Академический Документы
Профессиональный Документы
Культура Документы
Cabt10i4p291 Fraktur Mandibula
Загружено:
Trefina Prana0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров6 страницThis article provides a review of literature regarding the management of mandibular body fracture in young children. The goal of treatment of these fractures is to restore the underlying bony architecture to pre-injury position, in a stable fashion, with minimal residual esthetic and functional impairment.
Исходное описание:
Оригинальное название
cabt10i4p291 fraktur mandibula
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis article provides a review of literature regarding the management of mandibular body fracture in young children. The goal of treatment of these fractures is to restore the underlying bony architecture to pre-injury position, in a stable fashion, with minimal residual esthetic and functional impairment.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров6 страницCabt10i4p291 Fraktur Mandibula
Загружено:
Trefina PranaThis article provides a review of literature regarding the management of mandibular body fracture in young children. The goal of treatment of these fractures is to restore the underlying bony architecture to pre-injury position, in a stable fashion, with minimal residual esthetic and functional impairment.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 6
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 291
Management of mandibular body fractures in pediatric patients: A case
report with review of literature
BABY JOHN, REENA R. JOHN
1
, STALIN A., INDUMATHI ELANGO
Abstract
Mandibular fractures are relatively less frequent in children when compared to adults, which may be due to the childs protected
anatomic features and infrequent exposure of children to alcohol related trafc accidents. Treatment principles of mandibular
fractures differ from that of adults due to concerns regarding mandibular growth and development of dentition. A case of a
4.5-year-old boy with fractured body of mandible managed by closed reduction using open occlusal acrylic splint and circum
mandibular wiring is presented. This article also provides a review of literature regarding the management of mandibular body
fracture in young children.
Keywords: Circum mandibular wiring, mandibular body fractures, open occlusal acrylic splint, pediatric dental trauma
Department of Pediatric and Preventive Dentistry, KSR College
of Dental Sciences and Research Institute, Trichengode, India.
1
Department of Oral and Maxillofacial Surgery, Vinayaka
Missions Sankarachariar Dental College, Salem, India.
Correspondence: Dr. J. Baby John, 21/88c, West Main Road,
Mettur Dam 636 401, Tamil Nadu, India.
E-mail: johnbjohn2005@yahoo.com
Introduction
The reported incidence of pediatric injuries accounts for
46% of the total. Below the age of 5 years, the incidence
of pediatric facial fractures is even lower, ranging from 0.6
to 1.2%.
[1]
The principles of management of mandibular
fractures differ in children when compared to adults. While
in the adults, absolute reduction and fixation of fractures is
indicated, in children minimal manipulation of facial skeleton
is mandated. The goal of treatment of these fractures is
to restore the underlying bony architecture to pre-injury
position, in a stable fashion, as non-invasively as possible,
with minimal residual esthetic and functional impairment.
Depending on the type of fracture and the stage of
skeletal development the treatment modalities range from
conservative non-invasive through closed reduction and
immobilization methods to open reduction with internal
fixation. Disruption of the periosteal envelope of the
mandibular body may have an unpredictable effect on growth.
Thus, if reduction is required, closed reduction is favored.
Case Report
A 4.5-year-old boy reported to the dental clinic with
bleeding from oral cavity following fall from bicycle. Clinical
examination revealed bruise on the chin, open mouth
appearance with profuse bleeding from the oral cavity and
derangement of occlusion [Figure 1]. Step deformity with
tenderness and mobility was elicited along the lower border
of the mandible on the left side canine region. Preoperative
orthopantamogram (OPG) could not be taken due to the
profuse bleeding needing immediate intervention.
Under sedation, upper and lower arch alginate impressions
were taken and stone casts were poured. An open occlusal
acrylic splint was fabricated [Figure 2], and under general
anesthesia, the mandibular body fracture was immobilized,
fixed with the acrylic splint which was retained by circum
mandibular wiring [Figures 3 and 4]. Patient was reviewed
every week, and on the third postoperative week, the
circum-mandibular wiring and splint was removed under
local anesthesia. No mobility was present at the fracture site.
