Академический Документы
Профессиональный Документы
Культура Документы
Association Between Intraocular...
Загружено:
Selfima Pratiwi0 оценок0% нашли этот документ полезным (0 голосов)
22 просмотров8 страницmata
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документmata
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
22 просмотров8 страницAssociation Between Intraocular...
Загружено:
Selfima Pratiwimata
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
Association Between Intraocular Pressure Variation
and Glaucoma Progression: Data from a United States
Chart Review
PAUL P. LEE, JOHN W. WALT, LISA C. ROSENBLATT, LISA R. SIEGARTEL, AND LEE S. STERN, ON BEHALF
OF THE GLAUCOMA CARE STUDY GROUP
PURPOSE: To evaluate whether greater intraocular
pressure (IOP) variation between visits was associated
with higher likelihood of glaucoma progression.
DESIGN: Cohort study.
METHODS: A ve-year minimum of data (June 1, 1990
through January 22, 2002) was collected on 151 patients
(302 eyes) from 12 United States specialty centers. A
post hoc analysis of visual eld (VF) progression, glau-
coma medication, intraocular pressure (IOP), and other
ocular data was conducted for two nonmutually exclusive
cohorts based on retrospective data abstracted well after
actual patient visits. Mean IOP and standard deviations
(SD) were calculated before treatment (medication or
surgery) or progression, whichever occurred rst, and
before progression regardless of treatment. IOP variables
were assessed in a univariate fashion; Cox proportional
hazards models evaluated glaucoma progression as an
outcome measure and IOP SD as a main predictor,
controlling for covariates.
RESULTS: In cohort 1 (55 patients; 84 eyes), mean age
was 63 years (range, 37 to 85 years), 58% were female,
and 19% of eyes underwent VF progression. In cohort 2
(129 patients; 251 eyes), mean age was 66 years (range,
19 to 88 years), 55% were female, and 27% of eyes
underwent VF progression. Mean IOP was 16.5 mm Hg
(IOP SD, 2.0 mm Hg), and 16.4 mm Hg (IOP SD, 2.7
mm Hg) in cohorts 1 and 2, respectively. Controlling for
age, mean IOP, VF stage, and other covariates, each unit
increase in IOP SD resulted in a 4.2 times and 5.5 times
higher risk of glaucoma progression for cohort 1 (95%
condence interval [CI], 1.3 to 12.9) and cohort 2 (95%
CI, 3.4 to 9.1), respectively.
CONCLUSIONS: IOP variability is an important predic-
tor of glaucoma progression; SD is a convenient measure
of variability to assess glaucoma progression risk. (Am
J Ophthalmol 2007;144:901907. 2007 by Elsevier
Inc. All rights reserved.)
G
LAUCOMA CURRENTLY AFFECTS MORE THAN TWO
million people in the United States. This number
is expected to grow as the number of aging
individuals rises steadily in the United States, with an
estimated 3.36 million individuals affected by 2020.
1
Although it is known that old age, thin corneas, and
elevated or variable intraocular pressure (IOP) are factors
associated with the progression of visual eld loss (VFL)
from glaucoma,
1
half of the individuals affected with
glaucoma are not aware that they have the disease,
leaving them at greater risk for vision loss.
1
Better
detection of the disease and an understanding of what
contributes to progression of glaucoma are needed to
prevent vision loss effectively.
The course of primary open-angle glaucoma (POAG)
has been associated largely with IOP, with the progression
of POAG directly related to elevated IOP.
25
Numerous
studies have explored the predictors for progression of
POAG. The degree of optic nerve damage, resulting from
factors such as varying optic nerve sensitivities to IOP and
vascular insufciencies, has been noted as a key predictor
of glaucoma progression.
6
Other factors such as age, type
and length of treatment provided, and existing visual eld
(VF) damage also are among the prominent predictors of
POAG progression.
4,68
The Early Manifest Glaucoma Trial (EMGT) was de-
signed to evaluate the effect of immediate treatment on
glaucoma progression compared with no initial treatment
or later treatment.
4
The EMGT showed an association
between higher baseline IOP and an increased rate of
glaucoma progression.
1
Specic IOP parameters, such as
mean IOP and IOP variability, recently were examined for
their inuence on POAG progression.
6,7
Continuous sup-
pression of IOP has been found necessary in those with
POAG to minimize disease progression that eventually can
lead to blindness.
9
Various medical and surgical treatments
have focused on lowering a subjects IOP.
Nonetheless, studies have indicated that, although a
lower IOP exhibits a protective effect regarding glaucoma
progression, it does not necessarily indicate that one is free
of risk. In a study by Oliver and associates, patients
becoming legally blind from glaucoma were compared with
those who did not go blind.
6
It was found that progression
Accepted for publication Jul 30, 2007.
