Академический Документы
Профессиональный Документы
Культура Документы
Cluster Headache Acute and Prophylactic Therapy PDF
Загружено:
rommelsousaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cluster Headache Acute and Prophylactic Therapy PDF
Загружено:
rommelsousaАвторское право:
Доступные форматы
www.medscape.
com
AbstractandIntroduction
Abstract
Clusterheadache(CH)painisthemostsevereoftheprimaryheadachesyndromes.Itischaracterizedbyperiodicattacksofstrictlyunilateralpainassociatedwith
ipsilateralcranialautonomicsymptoms.ThemajorityofpatientshaveepisodicCH,withclusterperiodsthattypicallyoccurinacircannualrhythm,while10%suffer
fromthechronicform,withnosignificantremissionsbetweenclusterperiods.SumatriptaninjectionoroxygeninhalationisthefirstlinetherapyforacuteCHattacks,
withthemajorityofpatientsrespondingtoeithertreatment.ThecalciumchannelblockerverapamilisthedrugofchoiceforCHprevention.Otherdrugsthatmaybe
usedforthispurposeincludelithiumcarbonate,topiramate,valproicacid,gabapentin,andbaclofen.Transitionalprophylaxis,mostcommonlyusingcorticosteroids,
helpstocontroltheattacksatthebeginningofaclusterperiod.Peripheralneuralblockadeiseffectiveforshorttermpaincontrol.Recently,thetherapeuticoptionsfor
refractoryCHpatientshaveexpandedwiththeemergenceofbothperipheral(mostlyoccipitalnerve)andcentral(hypothalamic)neurostimulation.Withtheemergence
ofthesenoveltreatments,theroleofablativesurgeryinCHhasdeclined.
Introduction
Clusterheadache(CH)painisconsideredthemostsevereoftheprimaryheadachesyndromesandisarguablyoneofthemostseverepainsyndromesthatafflict
humans.
[1]
Thedisorderischaracterizedbyattacksofsevere,strictlyunilateralpain,typicallyintheretroorbitalandfrontotemporalareas,associatedwithsymptoms
andsignsofcranialautonomicdysfunction(tearing,conjunctivalinjection,rhinorrhea/nasalcongestion,andHorner'ssyndrome)ipsilateraltothepain.Patientstypically
pacerestlesslyduringanacuteattack.ThehallmarkofCHisthecircadianperiodicityoftheattacks.Also,inepisodicCH(ECH),theclusterperiodsoftenoccurat
predictabletimesoftheyear(circannualperiodicity).RecentimagingstudiesconfirmactivationofthehypothalamusduringCHattacks.
[2]
Thesefindingsmayexplain
thecharacteristicperiodicityofCH.Activationofthetrigeminovascularsystemhasalsobeenshownduringacuteattacks.
ThemanagementofCHincludes:(1)patienteducationaboutthenatureofthedisorder(2)adviceonlifestylechanges(eg,avoidingalcoholduringanactivecluster
period)(3)prompttreatmentoftheacuteattackand(4)prophylactictreatment.Mostpatientscanbemanagedwithmedicaltherapy.Rarely,surgicaltreatmentis
indicated.Recently,neurostimulationhasemergedasatherapeuticoptionforselectpatients.
WeperformedaPubMedsearchoftheEnglishliteraturetofindstudiesontheacuteandprophylactictreatmentofCH.SearchtermswereCHandeachofthe
following:acutetreatment,prophylactic(orpreventive)treatment,triptans,oxygen,ergotamine,dihydroergotamine,lidocaine,somatostatin,octreotide,verapamil,
lithium,topiramate,valproicacid,methysergide,gabapentin,baclofen,melatonin,botulinumtoxin,corticosteroids,neurostimulation,occipitalnerveblock/stimulation,
sphenopalatineganglionblock/stimulation,hypothalamicstimulation,radiofrequency,trigeminalrhizotomy,gammaknifesurgery,microvasculardecompression.Wedid
notlimitoursearchtoaspecifictimeperiod.Wefocusedonclinicalefficacyandtolerabilityofthevariousdrugsandproceduresbasedondatafromhumanstudies.
Weincludedthebestavailablestudiesforeachdiscusseddrugorprocedure.Theserangedfromrandomizedcontrolledtrialsforsometreatments,tosmallcaseseries
ClusterHeadacheAcuteandProphylacticTherapy
AviAshkenazi,MD,ToddSchwedt,MD
Headache.201151(2):272286.
forothers.
TreatmentoftheAcuteAttack(Table1)
Table1.DrugsfortheAcuteTreatmentofClusterHeadache
Therapy
LevelofEvidence
(EFNS
Guidelines)
42,87
*
Dose MoreCommonAEs Comments
Oxygen A
710L/min(higher
flowratesmaybe
needed)
None Inhaledviaanonrebreathablemaskfor1520minutes
SumatriptanSC A 6mg
Nausea,fatigue,paresthesias,
chest/throattightness
Maybetakenuptotwicedailyduringaclusterperiod
contraindicatedinpatientswithCVdiseases
SumatriptanIN A 20mg
Nausea,fatigue,paresthesias,
chest/throattightness,unpleasant
taste
SloweronsetofactionthensumatriptanSC
contraindicatedinpatientswithCVdiseases
ZolmitriptanIN A 510mg
Nausea,fatigue,paresthesias,
chest/throattightness,unpleasant
taste
ComparableinefficacytosumatriptanIN
contraindicatedinpatientswithCVdiseases
OctreotideSC B 100g
Injectionsitepain,abdominalpain,
nausea,hyperglycemia
CanbeusedinpatientswithCVdiseases
LidocaineIN B 1mL(410%) none Onlymoderateeffectonheadpain
Dihydroergotamine
IV,IM,SC,orIN
Notrated 1mg
Nausea,diarrhea,musclecramps,
chesttightness,unpleasanttaste
(IN)
IVprobablythemosteffectiveroutecontraindicatedin
patientswithCVdiseasescannotbeusedwithtriptans
*SeeAppendixfordetailedguidelines.
AEs=adverseeffectsCV=cardiovascularEFNS=EuropeanFederationofNeurologicalSocietiesIM=intramuscularIN=intranasalIV=intravenousL/min=
litersperminuteSC=subcutaneous.
BecausethepainofacuteCHattacksevolvesrapidly,oralmedicationsareusuallynotaseffectiveforthispurposeastheyareformigraineattacks.Forrapidand
effectivepaincontrol,thetherapeuticagentneedstobegivenparenterally.
[1]
Triptans
The5HT
1B/1D
agonists(knownastriptans),inaninjectableorintranasalpreparation,areamainstayofacuteCHtreatment.
[13]
Sumatriptan
Sumatriptan,injectedsubcutaneously,isthedrugofchoiceforacuteCHattacks.
[1]
Theefficacyofthedrugforthisindicationwasexaminedinanumberofwell
designedstudies.
[47]
In1randomized,placebocontrolledstudytheefficacyofsubcutaneoussumatriptan(6mg)foracuteCHtreatmentwasexamined.
[4]
Datafrom
39patientswereevaluated.Headacheseveritydecreasedwithin15minutesinasignificantlyhigherproportionofsumatriptantreated,ascomparedwithplacebo
treated,attacks(74%vs26%).Also,asignificantlyhigherproportionofsumatriptantreatedpatientswerepainfree15minutesafterinjection,ascomparedwiththose
whoreceivedplacebo(46%vs10%).Sumatriptanwaswelltolerated.Inanothercontrolledstudy,subcutaneoussumatriptanatadoseofeither6mgor12mg,or
placebo,wasgivento134CHpatients.
[5]
Fifteenminutesafterinjection,theproportionofpatientswhoexperiencedheadachereliefwas80%,75%and35%for
sumatriptan12mg,sumatriptan6mg,andplacebo,respectively.Thehigherdoseofsumatriptanwasnotsignificantlysuperiortothelowerdose,andwasassociated
withmoreadverseeffects(AEs).Inanopenlabelstudyfromthesamegroup,thelongtermsafetyandefficacyofsubcutaneoussumatriptanwasexaminedin138CH
patients.
[6]
Eachpatienttreatedamaximumof2attacksperdaywithasingleinjectionperattack.Atotalof6353attacks,thatoccurredover3months,were
evaluated.Headachereliefwasobtainedin96%ofattacks.Therewasnoevidencefordecreasedefficacyofthedrugwithcontinueduse.Sumatriptanwaswell
tolerated,andtherewasnoincreaseinAEswithhigherfrequencyofusingthedrug.Inanotheropenlabelstudy,theefficacyandtolerabilityofsumatriptaninCH
treatmentwereevaluatedoveraperiodofupto1year.
[7]
Themaximumdailydoseofsumatriptanwas12mg.Atotalof2031attacks,experiencedby52patients,
wereevaluated.In88%oftheattacks,treatmentwaseffectivewithin15minutesafterinjection,and57%ofpatientswerepainfreeatthattimepoint.Therewasno
significantchangeintheefficacyofthedrugwithrepeateduse.TheresponsetotreatmentofpatientswhohadchronicCH(CCH)wassomewhatlessrobust,and
slowertooccur,ascomparedwiththatofECHpatients.Adverseeffectswerereportedby62%ofpatients.Withdrawalratewas33%,with4(8%)patientswithdrawing
becauseofAEs.