Postoperative recovery was uneventful and occlusion achieved
was satisfactory, although spacing was seen in incisorcanine
region [Figure 5]. Patient was reviewed monthly for 6 months.
On 2 months follow-up, the spacing had closed and the child
had good alignment of teeth [Figure 6]. Patient had perfect
occlusion and good masticatory efficiency.
Review of literature
Facial fractures in children account for the approximately
5% of all facial fractures.
[2]
A male predilection is seen in
all age groups. The most common fracture in children
requiring hospitalization and/or surgery generally involves
the mandible and, in particular, the condyle. Fractures in the
condylar region are the most common, followed by angle
Access this article online
Quick Response Code:
Website:
www.contempclindent.org
DOI:
10.4103/0976-237X.76406
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 292
John et al.: Addressing the need for long term follow up after treatment of mandibular fractures in growing children
and body fractures. The etiologies of mandibular fractures
in children are usually falls and sports injuries.
The protective anatomic feature of a childs face decreases
the incidence of facial fractures. In young children (less than 5
years of age), the face is in a more retruded position relative
to the protective skull, therefore, there is a lower incidence
of midface and mandibular fractures and a higher incidence
of cranial injuries. With increasing age and facial growth
directed in a downward and forward direction, midface and
mandible becomes more prominent; thus, the incidence
of facial fractures increases, while that of cranial injuries
decreases.
[3]
The high elasticity of young bones, a thick layer
of the adipose tissue covering them, a high cancellous-to-
cortical bone ratio and flexible suture lines are some of the
Figure 1: Preoperative photograph following trauma
Figure 3: Postoperative photograph after circum mandibular
wiring
Figure 2: Mandibular cast with open occlusal acrylic splint
Figure 4: Postoperative orthopantamogram showing circum
mandibular wiring
Figure 5: Spacing evident in incisorcanine region following
wire and splint removal
Figure 6: Follow-up after 2 months showing space closure
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 293
John et al.: Addressing the need for long term follow up after treatment of mandibular fractures in growing children
reasons contributing to the low incidence of facial fractures
and minimal displacement of the fracture fragments.
[4-5]
The clinical features of a fractured mandible in a child are the
same as in an adult, which includes pain, swelling, trismus,
derangement of occlusion, sublingual ecchymosis, step
deformity, midline deviation, loss of sensation due to nerve
damage, bleeding, TMJ problems, tenderness, movement
restriction, open bite and crepitus. Thorough clinical
examination, however, may be impossible in uncooperative
young trauma patients. Lacerations should be evaluated to
reveal injuries to underlying structures. General palpation
should be applied over all bony surfaces of the mandible. The
mandibular range of motion must be examined as patients
actively open and close their mouth.
For children, the imaging technique which is of value,
especially following trauma, is a computed tomography
(CT) scan, since plain radiographs in young children are less
helpful than in adults due to unerupted tooth buds obscuring
fractures, the increased incidence of greenstick fractures
and the fact that the cortex is underdeveloped, leading to
difficulty in visualizing fractures.
[6]
Treatment of mandibular fracture in children depends
on the fracture type and the stage of skeletal and dental
development.
[7]
Mandibular growth and development of
dentition are the main concerns while managing pediatric
mandibular fractures. In adults, absolute reduction and
fixation of fracture is indicated, whereas in children minimal
manipulation of the facial skeleton is mandated. The small
size of the jaw, existing active bony growth centers and the
crowded deciduous teeth with permanent tooth buds located
in great proximity to the mandibular and mental nerves, all
significantly increase the therapy related risks of pediatric
mandibular fractures and their growth related abnormalities.
Intact active mandibular growth centers are important for
preserving mandibular function, which have a significant
influence on future facial development. Thus, restoration
of the mandibular continuity after fracture is important not
only for immediate function but also for future craniofacial
development. Accordingly, the goal of treatment is to restore
the underlying bony architecture to its pre-injury position in
a stable fashion as non-invasively as possible with minimal
residual esthetic and functional impairment.
Problems encountered in management of pediatric
mandibular fractures
Loose anchorage system due to attrition of deciduous
teeth and physiologic resorption of roots.