From the Duke University Eye Center, Durham, North Carolina
(P.P.L.); Allergan, Inc, Irvine, California (J.W.W.); and Analytica
International, New York, New York (L.C.R., L.R.S., L.S.S.).
Inquiries to Lee S. Stern, Analytica International, 450 Park Avenue
South, 12th Floor, New York, NY 10016; e-mail: lstern@analyticaintl.com
2007 BY ELSEVIER INC. ALL RIGHTS RESERVED. 0002-9394/07/$32.00 901
doi:10.1016/j.ajo.2007.07.040
to blindness was not associated with the mean level of
IOP, but rather with the baseline degree of VF damage and
increased uctuation in IOP levels across visits.
1
Nouri-
Mahdavi and associates investigated glaucoma risk factors
associated with VF progression.
7
Using data from the
Advanced Glaucoma Intervention Study (AGIS 7),
2
they
evaluated sequential VFs for clinically and statistically
signicant change and similarly found that the odds of VF
progression increased by 30% with a one-unit increase in
intervisit IOP variation.
7
Other studies also have found that rates of glaucoma
progression are associated with variability of IOP,
10
both
across visits on different days and within the same
day.
6,1114
Thus, the purpose of this study was to conrm
the ndings that IOP variation (as measured by standard
deviation [SD]) from visit to visit inuences the progres-
sion of VFL among patients cared for by leading glaucoma
specialists.
6,7
A second objective of the study was to
determine how the relationship between IOP variation
and glaucoma progression may differ between naturalistic
(i.e., this study) and clinical trial (i.e., AGIS) settings.
METHODS
STUDY POPULATION: In this retrospective cohort
study, medical charts of 151 patients were reviewed.
Records from June 1, 1990 to January 22, 2002 for patients
18 years of age and older with POAG, normal-tension
glaucoma, ocular hypertension (OHT), or glaucoma sus-
pect diagnosis were selected randomly from 12 specialist
practices across the United States.
15
Institutional review
board exemptions and approvals were obtained for 10 sites
and two sites, respectively. As described in an earlier study
examining resource consumption and direct costs of treat-
ing glaucoma at different levels of disease severity,
15
patient charts were selected randomly from those with at
least ve years of continuous follow-up and International
Classication of Diseases Ninth Edition diagnosis codes
16
for the above conditions. A minimum of ve years of both
clinical and Humphrey VF (HVF) examinations were
required. Initial glaucoma stage was determined based on
the aforementioned developed glaucoma severity system
(Table 1).
17
Medical records were collected from each site
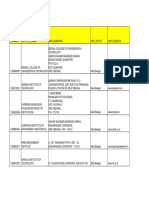
TABLE 1. Criteria for Assigning Glaucoma Stage to Patients
MD Score
Probability Plot (Pattern
Deviation)
Decibel Plot (Stages 2 to 4)
or CPSD/PSD (Stage 1)
Decibel Plot (Stages 2 to 4) or
Glaucoma Hemield Test
(Stage 1)
Stage 0: OHT/earliest
glaucoma
00 Does not meet any criteria for stage 1
Stage 1: early VF loss 0.01 to 6.00 Points 5%: three
contiguous and one
of the points is 1%
CPSD/PSD signicant
at P .05
Glaucoma hemield test
results outside normal
limits
Stage 2: moderate VF
loss
6.01 to 12 Points 5%: 19 to 36;
and points 1%: 12
to 18
Point(s) within central 5
degrees with
sensitivity of 15
dB: one; and
point(s) within central
5 degrees with
sensitivity of 0 dB:
zero
Point(s) with sensitivity
15 dB within 5
degrees of xation:
only in one hemield
(one or two)
Stage 3: advanced VF
loss
12.01 to 20 Points 5%: 37 to 55;
and points 1%: 19
to 36
Point(s) within central 5
degrees with
sensitivity of 0 dB:
one only
Point(s) with sensitivity
15 dB within 5
degrees of xation:
both hemields, at
least one in each
Stage 4: severe VF
loss
20.01 Points 5%: 56 to 74;
and points 1%: 37
to 74
Point(s) within central 5
degrees with
sensitivity of 0 dB:
two to four
Point(s) with sensitivity
15 dB within 5
degrees of xation:
both hemields, two
in each (all)
Stage 5: end-stage
glaucoma/blind
No static threshold
perimetry in
worst eye
Static threshold perimetry not possible because of central scotoma in worst eye or
worst eye acuity of 20/200 because of glaucoma. Best eye may fall into any of
earlier stages.
CPSD corrected pattern standard deviation; MD mean deviation; OHT ocular hypertension; PSD pattern standard deviation; VF
visual eld.
AMERICAN JOURNAL OF OPHTHALMOLOGY 902 DECEMBER 2007
and patients were staged according to glaucoma severity
using this system (from 0 OHT to 5 end-stage
glaucoma). Charts were collected until the group of records
from each site included at least two medical records per stage
for stages 0 to 4 and one record for stage 5.
