatic.
! nasal, ! lacrimal, ! inferior nasal conchae and ! palatine.
a. Mandile , the strongest and the longest bone of the face. )t is the bone of
the lower jaw.
b. Maxilla , the upper jaw is formed by the fusion of two maxillae which
articulate with the frontal bone.
c. @asal bone , paired nasal bones join to form the bridge of the nose.
d. 1alatine bone , two bones forming the posterior of the roof of the mouth
or hard palate.
e. Lygomatic bone , the two bones forming the prominence of the cheek
called malar bones and rest upon the maxillae articulating with their
0ygomatic processes.
f. %acrimal bone , the paired bone make up part of the orbit at the inner
angle of the eye.
g. @asal .onchae or )nferior Turbinae bones , lies immediately below each
nostril on the lateral side.
h. <omer , constitutes the lower posterior portion of the nasal septum.
D.' *ones of the middle ear
- A chain of three small bones extends acroos the middle ear. These are
the smallest bones of the body known as the ear ossicles.
a. =ammer or malleus
b. Anvil or )ncus
c. tirrup or stapes
:.' =yoid bone
<-2T-*2A% ./%CM@
- The vertebral column or backbone extends the full length of the back. The
vertebrae are grouped based on their location , cervical, 7! thoracic, H
lumbar and 7 coccyx.
7. .ervical vertebrae , smallest vertebrae, having oblong bodies which are
broader from side to side.
!. Thoracic <ertebrae , their bodies are no longer and more rounded than
those of the cervical region.
D. %umbar <ertebrae , largest and strongest of all vertebrae.
:. acrum , lies below the H
th
lumbar vertebrae and is triangular in shape.
H. .occyx , is formed by the fusion of four rudimentary coccygeal vertebrae
or segments and is attached to the tip of the s acrum.
T=/2AE
- The thorax encloses and protects the lungs and other structures of the
chest cavity. )t provides support for the bones of the shoulder girdle and
upper extremities. 2ed blood corpuscles are formed in the red bone
marrow of the ribs and sternum.
7.' ternum , lies in the midline of the thorax in front.
!.' 2ibs , are long slender and curved bones attached to the thoracic
vertebrae.
a. True ribs , first M pairs are attached to the sternum
b. (alse ribs , the J
th
, K
th
, and 7"
th
pairs and are attached to the M
th
ribs by
the costal cartilage.
c. (ree or floating ribs , last ! pairs and are attached in front.
- The spaces between the ribs are called intercostals spaces and are filled
with muscle.
*. A11-@+).C%A2 A-%-T/@
- The appendicular skeleton is composed of bones of the upper and lower
extremities including the shoulder and pelvic girdles.
. !ones o" the #pper E$tre%it&
a. houlder girdle , this is made of clavicle and scapula on each side of the
body. )t serves to attach the bones of the upper extremities to the axial
division of the skeleton and provides places for muscle attachments.
7.' .lavicle , known as the collar bone located at the root of the neck and
anterior to the first rib.
!.' capula , a large flat triangular bone located on the dorsal portion of the
thorax covering the area from the !
nd
rib to the M
th
rib. )t serves as the
origin for some muscles that move the arm.
b. =umerus , long bone of the upper arm
c. 2adium , lies on the lateral thumb side of the forearm
d. Clna , lies on the medial side of the forearm
e. .arpals , there are J in each extremity
f. Metacarpals , the palm of the hand consist of H metacarpal bones, each
with a base, shaft and head.
'. !ones o" the Lower E$tre%it&
a. 1elvic ;irdle , supports the trunk and provides attachment for the legs. )t is made
up of hip bone or os coxae on each side of the body. This is the broadest bone of
the body.
)lium , uppermost and largest portion of the pelvic bone
)schium , lowest and strongest portion of the pelvic bone
1ubic , lies superior and slightly anterior to the ischium. *etween the pubis and
the ischium is an obturator foramen.
b. (emur , form the bone of the thigh. )t is the heartiest, largest and strongest bone
in the body. )t transmits the entire weight of the trunk from the hip to the tibia.
c. 1atella or knee cap , largest seasamoid bone in the body and is embedded in the
tendon of the 6uadriceps femoris. )t is movable and serves to increase leverage of
muscles that straighten the knee.
d. !ones o" the le(
Tibia , medial and larger bone of the leg also known as skin bone
(ibula , a long, slender bone on the lateral side of the leg.
e. !ones o" the "oot
Tarsal bone , M in each foot are arranged in the hindfoot and forefoot.
Metatarsals , bases of the inner three five metatarsals articular with the D
cuneiform bones and those of the outer teo warticulates with the cuboid.
1halanges , there are 7: in each foot, ! of which are in the great toes and D in
each of the other toes.
+)A;@/T). A-M-@T
. )adiolo(ic Studies
a. 2oentgenograms &E3ray films' to establish presence of musculo3skeletal
problems, follow its progress and evaluate treatment effectiveness.
1lain E3ray film is common , usually from antero3posterior &A1'
and>or lateral view.
b. Arthrography , injection of a dye or air in the joint for x3ray study
c. Myelography , examines the spinal cord after introduction of the contrast
medium.
d. .T can , useful is assessing some bone and soft tissue tumors and
some spinal fractures.
'. !lood Studies
a. -2 , non3specific test for inflammation
b. Cric Acid , usually elevated in gout
c. Antinuclear antibody , assess presence of antibodies capable of
destroying cell nuclei.
- positive in about K:N of clients with %-
d. Anti +@A , detects serum antibodies that react with +@A
- most specific test for %-
e. Test of Mineral Metabolism
.alcium , decreased levels found in osteomalacia, hypoparathyroidism.
- increased levels found in bone tumors, acute osteoporosis,
hyperparathyroidism.
1hosphorus , increased levels found in healing fractures, chronic
renal disease.
f. Muscle -n0yme tests
.reatine 1hosphorus , highest concentration found in skeletal
muscle.
3 increased levels found in traumatic injuries, progressive muscular
dystrophy
Adolase , useful in monitoring muscular dystrophy and
dermatomyositis
D. Arthroscop& , direct visuali0ation of a joint usong an arthroscope after injection of
local anesthesia.
:. Arthrocentesis , method of aspirating synovial fluid, blood or pus via a needle
inserted into the joint cavity.
H. E*+ , Electro%&elo(raph& , non3invasive test that graphically records the
electrical activity of the muscle at rest and during contraction.
#. !one scannin( , radio isotope that are Ftaken upG by bones are injected
intravenous &usually @a pertechnetae KK MTc'.
Musculoskeletal care modalities
Managing care of the patient in a cast
.ast
)s a rigid external immobili0ing device that is molded to the contours of the body.
)ts purposes are to immobili0e a body part in a specific position and apply
uniform pressure on encased soft tissue.
A cast is used specifically to$
)mmobili0ed a reduced fracture
.orrect a deformity
Apply uniform pressure to underlying soft tissue
upport and stabili0e weakened joints.
;enerally, casts permit mobili0ation of the patient while restricting movements of
a body part.
