Академический Документы
Профессиональный Документы
Культура Документы
NCP For Laryngeal Cancer
Загружено:
Mădălina PinciucОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
NCP For Laryngeal Cancer
Загружено:
Mădălina PinciucАвторское право:
Доступные форматы
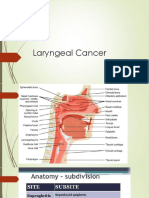
Cancer of the larynx is a malignant tumor in the larynx (voice box). It is potentially curable if detected early.
It
represents less than 1% of all cancers and occurs about four times more frequently in men than in women, and most
commonly in persons 50 to 70 years of age. Squamous cell carcinoma constitutes about 95% of laryngeal cancers.
Rare laryngeal cancer forms adenocarcinoma and sarcoma account for the rest. An intrinsic tumor is on the true
vocal cords and tends not to spread because underlying connective tissues lack lymph nodes. An extrinsic tumor is
on some other part of the larynx and tends to spread easily. Laryngeal cancer is classified by its location:
Supraglottis (false vocal cords)
Glottis (true vocal cords)
Sub glottis (rare downward extension from vocal cords).
Pathophysiology and Etiology of Laryngeal Cancer
Occurs predominantly in men older than age 60. Most patients have a history of smoking; those with Supraglottis
laryngeal cancer frequently have a history of smoking and a high alcohol intake. Other risk factors include vocal
straining, chronic laryngitis, industrial exposure, nutritional deficiency, and family predisposition.
About two-thirds of carcinomas of the larynx arise in the glottis, almost one-third arise in the Supraglottis region, and
about 3% arise in the subglottic region of the larynx. When limited to the vocal cords (intrinsic), spread is slow
because of lessened blood supply. When cancer involves the epiglottis (extrinsic), cancer spreads more rapidly
because of abundant supply of blood and lymph and soon involves the lymph nodes of the neck.
A malignant growth may occur in three different areas of the larynx: the glottis area (vocal cords), Supraglottis area
(area above the glottis or vocal cords, including epiglottis and false cords), and sub glottis (area below the glottis or
vocal cords to the cricoid).
Two thirds of laryngeal cancers are in the glottis area. Supraglottis cancers account for approximately one third of the
cases, subglottic tumors for less than 1%. Glottic tumors seldom spread if found early because of the limited lymph
vessels found in the vocal.
Causes for Laryngeal Cancer
The cause of laryngeal cancer is unknown. Major risk factors include smoking and alcoholism. Minor risk factors
include chronic inhalation of noxious fumes and familial disposition.
Nursing Diagnosis for Laryngeal Cancer. An initial assessment includes a complete history and physical
examination of the head and neck. This will include assessment of risk factors, family history, and any underlying
medical conditions.
Varied assessment findings in laryngeal cancer depend on the tumors location and its stage. With stage I disease,
the patient may complain of local throat irritation or hoarseness that lasts about 2 weeks. In stages II and III, he
usually reports hoarseness. He may also have a sore throat, and his voice volume may be reduced to a whisper. In
stage IV, he typically reports pain radiating to his ear, dysphagia, and dyspnea. In advanced (stage IV) disease,
palpation may detect a neck mass or enlarged cervical lymph nodes.
Diagnostic tests
The usual workup includes laryngoscopy, xeroradiography, biopsy, laryngeal tomography and computed tomography
scans, and laryngography to visualize and define the tumor and its borders. Chest X-ray findings can help detect
metastases.
An indirect laryngoscopy, using a flexible endoscope, is initially performed in the otolaryngologists office to visually
evaluate the pharynx, larynx, and possible tumor. Mobility of the vocal cords is assessed; if normal movement is
limited, the growth may affect muscle, other tissue, and even the airway. The lymph nodes of the neck and the thyroid
gland are palpated to determine spread of the malignancy.
If a tumor of the larynx is suspected on an initial examination, a direct laryngoscopic examination is scheduled. This
examination is done under local or general anesthesia and allows evaluation of all areas of the larynx. Samples of the
suspicious tissue are obtained for histologic evaluation. The tumor may involve any of the three areas of the larynx
and may vary in appearance.
Computed tomography and magnetic resonance imaging (MRI) are used to assess regional adenopathy and soft
tissue and to help stage and determine the extent of a tumor. MRI is also helpful in post-treatment follow-up in order
to detect a recurrence. Positron emission tomography (PET scan) may also be used to detect recurrence of a
laryngeal tumor after treatment.
