Академический Документы
Профессиональный Документы
Культура Документы
The Future of Insulin Therapy For Patients
Загружено:
Mike zombieИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Future of Insulin Therapy For Patients
Загружено:
Mike zombieАвторское право:
Доступные форматы
S29 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No.
4 | Supplement 2
From the Albert Einstein College of
Medicine in Flushing, New York.
This article is based on a continuing
medical education symposium held
on October 10, 2012, during the
American Osteopathic Associations
2012 annual Osteopathic Medical
Conference & Exposition in
San Diego, California. This article was
developed with assistance from
Global Directions in Medicine.
The author has approved
the article and all of its content.
Financial Disclosures:
Dr Tibaldi is on the speakers
bureaus for Daiichi Sankyo Company,
Merck & Co, Inc, and Novo Nordisk Inc.
He is also a consultant for
Novo Nordisk Inc.
Address correspondence to
Joseph M. Tibaldi, MD,
Queens Diabetes and
Endocrinology Associates,
59-45 161st St,
Flushing, NY 11365-1414.
E-mail: jtibaldi@aol.com
The Future of Insulin Therapy for Patients
With Type 2 Diabetes Mellitus
Joseph M. Tibaldi, MD
Insulin therapy has been the mainstay of therapy for patients
with type 2 diabetes mellitus for the past 90 years. This trend
is likely to continue as new formulations are developed to more
closely mimic physiologic insulin secretion and to provide
patients who have diabetes with more convenient options for
integrating this therapy into their lifestyle. The present article
reviews how the role of insulin continues to evolve, from its
earlier use in the treatment paradigm (even at frst diagnosis)
to its role in combination therapy with incretin-based thera-
pies, as well as new formulations that provide more-convenient
forms of insulin replacement therapy.
J Am Osteopath Assoc. 2013;113(4 suppl 2):S29-S39
S30 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
patients with T2DM, the normal post-
prandial suppression of glucagon secre-
tion is inadequate, leading to increased
hepatic glucose output that worsens
hyperglycemia. In turn, chronic hyper-
glycemia leads to glucose toxicity that
paradoxically results in reduced syn-
thesis and secretion of insulin.
6
Native
glucagon-like peptide-1 (GLP-1) is an
incretin hormone secreted by the gut
that normally slows gastric emptying,
acts on the pancreas to stimulate glu-
cose-dependent insulin secretion, and
suppresses the release of glucagon.
7
Incretin deficits or incretin resistance
may result in the abnormal regulation
of insulin and glucagon secretion that
characterizes T2DM.
8
Like insulin, GLP-1
and glucagon are important targets of
pharmacologic treatment strategies for
improving glycemic control.
9
Use of Insulin Therapy
Early in the T2DM
Treatment Paradigm
Insulin remains integral to the treatment
of patients with diabetes.
10
For patients
with T1DM, insulin therapy is essential
and lifesaving. For patients with T2DM,
use of insulin therapy was formerly
relegated to use during later stages of
the disease. This approach is being
reexamined as more recent treatment
paradigms encourage earlier use of in-
sulin treatment algorithms for patients
with T2DM.
11
On the basis of guidelines
from the American Association of Clini-
cal Endocrinologists, insulin therapy
clearly is recommended for patients
with severe hyperglycemia and for pa-
cated and patient-friendly agents.
2
The
present review article discusses ini-
tiation of insulin replacement therapy at
the time of diagnosis, basal insulin ther-
apy used in combination with incretin
therapy, and second-generation basal
insulin analog therapy, using a case
study to demonstrate clinical applica-
tion. Other means of enhancing delivery
of insulin to patients are also discussed.
Pathophysiologic
Profle of T2DM Drives
Treatment Choices
Insulin is instrumental in managing T2DM,
which is a complex, multihormonal, and
progressive chronic disease.
3
Our ap-
proach to the treatment of patients with
T2DM requires an understanding of the
pathophysiologic profle of this condition
to determine when and how to use the
many pharmacologic agents available.
Type 2 diabetes mellitus results from
the abnormal secretion or abnormal
actions of key hormones that regulate
glucose production by the liver and glu-
cose uptake in the peripheral muscle
and adipose tissue. In patients with
established T2DM, insulin secretion is
reduced because of progressive loss
of pancreatic -cell function.
4
Plasma
glucose levels increase as insulin
defciency and insulin resistance reduce
normal insulin activity, leading to dimin-
ished stimulation of peripheral glucose
uptake and decreased inhibition of he-
patic glucose production.
5
Glucagon normally helps maintain
fasting plasma glucose levels by stim-
ulating hepatic glucose production. In
T
he number of patients with type
2 diabetes mellitus (T2DM) far
exceeds the number of endo-
crinologists and diabetes specialists
available to treat them. The majority
of patients are treated in primary care
environments, and by virtue of the com-
mon comorbidities that travel with
diabetes, including hypertension, dys-
lipidemia, and obesity or overweight,
comprehensive and holistic approaches
to care are required. Osteopathic physi-
cians are likely to encounter more and
more such patients in their practices. As
a result of improvements in health care
and increases in longevity, patients are
more likely to require insulin therapy at
some point during the progression of
T2DM. With advances in insulin therapy
still occurring, it is well worth keeping
up to date on trends in the use of this
powerful glucose-lowering agent.
Patients with T2DM are insulin resis-
tant, have relatively low insulin produc-
tion, or have both characteristics. Most
patients with T2DM eventually require
insulin if other medications fail to control
their blood glucose levels adequately.
1
Insulin replacement therapy lets pa-
tients know that a key component of
their natural glucose-regulating system
is being restored. When insulin replace-
ment therapy was introduced more than
90 years ago,
2
it was a lifesaving option
for patients with type 1 diabetes mellitus
(T1DM), even though the formulations
used were relatively crude. During past
decades, major advances in our abil-
ity to synthesize more reproducible and
physiologic formulations have enabled
the production of much more sophisti-
S31 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
tients receiving oral antidiabetic drugs
who have glycated hemoglobin (HbA
1c
)
levels greater than 9%.
