Академический Документы
Профессиональный Документы
Культура Документы
Journal
Загружено:
maazioОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Journal
Загружено:
maazioАвторское право:
Доступные форматы
Copyright 1990 by
The Gemntological Society of America
This paper views caregiver stress as a consequence of a process comprising a number of
interrelated conditions, including the socioeconomic characteristics and resources of
caregivers and the primary and secondary stressors to which they are exposed. Primary
stressors are hardships and problems anchored directly in caregiving. Secondary stressors fall
into two categories: the strains experienced in roles and activities outside of caregiving, and
intrapsychic strains, involving the diminishment of self-concepts. Coping and social support
can potentially intervene at multiple points along the stress process.
Key Words: Caregiver strains; Role strains; Loss; Self-concept; Stress mediators
Caregiving and the Stress Process: An
Overview of Concepts and Their Measures
1
Leonard I. Pearlin, PhD,
2
Joseph T. Mullan, PhD,
2
Shirley J. Semple, MA,
2
and Marilyn M. Skaff, MA
2
It can hardly go unnoticed that research into care-
giving has become a flourishing enterprise. Several
reasons explain this striking growth of interest. One
concerns the changing demographic landscape of
contemporary societies: people live longer; the
longer they live, the more at risk they are for chronic
ailments that impair their ability to care for them-
selves; and, because of medical advances, impaired
people survive for longer periods of time despite
their health problems. It is also clear, painfully so to
many, that as the need for care for the chronically
impaired grows, so do its costs and the elusiveness
of its quality. We know that most families are com-
mitted to caring for impaired relatives at home
(Shanas, 1979; Brody, 1985). It is likely that because
of the formidable barriers to suitable institutional
care, however, many families continue to keep their
relatives at home even after their resolve has been
worn down.
Given that these kinds of changes have made infor-
mal family caregiving a typical experience, it is un-
derstandable that its economic, social, and psycho-
logical impacts would become areas of intense
research concern. The research, of course, has been
driven by several disciplinary perspectives and theo-
retical orientations. Probably none is more promi-
nent in current research into caregiving than that
concerned, either explicitly or implicitly, with stress
and its mediation. Indeed, caregiving is potentially a
fertile ground for persistent stress. A brief consider-
ation of caregiving will help to reveal why this is so.
Support for this work was provided by the National Institute of Mental
Health, under grant #MH42122. We thank our co-investigators, Drs. Carol
Ancshensel, William lagust, and David Lindeman, as well as Lisa Hoffman
and Jane Karp for their collaboration on this work. We are also grateful for
the generous help and encouragement of William Fisher and Peter Braun.
Address correspondence to Dr. Leonard I. Pearlin, Human Development
and Aging Program, 1350 7th Ave., CSBS 237, University of California, San
Francisco, CA 94143-0848.
-Human Development and Aging Program, University of California, San
Francisco.
Caregiving and Stress
Informal caregiving simply refers to activities and
experiences involved in providing help and assistance
to relatives or friends who are unable to provide for
themselves. Whereas caring is the affective compo-
nent of one's commitment to the welfare of another,
caregiving is the behavioral expression of this com-
mitment. Giving care to someone is an extension of
caring about that person. Looked at this way, caring
and caregiving are intrinsic to any close relationship;
that is, they are present in all relationships where
people attempt to protect or enhance each other's
well-being. Caring and caregiving are the sine qua
non of what Cooley (1915) described as primary rela-
tionships. Indeed, because caregiving is embedded
in ordinary relationships, it is, strictly speaking, not
accurate to treat it as though it were itself a role.
Instead, caregiving refers to particular kinds of
actions that are found in the context of established
roles, such as wife-husband, child-parent.
Considering how quotidian caregiving is, it hardly
seems the stuff out of which severe stress springs.
Under some circumstances, however, caregiving is
transformed from the ordinary exchange of assis-
tance among people standing in close relationship to
one another to an extraordinary and unequally dis-
tributed burden. The emergence of a serious and
prolonged impairment, such as Alzheimer's disease,
is such a circumstance. Where impairment leads to
increasing dependency on others for the satisfaction
of basic needs, a profound restructuring of the estab-
lished relationship can occur. Caregiving, which pre-
viously might have been but one fleeting component
of an encompassing relationship, can now come to
be the dominant, overriding component. Under con-
ditions of chronic and progressive impairment,
therefore, caregiving may imperialistically expand to
the point where it occupies virtually the entirety of
the relationship.
As the capabilities of parties to the relationship
583 The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
become increasingly imbalanced, the reciprocities
and give and take that had existed fade into the past.
This is especially the case where the disability in-
volves cognitive deterioration, as in Alzheimer's dis-
ease and other dementias. Help, assistance, and af-
fection become unidirectional, eventually going only
from the caregiver to the recipient. We shall later
spell out some of the specific ingredients of caregiv-
ing that can exert a stressful impact. Whatever these
specific ingredients are, the sheer dramatic and in-
voluntary transformation of a cherished relationship
is itself a major source of stress (Pearlin, 1983). It is
altogether understandable, then, that scholars who
study caregiving would be interested in the stress
that befalls the caregiver. There are caregivers, of
course, who manage to find some inner enrichment
and growth even as they contend with mounting
burdens. Nevertheless, it is difficult to imagine many
situations that equal let alone surpass the
stressfulness of caregiving to relatives and friends
with severe chronic impairments.
Although caregiving has acted as a magnet in at-
tracting the interests of stress researchers, those
drawn to it don't necessarily view it through the same
theoretical or methodological lens. The confusing
diversity and the shortcomings found generally in
psychosocial stress research certainly find their way
into research that deals specifically with caregiving.
Diversity and confusion are not necessarily to be
abhorred; perhaps these are the unavoidable by-
products of any field that has rapidly generated in-
tense research activity. But these by-products have
their costs, primarily in the sprouting of inconsistent
or seemingly discontinuous knowledge. There have
been recent calls to move caregiving research toward
greater sophistication (Zarit, 1989; Romeis, 1989).
And there have also been efforts to bring sound
measurement closer to the many aspects of caregiv-
ing and its impact (Lawton et al., 1989). The aim of
this paper is to join in these efforts.
Procedures
To implement our aim, we do two things. First, we
lay out a conceptual scheme for the study of care-
giver stress and, second, we present a number of the
measures we have developed to assess the multiple
components of the scheme. Because the utility of
measures depends on how well they reflect the con-
cepts they are intended to assess, the measures we
introduce here were developed after our conceptual
framework. This framework is a product both of
many years of research into the stress process and of
considerable exploratory research among spouses
and adult children who care for relatives with Alzhei-
mer's disease. Much of our general understanding of
the stress process usefully applies to the study of
caregivers, and what we have learned from the study
of caregivers has usefully informed our general un-
derstanding of the stress process.
The measures that are presented were constructed
from our current multiwave study of 555 caregivers in
the San Francisco Bay Area and Los Angeles, proba-
bly the largest such study undertaken to date. The
caregivers were recruited primarily from the pool of
people who contacted local Alzheimer's Associa-
tions (ADRDA) in the San Francisco Bay Area and in
Los Angeles County. We attempted to contact every-
one who was a self-described primary caregiver of a
noninstitutionalized spouse or parent (or parent-in-
law) with Alzheimer's or a similar dementia. In a
subsequent screening call, we verified that these
criteria were met. In those instances in which the
person was not the primary caregiver, we asked for
the identification and location of the family member
who was primarily responsible for caregiving. When
the caregiving was shared, we chose the spouse
whenever possible. Three interviews will be con-
ducted over a 2-year period, providing an opportu-
nity to chart changes brought on by the institutional-
ization and death of patients, as well as changes that
occur within the household caregiving situation.
Two interviews have been completed, but only the
framework guiding the first is presented here.
In Table 1 the distributions of key characteristics of
the sample are shown separately for spousal and
adult children caregivers. It can be noted that the
proportions who are husbands, wives, daughters, or
sons are almost the same as in a national study of
caregivers (Stone, Cafferata, & Sangl, 1987). The sam-
ple is tilted toward the middle class, as indicated by
educational status. In this respect, too, it is similar to
other caregiver studies. By no means can this sample
be thought of as representative of all caregivers.