Nursing Assessment for Laryngeal Cancer
The nurse assesses the patient for the following symptoms: hoarseness, sore throat, dyspnea, dysphagia, or pain
and burning in the throat. The neck is palpated for swelling. If treatment includes surgery, the nurse must know the
nature of the surgery to plan appropriate care. If the patient is expected to have no voice, a preoperative evaluation
by the speech therapist is indicated. The patients ability to hear, see, read, and write is assessed. Visual impairment
and functional illiteracy may create additional problems with communication and require creative approaches to
ensure that the patient is able to communicate any needs.
In addition, the nurse determines the psychological readiness of the patient and family. The idea of cancer is terrifying
to most people. Fear is compounded by the possibility of permanently losing voice and, in some cases, of having
some degree of disfigurement. The nurse evaluates the patients and familys coping methods to support them
effectively both preoperatively and postoperatively.
Nursing Diagnosis For Laryngeal Cancer
Common Nursing Diagnosis found in patient with Laryngeal Cancer
Ineffective airway clearance
Impaired verbal communication
Impaired skin/tissue integrity
Impaired oral mucous membrane
Acute pain
Imbalanced nutrition: less than body requirements
Disturbed body image/ineffective role performance deficient knowledge [learning need] regarding prognosis,
treatment, self-care, and discharge needs
Impaired swallowing
Risk for infection
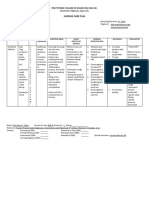
Nursing Care plan for Laryngeal Cancer. Common nursing diagnosis found in Nursing Care plan for Laryngeal
Cancer: Ineffective airway clearance, Impaired verbal communication, Impaired skin/tissue integrity, Impaired oral
mucous membrane, Acute pain, Imbalanced nutrition: less than body requirements, Disturbed body image/ineffective
role performance deficient knowledge [learning need] regarding prognosis, treatment, self-care, and discharge needs,
Impaired swallowing, Risk for infection
Nursing interventions and rationale Nursing Care plan for Laryngeal Cancer
Nursing Diagnosis Ineffective Airway Clearance May be related to:
Partial or total removal of the glottis, altering ability to breathe, cough, and swallow
Temporary or permanent change to neck breathing dependent on patent stoma
Edema formation surgical manipulation and lymphatic accumulation
Copious and thick secretions
Nursing Outcomes Evaluation Criteria, Client Will:
Respiratory Status: Airway Patency
Maintain patent airway with breath sounds clear or clearing.
Clear secretions and be free of aspiration.
Nursing Intervention and Rationale Nursing Diagnosis Ineffective Airway Clearance:
Monitor vital sign respiratory rate and depth note ease of breathing. Auscultate breath sounds. Investigate
restlessness, Dyspnea, and development of cyanosis. Rationale Changes in respirations, use of accessory
muscles, and presence of crackles or wheezes suggest retention of secretions. Airway obstruction can lead to
ineffective breathing patterns even partial Airway obstruction and impaired gas exchange, resulting in complications,
such as pneumonia and respiratory arrest.
Elevate head of bed 30 to 45 degrees. Rationale Facilitates drainage of secretions, work of breathing, and lung
expansion.
Encourage swallowing, if client is able. Rationale reducing risk of aspiration with Prevents pooling of oral secretions
Encourage and teach effective coughing and deep breathing. Rationale Mobilizes secretions to clear airway and
helps prevent respiratory complications.
Suction laryngectomy and tracheostomy tube and oral and nasal cavities. Note amount, color, and consistency of
secretions. Rationale Changes in character of secretions may indicate developing problems, such as dehydration
and infection, and need for further evaluation and treatment. Prevents secretions from obstructing airway, especially
when swallowing ability is impaired.
Teach and encourage client to begin self suction procedures as soon as possible. Educate client in clean
techniques. Rationale Reduces anxiety associated with difficulty in breathing or inability to handle secretions when
alone.
Maintain proper position of laryngectomy or tracheostomy tube. Check and adjust ties as indicated.Rationale As
edema develops or subsides, tube can be displaced, compromising airway. Ties should be snug but not constrictive
to surrounding tissue or major blood vessels.