STAGING SYSTEM DEVELOPMENT AND DEFINITION
OF PROGRESSION: The Bascom Palmer (Hodapp-Ander-
son-Parrish) glaucoma staging system (GSS) was selected
from among several staging systems as the basis for a
six-stage GSS and denition of glaucoma progression.
Based on the actual data elements available in patient
chart data and on expert opinion, modications were made
to the Bascom Palmer GSS to allow it to encompass the
complete range of disease severity to ensure that respective
threshold values within each stage were consistent with
typical VF progression patterns. In particular, visual acuity
was found to be an important addition in assigning
end-stage categorization. To facilitate ease of GSS use,
staging tables were created and were customized for various
types of HVF, including 10-2, 24-2, and 30-2.
17
Staging
criteria for the nal, six-stage GSS are based on HVF, with
mean deviation (MD) as the primary measure.
17
Adjust-
ments can be made depending on corrected pattern stan-
dard deviation or pattern standard deviation and hemield
test results for stages 0 and 1, the numeric (decibel) plot for
stages 2 through 4, and the pattern deviation plot for stages
1 through 4.
17
Stage 5 is based solely on visual acuity and
inability to perform VF testing because of severe loss of
VF.
17
Decision rules used to stage patients, in addition to
the modied GSS staging table, are dened as follows: if a
patient meets the MD criteria for a particular stage (stages
1 to 4) but does not meet one of the additional criteria for
that stage, the patient is categorized in the preceding stage;
if a patient meets the MD criteria for a particular stage
(stages 1 to 4) and meets one of the additional criteria for
a succeeding stage, then the patient is categorized in the
succeeding stage; if a patient meets the MD criteria for a
particular stage (stages 1 to 4) and meets one or more of
the additional criteria for a preceding stage as well as one
or more of the criteria for a succeeding stage, then the
patient is categorized based on MD criteria.
17
DATA ANALYSIS: A Microsoft Access (Microsoft, Inc,
Redmond, Washington, USA) electronic database was
created for data collection purposes; the database included
elds for patient demographic information, past medical
and ocular history including glaucoma risk factors, oph-
thalmologist visits, medications, surgical procedures, and
HVF data. Fields also were created for relevant clinical
examinations and tests and their respective ndings, in-
cluding IOP assessments and diurnal curves, slit-lamp
examinations, gonioscopies, optic nerve assessments, reti-
nal and macular examinations, nerve ber thickness
assessments, optic disk photographs, and dilated eye
examination results. Both eye-level and patient-level
variables were measured. Eye-level IOP variables consisted
of SD of IOP (the variability of serial IOP measurements),
mean IOP (tested as continuous and categorical), change
between best and worst (highest and lowest) IOP, and
change between rst and last IOP. If more than one IOP
measurement was obtained for an eye on a given day (e.g.,
for diurnal curve evaluation), the average of the IOP
measurements for that day was used. Other eye-level
variables considered were: whether there was VFL progres-
sion, stage before progression, presence of surgery before
progression, medication use before progression (tested as
number of medications and yes vs no), and whether
treatment with medication preceded surgery. Patient-level
variables included age, gender, lowest overall VFL stage,
and rst calendar year of follow-up.
Treatment was dened as either receipt of an IOP-
lowering medication (-agonist, -blocker, carbonic an-
hydrase inhibitor, combination -blocker and carbonic
anhydrase inhibitor, sympathomimetic, parasympathomi-
metic, prostaglandin and prostamide) or surgery (laser
trabeculoplasty or trabeculectomy). Patients were grouped
by those who were treated (surgery or medication) before
progression (VFL stage progression) and those who pro-
gressed before receiving treatment (to establish the end of
IOP data collection for each patient).
All analyses beyond descriptive analyses were conducted
with the eye as the unit of analysis (n 302 eyes). Data
analysis was performed using SAS software version 9.1
(SAS Institute, Cary, North Carolina, USA).
UNIVARIATE ANALYSES: Analyses were conducted on
two types of cohorts: cohort 1 had two or more IOP
measurements before treatment or progression (whichever
occurred rst), and cohort 2 had two or more IOP measure-
ments before progression, regardless of whether they had
undergone treatment. These cohorts were not mutually ex-
clusive; that is, all patients in cohort 1 fullled criteria for cohort
2 and therefore were included in cohort 2 analyses. Both cohorts
were based on retrospective and post hoc analyses, with data
abstracted well after the actual patient visits.
In cohort 1, the IOP measurements on dates before
treatment or progression, whichever event occurred rst,
were used to determine mean IOP and SD of IOP. Patients
who did not receive treatment and did not progress had
IOP measurements collected until the end of follow-up.
Each eye in these analyses required a minimum of two
dates before the event on which IOP readings occurred,
because multiple IOP measurements in one day were
averaged into a single IOP value.