Types of .ast
7.' T2C@A
.ollar cast affectations of the cervical spine
Minerva .ast , affectations of the upper dorsal and cervical spine
Trauma
1/tt?s disease
coliosis
2i00ers Jacket .ast , scoliosis
1laster hell , surgeries involving the spine
*ody cast , affectations of the lower dorso , lumbar spine
houlder apica , affectations on shoulder joint, upper portion of the humerus
/bservations of 1ateints with .ast involving the trunk
7. igns or respiratory distress
!. igns of cast syndrome
1rolonged nausea and vomiting
2epeated vomiting
Abdominal distention
<ague abdominal pain
Absence of bowel sound
D. 1ressure on the chin, jaw, ear, face, axilla, clavicular area, anterior3
superior iliac crest, groin, buttocks
:. Crinary and bowel disturbance
H. igns of 1laster ore
)tchiness and burning sensation
evere pain
2ise of temperature
+isturbed sleep
2estlessness
/ffensive odor
+ischarge on case
!.' C@+-2 -ET2-M)TB , .)2.C%A2 .AT
a. hort Arm circular cast , affections of the wrist and fingers
b. %ong Arm .ircular .ast , affections on the forearm
c. =anging .ast , fracture of radius , ulnar with callus
D.' %/9-2 -ET2-M)TB , .)2.C%A2 .AT
a. hort leg circular cast &boot cast' , affections of ankle and toes
b. 9alking .ast , affections of the ankle with callus formation
c. 1T* 1atellar Tendon *earing .ast , fracture of the tibia , fibula with callus
d. %ong %eg .ircular .ast , fracture of tibia , fibula
e. Iuadrilateral .ast , fracture of the shaft femur with good callus formation
f. .ylinder .ast , fracture of patella
/*-2<AT)/@ /@ 1AT)-@T? .AT-+ -ET2-M)TB
7. igns of impaired circulation on toes and fingers
a. color3 cyanosis of the skin
b. temperature , coldness of the skin
c. movement , loss of function
d. sensation , numbness
e. pulsation , pulselessness in extremity
f. severe pain
g. marked swelling
!. @erve damage due to pressure in a nerve as it passes over body prominence.
a. increasing pain, persistent and locali0ed
b. numbness
c. feeling of deep pressure
d. paresthesias
e. motor weakness or paralysis
D. )nfection, tissue necrosis due to skin breakdown
a. unpleasant odor over the cast or at edges of cast
b. drainage through cast
c. sudden unexplained fever
d. hot spot on cast over lesion
:. 1ressure on axilla, elbow, wrist, metacarpals, iliac crest, groin, knee, ankle and
metatarsals.
;C)+-%)@- (/2 *)<A%<)@; A .AT
9hen cutting a cast in half &bivalving', the physician or nurse practitioner
proceeds as follows$
7. 9ith a cast cutter, a longitudinal cut is made to divide the cast in half.
!. The underpadding is cut with scissors.
D. The cast is spread apart with a cast spreaders to relieve pressure and to inspect
and treat the skin without interrupting the reduction and alignment of the bone.
:. After the pressure is relieved, the anterior and posterior parts of the cast are
secured together with an elastic compression bandage to maintain immobili0ation.
H. to control swelling and promote circulation, the extremity is elevated &but no higher
than heart level, to minimi0e the affect of gravity on perfusion of the tissue'.
:.' 1).A TB1-
ingle spica , affections of the hip and femur
7 4 O hip spica
+ouble hip spica
(rog .ast , congenital hip dislocation
1anatalon .ase , fracture of the pelvis
/bservations on patients in spica type
7. igns of respiratory distress
!. igns of cast syndrome
D. igns of impaired circulation on toes
:. signs of urinary , bowel disturbance
H. signs of infection , tissue necrosis
#. pressure around edge of cast below nipple axillary, iliac crest, buttocks, sacral,
groin, knee and metatarsals.
.asting materials
@on plaster
2eferred to as fiberglass casts, these water3activated polyurethane materials
have the versatility of plaster but are lighter in weight, stronger, water resistant,
and durable.
They are used for non displaced fractures with minimal swelling and for long
term wear.
1laster
The traditional cast is made of plaster. 2olls of plaster bandage are wet in cool
water and applied smoothly to the body.
A crystalli0ing reaction occurs, and heat is given off.
1%)@T /2 1/T-2)/2 M/%+
). C11-2 -ET2-M)TB
a. hort arm posterior mold , affections of the wrist and infection, open wounds
b. %ong arm, posterior mold , infections of the forearm, open wounds
c. ugar tong , affections of the shoulder, upper portion of humerus with infections,
open wounds.
d. Abduction plint , fracture of the neck of humerus
e. .ock3up3splint , fracture of the neck of humerus
f. *anjo splint , brachial nerve paralysis
g. +ennis *rowne splint , congenital clubfoot
)). %/9-2 -ET2-M)TB
a. hort leg posterior mold , affections of the ankle and toes with infections, open
wounds.
b. %ong leg posterior mold , affections of the knees, tibia , fibula with infections,
open wounds
c. @ight splint , post polio with residual paralysis of lower extremity
d. pica Mold , affections of the hip, femur3like septic hip, osteomyelitis
@/T-$ /bservations same as in a circular type of cast for upper and lower extremity.
*2A.-
Types$
a. Milwaukee brace , scoliosis
b. Taylor body brace , 1otts disease on thoracic vertebrae
c. Jawet brace , compression fracture of vertebral body
d. hant0 collar , cervical spine affection
e. /M) , sterno occipito madibular immobili0er , cervical spine affection
f. (orester , cervico thoraco3lumbar affections
g. .hair back , dorso3lumbar affections
T2A.T)/@
is an act pulling and drawing which is associated with counter traction.
1C21/->)@+).AT)/@
(or immobili0ation
To prevent and correct deformity
To maintain good alignment
To give support to reduce pain and muscle spasm
To reduce fracture
12)@.)1%- /( T2A.T)/@
7. Aeep body alignment at normal , position the client in dorsal recumbent
!. (or every traction, there is always a counter traction
use shock blocks
use half ring Thomas splint
D. (or traction to be effective, it must be applied continuously
:. The line of pull must be in line with deformity
H. (riction should be eliminated
9eights should be hanging freely
2ope of sash cord runs freely along the pulley
Anots should be away from the pulley
9eights should not be resting on the floor
/bserve the rope and bag weights for signs of wear and tear.
TB1- /( T2A.T)/@ according to manner of application
7. Manual Traction , traction applied to the body by the hand of operator
!. kin Traction , traction applied at the surface of the skin and soft tissue and
indirectly to the bone using adhesive elastic bandage and spreader
E$a%ples$ *ryant Traction, 2ussell Traction
D. keletal Traction , traction applied directly to the bone using pin, wires, tongs
-xample$ =alo pelvic traction, .rutchfiels tong traction
:. (illed or adjustable traction , traction applied to the body using devices like
canvass, laces, buckles, leathers used according to the side of the patient.
E$a%ples$ Anklet Traction
1elvic trap Traction
=ead =alter Traction
@C2)@; +)A;@/) (/2 .%)-@T )@ T2A.T)/@
7. 1otential for immobility related to therapy
3 provide for active motion of the unaffected joints
3 deep breathing , coughing exercise
!. 1otential for neurovascular compromise related to traction
D. 1otential for skin breakdown related to pressure on soft tissues.
:. 1otential for complication like
)nfection at the pin>wire site , inspect insertion sites carefully every shift, cleanse
sites with saline, peroxide or betadine, use antibiotic ointments and dry sterile
dressing if ordered.
1neumonia, atelectasis
.ontractures
.onstipation
*edstore
H. 1otential for boredorm
#. ocial isolation
M. 1artial self3care deficit
.ommon musculoskeletal problems$
Acute lower back pain
Acute low back pain refers to patients who have a problem with their back that
occurred within hours to 7 month.
)s the recent onset of back pain in the lumbar region.
1ain in this area can derive from any of the regionPs structures, including the
spinal bones, the discs between the vertebrae, the ligaments around the spine,
the spinal cord and nerves, muscles of the low back, internal organs of the pelvis
and abdomen, and the skin covering the lumbar area.
*ack pain is classified into three categories based on the duration of symptoms $
Acute back pain is arbitrarily defined as pain that has been present for six weeks
or less.
ubacute back pain has a six3 to 7!3week duration.