Observe tissues surrounding tube for bleeding. Change clients position to check for pooling of blood behind neck or
on posterior dressings. Rationale bleeding or sudden eruption of uncontrolled hemorrhage presents a sudden and
real possibility of airway obstruction and suffocation.
Provide supplemental humidification Rationale: Normal physiological on nasal passages means of filtering and
humidifying air are bypassed. Supplemental humidity decreases mucous crusting and facilitates coughing or
suctioning of secretions through stoma.
Resume oral intake with caution Rationale Changes in muscle mass and strength and nerve innervations increase
likelihood of aspiration.
Monitor serial ABGs or pulse oximetry and chest x-ray. Rationale Pooling of secretions or presence of atelectasis
may lead to pneumonia, requiring more aggressive therapeutic measures.
Nursing Diagnosis Impaired Verbal Communication related to:
1. Anatomical deficit removal of vocal cords
2. Physical barrier tracheostomy tube
3. Required voice rest
Nursing Outcomes Evaluation Criteria Client Will:
Communication Enhancement: Speech Deficit Independent
Communicate needs in an effective manner.
Identify and plan for appropriate alternative speech methods after healing.
Nursing Intervention and Rationale Nursing Diagnosis Impaired Verbal Communication:
Review preoperative instructions and discussion of why speech and breathing are altered, RationaleReinforces
teaching at a time when fear of surviving surgery is past.
Determine whether client has other communication impairments, such as hearing, vision, and
literacy.Rationale Presence of other problems influences plan for alternative communication.
Provide immediate and continual means to summon nurse Prearrange signals for obtaining immediate
help Rationale Client needs assurance that nurse is vigilant and will respond to summons. May decrease clients
anxiety about inability to speak.
Allow sufficient time for communication. Rationale Loss of speech and stress of alternative communication can
cause frustration and block expression, especially when caregivers seem too busy or preoccupied.
Encourage ongoing communication with outside world, such as newspapers, television, radio, calendar, and
clock. Rationale Maintains contact with normal lifestyle and continued communication through other avenues.
Caution client not to use voice until physician gives permission. Rationale Promotes healing of vocal cord and limits
potential for permanent cord dysfunction.
Consult or refer with appropriate healthcare team members, therapists, speech pathologist, and social services.
Refer to hospital-based rehabilitation, and community resources, such as Lost Chord or New Voice Club,
International Association of Laryngectomees, and American Cancer Society. RationaleAbility to use alternative
voice and speech methods, such as electrolarynx, TEP, voice prosthesis, and esophageal speech. Rehabilitation
time may be lengthy and require a number of agencies and resources to facilitate or support learning process.
Nursing diagnosis Impaired Skin/Tissue Integrity related to:
Surgical removal of tissues and grafting
Radiation or chemotherapeutic agents
Altered circulation or reduced blood supply
Compromised nutritional status
Edema formation
Pooling or continuous drainage of secretions oral, lymph, or chyle
Nursing Outcomes Evaluation Criteria Client Will:
Wound Healing: Primary Intention
Display timely wound healing without complications.
Demonstrate techniques to promote healing and prevent complications.
Nursing Intervention and Rationale Nursing Diagnosis Impaired Verbal Communication:
Assess skin color, temperature, and capillary refill in operative and skin graft areas. RationaleCyanosis and slow
refill may indicate venous congestion, which can lead to tissue ischemia and necrosis.
Protect skin flaps and suture lines from tension or pressure. Provide pillow or rolls and instruct client to support head
and neck during activity. Rationale Pressure from tubing and tracheostomy tapes or tension on suture lines can
alter circulation and cause tissue injury.
Monitor bloody drainage from surgical sites, suture lines, and drains Rationale Bloody drainage usually declines
steadily after first 24 hours. Steady oozing or frank bleeding indicates problem requiring medical attention.
Note and report any milky-appearing drainage. Rationale Milky drainage may indicate thoracic lymph duct leakage,
which can result in depletion of body fluids and electrolytes. Such a leak may heal spontaneously or require surgical
closure.
Change dressings, as indicated. Rationale Damp dressings increase risk of tissue damage and infection.
Cleanse thoroughly around stoma and neck tubes (if in place), avoiding soap or alcohol. Show client how to do self -
care of stoma and tube with clean water and peroxide, using soft, lint-free cloth, not tissue or cotton. Rationale
Keeping area clean promotes healing and comfort. Soap and other drying agents can lead to stomal irritation and
possible inflammation. Materials other than cloth may leave fibers in stoma that can irritate or be inhaled into lungs.