[7]
Precarious dental stability in the mixed dental
development period.
Difficulties in securing IMF using arch bars and eyelets
as primary teeth are not sufficiently stable and may be
avulsed due to the pressure exerted. In addition, the
partially erupted secondary teeth are not sufficiently
stable in the pediatric soft bone.
[2,7]
Shape of the primary teeth: Conical shape with wide
cervical margins and tapered occlusal surface makes
placement of wires technically challenging.
[4]
Restricted normal dietary intake in children on IMF was
reported to result in significant weight and protein loss
and reduced tidal volume.
[7]
Children on IMF are at an increased risk of aspirating
gastric contents should they vomit.
[7]
The wires cause discomfort and damage periodontal
tissues.
[2,7]
Despite the fact that the goal of treatment is to establish
the bony architecture to pre-injury state as non-invasively
as possible, the challenges with closed reduction and IMF
are many. However, some authors have indicated that IMF
using arch bars is safe in children, especially those older
than 9 or 11 years.
Alternative devices for closed reduction
Several studies have recommended the use of pre-fabricated
acrylic splints as a treatment for pediatric mandibular
fractures. These splints are more reliable than open reduction
or IMF techniques with regard to cost effectiveness, ease of
application and removal, reduced operating time, maximum
stability during healing period, minimal trauma for adjacent
anatomical structures and comfort for young patients.
[8]
Laster et al,
[9]
described nickel titanium staples which are
inserted in a relatively non-invasive and pain free manner
and their eventual removal, if required, is done as quickly
as their insertion, facilitated by the fact that the staples
are not osseointegrated. Due to their superficial location,
there is little risk for inhibiting and deforming facial bone
development or having any proximal strategic structures
such as nerves and developing dentition. Furthermore, the
reduced compression rendered by the staples on the bony
fragments result in primary healing with no callus produced.
Modified orthodontic brackets have been used for
maxillomandibular fixation (MMF).
[10]
Orthodontic resin has been used for fixation of
mandibular fractures in children.
[2]
Orthodontic rubber elastics in combination with fixed
orthodontic brackets were used to create compressive
horizontal force marginally over the mandibular fracture
site from one side to the other.
[2]
A modified orthodontic splint appliance has been applied
to fractures where two orthodontic bands are fit on the
primary second molars with rounded stainless steel arch
wires soldered to them on the buccal and lingual side.
[11]
The most common pediatric mandibular fracture: Greenstick
fractures
A greenstick fracture is a fracture in which one cortex of
the bone is broken and the other cortex is bent. Pediatric
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 294
John et al.: Addressing the need for long term follow up after treatment of mandibular fractures in growing children
patients are more likely than adults to sustain greenstick
or incomplete fractures. The relatively high elasticity of the
mandibular bodys thin cortical bone and a thick surrounding
layer of adipose tissue and the relatively larger amount of
medullary bone held by a strong periosteal support results
in a high incidence of greenstick fractures in children.
[5]
A greenstick fracture will ensure stability of the undisplaced
segments in children less than 5 years.
[5]
Furthermore, the
osteogenic potential of the periosteum in the developing
craniofacial skeleton is very high and will lead to somewhat
rapid and easier healing which occurs under the influence of
masticatory stress, even when there is imperfect apposition
of bone surfaces.
[12]
Thus, there is a greater degree of
tolerance permissible in the alignment of fragments and
restoration of occlusion, which will subsequently be corrected
by alveolar bone growth at the time of eruption of permanent
teeth.
[5]
Therefore, management of greenstick fractures
without displacement and malocclusion would merely be
close observation, a liquid-to-soft diet, and avoidance of
physical activities (e.g. sports and analgesics).
[4]
There may
be cases in which the fractures can be snapped back into a
good reduced position and held by the periosteal sleeve, the
fracture surfaces and even by the occlusion.
[5]
For greenstick/
minimally displaced fractures, conservative closed reduction
is the most recommended treatment.
[9]
The closed reduction and immobilization approach can
be achieved by means of acrylic splints, circumferential
wiring, arch bar or gunning splints.