Table1.DrugsfortheAcuteTreatmentofClusterHeadache
Therapy
LevelofEvidence
(EFNS
Guidelines)
42,87
*
Dose MoreCommonAEs Comments
Oxygen A
710L/min(higher
flowratesmaybe
needed)
None Inhaledviaanonrebreathablemaskfor1520minutes
SumatriptanSC A 6mg
Nausea,fatigue,paresthesias,
chest/throattightness
Maybetakenuptotwicedailyduringaclusterperiod
contraindicatedinpatientswithCVdiseases
SumatriptanIN A 20mg
Nausea,fatigue,paresthesias,
chest/throattightness,unpleasant
taste
SloweronsetofactionthensumatriptanSC
contraindicatedinpatientswithCVdiseases
ZolmitriptanIN A 510mg
Nausea,fatigue,paresthesias,
chest/throattightness,unpleasant
taste
ComparableinefficacytosumatriptanIN
contraindicatedinpatientswithCVdiseases
OctreotideSC B 100g
Injectionsitepain,abdominalpain,
nausea,hyperglycemia
CanbeusedinpatientswithCVdiseases
LidocaineIN B 1mL(410%) none Onlymoderateeffectonheadpain
Dihydroergotamine
IV,IM,SC,orIN
Notrated 1mg
Nausea,diarrhea,musclecramps,
chesttightness,unpleasanttaste
(IN)
IVprobablythemosteffectiveroutecontraindicatedin
patientswithCVdiseasescannotbeusedwithtriptans
*SeeAppendixfordetailedguidelines.
AEs=adverseeffectsCV=cardiovascularEFNS=EuropeanFederationofNeurologicalSocietiesIM=intramuscularIN=intranasalIV=intravenousL/min=
litersperminuteSC=subcutaneous.
TheefficacyofintranasalsumatriptaninthetreatmentofacuteCHattackswasexaminedin1placebocontrolledstudy.
[8]
PatientswithECHorCCH,whoseattacks
lastedatleast45minutes,weregivenintranasalsumatriptan20mg,orplacebo.Datafrom154attacks,experiencedby118patients,wereanalyzed.At30minutes
aftertreatment,headacheresponseratesweresignificantlyhigherforsumatriptancomparedwithplacebotreatedattacks(57%vs26%).Thecorrespondingpainfree
ratesatthattimewere47%and18%.Thedrugwaswelltolerated.Anotherstudy,thatwasopenlabel,reportedonlowerefficacyofintranasal,ascomparedwith
subcutaneoussumatriptan,inacuteCHtreatment.
[9]
Alimitationofthatstudy,inadditiontoitsopenlabeldesign,wasthefactthattreatmentoutcomeswere
evaluatedatarelativelyearlytimepoint(15minutesposttreatment).
Insummary,injectablesumatriptaniseffectiveandwelltoleratedforthemajorityofCHpatients.Thedrughasarapidonsetofaction.Itremainswelltoleratedand
effectiveevenwhentakenfrequently(uptotwicedaily)duringaclusterperiod.Therecommendeddoseis6mg,althoughlowerdoses(23mg)maybeeffectivein
somepatients.
[10]
Intranasalsumatriptanappearstobelesseffective,andtohaveasloweronsetofactionthantheinjectablepreparation.Sumatriptanis
contraindicatedinpatientswithcoronaryarterydiseaseorcerebrovasculardisease.BecauseCHtypicallyafflictsmiddleagedmen,manyofwhomsmoke,aclinical
evaluation,orientedtowardtheriskofvasculardiseases,needstobedonebeforeprescribingthedrug.
Zolmitriptan
TheefficacyofintranasalzolmitriptanforacuteCHattackshasbeenstudiedin2controlledtrials.
[11,12]
In1study,92patientsreceivedeitherintranasalzolmitriptan(5
mgor10mg)orplacebo,foracuteattacks.
[11]
Thirtyminutesaftertreatment,headachereliefratesweresignificantlyhigherforzolmitriptancomparedwithplacebo
(62%,40%,and21%forzolmitriptan10mg,zolmitriptan5mg,andplacebo,respectively).PatientswithECHhadhigherresponseratestozolmitriptan(andto
placebo)comparedwiththosewhohadCCH.Zolmitriptanwaswelltolerated.Inasimilarlydesignedstudy,52CHpatientstreated151attackswithintranasal
zolmitriptan(10mgor5mg)orplacebo.
[12]
Zolmitriptan,atbothdoses,wassuperiortoplacebowithregardstoheadachereliefat30minutes(63%,50%and30%for
zolmitriptan10mg,zolmitriptan5mg,andplacebo,respectively).Thecorrespondingpainfreeratesatthattimepointwere47%,39%,and20%.Zolmitriptan,atboth
doses,waswelltolerated.
OralzolmitriptanwasevaluatedasanacutetreatmentforCHattacksinarandomizedcontrolledstudy.
[13]
ThedrugwasfoundtobesuperiortoplaceboinECH,but
notCCH,patients.Thirtyminutesaftertreatment,headacheresponseratesinECHpatientswere47%and29%,forzolmitriptan10mgandplacebo,respectively.
Insummary,intranasalzolmitriptanmaybeusedfortheacutetreatmentofCH,withcomparableefficacytothatofintranasalsumatriptan.Oralzolmitriptanhasonly
limitedefficacyforthispurpose.Aswithsumatriptan,zolmitriptaniscontraindicatedinpatientswithahistoryofcardiovascularorcerebrovasculardisease.
Oxygen
OxygeninhalationhasbeenusedforthetreatmentofacuteCHattacksfordecades.
[1]
ThemajoradvantageofoxygenisthevirtuallackofAEs.Asopposedto
triptans,oxygencanbegiventopatientswithahistoryofcardiovascularorcerebrovasculardisease.ThemechanismofactionofoxygenonCHhaslongbeenrelated
toitsvasoconstrictiveeffect.
[14]
Morerecently,however,ithasbeenshownthatoxygeninhibitsneuronalactivationinthetrigeminalnucleuscaudaliswhenthis
activationisinitiatedbystimulationoftheparasympatheticoutflowthroughthefacialnerve.
[15]
OxygenhasbeenevaluatedasanacutetreatmentofCHinanumber
ofstudies.
[16]
Inanopenstudy,KudrowexaminedtheefficacyofoxygenforacuteCHattacksin52patients.
[17]
Oxygen100%wasinhaledviaafacialmaskatarate
of7liters/minute(L/min)for15minutes.Thirtynine(75%)patientsexperiencedsignificantpainreliefwithin15minutes.Thebestresponsewasobservedinyounger
(<50yearsold)patientswhohadECH.FoganexaminedtheefficacyofoxygenforacuteCHinadoubleblindcrossoverstudy.
[18]
Nineteenmenweretreatedwith
eitheroxygen,orairinhalation,atarateof6L/min.Aftertreatment,averagepainreliefscorewassignificantlyhigherforoxygen,ascomparedwithair.Rozen
examinedtheeffectofhighflowoxygenonCHpainin3patientswhohadbeenrefractorytooxygengivenatthestandardflowrateof710L/min.
[19]
All3patients(2
withCCHand1withECH)hadcompleteornearcompleteheadacheresponseafterinhaling100%oxygenatarateof1415L/min.Twoofthepatientswereheavy
smokers.Theauthorsuggestedthatpatientswhofailtorespondtooxygenatthestandardflowrateshouldbetriedonhigherflow.Inarecentlargecontrolledtrial,
CohenetalexaminedtheefficacyofhighflowoxygeninthetreatmentofacuteCHattacks.
[20]
Atotalof109patientstreated4CHattackswitheitheroxygen(12
L/min)orinhaledair,givenviaafacialmaskfor15minutes.Oxygenwassignificantlysuperiortoplacebowithregardstotheprimaryendpoint(eliminationofpainor
"adequatepainrelief"at15minutes78%vs20%,withoxygenandair,respectively).
Hyperbaricoxygen(HBO)hasalsobeenstudiedasatreatmentforacuteCHattacks.
[21,22]
WeissetaltreatedaCHpatientwithhyperbaric(2atmospheres)100%
oxygen,aftershehadbeenrefractorytoconventionaloxygentherapy.
[21]
TwoattacksweretreatedwithHBO,withpromptandcompletepainrelief.DiSabatoetal
treated7ECHpatientswithHBOinaplacebocontrolledstudy.
[22]
Sixpatientsrespondedwelltotreatment,withinterruptionoftheirattack.Moreover,in3ofthe
responderstheCHperiodendedafterHBOtreatment.Placebotreatmenthadnoeffectonpain.
Insummary,normobaricoxygenisaneffectivetreatmentofacuteCHattacksinthemajorityofpatients.ItiswelltoleratedandhasvirtuallynoAEs.Asopposedto
triptans,thereisnolimitationtothenumberoftimesperdayitcanbeused.Apropertechniqueofuseiscrucialforgoodresultswithoxygentherapy.Thepatient
shouldbeinstructedtousetheoxygenviaanonrebreathablemask,atarateof710L/min,inasittingposition,foratleast1520minutes.Patientsmayincrease
theflowrateupto15L/minifneeded.Theoptimalflowrateshouldbedeterminedindividuallyforeachpatient.Themajordisadvantageofoxygentherapyisits
inconvenienceofuse,particularlywhenthepatientisoutofhome.Portableoxygentanksareavailableforpatientswhowishtouseitinthesecircumstances.Oxygen
therapyforCHshouldbeusedwithcaution,orevenavoided,inpatientswithchronicobstructivepulmonarydisease,becauseoftheriskofrespiratorydepression.HBO
maybeconsideredforrefractoryCHpatients.However,becausethisisnotareadilyavailabletherapy,andthereisnoevidenceforasustainedeffectofitonCH,
[23]
themajorityofpatientsarenotlikelytobenefitfromit.