In cohort 2, the IOP measurements on dates before
progression were used to determine mean IOP and SDof IOP.
Patients who did not progress had IOP measurements col-
lected until the end of follow-up. Each eye in these analyses
required a minimum of two dates before progression on which
IOP readings occurred, because multiple IOP measurements
in one day were averaged into a single IOP value.
IOP VARIATION AND GLAUCOMA PROGRESSION VOL. 144, NO. 6 903
MULTIVARIATE ANALYSES: A multivariate model was
developed for cohort 1 with POAG VFL progression as the
outcome variable and SD of IOP as a key predictor
variable. Several eye- and patient-level variables were
tested in the model. Eye-level variables included SD of
IOP, mean IOP, absolute difference between best (lowest)
and worst (highest) IOP (also referred to as range of IOP
in the literature), absolute difference between rst and last
IOP, stage before progression, medication use before pro-
gression (tested as two variables: yes or no and number of
medications), and whether treatment with medication
preceded surgery. Patient-level variables tested were age,
gender, lowest overall VFL stage per person, and rst
calendar year of follow-up. The nal model was a Cox
proportional hazards model with progression (time to
progression) as the outcome measure and SD of IOP as the
main predictor, while controlling for covariates. Mean IOP
was included as a continuous variable in the model. All
independent variables of interest with adequate sample size
were tested in a model. Variables with P .2 were
removed from the nal model. Although nonsignicant in
the cohort 1 model, gender was retained because of
previously demonstrated associations between gender and
glaucoma treatment. The Cox proportional hazards model
for cohort 2 was based on the same variables as were used
in cohort 1 as a means of comparison.
RESULTS
DESCRIPTIVE STATISTICS: This study evaluated data
from a chart review of 302 eyes among 151 patients. Mean
age was 66.3 years (SD, 11.9 years). Sixty-three individuals
(42%) in the study population were male, and 86 (57%)
were female. Breakdown by race revealed that 70 patients
(46%) were White, 33 (22%) were Black, and seven (5%)
were Asian; no data on race were available for the
remaining 27%. Of those patients with data available on
family history of glaucoma (n 109, or 72%), 53% had a
positive family history for the disease.
UNIVARIATE ANALYSES: Univariate analyses of cohort
1 were performed to determine IOP variation, as measured by
SD of IOP, before treatment or VF progression, whichever
occurred rst; this cohort consisted of 55 patients (84 eyes).
More than half of these individuals (58.2%) were female. The
patients ranged in age from 37 to 85 years, with the mean age
of this population being 62.9 years (SD, 11.4 years). Among
the eyes examined, 19% were found to have had VF progres-
sion (Table 2). Before progression or treatment, mean IOP
was found to be 16.5 mm Hg, with a mean SD of IOP of 2.0
mm Hg (range, 14.2 to 22.1 mm Hg; Table 2).
Univariate analyses of cohort 2 were performed to
determine IOP variation, as measured by SD of IOP,
before VF progression, regardless of treatment; this
cohort consisted of 129 patients (251 eyes). Demographics
were similar to those of cohort 1: 55% were female, and
mean age was 66 years (SD, 12 years; range, 19 to 88
years). Among these eyes, 27% were found to have had VF
progression (Table 3). Before progression, mean IOP was
found to be 16.4 mm Hg, with a mean SD of IOP of 2.7
mm Hg (range, 4.6 to 27.3 mm Hg; Table 3).
MULTIVARIATE ANALYSES: The Cox proportional haz-
ards model for cohort 1, with VF progression (time to
progression) as the outcome measure and SD of IOP as the
main predictor while controlling for key covariates, found
both the mean and SDof IOP before treatment or progression
to be associated signicantly with the likelihood of progres-
sion. Each 1-mm Hg unit increase in IOP SD increased the
likelihood for glaucoma progression by a factor of 4.2 (95%
condence interval [CI], 1.3 to 12.9). Each 1-mmHg increase
in mean IOP resulted in a 20% increase in likelihood of
glaucoma progression (95% CI, 1.0 to 1.4). An increased
difference between highest and lowest IOP was associated
with a decreased likelihood of progression (odds ratio [OR],
TABLE 2. Demographic Characteristics and Baseline
Ophthalmic Measures of Cohort 1
Descriptive statistics
Mean age (range), yrs 62.9 (37 to 85)
Proportion of females 58.2%
Visual eld progression among the eyes
examined 19%
IOP analyses (mm Hg)
Mean IOP (before progression or treatment) 16.5
Mean SD of IOP (before progression or
treatment) 2.0
IOP intraocular pressure; SD standard deviation.
Cohort 1 consisted of patients with two or more IOP measure-
ments before treatment or progression (whichever occurred
rst); n 55 patients, 84 eyes.