Monitor all sites for signs of wound infection, such as unusual redness; increasing edema, pain, exudates; and
temperature elevation. Rationale Impedes healing, which may already be slow because of changes induced by
cancer, cancer therapies, or malnutrition.
Administer oral, IV, and topical antibiotics, as indicated. Rationale Prevents or controls infection.
Nursing Diagnosis Impaired Oral Mucous Membrane related to
Dehydration or absence of oral intake, decreased saliva production secondary to radiation or surgical procedure
Poor or inadequate oral hygiene
Pathological condition oral cancer, mechanical trauma oral surgery
Difficulty swallowing and pooling of secretions and drooling
Nutritional deficits
Nursing Outcomes and Evaluation Criteria Client Will:
Tissue Integrity: Skin and Mucous Membranes
Report or demonstrate a decrease in symptoms.
Identify specific interventions to promote healthy oral mucosa.
Demonstrate techniques to restore and maintain mucosal integrity.
Oral Health Restoration
Nursing Intervention and Rationale Nursing Diagnosis Impaired Oral Mucous Membrane:
Inspect oral cavity, Tongue, Lips Teeth and gums and Mucous membranes note changes in:
SalivaRationale Surgery or Damage to salivary glands Tongue, Lips Teeth and gums and Mucous membranes may
decrease production of saliva, resulting in dry mouth. Pooling and drooling of saliva may occur because of
compromised swallowing capability or pain in throat and mouth.
Suction oral cavity frequently. Have client perform self-suctioning when possible or use gauze wick to drain
secretions. Rationale Saliva contains digestive enzymes that may be erosive to exposed tissues.
Show client how to brush inside of mouth, palate, tongue, and teeth. Rationale Frequent oral care reduces bacteria
and risk of infection and promotes tissue healing and comfort.
Apply lubrication to lips; provide oral irrigations as indicated. Rationale Counteracts drying effects of therapeutic
measures and negates erosive nature of secretions.
Avoid alcohol based mouthwashes. Rationale: Alcohol can be drying and irritating.
Nursing Diagnosis Acute Pain related to:
Surgical incisions
Tissue swelling
Presence of nasogastric or orogastric feeding tube
Nursing Outcomes and Evaluation Criteria Client Will:
Report pain is relieved or controlled.
Demonstrate relief of pain and discomfort by reduced tension and relaxed manner.
Nursing Intervention and Rationale Nursing Diagnosis Acute Pain:
Evaluate pain level frequently. Rationale : Pain is a major concern for clients undergoing laryngectomy and it is
believed as many as 32% still suffer severe distress, with the administered dosing less than needed to obtain
optimal pain relief
Investigate changes in characteristics of pain. Check mouth and throat suture lines for fresh trauma. Rationale May
reflect developing complications requiring further evaluation or intervention.
Provide comfort measures, such as back rub and position change, and Diversional activities, such as television,
visiting, and reading. Rationale Promotes relaxation and helps client refocus attention on something beside pain.
Schedule care activities to balance with adequate periods of sleep or rest. Rationale Prevents fatigue or exhaustion
and may enhance coping with stress or discomfort.
Administer analgesics such as on a scheduled basis or via patient-controlled analgesia; adjust dosages according to
pain level per protocols. Rationale Degree of pain is related to extent and psychological impact of surgery as well as
general body condition.
Patient Teaching Discharge and Home Healthcare Guidelines for Patient with Laryngeal Cancer
Patient Teaching Discharge and Home Healthcare Guidelines for Patient with Laryngeal Cancer. Teach the patient
signs and symptoms of potential complications and the appropriate actions to be taken. Complications include
infection (wound drainage, poor wound healing, fever, achiness, chills), airway obstruction and tracheostomy stenosis
(noisy respirations, difficulty breathing, restlessness, confusion, increased respiratory rate), vocal straining; fistula
formation (redness, swelling, secretions along a suture line), and ruptured carotid artery (bleeding,
hypotension).Teach the patient the name, purpose, dosage, schedule, common side effects, and importance of taking
all medications.
Teach the patient the appropriate devices and techniques to ensure a patent airway and prevent complications.
