Академический Документы
Профессиональный Документы
Культура Документы
Atrial Natriuretic Peptides
Загружено:
Sava1988Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Atrial Natriuretic Peptides
Загружено:
Sava1988Авторское право:
Доступные форматы
ATRIAL NATRIURETIC PEPTIDES (ANP)
1. Characteristics of ANP
The circulating (biological active) form of human ANP, as shown in the figure, comprises a 28
amino acid peptide with a 17 amino acid ring closed by a disulfide bond between two cysteine
residues. Its amino acid sequence is highly conserved across species.
ANP (1-28) - the biologically active hormon
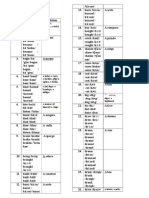
2. Biosynthesis of ANP
proANP is stored in membrane-bound granules in atrial cardiocytes. Upon stimulation, these
granules move to the cell surface, releasing the stored proANP (1-126). The precise location
and identity of this mechanism are still the subject of some debate. This prohormone is
cleaved into the mature 28 amino acid peptide ANP, also known as ANP (1-28) or -ANP,
and the amino terminal fragment ANP (1-98). The 98 aminoacid N-terminus is further
processed proteolytically within the circulation to form proANP (1-30), proANP (31-67) and
proANP (79-98).
proANP (1-30) proANP (31-67) proANP (79-98)
proANP (1-98)
Biomedica cat.no.
BI-20892
proANP (99-126)
= ANP (1-28)
= -ANP
(biologically active)
proANP (1-126)
3. Function of Natriuretic Peptides
The natriuretic peptides can affect systemic blood pressure by several mechanisms, including
modification of renal function and vascular tone, counteracting of the renin-angiotensin-
aldosterone system and action on brain regulatory sites. These systems maintain a balance
which ensures relative constancy of body electrolyte and water content and circulatory
homeostasis.
Main biologic actions of natriuretic peptides
cause of natriuresis and diuresis
cause of vasodilatation
suppression of renin action
suppression of aldosterone action
suppression of sympathetic activity
suppression of antidiuretic hormone (ADH)
inhibition of growth of vascular smooth muscle
4. Relevance of proANP
proANP has a significantly longer half-life compared to -ANP, which is very short lived (half-
life 2.5 minutes) and thus has up to 50 times the plasma concentration of -ANP. As
circulating levels of immunoreactive proANP moieties are less sensitive to rapid fluctuations
of -ANP levels, they better reflect the total amount of secreted ANP.
Samples are directly assayed to measure proANP, and need no prior extraction as with
-ANP.
Conclusion:
Several studies reported that plasma-levels of -ANP and proANP were significantly elevated
even in asymptomatic patients with left ventricular dysfunction and support a clinical
relevance for proANP as an important non-invasive marker.
5. Clinical Applications and Pathophysiology
Circulating plasma levels of proANP are elevated in a number of diseases and have shown to
be important markers for:
discriminating NYHA Class I CHF subjects
left ventricular dysfunction in asymptomatic patients
prediction of the general cardiac status
prediction of early heart failure in asymtomatic patients
prognosis after acute myocardial infarction (AMI)
diagnosis of chronic renal failure (CRF)
optimisation of ACE-I (Angiotensin Converting Enzyme-Inhibitors) therapy
diagnosis of preeclamsia
diagnosis of liver disease
diagnosis of volume overload in patients undergoing continuous ambulatory
peritoneal dialysis
7. Implications
proANP and the HEART CARDIOLOGY
Adrenomodullin, endothelin, neuropeptide Y, atrial, brain, and C-natriuretic
prohormone compared as early heart failure indicators
(1) Daggubati et al., Cardiovascular Research (1997), 246-255
pro ANPs (31-67), (1-30) and (79-98) had 100%, 83% and 50% sensitivity in differentiating
Class I CHF subjects from healthy subjects. proANP (31-67) is the most sensitive marker in
discriminating NYHA Class I CHF subjects from healthy individuals.