12
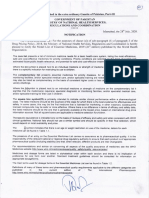
Of particular interest are data as-
sessing the use of insulin as a frst-line
treatment option for T2DM, often in pa-
tients who initially have very high levels
of glucose toxicity. This treatment op-
tion was reviewed by Rolla
13
in 2009,
and additional data have since been
published. Several studies
14-16
have
shown prolonged remission of T2DM
in patients receiving intensive insulin
therapy for 2 weeks. A 2- to 3-week
course of intensive insulin therapy can
lay the foundation for prolonged good
glycemic control in patients with newly
diagnosed T2DM who have elevated
fasting glucose levels. Figure 1 shows
an example of the effects of short-term
intensive insulin therapy on glucose and
insulin levels.
14
In a more recent study, the use of
low-dose insulin therapy (given as pre-
mixed insulin in one study) for patients
with newly diagnosed T2DM led to evi-
dence of -cell recovery, as document-
ed by plasma insulin and C-peptide lev-
els.
17
It appears that reversing glucose
toxicity may result in a rapid improve-
ment in -cell function, which then al-
lows the cell to start to function and
to secrete adequate amounts of insulin
for clinically signifcant periods of up to
1 year.
14-16
This series of events is also
known as a second-wind phenomenon
for the cell.
13
After symptom relief oc-
curs and glucose levels are normalized
in such patients, oral agents often can
be added to therapy, and it may be pos-
sible to withdraw insulin.
G
l
u
c
o
s
e
,
m
g
/
d
L
I
n
s
u
l
i
n
,
p
m
o
l
/
L
420
360
270
180
90
0
600
500
400
300
200
100
0
Time, min
Time, min
0 30 60 90 120 150 180
0 30 60 90 120 150 180
Before insulin therapy
Immediately after insulin therapy
1 year after insulin therapy
1 year after insulin therapy
Immediately after insulin therapy
Before insulin therapy
Figure 1.
Glucose and insulin levels before insulin therapy, immediately
after insulin therapy, and 1 year after insulin therapy,
demonstrating the effects of short-term intensive insulin therapy
in patients with newly diagnosed type 2 diabetes mellitus.
14
Reprinted with permission from the American Diabetes
Association, from Ryan EA, Imes S, Wallace C. Short-term
intensive insulin therapy in newly diagnosed type 2 diabetes
mellitus. Diabetes Care. 2004;27(5):1028-1032; permission
conveyed through Copyright Clearance Center, Inc.
S32 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
Harry, 2-Year Follow-Up
Harrys diabetes treatment regimen
now includes basal insulin as well as
metformin. During the 2 years since
Harry was frst seen in the physicians
offce, he has been self-titrating his bas-
al insulin and has generally been able
to keep his HbA
1c
level at less than 7%.
However, despite engaging in exercise
on a relatively consistent basis, he has
gained 11 lbs. For the past 6 months,
however, his HbA
1c
level has been
8.3%, in spite of fasting blood glucose
levels between 90 and 115 mg/dL.
Harrys goal is to once again attain an
HbA
1c
level of less than 7%.
Many patients who receive basal
insulin therapy will ultimately require
treatment intensifcation. Notably, the
HbA
1c
level reflects not only fasting
blood glucose levels but also postpran-
dial glucose levels.
19
Adding a sulfonyl-
urea to insulin-based therapy increases
the risk of hypoglycemia without pro-
viding much benefit. Sulfonylureas
also lower fasting glucose levels much
more than postprandial glucose levels,
so they may not be the best treatment
option for Harry. At this point, the clini-
cal decision traditionally is to switch to
a premixed insulin or move toward a
basal-bolus regimen (which is often
done by sequentially adding prandial
insulin before meals as needed and as
tolerated).
11,20-22
This clinical decision
is certainly a well-validated and effec-
tive treatment strategy, but there are
drawbacks for some patientsnamely,
an increased risk of hypoglycemia,
weight gain, and number of complica-
tions for patients in terms of the number
thinking that he might have diabetes.
After talking with the owner, Harry real-
ized that he had unquenchable thirst.
He promptly made an appointment to
see his primary care physician, even
though he had been negligent in doing
so for the past year.
The findings from Harrys visit to
his physician were notable. He had a
weight loss of 15 lbs, a nonfasting glu-
cose level of 430 mg/dL, an HbA
1c
level
of 12%, and trace levels of ketone bod-
ies in his urine sample. Insulin replace-
ment therapy was recommended as
initial treatment.
In Harrys case, insulin therapy was
clearly indicated. He had T2DM, clini-
cally significant hyperglycemia, and
signs of catabolism (weight loss), and
no oral agent or other noninsulin agent
would begin to bring him close to his
goal HbA
1c
level. Pathophysiologic fnd-
ings revealed that his liver was secret-
ing excess glucose that was unable to
enter the muscle. His problematic glu-
cose levels occurred in part because
Harry has diminished insulin levels.
However, it also occurred because Har-
ry has a GLP-1 deficit, and because,
with that defcit, he was producing too
much glucagon.
It is gratifying to treat a patient like
Harry, who arrives at the offce feeling
poorly but who, after approximately 3 to
6 months, is in much better health and
can have blood glucose levels that are
close to normal. Chronic hyperglycemia
leads to reduced insulin secretion
(Figure 2).
6
By reversing glucotoxicity,
it is possible for the body to resume
insulin secretory capacity.
Other recent data show that -cell
function can be preserved for at least
3.5 years with the use of early and in-
tensive T2DM therapy involving admin-
istration of either insulin plus metfor-
min or triple oral therapy after an initial
3-month period of insulin-based treat-
ment.
18
These data support the premise
that insulin should not be relegated to
use as a last-line therapy but, rather,
could be used earlier in the disease
paradigm, when some -cell function
remains intact. Insulin therapy can be
discontinued in patients who have early
disease, and it can be restarted when
necessary or continued in conjunction
with other oral agents or GLP-1 recep-
tor agonists.