Explore methods of communication that work effectively. Encourage the patient to wear a Medic Alert bracelet or
necklace, which identifies her or him as a mouth breather. Provide the patient with a list of referrals and support
groups, such as visiting nurses, American Cancer Society, American Speech-Learning-Hearing Association,
International Association of Laryngectomees, and the Lost Cord Club
Patient Teaching Discharge and Home Healthcare Guidelines for Patient with Laryngeal Cancer:
Before partial or total laryngectomy, instruct the patient in good oral hygiene practices. If appropriate, instruct a male
patient to shave off his beard to facilitate postoperative care.
Explain postoperative procedures, such as suctioning, NG tube feeding, and laryngectomy tube care. Carefully
discuss the effects of these procedures (breathing through the neck and speech alteration, for example).
After surgery Teach and encourage client to begin self suction procedures as soon as possible. Educate client in
clean techniques. To Reduces anxiety associated with difficulty in breathing or inability to handle secretions when
alone.
Also, prepare the patient for other functional losses. Forewarn him that he wont be able to smell aromas, blow his
nose, whistle, gargle, sip, or suck on a straw.
Reassure the patient that speech rehabilitation measures (including laryngeal speech, esophageal speech, an
artificial larynx, and various mechanical devices) may help him communicate again.
Encourage the patient to take advantage of services and information offered by the American Speech-Language-
Hearing Association, the International Association of Laryngectomees, the American Cancer Society, or the local
chapter of the Lost Chord Club.
Вам также может понравиться
- NCP PryllДокумент6 страницNCP PryllpjcolitaОценок пока нет
- Doxofylline: D 400 MG TabletsДокумент33 страницыDoxofylline: D 400 MG TabletsBibek Singh Mahat100% (2)
- Assessing and Managing Risk of AspirationДокумент6 страницAssessing and Managing Risk of AspirationaianrОценок пока нет
- BPN NCPДокумент6 страницBPN NCPJoart EspinozaОценок пока нет
- NCP For ConcussionДокумент3 страницыNCP For Concussiontamtam_antonio100% (1)
- Nursing Care PlanДокумент4 страницыNursing Care Planapi-309251523Оценок пока нет
- Breast Cancer Risk For InfectionДокумент6 страницBreast Cancer Risk For Infectionam peОценок пока нет
- Nursing Diagnosis: AdvertisementsДокумент7 страницNursing Diagnosis: AdvertisementsJamea TumbagaОценок пока нет
- Breast Ca NCPДокумент3 страницыBreast Ca NCPThirdy AquinoОценок пока нет
- Cva NCP AnxietyДокумент1 страницаCva NCP AnxietyQueenElsaDeVeraОценок пока нет
- Mrs. Ma. Lourdes B. Domingo, RNДокумент3 страницыMrs. Ma. Lourdes B. Domingo, RNRomzy BasañesОценок пока нет
- NCP Nephrolithiasis FeverДокумент1 страницаNCP Nephrolithiasis Feverm_r0se_k0h100% (1)
- Nursing Care Plan for Breast CancerДокумент2 страницыNursing Care Plan for Breast CancerMaina BarmanОценок пока нет
- NCP Laryngeal CancerДокумент10 страницNCP Laryngeal CancerAnonymous XvwKtnSrMR100% (2)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveДокумент3 страницыAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimОценок пока нет
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Документ3 страницыNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaОценок пока нет
- Schizophrenia Nursing ManagementДокумент56 страницSchizophrenia Nursing ManagementHumphreyОценок пока нет
- Physical Assessment On GERD PatientДокумент8 страницPhysical Assessment On GERD PatientRobert Medina100% (1)
- Nursing Care Plan Impaired AdjustmentДокумент1 страницаNursing Care Plan Impaired Adjustmentderic100% (2)
- NCP Alcoholic NeuropathyДокумент5 страницNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- Cancer Nursing Care Plan (NCP) - Risk For InfectionДокумент2 страницыCancer Nursing Care Plan (NCP) - Risk For InfectionAngie MandeoyaОценок пока нет