[9]
These techniques
provide a good reduced position, continuity of periosteal
sleeve and maintenance of the soft tissue, thus creating a
positive environment for rapid osteogenesis and remodeling
processes as well as prevention of any type of non-fibrous
union.
[12]
Furthermore, in the splinted mandible, the fracture
segments are tightly fixed and serve in reducing tenderness
and pain reactions during a childs daily activity.
[12]
Open reduction management of mandibular body fractures
in children
Till the mid-seventies, closed reduction by means of IMF
was used for all types of pediatric fractures.
[12]
Today, open
reduction and rigid internal fixation (ORIF) has become the
standard of care for management of displaced fractures.
[4]
ORIF includes micro or miniplates or biodegradable devices
which significantly increase the therapy related risks
previously mentioned. Nonetheless, this technique provides
stable three-dimensional reconstruction, promotes primary
bone healing and shortens treatment time. Posnick et al,
[6]
claimed that a decreased dependence in IMF improved
postoperative respiratory care, nutritional intake and oral
hygiene measures.
The treatment modality for displaced mandibular fractures
is debatable between closed reduction and open reduction.
While different open reduction techniques have been the
standard of care for adults for a long time, its suitability for
children remains controversial.
[5]
The effect of implanted
hardware in the mandible of a growing child is not completely
understood. Damage to the periosteum and surrounding soft
tissues and potential damage to primary teeth and permanent
tooth gums is to be considered when choosing internal
fixation.
[6,7]
Rigid internal fixation might create artifacts on
CT scans or magnetic resonance imaging (MRI) and may be
visible or palpated through the childs thin skin and cause
pain and early or late infection.
[4]
Therefore, the decision to use ORIF in children should be
taken with great caution and only if other means of reduction
and fixation are not attainable. Miniplate and screw devices
have revolutionized the modern management of facial
fractures by enabling precise anatomical reduction and
fixation under direct vision.
Problems with ORIF in pediatric trauma
Presence of developing tooth germs, though the inferior
border of the mandible can be plated either through an
intraoral/extraoral approach. Additionally, the extraoral
approach carries the risk of scarring and damage to the
marginal mandibular nerve.
[5,7]
Interference with growth due to placement of miniplates.
[5]
General anesthesia and hospitalization is needed for
removal of the hardware after complete healing.
[2]
Allergic reactions to the metal resulting in inflammation
that needs removal of plate have been reported.
[2]
Stress shielding, especially after rigid plate fixation, has
been reported and may cause weakening of the bone
after removal of the implant.
[2]
Corrosion and release of metal ions can lead to removal
of the fixation device.
[2]
Recent advances in ORIF
Currently, ORIF with resorbable osteosynthesis plates
and screws is increasingly being used in children. These
biodegradable materials do not interfere with radiodiagnostic
techniques due to their radiolucency and they are sufficiently
rigid and stable. They eventually degrade, resorb and are
eliminated from the body. Although the secondary implant
removal operations are avoided and there are no side effects
on the growing skeleton, the risk of damaging tooth buds
in the pediatric jaw is still present due to drilling for direct
application of the resorbable plates and screws.
[2]
Eppley
[2]
claims that this risk is minimal since the drill hole and the
tapping of the screw penetrate only the outer cortex of the
bone. Even if the resorbable screw tip encroaches upon
a tooth, its tip is blunt and non-penetrating. Subsequent
resorption of the screw removes any potential obstruction
to tooth eruption.
Despite the above reports, the literature advocates
conservative management of mandibular body fractures
at young ages with the added advantage of decreased
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 295
John et al.: Addressing the need for long term follow up after treatment of mandibular fractures in growing children
immobilization time, decreased muscular atrophy and better
oral hygiene.
[2]
Complications
Complications per se are very rare in pediatric trauma due
to the childs greater osteogenic potential, faster healing
rate and less frequent requirement of ORIF. Furthermore, a
greater number of fractures are minimal to non-displaced.
Late complications such as damage to permanent teeth
may occur in 50% of mandibular fractures. TMJ dysfunction
(recurrent subluxation, noise and pain, limited condylar
translation, deviation on opening, ankylosis) and growth
disturbances (e.g. secondary mid face deformity, mandibular
hypoplasia and asymmetry) usually occur in pediatric patients
with severely comminuted fractures.