TABLE 3. Demographic Characteristics and Baseline
Ophthalmic Measures of Cohort 2
Descriptive statistics
Mean age (range), yrs 66 (19 to 88)
Proportion of females 55%
Visual eld progression among the eyes
examined 27%
IOP analyses (mm Hg)
Mean IOP (before progression or treatment) 16.4
Mean SD of IOP (before progression or
treatment) 2.7
IOP intraocular pressure; SD standard deviation.
Cohort 2 consisted of patient with two or more IOP measure-
ments before progression, regardless of whether they had
undergone treatment; n 129 patients, 251 eyes.
AMERICAN JOURNAL OF OPHTHALMOLOGY 904 DECEMBER 2007
0.4; 95% CI, 0.3 to 0.7; Table 4). This did not take into
account direction of change, that is, whether a patient had
the lowest IOP before or after the highest IOP.
The Cox proportional hazards model for cohort 2 based
on IOP values before progression demonstrated results
similar to those of cohort 1. Although mean IOP was less
strongly associated with progression, SD of IOP was more
strongly associated with progression in this model; each
1-mm Hg unit increase in IOP SD increased the likelihood
of progression by a factor of 5.5 (95% CI, 3.4 to 9.1), and
each 1-mm Hg increase in mean IOP resulted in a 10%
increase in likelihood of glaucoma progression (95% CI,
1.0 to 1.2). An increased difference between highest and
lowest IOP was associated with a decreased likelihood of
progression (OR, 0.5; 95% CI, 0.4 to 0.6; Table 5). Other
signicant predictors of glaucoma progression in this model
were increasing age (OR, 1.1; 95% CI, 1.0 to 1.1), male
gender (OR, 1.7; 95% CI, 1.1 to 2.9), and receiving
medication in baseline stage (OR, 2.6; 95% CI, 1.3 to 5.4).
However, 79% of eyes received medication in baseline
stage, compared with 37% of eyes in cohort 1, making it
difcult to interpret this result in this model.
DISCUSSION
CONSISTENT WITH PRIOR RESEARCH,
7
THIS STUDY DEMON-
strated that variability in IOP from visit to visit is a
signicant predictor of VFL progression. Specically, the
results of the multivariate analysis indicated that with each
1-mm Hg increase in SD of IOP, glaucoma progression was
4.2 times more likely. Together with results obtained from
the AGIS data showing that IOP variation increased the
odds of VF progression by 30% for each 1-mm Hg increase
in SD of IOP,
7
these results suggest that IOP variation
between visits is a signicant predictor of disease progression
in both clinical trial and naturalistic settings. Unlike patients
seen in AGIS,
2
there were no study protocols determining
the minimum frequency or extent of care, extending the
potential generalizability of the prior ndings.
This study also found evidence for an association be-
tween mean IOP and progression. After controlling for
several key covariates, the multivariate analysis demon-
strated a signicant association between mean IOP and
progression (hazard ratio, 1.2; 95% CI, 1.0 to 1.4). Of note,
this nding contrasts with that of the AGIS analysis,
although the AGIS results did approach signicance.
2
Differences in the different study populations, with less
severely affected patients included prominently in this
study, may help account for the difference.
Interestingly, IOP range, often used as a measure of
variation, was associated signicantly with a decreased
likelihood of progression in both models. It is important to
note, however, that this measurement was based on abso-
lute difference and does not take into account chronology
of highest vs lowest IOP; it is entirely possible that many
patients had wide IOP ranges because of large decreases in
IOP, and therefore had less likelihood of POAG progres-
sion. Further, this may reect the benets of treatment in
lowering IOP in cohort 2, although not in cohort 1. Based
on the results of our analyses, the associated impact of SD
of IOP on VF progression was evident; this was not the
TABLE 4. Cox Proportional Hazards Model Determining
Likelihood of Progression for Cohort 1
Variable
Hazard
Ratio 95% CI P value
Mean IOP (increase in mm Hg) 1.2 1.0 to 1.4 .03
SD of IOP (increase in mm Hg) 4.2 1.3 to 12.9 .01
Absolute difference between
lowest and highest IOP
(increase in mm Hg) 0.4 0.3 to 0.7 .001
Age (increase in yr) 1.1 1.0 to 1.1 .02
Gender (male vs female) 0.8 0.2 to 2.4 .63
Baseline glaucoma stage (higher
vs lower) 0.3 0.1 to 1.4 .12
Received medication in baseline
stage (yes vs no) 0.1 0.03 to 0.5 .004
Best overall stage of patient
(higher vs lower) 4.1 0.8 to 22.6 .10
CI condence interval; IOP intraocular pressure; SD
standard deviation.
Cohort 1 consisted of patients with two or more IOP measure-
ments before treatment or progression (whichever occurred
rst); n 84.