- Biperiden Generic and Brand Names, Uses, Side EffectsДокумент1 страницаBiperiden Generic and Brand Names, Uses, Side EffectsMFQ.RN100% (2)
- NCPДокумент2 страницыNCPJhel NabosОценок пока нет
- NCP PTBДокумент2 страницыNCP PTBMack Jhed AnarconОценок пока нет
- Child - ImmunizationsДокумент1 страницаChild - ImmunizationsJOHN100% (1)
- Nursing Assessment Objectives and Intervention for ConjunctivitisДокумент2 страницыNursing Assessment Objectives and Intervention for ConjunctivitisIna Marie Calungcaguin Castro100% (1)
- Case Scenario: Prostate CancerДокумент5 страницCase Scenario: Prostate Cancer24 PAULINO ALDRIN MUJARОценок пока нет
- Impaired Verbal CommunicationДокумент6 страницImpaired Verbal CommunicationLaura Sansonetti100% (1)
- Hemorrhoidectomy Case StudyДокумент19 страницHemorrhoidectomy Case StudyJoyJoy Tabada CalunsagОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care PlanJoshua Pascasio100% (1)
- Hearing Loss in Older AdultsДокумент2 страницыHearing Loss in Older AdultsFran Lan100% (1)
- Pleural EffusionДокумент5 страницPleural EffusionTerizla MobileОценок пока нет
- NCP FormatДокумент3 страницыNCP FormatAl Bhert Timbal MagbalotОценок пока нет
- NCP PTBДокумент2 страницыNCP PTBKath TalubanОценок пока нет
- Risk For AspirationДокумент11 страницRisk For AspirationSanket TelangОценок пока нет
- OCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale EvaluationДокумент2 страницыOCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale Evaluationchurva_freak433533% (9)
- Aminogen Drug StudyДокумент2 страницыAminogen Drug Studymilesmin100% (1)
- NCP For Ears Nose ThroatДокумент1 страницаNCP For Ears Nose ThroatMcmac YangoОценок пока нет
- Oxygenation - NCPДокумент5 страницOxygenation - NCPCazze SunioОценок пока нет
- 2 NCPДокумент2 страницы2 NCPJohn CenasОценок пока нет
- As Needed.: Environmental Stimuli 6Документ4 страницыAs Needed.: Environmental Stimuli 6Nicole GumolonОценок пока нет
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationДокумент4 страницыCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Case Study Pleural EffusionДокумент4 страницыCase Study Pleural EffusionKhristine Anne FabayОценок пока нет
- Nursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale EvaluationДокумент1 страницаNursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale Evaluationeihjay-bravo-8041Оценок пока нет
- NCPДокумент3 страницыNCPeun kyung shinОценок пока нет
- DS OfloxacinДокумент2 страницыDS OfloxacinjessicamaysОценок пока нет
- Care Plan ExampleДокумент2 страницыCare Plan Exampleincess27100% (1)
- Nursing Care Plan for Rheumatoid ArthritisДокумент3 страницыNursing Care Plan for Rheumatoid ArthritisJashAnia MarIe EvArdo FloresОценок пока нет
- NCP KoДокумент3 страницыNCP KoGerard Paul OrizaОценок пока нет
- NCP Risk Infection Papillary Thyroid CAДокумент2 страницыNCP Risk Infection Papillary Thyroid CAjazvОценок пока нет
- Caring for TB Patients Using Orem's TheoryДокумент13 страницCaring for TB Patients Using Orem's TheoryRazel Kinette AzotesОценок пока нет
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Implementio N EvaluationДокумент3 страницыNursing Care Plan: Assessment Nursing Diagnosis Planning Implementio N EvaluationAndrew James Javier Quidez100% (1)
- Nursing Care Plan For Laryngeal Cancer - LifenursesДокумент6 страницNursing Care Plan For Laryngeal Cancer - LifenursesMădălina Pinciuc100% (2)
- Laryngeal CancerДокумент13 страницLaryngeal CancerJils SureshОценок пока нет
- Laryngeal Cancer 1Документ49 страницLaryngeal Cancer 1Kpj KpjОценок пока нет
- Malignant Tumors of The LarynxДокумент65 страницMalignant Tumors of The LarynxAlina AlinaОценок пока нет
- Oral Cancer SeminarДокумент69 страницOral Cancer SeminarShubham gaurОценок пока нет