Case Study
Harry
Harry is a 52-year-old man who, for the
past 6 months, has been struggling with
a new job that has required his attention
during most of his waking hours. His
past medical history includes hyperten-
sion, for which he takes a diuretic, and
mixed hyperlipidemia managed with a
modest dose of a statin.
Harry has been fastidious in taking
his medications, but his job keeps him
at his desk most of the time. His only
exercise is walking to the local fast food
restaurant where he buys most of his
meals. The owner of the restaurant
noted that Harry was returning more
frequently and buying more juice and
soda. The owners wife had diabetes,
so the owner gently questioned Harry
about his thirst levels and weight loss,
S33 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
lower postprandial glucose levels, with
a low associated risk of hypoglycemia
and without weight gain (an advan-
tage over prandial insulin analogs).
28-33
However, basal insulin doses may need
to be adjusted downward or sulfonyl-
ureas may need to be discontinued.
34
Table 1 provides a summary of some
of the available published literature on
DPP-4 inhibitors used in combination
with insulin therapy.
28,29,35
The use of GLP-1 agonists in com-
bination with insulin therapy for post-
prandial glucose control also may
result in some weight loss.
33
Some
clinicians prefer to start with a GLP-1
agonist or an incretin-based therapy
early in the treatment paradigm, before
initiating insulin.
36,37
effcacy in lowering glucose levels.
24-27
The beneft of using these approaches
is that incretin-based therapies work
in a glucose-dependent manner (ie,
only in the presence of hyperglycemia).
They also are weight neutral (dipepti-
dyl peptidase-4 [DPP-4] inhibitors) or
are associated with weight loss (GLP-1
receptor agonists).
Currently, DPP-4 inhibitors, as well
as both liraglutide and short-acting
exenatide, are approved for use with
long-acting basal insulin analogs in pa-
tients with T2DM who are not achiev-
ing their goals for glycemic control. In-
cretin-based therapies primarily target
postprandial hyperglycemia (although
longer-acting GLP-1 agonists also af-
fect fasting plasma glucose levels) and
of injections needed and the complex-
ity of titrating both basal and prandial
insulin doses.
23
Basal Insulin Therapy
in Combination With
Incretin-Based Therapy
Another approach used to augment
insulin therapy is to add incretin-based
agents to the treatment regimens of
patients who are receiving basal in-
sulin therapy but who are no longer
achieving treatment goals. Although
these approaches are similar, they
have important differences (Figure 3).
9
Glucagon-like peptide-1 receptor ago-
nists provide supraphysiologic levels of
the incretin hormone and have greater
Chronic
hyperglycemia
PDX-1 activity
Glucose
Glucokinase activity
Insulin biosynthesis Insulin secretion
Oxidative stress (ROS)
Pancreatic cell
Figure 2.
The mechanism of insulin secretion reduction caused by glucose toxic effects.
The binding capacity of PDX-1 decreases as a result of oxidative stress caused
by hyperglycemia, while insulin biosynthesis and secretion also decrease.
Reprinted from Kawahito et al.
6
Abbreviations: PDX-1, pancreatic duodenal
homeobox-1; ROS, reactive oxidative species.
S34 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
Case Study Revisited
Harry Follow-Up
Harry was presented with options to
help him return to his goal HbA
1c
level of
7%. A DPP-4 inhibitor would be a sim-
ple treatment option but would not al-
low him to attain this goal. A successful
treatment option that could achieve this
goal is the addition of prandial insulin
injections at mealtimes.
Harry was also concerned about
losing weight, so it was decided to use
GLP-1 receptor agonists. Because Har-
ry was traveling a great deal and eat-
ing at irregular times (usually at a res-
taurant), he wanted a simple treatment
plan that involved the least number of
injections and a medication that did not
require strict dosing in relation to meals.
Therefore, once-daily liraglutide was se-
lected. Liraglutide is administered once
daily, without regard to mealtime, but it
Table 2.
Comparison of Onset, Peak, and Duration of Longer-Acting Basal Insulins
Basal Insulin Onset Peak Duration
Neutral protamine 1-2 h 4-8 h 8-12 h
Hagedorn
Glargine 30-60 min Relatively peakless 16-24 h
Detemir 30-60 min Relatively peakless 16-24 h
Degludec 30-90 min Peakless >24 h
Source: Reprinted from Nasrallah SN, Reynolds LR. Insulin degludec, the new generation basal insulin
or just another basal insulin? Clin Med Insights Endocrinol Diabetes. 2012;5:31-37.
38
Copyright 2012,
with permission from Libertas Academica Ltd.
Table 1.
Outcomes of Select Studies of Dipeptidyl Peptidase-4 Inhibitors
in Combination With Insulin Over 24 Weeks Duration
Source Agent Comparison Patients Outcome
Hong et al, Sitagliptin Add-on to insulin vs Patients with T2DM (n=140); Compared with a 25% increase
2012
28
an insulin dose increase baseline HbA
1c
level, 9.2% in the insulin dose, adding
sitagliptin to an insulin-based
regimen was more effective
at lowering HbA
1c
levels and
was associated with less
hypoglycemia and weight gain
Barnett et al, Saxagliptin Insulin alone or insulin Patients with T2DM (n=455); Addition of saxagliptin improved
2012
35
plus metformin, addition baseline HbA
1c
level, glycemic control and was
of saxagliptin vs placebo 7.5% to 11% generally well tolerated
Vilsboll et al, Sitagliptin Add-on to basal or Patients with T2DM (n=451); Addition of sitagliptin improved
2010
29
premixed insulin vs baseline HbA
1c
level, glycemic control and was
placebo 7.5% to 11% generally well tolerated
Abbreviations: HbA
1c
, glycated hemoglobin; T2DM, type 2 diabetes mellitus.
S35 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
using the insulin pen. At that visit,
mild nausea had occurred; however,
it abated 3 weeks later. Harry had a
weight loss of 5 lbs, and he noted that
his fasting blood glucose level was still
between 80 and 120 mg/dL.
The next follow-up visit occurred af-
ter Harry had been receiving the new
medication for 12 weeks. At that time,
he had lost an additional 4 lbs, and his
HbA
1c
level was 6.8%.
What Else Is New?