Prognostic Significance of N-terminal pro-atrial natriuretic factor (1-98) in acute
myocardial infarction: comparison with atrial natriuretic factor (99-126) and clinical
evaluation
(2) Omland et al., Br Heart Journal (1993) 70, 409-414
Determination of plasma N-terminal proatrial natriuretic factor (1-95) in the subacute phase of
myocardial infarction may provide clinically relevant prognostic information that is superior to
that obtained from atrial natriuretic factor (99-126) measurements and clinical evaluation.
Comparison of Atrial Natriuretic Peptide, B-Type Natriuretic Peptide, and N-Terminal
Proatrial Natriuretic Peptide as Indicators of Left Ventricular Systolic Dysfunction
(3) Davidson et al., Am J Cardiol (1996) 77, 828-831
Plasma concentrations of Nt-proANP provides a sensitive indicator of moderate to severe LV
dysfunction; both peptides are objectively superior to ANP for identifying patients with LVEF
< 35%. These simple tests could be used to screen patients with suspected ventricular
dysfunction to reduce the demand for further cardiac investigations.
Plasma levels and molecular forms of proatrial natriuretic peptides in healthy subjects
and in patients with congestive heart failure.
(4) Azizi et al., Journal of Endocrinology (1996) 148, 51-57
The rise of immunoreactive proANP (1-39) levels is more pronounced than the variation of
immunreactive -ANP (99-126). Nt-proANP (1-30) plasma levels may prove to be a more
sensitive marker of left ventricular dysfunction than ANP.
See also figure on next page.
-ANP and Nt-proANP as markers for CHF
Plasma Proatrial Natriuretic Factor is Predictive of Clinical Status in Patients with
Congestive Heart Failure
(5a) Dickstein et al., Am J Cardiol (1995) 76, 679-683
Concentration of proANP is related to the degree of clinical heart failure. Analysis is simple
and should be of practical value as a supplement in the routine assessment of cardiac status
in this heterogenous population.
Three Peptides From the Atrial Natriuretic Factor Prohormone Amino Terminus Lower
Blood Pressure and Produce Diuresis, Natriuresis, and/or Kaliuresis in Humans
(5b) Vesely et al., Circulation (1994) 90, 1129-1140
proANPs (1-30) and (31-67) have significant blood pressure-lowering, diuretic properties.
Natriuretic properties in humans are significantly prolonged compared with ANP.
Serum N-terminal proatrial natriuretic factor in children with congenital heart disease
(6) Holmstrm et al., European Heart Journal (1996) 17, 1737-1746
Elevation of Nt-proANP (= proANF) level is related to atrial pressures, heart failure and a
high pulmonary to systemic flow ratio. These findings make proANP a potential new
diagnostic tool in heart disease in children.
proANP and PREECLAMPSIA GYNECOLOGY
An Increase of the Plasma N-terminal Peptide of Proatrial Natriuretic Peptide in
Preeclampsia
(7) Anneli et al., Obstet Gynecol (1997) 89, 747-753
A marked elevation in N-terminal peptide of proatrial natriuretic peptide may predict
development of severe preeclampsia and/or in small for gestational age (SGA) infant.
proANP and LIVER DISEASE HEPATOLOGY
(8) Hartter et al., unpublished
Data show marked elevated levels of proANP (1-30) and proANP (31-67) in liver disease
patients. See also figure below.
proANP levels in liver disease
proANP and TREAD MILL EXERCISE REHABILITATION
(9) Hartter et al., unpublished
See also figure below.
proANP levels during tread mill exercise
proANP and PERITONEAL DIALYSIS NEPHROLOGY
Plasma Atrial Natriuretic Peptide Levels in Continuous Ambulatory Peritoneal Dialysis
Patients
(10) Shiota et al., Nepron (1997) 75, 360-361
The present study showed the plasma level of atrial natriuretic peptide to be a more reliable
method for determination of the volume overload status in patients undergoing continuous
ambulatory peritoneal dialysis.