[2,7]
Malocclusion as a complication of pediatric facial fractures is
rare. It has been attributed to short fixation time in alveolar
fractures and may be caused by growth abnormalities
following condylar fractures.
[3]
Spontaneous correction of
malocclusion is seen as deciduous tooth shed and permanent
teeth erupt.
[7]
Ellis et al,
[2]
did not find occlusal complication
associated with the use of closed treatment and IMF.
Lois et al,
[2]
found no difference in the complication rates
of fractures treated by MMF versus ORIF (4.3% and 5.45%,
respectively). They concluded that in fractures with
displacement in the range of 24 mm, there is no difference
between MMF and ORIF.
A recent study of mandibular fracture complications in
children
[2]
noted a lower complication rate (9.1%) with closed
treatment of mandibular body, angle and parasymphyseal
fractures, while open reduction using miniplate, mandibular
plate and mandibular/miniplate fixation revealed a higher
rate of complication (30%, 28.6% and 29.2%, respectively).
Infection and wound dehiscence occur less frequently with
closed versus open.
Nonunion occurs significantly less often in closed reduction
than in open treatment. Nonunions of the mandible may
develop due to a number of factors, including poor patient
compliance with postoperative care, metabolic disturbances
and generalized disease states, which can all lead to
inadequate bone healing.
[2]
Other local causes for non union
may be related to inadequate immobilization of fracture
segments, infections at the fracture site, tissue or foreign
body between the segments and the inadequate reduction
the fracture segments.
[2]
However, Ellis et al,
[2]
found lower complication rates
in patients with comminuted mandibular fracture, who
underwent open reduction and fixation (10.3%) than in those
who were treated with closed reduction with IMF (17.1%).
Yerit et al,
[2]
found uneventful healing and no complications
when using resorbable osteosynthesis plates and screws for
ORIF, while others described the same type of complications
as mentioned for non-resorbable miniplates infections due to
mucosal exposure of the plates, premature occlusal contact
and TMJ disorders.
[2]
Long-term follow-up on facial and teeth development
A long-term follow-up period is recommended postoperatively
in cases of mandibular body fractures in children.
[8]
Facial
growth pattern and mandibular movements should be
recorded. Ranta and Ylipaavalniemi
[2]
pointed out that teeth
in which root development has already begun at the time
of fracture, appear to erupt normally; however, marked
deformation of the crown and roots occur in teeth located
on the fracture line when the calcification process is still in
progress at the time of fracture.
Developmental disturbances occur in the lower tooth buds
at the pre-calcification stages involved in the fracture and
internal fixation site, which include damage to the pulp
causing pulp obliteration and extensive root resorption
as well as impaction. Koenig et al,
[2]
pointed out that the
developing follicle is more elastic than the surrounding bone
and better able to survive mechanical injury. Nevertheless,
it is difficult to predict the facts of tooth buds and fracture
and the implanted hardware fixation.
Suei et al,
[2]
mentioned that the presence of infection in the
fracture site is a crucial factor affecting odontogenic cells in
the dental follicle. Surgical procedures as well as fixation and
reduction are also potential causes of impaction. Eleonora
Schiller et al,
[13]
report that trauma occurring between 0
and 3 years of age is likely to disturb the formation and
mineralization of the permanent teeth.
Nixon and Lowey
[2]
concluded that mandibular fractures
which occur during mixed dentition can be associated with
subsequent failed eruption of permanent teeth when the
fracture line is reduced using an open surgical approach.
Yocheved Ben Bassat et al,
[14]
reported discoloration of the
crown of permanent tooth in 16% of the children with the
incisal one third being the most common site. Hypoplasia
was evident in 9% of the permanent teeth.
In our case, the deciduous teeth seem to have aligned well
over a period of 2 months, thereby closing the spacing initially
seen between the teeth. We opted for the open occlusal acrylic
splint because of its ease in lab fabrication, preservation of
periodontal tissue integrity, patient compliance and ease in
assessing the occlusion after reduction.