Ultra-Long-Acting Basal
Insulin in Development
Current research efforts are focusing
on improving the pharmacokinetics and
pharmacodynamics of long-acting insu-
lin analogs to make them even less vari-
able and longer acting (ie, make them
truly once-daily insulin analogs). These
GLP-1 receptor agonists, the need for
lower doses of insulin has been ob-
served. There also is the possibility
that patients may transiently eat less if
nausea is problematic, which may in-
crease the possibility of insulin-related
hypoglycemia developing. Furthermore,
by means of mechanisms independent
of adverse gastrointestinal effects, pa-
tients treated with GLP-1 receptor ago-
nists experience greater satiety than
placebo-treated patients, and their food
intake may decrease.
Harry already knew how to use an
insulin pen delivery device, so he was
told to start with a dose of 0.6 mg of
insulin given subcutaneously daily.
One week later, Harry increased the
insulin dose to 1.2 mg given subcuta-
neously daily.
A follow-up appointment was sched-
uled for 6 weeks after Harry started
should be administered at approximate-
ly the same time each day, if possible.
Short-acting exenatide is administered
twice daily before meals. It should be
noted that the once-weekly formulation
of exenatide is not currently approved
by the US Food and Drug Administra-
tion (FDA) for use with insulin.
The physician discussed the possi-
bility of nausea occurring in association
with initiation of GLP-1 receptor agonist
therapy. The nausea tends to be mild
to moderate and of a transient nature.
Harry was told that if severe nausea or
abdominal pain were to occur, he would
need to call the physicians offce right
away, because the presence of these
symptoms might be a sign of a more se-
rious condition, such as pancreatitis.
Harrys basal insulin dose was re-
duced by 20%, from 40 U to 33 U, at
night. When basal insulin is used with
Liver
Brain
Muscle
Adipose tissue
Glucose
Native GLP-1
Pancreas
Glucagon
( cells)
Amylin
( cells)
I
n
s
u
l
i
n
(
c
e
l
l
s
)
I
n
s
u
l
i
n
(
c
e
l
l
s
)
Figure 3.
Different approaches to enhancing the effects of the naturally
occurring incretin hormonepharmacologic replacement or minimizing
degradation.
9
Abbreviation: GLP-1, glucagon-like peptide 1.
S36 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
reduced risk of hypoglycemia and more
convenience for the patient.
39,40
Advances have been made in the
clinical development of both insulin
degludec (administered alone or in
combination with insulin aspart) and
pegylated insulin lispro. Insulin de-
analogs at a consistent time each day,
on the basis of their duration of action.
Table 2 provides a comparison of the
pharmacodynamics of longer-acting
insulin analogs.
38
The goal of ongoing
research is to come close to achieving
glycemic control while beneftting from a
longer-acting insulin analogs will be
more forgiving of the busy schedules of
patients, because they have little to no
impact on glucose levels if there is some
variation in the time of administration.
Optimal glycemic benefts are achieved
with the injection of current basal insulin
Table 3.
Published Trials of Ultra-Long-Acting Insulins
Insulin Patient Insulin
Source Agent Characteristics Comparator Design Outcomes
Rosenstock LY2605541 T1DM; basal-bolus Glargine 8-wk randomized, Greater improvements in glycemic
et al, 2013
56
(pegylated therapy phase 2, open-label, control, increased total hypoglycemia,
insulin lispro) 22 crossover study reduced nocturnal hypoglycemia,
reduced weight, and lowered insulin
doses at mealtime
Bergenstal LY2605541 T2DM (HbA
1c
level Glargine 12-wk, randomized, Comparable glucose control; total
et al, 2012
57
(pegylated 10.5%); metformin open-label, phase 2 hypoglycemia rates, reduced intraday
insulin lispro) and/or sulfonylurea study variability, and lower nocturnal hypo-
with glargine or NPH glycemia, as well as weight loss,
insulin once daily relative to glargine
Birkeland Degludec T1DM; mean HbA
1c
Glargine 16-wk randomized, Comparable glucose control at
et al, 2011
43
level 8.4% phase 2 controlled trial similar doses, with reduced rates
of hypoglycemia
Heise et al, Degludec/ T2DM; background Glargine 16-wk, open-label trial Comparable glucose control at
2011
45
aspart metformin therapy similar doses, similar low rates
of hypoglycemia, and better
glucose control after dinner
Zinman et al, Degludec T2DM; background Glargine 1-year treat-to-target, Comparable glucose control,
2012
50
therapy for OAD; open-label, randomized much lower rates of nocturnal
baseline HbA
1c
level trial hypoglycemia
7% to 10%
Heller et al, Degludec T1DM; basal-bolus Glargine 1-year treat-to-target, Comparable glucose control and
2012
46
insulin therapy; open-label, randomized much lower rates of nocturnal
HbA
1c
level 10% trial hypoglycemia
Garber et al, Degludec T2DM; basal-bolus Glargine 1-year treat-to-target, Comparable glucose control and
2012
44
insulin; HbA
1c
level, open-label, randomized much lower rates of overall and
7% to 10% trial nocturnal hypoglycemia
Niskanen Degludec/ T2DM; HbA
1c
level Biphasic 16-wk, open-label, Comparable glucose control and
et al, 2012
58
aspart (twice 7% to 11% insulin aspart randomized, lower rates of hypoglycemia
daily) and an twice daily treat-to-target trial
alternative
formulation
Abbreviations: HbA
1c
, glycated hemoglobin; NPH, neutral protamine Hagedorn; OAD, oral antidiabetic drugs; T1DM, type 1 diabetes mellitus;
T2DM, type 2 diabetes mellitus.
S37 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
Technosphere insulin (MannKind Cor-
poration, Valencia, California), another
inhaled insulin, was compared with sub-
cutaneous regular human insulin in a
randomized, open-label study of their
effcacy and safety in covering prandial
insulin needs.
54,55
Technosphere insulin
substantially improved postprandial glu-
cose levels and had a more favorable
pharmacodynamic profle than subcuta-
neous regular human insulin. The Tech-
nosphere insulin system is currently
undergoing phase 3 trials.