Indeed, even if it were, we would not know it be-
cause the universe it would represent is unknown.
What is important to recognize is that the distribu-
tion of characteristics is sufficiently broad to permit
the analysis of their associations with other attributes
of the caregivers.
The measures are presented as appendices rather
than as part of the text; this better allows for their
separate and detailed examination. Not all of the
measures and scales used in our research are in-
cluded in the appendices. Essentially, only newly
created measures of key experiences or dispositions
are included. Several others are described in the text
but not appended. Although most of the measures
presented in the appendices are based on the factor
analyses of data gathered from the 555 participants,
the construction of these measures began with the
open-ended exploratory interviews. In these inter-
views, caregivers were asked about the problems
they faced, the actions, feelings, and sentiments
evoked by these problems, and their attempts to
manage their difficulties. From the transcripts of the
interviews, conceptual themes were identified and
structured questions formed. These questions were
then put through a series of pretests and revisions
before being incorporated into the final scheduled
interview. The manner in which the measures were
developed as well as their psychometric properties
provide us with an overall sense of confidence that
they are serviceable and reliable indicators of our
concepts.
A final introductory comment. The conceptual
Vol. 30, No. 5,1990 584
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
framework we shall outline and the measures of its
components are not presented as footsteps to be
followed by others engaged in caregiver research.
Fortunately, there is more than one way to think
about the issues we address and more than one way
to measure constructs. Our hope is to provoke criti-
cal thinking about issues that deserve attention and
to bring choices into clearer awareness as future
research is planned. In this way, perhaps, these ma-
terials will contribute to the coherence of a field of
research that is somewhat fragmented and not as
substantial as is warranted by the importance of its
subject matter.
The Conceptual Components of Caregiver Stress
One will find that a number of the elements of
caregiver stress in which we are interested are also to
be found in the research of others. However, areas of
overlapping interest are likely to have different con-
ceptual underpinnings. Basically, we approach the
study of caregiver stress from the perspective of what
has come to be referred to as the stress process. The
very notion of process forces attention on the rela-
tionships among the many conditions leading to per-
sonal stress and the ways these relationships develop
and change over time. From this perspective, we are
not interested in simply identifying conditions that
might be associated with stress as much as in know-
ing how these conditions arise and how they come to
be related to each other. Four domains make up this
process, each comprising multiple components. The
domains are: the background and context of stress;
the stressors; the mediators of stress; and the out-
comes or manifestations of stress. As we describe
each of these, the notion of a stress process in
caregiving will become clearer. Figure 1 is presented
as a graphic guide to our discussion.
The Background and Contexts of the Stress Process
Virtually everything we are interested in learning
about caregiving and its consequences is poten-
tially influenced by key characteristics of the care-
giver. The effects of ascribed statuses, such as age,
gender, and ethnicity, along with educational, occu-
pational, and economic attainments are expected to
be threaded throughout the entire stress process.
These characteristics signify where people stand
within stratified orders having unequal distributions
of rewards, privileges, opportunities, and responsi-
bilities. The kinds and intensities of stressors to
which people are exposed, the personal and social
resources available to deal with the stressors, and the
ways stress is expressed are all subject to the effects
of these statuses.
Links between social and economic characteristics
of caregivers and other components of the stress
process in which they are caught up are of utmost
importance. They demonstrate that even seemingly
random exigencies, such as the occurrence of Alz-
heimer's disease, can set in motion processes that to
some extent are regulated and directed by the larger
Table 1. Distributions of Sample Characteristics
of Alzheimer's Caregivers
Variable
City
San Francisco
Los Angeles
Caregiver relationship
Wife
Husband
Daughter
Son
Daughter-in-law
Son-in-law
Marital status
Married
Divorced/separated
Widowed
Never married
Living with AD person
Yes
No
Race
White
Black
Asian
Hispanic
Respondent education
Less than high school
High school
Some college
College graduate
College +
Employment status
Employed
Not employed
Respondent age-
1
Less than 44
45-54
55-64
65-74
75-88
AD person age
b
Less than 44
45-54
55-64
65-74
75-84
85-94
Years caregiving
Less than 1
1-2
3-5
6 or more
Spousal
caregivers
(N = 326)
56%
44
58
42
100
99
1
87
7
2
4
18
29
22
14
17
17
83
1
5
17
45
32
1
2
14
39
39
5
27
37
30
6
Children
caregivers
(N = 229)
52%
48
76
16
8
58
19
8
15
61
39
80
15
3
2
6
25
32
18
19
57
43
27
39
28
6
2
18
54
26
21
36
33
10
"Spousal mean age = 70; child mean age = 51.
''Spousal mean age = 72; child mean age = 80.
social orders of the society and the statuses of people
within them. Caregivers may come to feel cut off
from the larger society, but they are still very much
influenced by its organization. Although these kinds
of linkages have had some analytic attention in stud-
ies of caregiver stress, particularly with regard to
gender (e.g., Zarit, Todd, & Zarit, 1986; Young &
Kahana, 1989), they deserve much more. As we have
585
The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
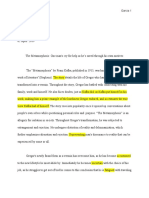
BACKGROUND AND CONTEXT
SES Characteristics
Caregiving History
Family & Network
Composition
Program Availability
PRIMARY STRESSORS
Objective Indicators
Cognitive Status
Problematic Behavior
AOL, IADL Dependencies
Subjective Indicators
Overload
Relational Deprivation
SECONDARY ROLE STRAINS
Family Conflict
Job-Caregiving Conflict
Economic Problems
Constriction of Social
Life
SECONDARY
INTRAPSYCHIC STRAINS
Global
Self-Esteem
Mastery
Situational
Loss of Self
Role Capt i vi t y
Competence
Gain
MEDIATORS
Coping
Social Support
OUTCOMES
Depression
Anxi et y
Irasci bi l i ty
Cognitive Disturbance
Physical Health
Yielding of Role
Figure 1. A conceptual model of Alzheimer's caregivers' stress. The stress process is made up of four domains: the background and
context of stress; the stressors; the mediators of stress; and the outcomes or manifestations of stress.
observed elsewhere (Pearlin, 1989), information
about people's statuses is too frequently gathered
and then used only as statistical controls while look-
ing at relationships among other conditions.
Aspects of the caregiving history are also taken
into account. A number of items of information make
up this history. Among them is the relationship of the
caregiver to the patient, whether a husband or wife,
son or daughter (or daughter-in-law). Information is
also gathered about conflict and distance that might
have existed in the past caregiver-patient relation-
ship. Additional questions are asked about a range of
physical health problems of the patient that could
bear on caregiving demands. Finally, the length of
time that the patient has required care is established.
The duration of caregiving activities is, of course, a
marker of the chronicity of the stressors that the
caregiver experiences.
As can be seen in Figure 1, we also consider access
to and use of resources and programs as important
contextual elements of the stress process. We refer
here to networks (including family) to which care-
givers have attachments, the composition of the net-
works, and the nature and frequency of contacts with
their members. It can be noted that the notion of
network is different from that of social support. Net-
work represents the totality of one's relationships,
whereas support, which we treat as a mediator, per-
tains to the assistance one may derive from but a
portion of the network (Pearlin, 1985). Although one
cannot have social support without having a net-
work, one may conceivably have a network without
support.
Another type of resource is represented by com-
munity-based formal programs created to benefit
patients, caregivers, or both. There are many pro-
grams that are designed to provide specialized ser-
vices for patients or caregivers. However, the avail-
ability of such programs varies considerably from
one community to another. They also vary in cost
(and their affordability by caregivers), the availability
of transportation to the programs, the hours of the
day they function, and, of course, their proximity to
the caregiver. Consequently, the actual use of pro-
grams by caregivers may be limited by a number of
extraneous factors. To the extent that one can and
does draw upon these kinds of resources, one can
escape some of the vicissitudes and hardships of
caregiving one might otherwise experience. From a
structural perspective, many of these programs link
the caregiver to the larger community. This linkage
itself might help to reduce the isolation and aliena-
tion that many caregivers experience.