TABLE 5. Cox Proportional Hazards Model Determining
Likelihood of Progression for Cohort 2
Variable
Hazard
Ratio 95% CI P value
Mean IOP (increase in mm Hg) 1.1 1.0 to 1.2 .02
SD of IOP (increase in mm Hg) 5.5 3.4 to 9.1 .001
Absolute difference between
lowest and highest IOP
(increase in mm Hg) 0.5 0.4 to 0.6 .001
Age (increase in yr) 1.1 1.0 to 1.1 .001
Gender (male vs female) 1.7 1.1 to 2.9 .03
Baseline glaucoma stage (higher
vs lower) 0.8 0.6 to 1.2 .37
Received medication in baseline
stage (yes vs no) 2.6 1.3 to 5.4 .01
Best overall stage of patient
(higher vs lower) 1.1 0.7 to 1.7 .62
CI condence interval; IOP intraocular pressure; SD
standard deviation.
Cohort 2 consisted of patients with two or more IOP measure-
ments before progression, regardless of whether they had
undergone treatment; n 251.
IOP VARIATION AND GLAUCOMA PROGRESSION VOL. 144, NO. 6 905
case with IOP range. One also may consider SD of IOP to be
a more accurate measure of variation than range, because it
can capture better the impact of small variations over time,
which range cannot do.
There were important limitations in this study. One
limitation was the relatively small sample size in both
cohorts. However, the study sample is quite diverse, given
the gender proportions and the mix of ethnicities consti-
tuting the sample population. In addition, even with a
small sample size, we were able to detect a statistically
signicant association between IOP variation and glau-
coma progression.
Another possible limitation is that of selection bias. Five
or six or more IOP measurements before treatment or
progression were not available for many participants. In
cohort 1, only patients with a minimum of two IOP
readings before progression or treatment and patients with
minimum two years of follow-up were included in all
analyses. Patients with only one IOP measurement may
have been more or less likely to progress than patients who
had multiple IOP measurements. For example, it is possible
that patients who progressed more rapidly may have had
the opportunity to receive only one IOP measurement
before progression. It therefore is possible that we are
missing a large proportion of patients who progressed from
both model populations. However, the progression rates
noted in our samples here are quite similar to the progres-
sion rates reported with the overall study sample in our
earlier paper with this cohort.
7
Also, it is possible that
patients with at least two readings may have been receiv-
ing better care and therefore were less likely to progress.
The criteria of requiring at least two years overall of
follow-up also may have introduced selection bias. For
example, it is possible that patients with the required
follow-up may have been more likely to progress than
those not included in the study population. Although we
could not account for patients with follow-up of less than
two years, controlling for follow-up time in preliminary
models did not change results signicantly.
Another important factor to consider when looking at
SD of IOP as a measure of variation is the number of IOP
readings used in the calculation. For example, a patient
with the minimum of two visits with IOP readings may
have a large SD, whereas a patient with multiple visits may
end up with a smaller SD because of an increased number
of measurements contributing to the estimate. However,
the number of visits was controlled for in a preliminary
model, and it was nonsignicant, whereas SD of IOP
remained a signicant predictor of progression.
In cohort 2, where the sample size was increased because
of more opportunity for patients to have two dates with
IOP measurements, the results for SD of IOP were even
more signicant than for cohort 1. However in cohort 2,
most patients were taking medication; therefore, looking at
medication use at baseline was not very telling regarding
progression in this population and likely should be elimi-
nated from this nal model.
A major advantage of this study is its real-world study
population. Prior studies of long-term IOP variability have
been clinical trials in which patients tend to receive better
health care than the general population. This chart review
therefore may be even more generalizable than a clinical
trial because of its basis in a real-world patient population
with routine care. Further, it demonstrates that analysis of
intermittent visits carried out in routine care can be
assessed in a meaningful way for variation, such that
variation analyses need not be limited to study-driven
follow-up schedules.
This study demonstrated that SD of IOP is an important
factor related to POAG progression that should be inves-
tigated further. These results indicate that the stability of
IOP over time has an inuence on disease progression that
may be on par or even greater than other parameters such as
mean IOP, age, or glaucoma stage. Monitoring SD of IOP
measurements is a practical method that can be used to
measure potential for disease progression. Practitioners should
consider monitoring patient SD of IOP over the long-term to
ensure that proper treatments are implemented for preven-
tion of POAG progression, whereas other parties may wish to
explore means of making these data easily accessible and
interpretable while seeing patients.
THIS STUDY WAS SUPPORTED BY AN UNRESTRICTED GRANT FROM ALLERGAN, INC, IRVINE, CALIFORNIA. DR LEE IS A
consultant and has received research support and travel funds from Allergan, Inc. Dr Walt is an employee of Allergan, Inc. Drs Rosenblatt and Stern
are employees of Analytica International and were employed by Allergan, Inc, to conduct research and analyses. Dr Siegartel was an employee of
Analytica International at the time this study was conducted. Involved in the design of study (P.P.L., J.W.W.); conduct of study (P.P.L., J.W.W.,
L.C.R.); data collection (P.P.L., L.C.R.); management (J.W.W., L.S.S.); and analysis, interpretation, manuscript preparation, review, and approval
(P.P.L., J.W.W., L.C.R., L.R.S., L.S.S.).