All of these efforts illustrate the diff-
culty of working with complex proteins,
such as hormones, and highlight the
successes that have been achieved
with current and emerging formula-
tions as they continue through the
approval process.
Oral Insulin
The physiologic barriers of the gastro-
intestinal tract pose a major challenge
for the optimal delivery of any hormone,
including insulin. Oral insulin would pro-
vide a convenient method of adminis-
tration, potentially leading to improved
glycemic control for patients with poor
adherence to subcutaneous insulin
regimens.
2
Conclusion
Development of insulin replacement
therapy is ongoing. Physicians need to
understand the central role of insulin in
the pathophysiologic profle of diabetes,
how it can be used early or late in the
disease process, and how it comple-
ments other agents. As more insulin
tively. Low rates of hypoglycemia were
noted with both regimens. This trial
49
showed that insulin degludec can be
administered at varying times without
resulting in either a loss of glycemic
control or the development of hypogly-
cemia to accommodate changes in a
patients daily schedule.
Another new agent, pegylated in-
sulin lispro, is currently moving into
phase 3 of clinical development. This
agent appears to be associated with
less variability, less nocturnal hypogly-
cemia, perhaps slightly more overall
hypoglycemia (which may be related to
some dosing and titration issues), and
some interesting effects on weight. To
my knowledge, few data on this com-
pound have been published in the peer-
reviewed literature to date.
A summary of available data from
clinical trials is shown in Table 3.
43-46,50
Overall, these exciting developments
may be used by physicians to improve
glycemic control and to increase pa-
tient acceptance of and adherence to
insulin therapy.
Inhaled Insulin
Inhaled insulin has been under devel-
opment for many years, but a product
that actually reached market (Exubera,
an insulin human [recombinant DNA
origin] inhalation powder; Pfzer, New
York, New York) was eventually with-
drawn because of poor market up-
take,
51
perhaps because of the complex
requirements for its administration.
52
Other inhaled insulin agents that have
been investigated have been found
to produce nocturnal hypoglycemia.
53
gludec has been submitted to the FDA
for review. This ultra-long-acting basal
insulin has a fat and stable glucose-
lowering effect,
41
and it is associated
with a much lower risk of nocturnal
hypoglycemia than insulin glargine, as
has been demonstrated in studies of
patients with T1DM and T2DM.
42-47
The
pharmacodynamic variability of insulin
degludec is much lower than that of in-
sulin glargine.
41,48
Insulin degludec has
received an approvable status from an
FDA regulatory panel and has been ap-
proved for use in Europe.
Because insulin degludec has a sta-
ble and prolonged time-action profle,
coupled with low within-subject variabil-
ity, it allows for more-fexible once-daily
dosing. Insulin degludec has a fat and
stable glucose-lowering effect that is not
affected by dose.
48
This concept was
tested in patients with T2DM participat-
ing in a 26-week randomized trial
49
in
which insulin degludec (administered
in variable dosing intervals in a fexible
regimen) was compared with insulin
glargine (administered at the same time
each day). Both insulins were added
to an existing regimen of oral glucose-
lowering therapy, as in the case study
described here, and study patients
were titrated to achieve fasting plasma
glucose levels of less than 90 mg/dL.
The once-daily regimen of insulin de-
gludec involved a compulsory, rotating
morning-and-evening schedule of dos-
ing that created 8- to 40-hour dosing
intervals. From a baseline HbA
1c
level
of 8.4%, HbA
1c
values were reduced by
1.28% and 1.26% with the use of insulin
degludec and insulin glargine, respec-
S38 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
23. Holman RR, Farmer AJ, Davies MJ, et al;
for the 4-T Study Group. Three-year effcacy
of complex insulin regimens in type 2 diabetes.
N Engl J Med. 2009;361(18):1736-1747.
24. Pratley RE, Nauck M, Bailey T, et al; for the
1860-LIRA-DDP-4 Study Group. Liraglutide
versus sitagliptin for patients with type 2
diabetes who did not have adequate glycaemic
control with metformin: a 26-week, randomised,
parallel-group, open-label trial. Lancet.
2010;375(9724):1447-1456.
25. Pratley RE, Nauck MA, Bailey T, et al. Effcacy
and safety of switching from the DPP-4 inhibitor
sitagliptin to the human GLP-1 analog liraglutide
after 52 weeks in metformin-treated patients with
type 2 diabetes: a randomized, open-label trial.
Diabetes Care. 2012;35(10):1986-1993.
26. Bergenstal RM, Wysham C, Macconell L, et al.
Effcacy and safety of exenatide once weekly
versus sitagliptin or pioglitazone as an adjunct
to metformin for treatment of type 2 diabetes
(DURATION-2): a randomised trial. Lancet.
2010;376(9739):431-439.
27. Russell-Jones D, Cuddihy RM, Hanefeld M,
et al; DURATION-4 Study Group. Effcacy
and safety of exenatide once weekly versus
metformin, pioglitazone, and sitagliptin used as
monotherapy in drug-naive patients with type
2 diabetes (DURATION-4): a 26-week double-
blind study. Diabetes Care. 2012;35(2):252-258.
28. Hong ES, Khang AR, Yoon JW, et al.
Comparison between sitagliptin as add-on
therapy to insulin and insulin dose-increase
therapy in uncontrolled Korean type 2
diabetes: CSI study. Diabetes Obes Metab.
2012;14(9):795-802.
29. Vilsboll T, Rosenstock J, Yki-Jarvinen H, et al.
Effcacy and safety of sitagliptin when added to
insulin therapy in patients with type 2 diabetes.
Diabetes Obes Metab. 2010;12(2):167-177.
30. Levin P, Wei W, Wang L, Pan C, Douglas D,
Baser O. Combination therapy with insulin
glargine and exenatide: real-world outcomes
in patients with type 2 diabetes. Curr Med Res
Opin. 2012;28(3):439-446.
31. Lind M, Jendle J, Torffvit O, Lager I. Glucagon-
like peptide 1 (GLP-1) analogue combined with
insulin reduces HbA1c and weight with low risk
of hypoglycemia and high treatment satisfaction.