Primary and Secondary Stressors
We turn next to stressors, which are at the heart of
the stress process in which caregiving may be em-
bedded. These are the conditions, experiences, and
activities that are problematic for people; that is, that
threaten them, thwart their efforts, fatigue them, and
defeat their dreams. Giving care to the seriously
impaired can produce a variety of stressors. In earlier
investigations of caregiving, especially those bor-
rowing from the ground-breaking work of Zarit,
Reeves, and Bach-Peterson (1980), multiple stressors
were usually aggregated into unitary measures. Al-
though these measures were discovered to be re-
Vol. 30, No. 5,1990 586
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
lated to depression and other outcomes, their com-
posite characters made it difficult to discern the
particular stressors that contribute most to these
outcomes. Although it is useful to know that global
burden contributes to depression, eventually we
need to know which specific burdens are most likely
to result in depression and the conditions under
which these burdens are most likely to be present. In
this paper, we seek to identify and disaggregate
some of the more salient stressors subsumed by the
global notion of burden.
As seen in Figure 1, we divide stressors into those
that are primary and secondary. We view primary
stressors as driving the process that follows. By and
large, they stem directly from the needs of the pa-
tient and the nature and magnitude of the care de-
manded by these needs. It is almost axiomatic that
serious stressors, especially those that are chronic,
generate other stressors. We conceive of the de-
mands of caregiving as encompassing primary stress-
ors that in turn lead to other problems and hard-
ships, which we refer to as secondary. The labels of
primary and secondary are not intended to suggest
that one is more important than the other but only to
point up that a configuration of interrelated stressors
can and often does emerge as individuals are im-
mersed in the long-term care of an impaired relative.
Primary stressors. One indicator of a primary
stressor is the cognitive status of the Alzheimer's
patient. The range and difficulty of caregiving activi-
ties and the ability of caregivers to manage their
relationships with their impaired relatives grow out
of the patient's memory loss, communication defi-
cits, and recognition failures. The evaluation of cog-
nitive status, although made by the caregiver, is
based on standard tests typically used in the clinic
(Folstein, Folstein, & McHugh, 1975). The questions
asking about cognitive status can be found in Appen-
dix A. Questions about the validity of caregivers'
judgments of patients' cognitive functioning may
understandably arise. In this regard, it can be noted
that about 75 of our participants care for relatives
who are clients of the Northern California Alzhei-
mer's Disease Center, where independent clinical
tests were administered to the patients. There is a
strong correlation (r = .65) between the ratings care-
givers give their relatives on our scale of cognitive
functioning and the ratings of the same relatives
made by clinical workers using the Mini-Mental Test.
It would appear that caregivers are quite able to
evaluate the cognitive abilities of their relatives with
a high degree of accuracy.
A second and somewhat related indicator of a
primary stressor entails the problematic behavior of
the patient and the surveillance, control, and work
such behaviors require on the part of the caregiver
(Appendix B). The level of vigilance that must be
maintained and the "damage control " that must be
exercised to ensure that the patient harms neither
himself nor others constitute, from all indications, a
formidable stressor (Pruchno & Resch, 1989). More-
over, the special kind of attention required by such
behavior serves as a constant and painful reminder of
the changed persona of the patient.
A third indicator of a primary stressor is familiar to
many studies of caregivers. It consists of the number
of activities for which the impaired person is depen-
dent on the caregiver and the extent of dependency
for each activity. Activities for which this information
is gathered are fairly standard (and, therefore, not
appended) and include both those involved in satis-
fying daily needs (ADL) and instrumental logistical
needs (IADL) (Katz et al., 1963; Lawton & Brody,
1969). It can be assumed that the more dependent
impaired persons are, the greater is the sheer
amount and difficulty of work caregivers must per-
form for them. Although it is entirely reasonable to
treat daily dependencies as an indicator of hardship,
research results do not show that the condition of
the patient has a strong or consistent relationship to
caregiver stress (e.g., George & Gwyther, 1986). It
would seem that the magnitude of the workload by
itself is not a potent stressor. We have learned,
however, that when the efforts of the caregiver to
satisfy daily and instrumental needs are met by resist-
ance on the part of the recipient, then stress is more
likely to result. Having to satisfy dependencies is by
itself less difficult than having to do it with a recalci-
trant relative. Consequently, we added to the assess-
ment of daily dependencies a single question regard-
ing the patient's overall resistance to help.
Daily dependencies, problematic behaviors, and
cognitive status are objective indicators of stressors
in the sense that they are based on the health, behav-
ior, and functional capabilities of the impaired rela-
tive. From this kind of information about patients,
inferences can be drawn about the custodial care and
attention the patient needs and the demands and
hardships caregivers presumably encounter. It is also
likely that the scope and difficulty of caregiving activ-
ities come to symbolize the changes that have over-
taken the life and the self of the caregiver. Thus,
these objective assessments of the patients' behav-
iors and capabilities serve two purposes in our
model: as indicators of the current demands of care-
giving and as benchmarks of transformations that
have already occurred and those that are expected.
Two additional indicators of primary stressors by-
pass the condition of the patient and inquire directly
about hardships subjectively experienced by care-
givers. One of these taps the overload or burnout felt
by caregivers (Appendix C). The items constituting
the measure bespeak not only the level of fatigue felt
by caregivers but also the relentlessness and uncom-
promising nature of its source. The other we refer to
as relational deprivation. As we have emphasized,
Alzheimer's disease and other dementias have a
transforming effect on the patient and this, then,
unavoidably restructures the caregiver-patient rela-
tionship, stripping it of its former reciprocities. As
the impairment progresses, caregivers may come to
feel increasingly separated from the parts of their
lives that have been supported by or shared with
their relatives.
The items making up the measure of relational
587 The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
deprivation are found in Appendix D. It can be noted
that this measure is divided into two subscales. One
involves the exchange of intimacy, seen in items A, B,
and C. The second pertains more to goals and social
activities that were once shared with the patient but
that are no longer attainable. This is tapped by items
D, E, and F. Although each subscale forms a distinct
factor, these two aspects of relational deprivation are
related to each other (r = .52).
Secondary stressors: Role strains and intrapsychic
strains. The stressors identified thus far are an-
chored either in the needs and demands of the
patient and the caregiving required to satisfy them or
in the restructured relationship between caregiver
and patient. Although they may plateau or even re-
cede, we assume that the natural history of these
kinds of stressors is in the general direction of
greater severity. Thus, the primary stressors are
likely to be both durable and intensified over time.
These conditions are productive of other stressors,
those we call secondary. As seen in Figure 1, we
distinguish two types of secondary stressors. One
type, comprising role strains, is found in roles and
activities outside the caregiving situation. The sec-
ond is made up of a variety of intrapsychic strains. It
should be reemphasized that neither type is second-
ary in terms of their potency. Once established,
there is reason to believe that secondary stressors
are every bit as powerful as those that are primary in
producing stress outcomes.
The family, of course, is a central arena for second-
ary role strains (e.g., Rabins, Mace, & Lucas, 1982),
and having a close relative who needs care can cer-
tainly reawaken old family grievances and create new
ones as well. Three dimensions of conflict were iden-
tified in exploratory interviews and developed as
scales for use in our survey (Appendix E). As seen in
Appendix E, the sheer level of conflict along these
dimensions is modest. However, because people
typically have a strong stake in family relations, any
threat to them can have a strong impact (Pearlin &
Turner, 1987). One type of conflict between care-
givers and other family members arises out of differ-
ences around issues of impairment: beliefs about
the disability of the patient, its seriousness, and
appropriate strategies for dealing with it. A second
conflict, also between the caregiver and other rela-
tives of the disabled person, is rooted in disagree-
ments over both the amount and quality of attention
given to the patient by the other family members.
The third dimension of conflict is around the atten-
tion and acknowledgment accorded the caregiver for
the care that person gives to the relative. The inter-
correlations between these three dimensions are
quite high: between the issues and patient scales r =
.55; between issues and caregivers r = .51; and for
the measures of conflicts involving the patient and
the caregiver r = .71. Despite their close interrela-
tionships, they appear to be quite different in their
effects, with conflicts directly involving the caregiver
most likely to arouse distress.