.hronic back pain lasts longer than 7! weeks.
.linical manifestations$
.ondition$ .linical clues$
@onspecific back pain &mechanical
back pain, facet joint pain,
osteoarthritis, muscle sprains,
spasms'
@o nerve root compromise,
locali0ed pain over lumbosacral
area
ciatica &herniated disc' *ack3related lower extremity
symptoms and spasm in radicular
pattern, positive straight leg raising
test
pine fracture &compression
fracture'
=istory of trauma, osteoporosis,
locali0ed pain over spine
pondylolysis Affects young athletes
&gymnastics, football, weight
lifting'5 pain with spine extension5
obli6ue radiographs show defect of
pars interarticularis
Malignant disease &multiple
myeloma', metastatic disease
Cnexplained weight loss, fever,
abnormal serum protein
electrophoresis pattern, history of
malignant disease
.onnective tissue disease
&systemic lupus erythematosus'
(ever, increased erythrocyte
sedimentation rate, positive for
antinuclear antibodies,
scleroderma, rheumatoid arthritis
)nfection &disc space, spinal
tuberculosis'
(ever, parenteral drug abuse,
history of tuberculosis or positive
tuberculin test
Abdominal aortic aneurysm )nability to find position of comfort,
back pain not relieved by rest,
pulsatile mass in abdomen
.auda e6uina syndrome &spinal
stenosis'
Crinary retention, bladder or bowel
incontinence, saddle anesthesia,
severe and progressive weakness
of lower extremities
=yperparathyroidism )nsidious, associated with
hypercalcemia, renal stones,
constipation
Ankylosing spondylitis &morning
stiffness'
ostly men in their early !"s,
positive for =%A3*!M antigen,
positive family history, increased
erythrocyte sedimentation rate
.ommon problems of the upper extremity$
*ursitis
9hether youPre at work or at play, if you overuse or repetitively stress your bodyPs
joints, you may eventually develop a painful inflammation called bursitis.
Bou have more than 7H" bursae in your body. These small, fluid3filled sacs
lubricate and cushion pressure points between your bones and the tendons and
muscles near your joints. They help your joints move with ease.
*ursitis occurs when a bursa becomes inflamed. 9hen inflammation occurs,
movement or pressure is painful.
*ursitis often affects the joints in your shoulders, elbows or hips. *ut you can
also have bursitis by your knee, heel and the base of your big toe.
*ursitis pain usually goes away within a few weeks or so with proper treatment,
but recurrent flare3ups of bursitis are common.
igns and symptoms
)f you have bursitis, you may notice$
A dull ache or stiffness in the area around your elbow, hip, knee, shoulder, big
toe or other joints
A worsening of pain with movement or pressure
An area that feels swollen or warm to the touch
/ccasional skin redness in the area of the inflamed bursa
Tendinitis
Tendinitis is inflammation or irritation of a tendon Q any one of the thick fibrous
cords that attach muscles to bones.
The condition, which causes pain and tenderness just outside a joint, can occur
in any of your bodyPs tendons.
Tendinitis is common around your shoulders, elbows, wrists and heels.
igns and ymptoms
Tendinitis that is produced near a joint aggravated by movement include the following$
1ain
Tenderness
Mild swelling, in some cases
Tendinitis in various locations in your body produces these specific types of pain$
Tennis elbow. This type causes pain on the outer side of your forearm near your
elbow when you rotate your forearm or grip an object. ;olferPs elbow causes pain
on the inner part of your elbow.
Achilles tendinitis. This form causes pain just above your heel.
Adductor tendinitis. This type leads to pain in your groin.
1atellar tendinitis. )n this type, you experience pain just below your kneecap.
2otator cuff tendinitis. This tendinitis leads to shoulder pain.
.arpal tunnel syndrome
*ounded by bones and ligaments, the carpal tunnel is a narrow passageway Q
about as big around as your thumb Q located on the palm side of your wrist.
This tunnel protects a main nerve to your hand and nine tendons that bend your
fingers.
1ressure placed on the nerve produces the numbness, pain and, eventually,
hand weakness that characteri0e carpal tunnel syndrome.
igns and symptoms
.arpal tunnel syndrome typically starts gradually with a vague aching in your
wrist that can extend to your hand or forearm. /ther common carpal tunnel
syndrome symptoms include$
Tingling or numbness in your fingers or hand, especially your thumb, index,
middle or ring fingers, but not your little finger. This sensation often occurs
while driving a vehicle or holding a phone or a newspaper or upon
awakening. Many people Rshake outR their hands to relieve their symptoms.
1ain radiating or extending from your wrist up your arm to your shoulder or
down into your palm or fingers, especially after forceful or repetitive use. This
usually occurs on palm side of your forearm.
A sense of weakness in your hands and a tendency to drop objects.
A constant loss of feeling in some fingers. This can occur if the condition is
advanced.
;anglion cysts
;anglion cysts are noncancerous fluid3filled lumps &cysts' that most commonly
develop along the tendons or joints of your wrists or hands.
They may also appear in your feet.
;anglion cysts may develop suddenly or progress gradually.
They occur when the lubricating fluid in your joints or around the nearby tendons
accumulates, giving rise to a cyst.
The exact cause of this process is unknown.
igns and symptoms
)n most cases, ganglion cysts appear as raised lumps near your wrist or finger
joints.
They are generally round, firm and smooth.
Though they are fixed in one place, they may RgiveR a little when you push
against them.
+upuytrenPs contracture
+upuytrenPs contracture is a rare hand deformity in which the connective tissue
&fascia' under the skin of the palm thickens and scars.
Anots &nodes' and cords of tissue form under the skin, often pulling one or more
of the fingers into a bent &contracted' position.
Though the fingers affected by +upuytrenPs contracture bend normally, they canPt
be straightened, making it difficult to use your hand.
igns and symptoms
+upuytrenPs contracture usually begins as a thickening of the skin on the palm of
your hand. As +upuytrenPs contracture progresses, the skin on the palm of your
hand may appear dimpled.
A firm lump of tissue may form on your palm. This lump may be sensitive to the
touch, but usually isnPt painful.
)n later stages of +upuytrenPs contracture, cords of tissue form under the skin on
your palm. .ords may extend up to your fingers. As these cords tighten, your
fingers may be pulled toward your palm, sometimes severely.
The ring finger and the little finger are most commonly affected, though the
middle finger may also be involved. /nly rarely are the thumb and index finger
affected.
+upuytrenPs contracture often affects both hands, though one hand is usually
affected more severely than the other.
+upuytrenPs contracture usually progresses slowly, over several years.
/ccasionally it can develop over weeks or months. )n some people it progresses
steadily and in others it may start and stop. =owever, +upuytrenPs contracture
never regresses.
.ommon foot problems$
1lantar fasciitis
Most commonly, heel pain is caused by inflammation of the plantar fascia Q the
tissue along the bottom of your foot that connects your heel bone to your toes.
1lantar fasciitis causes stabbing or burning pain thatPs usually worse in the
morning because the fascia tightens &contracts' overnight. /nce your foot
limbers up, the pain of plantar fasciitis normally decreases, but it may return after
long periods of standing or after getting up from a seated position.
igns and symptoms
harp pain in the inside part of the bottom of your heel, which may feel like a knife
sticking in the bottom of your foot
=eel pain that tends to be worse with the first few steps after awakening, when
climbing stairs or when standing on tiptoe
=eel pain after long periods of standing or after getting up from a seated position
=eel pain after, but not usually during, exercise
Mild swelling in your heel
.orns and calluses
Bour skin often protects itself by building up corns and calluses Q thick,
hardened layers of skin.