Renal Actions of Atrial Natriuretic Peptide
(11) Meyer et al., Contemporary Endocrinology:
Natriuretic Peptides in Health and Disease, (1998) Chapter 9, 147-170
-ANP serves primarily as a regulator of the cardiovascular system with relatively little effect
on the kidney, whereas proANP (95-126) (Urodilatin) serves as a physiological ligand for the
receptors in the inner medullary collecting duct, relating to the intrarenal regulation of sodium
excretion.
Вам также может понравиться
- A Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesДокумент6 страницA Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesSava1988Оценок пока нет
- RW A Review On 13 Thiazolidin 4 OnesДокумент10 страницRW A Review On 13 Thiazolidin 4 OnesSava1988Оценок пока нет
- 83Документ7 страниц83Sava1988Оценок пока нет
- A Bate, A Măcina, A Strivi: Vt/viДокумент5 страницA Bate, A Măcina, A Strivi: Vt/viElisaveta VicleanuОценок пока нет
- Dissolution Testing (Kel 3)Документ28 страницDissolution Testing (Kel 3)Anonymous QEVAyPMОценок пока нет
- NinhydrinДокумент26 страницNinhydrinSava1988Оценок пока нет
- NinhydrinДокумент26 страницNinhydrinSava1988Оценок пока нет
- Molecular Properties Impact Oral Drug AbsorptionДокумент21 страницаMolecular Properties Impact Oral Drug AbsorptionSava1988100% (1)
- Analysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationДокумент16 страницAnalysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationSava1988Оценок пока нет
- Designing Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesДокумент8 страницDesigning Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesSava1988Оценок пока нет
- Evalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Документ14 страницEvalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Sava1988Оценок пока нет
- Conversion of Tryptophab To Indole 3 Acetic AcidДокумент7 страницConversion of Tryptophab To Indole 3 Acetic AcidSava1988Оценок пока нет
- Design, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsДокумент10 страницDesign, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsSava1988Оценок пока нет
- Chapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentДокумент25 страницChapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentSava19880% (1)
- Structure-Activity Relationship of Indomethacin Analogues ForДокумент10 страницStructure-Activity Relationship of Indomethacin Analogues ForSava1988Оценок пока нет
- IndometacinДокумент47 страницIndometacinSava1988Оценок пока нет
- 101 Full PDFДокумент9 страниц101 Full PDFSava1988Оценок пока нет
- 101 Full PDFДокумент9 страниц101 Full PDFSava1988Оценок пока нет
- Emodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionДокумент11 страницEmodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionSava1988Оценок пока нет
- Alfa TomatinaДокумент11 страницAlfa TomatinaSava1988Оценок пока нет
- MisoprostolДокумент7 страницMisoprostolSava1988Оценок пока нет
- Akt 1Документ11 страницAkt 1Sava1988Оценок пока нет
- Mechanism of Actions Ofcarbamazepine and DerivatesДокумент10 страницMechanism of Actions Ofcarbamazepine and DerivatesSava1988Оценок пока нет
- Sinteza IndometacinДокумент18 страницSinteza IndometacinSava1988Оценок пока нет
- Pi 3 KДокумент8 страницPi 3 KSava1988Оценок пока нет
- Ejaculare PrecoceДокумент6 страницEjaculare PrecoceSava1988Оценок пока нет
- Flavonoide Si Sist ImunДокумент14 страницFlavonoide Si Sist ImunSava1988Оценок пока нет