Occupation is another institution in which prob-
lems and conflicts are likely to have serious conse-
quences. It is entirely possible that occupation,
along with incumbency in other outside roles, may
have some beneficial effects for caregivers (Stoller &
Pugliesi, 1989). However, our exploratory interviews
have confirmed earlier studies (e.g., Scharlach &
Boyd, 1989) showing that caregivers who are em-
ployed outside the home frequently experience
cross-pressures and dilemmas at the junctures of
caregiving and occupation. Our measure of job-care-
giving conflicts appears in Appendix F.
Economic strains, too, can be formidable. These
strains are appraised by three indicators: reductions
in household income, increases in expenditures re-
lated to the care and treatment of the patient, and
whether there is enough money to make ends meet
month to month (Appendix G). The answer to these
three queries can be independent of one another,
and therefore, there is no basis for scaling the items.
Furthermore, it can be recognized that economic
hardships might have existed prior to and indepen-
dently of the impairment of the relative and of the
caregiving situation. Therefore, the causal links of
impairment and caregiving to economic strains are
best established by observing changes in the eco-
nomic circumstances of the household at the multi-
ple points of the interviewing.
A final secondary role strain involves informal
rather than institutional roles and statuses. There is
often a marked constriction of social and recrea-
tional life as caregiving responsibilities escalate.
These social activities, in which one no longer en-
gages at previous levels, can be longingly missed. To
evaluate the constriction of social life we rely on the
extensive information we have gathered about con-
tacts and activities with friends and relatives and their
changes overtime.
An underlying premise of our conceptual scheme
is that one set of stressors can lead to another. As
noted earlier, we refer to role strains as secondary
stressors because they are viewed as an outgrowth of
the ongoing caregiving situation. Another type of
stressor is distinctly different from the role strains
but, because it is under the influence of other stress-
ors, is also considered to be secondary. These are
what we refer to as intrapsychic strains, which, for
the most part, involve dimensions of self-concept
and kindred psychological states. Past research has
indicated that under conditions of enduring hard-
ships, self-concepts may be damaged (Pearlin et al.,
1981), and when this happens, people are more likely
to suffer symptoms of depression. Caregiving to
chronically disabled relatives fits this scenario. The
relentless and progressively expanding demands of
caregiving, together with ensuing secondary role
strains, are capable of diminishing positive elements
of self; this, in turn, leaves people increasingly vul-
nerable to stress outcomes. In the conceptual frame-
work portrayed by Figure 1, the intrapsychic strains
represent the final but crucial step in an antecedent
process.
Some of the self-concepts in which we are inter-
ested have traditionally been labeled in positive
Vol. 30, No. 5,1990 588
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
terms. These positive labels might appear discrepant
with our references to stressful intrapsychic strains;
however, what is regarded as strainful is not the
presence of a positive self-concept but either its di-
minishment or barriers to its development. This is
certainly the case with self-esteem and mastery, two
elements of self-concept that have been closely stud-
ied in earlier stress research (Pearlin etal ., 1981). Self-
esteem, which simply refers to the regard in which
one holds oneself, is measured by the Rosenberg
(1965) scale. Mastery, or the control that individuals
feel they are able to exercise over forces importantly
affecting their lives, is measured by a scale previously
developed by Pearlin (Pearlin & Schooler, 1978).
Self-esteem and mastery represent rather global
and overarching elements of self. That is, they are
constructs whose assessment is not tied to a particu-
lar context. In our current study of caregivers, we
sought to expand our understanding of the place of
the self in the stress process by including dimensions
of self-concept that are anchored specifically in the
caregiving situation and whose measurement re-
flects this context. There are four of these, one of
which is role captivity (Appendix H). This is an intra-
psychic strain that refers to being an unwilling, invol-
untary incumbent of a caregiver role. Essentially, the
sense of being a captive exists when one wants to be
and to do something other than that in which they
feel compelled to engage. It is a concept that first
emerged in a study of gender and depression
(Pearlin, 1975) and was identified as an underlying
theme in some of our exploratory interviews with
caregivers. The loss of self is yet another theme that
emerged from these exploratory interviews. To the
extent that the identity and life of the caregiver has
been closely bound to that of the patient, the care-
giver may experience a loss of his or her own identity
as the patient's persona becomes fragmented and
blurred. This loss may also be exacerbated when
caregiving comes to exclude other activities and
roles in which the caregiver previously found self-
validation. Self-loss is measured by a simple two-
item scale (Appendix I).
Two additional measures of intrapsychic strain,
each phrased in positive terms, are competence and
gain. Competence is measured by a four-item scale
that essentially asks people to rate the adequacy of
their performance as caregivers (see Appendix J).
The measure of personal gain or enrichment (Appen-
dix K) is testimony to the fact that many people
manage to find some inner growth as they face the
severe challenges of caregiving. Competence and
gain were included partly out of interest in whether
the enhancement of self is negatively related to
stress outcomes, just as we knew the diminishment
of self to be positively related to stress. They were
also included to determine if the enhancement of
some elements of self counterbalanced or compen-
sated for the diminishment of others. This issue
awaits further analysis.
These four measures of situational intrapsychic
strain involve closely kindred constructs whose inde-
pendence might be in question. In this regard, it is
useful to note that the intercorrelations among the
measures are not strikingly high. The strongest rela-
tionship (r = .35) is between role captivity and self-
loss, and next in magnitude is the correlation be-
tween role competence and role gain (r = .32). The
correlation between captivity and competence is
- . 17; between self-loss and competence it is - . 13;
and, finally, there is no correlation between self-loss
and gain.
The differentiation in our conceptual model of
primary and secondary stressors and the distinction
between role and intrapsychic strains are heuristi-
cally important. This conceptualization is useful in
revealing the dynamic character of caregiver stress,
especially in multiwave studies extending over a
broad time span. It treats stress not as stemming
from a happening or from a circumscribed problem,
but, rather, from the way caregivers' lives become
organized and the effects of this organization on
their self-judgments. This perspective is particularly
pertinent to caregiving, an activity that can result in
far-reaching and enduring repercussions in the life
of the caregiver and of every other family member in
close contact with the situation. As we shall discuss,
the distinction and specification of primary and sec-
ondary stressors also provides a more detailed pic-
ture of how and where the mediators may potentially
intervene in the stress process.
Mediating Conditions
It is virtually always observed in stress research that
people exposed to seemingly similar stressors are
affected by them in dissimilar ways. This is certainly
the case in studies of caregivers. It is the mediators
that are usually called upon to provide the explana-
tion for this outcome variability. Coping and social
support are generally regarded as the two principal
mediators. Analytic interest in these mediators in the
study of caregivers is essentially the same as in stress
research in general. That is, we seek to learn if differ-
ences in coping responses or in the use of social
support can account for the fact that caregivers con-
fronting equivalent life problems are unequally dam-
aged by the problems. Why is it that some caregivers
seem to fare better than others, though their life
circumstances might not be easier? As we have ar-
gued elsewhere (Pearlin, 1990), the answer to this
question probably cannot be answered solely by the
mediators. Yet there is no doubt that they can have a
major explanatory role.
Indeed, stress research may typically underesti-
mate the power of the mediators. The usual mode of
analysis is to determine if the strength of the relation-
ship between a stressor and an outcome is reinforced
or attenuated under different mediating conditions
(see Wheaton, 1985, for detailed discussion). Buf-
fering is assumed to take place when the cushioning
effect of the mediator increases with the severity of
the stressor. Buffering is a direct effect in the sense
that its effects can be judged by looking directly at the
outcome. However, the specification of primary and
secondary stressors in Figure 1 suggests that there
589
The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
might also be indirect effects, which, if not observed,
would lead to an underestimation of mediating ef-
fects. We refer specifically to the capacity of the
mediators to limit the proliferation of secondary
stressors. Thus, as suggested by the arrows in Figure
1, the mediators may serve both to lessen the inten-
sity of stressors and to block their contagion at the
junctures between the primary and secondary stress-
ors. To the extent that these kinds of interventions
occur, the mediators would indirectly be limiting del-
eterious outcomes. Obviously, these interventions
need to be examined along with those that more
directly reduce stressors and buffer the outcomes.
Coping. Turning to the assessment of the medi-
ators, we consider coping first. Coping represents
behaviors and practices of individuals as they act on
their own behalf. In keeping with our past research
(Pearlin & Aneshensel, 1986), we conceive of coping
in response to life problems as having three possible
functions: management of the situation giving rise to
stress; management of the meaning of the situation
such that its threat is reduced; and management of
the stress symptoms that result from the situation.