Prim Care Diabetes. 2012;6(1):41-46.
32. Buse JB, Bergenstal RM, Glass LC, et al.
Use of twice-daily exenatide in basal insulin-
treated patients with type 2 diabetes: a
randomized, controlled trial. Ann Intern Med.
2011;154(2):103-112.
12. Rodbard HW, Jellinger PS, Davidson JA,
et al. Statement by an American Association
of Clinical Endocrinologists/American College
of Endocrinology consensus panel on type 2
diabetes mellitus: an algorithm for glycemic
control. Endocr Pract. 2009;15(6):540-559.
13. Rolla AR. What about insulin as an immediate
frst step for type 2 diabetes? Diabetes Obes
Metab. 2009;11(suppl 5):19-22.
14. Ryan EA, Imes S, Wallace C.
Short-term intensive insulin therapy
in newly diagnosed type 2 diabetes.
Diabetes Care. 2004;27(5):1028-1032.
15. Weng J, Li Y, Xu W, et al. Effect of intensive
insulin therapy on -cell function and glycaemic
control in patients with newly diagnosed type 2
diabetes: a multicentre randomised parallel-
group trial. Lancet. 2008;371(9626):1753-1760.
16. Hu Y, Li L, Xu Y, et al. Short-term intensive
therapy in newly diagnosed type 2 diabetes
partially restores both insulin sensitivity
and -cell function in subjects with
long-term remission. Diabetes Care.
2011;34(8):1848-1853.
17. Bhattacharya S, Ammini AC, Jyotsna V,
Gupta N, Dwivedi S. Recovery of -cell functions
with low-dose insulin therapy: study in newly
diagnosed type 2 diabetes mellitus patients.
Diabetes Technol Ther. 2011;13(4):461-465.
18. Harrison LB, Adams-Huet B, Raskin P,
Lingvay I. -cell function preservation
after 3.5 years of intensive diabetes therapy.
Diabetes Care. 2012;35(7):1406-1412.
19. Monnier L, Lapinski H, Colette C. Contributions
of fasting and postprandial plasma glucose
increments to the overall diurnal hyperglycemia
of type 2 diabetic patients: variations with
increasing levels of HbA1c. Diabetes Care.
2003;26(3):881-885.
20. Hirsch IB. Intensifying insulin therapy
in patients with type 2 diabetes mellitus.
Am J Med. 2005;118(suppl 5A):21S-26S.
21. Jang HC, Guler S, Shestakova M; for the
PRESENT Study Group. When glycaemic
targets can no longer be achieved with
basal insulin in type 2 diabetes, can simple
intensifcation with a modern premixed
insulin help? results from a subanalysis
of the PRESENT study. Int J Clin Pract.
2008;62(7):1013-1018.
22. Meneghini L, Mersebach H, Kumar S,
Svendsen AL, Hermansen K. Comparison
of 2 intensifcation regimens with rapid-acting
insulin aspart in type 2 diabetes mellitus
inadequately controlled by once-daily insulin
detemir and oral antidiabetes drugs: the
step-wise randomized study. Endocr Pract.
2011;17(5):727-736.
products become available, an under-
standing of the relative characteristics,
benefts, and potential of these agents
in helping us to improve glycemic con-
trol in patients currently coping with
unsatisfactory glycemic control cannot
be overstated.
References
1. Best JD, Drury PL, Davis TM, et al. Glycemic
control over 5 years in 4,900 people with
type 2 diabetes: real-world diabetes therapy
in a clinical trial cohort. Diabetes Care.
2012;35(5):1165-1170.
2. Tibaldi JM. Evolution of insulin development:
focus on key parameters. Adv Ther.
2012;29(7):590-619.
3. Defronzo RA. From the triumvirate to the
ominous octet: a new paradigm for the treatment
of type 2 diabetes mellitus [Banting Lecture].
Diabetes. 2009;58(4):773-795.
4. LeRoith D. Beta-cell dysfunction and insulin
resistance in type 2 diabetes: role of metabolic
and genetic abnormalities. Am J Med.
2002;113(suppl 6A):3S-11S.
5. Fanelli CG, Porcellati F, Rossetti P, Bolli
GB. Glucagon: the effects of its excess and
defciency on insulin action. Nutr Metab
Cardiovasc Dis. 2006;16(suppl 1):S28-S34.
6. Kawahito S, Kitahata H, Oshita S. Problems
associated with glucose toxicity: role of
hyperglycemia-induced oxidative stress.
World J Gastroenterol. 2009;15(33):4137-4142.
7. Drucker DJ. The biology of incretin hormones.
Cell Metab. 2006;3(3):153-165.
8. Holst JJ, Deacon CF, Vilsbll T, Krarup T,
Madsbad S. Glucagon-like peptide-1, glucose
homeostasis and diabetes. Trends Mol Med.
2008;14(4):161-168.
9. Drucker DJ. Enhancing the action of incretin
hormones: a new whey forward? Endocrinology.
2006;147(7):3171-3172.
10. American Diabetes Association.
Standards of medical care in diabetes2012.
Diabetes Care. 2012;35(suppl 1):S11-S63.
11. Inzucchi SE, Bergenstal RM, Buse JB, et
al. Management of hyperglycemia in type 2
diabetes: a patient-centered approachPosition
Statement of the American Diabetes Association
(ADA) and the European Association for the
Study of Diabetes (EASD). Diabetes Care.
2012;35(6):1364-1379.
S39 A Supplement to The Journal of the American Osteopathic Association April 2013 | Vol 113 | No. 4 | Supplement 2
53. Moses RG, Bartley P, Lunt H, et al. Safety
and effcacy of inhaled insulin (AERx iDMS)
compared with subcutaneous insulin therapy in
patients with type 1 diabetes: 1-year data from
a randomized, parallel group trial. Diabet Med.
2009;26(3):260-267.
54. Rave K, Heise T, Heinemann L, Boss AH.
Inhaled technosphere insulin in comparison
to subcutaneous regular human insulin: time
action profle and variability in subjects with
type 2 diabetes. J Diabetes Sci Technol.