THE GLAUCOMA CARE STUDY GROUP
Paul P. Lee, Duke University Medical Center, Durham, NC John G. Walt, Allergan, Inc, Irvine, CA John J. Doyle, The Analytica Group, New
York, NY Sameer V. Kotak, The Analytica Group, New York, NY Stacy J. Evans, The Analytica Group, New York, NY Donald L. Budenz,
University of Miami, Miami, FL Philip P. Chen, University of Washington, Seattle, WA Anne L. Coleman, University of Washington, Seattle, WA
Robert M. Feldman, University of Texas, Houston, TX Henry D. Jampel, Johns Hopkins University, Baltimore, MD L. Jay Katz, Wills Eye Hospital,
Philadelphia, PA Richard P. Mills, University of Kentucky, Lexington, KY Jonathan S. Myers, Wills Eye Hospital, Philadelphia, PA Robert J.
Noecker, University of Arizona, Tucson, AZ Jody R. Piltz-Seymour, University of Pennsylvania Health System, Philadelphia, PA Robert R. Ritch,
New York Eye & Ear Inrmary, New York, NY Paul N. Schacknow, Palm Beach Eye Foundation, Lake Worth, FL Janet B. Serle, Mount Sinai School
of Medicine, New York, NY Gary L. Trick, Henry Ford Health System, Detroit, MI.
AMERICAN JOURNAL OF OPHTHALMOLOGY 906 DECEMBER 2007
REFERENCES
1. Friedman DS, Wolfs RC, OColmain BJ, et al. Prevalence of
open-angle glaucoma among adults in the United States.
Arch Ophthalmol 2004;122:532538.
2. The Advanced Glaucoma Intervention Study (AGIS): 7.
The relationship between control of intraocular pressure and
visual eld deterioration. The AGIS Investigators. Am J
Ophthalmol 2000;130:429440.
3. Landers J, Goldberg I, Graham SL. Analysis of risk factors
that may be associated with progression from ocular hyper-
tension to primary open-angle glaucoma. Clin Experiment
Ophthalmol 2002;30:242247.
4. Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L,
Komaroff E. Factors for glaucoma progression and the effect
of treatment: the early manifest glaucoma trial. Arch Oph-
thalmol 2003;121:4856.
5. Suzuki Y, Shirato S, Adachi M, Hamada C. Risk factors for
the progression of treated primary open-angle glaucoma: a
multivariate life-table analysis. Graefes Arch Clin Exp Oph-
thalmol 1999;237:463467.
6. Oliver JE, Hattenhauer MG, Herman D, et al. Blindness and
glaucoma: a comparison of patients progressing to blindness
from glaucoma with patients maintaining vision. Am J
Ophthalmol 2002;133:764772.
7. Nouri-Mahdavi K, Hoffman D, Coleman AL, et al. Predic-
tive factors for glaucomatous visual eld progression in the
Advanced Glaucoma Intervention Study. Ophthalmology
2004;111:16271635.
8. Kim J, Dally LG, Ederer F, et al. The Advanced Glaucoma
Intervention Study (AGIS): 14. Distinguishing progression
of glaucoma from visual eld uctuations. Ophthalmology
2004;111:21092116.
9. Grant WM, Burke JF Jr. Why do some people go blind from
glaucoma? Ophthalmology 1982;89:991998.
10. Stewart WC, Hunt HH. Threshold variation in automated
perimetry. Surv Ophthalmol 1993;37:353361.
11. Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Linden-
muth K. Large diurnal uctuations in intraocular pressure are
an independent risk factor in patients with glaucoma. J
Glaucoma 2000;9:134142.
12. Bergea B, Bodin L, Svedbergh B. Impact of intraocular
pressure regulation on visual elds in open-angle glaucoma.
Ophthalmology 1999;106:9971004; discussion 10041005.
13. Sacca SC, Rolando M, Marletta A, Macri A, Cerqueti P,
Ciurlo G. Fluctuations of intraocular pressure during the day
in open-angle glaucoma, normal-tension glaucoma and nor-
mal subjects. Ophthalmologica 1998;212:115119.
14. Wilensky JT. The role of diurnal pressure measurements in
the management of open-angle glaucoma. Curr Opin Oph-
thalmol 2004;15:9092.
15. Lee PP, Walt JG, Doyle JJ, et al. A multi-center, retrospec-
tive pilot study of resource utilization and costs associated
with severity of disease in glaucoma. Arch Ophthalmol
2006;124:1219.
16. Swanson K. International Classication of Diseases, 9th
Revision. Clinical Modication, 5th ed., Vols. 1 to 3. Los
Angeles, California, Practice Management Information
Corp, 1998:1700.