We believe that it is strategically useful to measure
these three functional aspects of coping separately
and, more difficult, to measure each major life exi-
gency with instruments specific to that exigency
(Pearlin, Turner, & Semple, 1989). As others have also
recognized (e.g., Quayhagen & Quayhagen, 1988),
coping with caregiving cannot adequately be as-
sessed with general-duty instruments or with instru-
ments developed to measure how people cope with
other life problems. Our measures meet these crite-
ria: they assess the different functions of coping and
are specific to the study of caregivers.
The items used to measure management of the
situation (Appendix L) are not factored because there
is no theoretical reason to suppose that the items are
correlated in any structured order and, therefore,
they will be analyzed as single items. The items that
measure management of the meaning of the situa-
tion form three distinct factors (Appendix M). One
involves the reduction of expectations (items A, B, &
C), a second the use of positive comparisons (items
D, E, & F), and the third a search for a larger sense of
the illness (items G, H, & I). It can be seen that these
subscales do not have robust reliability coefficients.
Because of their instability, the measures assessing
the management of meaning should be used with
caution. Finally, we have a number of items that tap
individuals' efforts to lessen awareness of the situa-
tion or to decrease the symptoms of stress that result
from it. These items, shown in Appendix N, are not
scaled but will be analyzed separately. Note that the
efficacy of coping cannot be judged solely by the
manifest content of questions asking about coping,
no matter how reasonable the content might appear
to be. As we have described in detail elsewhere
(Pearlin, 1990; Pearlin & Aneshensel, 1986; Pearlin &
Schooler, 1978) the efficacy of coping can be evalu-
ated only through the analysis of its mediating effects
at various junctures of the stress process.
Social support. Our observations concerning
the direct and indirect interventions are as applicable
to social support as to coping. Thus, it should be
determined if, in addition to its direct buffering ef-
fects, social support prevents or inhibits the devel-
opment of secondary stressors. There is, of course, a
sizeable literature on the role of social support in the
stress process and the various ways to measure it
(House & Kahn, 1985; Lin, Dean, & Ensel, 1986). We
rely on assessments of two types of support that are
central to the construct: instrumental and expressive
support. The availability of instrumental support is
measured by discrete items asking, for example,
whether there is someone who assists the caregiver
in the care of the relative or who helps with house-
hold chores. Expressive support is scaled (Appendix
O), with its items tapping the perceived availability of
a person who is caring, trustworthy, uplifting, and a
confidant.
Outcomes
Social scientists are interested in the stress process
because it helps to highlight the structural arrange-
ments of the society and its institutional forces that
affect people's lives. The effects or outcomes
that are usually observed in social research involve
the well-being of people, their physical and mental
health, and their ability to sustain themselves in their
social roles. These are precisely the kinds of out-
comes we have taken for study. On the mental health
side, they include standard symptom measures of
depression, anxiety, irascibility, and cognitive dis-
ruptions. These measures (which are not appended)
are primarily drawn from the Hopkins Checklist (Lip-
man et al., 1969; Derogatis et al., 1971). We also
inquire fairly extensively about caregivers' physical
health, limitations in their ability to engage in usual
activities, and the occurrence of injuries. Still an-
other pivotal outcome is the yielding of caregiver
activities. This can be gradual or abrupt, and it may
entail either the transfer of responsibilities to others
or the institutional placement of the disabled rela-
tive. These kinds of changes will be observed over
the multiple waves of interviewing.
The various outcomes should not necessarily be
treated as interchangeable ways to assess the stress-
ful impact of the antecedent process. It may be more
fruitful to consider the different types and levels of
outcomes as interrelated. Our own view is that ele-
ments of emotional distress are likely to surface first
and, if they persist, they may be eventually inimical
to physical well-being. In instances where there is a
deterioration in both the mental and physical health
of the caregiver, it can be assumed that a reduction
or reluctant yielding of caregiving becomes more
likely to occur. Whether disengagement from active
caregiving helps to promote recovery from its nega-
tive emotional and physical effects remains to be
seen. In any event, it is evident that these kinds of
long-term relationships among outcomes are forged
only under sustained, chronic conditions of stress.
Vol. 30, No. 5,1990 590
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
Discussion
This is a very brief sketch of a complex process
whose components each merit a much more detailed
discussion than provided in this paper. However
brief, the paper is intended to convey some of the
conceptual specification and elaboration needed to
understand the web of conditions joined together as
the lives of caregivers move forward over time. It also
provides an array of newly created measures of the
various concepts. Although the development of
measures is time consuming and painstaking, it is
frequently necessary if we are to have a close union
between concepts and their measures.
We believe that it is useful to think of caregiver
stress not as an event or as a unitary phenomenon. It
is, instead, a mix of circumstances, experiences, re-
sponses, and resources that vary considerably
among caregivers and that, consequently, vary in
their impact on caregivers' health and behavior. The
mix is not stable; a change in one of its components
can result in the change of others. A great deal has
been learned in previous research about these com-
ponents of the stress process and how they are best
measured and evaluated. Obviously, however, much
remains to be learned of how they enter into and
shape the directions of caregivers' lives.
Certain caveats are in order pertaining to our con-
ceptual model or, for that matter, any model. The
constructs that are included and the hypothesized
relationships among them provide only general
guidelines for research. The model should be re-
garded as an heuristic device rather than as a literal
reflection of realities and the pathways that join
them, many of which are still unclear. In the case of
the conceptual framework described here, our past
work provides a level of confidence about its utility.
Yet we are just as confident that as studies of care-
giver stress advance and provide opportunities for
the empirical testing of the model, it will need to be
further modified and extended. Most certainly, some
of the relationships among constructs that we have
treated here as being unidirectional will prove to be
reciprocal. The model, consequently, should be re-
garded as something to be built upon rather than
something to be followed or perpetuated. The
result, we believe, will be a keener appreciation of
informal caregiving, what it entails and what it costs.
References
Brody, E. M. (1985). Patient care as a normative family stress. The Gerontolo-
gist, 25,19-29.
Cooley, C. N. (1915). Social organization. New York: Scribner.
Derogatis, L. R., Lipman, R. S., Covi, L, & Rickles, K. (1971). Neurotic
symptom dimensions. Archives of General Psychiatry, 24, 454464.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: A
practical method for grading the cognitive state of patients for the
clinician, journal of Psychiatric Research, 12,189-198.
George, L. K., & Gwyther, L. P. (1986). Caregiver well-being: A multi-
dimensional examination of family caregivers of demented adults. The
Gerontologist, 26, 253-259.
House, |. S., & Kahn, R. L. (1985). Measures and concepts of social support.
In S. Cohen and S. L. Syme (Eds.), Social support and health. Orlando,
FL: Academic Press.
Katz, S., Ford, R. W., Moskowitz, R. W., Jackson, B. A., & Jaffe, M. W.
(1963). Studies of illness in the aged: The index of ADL, a standardized
measure of biological and psychological function, lournal of the Ameri-
can Medical Association, 186, 914-919.
Lawton, M. P., & Brody, E. M. (1969). Assessment of older people: Self-
maintaining and instrumental activities of daily living. The Gerontolo-
gist, 9,179-186.
Lawton, M. P., Kleban,M. H.,Moss,M., Ravine, M., & Clicksman, A. (1989).
Measuring caregiving appraisal, lournal of Gerontology, 44, P61-P71.
Lin, N., Dean, A., & Ensel, W. (1986). Social support, life events, and
depression. Orlando, FL: Academic Press.
Lipman, R. S., Rickles, K., Covi, L., Derogatis, L., & Uhlenhuth, E. H. (1969).
Factors of symptom distress. Archives of General Psychiatry, 21, 328-338.
Pearlin, L. I. (1975). Sex roles and depression. In N. Datan and L. Ginsberg
(Eds.), Life-span developmental psychology: Normative life crises. New
York: Academic Press.
Pearlin, L. I. (1983). Role strains and personal stress. In H. B. Kaplan (Ed.),
Psychosocial stress: Trends in theory and research. New York: Academic
Press.
Pearlin, L. I. (1985). Social process and social supports. In S. Cohen and S. L.
Syme (Eds.), Social support and health. New York: Academic Press.