ErgotamineandDihydroergotamine
ErgotderivativeswereamongthefirstagentstobeusedinCHtreatment.Reportsontheefficacyofergotamineforthisindicationdatebacktothe1940sand1950s.
[1]
Thesedata,however,werebasedonsmall,openlabelstudiesandoncasereports.Thedrughasnotbeenevaluatedincontrolledstudiesforthisindication.
Kudrowcomparedtheefficacyofsublingualergotaminewiththatofoxygenin50patientswithCH.
[17]
Theresponseratetoergotaminewas70%,ascomparedwith
82%foroxygen(withnosignificantbetweengroupdifference).Oxygenwasbettertoleratedthanergotaminehowever,thelatterwasmoreconvenienttouse.Because
oflimitedavailabilityandpotentiallyseriousAEs,mostnotablythoserelatedtothedrug'svasoconstrictiveeffect,ergotamineiscurrentlyrarelyusedforacuteCH.
Dihydroergotamine(DHE)isavailableininjectable(intravenous,intramuscular,orsubcutaneous)andintranasalformulations.Althoughnodatafromcontrolledtrials
areavailable,clinicalexperiencesuggestsefficacyofintravenousDHEforacuteCH.Thistreatment,however,isnotpracticalforthemajorityofpatientsbecauseof
thedifficultyinreceivingitpromptlywithattackonset.Basedonourclinicalexperience,intramuscularandsubcutaneousDHEinjectionsarenotaseffectiveasthe
intravenousroute,although,toourknowledgetherearenostudiesthatcomparedthevariousroutesofadministrationofthedrugforCH.Theefficacyandtolerability
ofintranasalDHE(1mg)inthetreatmentofacuteCHwasexaminedinacontrolledstudyof25patients.
[24]
IntranasalDHEdecreasedtheintensity,butnotthe
duration,oftheattacks,andwaswelltolerated.Theauthorssuggestedthatthemoderateefficacyofthedrugintheirstudymayhavebeenrelatedtothedosethey
used.Theyrecommendedthatthedrugbeexaminedatahigherdoseinfuturetrials(themaximalrecommendeddoseofintranasalDHEforacuteheadache
treatmentinadultsis2mg).
Insummary,becauseofthemoderateefficacyofmostergotpreparationsandthedifficultyofreceivingintravenousDHE(probablythemosteffectivepreparationfor
thispurpose)inatimelymanner,theroleofergotsintheacutetreatmentofCHislimited.
Lidocaine
DataontheefficacyoflocallyappliedlidocaineonacuteCHattacksarederivedfromseveralnoncontrolledstudiesand1randomizedcontrolledtrial.
[2528]
Kittrelleet
alexaminedtheeffectoflidocaine,appliedtopicallytothesphenopalatinefossa,onacuteCHattacks.
[25]
Fourofthe5treatedpatientsexperiencedrapidrelieffrom
painandassociatedsymptomsofnitrateinducedCHattacks.Thetreatmentwasalsoeffectiveforspontaneousattacks.Inanotherstudy,HardeboandElner
examinedtheeffectoflidocaine4%,selfappliedusinganasaldropperthroughthenostrilipsilateraltothepain,onCHpainandassociatedsymptoms.
[26]
Twentyfour
patientswerestudied,withmoderatelypositiveresults.Robbinsexaminedtheeffectofintranasallidocaine,administeredthroughaspraybottle,onpainin30men
withECH.
[27]
Patientstreated2consecutiveCHattacks.Resultsweremodest,with27%reportingon"moderaterelief,"27%on"mildrelief,"and46%onnorelief.In
aplacebocontrolledstudy,Costaetalexaminedtheefficacyoflidocaine10%,appliedbilaterallytothesphenopalatinefossaviaacottonswabusinganterior
rhinoscopy,onnitroglycerininducedCHattacks.
[28]
Lidocaineapplicationresultedineliminationofpaininall(15)patients.However,therewasaconsiderabledelay(of
37minutesonaverage)betweenthetimeoflidocaineapplicationandpainrelief(thecorrespondingtimeintervalforplacebowas59minutes).
Insummary,intranasallidocaineisatbestmoderatelyeffectiveinthetreatmentofacuteCHattacks.Itshouldnotbeusedasafirstlinetherapyforthisindication.
Thistreatmentmaybeusedasadjunctivetherapyinsomepatientswhoseattacksdonotcompletelyrespondtoother,moreeffective,therapies.
SomatostatinandOctreotide
SicuterietalconductedacontrolledstudytoexaminetheefficacyofintravenoussomatostatinforacuteCHattacks.
[29]
Seventytwoattacks,experiencedby8men,
werestudied.Somatostatininfusionwassuperiortoplacebo,andcomparabletointramuscularergotamine,inrelievingCHpain.Matharuetalevaluatedtheefficacyof
octreotide,asomatostatinanalogthatcanbegivensubcutaneously,foracuteCH.
[30]
Octreotide100gwassignificantlysuperiortoplacebowithregardtoheadache
responserates(52%vs36%).
Animportantadvantageofthesedrugsistheirlackofvasoconstrictiveeffect,makingthemaviabletreatmentoptionforpatientswhocannotusetriptansbecauseof
vasculardiseases.
SummaryTreatmentoftheAcuteAttack
Insummary,injectablesumatriptanandinhaledoxygenarebothafirstlinetherapyforacuteCH.Thedecisiononwhichoftheseoptionstouseshouldbemadeafter
consideringthepatient'smedicalcomorbiditiesandpersonalpreference.Inpatientswhodonotrespondwelltothesetreatments(orinthosewhocannotusetriptans),
somatostatinoritsanalogsappeartobeapromisingtherapeuticoption.Intranasallidocainemaybetriedasadjunctivetherapyinrefractorypatients.
TherearelittledatawithregardtoclinicalparametersthatmaypredictresponsetothevariousacuteCHtreatments.Inaprospectivestudyof246CHpatients,older
agewasapredictorfordecreasedresponsetotriptans,whereasnausea,vomiting,andrestlessnesspredicteddecreasedresponsetooxygen.
[31]
Asopposedto
migraine,therearefewknowntriggerstotheacuteCHattack,mostnotableofwhichisalcohol.Patientsshouldbeadvisedtoavoidalcoholicbeveragesduringa
clusterperiod(or,inthecaseofCCH,toavoiditaltogether).
ProphylacticTherapy
ProphylactictherapyforCHisdividedintomaintenanceprophylaxisandtransitionalprophylaxis.Maintenanceprophylactictherapiesareusedthroughouttheentire
courseoftheclusterperiodwiththeintentofreducingthefrequencyandseverityofclusterattacks.WhentreatingECH,maintenanceprophylacticsaregenerally
discontinuedafterresolutionoftheclusterperiodandthenrestartedattheonsetofthenextclusterperiod.Althoughmaintenanceprophylaxismonotherapyisoptimal,
somepatientswillrequireacombinationofmaintenancemedicationsforadequatecontrolofCH.However,caremustbetakentoavoidpotentiallynegativedrug
interactions.Transitionalprophylacticsareadministeredforshortdurationsasadjunctivetherapiestomaintenanceprophylacticsinanattempttoabortthecluster
periodortofurtherreducethefrequencyandseverityofclusterattacks.Theyareoftenbegunsimultaneouslywithinitiationofmaintenanceprophylaxisbecausethey
tendtoworkmorequicklyandthusprovidecontrolofCHuntilthemaintenancetherapyhastimetotakeeffect.
MaintenanceProphylaxis(Table2)
FirstlineTherapy
Table2.MaintenanceProphylacticTherapyforClusterHeadache
Therapy
LevelofEvidence(EFNS
Guidelines)
42,87
*
TargetDose
perDay
Monitoring MoreCommonAEs
Verapamil A 200900mg EKG Hypotension,constipation,peripheraledema
Lithium
carbonate
B 600900mg
Lithiumlevels,renalfunction,
thyroidfunction
Diarrhea,tremor,polyuria
Topiramate B 50200mg Serumbicarbonate
Paresthesias,weightloss,cognitivedysfunction,fatigue,
dizziness,tastealteration
Valproicacid C 5002000mg CBC,liverfunction Weightgain,fatigue,tremor,hairloss,nausea
Melatonin C 10mg None Fatigue,sedation
Baclofen C 1530mg None Drowsiness,dizziness,ataxia,muscleweakness
Botulinum
toxin
Notrated 50units None Muscleweakness,injectionsitepain
Gabapentin Notrated 8003600mg CBC
Somnolence,fatigue,dizziness,weightgain,peripheral
edema,ataxia
Clonidine Notrated 0.20.3mg None Fatigue,hypotension
*SeeAppendixfordetailedguidelines.