Although corns and calluses can be unsightly, you need treatment only if they
cause discomfort.
)f you have diabetes or another condition that causes poor circulation to your
feet, youPre at greater risk of complications.
igns and symptoms
Bou may have a corn or callus if you notice$
A thick, rough area of skin
A hardened, raised bump
Tenderness or pain under your skin
(laky, dry or waxy skin
.orns and calluses are often confused, but theyPre not the same thing.
.orns
Are smaller than calluses and have a hard center surrounded by inflamed
skin.
.orns usually develop on parts of your feet that donPt bear weight, such
as the tops and sides of your toes.
.orns can be painful when pushed or may cause a dull ache.
.alluses
Csually develop on the soles of the feet, especially under the heels or
balls, on the palms, or on the knees.
.alluses are rarely painful and vary in si0e and shape.
They can be more than an inch in diameter, making them larger than
corns.
)ngrown toenails
An ingrown toenail is a common condition in which the corner or side of one of
your toenails grows into the soft flesh of that toe.
The result is pain, redness, swelling and, sometimes, an infection. An ingrown
toenail usually affects your big toe.
igns and symptoms
1ain and tenderness in your toe along one or both sides of the nail
2edness around your toenail
welling of your toe around the nail
)nfection of the tissue around your toenail
=ammertoe and mallet toe
A hammertoe is a toe thatPs curled due to a bend in the middle joint of a toe.
Mallet toe is similar, but affects the upper joint of a toe.
*oth conditions are commonly caused by shoes that are too short or heels that
are too high. Cnder these conditions, your toe may be forced against the front of
your shoe, resulting in an unnatural bending of your toe.
igns and symptoms
A hammer3like or claw3like appearance of a toe
)n mallet toe, a deformity at the end of the toe, giving the toe a mallet3like
appearance
1ain and difficulty moving the toe
.orns and calluses resulting from the toe rubbing against the inside of your
footwear
*unions > hallux valgus
A bunion is an abnormal, bony bump that forms on the joint at the base of your
big toe.
Bour big toe joint becomes enlarged, forcing the toe to crowd against your other
toes. This puts pressure on your big toe joint, pushing it outward beyond the
normal profile of your foot, and resulting in pain.
*unions can also occur on the joint of your little toe &bunionette'.
*unions can occur for a number of reasons, but a common cause is wearing
shoes that fit too tightly. They can also develop as a result of inherited structural
defect, injury, stress on your foot or another medical condition.
igns and symptoms
A bulging bump on the outside of the base of your big toe
welling, redness or soreness around your big toe joint
Thickening of the skin at the base of your big toe
.orns or calluses Q these develop where the first and second toes overlap
1ersistent or intermittent pain
2estricted movement of your big toe
MortonPs neuroma
A neuroma is a noncancerous &benign' growth of nerve tissue that can develop in
various parts of your body.
MortonPs neuroma occurs in a nerve in your foot, often between your third and
fourth toes.
The condition isnPt a true tumor, but instead involves a thickening of the tissue
around one of the digital nerves leading to your toes.
MortonPs neuroma causes a sharp, burning pain in the ball of your foot. Bour toes
also may sting, burn or feel numb if you have MortonPs neuroma.
Also called plantar neuroma or intermetatarsal neuroma, MortonPs neuroma may
occur in response to irritation, injury or pressure Q such as from wearing
tightfitting shoes.
igns and symptoms
A burning pain in the ball of your foot that may radiate into your toes
Tingling or numbness in your toes
At first, the pain may worsen when you wear tight or narrow shoes or engage in
activities that place pressure on your foot.
(latfeet > pes planus
)f you have flatfeet, the arch on the inside of your feet is flattened.
(latfeet usually doesnPt cause a problem. =owever, flatfeet can contribute to
problems in your feet, ankles and knees.
igns and symptoms
A flat look to one or both of your feet
Cneven shoe wear and collapse of your shoe toward the inside of your flat foot
%ower leg pain or weakness
1ain on the inside of your ankle
welling along the inside of your ankle
(oot pain
)@(%AMMAT/2B ./@+)T)/@$
TB1-
7. Arthritis , rheumatic disease involving joint symptoms and abnormalities
!. @on3articular rhematic diseases , involves pathologic changes in structures
related to joints but not within joint themselves.
a. (ibrositis , connective tissue inflammation in any location especially around
the joints, and in or near the tendons, muscle sheats or other fasciae layers.
b. *ursitin , inflammation of the bursa major. *ursa are located in shoulder,
elbow, hips, knees
c. Tendinitis , inflammation of the tendons.
d. Myositis , inflammation of voluntary muscles
e. 1eritendinitis , inflammation of tendon sheats
f. ynovitis , inflammation of synovial membrane
g. Tenosinovitis , inflammation of tendon, tendon sheats, and synovial
membrane commonly in hands, wrists, ankle and feet.
);@ A@+ BM1T/M
%imited movement
%oss of function
1ain
welling
2edness
ACT/3)MMC@- +)/2+-2$
2=-CMAT/)+ A2T=2)T)
)t is a connective tissue disease characteri0ed by chronic inflammatory changes
in the synovial membrane and other structure.
)s a chronic systemic disease although most prominent as a non suppurative
inflammation in the diarthroidal joints, may also be manifested by lesion of the
vasculature, lungs, nervous system, and other major organs of the body.
-tiology
-xact cause is unknown
=ereditary
)nfection
tress
Metabolic disorder
Auto3immune
Allergic phenomenon
1athology
- sta(es o" rheu%atoid arthritis.
TA;- 7 , )@/<)T) TA;-
- inflammation of the synovial membrane
- tissue thickens with edema and congestion of the synovial membrane
TA;- ! , 1A@@C TA;-
- Thickened synovial tissue grows inward along the surface of the articular
cartilage
- 1annus appears to be reddish, rough and adheres tightly to the
underlying cartilage and damages it.
TA;- D , ()*2/C A@AB%/) TA;-
- ;ranulation of tissue becomes invaded with tough fibrous tissue and
converted into scar tissue which inhibits joint movement.
- .ause subluxation and distortion of affected joints
TA;- : , */@B A@AB%/)
- there is form bony union as bone tissue calcifies and changes into
osseous tissues.
1AT=/1=B)/%/;B
The disease process with in the joints &intraarticular' begins as an inflammation
of the synovium wuth edema vascular congestion, fibrin exudates and cellular
infiltrate.
1articularly damaging to joint tissue is the en0yme collagenase because it breaks
down collagen, the main structural protein of connective tissue.
2A may also affect other body system and rheumatoid nodules may form in the
heart, lung and spleen.
igns and ymptoms
7. ubcutaneous nodules , appear over tendon sheaths particularly over pressure
areas like the elbow
!. 1ainful, swollen joints especially proximal interphargeal joints of fingers, wrist
knees, feet and ankle.
D. -levated body temperature
:. Morning stiffness
H. 1aresthesias of hands and feet
#. plenomegaly
M. -nlarged lymph nodes
J. igns of anemia
.%A). 2A S even or more criteria observed
+-()@)T- 2A S H criteria with joint signs or symptoms continues for at least #
weeks
12/*A*%- 2A S D criteria with joint signs or symptoms continuous for at least #
weeks
1/)*%- 2A S ! criteria with joint signs or symptoms continuous for at least #
weeks.
%aboratory +iagnosis
-levated -2
%eukocytes
Anemia
%atex fixation test , presence of rheumatoid factor
@arrowing of the joint spaces and crosion of articular surfaces on E3ray
examination
)nflammatory changes in synovial tissue obtained by biopsy
@ursing )nterventions
7. 1rovide rest , keep joints as straight as possible. 1revent flexion deformities , firm
mattress, no pillows under his knees use footboard and trochanter roll to prevent
external rotation.