Pearlin, L. I. (1989). The sociological study of stress, lournal of Health and
Social Behavior, 30, 241-256.
Pearlin, L. I. (1990). The study of coping: An overview of problems and
directions. In ). Eckenrode (Ed.), The social context of coping. New
York: Plenum Press.
Pearlin, L. I., & Aneshensel, C. (1986). Coping and social supports: Their
functions and applications. In L. H. Aiken and D. Mechanic (Eds.),
Applications of social science to clinical medicine and health. New
Brunswick, N|: Rutgers University Press.
Pearlin, L. I., & Schooler, C. (1978). The structure of coping, lournal of
Health and Social Behavior, 19, 2-21.
Pearlin, L. I., & Turner, H. A. (1987). The family as a context of the stress
process. In S. V. Kasland C. L. Cooper (Eds.), Stress and health: Issues in
research methodology. New York: John Wiley and Sons.
Pearlin, L. I., Turner, H. A.,& Semple, S. |. (1989). Coping and the mediation
of caregiver stress. In E. Light and B. Lebowitz (Eds.), Alzheimer's
disease treatment and family stress: Directions for research. Washing-
ton, DC: National Institute of Mental Health.
Pearlin, L. I., Lieberman, M. A., Menaghan, E. G., & Mullan, |. T. (1981). The
stress process, lournal of Health and Social Behavior, 22, 337-356.
Pruchno, R. A., & Resch, N. L. (1989). Aberrant behaviors and Alzheimer's
disease: Mental health effects of spouse caregivers. Journal of Geron-
tology, 44, S177-S182.
Quayhagen, M. P., & Quayhagen, M. (1988). Alzheimer's stress: Coping
with the caregiving role. The Gerontologist, 28, 391-396.
Rabins, P., Mace, N., & Lucas, M. J. (1982). The impact of dementia on the
family, lournal of the American Medical Association, 248, 333-335.
Romeis, |. C. (1989). Caregiving strain: Toward an enlarged perspective.
lournal of Aging and Health, 1,188-208.
Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, N|:
Princeton University Press.
Scharlach, A. E., & Boyd, S. L. (1989). Caregiving and employment: Results
of an employee survey. The Gerontologist, 29, 382-387.
Shanas, E. (1979). The family as a support system in old age. The Gerontolo-
gist, 79,169-174.
Stoller, E. P., & Pugliesi, K. L. (1989). Other roles of caregivers: Competing
responsibilities or supportive resources, lournal of Gerontology, 44,
S231-S238.
Stone, R., Cafferata, G. L., & Sangl,). (1987). Caregivers of the frail elderly:
A national profile. The Gerontologist, 27, 616-626.
Wheaton, B. (1985). Models for the stress-buffering functions of coping.
lournal of Health and Social Behavior, 26, 352-364.
Young, R. F., & Kahana, E. (1989). Specifying caregiver outcomes: Gender
and relationship aspects of caregiving strain. The Gerontologist, 29,
660-666.
Zarit, S. H. (1989). Do we need another "stress and caregiving" study? The
Gerontologist, 29,147.
Zarit, S. H., Reeves, K. E., & Bach-Peterson, |. (1980). Relatives of the
impaired elderly: Correlates of feelings of burden. The Gerontologist,
20, 649-655.
Zarit, S. H., Todd, P., & Zarit,). (1986). Subjective burden of husbands and
wives as caregivers. The Gerontologist, 26, 260-266.
591
The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
APPENDICES
Note: The reliability (alpha) of each scale is parenthetically
noted next to the name of the scale. Next to each item is
the mean value of responses to the item.
A. Cognitive Status (alpha = .86)
Now, I'd like to ask you some questions about your (rela-
tive's) memory and the difficulty (he/she) may have doing
some things. How difficult is it for your (relative) to:
A. Remember recent events (2.8)
B. Know what day of the week it is (3.0)
C. Remember (his/her) home address (2.4)
D. Remember words (2.0)
E. Understand simple instructions (2.2)
F. Find (his/her) way around the house (1.3)
G. Speak sentences (1.7)
H. Recognize people that (he/she) knows (1.5)
Response categories: (4) Can't do at all; (3) Very difficult;
(2) Fairly difficult; (1) Just a little difficult; (0) Not at all
difficult.
B. Problematic Behavior (alpha - .79)
In the past week, on how many days did you personally
have to deal with the following behavior of your (relative)?
On how many days did (she/he):
A. Keep you up at night (1.8)
B. Repeat questions/stories (2.6)
C. Try to dress the wrong way (2.1)
D. Have a bowel or bladder "accident" (1.9)
E. Hide belongings and forget about them (2.3)
F. Cry easily (1.6)
G. Act depressed or downhearted (2.1)
H. Cling to you or follow you around (2.4)
I. Become restless or agitated (2.6)
J. Become irritable or angry (2.3)
K. Swear or use foul language (1.6)
L. Become suspicious, or believe someone is going to
harm (him/her) (1.8)
M. Threaten people (1.3)
N. Show sexual behavior or interests at wrong time/
place (1.1)
Response categories: (4) 5/more days; (3) 3^4 days; (2) 1-2
days; (1) No days.
C. Overload (alpha = . 80)
Here are some statements about your energy level and the
time it takes to do the things you have to do. How much
does each statement describe you?
A. You are exhausted when you go to bed at night (2.6)
B. You have more things to do than you can handle (2.6)
C. You don't have time just for yourself (2.6)
D. You work hard as a caregiver but never seem to make
any progress (2.4)
Response categories: (4) Completely; (3) Quite a bit; (2)
Somewhat; (1) Not at all.
D. Relational Deprivation
Caregivers sometimes feel that they lose important things
in life because of their relative's illness. To what extent do
you feel that you personally have lost the following? How
much have you lost:
Deprivation of Intimate Exchange: (alpha = .77)
A. Being able to confide in your (relative) (3.1)
B. The person that you used to know (3.3)
C. Having someone who really knew you well (2.6)
Deprivation of Goals and Activities: (alpha = .67)
D. The practical things (he/she) used to do for you (2.0)
E. A chance to do some of the things you planned (2.9)
F. Contact with other people (2.3)
Response categories: (4) Completely; (3) Quite a bit; (2)
Somewhat; (1) Not at all.
E. Family Conflict (Scales created by Shirley J. Semple)
Issues of Seriousness/Safety of AD Patient (alpha = .80)
Family members don't always see eye to eye when it comes
to their relative who is ill. How much disagreement have
you had with anyone in your family concerning any of the
following issues?
A. The seriousness of your (relative's) memory problem
(1.67)
B. The need to watch out for your (relative's) safety (1.41)
C. What things your (relative) is able to do for (him/
herself) (1.46)
D. Whether your (relative) should be placed in a nursing
home (1.49)
Attitudes and Actions Toward Patient (alpha = .86)
Family members may differ among themselves in the way
they deal with a relative who is ill. Thinking of all your
relatives, how much disagreement have you had with any-
one in your family because of the following issues? How
much disagreement have you had with anyone in your
family because they:
E. Don't spend enough time with your (relative) (1.65)
F. Don't do their share in caring for your (relative) (1.61)
G. Don't show enough respect for your (relative) (1.37)
H. Lack patience with your (relative) (1.46)
Attitudes and Actions Toward Caregiver (alpha = .84)
I've just asked you how your relatives act toward your
(relative). Now I'd like to ask how they act toward you, the
caregiver. Again, thinking of all your relatives, how much
disagreement have you had with anyone in your family
because of the following issues? How much disagreement
have you had with anyone in your family because they:
I. Don't visit or telephone you enough (1.39)
J. Don't give you enough help (1.48)
K. Don't show enough appreciation for your work as a
caregiver (1.35)
L. Give you unwanted advice (1.49)
Response categories: (4) Quite a bit of disagreement; (3)
Some disagreement; (2) Just a little disagreement; (1) No
disagreement.
F. Job-Caregiving Conflict (alpha = .75)
From your own personal experience, how much do you
agree or disagree with the following statements about your
present work situation? In the last 2 months or so:
A. You have had less energy for your work (2.4)
B. You have missed too many days (1.8)
C. You've been dissatisfied with the quality of your work
(2.0)
D. You worry about your (relative) while you're at work
(2.6)
E. Phone calls about or from your (relative) interrupt you
at work (2.0)
Response categories: (4) Strongly agree; (3) Agree; (2)
Disagree; (1) Strongly disagree.