AEs=adverseeffectsCBC=completebloodcountEFNS=EuropeanFederationofNeurologicalSocietiesEKG=electrocardiogram.
Verapamil,acalciumchannelblocker,isthefirstlinemaintenanceprophylacticmedicationforCH.Verapamilisconsideredfirstlinetherapybecauseofitsefficacy,
relativesafety,andtheabilitytocoadministersymptomaticandtransitionaltherapieswithlessconcernaboutdruginteractionscomparedwithsomeoftheother
maintenanceprophylacticmedications(eg,lithiumcarbonate).Inopenlabelstudies,approximately70%ofECHandCCHpatientshavesubstantialimprovementwith
verapamiltherapy.
[32]
InadoubleblindplacebocontrolledtrialofverapamilformaintenanceprophylaxisofECH,15patientswererandomizedto120mgofverapamil
3timesdailywhile15subjectswererandomizedtoplacebo.
[33]
During2weeksoftreatment,80%ofpatientsreceivingverapamilhadagreaterthan50%reductionin
headachefrequency,including4patientswhobecameattackfree.Verapamiltookeffectquickly,withonehalfofrespondershavingsubstantialimprovementwithinthe
firstweekandtheotheronehalfrespondingduringthesecondweek.Meanwhile,zeropatientsreceivingplacebohadagreaterthan50%reductioninheadache
frequency.Adverseeffectsduetoverapamilweremild,withconstipationbeingthemostcommonandmostbothersome.Adoubleblind,crossoverstudyofverapamil
vslithiumcarbonateforCCHsuggeststhatverapamilisasuperiortreatment.
[34]
Inthisrandomizedtrial,eachofthe24subjectsreceivedverapamil360mgperdayor
lithiumcarbonate300mg3timesdailyfor8weeks,andthenfollowinga2weekwashoutperiodwasswitchedtotheothertherapyforanadditional8weeks.
Verapamilandlithiumbothprovidedsimilarreductionsinbothheadacheindexandanalgesicconsumption.However,verapamilworkedmorequickly,withover50%of
patientshavingsignificantimprovementinheadacheindexwithinthefirstweekcomparedwith37%ofthosetakinglithium.Furthermore,only12%ofthosetaking
verapamilreportedAEscomparedwith29%ofthosetakinglithium.
Targetdosagesofverapamilrangingfrom200mgto960mgperdayindivideddosesaretypicallyusedforclusterprophylaxis.
[35]
Mostpatientswillrespondtodoses
of200mgto480mgperday.
[36]
Immediateorextendedreleaseformulationsmaybeused.SlowtitrationsuptothetargetdosemayreduceAEsincluding
hypotension,constipation,andperipheraledema.Amethodoftitratingandtaperingverapamildosagein40mgintervalsisdescribedinapaperbyBlauandEngel.
[36]
EKGmonitoringisnecessaryduringverapamiltherapybecauseoftheriskofheartblockandbradycardia,AEsthatcandevelopwithinitiationoftherapy,increasesin
dose,andevenduringcontinuedstabledosetherapy.
[37]
Inourpractice,weobtainabaselineEKGbeforeinitiatingverapamiltherapy,repeatEKGwitheachincrease
indoseofatleast80mg,andanEKGeach3monthsifthedosehasbeenunchanged.Patientsshouldbeinformedofthepossibilityofdevelopinggingival
hyperplasiabecauseoflongtermuseofverapamil.
Table2.MaintenanceProphylacticTherapyforClusterHeadache
Therapy
LevelofEvidence(EFNS
Guidelines)
42,87
*
TargetDose
perDay
Monitoring MoreCommonAEs
Verapamil A 200900mg EKG Hypotension,constipation,peripheraledema
Lithium
carbonate
B 600900mg
Lithiumlevels,renalfunction,
thyroidfunction
Diarrhea,tremor,polyuria
Topiramate B 50200mg Serumbicarbonate
Paresthesias,weightloss,cognitivedysfunction,fatigue,
dizziness,tastealteration
Valproicacid C 5002000mg CBC,liverfunction Weightgain,fatigue,tremor,hairloss,nausea
Melatonin C 10mg None Fatigue,sedation
Baclofen C 1530mg None Drowsiness,dizziness,ataxia,muscleweakness
Botulinum
toxin
Notrated 50units None Muscleweakness,injectionsitepain
Gabapentin Notrated 8003600mg CBC
Somnolence,fatigue,dizziness,weightgain,peripheral
edema,ataxia
Clonidine Notrated 0.20.3mg None Fatigue,hypotension
*SeeAppendixfordetailedguidelines.
AEs=adverseeffectsCBC=completebloodcountEFNS=EuropeanFederationofNeurologicalSocietiesEKG=electrocardiogram.
SecondlineTherapy
LithiumcarbonateisasecondlinetherapyformaintenanceprophylaxisofCH.Weconsiderlithiumasasecondlinetherapybecauseofitspotentialforcausing
numerousAEs,theneedforbloodtestmonitoringduringtherapy,anditspotentialforcausingseveraldruginteractions.Nonetheless,lithiumcarbonatehasbeen
demonstratedtoprovidesignificantbenefitinthetreatmentofCCH.ItsefficacyfortreatingCCHhasbeendemonstratedintheinvestigationdiscussedin"FirstLine
Therapy"andinastudyof8additionalCCHpatients.
[34,38]
Inthelatterstudy,all8patientshadatleasta75%improvementwithinthefirst2weeksoftherapy.
However,only1of3whowerefollowedlongtermhadcontinuedimprovementafter18monthsoftherapy.Theevidencefortheutilityoflithiumcarbonateforthe
treatmentofECHislessclear,withgenerallysmallstudiesprovidingcontradictoryresults.
[34,38,39]
Lithiumcarbonatedosesof600mgto900mgperdayaretypically
neededtoobtaintargettherapeuticserumlithiumlevelsof0.4to0.8mEq/L.Lithiumserumlevels,renalfunction,andthyroidfunctionshouldbemonitoredduring
lithiumtherapy.CommonAEstolithiumincludediarrhea,tremorandpolyuria.Symptomsandsignsoftoxicityincludenausea,vomiting,diarrhea,confusion,
nystagmus,extrapyramidalsigns,ataxia,andseizures.
Topiramate,indosesrangingfrom50mgto200mgperday,isconsideredsecondlinetherapyforCHprophylaxis.Althoughwehavedesignatedtopiramateas
secondlinetherapy,consistentwiththeGradeBrecommendationintheEuropeanFederationofNeurologicalSocietiesguidelines,topiramateuseforCHprophylaxis
hasbeeninvestigatedinopenlabelstudiesonly.
[4042]
CommonAEstotopiramateincludecognitivedysfunction,paresthesias,alterationintaste,weightloss,fatigue,
anddizziness.Patientswithahistoryofnephrolithiasisshouldnotreceivetopiramatebecauseofanincreasedriskofrecurrentstoneswhiletakingthismedication.
ThirdlineTherapy
Othertherapiesthatmaybeeffectiveformaintenanceclusterprophylaxisincludemethysergide,valproicacid,melatonin,gabapentin,baclofen,clonidine,and
botulinumtoxin.AlthoughmethysergideislikelyeffectiveforpreventingCH,itisnotavailableintheUSAandlongtermuseisassociatedwithfibroticcomplications.
Thus,wecannotrecommenditsuse.Valproicacidhasbeenshowntoprovidebenefitinopenlabelandretrospectivestudiesonly.
[43,44]
Adoubleblindplacebo
controlledstudyofsodiumvalproatedidnotsupportitsefficacyhowever,thismayhavebeenduetoanexceedinglyhighresponserateof62%intheplacebogroup.
[45]
Effectivedosesrangefrom500mgto2000mgdailyindivideddoses.CommonAEsincludeweightgain,fatigue,tremor,hairloss,andnausea.Monitoringwith
completebloodcountsandliverfunctiontestsarenecessaryduringvalproicacidtherapy.Limitedevidencesupportstheuseofmelatoninforclusterprophylaxis.Ina
doubleblind,placebocontrolledtrialof10mgmelatonin,5of10subjectsrandomizedtomelatoninhadclusterremissionwithin5dayswhilenoneofthe10subjects
takingplacebowentintoremission.
[46]
OpenlabelstudiesofgabapentinsuggestitsvalueinmaintenanceprophylaxisofCHindosesrangingfrom800mgto3600mg
perday.
[47,48]
GabapentinistypicallyawelltoleratedmedicationbutmorecommonAEsincludesomnolenceandfatigue,dizziness,weightgain,peripheraledema,
andataxia.Inasmallopenlabelstudyofbaclofen10mg3timesdaily,6of9subjectswentintoremissionwithin1weekandanadditional1subjecthadimprovement
followedbyremissionatweek2.
[49]
Althoughadverseeventswerenotreportedbysubjectsinthisstudy,morecommonAEstobaclofenincludedrowsiness,dizziness,
ataxia,andmuscleweakness.Clonidine,givenasa5mgto7.5mgtransdermalpatch(thatdeliversthedrugatarateof0.20.3mgdailyfor1week),hasbeen
studiedin2smallopenlabelstudies.
[50,51]
Inthefirst,whichincluded8ECHand5CCHpatients,thereweresignificantreductionsinmeanattackfrequency,pain
intensity,andattackduration.