!. 2elieve pain , by analgesics and @A)+, provide heat therapy as ordered
3 warm compresses.
3 heat paraffin to 7!H to 7!K ( &H!3H: .'
D. +iet should be well balanced
:. Anemia should be treated
H. Maitain mobility , exercises are done slowly, increased gradually and not carried
past the point of being painful.
1assive exercises
)sometric -xercises , client exerts force without changing the length of the
muscle setting exercises, & alternating tightening and relaxing the muscle',
gluteal muscles setting by contracting and relaxing the buttocks, 6uadriceps
setting , pressing the popliteal space against the mattress.
2esistive -xercises , those actively done by the client with manual or
mechanical resistance. To develop muscle strength.
Treatment
7. Analgesic , aspirin
!. @on3steroidal anti3inflammatory drugs &@A)+' , )ndocin , )ndomethacin
D. ;old compounds , myochrysine , sodium thiomalate
:. Antimalaria drugs
.hloro6uine
=ydroxychloro6uine
H. .orticosteroids
#. Antacids
M. 1araffin dips of affected extremity for relief of joint pain by providing uniform heat.
J. urgery , when medical therapy fails to reduce inflammation
ynovectomy , to remove access synovial fluid and tissue in order to
prevent recurrence of inflammation.
Arthrotomy , opening in the joints to remove damaged tissue or calcium
deposits.
Arthrodesis , fusion of the joint to give stability, correct deformity and
relieve pain.
Arthroplasty , plastic reconstruction of a joint to permit mobility and weight
bearing and alleviate pain.
BT-M). %C1C -2BT=-MAT/C , %-
.hronic connective tissue disease involving multiple organ system.
)s a chronic inflammatory disease of autoimmune origin that affects primarily the
skin, joints and kidneys, although it may affect virtually every organ of the body.
.linical features
7. etiology not clearly understood , but believed to be auto3immune, hereditary and
viral cause, drug3induced
!. most fre6uently found in young woman with signs and symptoms referable to
joints and skin
D. remissions and exacerbation
:. very difficult to validate diagnosis
D major areas are currently being researched as possible causes of %-$
7. +enetic Factors , family members of persons with %- have an increased chance of
developing the disease.
!. En/iron%ental Factors , ultraviolet light is known to cause exacerbations.
D. Alteration in the I%%une )esponse , cause immune complexes containing antibodies
to be deposited in tissue, causing tissue damage.
@ecrosis of the glomerular capillaries, inflammation of cerebral and ocular blood
vessels, necrosis of lymph nodes, vasculitis of the ;) tract and pleura, and
degeneration of the basal layer of the skin.
igns and ymptoms$
. Sub0ecti/e.
Malaise
1hotosensitivity
Joint pain
'. Ob0ecti/e
(ever
*utterfly erythema on the face
1ositive %- prep.
+iagnostic Tests
.linically documented multiorgan damage
1ositive fluorescent anti , nuclear antibody test &A@A'
)ncrease -2
-levated serum rheumatoid factor
)ncreased 9*.
+ecreased 2*. and hemoglobin
2enal function test is elevated
1ositive %- , cell test
Treatment
.orticosteroids and analgesics to reduce pain and inflammation
upportive therapy as major organs become affected &heart, kidneys, .@, ;)'
@ursing .are
7. Administer medications and observe for side effects .
!. =elp the clients and family code with severity of the disease as well as its poor
prognosis.
D. )mprove and maintain nutritional status.
M-TA*/%). ./@+)T)/@
;/CTB A2T=2)T)
)nflammation of the joints secondary to abnormal metabolism of uric acid.
Csually affects the big toe
)s ametabolic disorder that develops as a result of prolonged hyperuricemia
&elevated serum uric acid ' caused by problems in synthesi0ing purines or by
poor renal excretion of uric acid.
)ncidence highest in males, a familial tendency has been demonstrated.
May have deposition of uric acid crystal &tophi' in tissue or renal urate lithiasis
&kidney stone' may result from precipitation of uric acid in the presence of a low
urinary p=.
-tiology
;enetic defect in purine metabolism , overproduction of uric acid
+ecreased uric acid excretion , .2(
+iet , high in purine
+iagnostic Test
-levated -2, 9*.
)ncrease serum uric acid levels
ynovial fluid reveal urate crystals
igns and ymptoms
2edness, swelling joints
Joint pain
%imited movement
Tophi , urate crystals deposited in great toe, ankle, or increase wherein there is
dimished blood flow.
Management
Administration of anti3inflammatory and &A@T) ;/CT' agents to decrease
synthesis of uric acid
- 1urinase
- %lanol
- ynol
- yloprim
- Allopurinol
alicytes
@A)+
alkaline3ash diet to increase the p= of urine to discourage precipitation of uric
acid and enhance the action of drugs &C2)./C2). A;-@T' increase excretion
of uric acid
*enemid 3 1robenecid
.olsalide 3 .olchicine
elimination of foods high in purines
weight loss is encouraged if indicated
+iet , low purine diet, alkaline ash diet , avoid shellfish, sardines, liver, kidneys,
internal organs
@ursing .are$
7. Assess joint pain, motion and appearance
!. Administer anti3 inflammatory agents such as *uta0olicin, oxypheabuta0one
&Tandearil', or endomethacin &)ndocin' with antacids or milk to prevent peptic
ulcers. /bserve therapeutic response.
D. .areful align joints so they are slightly flexed during acute stage, encourage
regular exercise, which is important for long term management.
:. Cse a bed cradle during the acute phase to keep pressue of sheets off joints.
H. )ncrease fluid intake to !""" to D""" ml > day to prevent formation of calculi
#. )nstruct client to avoid high3purine foods suchs as organ meats, anchovies,
sardines and shellfish diet.
/T-/A2T=2)T)
+egenerative joint disease also known as osteoarthritis is an extremely common
disease that is probably as old as civili0ation.
9omen are more severely affected by the disease, although the incidence rates
are the same for males and females
1rimary joint disease is the most common type of noninflammatory joint disease.
1rimary degenerative joint disease is distributed throughout the central and
peripheral joints of the body, usually affecting the joints of the hand, wrist, neck,
lumbar spine, hips, knees and ankle.
The etiology is unknown, but age is an important factor in the development of the
disease.
The 6uantity and 6uality of proteoglycans decrease with the aging process and
predispose the cartilage to breakdown and degenerate.
.linical Manifestations
7. 1ain , worse with weight bearing, improves with rest.
!. welling and joint enlargement$
a. =eberden?s @odes , bony protuberances occurring on the dorsal surface of the
distal interphalangeal joints of the finger.
b. *ouchard?s @odes , bony protuberance occurring on the proximal
interphalangeal joints of the finger
c. .oxachrosis &+egenerative Joint +isease of the hip' , pain in the hip on weight
bearing, with pain progressing to include groin and medial knee pain.
D. Muscular Atrophy , from disuse, joint instability and deformity
:. +ecreased 2ange of Motion , depends on amount of destroyed cartilage
H. Join stiffness , worse in the morning and after a period of rest or disuse.
.=A2A.T-2)T). 1AT=/%/;). .=A@;- A((-.T)@; T=- A2T).C%A2
.A2T)%A;-
7. -rosion of articular cartilage
!. Thickening of underneath the cartilage
D. Medications to reduce symptoms such as analgesics, anti3inflammatory agents,
and steroids.
:. -xercise of affected extremities.