Vol. 30, No. 5,1990
592
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
G. Economic Strains (To be assessed by separate items)
These questions ask about your household expenses and
your standard of living. Think back over your financial
situation as it was just before you began to take care of
your (relative).
A. Compared to that time, how would you describe your
total household income from all sources? (3.4)
B. Compared to that time, how would you describe your
monthly expenses? (2.4)
Response categories: (5) Much less now; (4) Somewhat
less now; (3) About the same; (2) Somewhat more now; (1)
Much more now.
C. In general how do your family finances work out at the
end of the month? (1.6)
Response categories: (3) Not enough to make ends meet;
(2) Just enough to make ends meet; (1) Some money left
over.
H. Role Captivity (alpha = .83)
Here are some thoughts and feelings that people some-
times have about themselves as caregivers. How much
does each statement describe your thoughts about your
caregiving? How much do you:
A. Wish you were free to lead a life of your own (2.5)
B. Feel trapped by your (relative's) illness (2.6)
C. Wish you could just run away (1.9)
Response categories: (4) Very much; (3) Somewhat; (2)
Just a little; (1) Not at all.
I. Loss of Self (alpha = .76)
Caregivers sometimes feel that they lose important things
in life because of their relative's illness. To what extent do
you feel that you personally have lost the following? How
much have you lost:
A. A sense of who you are (1.6)
B. An important part of yourself (2.0)
Response categories: (4) Completely; (3) Quite a bit; (2)
Somewhat; (1) Not at all.
J. Caregiving Competence (Scale created by Marilyn M.
Skaff) (alpha = .74)
Here are some thoughts and feelings that people some-
times have about themselves as caregivers. How much
does each statement describe your thoughts about your
caregiving? How much do you:
A. Believe that you've learned how to deal with a very
difficult situation (3.3)
B. Feel that all in all, you're a good caregiver (3.6)
Response categories: (4) Very much; (3) Somewhat; (2)
Just a little; (1) Not at all.
Think now of all the things we've been talking about: the
daily ups and downs that you face as a caregiver; the job
you are doing; and the ways you deal with the difficulties.
Putting all these things together, how (WORD) do you
feel?
C. Competent (3.3)
D. Self-confident (3.3)
Response categories: (4) Very; (3) Fairly; (2) Just a little; (1)
Not at all.
K. Personal Gain (alpha = .76)
Sometimes people can also learn things about themselves
from taking care of a close relative. What about you? How
much have you:
A. Become more aware of your inner strengths (3.3)
B. Become more self-confident (2.7)
C. Crown as a person (2.9)
D. Learned to do things you didn't do before (3.1)
Response categories: (4) Very much; (3) Somewhat; (2)
Just a little; (1) Not at all.
L. Management of Situation (To be assessed by separate
items)
Here are some things that people do to make caregiving
easier for themselves. How often do you:
A. Try to be firm in directing your (relative's) behavior
(2.9)
B. Do the things you really have to do and let the other
things slide (2.9)
C. Try to find ways to keep your (relative) busy (2.5)
D. Try to learn as much as you can about the illness (e.g.,
read books, talk to doctors, go to lectures) (3.2)
Response categories: (4) Very often; (3) Fairly often; (2)
Once in a while; (1) Never.
Have you done anything to try to prevent your (relative)
from having accidents or from wandering? If so, could you
give me one or two examples of something you've done?
M. Management of Meaning
Here are ways that some people think about caregiving,
and about their relative with memory problems. How often
do you think in these ways? How often do you:
Reduction of Expectations (alpha = .48)
A. Try to accept your (relative) as (he/she) is, not as you
wish (he/she) could be (3.4)
B. Try to think about the present rather than the future
(3.3)
C. Try to keep your sense of humor (3.5)
Making Positive Comparisons (alpha = .63)
D. Remind yourself that others are worse off (3.2)
E. Try to think about the good times you had in the past
(2.9)
F. Look for the things that you always liked and admired
in your (relative) (2.9)
Construction of Larger Sense of Illness (alpha = .49)
C. Try to make sense of the illness (2.6)
H. Pray for strength to keep going (3.2)
I. Remind yourself that this is something to expect as
people get older (2.3)
Response categories: (4) Very often; (3) Fairly often; (2)
Once in a while; (1) Never.
N. Management of Distress (To be assessed by separate
items)
Here are things that some people do when they are under
stress from caregiving. How often do you do them?
A. Spend time alone (2.3)
B. Eat (2.0)
C. Smoke (1.4)
D. Get some exercise (2.3)
E. Watch TV (2.6)
F. Read (2.6)
G. Take some medication to calm yourself (1.3)
H. Drink some alcohol (1.4)
Response categories: (4) Very often; (3) Fairly often; (2)
Once in a while; (1) Never.
593
The Gerontologist
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
O. Expressive Support (alpha = .87)
Let's turn now to the help and support you get from your
friends and relatives. Thinking about your friends and fam-
ily, other than your (relative), please indicate the extent to
which you agree or disagree with the following statements.
A. There is really no one who understands what you are
going through (Reversed) (2.8)
B. The people close to you let you know that they care
about you (3.4)
C. You have a friend or relative in whose opinions you
have confidence (3.4)
D. You have someone who you feel you can trust (3.6)
E. You have people around you who help you to keep
your spirits up (3.3)
F. There are people in your life who make you feel good
about yourself (3.4)
G. You have at least one friend or relative you can really
confide in (3.5)
H. You have at least one friend or relative you want to be
with when you are feeling down or discouraged (3.2)
Response categories: (4) Strongly agree; (3) Agree; (2)
Disagree; (1) Strongly disagree.
NEW YORK UNIVERSITY PRESS
New in the CLINICAL GERONTOLOGY SERIES
GROUP WORK WITH
OLDER ADULTS
RONALD W. TOSELAND
This practical guide is for experi-
enced practitioners who wish to
improve their skills in working with
groups of older adults, and also
serves as a primer for students who
want to learn how to do group work.
The first book of its kind, Group Work
with Older Adults offers a compre-
hensive introduction to this form of
clinical intervention with the elderly
population. It examines the particu-
lar issues which arise in treating older
adults and offers many rich case ex-
amples of the varieties of experience
a clinician can expect to face.
224pages/$35.00
New in Paperback!
MENTAL HEALTH
CONSULTATION IN
NURSING HOMES
MICHAEL A. SMYER, DIANE
BRANNON, and MARGARET COHN
Over fifty percent of nursing home
residents suffer from mental impair-
ment. This pathbreaking book ex-
plores effective .ways to assess and
treat these problems and can help
you adhere to the new OBRA regula-
tions. "The most complete book to
date concerning the institutionalized
care of the mentally ill elderly....
Essential reading...." Professor
Bertram J. Cohler, University of Chi-
cago "Scholarly in breadth and
.thoroughness, the authors draw on
their wealth of practical experience
to edify topics on the nursing home
industry..." Carroll Wendland,
President, Beverly Foundation
296pages/$15.00
New in Paperback!
OUTREACH WITH
THE ELDERLY
Community Education,
Assessment, and Therapy
BOB G. KNIGHT
In Outreach with the Elderly, Bob G.
Knight provides concrete directions
for providing successful community
mental health services as well as case
examples to show the day-to-day re-
ality of working with the aged, based
upon a successful and effective pro-
gram that he directed in Ventura,
California.