[50]
However,asecondstudyincluding16ECHpatientsfailedtoconfirmthesepositiveresults.
[51]
Tirednessandreductioninblood
pressurewereAEsnotedinthesestudies.AnopenlabelstudyofbotulinumtoxintypeAasaddontherapyin3ECHand9CCHpatientshadmixedresults.
[52]
Fifty
unitsinjectedipsilateraltotheheadacheresultedinheadacheremissionin1CCHpatient,improvementinattackfrequencyandseverityinanadditional2CCH
patients,improvementinacontinuousbaselineheadachewithnochangeinsuperimposedclusterattacksinanadditional1CCHpatient,andnobenefitinthe
remaining8patients.MorecommonAEstobotulinumtoxintherapyincludeweaknessofinjectedmusclesandpainatinjectionsites.
TransitionalProphylaxis
Corticosteroidsareoftenprescribedconcurrentwithinitiationofmaintenanceprophylaxisinordertoquicklyobtainclustercontrol.Oralandintravenouscorticosteroids
maybothprovidebenefit.Varyingdosesoforalprednisone,rangingfrom10mg/dayto80mg/day,wereevaluatedinastudyof9episodicand10chroniccluster
patients.
[53]
Peakprednisonedosewasgivenfor3to10daysandtaperedover10to30days.CompleterelieffromCHwasseenin11patients,3had5099%relief,
3had2550%relief,and2patientshadnobenefit.TheECHandCCHpatientshadsimilarresponses.Investigatorsobservedthatprednisonedosesof40mgor
higherwereneededforbenefit.Headacherecurrencewascommonduringtheprednisonetaper.Otherstudiesoforalprednisonehavehadsimilarresults.
[54,55]
Intravenouscorticosteroids,sometimesfollowedbyoralsteroids,mayalsoprovidebenefitfortransitionalclustertherapy.
[56,57]
Asinglehighdoseofintravenous
methylprednisolone(30mg/kgbodyweightover3hours)deliveredontheeighthdayofanactiveclusterperiodprovided10of13treatedpatientswith2ormoredays
ofattackcessation.
[56]
Themeanintervalbetweensteroidtreatmentandattackrecurrencewas3.8days.Threepatientshadcompleteclusterremission.
Althoughadequatetrialssupportingtheirusearelacking,ergotaminetartrateandDHEmaybeusedfortransitionalprophylaxis.
[58,59]
Inanopenlabelstudy,23ECH
and31CCHpatientswereadmittedtothehospitalfortreatmentwithrepetitiveintravenousDHE.
[60]
AllpatientsbecameheadachefreewhilebeingtreatedwithIV
DHE:10patients(16%)afterthefirstdose,anadditional12(19%)duringthefirstdayofhospitalization,and22(34%)morebecameheadachefreebythesecondday
ofhospitalization.Byday3,greaterthan90%ofpatientswereheadachefreeandbyday5allwereheadachefree.At3monthsafterdischarge,>90%ofECH
patientsand44%ofCCHpatientsremainedheadachefree.Approximately83%ofpatientsreportednoAEsfromIVDHE.ReportedAEsincludednausea,noncardiac
chesttightness,andametallictaste.Ergotaminetartrate,34mgperdayindivideddoses,maybeadministeredfor2to3weeksfortransitionalprophylaxis.
[58,61]
Administrationjustbeforebedtimemayhelptopreventnighttimeattacks.
InvasiveProceduresforClusterHeadacheTreatment
Withanindividuallytailoredpharmacologictreatmentplan,themajorityofCHpatientswillachievesatisfactoryresults.Forthosewhoremainrefractorytomedical
treatment,anumberofinvasiveproceduresareavailable.Theseincludeperipheralnerveblocks,peripheralorcentralneurostimulationand,asalastresort,ablative
surgery.Peripheralnerveblock,mostlytargetingthegreateroccipitalnerve(GON),mayalsobeusedinlessrefractorypatients,asanadjuncttopharmacologic
therapy.
PeripheralNerveandSphenopalatineGanglionBlock
EfficacyofGONblockinCHtreatmentwassuggestedbyAnthonyinthe1980s.
[62]
Morerecently,theprocedurewasinvestigatedasCHtreatmentinanumberof
studies,withthemajorityshowingpositiveresults.
[6366]
PeresetalevaluatedtheeffectofGONblockin14patientswithCH.
[63]
PatientsreceivedGONblock
ipsilateraltotheheadpainusinglidocaine1%andtriamcinolone40mg.Patientswereevaluatedbeforeand1weekaftertheblock.Nine(64%)patientshadgoodor
moderateresponse.Theprocedurewaswelltolerated.Ambrosinietalevaluatedtheeffectofsuboccipitalinjectionoflidocaine2%withbetamethasone,compared
withlidocaineandsaline,in23CHpatientsinarandomized,controlledstudy.
[64]
TheCHattacksdisappearedwithin72hoursin85%ofthelidocaine+
betamethasonegroup(with61%remainingattackfreefor4weeks)comparedwithnoneinthelidocaine+salinegroup.Injectionswerewelltolerated.Afridietal
examinedtheefficacyofGONblock,usinglidocaine2%andmethylprednisolone,inpatientswithrefractorychronicdailyheadache.
[65]
Theirsampleincluded19
patientswithCHwhoreceived22injections.Thirteenoftheinjections(59%)resultedinacompleteorpartialresponse,withamediandurationof12and21days,for
completeandpartialresponse,respectively.Incontrasttotheseresults,Buschetalreportedononlyminorheadacheimprovementin60%of15CHpatientswho
receivedGONblockusingprilocaine.
[66]
Endoscopicallyguidedsphenopalatineganglion(SPG)blockadehasbeenevaluatedbyFelisatietalforCHtreatment.
[67]
Of20refractoryCCHpatientswho
underwenttheprocedure,11experiencedsignificant,albeittemporary,symptomrelief.
PeripheralNerveandSphenopalatineGanglionStimulation
PeripheralnervestimulationmaybeeffectiveandindicatedfortheprophylactictherapyofCCHpatientswhoarerefractoryorintoleranttomedicationtherapy.Several
smallstudieshavenowshownoccipitalnervestimulation(ONS)tobeapromisingtherapyforsuchpatients.EightpatientswithdrugresistantCCH,treatedwith
unilateralONS,werefollowedforanaverageof15.1months.
[68]
Atthetimeoflastfollowup,2of8patientswerepainfree,3hada~90%reductioninheadache
frequency,2had~40%reduction,and1patientderivednobenefit.Twopatientshadsideshiftoftheirclusterattacksrequiringtreatmentwithsuboccipitalsteroid
injection.Complicationsincludedelectrodemigration(n=1),leaddisplacementafterafall(n=1),andthoracicdiscomfortortingling(n=2).BilateralONSwas
investigatedin8patientswithmedicallyintractableCH.
[69]
Atmedianfollowupof20months,subjectiveselfassessmentofbenefitwasgradedassubstantial(90%)
in2patients,moderate(40%)in3,mild(25%)in1,andnilin2patients.SixpatientsreportedthattheywouldrecommendtheuseofONStoothersimilarcluster
patients.Complications,affecting4ofthepatients,included:excessivepainatincisionsite(n=1),electrodemigration(n=3),electrodefracture(n=1),andshock
likesensationbecauseofkinkingofwires(n=1).In2009,resultsfromextendedfollowupofthese8patientsandanadditional6patientstreatedwithbilateralONS
werereported.
[70]
Atamedianfollowupof17.5months,10of14patientsreportedimprovement,including3with>90%improvement,3with4060%improvement,
and4with2030%improvement.NinepatientsstatedthattheywouldrecommendONStootherpatients.Complications/AEsincludedleadmigration,painful
paresthesias,musclerecruitment,neckstiffness,skinpain,andinfection.Meanbatterylifewas15.1months.
TheSPGstimulationmayalsobeaneffectivetreatmentforrefractoryCH.FivepatientswithCCH,refractorytomoreconventionaltherapies,weretreatedwithSPG
stimulationduring18acuteclusterattacks.
[71]
Stimulationresultedincompleteattackresolutionfor11oftheattacks,greaterthan50%reductioninpainseverity
withoutcompleteresolutionfor3attacks,andminimaltonorelieffor4attacks.Benefitsfromstimulationwerenotedwithin1minuteto3minutesoftreatment
initiation.StimulationwaswelltoleratedwithonlymildAEsfromstimulatorplacement,includingtransientepistaxisandtransientmildfacialpain.Further
investigationsofSPGstimulationfortheacuteandprophylactictherapyofCHareneeded.
DeepBrain(Hypothalamic)Stimulation
Leoneetalreportedin2001ona39yearoldmanwithintractableCHwhoseattacksimprovedsignificantlyafterimplantationofastimulatingelectrodetotheposterior
hypothalamus,ipsilateraltothepain.
[72]
Sincethisfirstreport,severalstudieshavebeenpublishedontheefficacyandtolerabilityofhypothalamicstimulation(HS)for
CH.
[7375]
SchoenenetalexaminedtheeffectofunilateralHSin6refractoryCCHpatients.
[73]
Threepatientshad"excellent"results,whileanotherhadonlya
transientremission.In1patienttreatmenthadtobestoppedbecauseofAEs(autonomicdisturbancesandpanicattacks),and1diedofintracerebralhemorrhage
shortlyaftertheprocedure.Leoneetalreportedonthelongtermresultsof16previouslyrefractoryCCHpatientswhohadHS.