Conclusion
The anatomical complexity of the developing mandible and
teeth and concerns regarding biocompatability of implanted
hardware often mandate the use of surgical techniques
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Contemporary Clinical Dentistry | Oct-Dec 2010 | Vol 1| Issue 4 296
John et al.: Addressing the need for long term follow up after treatment of mandibular fractures in growing children
that differ markedly from those used in adults. In cases of
mandibular fractures of a young child, disruption of periosteal
envelope may have unpredictable effects on growth. Thus,
if intervention is required, closed reduction is favored.
Due to the technical difficulties of IMF, acrylic splints with
circumferential wiring are recommended.
References
1. Tandon S. Textbook of Pedodontics. 1st ed. Hyderabad: Paras
Medical Publisher; 2001. p. 490.
2. Aizenbud D, Hazan-Molina H, Emodi O, Rachmiel A. The
management of mandibular body fractures in young children.
Dental Traumatol 2009;25:565-70.
3. McGraw BL, Cole RR. Pediatric maxillofacial trauma, age
related variations in injury. Arch Otolaryngol Head Neck Surg
1990;116:41-5.
4. Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures,
recent advances in prevention, diagnosis and management. Int
J. Oral Maxillofacial Surg 2006;35:2-13.
5. Crean ST, Sivarajasingam V, Fardy MJ. Conservative approach
in the management of mandibular fractures in the early dentition
phase: A case report and review of the literature. Int J Pediatr
Dent 2000;10:229-33.
6. Posnick JC, Wells M, Pron GE. Pediatric facial fractures: Evolving
patterns of treatment. J Oral Maxillofacial Surg 1993;51:836-44;
discussion 44-5.
7. Kaban LB. Diagnosis and treatment of fractures of the facial bones
in children 1943-1993. J Oral Maxillofacial Surg 1993;51:722-9.
8. Kocabay C, Atac MS, Oner B, Gungor N. The conservative
approach of pediatric mandibular fractures with prefabricated
surgical splint: A case report. Dent Traumatol 2007;23:247-50.
9. Laster Z, Musaka EA, Nagler R. Pediatric mandibular fractures:
Introduction of a novel therapeutic modality. J Trauma 2008;64:
225-9.
10. Magennis P, Craven P. Modication of orthodontic brackets for use
in intermaxillary xation. Br J Oral Maxillofac Surg 1990;28:136-7.
11. Aizenbud D, Emodi O, Rachmiel A. Nonsurgical orthodontic
splinting of mandibular fracture in a young child: 10-year follow-up.
J Oral Maxillofac Surg 2008;66:575-7.
12. Rowe NL. Fracture of the jaws in children. J Oral Surg
1969;27:497-507.
13. Schiller E, Bratu E, Bratu C, Talpos M. Traumatic injuries to the
primary teeth and their impact on permanent teeth. Timisoara
Medical Journal 2003. p. 2.
14. Ben Bassat Y, Fuks A, Brin I, Zilberman Y. Effect of trauma
to the primary incisors on permanent successors in different
development stages. Pediatr Dent 1985;7:37-40.
Source of Support: Nil, Conict of Interest: None declared.