176 pages I $15.00
n
New York University Press
70 Washington Square South
New York, NY 10003
Phone Orders: (914) 591-9111
Vol. 30, No. 5,1990 594
a
t
U
n
i
v
e
r
s
i
t
i
P
u
t
r
a
M
a
l
a
y
s
i
a
o
n
N
o
v
e
m
b
e
r
2
5
,
2
0
1
2
h
t
t
p
:
/
/
g
e
r
o
n
t
o
l
o
g
i
s
t
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
Вам также может понравиться
- Create PDF With Modern PDF Creator, PDF Printer, PDF Writer, PDF Converter. Buy Full Version NowДокумент1 страницаCreate PDF With Modern PDF Creator, PDF Printer, PDF Writer, PDF Converter. Buy Full Version NowmaazioОценок пока нет
- Comparing Rate of ReactionДокумент2 страницыComparing Rate of ReactionmaazioОценок пока нет
- Comparing Rate of ReactionДокумент2 страницыComparing Rate of ReactionmaazioОценок пока нет
- Choose The Correct AnswerДокумент6 страницChoose The Correct Answerairies92Оценок пока нет
- Zilog DatasheetДокумент282 страницыZilog DatasheetmaazioОценок пока нет
- Math PT3 PDFДокумент34 страницыMath PT3 PDFmaazioОценок пока нет
- Kertas 1 Pep Percubaan SPM Terengganu 2010 - Soalan PDFДокумент24 страницыKertas 1 Pep Percubaan SPM Terengganu 2010 - Soalan PDFmaazioОценок пока нет
- IntegrationДокумент1 страницаIntegrationmaazioОценок пока нет
- Science Activity PDFДокумент2 страницыScience Activity PDFmaazioОценок пока нет
- Bubble Wands Come in A Large Variety of Shapes andДокумент2 страницыBubble Wands Come in A Large Variety of Shapes andmaazioОценок пока нет
- Forecast QuestionДокумент2 страницыForecast QuestionmaazioОценок пока нет
- Math Worksheet - Using Variables PDFДокумент2 страницыMath Worksheet - Using Variables PDFmaazioОценок пока нет
- NOMBOR Cabutan 10Документ1 страницаNOMBOR Cabutan 10maazioОценок пока нет
- Add Math SPM KCM Exam Tips 1®Документ24 страницыAdd Math SPM KCM Exam Tips 1®Ciern TanОценок пока нет
- Internship Program ModuleДокумент2 страницыInternship Program ModulemaazioОценок пока нет
- Evaluating Student Views on Facebook as an Educational EnvironmentДокумент12 страницEvaluating Student Views on Facebook as an Educational EnvironmentmaazioОценок пока нет
- Motion in Straight Line Particle Problems SPM Additional MathematicsДокумент1 страницаMotion in Straight Line Particle Problems SPM Additional MathematicsmaazioОценок пока нет
- ADD MATHS: Function TrigonometryДокумент10 страницADD MATHS: Function TrigonometrymaazioОценок пока нет
- Medical JournalДокумент6 страницMedical JournalmaazioОценок пока нет
- Linear Motion 2008 2011Документ1 страницаLinear Motion 2008 2011maazioОценок пока нет
- Wireless Detection SystemДокумент14 страницWireless Detection SystemmaazioОценок пока нет
- Linear Motion 2012 2013Документ2 страницыLinear Motion 2012 2013maazioОценок пока нет
- Timetable Haziq: Homework Homework Homework HomeworkДокумент2 страницыTimetable Haziq: Homework Homework Homework HomeworkmaazioОценок пока нет
- Facebook Influence To StudentДокумент34 страницыFacebook Influence To Studentmaazio100% (1)
- Program Motivasi FuyoohДокумент5 страницProgram Motivasi FuyoohmaazioОценок пока нет
- Alkane: Carbon CompoundДокумент5 страницAlkane: Carbon CompoundmaazioОценок пока нет
- Evaluating Student Views on Facebook as an Educational EnvironmentДокумент12 страницEvaluating Student Views on Facebook as an Educational EnvironmentmaazioОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Effect of Organizational Culture On Organization Performance in The Case of Commercial Bank of Ethiopia Southern Addis Ababa DistrictДокумент119 страницThe Effect of Organizational Culture On Organization Performance in The Case of Commercial Bank of Ethiopia Southern Addis Ababa DistrictFasilОценок пока нет
- LING150-250 EW - The Silent Finn RevisitedДокумент12 страницLING150-250 EW - The Silent Finn RevisitedЛеит МотифОценок пока нет
- The Metamorphosis Revised-2Документ7 страницThe Metamorphosis Revised-2api-459551001100% (1)
- The Worldwide Distribution and Characteristics of Existential Counsellors and PsychotherapistsДокумент19 страницThe Worldwide Distribution and Characteristics of Existential Counsellors and Psychotherapistsjose nobreОценок пока нет
- Measurement Lesson PlanДокумент3 страницыMeasurement Lesson PlanCaitlin MoreauОценок пока нет
- Full Download Leadership Theory and Practice 8th Edition Northouse Solutions ManualДокумент35 страницFull Download Leadership Theory and Practice 8th Edition Northouse Solutions Manualdanielcmmmadams100% (37)
- Effective Communication Skills for WorkplaceДокумент53 страницыEffective Communication Skills for Workplacefloreson 16Оценок пока нет
- Tosto, Et Al. (2015) - A Systematic Review of ADHD and Mathematical AbilityДокумент14 страницTosto, Et Al. (2015) - A Systematic Review of ADHD and Mathematical AbilityjuanОценок пока нет
- Humanities Training Most ImportantДокумент5 страницHumanities Training Most ImportantSeph TorresОценок пока нет
- Employee Motivation Schedule Test: Practical 3Документ17 страницEmployee Motivation Schedule Test: Practical 3Namal LovesОценок пока нет
- Inverse Zombies, Anesthesia Awareness, and The Hard Problem of UnconsciousnessДокумент6 страницInverse Zombies, Anesthesia Awareness, and The Hard Problem of UnconsciousnessRose DarugarОценок пока нет
- Science 10 q1 Dlp5Документ3 страницыScience 10 q1 Dlp5ndramonedaОценок пока нет
- Psychology ReflectionДокумент3 страницыPsychology Reflectionapi-253517356Оценок пока нет
- Young, Robert 2005 Harold SearlesДокумент11 страницYoung, Robert 2005 Harold SearlesblopОценок пока нет
- Chapter TwoДокумент4 страницыChapter TwoMervi DeypalanОценок пока нет
- Anticipatory ThinkingДокумент3 страницыAnticipatory ThinkingAREEJ RANAОценок пока нет
- DSS & Warehousing Systems: Efrem MallachДокумент13 страницDSS & Warehousing Systems: Efrem MallachsumitОценок пока нет
- The Art of Effective Questioning: Asking the Right QuestionsДокумент3 страницыThe Art of Effective Questioning: Asking the Right QuestionsEjTcherОценок пока нет
- Managing Stress in Time of Covid-19 PandemicДокумент5 страницManaging Stress in Time of Covid-19 PandemicKim Rose BorresОценок пока нет
- Evaluate Teacher Feedback FormДокумент1 страницаEvaluate Teacher Feedback FormAnurag KumarОценок пока нет
- Exploring Curriculum ConceptsДокумент64 страницыExploring Curriculum ConceptsRalph Julius Domingo50% (2)
- DeNisi Sarkar HR PPT Ch07Документ46 страницDeNisi Sarkar HR PPT Ch07Rohit KumarОценок пока нет
- Psychodynamic PsychotherapyДокумент5 страницPsychodynamic Psychotherapyshivani singhОценок пока нет
- Characteristics of Research NotesДокумент3 страницыCharacteristics of Research NotesRaissa Dea100% (2)
- Inmates' Lawsuit Against Allegheny County Jail (Full Text)Документ60 страницInmates' Lawsuit Against Allegheny County Jail (Full Text)jmicekОценок пока нет
- Weekly-Home-Learning-Plans-Q2 PE WEEK 1-8Документ3 страницыWeekly-Home-Learning-Plans-Q2 PE WEEK 1-8Arenas JenОценок пока нет
- Complicated Grief How Is It Conceptualized by ProfessionalsДокумент14 страницComplicated Grief How Is It Conceptualized by ProfessionalsPaula RodriguezОценок пока нет
- Interpretation of The HouseДокумент4 страницыInterpretation of The HouseNelson VersozaОценок пока нет
- Chin, Atkinson, Raheb, Harris - Verson, 2016. The Dark Side of Romantic JealousyДокумент7 страницChin, Atkinson, Raheb, Harris - Verson, 2016. The Dark Side of Romantic JealousySamanta ZuchettoОценок пока нет
- Becoming Partners - Marriage and Its AlternativesДокумент264 страницыBecoming Partners - Marriage and Its AlternativesBotezat-AntonescuRaduAndreiОценок пока нет