[74]
Atameanfollowupof23months,
majorimprovementinpain,orcompletepainelimination,wasobtainedin13(81%)patients.Themeantimetoheadachebenefitwas42days.Overall,theprocedure
waswelltolerated.Nohormonal,affectiveorsleeprelatedabnormalitieswereobserved.Onepatienthadanasymptomaticintracerebralhemorrhagethatsubsequently
resolved.TransientdiplopiawasacommonAEwithhighamplitudestimulation.Bartschetalreportedon6CCHpatientswhounderwentHS.
[75]
Atameanfollowup
of17months,3patientsrespondedwelltotreatment,beingalmostattackfree,while3patientsfailedtorespond.Theprocedurewaswelltolerated.Theauthors
concludedthatHSiseffectiveinasubsetofrefractoryCCHpatients.Interestingly,inanotherstudy,HSwasnoteffectiveinthemajorityofpatientswhenusedasan
acuteCHtreatment,suggestingthatthistreatmentaffectsCHthroughmorecomplexpainmodulatingmechanisms.
[76,77]
Insummary,HSisanemergingviabletreatmentforrefractoryCCH.Itappearstobeeffectiveinsome,butnotall,patients.Althoughthetreatmentisgenerallywell
tolerated,theriskofintraceberalhemorrhage,andevendeath,shouldbekeptinmindwhenconsideringthistreatmentoption.
AblativeSurgicalProcedures
WiththeemergenceofavarietyofpharmacologicandnonpharmacologictherapiesforCH,theroleofablativesurgeryinthisdiseasehasdeclined.
[1]
Candidatesfor
surgeryshouldhavestrictlyunilateral,sidelocked,CHattacks.Anumberofprocedureshavebeenusedwithsomesuccessforthisindication,includingradiofrequency
ablationofthetrigeminalganglion,trigeminalsensoryrhizotomy,gammaknifesurgery,andmicrovasculartrigeminalnervedecompression.
[1]
Radiofrequency
trigeminalgangliorhizolysishasbeenshownaseffectiveinupto75%ofrefractoryCCHpatients.
[78,79]
Inacaseseriesof27patientswhounderwentthisprocedure,2
developedanesthesiadolorosa.
[79]
Othercomplicationsincludedcornealanesthesia,keratitis,anddiplopia.Trigeminalrootsectionhasbeenreportedtobeeffectivein
88%of17patientswithrefractoryCCH,with76%experiencinglongtermpainrelief.
[80]
Complicationsincludedcornealabrasion,masticatorymuscleweakness,
anesthesiadolorosaandthedevelopmentofCHontheotherside.Onepatient,whounderwenttheproceduretwice,diedafterthesecondsurgery.Theauthors
concludedthattrigeminalnervesectionisaviabletherapeuticoptionforselectedrefractoryCCHpatients.Microvasculardecompressionofthetrigeminalnerve,withor
withoutsectionofthenervusintermedius,hasshownsomeefficacyinrefractoryCCHhowever,responseratedecreasedovertime.
[81]
Gammakniferadiosurgeryisa
relativelyrecenttherapeuticapproachforCH.
[82,83]
Despiteearlyencouragingresults,
[82]
morerecentdatashowedonlymodestlongtermpainreliefandhighrateof
AEs,includingdeafferentationpain.
[83]
AnothersurgicalapproachforCHtargetstheparasympatheticcomponentofthedisease,typicallybyblockingorablatingtheSPG.
[67,84,85]
In1study,radiofrequency
blockadeoftheSPGwasperformedin66CHpatients.
[84]
Completepainreliefwasachievedin61%and30%ofECHandCCHpatients,respectively.Inamore
recentstudy,15refractoryCCHpatientsweretreatedwithradiofrequencyablationoftheSPG.
[85]
Thetreatmentdecreasedsignificantlythemeanattackfrequency,
meanpainintensityandpainrelateddisability,andtheseeffectslastedfor1218months.
Insummary,ablativesurgicalproceduresshouldbereservedasthelastresortforrefractoryCHpatients.Theproceduresthatappeartobemoreeffectiveinthelong
termmanagementofthediseaseareradiofrequencytrigeminalganglionablationandtrigeminalrhizotomy.Itshouldbenoted,however,thatCHattackshavebeen
showntopersistaftertrigeminalrootsectioninacasereportofmanwithCH,supportingthehypothesisofacentralpaingeneratorinthisdisease.
[86]
Appendix
EuropeanFederationofNeurologicalSocieties(EFNS)guidelinesevidenceclassificationschemeforatherapeuticintervention
ClassI:Anadequatelypoweredprospective,randomized,controlledclinicaltrialwithmaskedoutcomeassessmentinarepresentativepopulationoranadequately
poweredsystematicreviewofprospectiverandomizedcontrolledclinicaltrialswithmaskedoutcomeassessmentinrepresentativepopulations.Thefollowingare
required:
a. Randomizationconcealment.
b. Primaryoutcome(s)is/areclearlydefined.
c. Exclusion/inclusioncriteriaareclearlydefined.
d. Adequateaccountingfordropoutsandcrossoverswithnumberssufficientlylowtohaveminimalpotentialforbias.
e. Relevantbaselinecharacteristicsarepresentedandsubstantiallyequivalentamongtreatmentgroupsorthereisappropriatestatisticaladjustmentfor
differences.
ClassII:Prospectivematchedgroupcohortstudyinarepresentativepopulationwithmaskedoutcomeassessmentthatmeetsaeorarandomized,controlledtrialina
representativepopulationthatlacks1criteriaae.
ClassIII:Allothercontrolledtrials(includingwelldefinednaturalhistorycontrolsorpatientsservingasowncontrols)inarepresentativepopulation,whereoutcome
assessmentisindependentofpatienttreatment.
ClassIV:Evidencefromuncontrolledstudies,caseseries,casereports,orexpertopinion.
Ratingofrecommendations:
LevelArating(establishedaseffective,ineffective,orharmful)requiresatleast1convincingclassIstudyoratleast2consistent,convincingclassIIstudies.
LevelBrating(probablyeffective,ineffective,orharmful)requiresatleast1convincingclassIIstudyoroverwhelmingclassIIIevidence.
LevelC(possiblyeffective,ineffective,orharmful)ratingrequiresatleast2convincingclassIIIstudies.
AdaptedwithpermissionfromBraininetal.GuidanceforthepreparationofneurologicalmanagementguidelinesbyEFNSscientifictaskforcesrevised
recommendations2004.EurJNeurol200411:577581.
Sidebar
StatementofAuthorship
Category1
a. ConceptionandDesign
AviAshkenazi
b. AcquisitionofData
AviAshkenaziToddSchwedt
c. AnalysisandInterpretationofData
AviAshkenaziToddSchwedt
Category2
a. DraftingtheManuscript
AviAshkenaziToddSchwedt
b. RevisingItforIntellectualContent
AviAshkenaziToddSchwedt
Category3
a. FinalApprovaloftheCompletedArticle
AviAshkenaziToddSchwedt
References
1. MatharuMS,GoadsbyPJ.TrigeminalautonomicCephalalgias:Diagnosisandmanagement.In:SilbersteinSD,LiptonRB,DodickDW,eds.Wolff'sHeadache
andOtherHeadPain,Eighthedn.NewYork:OxfordUniversityPress2008:379430.
2. MayA.Clusterheadache:Pathogenesis,diagnosis,andmanagement.Lancet.2005366:843855.
3. LawS,DerryS,andMooreRA.Triptansforacuteclusterheadache.CochraneDatabaseSystRev.20104:CD008042.
4. TheSumatriptanClusterHeadacheStudyGroup.Treatmentofacuteclusterheadachewithsumatriptan.NEnglJMed.1991325:322326.
5. EkbomK,MonstadI,PrusinskiA,etal.Subcutaneoussumatriptanintheacutetreatmentofclusterheadache:Adosecomparisonstudy.TheSumatriptan
ClusterHeadacheStudyGroup.ActaNeurolScand.199388:6369.
6. EkbomK,KrabbeA,MicieliG,etal.Clusterheadacheattackstreatedforuptothreemonthswithsubcutaneoussumatriptan(6mg).SumatriptanCluster
HeadacheLongtermStudyGroup.Cephalalgia.199515:230236.
7. GobelH,LindnerV,HeinzeA,etal.Acutetherapyforclusterheadachewithsumatriptan:Findingsofaoneyearlongtermstudy.Neurology.199851:908
911.
8. vanVlietJA,BahraA,MartinV,etal.Intranasalsumatriptaninclusterheadache:Randomizedplacebocontrolleddoubleblindstudy.Neurology.200360:630
633.
9. HardeboJE,DahlofC.Sumatriptannasalspray(20mg/dose)intheacutetreatmentofclusterheadache.Cephalalgia.199818:487489.
10. GregorN,SchlesigerC,AkovaOzturkE,etal.Treatmentofclusterheadacheattackswithlessthan6mgsubcutaneoussumatriptan.Headache.2005
45:10691072.
11. CittadiniE,MayA,StraubeA,etal.Effectivenessofintranasalzolmitriptaninacuteclusterheadache:Arandomized,placebocontrolled,doubleblind
crossoverstudy.ArchNeurol.200663:15371542.