[Downloadedfreefromhttp://www.contempclindent.orgonThursday,July18,2013,IP:164.100.31.82]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Вам также может понравиться
- 3123 PDFДокумент4 страницы3123 PDFTrefina PranaОценок пока нет
- InTech-Epidemiology and Risk Factors of Periodontal DiseaseДокумент18 страницInTech-Epidemiology and Risk Factors of Periodontal DiseaseTrefina PranaОценок пока нет
- Wired For Learning - Orthodontic Basics: Lori Garland Parker, BS, MAOM, RDAEF, CDA, COAДокумент27 страницWired For Learning - Orthodontic Basics: Lori Garland Parker, BS, MAOM, RDAEF, CDA, COATrefina PranaОценок пока нет
- 44 PodjДокумент8 страниц44 PodjTrefina PranaОценок пока нет
- Cnsv8n1 - 3q1497 Enamel MicroabrasionДокумент6 страницCnsv8n1 - 3q1497 Enamel MicroabrasionTrefina PranaОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
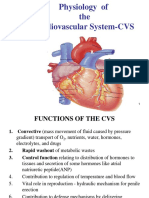
- Physiology of The Cardiovascular System-CVSДокумент56 страницPhysiology of The Cardiovascular System-CVSAmanuel MaruОценок пока нет
- Philippine Dental Association Covid 19 Monitoring FormДокумент1 страницаPhilippine Dental Association Covid 19 Monitoring Formrhusolano rhusolanoОценок пока нет
- Trilemma Adventures BestiaryДокумент17 страницTrilemma Adventures BestiaryZamak50% (2)
- 5a - Osteology of Thorax - Intercostal SpacesДокумент68 страниц5a - Osteology of Thorax - Intercostal SpacesINTERNET MONEY HACKОценок пока нет
- 1 Slide BiasaДокумент19 страниц1 Slide BiasaFransiska Padma Dewi100% (1)
- Acute Coronary Syndrome: An Essential & Practical ApproachДокумент35 страницAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiОценок пока нет
- Spina Bifida PresentationДокумент11 страницSpina Bifida Presentationapi-242435091Оценок пока нет
- Biology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Документ3 страницыBiology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Anonymous WDvB6A0Оценок пока нет
- The Tonsils (Waldeyer's Ring) - Lingual - Pharyngeal - Palatine - Tubal - TeachMeAnatomyДокумент4 страницыThe Tonsils (Waldeyer's Ring) - Lingual - Pharyngeal - Palatine - Tubal - TeachMeAnatomywachito ricoОценок пока нет
- Mother's Class BFДокумент55 страницMother's Class BFriz04_fortitudessa5178Оценок пока нет
- WT Classifieds 230714Документ5 страницWT Classifieds 230714Digital MediaОценок пока нет
- NazeerДокумент23 страницыNazeerDrGurinder KanwarОценок пока нет
- History of Leprosy in MaltaДокумент5 страницHistory of Leprosy in MaltacoleiroОценок пока нет
- AP Psychology Chapter 2 Study Guide (W/ Answers)Документ24 страницыAP Psychology Chapter 2 Study Guide (W/ Answers)JeremiahUmaleОценок пока нет
- Tropical Medicine: Departement of Parasitology Faculty of Medicine USUДокумент40 страницTropical Medicine: Departement of Parasitology Faculty of Medicine USUSartika NapitupuluОценок пока нет
- FELINE-Upper Airway Obstruction in CatsДокумент11 страницFELINE-Upper Airway Obstruction in Catstaner_soysuren100% (1)
- ParaphrasingДокумент12 страницParaphrasingXia U Rong100% (1)
- The Endocrine SystemДокумент12 страницThe Endocrine Systemmagma_pt9888Оценок пока нет
- AppendicitisДокумент8 страницAppendicitisPhoebe Corazon Cercado100% (1)
- 1-1 Animal Vaccine Business Opportunity With CavacДокумент34 страницы1-1 Animal Vaccine Business Opportunity With CavacFamar HiveОценок пока нет
- Marine Science - Marine WormsДокумент20 страницMarine Science - Marine Wormssgw67Оценок пока нет
- Useful Phrases For Sensational WritingДокумент3 страницыUseful Phrases For Sensational WritingNor Azizah BachokОценок пока нет
- Digestive System of GoatsДокумент4 страницыDigestive System of Goatssoliun2556100% (2)
- Bowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreДокумент58 страницBowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreMariajanОценок пока нет
- Physical DiagnosisДокумент97 страницPhysical Diagnosisaxmedfare138Оценок пока нет
- Power Taiji Vol 1Документ99 страницPower Taiji Vol 1English Teaching100% (3)
- Diagnostic MethodsДокумент93 страницыDiagnostic MethodsSyukri La Ranti100% (3)
- Maternal Ob NotesДокумент37 страницMaternal Ob Notesshenric16Оценок пока нет
- Viral ZoonosesДокумент12 страницViral ZoonosesGeriel QuidesОценок пока нет
- Portal HypertensionДокумент4 страницыPortal HypertensiondrstalamОценок пока нет