17. Mills RP, Budenz DL, Lee PP, et al. Categorizing the stage of
glaucoma from pre-diagnosis to end-stage disease. Am J
Ophthalmol 2005;141:2430.
IOP VARIATION AND GLAUCOMA PROGRESSION VOL. 144, NO. 6 907
Biosketch
Paul P. Lee is the James Pitzer Gills III, MD, and Joy Gills Professor of Ophthalmology, Vice Chair at Duke Medical
School, Senior Fellow in Duke Center on Aging and Human Development and of Duke Center for Clinical Health Policy
Research, and a glaucoma specialist at Duke, Durham, North Carolina. Dr Lee service activities include Associate
Examiner for the American Board of Ophthalmology, section Editor for several journals, Chair of the AGS Quality of
Care Subcommittee, and Co-Chair of an AMA taskforce.
AMERICAN JOURNAL OF OPHTHALMOLOGY 907.e1 DECEMBER 2007
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- How To Block HTTP DDoS Attack With Cisco ASA FirewallДокумент4 страницыHow To Block HTTP DDoS Attack With Cisco ASA Firewallabdel taibОценок пока нет
- Lecture2 GranulopoiesisДокумент9 страницLecture2 GranulopoiesisAfifa Prima GittaОценок пока нет
- WBДокумент59 страницWBsahil.singhОценок пока нет
- Test 51Документ7 страницTest 51Nguyễn Hiền Giang AnhОценок пока нет
- Government College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniqueДокумент11 страницGovernment College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniquepriyankaОценок пока нет
- Jakub - BaZi CalculatorДокумент3 страницыJakub - BaZi Calculatorpedro restinxОценок пока нет
- PresentationДокумент27 страницPresentationMenuka WatankachhiОценок пока нет
- Case Study 2Документ5 страницCase Study 2api-247285537100% (1)
- 50114a Isolemfi 50114a MonoДокумент2 страницы50114a Isolemfi 50114a MonoUsama AwadОценок пока нет
- Performance Monitoring and Coaching FormДокумент3 страницыPerformance Monitoring and Coaching Formjanine masilang100% (2)
- Patrick Meyer Reliability Understanding Statistics 2010Документ160 страницPatrick Meyer Reliability Understanding Statistics 2010jcgueinj100% (1)
- Lieh TzuДокумент203 страницыLieh TzuBrent Cullen100% (2)
- Sandstorm Absorbent SkyscraperДокумент4 страницыSandstorm Absorbent SkyscraperPardisОценок пока нет
- Where We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Документ1 страницаWhere We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Safia-umm Suhaim- FareedОценок пока нет
- Interlocking Block TechnologyДокумент15 страницInterlocking Block TechnologyChaula Trivedi100% (5)
- Week 4 - Theoretical Framework - LectureДокумент13 страницWeek 4 - Theoretical Framework - LectureRayan Al-ShibliОценок пока нет
- ELEVATOR DOOR - pdf1Документ10 страницELEVATOR DOOR - pdf1vigneshОценок пока нет
- The RBG Blueprint For Black Power Study Cell GuidebookДокумент8 страницThe RBG Blueprint For Black Power Study Cell GuidebookAra SparkmanОценок пока нет
- Aleutia Solar Container ClassroomДокумент67 страницAleutia Solar Container ClassroomaleutiaОценок пока нет
- Cloud Comp PPT 1Документ12 страницCloud Comp PPT 1Kanishk MehtaОценок пока нет
- Notes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0MДокумент1 страницаNotes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0Mسجى وليدОценок пока нет
- SLA in PEGA How To Configue Service Level Agreement - HKRДокумент7 страницSLA in PEGA How To Configue Service Level Agreement - HKRsridhar varmaОценок пока нет
- Kiritsis SolutionsДокумент200 страницKiritsis SolutionsSagnik MisraОценок пока нет
- Sociology As A Form of Consciousness - 20231206 - 013840 - 0000Документ4 страницыSociology As A Form of Consciousness - 20231206 - 013840 - 0000Gargi sharmaОценок пока нет
- LSCM Course OutlineДокумент13 страницLSCM Course OutlineDeep SachetiОценок пока нет
- Technology Based Project: Special Track 1)Документ14 страницTechnology Based Project: Special Track 1)Kim ChiquilloОценок пока нет
- Clockwork Dragon's Expanded ArmoryДокумент13 страницClockwork Dragon's Expanded Armoryabel chabanОценок пока нет
- Biography Thesis ExamplesДокумент7 страницBiography Thesis Examplesreneewardowskisterlingheights100% (2)
- Department of Education: Republic of The PhilippinesДокумент1 страницаDepartment of Education: Republic of The PhilippinesJonathan CayatОценок пока нет
- ML Ass 2Документ6 страницML Ass 2Santhosh Kumar PОценок пока нет