- Oral CancerДокумент11 страницOral CancerJils SureshОценок пока нет
- Laryngeal CarcinomaДокумент52 страницыLaryngeal CarcinomaEjay Jacob Ricamara67% (3)
- CASE ANALYSIS - Nasopharyngeal CancerДокумент8 страницCASE ANALYSIS - Nasopharyngeal CancerTerry Mae Atilazal SarciaОценок пока нет
- SANKARA COLLEGE OF OPTOMETRY BINOCULAR VISION EXAMДокумент2 страницыSANKARA COLLEGE OF OPTOMETRY BINOCULAR VISION EXAMDiwakar RaoОценок пока нет
- Educational Credential Assessment TableДокумент4 страницыEducational Credential Assessment TablezhobeysОценок пока нет
- Pharmacy Law Name - 2 Year Pharmacy TechnicianДокумент9 страницPharmacy Law Name - 2 Year Pharmacy TechnicianridaОценок пока нет
- Getting in Touch SimiliaДокумент3 страницыGetting in Touch Similiatakne_007Оценок пока нет
- Biochem-Rebecca NEET Recall 2020 PDFДокумент21 страницаBiochem-Rebecca NEET Recall 2020 PDFNaazneen MohammedОценок пока нет
- Benjamin A. Root Understanding Panic and Other Anxiety Disorders 2000Документ122 страницыBenjamin A. Root Understanding Panic and Other Anxiety Disorders 2000StefanОценок пока нет
- A Simulation Study of The Number of Events Per Variable inДокумент7 страницA Simulation Study of The Number of Events Per Variable inMario Guzmán GutiérrezОценок пока нет
- The Human Body: An OrientationДокумент59 страницThe Human Body: An OrientationShery Han Bint HindawiОценок пока нет
- CTДокумент183 страницыCTfunky_docОценок пока нет
- Slipped Disc Syndrome ExplainedДокумент9 страницSlipped Disc Syndrome ExplainedAndrei MarinОценок пока нет
- Recording Neutral Zone.Документ3 страницыRecording Neutral Zone.rekabiОценок пока нет
- Electrophysiology Catheters & Control Units (RL-200-Fly)Документ4 страницыElectrophysiology Catheters & Control Units (RL-200-Fly)Pankaj SarkarОценок пока нет
- Torts Cases: I. Fe Cayao vs. Ramolete FactsДокумент16 страницTorts Cases: I. Fe Cayao vs. Ramolete FactsJana GonzalezОценок пока нет
- 1 Manufacture: A Typical Analysis of Commercial Chlorosulfonic Acid Would Be AsДокумент6 страниц1 Manufacture: A Typical Analysis of Commercial Chlorosulfonic Acid Would Be Asapi-19738746Оценок пока нет
- Provision of Higher Education Opportunities for Students of Balochistan & FATAДокумент2 страницыProvision of Higher Education Opportunities for Students of Balochistan & FATAAziz okz100% (1)
- Kuay Lol Fuck You ScribdДокумент73 страницыKuay Lol Fuck You ScribdBook BookОценок пока нет
- Keever FamilyДокумент2 страницыKeever FamilymarylcookpubliclibraОценок пока нет
- EHealthДокумент14 страницEHealthgomezt888Оценок пока нет
- Intervenciones en Rehabilitación Psiquiátrica - RevisiónДокумент17 страницIntervenciones en Rehabilitación Psiquiátrica - RevisiónpsychforallОценок пока нет
- Clostridium: There Are Four Main Types of ClostridiumДокумент2 страницыClostridium: There Are Four Main Types of ClostridiumHardeeshОценок пока нет
- Overview and Treatment Option: SkizofreniaДокумент8 страницOverview and Treatment Option: SkizofreniaEvi LoОценок пока нет
- Slipped Capital Femoral EpiphysisДокумент7 страницSlipped Capital Femoral EpiphysisRusu AdrianОценок пока нет
- Nursing Fundamental Q&AДокумент26 страницNursing Fundamental Q&ALinjumol T GОценок пока нет
- Peta Rsud Bangil Periode Desember 2018Документ2 страницыPeta Rsud Bangil Periode Desember 2018pkpo dktОценок пока нет
- Anesthesia Options ExplainedДокумент6 страницAnesthesia Options ExplainedSilvio DTОценок пока нет
- I Notes StrabismusДокумент92 страницыI Notes StrabismusPrincess EzzlynnОценок пока нет
- 3 Adime Form For Diabete Case 1Документ2 страницы3 Adime Form For Diabete Case 1api-309275032Оценок пока нет
- Neonatal ExaminationДокумент132 страницыNeonatal ExaminationMohamad Saleh100% (2)
- Daftar Permintaan ObatДокумент3 страницыDaftar Permintaan ObatEfhan SalaputaОценок пока нет