H. urgical intervention
a. ynovectomy , removal of the enlarged synovial membrane before bone and
cartilage destruction occurs.
b. Arthrodeseis , fusion of a joint performed when the joint surfaces are severely
damaged, this leaves the client with no range of motion of the affected joint.
c. 2econstructive urgery , replacement of a badly damaged joint with a prosthetic
device.
/T-/1/2/)
A clinical condition in which there is a decrease in total amount of bone to the
point that factures occur with minor trauma.
.alcium in the bone is depleted and the bone matrix fails to produce replacement
bone. The result is a weakening of the structure.
.auses
-xact cause is not known
@utritional deficiency , <itamin ., calcium deficiency
-ndocrine disease , hyperthyroidism, hyperparathyroidism, cushing?s syndrome,
women past menopause
1rolonged immobility , due to lack of normal stresses and strains.
igns and ymptoms
%ow back pain or musculo3skeletal aching
1athological fracture
)ncrease in urinary calcium especially at night as calcium withdrawal increase.
Management
-xercise with fre6uent rest periods
Avoidance of severe fatigue
pinal support , corset or light brace in upright position
Analgesic
Muscle relaxants
Ade6uate intake of protein, <itamin + and .alcium
-strogen therapy to post menopausal women.
/T-/MA%A.)A
+ecalcification, softening of bones
+efined as a defect in minerali0ation of adult bone, generally resulting from
abnormalities in <itamin + metabolism.
.ause
1oor intake of <itamin +
+ecrease exposure to sunlight
)ntestinal malabsorption
Anticonvulsant therapy and hepatic and renal disease
igns and ymptoms
9idespread softening of bones especially on spine, pelvis and lower extremities
*ones are deformed, maybe bent or flattened as the bone soften
1ain
Tenderness
x3ray changes reveal pseudofractures or cyst formation
Management
Ade6uate nutrition
unshine exposure
<itamin + supplements
)@(-.T)/C ./@+)T)/@
*A.T-2)A% A2T=2)T)
-tiology
invasion of the synovial membrane by microorganism, most often ;onocossi,
meningococci, coliforms, salmonellae and =aemophilus )nfluen0ae.
-pidemiology
susceptible to patient who had recent joint surgery and trauma, intraarticular
injections and rheumatoid arthritis.
1athophysiology
synovial tissue respond to bacterial invasion by becoming inflamed. The joint
cavity may become involved, and pus will be present in the synovial membrane
and synovial fluid.
patient complain of pain, swelling, and tenderness of the joint
joint aspiration is helpful in making the diagnosisi if the presence of organism can
be demonstrated in the synovial fluid. 9hite blood cell will be high, and glucose
content of fluid may be reduced.
Medical Management
7. Appropriate antibiotic therapy.
!. 2est or immobili0ation of the joint.
D. urgical drainage if infection does not respond to antibiotic therapy
:. 2esumption of active range of motion when infection subsides and motion can be
tolerated.
@ursing Management
7. 1romoting rest of the affected joint.
!. Administering antibiotics and pain medication as prescribed.
D. -ncouraging the patient to participate within restriction of prescribed rest for joint.
:. 1atient teaching$
a. -ncouraging active joint motion when motion is permitted.
b. )nstructing in proper administration of antibiotics if theraphy is to be continued
after discharge.
c. Assuring that patient is aware of plans for follow up with physician.
/T-/MB-%)T)
*one infection from pyrogenic microorganism
i.e., taphylococcus Aureus , K"N of cases
treptococcus
almonella
although the development of osteomyelitis is often precipitated by a traumatic
event or is a complication of trauma. )t is included with the degenerative
disorders because of its chronic and debilitating aspect.
! Types
a. E$o(enous Osteo%&elitis , caused by pathogen from outside the body, such as
from an open fracture or surgical procedure.
b. 1e%ate(enous Osteo%&elitis , caused by blood3borne pathogen originating from
infectious site within the body. E$a%ples include sinus, ear, dental, respiratory
and genitourinary infectious.
1athophysiology
- )n hematogenous /steomyelitis, the organism reach the bone through the
circulatory and lymphatic system. The bacteria lodge in the small vessels
of the bone, triggering an inflammatory response.
- The femur, tibia, humerus and radius are commonly affectede.
- *one inflammation is marked by edema, increased vasculature and
leukocyte activity. The infectious process weakens the cortex, thereby
increasing the risk of pathologic fracture.
- *rodie?s Abcesses are characteristic of chronic osteomyelitis.
- )n cases of exogenous esteomyelitis, the infections begin in the soft
tissue and eventually forming abscess.
- .hronic /steomyelitis is difficult to treat. 2ecurrent infections, areas of
dead bone &se6uestrum', and scar tissues are contributing factors to its
resistance to treatment.
- 1atient may report fever, malaise, anorexia and headache. The affected
body part maybe erythematous, tender and edematous. There maybe an
opening in the skin, draining purulent material.
igns and ymptoms
1ain
=eat, redness, swelling, tenderness
%imited movement
2ise in temperature, chills
;eneral body malaise and weakness
Marked leukocytosis
-levated -2
1ossibly, positive blood cultures
Management
Analgesic
Anti3inflammatory
Antibiotic especially 1enicillin
9ound )rrigation
)ncision and drainage
+ebridement
.omplete removal of dead bone and soft tissue
.ontrol of infection
-limination of dead space &after removal of necrotic bone'
e6uestrectomy , surgical removal of the dead infected bone and cartilage
@ursing .are
Cse surgical aseptic techni6ue when changing dressings
Maintain functional body augment and promote comfort.
Allow the client ample time to express feelings about long term hospitali0ation.
Ctili0e room deori0er is a foul odor is apparent
-ncourage nutrient dense diet to compensate for antibiotic impact on nutritional
status.
T* of the pine , 1/TT? +isease
- bone infection caused by invasion in the body by Aock?s bacillus
igns and ymptoms
Muscle spasm
tiffness
Tendency to reach things on the floor by bending the knees rather than the back.
-ffects usually the lower dorsal spine and upper lumbar spine.
;ibbus formation angulation or pronounce antero3posterior curve of the spine as in
hunchback due to collapse of the vertebrae
1aralysis occasionally
Afternoon fever
.omplications , abscess formation
7. .ervical region , pharynx respiratory problems.
!. +orsal region , mediastinum and may rupture into the lungs.
D. %umbar spine , lumbar muscles or gluteal region or may follow the course of
ilopsoas muscles and point in the groin &psoas abscess' 3 most common.
Management
7. Anti T* drugs
- 2ifampicin
- 1LA
- )@=
!. )mmobili0ation , Taylor body brace
D. (resh air, sunshine and proper diet
+B1%A)A /( T=- =)1
.ondition in which the head of the femur is improperly seated in the acetabulum,
or hip socket, of the pelvis
.ongenital or develop after birth
Neonate. 3 due to laxity of ligament around the hip, allowing the femoral head to
be displaced from the acetabulum upon manipulation.
I%ple%entation$ splinting of the hips with 1avlik harness to maintain flesion and
abduction and external rotation &neonatal period'
Assess%ent. 3 infacnts has asymmetry of the gluteal and thigh skin folds when
the child is placed prone and the legs are extended against the examining table.
%imited range of motion in the affected hip.
Asymmetric abduction of the affected hip when the child is placed supine with the
knees and hips flexed.
Apparent short femur on the affected side.
./@;-@)TA% =)1 +B1A)A
Traction and surgery to release muscles and tendons
Maintain abduction and external rotation & application of double diapers when
changing the infant '.
(ollowing surgery, positioning and immobili0ation in a spica cast until healing is
achieved.
9alking child has minimal to pronounced variation in gait with lurching toward the
affected side.
1ositive Trendelenburg sign
1ositive *arlow or /rtolani?s maneuver.