2008;2(2):205-212.
55. Rave K, Heise T, Pfutzner A, Boss AH.
Coverage of postprandial blood glucose
excursions with inhaled technosphere insulin in
comparison to subcutaneously injected regular
human insulin in subjects with type 2 diabetes.
Diabetes Care. 2007;30(9):2307-2308.
56. Rosenstock J, Bergenstal RM, Blevins TC,
et al. Better glycemic control and weight
loss with the novel long-acting basal insulin
LY2605541 compared with insulin glargine in
type 1 diabetes: a randomized, crossover study
[published online ahead of print November 27,
2012]. Diabetes Care. 2013;36(3):522-528.
57. Bergenstal RM, Rosenstock J, Arakaki RF,
et al. A randomized, controlled study of once
daily LY2605541, a novel long-acting basal
insulin, versus insulin glargine in basal
insulin-treated patients with type 2 diabetes.
Diabetes Care. 2012;35(11):2140-2147.
58. Niskanen L, Leiter LA, Franek E, et al.
Comparison of a soluble co-formulation of insulin
degludec/insulin aspart vs biphasic insulin
aspart 30 in type 2 diabetes: a randomised trial.
Eur J Endocrinol. 2012;167(2):287-294.
2013 American Osteopathic Association
44. Garber AJ, King AB, Del Prato S, et al; for
the NN1250-3582 (BEGIN BB T2D) Trial
Investigators. Insulin degludec, an ultra-
longacting basal insulin, versus insulin glargine
in basal-bolus treatment with mealtime insulin
aspart in type 2 diabetes (BEGIN Basal-Bolus
Type 2): a phase 3, randomised, open-label,
treat-to-target non-inferiority trial. Lancet.
2012;379(9825):1498-1507.
45. Heise T, Tack CJ, Cuddihy R, et al.
A new-generation ultra-long-acting basal
insulin with a bolus boost compared with
insulin glargine in insulin-naive people with
type 2 diabetes: a randomized, controlled trial.
Diabetes Care. 2011;34(3):669-674.
46. Heller S, Buse J, Fisher M, et al. Insulin
degludec, an ultra-longacting basal insulin,
versus insulin glargine in basal-bolus treatment
with mealtime insulin aspart in type 1 diabetes
(BEGIN Basal-Bolus Type 1): a phase 3,
randomised, open-label, treat-to-target
non-inferiority trial. Lancet.
2012;379(9825):1489-1497.
47. Home PD, Meneghini L, Wendisch U, et al.
Improved health status with insulin degludec
compared with insulin glargine in people
with type 1 diabetes. Diabet Med.
2012;29(6):716-720.
48. Heise T, Nosek L, Bottcher SG, Hastrup H,
Haahr H. Ultra-long-acting insulin degludec
has a fat and stable glucose-lowering effect
in type 2 diabetes. Diabetes Obes Metab.
2012;14(10):944-950.
49. Meneghini L. Flexible once-daily dosing of
insulin degludec does not compromise glycemic
control or safety compared to insulin glargine
compared to insulin glargine given once
daily at the same time each day in people
with type 2 diabetes. In: Program and
Abstracts of the American Diabetes Association
71st Scientifc Sessions, June 24-28, 2011.
San Diego, CA. Abstract 35-LB.
50. Zinman B, Philis-Tsimikas A, Cariou B, et al;
for the NN1250-3579 (BEGIN Once Long)
Trial Investigators. Insulin degludec versus
insulin glargine in insulin-naive patients with
type 2 diabetes: a 1-year, randomized, treat-to-
target trial (BEGIN Once Long). Diabetes Care.
2012;35(12):2464-2471.
51. Keegan A. Exit Exubera: inhalable
insulin is withdrawn due to weak sales.
Diabetes Forecast. 2007;60(13):19.
52. Harper NJ, Gray S, De Groot J, et al.
The design and performance of the Exubera
pulmonary insulin delivery system. Diabetes
Technol Ther. 2007;9(suppl 1):S16-S27.
33. Arnolds S, Dellweg S, Clair J, et al.
Further improvement in postprandial glucose
control with addition of exenatide or sitagliptin
to combination therapy with insulin glargine
and metformin: a proof-of-concept study.
Diabetes Care. 2010;33(7):1509-1515.
34. Thong KY, Jose B, Sukumar N, et al.
Safety, effcacy and tolerability of exenatide
in combination with insulin in the Association
of British Clinical Diabetologists nationwide
exenatide audit. Diabetes Obes Metab.
2011;13(8):703-710.
35. Barnett AH, Charbonnel B, Donovan M,
Fleming D, Chen R. Effect of saxagliptin as
add-on therapy in patients with poorly controlled
type 2 diabetes on insulin alone or insulin
combined with metformin. Curr Med Res Opin.
2012;28(4):513-523.
36. DeVries JH, Bain SC, Rodbard HW, et al; for
the Liraglutide Detemir Study Group. Sequential
intensifcation of metformin treatment in type 2
diabetes with liraglutide followed by randomized
addition of basal insulin prompted by A1C
targets. Diabetes Care. 2012;35(7):1446-1454.
37. DeFronzo RA. Overview of newer agents: where
treatment is going. Am J Med.
2010;123(3 suppl):S38-S48.
38. Nasrallah SN, Reynolds LR. Insulin degludec,
the new generation basal insulin or just another
basal insulin? Clin Med Insights Endocrinol
Diabetes. 2012;5:31-37.
39. Moser EG, Morris AA, Garg SK. Emerging
diabetes therapies and technologies. Diabetes
Res Clin Pract. 2012;97(1):16-26.
40. Owens DR. Insulin preparations with
prolonged effect. Diabetes Technol Ther.
2011;13(suppl 1):S5-S14.
41. Heise T, Hermanski L, Nosek L, Feldman A,
Rasmussen S, Haahr H. Insulin degludec:
four times lower pharmacodynamic variability
than insulin glargine under steady-state
conditions in type 1 diabetes. Diabetes Obes
Metab. 2012;14(9):859-864.