- Oral Analgesics For Chronic Low Back PainДокумент7 страницOral Analgesics For Chronic Low Back PainSava1988Оценок пока нет
- DesloratadinaДокумент3 страницыDesloratadinaSava1988Оценок пока нет
- 101 Full PDFДокумент9 страниц101 Full PDFSava1988Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Rejuvenation MesotherapyДокумент40 страницRejuvenation MesotherapyerlanggawidyaputriОценок пока нет
- WinnicotДокумент12 страницWinnicotfafariolaОценок пока нет
- The Effect of Shiatsu Massage On Pain Reduction in Burn PatientsДокумент4 страницыThe Effect of Shiatsu Massage On Pain Reduction in Burn Patientskaterine viafaraОценок пока нет
- Ethiopia EmlДокумент99 страницEthiopia EmlWuri OktafianaОценок пока нет
- Free Report-Smoking CessationДокумент5 страницFree Report-Smoking CessationdapextilburyОценок пока нет
- Dance TherapyДокумент13 страницDance TherapyCaress Mae Gubaton Cabudoy100% (2)
- CPG Uterine InversionДокумент3 страницыCPG Uterine InversionRahmayanti YuliaОценок пока нет
- Physical ExaminationДокумент2 страницыPhysical ExaminationPopa Elena0% (1)
- Advanced Ventilator y ModesДокумент42 страницыAdvanced Ventilator y ModesCarlos O JaramilloОценок пока нет
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaДокумент19 страницRajiv Gandhi University of Health Sciences Bangalore, KarnatakaARJUN BОценок пока нет
- Reproductive System DiseasesДокумент3 страницыReproductive System Diseasesirish xОценок пока нет
- Aromatherapy: A: andДокумент7 страницAromatherapy: A: andRahul JoshiОценок пока нет
- Prehospital Care Scoop and RunДокумент4 страницыPrehospital Care Scoop and RunKmilo EstrellaОценок пока нет
- Corrective Exercise The Lumbo Pelvic GirdleДокумент9 страницCorrective Exercise The Lumbo Pelvic GirdlealmaformaОценок пока нет
- Obstetrical Hemorrhage: Reynold John D. ValenciaДокумент82 страницыObstetrical Hemorrhage: Reynold John D. ValenciaReynold John ValenciaОценок пока нет
- Aquatic TherapyДокумент2 страницыAquatic Therapyonix2000Оценок пока нет
- Ranolazine and Hallucinations: Case ReportДокумент3 страницыRanolazine and Hallucinations: Case ReportKenny KenОценок пока нет
- Iaea Tecdoc 896Документ273 страницыIaea Tecdoc 896Anthony KarlОценок пока нет
- ECG NotesДокумент7 страницECG NotesShams NabeelОценок пока нет
- Technique For Awake Fibre Optic IntubationДокумент3 страницыTechnique For Awake Fibre Optic Intubationmonir61Оценок пока нет
- Telenursing Di IntensifДокумент9 страницTelenursing Di IntensifrimbaОценок пока нет
- Depression: Answers To Students' Frequently Asked Questions About DepressionДокумент4 страницыDepression: Answers To Students' Frequently Asked Questions About DepressionRalphОценок пока нет
- OsteoporosisДокумент15 страницOsteoporosisCamille Marie ReyesОценок пока нет
- Medical Writing SampleДокумент2 страницыMedical Writing SampleJusteena KaithaparambilОценок пока нет
- BRP PharmaceuticalsДокумент41 страницаBRP PharmaceuticalsBRP Pharmaceuticals100% (1)
- Comprehensive Pharmacy Review For NAPLEX 8th Ed - Chapter 54Документ50 страницComprehensive Pharmacy Review For NAPLEX 8th Ed - Chapter 54DrSamia El WakilОценок пока нет
- Mot SyllabusДокумент30 страницMot SyllabusShanthoshini Baskaran100% (1)
- Working With Whiplash, Part I (Myofascial Techniques)Документ5 страницWorking With Whiplash, Part I (Myofascial Techniques)Advanced-Trainings.com100% (4)
- S 016 LBLДокумент23 страницыS 016 LBLMuhammadAmdadulHoqueОценок пока нет
- Physical Therapy Resume PDFДокумент3 страницыPhysical Therapy Resume PDFAmit KumarОценок пока нет