+-<-%/1M-@TA% A@/MA%)- /( T=- -ET2-M)T)-
A. polydactyl , extra digits
*. yndactyly , partial or complete fusion of two or more digits
.. Amelia , absence of a limb
+. Treatment , if possible, early correction and preparation for use of a prosthesis.
MC.C%/3A-%-TA% ./@+)T)/@
Traumatic .onditions
7. .ontusion , an injury to soft tissue produced by blunt force, blow, kick or fall.
igns and ymptoms
=emorrhage into the injured part &ecchymosis' from rupture of small blood vessels
1ain, swelling
Treatment
-levate the affected part
.old compress to diminish edema formation
1ressure bandage to reduce swelling
Apply heat to affected area after # hours to promote absorption
!. train , injury to muscle or tendons. Treatment same as contusion
D. prain , injury to ligamentous structures surrounding a joint, caused by wrenching or
twisting
:. +islocation , a condition in which the articular surfaces of the bones forming the joints
are no longer in anatomic contact with one another.
.linical Manifestations
.hange in contour of the joint
.hange in length of extremity
%oss of normal movement
.hange in axis of dislocated bones.
H.(racture , a break in the continuity of a bone
;eneral .lassification
a. .omplete (racture , fracture involving the entire cross3section of the bones
b. )ncomplete (racture , a fracture involving only a portion of the cross section of
the bone.
c. /pen (racture &compound' , break in the bone, skin and there?s communication
between the fracture site and the external air.
d. .losed (racture , &simple' , break in the bone, skin and there?s communication
between the fracture site and the external air.
pecific types of fracture
a. ;reenstick (racture , fracture in which one side of a bone is broken, the other
side is being beat.
b. .omminuted , a fracture in which bone has splintered into fragments.
c. +epressed , a fracture in which a fragment is driven inward &fracture of skull,
facial bones'
d. Transverse , a break straight across the bone
e. piral , with the fracture lines partially encircling the bone
f. piral , with the line of fracture at an obli6ue angle to the bone shaft.
igns and ymptoms
7. igns of local trauma &injury to soft tissue'
pain
tenderness
swelling
bruising
muscle spasm
redness
!. +ue to damage to blood vessels
bleeding
D. .repitus sound , grafting sound produced as bones rub against each other
:. hortening of extremity
H. 1resence of deformity
#. %imited function>loss of function
M. @umbness if with injury to the nerves
.omplication of (racture
7. )mmediate
3 shock
3 fat embolism
3 injury to skin, muscle, blood vessels and nerves
!. -arly
3 infection , gas gangrene, tetanus, osteomyelitis
D. %ate
3 non3union
3 delayed union
3 mal3union
3 avascular necrosis of the bone
MA@A;-M-@T /( (2A.TC2- & - )2s3
7. )ECO+NITION , of presence of fracture
!. )E4#CTION
a. .losed 2eduction , done by manipulation
b. /pen 2eduction
c. Traction
D. )ETENTION
a. .ast
b. Traction
c. *races and splints
d. *andage
:. )E1A!ILITATION , restoration to normal function
Вам также может понравиться
- Bone Development and Growth: Rosy Setiawati and Paulus RahardjoДокумент20 страницBone Development and Growth: Rosy Setiawati and Paulus Rahardjoputri aisheОценок пока нет
- The Power of Partnership: Underground Room & Pillar Lateral Development and DownholesДокумент4 страницыThe Power of Partnership: Underground Room & Pillar Lateral Development and DownholesjoxegutierrezgОценок пока нет
- I. Leadership/ Potential and Accomplishments Criteria A. InnovationsДокумент5 страницI. Leadership/ Potential and Accomplishments Criteria A. InnovationsDEXTER LLOYD CATIAG100% (1)
- Lecture Guide Assessment-Of-Musculoskeletal-Function HPДокумент85 страницLecture Guide Assessment-Of-Musculoskeletal-Function HPBlessed GarcianoОценок пока нет
- Skeletal SystemДокумент40 страницSkeletal System119286kinОценок пока нет
- Tricald 130524041738 Phpapp01Документ57 страницTricald 130524041738 Phpapp01Vishwas U MadanОценок пока нет
- BSN1 Unit 5 Skeletal SystemДокумент101 страницаBSN1 Unit 5 Skeletal SystemCherub Chua100% (1)
- Skeletal System: CartilageДокумент20 страницSkeletal System: CartilageGrace PascualОценок пока нет
- Chapter 6 Bone Tissue 2304Документ37 страницChapter 6 Bone Tissue 2304Sav Oli100% (1)
- HANDOUTS Prelim CH 6Документ40 страницHANDOUTS Prelim CH 6Abia Annieson A. LorenzoОценок пока нет
- BoneДокумент33 страницыBoneNihal BilalОценок пока нет
- Overview of The Musculoskeletal System: For Year 1 Medicine By: Zelalem.aДокумент36 страницOverview of The Musculoskeletal System: For Year 1 Medicine By: Zelalem.aAmanuel MaruОценок пока нет
- Lec 1516 Bone Tissue and Skeletal SystemДокумент28 страницLec 1516 Bone Tissue and Skeletal SystemonegaonnweОценок пока нет
- Bone TissueДокумент66 страницBone TissueFunikawati Baldiyah100% (1)
- The Skeletal SystemДокумент52 страницыThe Skeletal SystemrizzamaearancesОценок пока нет
- Dr. Sassia Lecture Bone Histology Part II July 4 2023Документ39 страницDr. Sassia Lecture Bone Histology Part II July 4 2023Ali ELKARGHALYОценок пока нет
- MusculoSkeletal SystemДокумент56 страницMusculoSkeletal Systemmaj71% (7)
- Exam A-3Документ11 страницExam A-3yapues87Оценок пока нет
- Introduction To Skeletal 1Документ196 страницIntroduction To Skeletal 1Earl TrinidadОценок пока нет
- Bone Fracture & RemodellingДокумент39 страницBone Fracture & Remodellingokware rodrickОценок пока нет
- Bone TissueДокумент66 страницBone TissueWalter Macasiano GravadorОценок пока нет
- UNIT - 7 Skeletal SystemДокумент163 страницыUNIT - 7 Skeletal SystemChandan ShahОценок пока нет
- Bone HistologyДокумент30 страницBone HistologyVicОценок пока нет
- The Skeletal SystemДокумент30 страницThe Skeletal SystemFAtma HAnysОценок пока нет
- Skeletal System Lesson 2Документ40 страницSkeletal System Lesson 2Ella Nika FangonОценок пока нет
- Bone & Ossification: Histology Part: Module2, Unit 3Документ14 страницBone & Ossification: Histology Part: Module2, Unit 3Obansa John100% (1)
- SKELETAL SYSTEM ReviewerДокумент7 страницSKELETAL SYSTEM ReviewerKrize Colene dela CruzОценок пока нет
- Skeletal System 1: Dr. Garry NiedermayerДокумент57 страницSkeletal System 1: Dr. Garry NiedermayerWeng Sze TingОценок пока нет
- Biochemistry of Bone (Assignment)Документ7 страницBiochemistry of Bone (Assignment)haseeb ShafaatОценок пока нет
- Chap 6 AnaphyДокумент8 страницChap 6 AnaphyNicholle VelosoОценок пока нет