42. Zinman B, Fulcher G, Rao PV, et al. Insulin
degludec, an ultra-long-acting basal insulin,
once a day or three times a week versus insulin
glargine once a day in patients with type 2
diabetes: a 16-week, randomised, open-label,
phase 2 trial. Lancet. 2011;377(9769):924-931.
43. Birkeland KI, Home PD, Wendisch U, et
al. Insulin degludec in type 1 diabetes: a
randomized controlled trial of a new-generation
ultra-long-acting insulin compared with insulin
glargine. Diabetes Care. 2011;34(3):661-665.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Antibodies: Immunoglobulins - A Family of ProteinsДокумент21 страницаAntibodies: Immunoglobulins - A Family of ProteinsMike zombieОценок пока нет
- Antibodies: Immunoglobulins - A Family of ProteinsДокумент21 страницаAntibodies: Immunoglobulins - A Family of ProteinsMike zombieОценок пока нет
- Drug Study 1 Ferrous SulfateДокумент2 страницыDrug Study 1 Ferrous SulfateKrizzia Mae ColladoОценок пока нет
- Chemotherapy: Chemotherapy, in Its Most General Sense, Refers To Treatment of Disease byДокумент42 страницыChemotherapy: Chemotherapy, in Its Most General Sense, Refers To Treatment of Disease byMalueth AnguiОценок пока нет
- Care of Ventilator PatientДокумент39 страницCare of Ventilator Patientsandhya100% (1)
- Lista Produselor 2-8 CДокумент5 страницLista Produselor 2-8 Cadelina78100% (3)
- Chikungunya Viral Infections An Emerging ProblemДокумент6 страницChikungunya Viral Infections An Emerging ProblemMike zombieОценок пока нет
- Mechanisms Ofcancerdrug ResistanceДокумент15 страницMechanisms Ofcancerdrug ResistanceMike zombieОценок пока нет
- Juno Is The Egg Izumo Receptor and IsДокумент16 страницJuno Is The Egg Izumo Receptor and IsMike zombieОценок пока нет
- Antibody Drug ConjugatesДокумент6 страницAntibody Drug ConjugatesMike zombieОценок пока нет
- Enterobius GregoriiДокумент4 страницыEnterobius GregoriiMike zombieОценок пока нет
- Parasites Evade TheДокумент7 страницParasites Evade TheMike zombieОценок пока нет
- Pharmacology Assignment Breast CancerДокумент21 страницаPharmacology Assignment Breast CancerNikki YerakiahОценок пока нет
- Rocuronium Bromide Manufacturer - Teena LabsДокумент2 страницыRocuronium Bromide Manufacturer - Teena Labsteena labsОценок пока нет
- Hemodialysis Patient's Endorsement FormДокумент1 страницаHemodialysis Patient's Endorsement FormHacienda Galea Resort and Events Place100% (1)
- Teratology and Drug Use During Pregnancy and Lactation-1Документ90 страницTeratology and Drug Use During Pregnancy and Lactation-1kbОценок пока нет
- It An To: With Ina With orДокумент1 страницаIt An To: With Ina With orShyra MustakimОценок пока нет
- Campral (Acamprosate Calcium)Документ1 страницаCampral (Acamprosate Calcium)E100% (1)
- Administering Z-Track Intramuscular InjectionДокумент5 страницAdministering Z-Track Intramuscular InjectionRina Abigail Belleza AguedanОценок пока нет
- Prescription MedicationsДокумент3 страницыPrescription MedicationsCarla PulgarОценок пока нет
- Parkinson's Article - PDF 66666666666Документ11 страницParkinson's Article - PDF 66666666666kavyasumanaОценок пока нет
- Regulatory Perspectives On Strength-Dependent Dissolution ProfilesДокумент11 страницRegulatory Perspectives On Strength-Dependent Dissolution ProfilesJminsОценок пока нет
- Ringer Lactate Infusion Product InsertДокумент1 страницаRinger Lactate Infusion Product InsertSmartishag BediakoОценок пока нет
- Proscript User Manual Cms July 2014Документ57 страницProscript User Manual Cms July 2014Alia KhanОценок пока нет
- National Essential Medicines List 2020Документ61 страницаNational Essential Medicines List 2020Parshant BajajОценок пока нет
- Chemical ACTIVITIES - DR DukeДокумент52 страницыChemical ACTIVITIES - DR DukeCuriousMan87Оценок пока нет
- Dipiro X New - Removed - Removed - RemovedДокумент35 страницDipiro X New - Removed - Removed - RemovedfinaОценок пока нет
- Psychopharmacology Article StyleДокумент9 страницPsychopharmacology Article StyleLizethОценок пока нет
- Methods and Materials: The Influence of The Biochemical Components of Marijuana On Several Systems in The BodyДокумент1 страницаMethods and Materials: The Influence of The Biochemical Components of Marijuana On Several Systems in The BodyFinaОценок пока нет
- A SEMINAR REPORT FinalДокумент7 страницA SEMINAR REPORT FinalOladokun Damilare ElijahОценок пока нет
- Biosimilars The Regulatory Framework by Peter Richardson EmaДокумент30 страницBiosimilars The Regulatory Framework by Peter Richardson EmaMiyyada AichaouiОценок пока нет
- 1 PBДокумент12 страниц1 PBLela MaelaОценок пока нет
- JunaidДокумент41 страницаJunaidShobhit GoswamiОценок пока нет
- A Guide To Calculating Parenteral Nutrition When T-2 - 1Документ2 страницыA Guide To Calculating Parenteral Nutrition When T-2 - 1Steve JacobОценок пока нет
- Approach To Treating Generalized Anxiety Disorder in Adults - UpToDate ViДокумент15 страницApproach To Treating Generalized Anxiety Disorder in Adults - UpToDate ViMonique GloverОценок пока нет
- Sample Questions For PBAДокумент3 страницыSample Questions For PBAsheikh SalmanОценок пока нет
- Nitroimidazole Wps OfficeДокумент10 страницNitroimidazole Wps OfficeCamelle DiniayОценок пока нет
- Essential Drug List PDFДокумент13 страницEssential Drug List PDFGaurav AcharyaОценок пока нет