12. RapoportAM,MathewNT,SilbersteinSD,etal.Zolmitriptannasalsprayintheacutetreatmentofclusterheadache:Adoubleblindstudy.Neurology.
200769:821826.
13. BahraA,GawelMJ,HardeboJE,etal.Oralzolmitriptaniseffectiveintheacutetreatmentofclusterheadache.Neurology.200054:18321839.
14. DrummondPD,AnthonyM.Extracranialvascularresponsestosublingualnitroglycerinandoxygeninhalationinclusterheadachepatients.Headache.
198525:7074.
15. AkermanS,HollandPR,LasalandraMP,etal.Oxygeninhibitsneuronalactivationinthetrigeminocervicalcomplexafterstimulationoftrigeminalautonomic
reflex,butnotduringdirectduralactivationoftrigeminalafferents.Headache.200949:11311143.
16. BennettMH,FrenchC,SchnabelA,etal.Normobaricandhyperbaricoxygentherapyformigraineandclusterheadache.CochraneDatabaseSystRev.
20083:CD005219.
17. KudrowL.Responseofclusterheadacheattackstooxygeninhalation.Headache.198121:14.
18. FoganL.Treatmentofclusterheadache.Adoubleblindcomparisonofoxygenvairinhalation.ArchNeurol.198542:362363.
19. RozenTD.Highoxygenflowratesforclusterheadache.Neurology.200463:593.
20. CohenAS,BurnsB,andGoadsbyPJ.Highflowoxygenfortreatmentofclusterheadache:Arandomizedtrial.JAMA.2009302:24512457.
21. WeissLD,RamasastrySS,andEidelmanBH.Treatmentofaclusterheadachepatientinahyperbaricchamber.Headache.198929:109110.
22. DiSabatoF,FuscoBM,PelaiaP,etal.Hyperbaricoxygentherapyinclusterheadache.Pain.199352:243245.
23. NilssonRemahlAI,AnsjonR,LindF,etal.Hyperbaricoxygentreatmentofactiveclusterheadache:Adoubleblindplacebocontrolledcrossoverstudy.
Cephalalgia.200222:730739.
24. AnderssonPG,JespersenLT.Dihydroergotaminenasalsprayinthetreatmentofattacksofclusterheadache.Adoubleblindtrialversusplacebo.Cephalalgia.
19866:5154.
25. KittrelleJP,GrouseDS,SeyboldME.Clusterheadache.Localanestheticabortiveagents.ArchNeurol.198542:496498.
26. HardeboJE,ElnerA.Nervesandvesselsinthepterygopalatinefossaandsymptomsofclusterheadache.Headache.198727:528532.
27. RobbinsL.Intranasallidocaineforclusterheadache.Headache.199535:8384.
28. CostaA,PucciE,AntonaciF,etal.Theeffectofintranasalcocaineandlidocaineonnitroglycerininducedattacksinclusterheadache.Cephalalgia.
200020:8591.
29. SicuteriF,GeppettiP,MarabiniS,etal.Painreliefbysomatostatininattacksofclusterheadache.Pain.198418:359365.
30. MatharuMS,LevyMJ,MeeranK,etal.Subcutaneousoctreotideinclusterheadache:Randomizedplacebocontrolleddoubleblindcrossoverstudy.Ann
Neurol.200456:488494.
31. SchurksM,RosskopfD,deJesusJ,etal.Predictorsofacutetreatmentresponseamongpatientswithclusterheadache.Headache.200747:10791084.
32. GabaiIJ,SpieringsELH.Prophylactictreatmentofclusterheadachewithverapamil.Headache.198929:167168.
33. LeoneM,D'AmicoD,FredianiF,etal.Verapamilintheprophylaxisofepisodicclusterheadache:Adoubleblindstudyversusplacebo.Neurology.
200054:13821385.
34. BussoneG,LeoneM,PeccarisiC,etal.Doubleblindcomparisonoflithiumandverapamilinclusterheadacheprophylaxis.Headache.199030:411417.
35. TfeltHansenP,TfeltHansenJ.Verapamilforclusterheadache.Clinicalpharmacologyandpossiblemodeofaction.Headache.200949:117125.
36. BlauJN,EngelHO.Individualizingtreatmentwithverapamilforclusterheadachepatients.Headache.200444:10131018.
37. CohenAS,MatharuMS,andGoadsbyPJ.Electrocardiographicabnormalitiesinpatientswithclusterheadacheonverapamiltherapy.Neurology.2007
69:668675.
38. EkbomK.Lithiumforclusterheadache:Reviewoftheliteratureandpreliminaryresultsoflongtermtreatment.Headache.198121:132139.
39. SteinerTJ,HeringR,CouturierEGM,etal.Doubleblindplacebocontrolledtrialoflithiuminepisodicclusterheadache.Cephalalgia.199717:673675.
40. WheelerSD,CarrazanaEJ.Topiramatetreatedclusterheadache.Neurology.199953:234236.
41. PascualJ,LainezMJ,DodickD,etal.Antiepilepticdrugsforthetreatmentofchronicandepisodicclusterheadache:Areview.Headache.200747:8189.
42. MayA,LeoneM,AfraJ,etal.EFNSguidelinesonthetreatmentofclusterheadacheandothertrigeminalautonomiccephalalgias.EurJNeurol.
200613:10661077.
43. HeringR,KuritzkyA.Sodiumvalproateinthetreatmentofclusterheadache:Anopenclinicaltrial.Cephalalgia.19899:195198.
44. GallagherRM,MuellerLL,andFreitagFG.Divalproexsodiuminthetreatmentofmigraineandclusterheadaches.JAmOsteopathAssoc.2002102:9294.
45. ElAmraniM,MassiouH,andBousserMG.Anegativetrialofsodiumvalproateinclusterheadache:Methodologicalissues.Cephalalgia.200222:205208.
46. LeoneM,D'AmicoD,MoschianoF,etal.Melatoninversusplacebointheprophylaxisofclusterheadache:Adoubleblindpilotstudywithparallelgroups.
Cephalalgia.199616:494496.
47. LeandriM,LuzzaniM,CruccuG,etal.Drugresistantclusterheadacherespondingtogabapentin:Apilotstudy.Cephalalgia.200121:744746.
48. SchuhHoferS,IsraelH,NeebL,etal.Theuseofgabapentininchronicclusterheadachepatientsrefractorytofirstlinetherapy.EurJNeurol.200714:694
696.
49. HeringHanitR,GadothN.Baclofeninclusterheadache.Headache.200040:4851.
50. D'AndreaG,PeriniF,GranellaF,etal.Efficacyoftransdermalclonidineinshorttermtreatmentofclusterheadache:Apilotstudy.Cephalalgia.199515:430
433.
51. LeoneM,AttanasioA,GrazziL,etal.Transdermalclonidineintheprophylaxisofepisodicclusterheadache:Anopenstudy.Headache.199737:559560.
52. SostakP,KrauseP,ForderreutherS,etal.BotulinumtoxintypeAtherapyinclusterheadache:Anopenstudy.JHeadachePain.20078:236241.
53. CouchJRJr,andZieglerDK.Prednisonetherapyforclusterheadache.Headache.197818:219221.
54. KudrowL.Comparativeresultsofprednisone,methysergideandlithiumtherapyinclusterheadache.In:GreeneR,ed.CurrentConceptsinMigraine
Research.NewYork:RavenPress1978:159163.
55. JammesJL.Thetreatmentofclusterheadacheswithprednisone.DisNervSyst.197536:375376.
56. AntonaciF,CostaA,CandeloroE,etal.Singlehighdosesteroidtreatmentinepisodicclusterheadache.Cephalalgia.200525:290295.
57. MirP,AlbercaR,NavarroA,etal.Prophylactictreatmentofepisodicclusterheadachewithintravenousbolusofmethylprednisolone.NeurolSci.200324:318
321.
58. HalkerR,VargasB,andDodickDW.Clusterheadache:Diagnosisandtreatment.SeminNeurol.201030:175185.
59. LeoneM,FranziniA,CecchiniAP,etal.Clusterheadache:Pharmacologicaltreatmentandneurostimulation.NatClinPractNeurol.20095:153162.
60. MatherPJ,SilbersteinSD,SchulmanEA,etal.Thetreatmentofclusterheadachewithrepetitiveintravenousdihydroergotamine.Headache.199131:525
532.
61. EkbomK,HardeboJE.Clusterheadache:Aetiology,diagnosisandmanagement.Drugs.200262:6169.
62. AnthonyM.Arrestofattacksofclusterbylocalsteroidinjectionoftheoccipitalnerveclinicalandresearchadvances:Proceedingsofthe5thInternational
MigraineSymposium,London,September1920,1984.In:CliffordRoseF,ed.Migraine.Basel:Karger1985:169173.
63. PeresMF,StilesMA,SiowHC,etal.Greateroccipitalnerveblockadeforclusterheadache.Cephalalgia.200222:520522.
64. AmbrosiniA,VandenheedeM,RossiP,etal.Suboccipitalinjectionwithamixtureofrapidandlongactingsteroidsinclusterheadache:Adoubleblind
placebocontrolledstudy.Pain.2005118:9296.