- Bone As A Living Dynamic TissueДокумент14 страницBone As A Living Dynamic TissueSuraj_Subedi100% (6)
- 1 Sistem MuskuloskeletalДокумент27 страниц1 Sistem MuskuloskeletalAshar AbilowoОценок пока нет
- It 2 - Pengantar Kartilago, Otot, Dan Tulang (Irw)Документ48 страницIt 2 - Pengantar Kartilago, Otot, Dan Tulang (Irw)RurieAwaliaSuhardiОценок пока нет
- BoneДокумент26 страницBoneAbdi Asiis Omar MohamedОценок пока нет
- Skeletal SystemДокумент123 страницыSkeletal SystemZekiah MagsayoОценок пока нет
- (Manzanares) Skeletal System Study GuideДокумент17 страниц(Manzanares) Skeletal System Study GuideKyla ManzanaresОценок пока нет
- Normal Bone Anatomy and Physiology: Go ToДокумент11 страницNormal Bone Anatomy and Physiology: Go TotariОценок пока нет
- SkeletalSystem 2Документ114 страницSkeletalSystem 2LYRA GUEVARRAОценок пока нет
- 7 Bone+TissueДокумент56 страниц7 Bone+Tissuegabbs_123Оценок пока нет
- Chapter 3Документ12 страницChapter 3Deolita BadiangОценок пока нет
- Skeletal SystemДокумент3 страницыSkeletal SystemFrederick ManaigОценок пока нет
- ALVEOLAR BoneДокумент72 страницыALVEOLAR BoneArchana50% (2)
- Bone and Joints 2Документ38 страницBone and Joints 2Eryn HooverОценок пока нет
- Bone Development, Healing, ConditionsДокумент31 страницаBone Development, Healing, ConditionsEnos ErastusОценок пока нет
- Bone Tissue-Growth and DevelopmentДокумент53 страницыBone Tissue-Growth and Developmentgalaxyduck100% (1)
- Formation: Blood Calcium Level - Calcium HydroxyapatiteДокумент13 страницFormation: Blood Calcium Level - Calcium HydroxyapatiteClarissa IsuriñaОценок пока нет
- The Skeletal SystemДокумент7 страницThe Skeletal SystemKathleenJoyGalAlmasinОценок пока нет
- Bone-LДокумент34 страницыBone-LurjaОценок пока нет
- Chapter 6 Content Review Questions 1-8Документ3 страницыChapter 6 Content Review Questions 1-8Rhonique MorganОценок пока нет
- Basic Bone BiologyДокумент3 страницыBasic Bone BiologyRuxandra Maria100% (1)
- The Skeletal System: Rzgar F. RashidДокумент23 страницыThe Skeletal System: Rzgar F. Rashidyıldız kubeОценок пока нет
- Bone Tissues and The Skeletal System: Jahangir Moini, MD, MPHДокумент108 страницBone Tissues and The Skeletal System: Jahangir Moini, MD, MPHAngella CharlesОценок пока нет
- 6.the Skeletal System Bone TissueДокумент25 страниц6.the Skeletal System Bone TissueKojo Yeboah EnchillОценок пока нет
- Skeletal System (2015 - 06 - 09 20 - 43 - 48 Utc)Документ120 страницSkeletal System (2015 - 06 - 09 20 - 43 - 48 Utc)DiazОценок пока нет
- Bone Tissue: Supportive Connective Tissue: CellsДокумент52 страницыBone Tissue: Supportive Connective Tissue: CellsCalin PopaОценок пока нет
- Document From TIFFIN XPRESSДокумент19 страницDocument From TIFFIN XPRESSloungehighwayОценок пока нет
- Skeletal System: - Composed of The Body's Bones and Associated Ligaments, Tendons, and Cartilages. - FunctionsДокумент66 страницSkeletal System: - Composed of The Body's Bones and Associated Ligaments, Tendons, and Cartilages. - FunctionsDenver TanhuanОценок пока нет
- ch07 Answer Key 13editionДокумент24 страницыch07 Answer Key 13editionAditya Madduluri100% (1)
- Carbonyl Compounds: Unit 4 Rates, Equilibria and Further Organic ChemistryДокумент5 страницCarbonyl Compounds: Unit 4 Rates, Equilibria and Further Organic ChemistryKirusaanth SathiyathasanОценок пока нет
- JeromeДокумент2 страницыJeromeNads DecapiaОценок пока нет
- Unit Weight of Materials Used at Construction Site - Online Civil PDFДокумент2 страницыUnit Weight of Materials Used at Construction Site - Online Civil PDFKeshav VarpeОценок пока нет
- The Learner The Learner : 1 QuarterДокумент4 страницыThe Learner The Learner : 1 QuarterRode Jane SumambanОценок пока нет
- 21 Day Level Up Challenge My PathДокумент52 страницы21 Day Level Up Challenge My PathDavid Stark100% (1)
- Minibeasts Differentiated Reading Comprehension ActivityДокумент15 страницMinibeasts Differentiated Reading Comprehension Activitymariam helmyОценок пока нет
- Northern NVProvider DirectoryДокумент82 страницыNorthern NVProvider DirectoryGuru NandeshwarОценок пока нет
- Diesel Generator 350-To-500-Kw-Specs-SheetДокумент9 страницDiesel Generator 350-To-500-Kw-Specs-SheetamrОценок пока нет
- How To Conduct A Situation AnalysisДокумент10 страницHow To Conduct A Situation AnalysisÂmany AymanОценок пока нет
- 1 s2.0 S0378517311000226 MainДокумент9 страниц1 s2.0 S0378517311000226 MainFIRMAN MUHARAMОценок пока нет
- Curriculum Vitae (CV) - Design-AM-KAWSAR AHMEDДокумент5 страницCurriculum Vitae (CV) - Design-AM-KAWSAR AHMEDEngr.kawsar ahmedОценок пока нет
- Maxipro NewДокумент2 страницыMaxipro NewLokendraОценок пока нет
- Tle Reviewer 3Документ7 страницTle Reviewer 3Pia louise RamosОценок пока нет
- Magic Coco Tiles: Green Building MaterialДокумент17 страницMagic Coco Tiles: Green Building MaterialnikoОценок пока нет
- Pulse Production in India: Major Constraints and Way ForwardДокумент33 страницыPulse Production in India: Major Constraints and Way ForwardDeus EXОценок пока нет
- Mouse HardyweinbergДокумент5 страницMouse Hardyweinbergapi-477617112Оценок пока нет
- Civrev2 2019 Case TitlesДокумент3 страницыCivrev2 2019 Case TitlesAnne VallaritОценок пока нет
- 1-1FlowCharts For HaccpДокумент3 страницы1-1FlowCharts For HaccpPeter George0% (1)
- Carcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistДокумент48 страницCarcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistMuhammad ArsalОценок пока нет
- English The RainДокумент2 страницыEnglish The RainsmitaОценок пока нет
- Left Side View: Electrical System G3516A and G3516B EngineДокумент2 страницыLeft Side View: Electrical System G3516A and G3516B EngineAM76100% (1)
- Motor DeiselShip Latest PDFДокумент154 страницыMotor DeiselShip Latest PDFCadet Prateek SaxenaОценок пока нет
- Recipes For Ceviche, Pebre and Pisco SourДокумент4 страницыRecipes For Ceviche, Pebre and Pisco SourJoaquín Rolón CarrerasОценок пока нет
- Geared Motor Device 100/130V E1/6-T8Документ2 страницыGeared Motor Device 100/130V E1/6-T8seetharaman K SОценок пока нет
- Nurs 512 Andersen Behavioral TheoryДокумент7 страницNurs 512 Andersen Behavioral Theoryapi-251235373Оценок пока нет
- Baobabs of The World Cover - For Print PDFДокумент1 страницаBaobabs of The World Cover - For Print PDFBelinda van der MerweОценок пока нет
- Chapter 4Документ6 страницChapter 4Aung MyatОценок пока нет
- 4a-Ancient Indian Engineering BotanyДокумент44 страницы4a-Ancient Indian Engineering BotanyAshok NeneОценок пока нет