65. AfridiSK,ShieldsKG,BholaR,etal.Greateroccipitalnerveinjectioninprimaryheadachesyndromesprolongedeffectsfromasingleinjection.Pain.
2006122:126129.
66. BuschV,JakobW,JuergensT,etal.Occipitalnerveblockadeinchronicclusterheadachepatientsandfunctionalconnectivitybetweentrigeminalandoccipital
nerves.Cephalalgia.200727:12061214.
67. FelisatiG,ArnoneF,LozzaP,etal.Sphenopalatineendoscopicganglionblock:Arevisionofatraditionaltechniqueforclusterheadache.Laryngoscope.
2006116:14471450.
68. MagisD,AllenaM,BollaM,etal.Occipitalnervestimulationfordrugresistantchronicclusterheadache:Aprospectivepilotstudy.LancetNeurol.20076:314
321.
69. BurnsB,WatkinsL,andGoadsbyPJ.Treatmentofmedicallyintractableclusterheadachebyoccipitalnervestimulation:Longtermfollowupofeightpatients.
Lancet.2007369:10991106.
70. BurnsB,WatkinsL,andGoadsbyPJ.Treatmentofintractablechronicclusterheadachebyoccipitalnervestimulationin14patients.Neurology.200972:341
345.
71. AnsariniaM,RezaiA,TepperSJ,etal.Electricalstimulationofsphenopalatineganglionforacutetreatmentofclusterheadaches.Headache.201050:1164
1174.
72. LeoneM,FranziniA,andBussoneG.Stereotacticstimulationofposteriorhypothalamicgraymatterinapatientwithintractableclusterheadache.NEnglJ
Med.2001345:14281429.
73. SchoenenJ,DiClementeL,VandenheedeM,etal.Hypothalamicstimulationinchronicclusterheadache:Apilotstudyofefficacyandmodeofaction.Brain.
2005128:940947.
74. LeoneM,FranziniA,BroggiG,etal.Hypothalamicstimulationforintractableclusterheadache:Longtermexperience.Neurology.200667:150152.
75. BartschT,PinskerMO,RascheD,etal.Hypothalamicdeepbrainstimulationforclusterheadache:Experiencefromanewmulticaseseries.Cephalalgia.
200828:285295.
76. LeoneM,FranziniA,BroggiG,etal.Acutehypothalamicstimulationandongoingclusterheadacheattacks.Neurology.200667:18441845.
77. LeoneM,ProiettiCA,FranziniA,etal.Lessonsfrom8years'experienceofhypothalamicstimulationinclusterheadache.Cephalalgia.200828:787797.
AbbreviationsAEsadverseeffects,CCHchronicclusterheadache,CHclusterheadache,DHEDihydroergotamine,ECHepisodicclusterheadache,GONgreater
occipitalnerve,HBOhyperbaricoxygen,HShypothalamicstimulation,NBOnormobaricoxygen,ONSoccipitalnervestimulation,SPGsphenopalatineganglion
ConflictofInterestNone
Headache.201151(2):272286.2011BlackwellPublishing
78. OnofrioBM,CampbellJK.Surgicaltreatmentofchronicclusterheadache.MayoClinProc.198661:537544.
79. MathewNT,HurtW.Percutaneousradiofrequencytrigeminalgangliorhizolysisinintractableclusterheadache.Headache.198828:328331.
80. JarrarRG,BlackDF,DodickDW,etal.Outcomeoftrigeminalnervesectioninthetreatmentofchronicclusterheadache.Neurology.200360:13601362.
81. LovelyTJ,KotsiakisX,andJannettaPJ.Thesurgicalmanagementofchronicclusterheadache.Headache.199838:590594.
82. FordRG,FordKT,SwaidS,etal.Gammaknifetreatmentofrefractoryclusterheadache.Headache.199838:39.
83. DonnetA,TamuraM,ValadeD,etal.Trigeminalnerveradiosurgicaltreatmentinintractablechronicclusterheadache:Unexpectedhightoxicity.Neurosurgery.
200659:12521257.
84. SandersM,ZuurmondWW.Efficacyofsphenopalatineganglionblockadein66patientssufferingfromclusterheadache:A12to70monthfollowup
evaluation.JNeurosurg.199787:876880.
85. NarouzeS,KapuralL,CasanovaJ,etal.Sphenopalatineganglionradiofrequencyablationforthemanagementofchronicclusterheadache.Headache.
200949:571577.
86. MatharuMS,GoadsbyPJ.Persistenceofattacksofclusterheadacheaftertrigeminalnerverootsection.Brain.2002125:976984.
87. BraininM,BarnesM,BaronJC,etal.GuidanceforthepreparationofneurologicalmanagementguidelinesbyEFNSscientifictaskforcesrevised
recommendations2004.EurJNeurol.200411:577581.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Neurology Question Bank 2015Документ99 страницNeurology Question Bank 2015Paz Vida100% (7)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Migraine in WomenДокумент10 страницMigraine in WomenInes StrenjaОценок пока нет
- Jurnal NurulДокумент50 страницJurnal NurulAPRILОценок пока нет
- Maju Jurnal MigrainДокумент7 страницMaju Jurnal MigrainRosyid PrasetyoОценок пока нет
- British J Pharmacology - 2021 - ZobdehДокумент20 страницBritish J Pharmacology - 2021 - ZobdehRenju KuriakoseОценок пока нет
- Adult Headache GuidelineДокумент7 страницAdult Headache GuidelineKhairunisaОценок пока нет
- Pharmacology of SerotoninДокумент52 страницыPharmacology of SerotoninSunilОценок пока нет
- Causes of Migraine PDFДокумент7 страницCauses of Migraine PDFJohn Christopher LucesОценок пока нет
- Drug Use During Pregnancy and LactationДокумент50 страницDrug Use During Pregnancy and LactationJuveria Fatima75% (4)
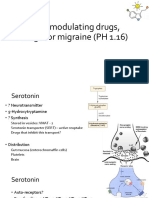
- 5-HT Modulating Drugs, Drugs For Migraine (PH 1.16)Документ13 страниц5-HT Modulating Drugs, Drugs For Migraine (PH 1.16)shruti sangwanОценок пока нет
- Migraine in Emergency Update DR Tanjim OveeДокумент2 страницыMigraine in Emergency Update DR Tanjim OveeAHMED TANJIMUL ISLAMОценок пока нет
- Cefaleia - ContinuumДокумент195 страницCefaleia - ContinuumRafaelОценок пока нет
- Adult Headache Pathway Patient Presents With HeadacheДокумент8 страницAdult Headache Pathway Patient Presents With HeadacheVIA RUSTIANIОценок пока нет
- Pharm - Chapter - 13 - Central Nervous System StimulantsДокумент42 страницыPharm - Chapter - 13 - Central Nervous System StimulantsFeliciaDorghamОценок пока нет
- Pain and Inflammation: (General Key Points)Документ38 страницPain and Inflammation: (General Key Points)susan2johnson-501300Оценок пока нет
- Neurological Deseases in PregnancyДокумент6 страницNeurological Deseases in PregnancyOdi KaiОценок пока нет
- Sign 155 Migraine 2022 v10 PDFДокумент58 страницSign 155 Migraine 2022 v10 PDFDeeОценок пока нет
- A Study of Migraine Characteristics in Joint Hypermobility Syndrome A.K.A. Ehlers-Danlos Syndrome, Hypermobility TypeДокумент11 страницA Study of Migraine Characteristics in Joint Hypermobility Syndrome A.K.A. Ehlers-Danlos Syndrome, Hypermobility TypeAndrea MorenoОценок пока нет
- FavotriptanДокумент12 страницFavotriptansandyriaaaОценок пока нет
- Shahdevinandar, JPHV 2241 PUBLISHДокумент6 страницShahdevinandar, JPHV 2241 PUBLISHGinanjar Putri SariОценок пока нет
- LEARNING MODULE IN NCM 106 Final Peroid 2Документ30 страницLEARNING MODULE IN NCM 106 Final Peroid 2Threcia RotaОценок пока нет
- Newer Formulations of The Triptans: Advances in Migraine ManagementДокумент21 страницаNewer Formulations of The Triptans: Advances in Migraine ManagementShivam BhadauriaОценок пока нет
- Peter Goadsby - Treatment of Cluster Headache PDFДокумент3 страницыPeter Goadsby - Treatment of Cluster Headache PDFharunОценок пока нет
- Practice Parameter: Evidence-Based Guidelines For Migraine Headache (An Evidence-Based Review)Документ10 страницPractice Parameter: Evidence-Based Guidelines For Migraine Headache (An Evidence-Based Review)Arifya Anggoro KasihОценок пока нет
- Migrraine Review 2017 NEJMДокумент9 страницMigrraine Review 2017 NEJManscstОценок пока нет
- Thesis Statement Heart DiseaseДокумент7 страницThesis Statement Heart Diseasexgkeiiygg100% (2)
- QB NeuroДокумент30 страницQB Neurorichard bolinaoОценок пока нет
- Jurnal SarafДокумент20 страницJurnal SarafAndreas NatanОценок пока нет
- Migraine and Risk of StrokeДокумент12 страницMigraine and Risk of StrokeGustavo PestanaОценок пока нет
- 11 875 670 Preparation and Utility of SuДокумент142 страницы11 875 670 Preparation and Utility of Suthathpurusha_5Оценок пока нет